ROS Signaling Mechanisms: From Molecular Foundations to Therapeutic Targeting in Disease
Reactive oxygen species (ROS) are central, dual-function regulators in cellular physiology, acting as crucial signaling molecules at low levels and as agents of oxidative damage at high concentrations.
ROS Signaling Mechanisms: From Molecular Foundations to Therapeutic Targeting in Disease
Abstract
Reactive oxygen species (ROS) are central, dual-function regulators in cellular physiology, acting as crucial signaling molecules at low levels and as agents of oxidative damage at high concentrations. This article provides a comprehensive analysis of ROS signaling mechanisms for researchers and drug development professionals. We explore the fundamental biology of specific ROS molecules and their homeostatic regulation, detail advanced methodological approaches for studying redox biology, address key challenges in targeting ROS for therapy, and critically evaluate emerging therapeutic strategies. By integrating foundational concepts with cutting-edge applications, this review aims to bridge molecular understanding with clinical translation in cancer, neurodegenerative, and metabolic diseases.
The Dual Nature of ROS: Molecular Identity, Homeostatic Control, and Physiological Signaling
Reactive oxygen species (ROS) are a collection of oxygen-containing, highly reactive molecules generated as byproducts of aerobic metabolism within cells [1] [2] [3]. In a biological context, ROS are pervasive due to their formation from abundant molecular oxygen (Oâ‚‚) and water [2]. These molecules are intrinsically involved in cellular functioning, existing at low, stationary levels in normal cells where they play crucial roles in signaling and homeostasis [4] [2]. The ROS spectrum encompasses both free radicals, which contain unpaired electrons, and non-radical oxidizing agents [1] [3]. The delicate balance between ROS production and elimination is critical for cellular health; disruption of this equilibrium can lead to oxidative stress, with significant implications for cell fate, disease progression, and therapeutic responses [1] [5].
The traditional view of ROS as merely toxic agents has evolved significantly. Contemporary research reveals that ROS function as important signaling molecules that regulate diverse biological processes, including inflammation, proliferation, and cell death [4] [3]. This dual nature of ROS—acting as both critical signaling molecules and potential toxic agents—forms the foundation of modern redox biology [4]. The specific roles and effects of ROS depend on factors such as concentration, cellular environment, duration of exposure, and subcellular localization [4] [3]. Understanding the distinct properties and behaviors of individual ROS species is thus essential for researchers and drug development professionals working in this field.
The Core ROS Spectrum: Chemical Properties and Relationships
Fundamental ROS Chemistry and Interconversion
The generation of reactive oxygen species occurs primarily through the sequential reduction of molecular oxygen in a series of one-electron transfer steps [3]. This process begins with the monovalent reduction of oxygen to form superoxide anion (•Oâ‚‚â»), which subsequently undergoes further reduction and protonation to yield hydrogen peroxide (Hâ‚‚Oâ‚‚), the hydroxyl radical (•OH), and finally water [3]. These three species—•Oâ‚‚â», Hâ‚‚Oâ‚‚, and •OH—represent the primary ROS in biological systems, with many other oxidants derived from these fundamental sources [3].
The interconversion between different ROS occurs through well-defined chemical reactions that are tightly regulated in biological systems. Superoxide dismutase (SOD) catalyzes the disproportionation (dismutation) of •Oâ‚‚â» to form Hâ‚‚Oâ‚‚ and Oâ‚‚ [1] [2]. The highly reactive hydroxyl radical is generated primarily through the Fenton reaction, where Hâ‚‚O2 reacts with ferrous (Fe²âº) or cuprous ions, and through the Haber-Weiss reaction, which involves •Oâ‚‚â» and Hâ‚‚O2 [1] [4] [3]. Additionally, •Oâ‚‚â» can react with nitric oxide (•NO) to form peroxynitrite (ONOOâ»), a reactive nitrogen species that contributes significantly to oxidative damage [1] [3].
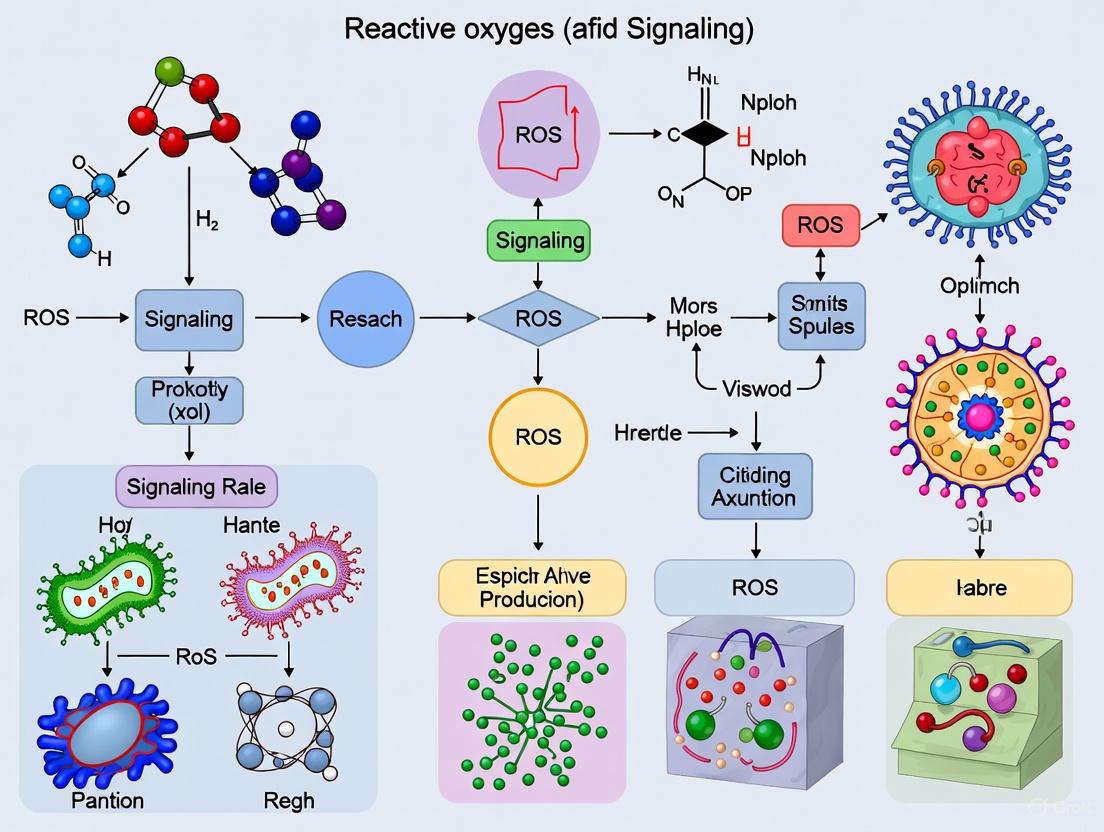
Figure 1: ROS Interconversion Pathways and Key Enzymatic Controls. This diagram illustrates the primary chemical pathways for ROS generation and elimination, highlighting the central role of antioxidant enzymes like superoxide dismutase (SOD), catalase (CAT), and glutathione peroxidase (GPx).
Comprehensive Inventory of ROS Molecules
The ROS spectrum includes diverse chemical species with varying reactivity, lifespan, and biological targets. Table 1 provides a systematic overview of the core ROS molecules, their chemical properties, and primary characteristics relevant to biological systems.
Table 1: Comprehensive Inventory of Reactive Oxygen Species (ROS)
| ROS Species | Chemical Formula | Type | Reactivity | Half-Life | Major Sources | Key Characteristics |
|---|---|---|---|---|---|---|
| Superoxide anion | •O₂⻠| Free radical | Moderate | 1-5 μs | Mitochondrial ETC (Complex I, III), NOX enzymes | Primary ROS; membrane-impermeable; precursor to other ROS; inactivates Fe-S cluster proteins [1] [4] [5] |
| Hydrogen peroxide | Hâ‚‚Oâ‚‚ | Non-radical | Low-moderate | ~1 ms | SOD activity, NOX enzymes, peroxisomes | Membrane-permeable; key signaling molecule; oxidizes cysteine residues in proteins [1] [4] [5] |
| Hydroxyl radical | •OH | Free radical | Extremely high | ~1 ns | Fenton reaction, Haber-Weiss reaction | Most potent oxidant; non-selective; reacts instantaneously with all biomolecules [1] [4] [3] |
| Hydroperoxyl radical | HO₂• | Free radical | High | - | Protonation of •O₂⻠| Protonated form of superoxide; more lipid-soluble; contributes to lipid peroxidation [1] |
| Peroxyl radicals | RO₂• | Free radical | High | ms-range | Lipid peroxidation chain reactions | Propagate lipid peroxidation; relatively stable and diffusible; oxidize proteins and DNA [1] |
| Alkoxyl radicals | RO• | Free radical | High | - | Decomposition of RO₂• | Formed during lipid metabolism; abstract hydrogen atoms from biomolecules [1] |
| Carbonate radical anion | CO₃•⻠| Free radical | High | - | Reaction of CO₂ with peroxynitrite | Efficiently oxidizes guanine in DNA; generated in physiological environments [1] |
| Singlet oxygen | ¹O₂ | Non-radical | High | ~1 μs | Photosensitization, chlorophyll | Electronically excited state of oxygen; highly reactive with unsaturated compounds [6] [2] |
| Ozone | O₃ | Non-radical | High | - | Atmospheric pollutant | Strong oxidizing agent; included in broader ROS definitions [1] |
| Hypochlorous acid | HOCl | Non-radical | High | - | Myeloperoxidase (MPO) activity | Powerful antimicrobial; oxidizes proteins, DNA, and lipids [1] [3] |
The reactivity of different ROS varies dramatically, spanning approximately nine orders of magnitude from the highly selective and relatively stable H₂O₂ to the extremely reactive and non-selective •OH [5]. This diversity in chemical behavior directly influences their biological roles, with less reactive species like H₂O₂ functioning effectively as signaling molecules due to their ability to diffuse and react selectively with specific cellular targets, while highly reactive species like •OH primarily cause oxidative damage [4] [5].
Endogenous ROS Generation Sites
Cellular ROS originate from multiple subcellular compartments, with the mitochondrial electron transport chain and NADPH oxidase (NOX) enzymes representing the most significant sources [1] [3]. Mitochondria generate ROS primarily at Complex I (NADH-ubiquinone oxidoreductase) and Complex III (ubiquinol-cytochrome c oxidoreductase) of the respiratory chain, where electron leakage to oxygen results in •O₂⻠formation [2] [3]. Under normal physiological conditions, approximately 0.1-2% of electrons passing through the transport chain contribute to ROS generation, though this percentage can increase dramatically during mitochondrial dysfunction or under stress conditions [2].
NADPH oxidase (NOX) enzymes represent another major source of cellular ROS, with these transmembrane enzymes specifically dedicated to ROS production [1] [4]. NOX enzymes utilize NADPH to reduce oxygen, directly producing H₂O₂ (as in the case of NOX4, DUOX1/2) or indirectly via •O₂⻠generation (NOX1-3) [1]. Unlike mitochondrial ROS production, which occurs as a byproduct of energy metabolism, NOX-derived ROS function primarily in signaling and defense mechanisms [4].
Additional intracellular ROS sources include the endoplasmic reticulum, where protein folding generates oxidative conditions; peroxisomes, which contain various oxidases; and cytochrome P450 systems involved in detoxification and steroid synthesis [1] [3]. Uncoupling of nitric oxide synthase (NOS), xanthine oxidase activity, and cyclooxygenases also contribute to the cellular ROS pool [3].
Experimental Systems for Controlled ROS Generation
For rigorous investigation of ROS effects and signaling pathways, researchers employ specific experimental systems to generate particular ROS species in a controlled manner. Table 2 outlines established methodologies for selective ROS generation in biological research contexts.
Table 2: Experimental Approaches for Selective ROS Generation in Research
| Target ROS | Experimental Approach | Mechanism | Key Considerations |
|---|---|---|---|
| Superoxide (•Oâ‚‚â») | Paraquat (PQ) or quinones | Redox cycling compounds that generate •Oâ‚‚â» | Increases both •Oâ‚‚â» and Hâ‚‚Oâ‚‚ (via dismutation); specific concentrations required for controlled generation [5] |
| Superoxide (•Oâ‚‚â») in mitochondria | MitoPQ | Mitochondria-targeted analog of paraquat | Generates •Oâ‚‚â» within mitochondria; allows compartment-specific investigation [5] |
| Hydrogen peroxide (Hâ‚‚Oâ‚‚) | Glucose oxidase | Enzyme that generates Hâ‚‚Oâ‚‚ while oxidizing glucose | Direct Hâ‚‚Oâ‚‚ production; flux can be regulated by glucose concentration [5] |
| Hydrogen peroxide (Hâ‚‚Oâ‚‚) in specific cellular compartments | d-amino acid oxidase (DAAO) expression | Genetically expressed enzyme generates Hâ‚‚Oâ‚‚ when provided with d-amino acids | Compartment-targeted expression possible; flux regulated by d-alanine concentration; enables spatiotemporal control [5] |
| Superoxide/Hydrogen peroxide | NADPH oxidase (NOX) activation/modulation | Physiological activation or genetic manipulation of NOX enzymes | Specific inhibitors or genetic deletion/knockdown of NOX components recommended for validation [5] |
These controlled generation systems enable researchers to establish causal relationships between specific ROS and biological outcomes, moving beyond correlative observations. The use of compartment-specific ROS generation is particularly valuable for investigating spatially restricted signaling events [5].
ROS Signaling Mechanisms and Molecular Targets
Redox-Sensitive Protein Modifications
ROS function as signaling molecules primarily through the reversible oxidation of specific amino acid residues in proteins, particularly cysteine and methionine [4] [7]. These oxidative post-translational modifications (Oxi-PTMs) serve as molecular switches that regulate protein function, localization, and interactions [7]. Cysteine residues exist as thiolate anions (Cys-Sâ») at physiological pH, making them particularly susceptible to oxidation by Hâ‚‚Oâ‚‚ to form sulfenic acid (Cys-SOH) [4]. This primary oxidation product can undergo further reversible modifications, including the formation of disulfide bonds (S-S), S-glutathionylation (SSG), and S-nitrosylation (SNO) [8] [7].
These oxidative modifications induce allosteric changes in protein structure that alter function, with the modifications being reversed by cellular reductase systems such as thioredoxin (Trx) and glutaredoxin (Grx) [4]. This reversible oxidation represents a fundamental mechanism of redox signaling that regulates diverse cellular processes, including proliferation, differentiation, and stress responses [4] [8]. At higher concentrations, further oxidation to sulfinic (Cys-SO₂H) and sulfonic (Cys-SO₃H) acids can occur, which may be irreversible and result in permanent protein damage, representing the transition from redox signaling to oxidative stress [4].
Specific Signaling Pathways Regulated by ROS
ROS, particularly Hâ‚‚Oâ‚‚, regulate several key signaling pathways central to cellular physiology and pathology. Growth factor signaling represents a well-characterized example, where receptor tyrosine kinase (RTK) activation by epidermal growth factor (EGF) or platelet-derived growth factor (PDGF) stimulates ROS production through NADPH oxidases [4]. The resulting Hâ‚‚Oâ‚‚ transiently oxidizes and inactivates protein tyrosine phosphatases (PTPs) such as PTP1B and PTEN by modifying their catalytic cysteine residues, thereby prolonging tyrosine phosphorylation and enhancing mitogenic signaling [4]. This precise spatial and temporal regulation is achieved through localized inactivation of peroxiredoxin I (PRXI) at cell membranes upon growth factor stimulation, allowing controlled Hâ‚‚Oâ‚‚ accumulation in specific microdomains [4].
In cancer biology, oncogenic transformation often involves hijacking these normal ROS signaling mechanisms. Cancer cells driven by oncogenes such as MYC and KRAS demonstrate dependence on both mitochondrial and NOX-derived ROS for proliferation, with antioxidant treatments or ROS inhibition suppressing tumorigenic signaling pathways [4]. The transcription factor NF-κB represents another important redox-sensitive signaling node, with ROS activating this pathway to promote cell survival in many tumor contexts [4].
Figure 2: ROS-Mediated Growth Factor Signaling Pathway. This diagram illustrates how hydrogen peroxide (Hâ‚‚Oâ‚‚) functions as a secondary messenger in growth factor signaling by reversibly inactivating protein tyrosine phosphatases (PTPs) and PTEN, thereby enhancing proliferative signaling pathways. The system is reset by reductase enzymes like thioredoxin.
Methodologies for ROS Measurement and Detection
Guidelines for Specific ROS Detection
Accurate measurement of specific ROS presents significant technical challenges due to their reactive nature, short half-lives, and low physiological concentrations. The field has established that different ROS require distinct detection approaches, and reliance on non-specific commercial "ROS detection kits" can yield misleading results [5]. Proper experimental design requires consideration of the specific chemical properties, reactivity, and biological context of the ROS being studied [5].
Electron paramagnetic resonance (EPR) spectroscopy, also known as electron spin resonance (ESR), represents one of the most specific methods for direct detection of radical species, particularly when used with spin traps that form stable adducts with short-lived radicals [5]. However, this technique requires specialized instrumentation and expertise. Fluorescent and luminescent probes offer more accessible alternatives but vary significantly in their specificity [5]. For example, dichloro-dihydro-fluorescein diacetate (DCFH-DA) and related probes are widely used but lack specificity for particular ROS and are subject to numerous artefacts, while more specific probes like Amplex Red for H₂O₂ or hydroxyphenyl fluorescein (HPF) for •OH provide better selectivity [5].
A critical principle in ROS measurement is that most probes capture only a small percentage of the ROS generated, and this percentage must remain relatively constant across different experimental conditions to allow valid comparisons [5]. Furthermore, researchers should recognize that complete scavenging of highly reactive species like •OH is chemically implausible in biological systems due to their nearly instantaneous reaction with biomolecules, making interpretations based solely on "•OH scavengers" problematic [5].
Assessment of Oxidative Damage Biomarkers
When direct ROS measurement proves challenging, researchers often quantify stable products of oxidative damage as biomarkers for ROS activity. The most common biomarkers include products of lipid peroxidation such as malondialdehyde (MDA) and 4-hydroxy-2-nonenal (4-HNE), which can be measured by thiobarbituric acid reactive substances (TBARS) assays or more specific chromatographic methods [1] [3]. Protein carbonylation represents another well-established marker of oxidative protein damage, typically detected through derivatization with 2,4-dinitrophenylhydrazine (DNPH) followed by immunoblotting or spectrophotometric analysis [5].
For DNA damage assessment, measurement of 8-hydroxy-2'-deoxyguanosine (8-OHdG) provides a specific marker of oxidative DNA lesions, typically quantified using HPLC with electrochemical detection or immunoassays [5]. Importantly, the measured level of any oxidative damage biomarker represents the net balance between its rate of production and its removal by cellular repair, degradation, and excretion mechanisms [5]. Therefore, changes in biomarker levels could reflect alterations in either production or clearance pathways.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for ROS Studies
| Reagent/Category | Specific Examples | Primary Function | Important Considerations |
|---|---|---|---|
| ROS Generators | Paraquat, MitoPQ | Selective •Oâ‚‚â» generation | Paraquat for general •Oâ‚‚â»; MitoPQ for mitochondrial-specific generation [5] |
| d-amino acid oxidase (DAAO) expression systems | Controlled Hâ‚‚Oâ‚‚ generation in specific compartments | Allows spatiotemporal control with d-alanine substrate [5] | |
| ROS Scavengers/Modulators | N-acetylcysteine (NAC) | Increases cellular cysteine and glutathione levels | Often misinterpreted as direct ROS scavenger; has multiple mechanisms including Hâ‚‚S generation [4] [5] |
| TEMPO/TEMPOL, mito-TEMPO | Redox modulators | Complex redox reactions; better described as redox modulators than specific antioxidants [5] | |
| Superoxide dismutase (SOD) mimetics | Catalyze •O₂⻠dismutation to H₂O₂ | Porphyrin-based compounds; validate specificity [5] | |
| Enzyme Inhibitors | NOX inhibitors (specific) | Inhibit NADPH oxidase activity | Use genetically validated inhibitors; avoid non-specific agents like apocynin and diphenyleneiodonium as sole evidence [5] |
| Detection Reagents | Amplex Red | Specific Hâ‚‚Oâ‚‚ detection | Fluorimetric detection of Hâ‚‚Oâ‚‚ via horseradish peroxidase-coupled reaction [5] |
| Hydroethidine (Dihydroethidium) | •O₂⻠detection | Specificity depends on separation and detection of 2-hydroxyethidium product [5] | |
| Spin traps (DMPO, DEPMPO) | EPR detection of radical species | Form stable adducts with short-lived radicals for EPR detection [5] | |
| Daraxonrasib | Daraxonrasib, CAS:2765081-21-6, MF:C44H58N8O5S, MW:811.0 g/mol | Chemical Reagent | Bench Chemicals |
| MB-0223 | MB-0223, MF:C26H27N5OS, MW:457.6 g/mol | Chemical Reagent | Bench Chemicals |
This toolkit provides researchers with essential reagents for manipulating and measuring ROS in experimental systems, though appropriate controls and validation are always necessary when interpreting results.
The ROS spectrum encompasses a diverse array of chemical species with distinct properties and biological activities. From the relatively stable signaling molecule H₂O₂ to the highly destructive hydroxyl radical, each ROS species plays specific roles in cellular physiology and pathology. Understanding these differences is fundamental to advancing redox biology research and developing targeted therapeutic approaches. The experimental frameworks and methodologies outlined in this technical guide provide researchers with essential tools for rigorous investigation of ROS in biological systems, with appropriate attention to the chemical specificity and technical considerations required for meaningful results. As the field continues to evolve, recognition of the dual nature of ROS—as both essential signaling molecules and potential agents of damage—will remain central to unraveling their complex roles in health and disease.
Reactive oxygen species (ROS) function as crucial signaling molecules in physiological processes, yet their overproduction leads to oxidative stress and cellular damage. Understanding the precise sources and generation mechanisms of ROS is fundamental to elucidating their dual role in health and disease. This whitepaper provides an in-depth technical analysis of three major cellular ROS sources: the mitochondrial electron transport chain (ETC), NADPH oxidase (NOX) enzymes, and the endoplasmic reticulum (ER). Within the broader context of ROS signaling mechanisms research, we detail the molecular architecture of each system, quantitative ROS production data, and advanced experimental methodologies for their study, providing a resource for researchers and drug development professionals targeting redox-based therapeutics.
Mitochondrial Electron Transport Chain
Structural Organization and ROS Generation Sites
The mitochondrial ETC is a primary source of endogenous ROS, comprising complexes I-IV alongside mobile electron carriers ubiquinone and cytochrome c. The complexes assemble into supercomplexes with specific configurations to function properly [9]. Electron flow through the ETC is coupled to proton pumping across the inner mitochondrial membrane, generating the proton motive force used by ATP synthase (Complex V) for ATP production [9].
During electron transfer, a small percentage of electrons directly leak to oxygen, generating superoxide anions (O₂•â») at specific sites within the ETC. Table 1 summarizes the characterized ROS generation sites within the ETC supercomplex.
Table 1: Mitochondrial ETC ROS Generation Sites
| Complex | ROS Generation Site | Substrate/Pathway | Primary ROS Product |
|---|---|---|---|
| Complex I | Site IF (Flavin mononucleotide) | NADH oxidation | O₂•⻠[9] |
| Complex I | Site IQ (Ubiquinone binding site) | Reverse electron transport from CoQ pool | O₂•⻠[9] [10] |
| Complex II | Site IIF (Flavin adenine dinucleotide) | Succinate oxidation | O₂•⻠[9] [10] |
| Complex III | Site IIIQo (Ubiquinol oxidation site) | Q-cycle during ubiquinol oxidation | O₂•⻠[9] |
The electron transfer process begins at Complex I (CI, NADH-ubiquinone oxidoreductase), which accepts electrons from NADH. The L-shaped eukaryotic CI contains a matrix arm with an FMN cofactor and multiple iron-sulfur (Fe-S) clusters, and a membrane arm with seven hydrophobic subunits [9]. Electrons from NADH reduce FMN to FMNHâ‚‚, then pass through a chain of Fe-S clusters before reducing ubiquinone to ubiquinol. The major ROS generation site in CI is the FMN cofactor (Site IF), particularly when the electron transport is slow and the flavin semiquinone state reacts with Oâ‚‚. Additionally, the ubiquinone binding site (Site IQ) can generate significant ROS, especially during reverse electron transport from a highly reduced ubiquinone pool [9].
Complex II (CII, succinate dehydrogenase) directly links the TCA cycle to the ETC, catalyzing succinate oxidation to fumarate. Its four subunits include a flavoprotein with FAD and three Fe-S clusters. Electrons from succinate reduce FAD to FADHâ‚‚, then pass through the Fe-S clusters to reduce ubiquinone. ROS (O₂•â») is generated primarily at the FAD site (Site IIF) [9].
In Complex III (CIII, cytochrome bc₠complex), the Q-cycle mechanism for ubiquinol oxidation creates a stabilized ubisemiquinone radical intermediate at the Qo site (Site IIIQo), which can directly reduce O₂ to O₂•⻠[9]. This site represents a significant source of mitochondrial ROS.
Regulatory Mechanisms and Physiological Significance
Mitochondrial ROS production is tightly regulated. A key mechanism is proton leak, which dissipates the proton gradient and reduces the driving force for ROS generation. This leak comprises basal proton leak and induced proton leak regulated by uncoupling proteins (UCP1-5) [9] [10]. UCP1 mediates non-shivering thermogenesis, while UCP2-5 primarily function to reduce oxidative stress and exert cytoprotective effects [9]. All diseases involving oxidative stress are associated with UCPs, highlighting their therapeutic relevance [10].
The following diagram illustrates the primary ROS generation sites within the mitochondrial ETC and their connectivity.
NADPH Oxidase (NOX) Enzyme Family
NOX Isoforms and Molecular Mechanisms
The NADPH oxidase (NOX) family comprises seven transmembrane enzymes (NOX1-5, DUOX1-2) dedicated to regulated, non-mitochondrial ROS generation. Unlike mitochondrial ROS production, which is a byproduct of metabolism, NOX enzymes are professional ROS producers, primarily generating superoxide anion (O₂•â») or hydrogen peroxide (Hâ‚‚Oâ‚‚) [11] [12]. Their core function is electron transfer from cytosolic NADPH across the membrane to molecular oxygen.
Table 2 outlines the key characteristics of human NOX isoforms, highlighting their tissue distribution, required regulatory components, and primary ROS products.
Table 2: Human NADPH Oxidase (NOX) Family Isoforms
| Isoform | Tissue Distribution | Regulatory Components | Primary ROS Product | Physiological & Pathological Roles |
|---|---|---|---|---|
| NOX1 | Colon, Vascularure | NOXO1, NOXA1, Rac | O₂•⻠| Host defense, vascular pathology [11] |
| NOX2 | Phagocytes, Endothelium | p47phox, p67phox, p40phox, Rac | O₂•⻠| Microbial killing, inflammation [11] |
| NOX3 | Inner Ear | p47phox, NOXO1 | O₂•⻠| Vestibular development [11] |
| NOX4 | Kidney, Vascularure | p22phox | Hâ‚‚Oâ‚‚ | Oxygen sensing, fibrosis, cancer [11] [13] |
| NOX5 | Spleen, Testis | Ca²⺠| O₂•⻠| Cell proliferation, angiogenesis [11] |
| DUOX1/2 | Thyroid, Lung | DUOXA1/2, Ca²⺠| H₂O₂ | Thyroid hormone synthesis, innate immunity [11] |
The catalytic core of a NOX enzyme typically consists of a transmembrane heterodimer (NOX/p22phox). The activation mechanisms vary by isoform. For example, NOX2, the prototype first identified in phagocytes, requires the assembly of cytosolic regulatory subunits (p47phox, p67phox, p40phox, and Rac GTPase) at the membrane for activation upon infection [11]. In contrast, NOX4 is constitutively active, primarily produces Hâ‚‚Oâ‚‚ due to its extracellular dehydrogenase domain, and requires only p22phox for stability and activity [11] [13]. NOX4 is also uniquely associated with the endoplasmic reticulum and other organelles [13].
NOX Enzymes as Therapeutic Targets in Disease
Dysregulation of NOX-derived ROS is implicated in the pathogenesis of atherosclerosis, hypertension, diabetic nephropathy, cancer, and neurodegenerative diseases [11] [12]. Consequently, NOX enzymes represent promising therapeutic targets. The development of isoenzyme-selective inhibitors is a critical focus, as broad-spectrum antioxidants have shown limited clinical efficacy and potential off-target effects [12]. Recent efforts have utilized in silico screening and high-throughput assays to identify selective inhibitors that target the active site of NOX enzymes, showing promise in pre-clinical cancer models, particularly in combination with KRAS modulators [12].
The diagram below depicts the general activation mechanism of a prototypical NOX complex, NOX2.
Endoplasmic Reticulum
Protein Folding, ER Stress, and ROS Generation
The endoplasmic reticulum is a central hub for protein synthesis, folding, and post-translational modification. The oxidative environment of the ER lumen is optimized for disulfide bond formation, a critical step in the maturation of secretory and membrane proteins. This process is a major source of ROS within the ER [13] [14].
The enzyme protein disulfide isomerase (PDI) catalyzes disulfide bond formation and isomerization in substrate proteins. During this reaction, PDI becomes reduced. To regenerate active, oxidized PDI, electrons are transferred via endoplasmic reticulum oxidoreductin 1 (ERO1) to molecular oxygen (Oâ‚‚), which acts as the final electron acceptor, thereby generating Hâ‚‚Oâ‚‚ as a byproduct [13]. It is estimated that approximately 25% of total cellular ROS are generated by disulfide bond formation in the ER during oxidative protein folding [13].
An imbalance between the protein-folding load and the ER's capacity leads to ER stress, triggering the unfolded protein response (UPR). The UPR is orchestrated by three main ER transmembrane sensors: IRE1α, PERK, and ATF6. Under severe or prolonged ER stress that cannot be resolved, the UPR switches from pro-survival to pro-apoptotic signaling [13] [14].
NOX4 and Calcium-Mediated ROS in the ER
Beyond protein folding, the ER hosts other ROS-generating systems. NADPH oxidase 4 (NOX4) is localized to the ER, among other organelles [13]. NOX4 constitutively produces Hâ‚‚Oâ‚‚ and its expression is upregulated during ER stress, contributing to the overall ROS load and influencing both pro-adaptive and pro-apoptotic UPR signaling [13]. For instance, NOX4-derived ROS can promote autophagy as a protective mechanism, but can also lead to apoptosis if the stress is severe [13].
Furthermore, ER stress can disrupt calcium (Ca²âº) homeostasis, leading to the release of Ca²⺠into the cytosol. This Ca²⺠can be taken up by mitochondria, stimulating mitochondrial ROS production and creating a damaging cycle of oxidative stress between the two organelles [14].
The interconnected pathways of ER stress and ROS generation are summarized in the diagram below.
The Scientist's Toolkit: Key Research Reagents and Methodologies
Quantitative ROS Measurement: Electron Paramagnetic Resonance (EPR)
Direct measurement of highly reactive and short-lived ROS is methodologically challenging. Electron Paramagnetic Resonance (EPR) spectroscopy, coupled with spin traps, is considered the gold standard for direct, quantitative detection of radical species like O₂•⻠in biological samples [15]. This technique provides an "instantaneous" snapshot of ROS production, unlike indirect methods that measure accumulated oxidative damage.
A validated microinvasive protocol involves collecting 50 μL of human capillary blood in heparinized tubes. The blood sample is immediately mixed with a spin trap molecule (e.g., CMH: 1-hydroxy-3-methoxycarbonyl-2,2,5,5-tetramethylpyrrolidine) [15]. The spin trap reacts with short-lived radicals to form stable, EPR-detectable adducts. The EPR spectrum is recorded, and the signal amplitude is proportional to the absolute concentration of ROS in the blood sample. This method has demonstrated a significant linear relationship (R² = 0.95) between ROS measured in capillary and venous blood, validating its reliability for clinical and research applications [15].
Experimental Protocol for Assessing NOX Inhibition
The development of specific NOX inhibitors is a key therapeutic endeavor. The following protocol outlines a combined in silico and experimental approach for identifying and validating NOX inhibitors, as described in recent research [12].
- In Silico Screening: Perform a virtual high-throughput screen of compound libraries against the crystal structure of the dehydrogenase (DH) domain of a NOX isoform (e.g., csNOX5). Docking simulations predict compounds that potentially occupy the NADPH-binding active site.
- In Vitro Enzymatic Assay: Validate hits using a cell-free system. Recombinantly express and purify the NOX DH domain. Measure the inhibitor's effect on the enzyme's ability to catalyze the reduction of an electron acceptor (e.g., cytochrome c or ferricyanide) in the presence of NADPH. A decrease in the reduction rate indicates inhibition.
- Binding Validation (Cellular Thermal Shift Assay - CETSA): Confirm direct binding in a cellular context. Treat cells expressing the target NOX with the inhibitor or vehicle control. Heat the cell lysates across a range of temperatures. The binding of a ligand stabilizes the protein, shifting its denaturation curve. This stabilization can be detected by immunoblotting, confirming target engagement within the complex cellular environment [12].
- In Cellulo ROS Measurement: Assess the functional consequence of inhibition in living cells. Use a cell-permeable, ROS-sensitive fluorescent probe (e.g., DCFH-DA or Amplex Red) in a high-throughput plate reader format. Treat various cancer cell lines with the inhibitor and measure the reduction in fluorescence, which corresponds to a decrease in cellular ROS production. This step also assesses selectivity and synergy with other drugs (e.g., KRAS modulators) [12].
Research Reagent Solutions
Table 3: Essential Reagents for ROS Source Research
| Reagent / Assay | Function / Target | Specific Example / Note |
|---|---|---|
| Spin Traps (e.g., CMH) | EPR: Forms stable adducts with O₂•⻠for direct detection | Used in microinvasive blood ROS measurement [15] |
| ROS-Sensitive Fluorescent Probes | General & In Cellulo: Becomes fluorescent upon oxidation | DCFH-DA (general ROS), Amplex Red (Hâ‚‚Oâ‚‚) [12] |
| Isozyme-Selective NOX Inhibitors | Pharmacology: Inhibits specific NOX isoforms; therapeutic potential | Identified via in silico screening of NOX5 active site [12] |
| CETSA (Cellular Thermal Shift Assay) | Target Engagement: Confirms drug binding to target protein in cells | Validates direct interaction between inhibitor and NOX [12] |
| Antibody for Nox4 | Localization/Expression: Detects endogenous NOX4 protein | First monoclonal antibody for Nox4 localized it to plasma membrane & ER [13] |
| ETF (Electron Transfer Flavoenzyme) | Model System: Study of flavoprotein magnetic field sensing & ROS | Recombinant human ETF used to study ROS partitioning (O₂•⻠vs H₂O₂) [16] |
| FPFT-2216 | FPFT-2216, MF:C12H12N4O3S, MW:292.32 g/mol | Chemical Reagent |
| 10-Deacetyl-7-xylosyl Paclitaxel | 10-Deacetyl-7-xylosyl Paclitaxel, MF:C50H57NO17, MW:944.0 g/mol | Chemical Reagent |
The mitochondrial ETC, NOX enzymes, and endoplasmic reticulum represent three structurally and functionally distinct cellular systems that collectively govern the delicate balance of ROS signaling and oxidative stress. The ETC generates ROS as a byproduct of aerobic metabolism, NOX enzymes produce ROS in a highly regulated manner for signaling and host defense, and the ER contributes to the ROS pool primarily through its oxidative protein folding machinery. Advanced techniques like EPR and the development of isozyme-specific inhibitors are refining our ability to dissect the contributions of these sources. A deep, mechanistic understanding of these systems is paramount for developing targeted therapeutic strategies aimed at manipulating redox pathways in a wide spectrum of human diseases, from cancer and neurodegeneration to metabolic and inflammatory disorders.
Reactive oxygen species (ROS) function as critical signaling molecules at physiological levels but induce oxidative damage and pathology at elevated concentrations. Antioxidant defense systems maintain this delicate balance through an integrated network of enzymatic and non-enzymatic components. This whitepaper provides a technical overview of these systems, focusing on the core enzymatic antioxidants—superoxide dismutase (SOD), catalase (CAT), and glutathione peroxidase (GPx)—and their coordination with non-enzymatic networks. Designed for researchers and drug development professionals, this guide includes summarized quantitative data, detailed experimental methodologies, and visualizations of key signaling pathways to support advanced research in redox biology and therapeutic development.
Reactive oxygen species are inevitable byproducts of aerobic metabolism, originating primarily from the mitochondrial electron transport chain and enzymatic systems like NADPH oxidases (NOX) [3] [4]. ROS include a range of molecules, such as the superoxide anion (O₂•â»), hydrogen peroxide (Hâ‚‚Oâ‚‚), and the highly reactive hydroxyl radical (•OH) [3] [17]. The biological role of ROS is fundamentally dualistic. At low, physiological levels, particularly Hâ‚‚Oâ‚‚, they act as crucial second messengers in redox signaling, regulating processes like proliferation, inflammation, and immune response through the reversible oxidation of cysteine residues in target proteins such as protein tyrosine phosphatases [4] [8]. However, when ROS generation overwhelms cellular detoxification capacity—a state known as oxidative stress—they cause indiscriminate damage to lipids, proteins, and DNA, contributing to aging, neurodegeneration, and cancer [3] [4] [8].
The antioxidant defense system exists to manage this delicate equilibrium, ensuring redox homeostasis. This network is not a simple scavenger but a sophisticated, multi-layered system. The first line of defense is composed of powerful enzymes like SOD, CAT, and GPx, which work in concert to directly neutralize specific ROS [18] [8] [19]. This enzymatic effort is supported by a second line of non-enzymatic antioxidants, including the glutathione (GSH) and thioredoxin systems, which help recycle oxidized cellular components and provide reducing power [8] [20]. Understanding the structure, function, and regulation of these components, particularly the core enzymatic antioxidants, is essential for developing therapeutic strategies against a myriad of oxidative stress-related diseases.
Core Enzymatic Antioxidants
The first line of defense comprises metalloenzymes that catalytically neutralize primary ROS. Their activity is compartmentalized, inducible, and essential for mitigating the chain-propagation of oxidative damage.
Superoxide Dismutase
SODs are a family of enzymes that catalyze the dismutation (or partitioning) of two superoxide anions into hydrogen peroxide and molecular oxygen. This reaction occurs at an extremely fast rate, close to the diffusion limit, and is the primary defense against O₂•⻠[19].
Table 1: Types and Properties of Superoxide Dismutase (SOD)
| Type / Acronym | Metal Cofactors | Subcellular Localization | Key Structural Features | Primary Function |
|---|---|---|---|---|
| SOD1 (Cu/Zn-SOD) | Cu²⺠(catalytic), Zn²⺠(structural) | Cytoplasm, nucleus, mitochondrial intermembrane space [19] | 32 kDa homodimer; electrostatic loop guides O₂•⻠to active site [19] | First defense against cytosolic O₂•â»; major intracellular SOD [18] [19] |
| SOD2 (Mn-SOD) | Mn³⺠(catalytic) | Mitochondrial matrix [19] | 96 kDa homotetramer; synthesized with a mitochondrial targeting signal [19] | Scavenges O₂•⻠generated by the electron transport chain [3] [19] |
| SOD3 (EC-SOD) | Cu²⺠(catalytic), Zn²⺠(structural) | Extracellular matrix, cell surfaces, extracellular fluids [19] | 135 kDa homotetramer; binds to heparan sulfate proteoglycans [19] | Maintains redox balance in extracellular space; regulates signaling [19] |
SOD activity is critical for preventing the formation of peroxynitrite (ONOOâ»), a highly damaging reactive nitrogen species generated from the reaction between O₂•⻠and nitric oxide (•NO) [3]. The Hâ‚‚Oâ‚‚ produced by SOD is further processed by other enzymes like CAT and GPx, placing SOD at the apex of the enzymatic antioxidant cascade.
Catalase
Catalase is a highly efficient enzyme located predominantly in peroxisomes, where it catalyzes the conversion of hydrogen peroxide into water and oxygen. It is a tetrameric heme-containing enzyme that operates most effectively at high H₂O₂ concentrations, making it a crucial buffer against significant peroxide loads [18] [8]. Its primary reaction is the disproportionation of H₂O₂: 2 H₂O₂ → 2 H₂O + O₂ [3]. While its role is often seen as purely detoxifying, the H₂O₂ it decomposes is also a signaling molecule, implying that catalase indirectly influences redox-sensitive signaling pathways [4].
Glutathione Peroxidase
Glutathione Peroxidase represents a family of enzymes that reduce Hâ‚‚Oâ‚‚ and organic hydroperoxides (LOOH) to water and corresponding alcohols, respectively. This activity is essential for protecting membranes from lipid peroxidation [18] [8]. Unlike catalase, GPx utilizes reduced glutathione (GSH) as its reducing agent, coupling Hâ‚‚Oâ‚‚ detoxification to the glutathione redox cycle.
The core reaction is: H₂O₂ + 2 GSH → 2 H₂O + GSSG (oxidized glutathione) [8]. The resulting GSSG is then reduced back to GSH by the enzyme glutathione reductase (GR), which consumes NADPH. This creates a metabolic link between antioxidant defense and cellular energy status [8]. GPx enzymes often contain selenium at their active site, which is critical for their catalytic activity [8].
Table 2: Key Enzymatic Antioxidants and Their Properties
| Enzyme | Catalytic Reaction | Cofactor / Cysteine | Cellular Localization | Key Role in Defense |
|---|---|---|---|---|
| Superoxide Dismutase (SOD) | 2 O₂•⻠+ 2H⺠→ H₂O₂ + O₂ | Cu/Zn, Mn, Fe | Cytosol (SOD1), Mitochondria (SOD2), Extracellular (SOD3) [19] | Primary defense against superoxide anion [18] [19] |
| Catalase (CAT) | 2 H₂O₂ → 2 H₂O + O₂ | Heme | Peroxisomes [8] | High-capacity removal of H₂O₂ [18] [8] |
| Glutathione Peroxidase (GPx) | H₂O₂ + 2 GSH → GSSG + 2 H₂O (or ROOH + 2 GSH → GSSG + ROH + H₂O) | Selenium (as selenocysteine) | Cytosol, Mitochondria [8] | Reduces H₂O₂ and lipid hydroperoxides using glutathione [18] [8] |
The following diagram illustrates the coordinated action of these primary enzymatic antioxidants and their integration with key regulatory systems.
Non-enzymatic Antioxidant Networks
The enzymatic defense is powerfully complemented by a suite of non-enzymatic molecules. These compounds act as direct ROS scavengers, cofactors for enzymes, and regulators of the redox proteome.
- Glutathione (GSH): This tripeptide (γ-glutamyl-cysteinyl-glycine) is the most abundant low-molecular-weight thiol in cells. It functions as a direct scavenger of ROS, a cofactor for GPx, and a redox buffer that maintains protein cysteine residues in their reduced state. The ratio of reduced glutathione (GSH) to its oxidized form (GSSG) is a key indicator of cellular redox status [8] [20].
- The Thioredoxin System: Comprising thioredoxin (Trx), thioredoxin reductase (TrxR), and NADPH, this system is crucial for reducing disulfide bonds in proteins, thus regulating protein function and signaling. It works in parallel with the glutathione system to control the cellular redox environment and is negatively regulated by TXNIP (Thioredoxin-Interacting Protein) [8] [20].
- Other Key Molecules:
- Ascorbate (Vitamin C): A potent water-soluble antioxidant that can directly scavenge various ROS and regenerate other antioxidants like vitamin E [21].
- Tocopherols (Vitamin E): Lipid-soluble antioxidants that are critical for terminating lipid peroxidation chain reactions in membranes [21].
- Polyphenols & Flavonoids: A diverse class of plant-derived compounds that can act as hydrogen donors, metal chelators, and in some cases, inducers of the Nrf2 pathway [17] [22].
Regulatory Signaling Pathways
The antioxidant defense system is not static; it is dynamically regulated by several signaling pathways that sense oxidative stress and mount a compensatory transcriptional response.
The Nrf2-Keap1-ARE Pathway
The transcription factor Nuclear factor erythroid 2-related factor 2 (Nrf2) is the master regulator of cytoprotective gene expression. Under basal conditions, Nrf2 is sequestered in the cytoplasm by its inhibitor, Keap1, and targeted for proteasomal degradation. Upon oxidative or electrophilic stress, specific cysteine residues in Keap1 are modified, leading to Nrf2 stabilization. Nrf2 then translocates to the nucleus, binds to the Antioxidant Response Element (ARE), and drives the expression of a vast network of genes, including those for SOD, CAT, GPx, glutathione synthesis enzymes (GCL, GSS), and proteins involved in xenobiotic metabolism and proteostasis [23] [8]. This pathway is a primary target for therapeutic interventions aimed at boosting endogenous antioxidant capacity.
Crosstalk with Inflammatory Pathways
A critical intersection exists between redox and inflammatory signaling. The transcription factor NF-κB is activated by various stimuli, including ROS, and promotes the expression of pro-inflammatory cytokines. Conversely, Nrf2 activation can suppress NF-κB signaling, creating a counter-regulatory loop that limits excessive inflammation [23] [17]. Furthermore, in metabolic syndrome, GLP-1 receptor signaling has been shown to downregulate the expression of TXNIP, thereby enhancing thioredoxin activity and attenuating oxidative stress and inflammation [20].
The following diagram illustrates the core Nrf2 signaling mechanism.
Experimental Protocols for Assessing Antioxidant Function
Robust methodologies are essential for evaluating the activity and function of antioxidant systems in research models. Below are detailed protocols for key assays.
Measuring SOD Activity
Principle: SOD activity is typically measured by its ability to inhibit the reduction of a tetrazolium salt (e.g., cytochrome c or nitrobue tetrazolium) by superoxide anion generated by a xanthine/xanthine oxidase system.
Protocol:
- Reaction Mixture: Prepare a solution containing 50 mM phosphate buffer (pH 7.8), 0.1 mM EDTA, 50 µM xanthine, and 25 µM nitrobue tetrazolium (NBT).
- Enzyme Source: Add the sample containing SOD (cell lysate, tissue homogenate, or purified enzyme).
- Initiate Reaction: Start the reaction by adding xanthine oxidase to a final concentration sufficient to produce a linear increase in absorbance at 560 nm in the absence of SOD.
- Kinetic Measurement: Monitor the increase in absorbance at 560 nm for 5-10 minutes. The reduction of NBT by superoxide produces a blue formazan.
- Calculation: One unit of SOD activity is defined as the amount of enzyme that causes 50% inhibition of the NBT reduction rate under specified conditions. Calculate activity relative to a standard curve of purified SOD [19].
Measuring Catalase Activity
Principle: Catalase activity is directly measured by the disappearance of its substrate, Hâ‚‚Oâ‚‚, which can be tracked spectrophotometrically by its absorbance at 240 nm.
Protocol:
- Reaction Mixture: Prepare a solution of 50 mM phosphate buffer (pH 7.0) containing 10-20 mM Hâ‚‚Oâ‚‚.
- Baseline: Record the initial absorbance at 240 nm.
- Initiate Reaction: Add the sample to the cuvette and mix rapidly.
- Kinetic Measurement: Immediately monitor the decrease in absorbance at 240 nm for 30-60 seconds. The molar extinction coefficient of Hâ‚‚Oâ‚‚ at 240 nm is 43.6 Mâ»Â¹cmâ»Â¹.
- Calculation: Enzyme activity is calculated using the formula: Activity (U/mL) = (ΔA₂₄₀ / min × Total Volume) / (43.6 × Sample Volume), where U is defined as the amount of enzyme that decomposes 1 µmol of H₂O₂ per minute [18].
Measuring GPx Activity
Principle: GPx activity is assayed indirectly by coupling the reduction of Hâ‚‚Oâ‚‚ (or tert-butyl hydroperoxide) to the oxidation of GSH, and then measuring the consumption of NADPH by glutathione reductase (GR), which recycles GSSG back to GSH.
Protocol:
- Reaction Mixture: Prepare a solution containing 50 mM Tris-HCl (pH 7.6), 1 mM EDTA, 0.2 mM NADPH, 2 mM GSH, and 1 unit of Glutathione Reductase.
- Enzyme Source: Add the sample.
- Baseline: Record the initial absorbance at 340 nm.
- Initiate Reaction: Start the reaction by adding Hâ‚‚Oâ‚‚ or cumene hydroperoxide to a final concentration of 0.2-0.5 mM.
- Kinetic Measurement: Monitor the decrease in absorbance at 340 nm (due to NADPH oxidation) for 3-5 minutes.
- Calculation: Enzyme activity is calculated using the molar extinction coefficient of NADPH (6.22 mMâ»Â¹cmâ»Â¹). One unit of GPx is defined as the amount that oxidizes 1 µmol of NADPH per minute [8].
Evaluating Intracellular ROS Levels
Principle: Cell-permeable, fluorescent dyes are oxidized by specific ROS, leading to an increase in fluorescence.
Protocol (using Hâ‚‚DCFDA):
- Cell Preparation: Seed cells in a black-walled, clear-bottom 96-well plate and treat as required.
- Loading Dye: Wash cells with PBS and load with 10-20 µM H₂DCFDA in serum-free media. Incubate for 30-60 minutes at 37°C in the dark.
- Stimulation and Measurement: Wash cells to remove excess dye. Add an oxidative stress inducer (e.g., Hâ‚‚Oâ‚‚). Immediately measure fluorescence (Ex/Em ~485/535 nm) kinetically over 60-120 minutes using a microplate reader [22].
- Analysis: Fluorescence intensity is normalized to cell number (e.g., via a parallel MTT assay) and expressed as a percentage of the control.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Antioxidant and Redox Research
| Reagent / Assay | Function & Application | Example Use Case |
|---|---|---|
| Hâ‚‚DCFDA (Dichloro-dihydro-fluorescein diacetate) | Cell-permeable fluorescent probe for general oxidative stress; measures Hâ‚‚Oâ‚‚ and peroxynitrite-related activity [22]. | Quantifying overall intracellular ROS levels in response to a drug treatment in cultured cells [22]. |
| MitoSOX Red | Mitochondria-targeted fluorescent probe for selective detection of mitochondrial superoxide [22]. | Assessing mitochondrial-specific ROS production in models of neurodegeneration or ischemia-reperfusion. |
| NADPH/NADP+ Assay Kits | Colorimetric or fluorometric measurement of the NADPH/NADP+ ratio, a key indicator of cellular redox state and reducing power [8]. | Evaluating the metabolic capacity for antioxidant defense (e.g., in GPx/GR and TrxR cycles). |
| GSH/GSSG Assay Kits | Quantifies the ratio of reduced to oxidized glutathione, a central biomarker of cellular redox status [8]. | Determining the effectiveness of an Nrf2 activator in maintaining a reduced cellular environment. |
| Nrf2 Activators (e.g., Sulforaphane, DMF) | Pharmacological or natural compounds that disrupt the Keap1-Nrf2 interaction, leading to Nrf2 stabilization and ARE-driven gene transcription [23]. | Experimental upregulation of the entire antioxidant network in disease models. |
| siRNA/shRNA for Nrf2, Keap1, SOD, etc. | Gene silencing tools to knock down specific antioxidant or regulatory components. | Establishing the causal role of a specific antioxidant protein in a phenotypic response. |
| Antibodies for Nrf2, Keap1, HO-1, NQO1, SOD, etc. | Used in Western Blot and Immunofluorescence to assess protein expression, localization (e.g., Nrf2 nuclear translocation), and degradation [22]. | Confirming pathway activation and target protein induction in treated cells or tissues. |
| Urease-IN-16 | Urease-IN-16, MF:C14H17BN2O4S, MW:320.2 g/mol | Chemical Reagent |
| DBCO-PEG3-Acid | DBCO-PEG3-Acid, MF:C28H32N2O7, MW:508.6 g/mol | Chemical Reagent |
The enzymatic antioxidants SOD, catalase, and GPx form an indispensable, coordinated network that constitutes the body's primary defense against ROS. Their function is deeply integrated with non-enzymatic systems like glutathione and thioredoxin, and their expression is dynamically regulated by master transcription factors like Nrf2. A sophisticated understanding of these systems—from their basic chemistry to their complex regulation and the experimental tools used to study them—is fundamental for advancing redox biology research. This knowledge is directly translatable, providing a rational basis for developing novel therapeutics that target oxidative stress in aging, neurodegenerative diseases, metabolic syndrome, and cancer by augmenting the body's innate antioxidant defenses.
Redox signaling is a fundamental biological process in which reactive oxygen species (ROS) and other reactive molecules act as deliberate messengers to modulate cellular functions, rather than solely as agents of damage [8] [24]. This signaling is integral to normal physiology, influencing processes ranging from endothelial cell growth to stress adaptation [24]. The core principle of redox signaling involves the specific, reversible chemical modification of target proteins, predominantly on cysteine residues, which alters their activity, interaction partners, and subcellular localization [24] [25] [26]. This stands in contrast to the traditional view of ROS as merely toxic byproducts.
The "Redox Code," a conceptual framework established in 2015, encapsulates the organizing principles for biological redox circuits. It encompasses the regulation of NADH and NADPH systems in metabolism, the dynamic control of thiol switches in the redox proteome, the activation and deactivation cycles of Hâ‚‚Oâ‚‚ production, and the multi-level response of redox signaling to environmental changes [8]. This code provides the foundational logic for understanding how redox signaling influences health and disease, offering a new perspective for identifying therapeutic targets.
Core Chemical Principles of Thiol-Based Redox Signaling
The Unique Reactivity of Protein Cysteines
Cysteine is one of the least abundant but most highly conserved amino acids in proteins, indicative of its critical functional roles [27]. Its sulfur-containing thiol group (-SH) is the key to its reactivity. A pivotal determinant of this reactivity is the thiol-thiolate equilibrium; the deprotonated thiolate form (-Sâ») is a much more powerful nucleophile than the protonated thiol [24] [27]. The propensity of a cysteine thiol to ionize is governed by its acid dissociation constant (pKâ‚). While the typical pKâ‚ for a cysteine in solution is approximately 8.3, the protein microenvironment can significantly lower this value, stabilizing the thiolate and enhancing reactivity [24] [28]. Factors such as proximity to positively charged amino acids, location within an alpha-helix dipole, and hydrogen-bonding networks can all contribute to this pKâ‚ perturbation [27].
This specialized chemistry means that redox signaling depends not on an abundance of cysteine residues, but on the presence of specific, strategically positioned cysteines with enhanced reactivity [24]. These reactive cysteines serve as molecular sensors for redox-active messengers.
Specificity, Kinetics, and Location in Signaling
For a molecule as potentially promiscuous as Hâ‚‚Oâ‚‚ to function as a specific signal, stringent biochemical constraints are in place:
- Specificity: Signaling depends on specific cysteines within sensor proteins that have evolved to be highly reactive towards particular electrophiles due to their unique microenvironments [24].
- Kinetics: The rate of reaction between an electrophilic second messenger (e.g., Hâ‚‚Oâ‚‚) and its protein target is determined by the second-order rate constant and the concentrations of both partners. Reactive sensor cysteines possess rate constants that are several orders of magnitude higher than those of bulk cellular thiols [24] [27].
- Location: The generation of redox messengers like Hâ‚‚Oâ‚‚ is compartmentalized, creating steep concentration gradients from the source. Effective signaling requires the target protein to be in close proximity to the source of the ROS, allowing for specific modification before the messenger is scavenged by antioxidant systems [24].
These principles ensure that redox signaling is a precise and regulated process, not a stochastic one.
The Cysteine Modification Landscape
The thiolate form of reactive cysteines is susceptible to a spectrum of oxidative post-translational modifications (OxiPTMs). These modifications form a complex language, the "redox code," that cells use to transmit information [8] [29] [26].
Table 1: Major Reversible Cysteine Oxidative Modifications
| Modification | Inducing Agent(s) | Chemical Structure | Functional Consequences & Notes |
|---|---|---|---|
| S-Sulfenylation | Hâ‚‚Oâ‚‚, ROOH | -SOH | Highly reactive intermediate; often leads to disulfide formation or glutathionylation [25] [28]. |
| Disulfide Bond | Hâ‚‚Oâ‚‚, via sulfenic acid | -S-S- (intra/intermolecular) | Can alter protein structure/activity; key in oxidative protein folding [25] [29]. |
| S-Glutathionylation | Hâ‚‚Oâ‚‚, via sulfenic acid | -SSG (mixed disulfide with GSH) | Protects cysteine from over-oxidation; can regulate activity (e.g., actin polymerization) [8] [29] [28]. |
| S-Nitrosylation | Nitric oxide (•NO), ONOO¯ | -SNO | Regulates a wide range of proteins; important in vascular and neural signaling [3] [29] [26]. |
| Persulfidation | Hâ‚‚S | -SSH | Provides protection from irreversible oxidation; can regulate abscisic acid signaling in plants [25] [26]. |
The following diagram illustrates the dynamic network of reversible cysteine modifications and their interconversions, driven by different reactive species.
Beyond the modifications listed in the table, cysteine residues can undergo further oxidation to sulfinic (-SO₂H) and sulfonic (-SO₃H) acids. Sulfinic acid can be reversed by the ATP-dependent enzyme sulfiredoxin, while sulfonylation is typically considered irreversible and often associated with pathological damage [25].
The Redox Code in Physiology and Disease
Regulation of Genomic Stability
Redox signaling plays a critical role in maintaining genomic integrity. Oxidative stress can directly cause DNA damage, such as missense mutations and double-strand breaks (DSBs) [8]. More subtly, redox signaling finely regulates the DNA repair machinery itself through the oxidative modification of key proteins. For instance, the activation of the ataxia-telangiectasia mutated (ATM) kinase, a master regulator of the DNA damage response, is triggered by the Mre11-Rad50-Nbs1 (MRN) complex and involves autophosphorylation, a process potentially regulated by the redox environment [8]. The precise redox modification of DNA repair proteins represents a crucial layer of control over genomic stability.
Implications in Neurodegeneration and Aging
The brain's high metabolic rate and relatively less robust antioxidant defenses make it particularly vulnerable to redox dysregulation [29]. In neurodegenerative diseases like Alzheimer's disease (AD), Parkinson's disease (PD), and amyotrophic lateral sclerosis (ALS), oxidative modifications of cysteine-sensitive proteins contribute to hallmark pathologies such as protein misfolding and aggregation [29]. The network of redox-modified proteins, sometimes termed the "cysteinet," is profoundly altered in these conditions, driving neuronal dysfunction [29].
The role of redox signaling in aging is complex and dualistic. While the long-held "free radical theory" posits aging as a result of accumulated oxidative damage, emerging evidence suggests that a mild, transient increase in ROS can activate adaptive signaling pathways that promote longevity [3] [25]. For example, interventions like dietary restriction and reduced insulin/IGF-1 signaling, which extend lifespan in model organisms, are associated with altered redox profiles and depend on specific redox-sensitive proteins [25]. This highlights that the goal of therapeutic intervention is not blanket antioxidant suppression, but the targeted restoration of healthy redox signaling.
Research Methodologies and Experimental Analysis
Deciphering the redox code requires specialized tools to detect, quantify, and functionally characterize cysteine OxiPTMs within the complex cellular environment.
Key Experimental Workflows
A generalized proteomic workflow for analyzing cysteine oxidation involves several critical stages, from cell preparation to functional validation, as outlined below.
This workflow allows for the proteome-wide identification of specific cysteine modifications. For example, the "biotin-switch technique" and its modern derivatives are cornerstone methods for detecting S-nitrosylation and other reversible modifications [30].
Essential Research Reagents and Tools
A successful investigation into redox signaling relies on a toolkit of specific reagents and model systems.
Table 2: Key Reagents and Models for Redox Signaling Research
| Category / Reagent | Function / Description | Application Example |
|---|---|---|
| Thiol-Blocking Agents (N-ethylmaleimide, Iodoacetamide) | Alkylates and blocks free thiols to prevent post-lysis oxidation artifacts. | Used in initial step of chemoproteomic workflows to "lock in" the redox state [30]. |
| Selective Reducing Agents (Ascorbate, Arsenite) | Selectively reduces specific OxiPTMs (e.g., Ascorbate for S-nitrosylation). | Allows for selective tagging and enrichment of specific modification types [30]. |
| Affinity Tags (Biotin-HPDP, Isotope-coded affinity tags - ICAT) | Tags reduced thiols for purification and quantification via mass spectrometry. | Enables purification and relative quantification of redox-modified peptides [30]. |
| Genetically Encoded Biosensors (roGFP, HyPer) | Fluorescent proteins that change emission/intensity upon redox change or Hâ‚‚Oâ‚‚ binding. | Real-time, compartment-specific monitoring of redox dynamics in live cells [25]. |
| Model Organisms (C. elegans, Mice with altered antioxidant genes) | In vivo systems to study the physiological role of redox signaling in aging/disease. | Identifying pro-longevity pathways activated by mild ROS [25]. |
Functional validation is the final and crucial step. This typically involves site-directed mutagenesis, where a redox-sensitive cysteine is replaced with a redox-insensitive residue like serine or alanine (to disrupt signaling) or sometimes aspartate (to mimic a constitutively oxidized state) [25]. The functional consequences of these mutations are then assessed using biochemical and cellular assays to establish a causal link between the specific cysteine modification and the observed biological outcome.
The study of redox signaling has evolved from a focus on oxidative damage to an appreciation of a sophisticated language of chemical modifications that govern cellular function. The principles of thiol switching, cysteine modifications, and the overarching Redox Code provide a framework for understanding how cells sense and respond to their metabolic and environmental status. The compartmentalized, specific, and reversible nature of these processes underscores their role as critical physiological regulators.
Future research will continue to expand the "thiol redox proteome," identifying new sensor proteins and delineating the complex networks they form [30]. A major challenge and opportunity lie in translating this fundamental knowledge into therapeutic strategies. Instead of non-specific antioxidants, the next generation of therapeutics will likely involve small molecule inhibitors or inducers that target specific redox-sensitive nodes in signaling pathways to re-establish redox balance in diseases like cancer, neurodegeneration, and age-related disorders [8]. Achieving this goal will require a deep, context-specific understanding of the redox code, combining chemical proteomics, systems biology, and functional genomics to unlock its full therapeutic potential.
Reactive oxygen species (ROS), particularly hydrogen peroxide (Hâ‚‚Oâ‚‚), have emerged as crucial physiological mediators in cellular signaling networks. Once considered solely as damaging agents, ROS are now recognized as fundamental second messengers that regulate processes including proliferation, differentiation, and metabolic adaptation [31] [32]. Among ROS, Hâ‚‚Oâ‚‚ best fulfills the requirements of a second messenger due to its relative stability, ability to diffuse across membranes, and enzymatic production and degradation that provide specificity for time and place [31]. This whitepaper examines the molecular mechanisms of ROS-mediated signaling, focusing on their roles in cellular fate decisions and the experimental frameworks for their investigation.
The "redox code" represents an organizational framework for biological operations where Hâ‚‚Oâ‚‚ plays a central role in spatiotemporal sequencing of differentiation and cellular life cycles through kinetically controlled redox switches [6]. These switches predominantly involve reversible oxidation of cysteine residues in target proteins, analogous to phosphorylation events in kinase-mediated signaling cascades [33]. The dual role of ROS as both essential signaling molecules and potential damaging agents creates a sophisticated regulatory system maintained through precise balance between production and elimination [34] [32].
Molecular Mechanisms of ROS-Mediated Signaling
Biochemical Basis of ROS Signaling
ROS signaling occurs primarily through specific, reversible oxidation of redox-sensitive cysteine residues in target proteins, particularly through sulfenic acid (-SOH) formation, which can progress to disulfide bonds or higher oxidation states [31] [34]. This oxidative modification alters protein structure, activity, and interaction networks, enabling propagation of redox signals throughout the cell [33].
Table 1: Principal Reactive Oxygen Species in Cellular Signaling
| ROS Species | Chemical Symbol | Reactivity | Stability | Primary Sources | Main Signaling Role |
|---|---|---|---|---|---|
| Superoxide anion | O₂•⻠| Moderate | Low | Mitochondrial ETC, NOX enzymes | Precursor to H₂O₂, limited direct signaling |
| Hydrogen peroxide | Hâ‚‚Oâ‚‚ | Selective | High | SOD activity, NOX enzymes | Primary redox messenger |
| Hydroxyl radical | •OH | Extreme | Very low | Fenton reaction | Minimal signaling, mainly damage |
| Singlet oxygen | ¹O₂ | High | Low | Photosensitization | Limited evidence for physiological signaling |
The specificity of Hâ‚‚Oâ‚‚ signaling is achieved through several mechanisms: (1) localized production by activated enzymes; (2) kinetic competition between peroxide-eliminating and peroxide-utilizing proteins; and (3) reversible oxidation of specific cysteine residues with particular microenvironments that lower their pKâ‚, making them more susceptible to oxidation [31] [5]. Peroxiredoxins (Prxs) play a particularly important role as both regulators and transducers of Hâ‚‚Oâ‚‚ signals through their own redox state, creating redox relays that transmit oxidizing equivalents to target proteins [34] [6].
Key Signaling Pathways Regulated by ROS
Multiple developmentally significant signaling pathways are modulated by ROS through oxidative modification of crucial components:
- NRF2/KEAP1 Pathway: ROS-induced modification of specific cysteine residues on KEAP1 disrupts NRF2 degradation, enabling NRF2 translocation to the nucleus where it activates cytoprotective genes involved in antioxidant response and metabolism [32].
- NF-κB Pathway: ROS modulate this central inflammatory pathway, though the precise mechanisms remain context-dependent, influencing both activation and inhibition [32].
- PI3K/AKT Pathway: Redox regulation of phosphatases that counterbalance this growth and survival pathway represents an important mechanism for controlling proliferation [32].
- MAPK Pathways: Multiple MAPK family members are sensitive to cellular redox state, connecting ROS signals to proliferation, differentiation, and stress response decisions [32].
The diagram below illustrates the core mechanism of redox signaling through cysteine oxidation:
ROS in Cellular Processes: Proliferation, Differentiation, and Metabolism
Regulation of Stem Cell Fate
ROS function as a "rheostat" in stem cells, translating metabolic and environmental cues to coordinate cellular responses including self-renewal, differentiation, and quiescence [32]. Different stem cell types maintain distinct ROS set points:
- Hematopoietic Stem Cells (HSCs): Lower ROS levels are associated with greater potency and quiescence, while increased ROS promote differentiation [35] [32].
- Neural Stem Cells (NSCs): ROS accumulation controls proliferation and self-renewal, with moderate increases promoting maintenance of the stem cell pool [32].
- Mesenchymal Stem Cells (MSCs): These cells demonstrate a dual role for ROS, where the undifferentiated state correlates with lower ROS levels, but self-renewal requires ROS upregulation [32].
Embryonic stem cells (ESCs) exhibit a unique metabolic configuration favoring glycolysis over oxidative phosphorylation, which maintains lower ROS levels and supports self-renewal by preventing oxidative stress-induced differentiation [35]. The transition to differentiated states involves a metabolic shift toward oxidative metabolism with coordinated increases in ROS that drive gene expression programs supporting specialized functions.
Metabolic Regulation and Signaling
ROS and cellular metabolism exist in a reciprocal relationship: metabolic activity generates ROS, which in turn regulate metabolic pathways through signaling functions [32]. Mitochondria serve as both major sources of ROS and key targets of redox regulation, creating feedback loops that adjust energy production to cellular needs.
Table 2: Major Cellular Sources of ROS and Their Regulation
| Source | Location | Primary ROS | Regulators | Role in Signaling |
|---|---|---|---|---|
| Complex I, Mitochondria | Mitochondrial matrix | O₂•⻠| NADH/NAD⺠ratio, RET | Metabolic sensing, hypoxic response |
| Complex III, Mitochondria | Intermembrane space | O₂•⻠| ΔΨm, UCP proteins | Glucose sensing, apoptosis |
| NADPH Oxidases (NOX) | Plasma membrane | O₂•â», Hâ‚‚Oâ‚‚ | Growth factors, cytokines | Receptor-mediated signaling |
| Endoplasmic Reticulum | ER lumen | Hâ‚‚Oâ‚‚ | Protein folding load | Unfolded protein response |
| Peroxisomes | Peroxisomal matrix | Hâ‚‚Oâ‚‚ | Fatty acid oxidation | Lipid metabolism signaling |
Mitochondrial complex I (NADH:ubiquinone oxidoreductase) represents a significant contributor to ROS generation, particularly through reverse electron transport (RET) when a high proton gradient coincides with abundant reduced ubiquinone [35]. This mechanism allows mitochondria to function as metabolic sensors, translating changes in energy state into redox signals that regulate gene expression and cell fate decisions.
The diagram below illustrates how ROS regulate key cellular fate decisions:
Experimental Approaches for ROS Research
Methodologies for ROS Detection and Measurement
Accurate assessment of ROS presents significant challenges due to their reactive nature, low concentrations, and compartmentalized production. Current guidelines emphasize the importance of specifying the particular ROS species being measured rather than treating "ROS" as a single entity [5].
Table 3: Experimental Approaches for ROS Measurement
| Method Category | Specific Techniques | ROS Detected | Key Considerations | Applications |
|---|---|---|---|---|
| Chemical probes | DCFH-DA, DHE, Amplex Red | H₂O₂, O₂•⻠| Specificity issues, compartmentalization | General screening, extracellular H₂O₂ |
| Genetically encoded biosensors | roGFP, HyPer | Hâ‚‚Oâ‚‚ | Subcellular targeting, ratiometric | Real-time intracellular monitoring |
| EPR/ESR spectroscopy | Spin traps (DMPO) | O₂•â», •OH | Direct detection, technical complexity | Specific radical identification |
| Oxidative damage markers | Protein carbonylation, 8-OHdG | Indirect | Downstream effects, not real-time | Cumulative oxidative stress |
Electron paramagnetic resonance (EPR) spectroscopy with spin trapping represents the gold standard for specific radical identification, while genetically encoded sensors like roGFP and HyPer enable compartment-specific monitoring of Hâ‚‚Oâ‚‚ dynamics in live cells [5]. For controlled ROS generation in experimental systems, researchers can use:
- Paraquat and quinones for O₂•⻠generation [5]
- MitoPQ for mitochondrial O₂•⻠generation [5]
- d-amino acid oxidase systems for controlled Hâ‚‚Oâ‚‚ production [5]
- Glucose oxidase for extracellular Hâ‚‚Oâ‚‚ generation [5]
Modulation of ROS Levels in Experimental Systems
To establish causal relationships between ROS and biological effects, researchers employ both pharmacological and genetic approaches:
- NOX inhibition: Specific inhibitors or genetic deletion of NOX components are preferred over non-specific inhibitors like apocynin or diphenyleneiodonium [5].
- Antioxidant systems: Modulation of SOD, catalase, or peroxiredoxin expression can reveal functions of specific ROS.
- Scavenging systems: Overexpression of catalase targeted to specific compartments can dissect location-dependent ROS effects.
The interpretation of antioxidant experiments requires careful consideration, as many commonly used "antioxidants" such as N-acetylcysteine (NAC) have multiple mechanisms beyond ROS scavenging, including effects on glutathione levels, protein disulfide reduction, and Hâ‚‚S generation [5].
The diagram below outlines a general experimental workflow for investigating ROS signaling:
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for ROS Signaling Studies
| Reagent Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| ROS generators | Paraquat, MitoPQ, d-amino acid oxidase systems | Controlled ROS production in specific compartments | MitoPQ targets mitochondria specifically |
| ROS sensors | DCFH-DA, MitoSOX, roGFP, HyPer | Detection and measurement of specific ROS | Genetically encoded sensors allow subcellular targeting |
| NOX inhibitors | GKT136901, VAS2870, NOX knockout models | Specific inhibition of NOX enzymes | Prefer specific inhibitors over apocynin |
| Antioxidant enzymes | Recombinant SOD, catalase, peroxiredoxins | Scavenging specific ROS species | Compartment-specific targeting needed |
| Thiol redox probes | Biotin-conjugated iodoacetamide, maleimide dyes | Detection of cysteine oxidation states | Enable redox proteomics approaches |
| ROS-activated prodrugs | Selenium-based Michael acceptor prodrugs | Selective drug release in high-ROS environments | Potential therapeutic applications |
| Vercirnon Sodium | Vercirnon Sodium, MF:C22H20ClN2NaO4S, MW:466.9 g/mol | Chemical Reagent | Bench Chemicals |
| VCH-286 | VCH-286, MF:C34H50F2N4O3, MW:600.8 g/mol | Chemical Reagent | Bench Chemicals |
Recent innovations include selenium-based prodrug strategies that leverage elevated ROS in pathological conditions for selective drug activation. These approaches utilize selenium ether derivatives that undergo Hâ‚‚Oâ‚‚-dependent elimination to release active Michael acceptor compounds, demonstrating potential for targeted therapies in cancer and inflammatory diseases [36].
ROS, particularly Hâ‚‚Oâ‚‚, function as sophisticated second messengers in the regulation of proliferation, differentiation, and metabolism through specific, reversible oxidation of protein targets. The compartmentalized production and elimination of ROS creates a signaling system that integrates metabolic state with cell fate decisions. Future research will continue to elucidate the specific molecular targets of ROS in different physiological contexts and develop increasingly precise tools for measuring and manipulating redox signaling. These advances hold promise for novel therapeutic approaches that target ROS signaling in cancer, degenerative diseases, and metabolic disorders.
Advanced Techniques for ROS Detection, Manipulation, and Pathway Analysis
Reactive oxygen species (ROS) are inevitable byproducts of cellular aerobic metabolism that play a dual role in health and disease. At physiological levels, ROS function as crucial signaling molecules in cellular processes, while excessive generation leads to oxidative stress, biomolecular damage, and disease progression. The accurate detection and quantification of specific ROS is therefore paramount for understanding redox biology and its implications in various pathological conditions [3] [37]. The term "ROS" encompasses a spectrum of chemically distinct molecules including superoxide anion (O₂•â»), hydrogen peroxide (Hâ‚‚Oâ‚‚), hydroxyl radical (HO•), and others, each with unique reactivity, lifespan, and biological targets [5]. This technical guide comprehensively reviews state-of-the-art methodologies for ROS detection, with emphasis on probes, biosensors, and live-cell imaging approaches, providing researchers with practical frameworks for implementing these technologies in investigative and drug development contexts.
Fundamental Chemistry and Biological Significance of ROS
Major Reactive Oxygen Species
ROS comprise both free radical and non-radical oxygen derivatives with diverse chemical properties and biological reactivities. The most biologically significant ROS include superoxide anion (O₂•â»), primarily generated through electron leakage from mitochondrial electron transport chain complexes I and III or via NADPH oxidase (NOX) enzymes; hydrogen peroxide (Hâ‚‚Oâ‚‚), produced through superoxide dismutation and functioning as a key redox signaling molecule; and the hydroxyl radical (HO•), an extremely reactive species generated via Fenton chemistry [3] [5]. Other biologically relevant species include peroxynitrite (ONOO¯), formed from the reaction between superoxide and nitric oxide, and hypochlorous acid (HOCl), produced by myeloperoxidase [3].
ROS Signaling and Oxidative Stress
ROS function as crucial signaling mediators at physiological concentrations, regulating processes such as cell proliferation, differentiation, and immune response through reversible oxidation of specific cysteine and methionine residues in target proteins [35] [37]. Hydrogen peroxide in particular serves as an important second messenger, with intracellular concentrations typically maintained in the low nanomolar range (1-100 nM) under homeostatic conditions [35]. When ROS production overwhelms cellular antioxidant capacity, oxidative stress occurs, leading to non-specific oxidation of proteins, lipids, and DNA, which contributes to aging, cancer, neurodegenerative disorders, and metabolic diseases [3] [37].
Advanced Methodologies for ROS Detection
Electrochemical Detection Systems
Electrochemical techniques have gained significant attention due to their high sensitivity, selectivity, and real-time monitoring capabilities. These systems employ both organic and inorganic molecules to detect ROS, enabling precise measurement in biological samples. Recent advances have focused on enhancing selectivity for specific ROS including O₂•â», Hâ‚‚Oâ‚‚, and HO• through electrode modification and functionalization strategies [38]. Electrochemical methods are particularly valuable for quantifying ROS release from cells and tissues, with applications extending to real-time monitoring in living systems. These platforms continue to evolve with improvements in nano-structured electrodes and selective catalytic surfaces that discriminate between different ROS species based on their oxidation-reduction potentials [38].
Fluorescent Probes and "Turn-On" Nanosensors
Fluorescent probes represent one of the most widely employed tools for ROS detection in cellular systems. Recent innovations have focused on "turn-on" nanoprobes that exhibit minimal background fluorescence until reacting with specific ROS species [39]. These designs offer significant advantages including high sensitivity, temporal and spatial resolution for live-cell imaging, and potentially infinite contrast against background signals [39].
Table 1: Nanomaterial-Based "Turn-On" ROS Probes
| Nanomaterial Platform | Detection Mechanism | Target ROS | Limit of Detection | Key Features |
|---|---|---|---|---|
| Boronic acid-functionalized carbon dots | FRET-based ratiometric | H₂O₂ | 0.5 μM | Small size (~4 nm), good in vivo utility |
| Boronate ester-MSNPs | Oxidative cleavage | H₂O₂ | 3.33 μM | Can be integrated with drug delivery systems |
| Zr(IV) MOF with boronic acid | Structural modification | H₂O₂ | 0.015 μM | First MOF for H₂O₂ sensing |
| 3D indium MOF | Structural modification | Hâ‚‚Oâ‚‚ | 420 nM | Improved selectivity for Hâ‚‚Oâ‚‚ |
| Carbon dots with diphenylphosphine | PET mechanism prevention | Hâ‚‚Oâ‚‚ | 84 nM | Fast response, high selectivity |
| Peroxalate-functionalized carbon nanodots | Chemiluminescence | Hâ‚‚Oâ‚‚ | 5 nM | Near-infrared detection, large penetration depth |
| DNA-AgNPs with UCNPs | LRET inhibition | H₂O₂ | 1.08 μM | Luminescence recovery mechanism |
| MnO₂-nanosheet-UCNPs | Quencher destruction | H₂O₂ | 0.9 μM | Rapid detection, high selectivity |
Nanoparticles exhibit tunable properties in size, shape, and functionality that make them highly adaptable for ROS detection applications. Design strategies include carbon dots, mesoporous silica nanoparticles (MSNPs), metal-organic frameworks (MOFs), and various nanocomposites that respond to specific ROS through mechanisms such as fluorescence resonance energy transfer (FRET), photo-induced electron transfer (PET), and luminescence resonance energy transfer (LRET) [39]. For instance, boronic acid-functionalized nanomaterials undergo oxidative cleavage in the presence of Hâ‚‚Oâ‚‚, generating fluorescent products, while manganese dioxide (MnOâ‚‚) nanosheets function as quenchers that are degraded by Hâ‚‚Oâ‚‚, restoring fluorescence [39].
Genetically Encoded Biosensors
Genetically encoded biosensors represent a revolutionary advancement for monitoring ROS dynamics in live cells with high spatial and temporal precision. These biosensors typically incorporate fluorescent proteins whose spectral properties change in response to redox conditions or specific ROS. A prominent example involves biosensors based on fluorescence lifetime imaging microscopy (FLIM), which provides quantitative measurements independent of expression levels, excitation power, or focus drift, resulting in highly robust readings [40]. These biosensors can be targeted to specific subcellular compartments (mitochondria, endoplasmic reticulum, nucleus) to monitor compartment-specific ROS production, which is crucial given the localized nature of redox signaling [40] [35]. Recent developments include circularly permuted fluorescent proteins coupled to redox-sensitive domains that undergo conformational changes upon oxidation, altering fluorescence intensity or spectrum.
Electron Paramagnetic Resonance (EPR) Spectroscopy
EPR spectroscopy, also known as electron spin resonance (ESR), represents the gold standard for direct detection of radical species due to its specificity for molecules with unpaired electrons. This technique often employs spin traps—compounds that react with short-lived radicals to form more stable adducts with characteristic EPR spectra. While technically demanding and less amenable to live-cell imaging, EPR provides unambiguous identification and quantification of specific radical species, making it invaluable for validating results obtained by other methods [5].
Experimental Protocols for ROS Detection
Protocol for Live-Cell Imaging with Genetically Encoded Biosensors
Materials Required:
- Plasmid DNA encoding the biosensor (e.g., roGFP, HyPer)
- Appropriate cell culture reagents and transfection reagents
- Confocal or fluorescence microscope with capabilities for ratiometric imaging
- Imaging chamber with environmental control (temperature, COâ‚‚)
- ROS-inducing agents (e.g., paraquat, menadione, Hâ‚‚Oâ‚‚) and antioxidants for controls
Procedure:
- Cell Preparation and Transfection: Culture cells in appropriate medium and transfect with biosensor plasmid using standard transfection methods. Allow 24-48 hours for expression.
- Microscope Setup: Configure microscope for ratiometric imaging using appropriate excitation/emission filters (e.g., 400/510 nm and 490/510 nm for roGFP).
- Image Acquisition: Plate transfected cells on imaging chambers and acquire baseline images. Maintain cells at 37°C with 5% CO₂ throughout imaging.
- Stimulation and Time-Course Imaging: Add ROS-inducing compounds or experimental treatments and continue time-lapse imaging to monitor dynamic changes.
- Data Analysis: Calculate emission ratios for each time point and normalize to baseline values. Generate quantitative traces of redox changes over time.
Validation and Controls: Include controls with antioxidant treatment (e.g., N-acetylcysteine) to confirm specificity. Calibrate biosensor response using defined redox buffers containing dithiothreitol (reduced) and diamide (oxidized) [40] [5].
Protocol for Hâ‚‚Oâ‚‚ Detection Using "Turn-On" Nanoprobes
Materials Required:
- Boronic acid-functionalized fluorescent nanoparticles
- Cell culture reagents
- Fluorescence plate reader or confocal microscope
- Hâ‚‚Oâ‚‚ standards for calibration
- Lysis buffer if measuring intracellular Hâ‚‚Oâ‚‚
Procedure:
- Probe Preparation: Prepare nanoparticle suspension according to manufacturer's instructions or published protocols.
- Cell Treatment and Incubation: Incubate cells with nanoparticles (typical concentration 50-200 μg/mL) for 2-4 hours to allow cellular uptake.
- Stimulation: Apply experimental treatments to modulate cellular Hâ‚‚Oâ‚‚ production.
- Fluorescence Measurement: Quantify fluorescence using appropriate instrumentation (excitation/emission wavelengths depend on specific nanoprobe).
- Quantification: Generate standard curve using known Hâ‚‚Oâ‚‚ concentrations and calculate sample concentrations from linear regression.
Technical Considerations: Include controls for potential interference from other ROS species. Assess cellular uptake and localization using microscopy. Note that detection limits vary by probe design, with some advanced systems detecting Hâ‚‚Oâ‚‚ in the nanomolar range [39].
ROS Detection Method Selection Workflow
Critical Considerations in ROS Detection
Method Validation and Specificity
A significant challenge in ROS detection lies in the lack of specificity of many commonly used probes and assays. Several commercial kits purportedly measure "ROS" as a single entity, failing to distinguish between chemically distinct species with different biological activities [5]. Proper validation should include multiple complementary methods to confirm results, use of specific ROS-generating systems (e.g., paraquat for O₂•â», glucose oxidase for Hâ‚‚Oâ‚‚), and genetic or pharmacological modulation of ROS production pathways [5]. Recommendation 1 from international guidelines emphasizes that researchers should identify the actual chemical species involved whenever possible and consider whether observed effects align with its known reactivity, lifespan, and reaction products [5].
Compartmentalization and Microenvironment
ROS signaling is highly compartmentalized within cells, with distinct pools in mitochondria, cytoplasm, nucleus, and other organelles. This spatial organization necessitates detection methods with subcellular resolution [35]. Genetically encoded sensors targetable to specific compartments or nanoparticle probes with organelle-specific localization address this need. Additionally, the local microenvironment (pH, antioxidant concentrations, enzyme activities) significantly influences ROS measurements and must be considered when interpreting results [5] [35].
Quantification and Artifact Avoidance
Many fluorescence-based methods provide relative rather than absolute quantification of ROS levels. Where possible, inclusion of standard curves with known concentrations of ROS generators enables more quantitative assessments. Common artifacts include auto-oxidation of probes, light-induced ROS generation during imaging, interference from other cellular components, and perturbation of the biological system by the detection method itself [5]. Appropriate controls should include probe-only samples, cells without probe, and antioxidant treatments to establish baseline signals.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for ROS Detection
| Reagent Category | Specific Examples | Primary Function | Notable Features |
|---|---|---|---|
| Chemical Probes | DCFH-DA, DHE, MitoSOX | Fluorescent detection of general ROS and specific species | Varying specificity; require careful interpretation |
| Genetically Encoded Biosensors | roGFP, HyPer, Grx1-roGFP | Ratiometric measurement of specific redox couples | Targetable to subcellular compartments; quantitative |
| Nanoparticle Probes | Boronic acid-functionalized carbon dots, MnOâ‚‚ nanosheets | "Turn-on" detection with amplification | High sensitivity; some enable therapeutic delivery |
| ROS Generators | Paraquat, Menadione, d-amino acid oxidase | Controlled ROS production for experimental modulation | Specific to superoxide or hydrogen peroxide |
| Antioxidants/Inhibitors | N-acetylcysteine, TEMPOL, NOX inhibitors | Modulate ROS levels for mechanistic studies | Varying specificity; multiple mechanisms of action |
| Spin Traps | DMPO, DEPMPO | Stabilize radicals for EPR detection | Enable direct radical identification |
| JNJ-65355394 | JNJ-65355394, MF:C19H26N4OS, MW:358.5 g/mol | Chemical Reagent | Bench Chemicals |
| Levamisole | Levamisole, CAS:14769-73-4; 16595-80-5, MF:C11H12N2S, MW:204.29 g/mol | Chemical Reagent | Bench Chemicals |
Future Perspectives and Emerging Technologies
The field of ROS detection continues to evolve with several promising directions. Multi-modal approaches that combine complementary techniques provide more comprehensive insights into redox biology. Advanced materials including quantum dots, upconversion nanoparticles, and surface-enhanced Raman scattering (SERS) probes offer new detection mechanisms with improved sensitivity and specificity [39] [40]. The integration of ROS detection with other 'omics' approaches (redox proteomics, lipidomics) enables systems-level understanding of oxidative modifications. In drug development, ROS detection technologies are being adapted for high-throughput screening of antioxidant compounds and for monitoring redox changes in response to therapeutic interventions. As these technologies mature, they will further illuminate the complex roles of ROS in health and disease, potentially identifying new therapeutic targets for conditions characterized by oxidative stress.
ROS Signaling and Detection Pathways
Reactive oxygen species (ROS) homeostasis represents a fundamental biological process where cells dynamically regulate intracellular ROS levels to ensure survival and execute physiological functions. These highly reactive molecules, including superoxide anion (•O2–), hydrogen peroxide (H2O2), and hydroxyl radicals (•OH), serve as critical signaling entities while posing potential toxic threats at dysregulated concentrations [1]. The precise maintenance of redox balance is crucial for cellular metabolism, differentiation, and programmed death pathways, with disruption leading to accelerated aging, neurodegenerative disorders, cardiovascular diseases, and cancer [1] [8] [41].
The emergence of CRISPR-based technologies has revolutionized our capacity to interrogate and manipulate redox systems with unprecedented precision. This genome-editing tool, derived from a bacterial adaptive immune system, utilizes a guide RNA (gRNA) and Cas9 nuclease to create targeted double-strand breaks in DNA, enabling specific gene knockouts, corrections, and transcriptional controls [42]. Compared to earlier technologies like zinc finger nucleases and transcription activator-like effector nucleases, CRISPR-Cas9 offers superior ease of design, cost-effectiveness, and specificity, with ongoing refinements continually enhancing its precision [42]. The application of CRISPR to redox biology has unlocked systematic dissection of redox regulatory networks, identification of essential nodes in antioxidant defense, and development of novel therapeutic strategies for oxidative stress-related pathologies.
CRISPR Tools for Redox Research
Core Editing Platforms
The CRISPR toolkit for redox research has expanded beyond standard CRISPR-Cas9 to include more precise editing technologies. Prime editing represents a particular advancement, utilizing a Cas9 nickase fused to a reverse transcriptase (MMLV-RT) guided by a prime-editing gRNA. This system introduces point mutations, insertions, or deletions without generating double-strand breaks, achieving greater precision with fewer unintended effects than previous editors [42]. Base editing offers an alternative approach that enables direct conversion of one DNA base to another without double-strand break formation, exemplified by YolTech Therapeutics' adenine base editor (hpABE5) which successfully reduced PCSK9 and LDL-C in heterozygous familial hypercholesterolemia patients [43].
For transcriptional control rather than DNA alteration, CRISPR activation (CRISPRa) and CRISPR interference (CRISPRi) employ a nuclease-dead Cas9 (dCas9) fused with transcriptional activators or repressors to modulate gene expression without altering the genetic code itself [42]. These tools enable reversible manipulation of redox gene expression, allowing researchers to study the functional consequences of graded changes in antioxidant enzymes or ROS-producing systems.
Advanced Delivery and Screening Systems
Effective delivery of CRISPR components remains a critical challenge, with recent advances including lipid nanoparticles (LNPs) that show particular tropism for hepatic tissue [44]. These LNPs form lipid droplets around CRISPR molecules and accumulate in the liver after systemic administration, making them ideal for targeting liver-expressed redox genes. Additionally, engineered extracellular vesicles incorporating self-cleaving mini-inteins for active loading and fusogenic VSV-G for endosomal escape enable efficient intracellular delivery of Cas9 ribonucleoproteins [43].
For systematic interrogation of redox networks, combinatorial CRISPR screening approaches enable high-throughput assessment of gene essentiality and interactions across metabolic pathways. This methodology involves generating dual-sgRNA libraries to target gene pairs simultaneously, revealing synthetic lethal interactions and compensatory pathways within redox regulatory networks [45]. Electrogenetic CRISPR (eCRISPR) systems represent another innovation, connecting electronic inputs to biological outputs through redox-responsive promoters that activate CRISPR-mediated gene regulation in response to electrode-generated chemical signals [46].
Experimental Models and Methodologies
In Vitro Screening Approaches
Combinatorial CRISPR screening provides a powerful methodology for mapping genetic interactions within redox metabolic networks. The experimental workflow begins with selecting a target gene set—for carbohydrate metabolism studies, this typically encompasses 51 genes representing glycolysis and the pentose phosphate pathway [45]. Researchers then design a dual-sgRNA library with three sgRNAs per gene, creating 9 unique constructs for each gene pair, resulting in a library comprising 459 single-gene targeting elements and 11,475 dual-gene targeting elements [45].
The library is cloned into a lentiviral vector and transduced into cells stably expressing Cas9, such as HeLa or A549 cell lines. After transduction, cells are sampled at multiple time points (days 3, 14, 21, and 28) to track sgRNA abundance through next-generation sequencing. Computational analysis of sgRNA frequency changes enables calculation of both gene-level fitness values (fg) and genetic interaction scores (Ï€gg), revealing synthetic lethal and suppressor relationships within the redox network [45]. Validation typically involves competition assays and metabolic flux measurements using 13C and 2H isotope tracing to confirm the functional impact of identified genetic interactions on redox metabolism.
Table 1: Key Metabolic Genes in Redox Homeostasis Identified via CRISPR Screens
| Gene | Pathway | Function | Essentiality | Interactions |
|---|---|---|---|---|
| G6PD | Pentose phosphate pathway | NADPH production | Critical | KEAP1, GAPDH |
| PGD | Pentose phosphate pathway | NADPH production | Critical | GAPDH, TALDO1 |
| GAPDH | Glycolysis | NADH production | Critical | Multiple partners |
| KEAP1 | NRF2 signaling | Redox sensor | Context-dependent | NRF2, G6PD, PGD |
| ALDOA | Glycolysis | Fructose metabolism | High | TPII, GAPDH |
| HK2 | Glycolysis | Glucose phosphorylation | High | GCK, HK1 |
In Vivo Modeling Techniques
For in vivo investigation of redox systems, CRISPR enables creation of specific disease models. The process begins with identifying a target gene relevant to redox homeostasis, such as DNMT3A, whose mutation alters DNA methylation patterns and impairs p53-PUMA signaling [43]. Researchers design sgRNAs with high on-target efficiency and minimal off-target potential, increasingly using machine learning tools like PAMmla—a neural network trained to predict PAM recognition across 64 million variants—to engineer custom enzymes with enhanced specificity [43].
Delivery methods vary by target tissue: lipid nanoparticles (LNPs) administer CRISPR components intravenously for hepatic editing, achieving >90% reduction in target proteins like transthyretin (TTR) in clinical trials [44]. For neurological applications, adeno-associated viruses (AAVs) deliver CRISPR constructs to the central nervous system, as demonstrated by Scribe Therapeutics' CasX-mediated editing in mouse CNS [43]. Extracellular vesicles show promise for brain delivery, with single infusions achieving >40% recombination in hippocampal cells [43].
Post-treatment assessment includes tracking protein reduction (e.g., TTR levels in serum for hATTR amyloidosis), histological examination of target tissues, and monitoring functional outcomes. In successful clinical applications, patients with hereditary transthyretin amyloidosis maintained approximately 90% reduction in TTR levels over two years following a single CRISPR treatment [44].
Key Signaling Pathways and Redox Regulation
KEAP1-NRF2 Antioxidant Response
The KEAP1-NRF2 axis represents the primary cellular defense mechanism against oxidative stress, serving as a critical regulator of redox homeostasis. Under basal conditions, KEAP1 functions as a substrate adaptor for a CUL3-based E3 ubiquitin ligase complex that continuously targets NRF2 for proteasomal degradation, maintaining low cellular levels of this transcription factor [45] [8]. During oxidative stress, specific cysteine residues in KEAP1 undergo modification, disrupting its ability to facilitate NRF2 ubiquitination and leading to NRF2 accumulation [8].
Stabilized NRF2 translocates to the nucleus and binds to antioxidant response elements (AREs) in the promoter regions of over 200 genes involved in antioxidant defense, glutathione synthesis, and NADPH regeneration [45] [8]. This transcriptional program enhances production of proteins like NAD(P)H quinone dehydrogenase 1 (NQO1), glutathione peroxidase 4 (GPX4), thioredoxin (TXN), and peroxiredoxin 1 (PRDX1), collectively strengthening cellular antioxidant capacity [8]. CRISPR-based screens have identified KEAP1 as a critical node in redox regulation, with its loss conferring resistance to oxidative stress through constitutive NRF2 activation [45].
Diagram 1: KEAP1-NRF2 signaling pathway in antioxidant response.
Redox Regulation of DNA Repair
Redox signaling exerts profound influence on genomic stability through regulation of DNA repair mechanisms, particularly for double-strand breaks (DSBs). ROS can directly induce DNA damage through chemical modifications including missense mutations, truncation mutations, and strand breakage [8]. Additionally, redox modifications fine-tune the activity of DNA repair proteins, creating a sophisticated regulatory interface between oxidative stress response and genomic maintenance [8].
The Mre11-Rad50-Nbs1 (MRN) complex senses DSBs and activates ataxia-telangiectasia mutated (ATM) kinase through redox-sensitive mechanisms [8]. Activated ATM phosphorylates numerous downstream targets including p53 and CHK2, coordinating cell cycle arrest and DNA repair processes. CRISPR-based studies have revealed that redox imbalances can disrupt these repair pathways, contributing to the genomic instability characteristic of cancer and accelerated aging disorders [8]. This intersection between redox biology and DNA repair represents a promising therapeutic target, particularly for malignancies with defective antioxidant systems.
Quantitative Analysis of Redox Manipulation Outcomes
Table 2: Quantitative Outcomes of CRISPR-Mediated Redox Manipulation in Disease Models
| Disease Model | Target Gene | Editing System | Key Metric | Result | Duration |
|---|---|---|---|---|---|
| Hereditary ATTR amyloidosis | TTR | LNP-CRISPR | TTR reduction | ~90% | 2 years |
| Hereditary angioedema | Kallikrein | LNP-CRISPR | Kallikrein reduction | 86% | 16 weeks |
| Heterozygous familial hypercholesterolemia | PCSK9 | ABE (YOLT-101) | LDL-C reduction | ~50% | Ongoing |
| Colorectal cancer | CISH | ex vivo CRISPR | Tumor regression | Complete response | 2+ years |
| CPS1 deficiency | CPS1 | bespoke LNP-CRISPR | Symptom improvement | Significant | 6 months |
Table 3: Redox Gene Interactions Identified Through Combinatorial CRISPR Screens
| Gene A | Gene B | Interaction Type | Biological Context | Pathway |
|---|---|---|---|---|
| G6PD | KEAP1 | Synthetic lethal | KEAP1-mutant cells | PPP/NFE2L2 |
| PGD | KEAP1 | Synthetic lethal | KEAP1-mutant cells | PPP/NFE2L2 |
| ENO1 | ENO3 | Compensatory | Both highly expressed | Glycolysis |
| GAPDH | PGD | Synergistic | NAD(P)H regeneration | PPP/Glycolysis |
| MBTPS1 | STAT1 | Regulatory | Immunotherapy response | Immune signaling |
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for CRISPR-Mediated Redox Manipulation
| Reagent/Category | Specific Examples | Function/Application | Key Characteristics |
|---|---|---|---|
| CRISPR Editors | Cas9, Cas12f1, Cas3, Base editors, Prime editors | Gene knockout, base conversion, precise editing | Varying PAM requirements, editing windows, specificities |
| Delivery Systems | Lipid nanoparticles (LNPs), AAVs, Engineered extracellular vesicles | Intracellular delivery of editing components | Tissue tropism, payload capacity, immunogenicity |
| Redox Modulators | Paraquat, MitoPQ, d-amino acid oxidase | Controlled ROS generation | Site-specific (mitochondrial/cytosolic), inducible |
| Screening Tools | Dual-sgRNA libraries, L2S2 web server | High-throughput gene interaction mapping | 1.678 million perturbation signatures |
| Detection Assays | EPR spectroscopy, CRISPR-CasΦ (TCC), CRISPR-GFET | ROS measurement, DNA/RNA detection | Direct ROS detection, attomolar sensitivity |
| AB-3Prgd2 | AB-3Prgd2, MF:C137H215IN30O45S, MW:3161.3 g/mol | Chemical Reagent | Bench Chemicals |
| NCX 466 | NCX 466, MF:C20H24N2O9, MW:436.4 g/mol | Chemical Reagent | Bench Chemicals |
Future Perspectives and Clinical Translation
The integration of artificial intelligence with CRISPR technology represents the next frontier in redox system manipulation. AI-driven approaches are revolutionizing gRNA design, off-target prediction, editing efficiency optimization, and novel CRISPR system development [42]. Tools like PAMmla—a neural network trained to predict PAM recognition—enable engineering of custom enzymes with enhanced specificity, as demonstrated by successful targeting of the P23H rhodopsin mutation causing retinitis pigmentosa [43]. These computational advances promise to accelerate the development of safer, more precise redox-directed therapies.
Clinical translation of CRISPR-based redox interventions has achieved remarkable milestones, with the first FDA-approved CRISPR therapy, Casgevy, providing a cure for sickle cell disease and transfusion-dependent beta thalassemia [44]. Ongoing clinical trials are exploring CRISPR applications for diverse redox-related disorders including heart disease, hereditary transthyretin amyloidosis, hereditary angioedema, and familial hypercholesterolemia [44] [43]. The emergence of personalized CRISPR treatments, exemplified by the bespoke therapy for an infant with CPS1 deficiency developed within six months, signals a new era of precision medicine for rare genetic disorders with redox components [44].
Despite these advances, significant challenges remain in delivery efficiency, tissue specificity, and long-term safety assessment. The field must also address ethical considerations surrounding germline editing and develop equitable access models for these transformative therapies. As CRISPR technologies continue evolving toward greater precision and controllability, their integration with deepening understanding of redox biology promises novel therapeutic paradigms for the multitude of human diseases rooted in oxidative stress.
Diagram 2: Combinatorial CRISPR screening workflow for identifying redox genetic interactions.
This technical guide provides an in-depth analysis of the NRF2/KEAP1, NF-κB, and HIF-1α signaling pathways, focusing on their roles in reactive oxygen species (ROS) signaling mechanisms. These transcription factors form a complex regulatory network that orchestrates cellular responses to oxidative stress, hypoxia, and inflammation. The interplay between these pathways significantly influences disease pathogenesis, particularly in cancer and chronic inflammatory conditions, making them prominent targets for therapeutic intervention. This whitepaper summarizes current mechanistic understandings, details experimental methodologies for pathway analysis, and visualizes the complex crosstalk between these critical regulatory systems, providing researchers and drug development professionals with a comprehensive resource for investigating redox biology and developing targeted therapies.
Reactive oxygen species (ROS) function as crucial signaling molecules that profoundly influence cellular homeostasis and disease pathogenesis. The "redox code" represents a fundamental organizing principle of biological systems, where reversible redox modifications regulate protein structure, function, and signaling networks [8]. Under physiological conditions, ROS generated by mitochondrial oxidative phosphorylation, endoplasmic reticulum, and NADPH oxidases (NOX) are balanced by sophisticated antioxidant defense systems [8]. Nuclear factor-E2-related factor 2 (NRF2) serves as the master regulator of antioxidant responses, elevating the synthesis of superoxide dismutase (SOD), catalase, and key molecules like NADPH and glutathione (GSH) to maintain cellular redox homeostasis [8].
Disruption of redox equilibrium is closely linked to the pathogenesis of a wide spectrum of diseases through two primary mechanisms: direct oxidative damage to biomolecules and dysregulation of redox-sensitive signaling pathways [8]. The transcription factors NRF2, NF-κB, and HIF-1α stand at the interface of these processes, integrating redox signals into adaptive transcriptional responses. Their coordinated activities determine cellular fate in response to oxidative stress, hypoxia, and inflammatory stimuli, creating an intricate regulatory network with profound implications for health and disease [47] [48]. Understanding the mechanistic details of these pathways and their interplay provides a foundation for developing novel therapeutic strategies aimed at re-establishing redox balance in pathological conditions.
Pathway Mechanisms and Regulatory Networks
NRF2/KEAP1 Signaling Pathway
The NRF2/KEAP1 system represents the primary cellular defense mechanism against oxidative and electrophilic stress. NRF2 is a Cap 'n' Collar (CNC) basic-region leucine zipper (bZIP) transcription factor comprising seven conserved NRF2-ECH homology (Neh) domains [49] [50]. The Neh2 domain contains DLG and ETGE motifs that mediate interaction with its negative regulator, KEAP1, while Neh1 facilitates DNA binding and heterodimerization with small musculoaponeurotic fibrosarcoma (sMaf) proteins [49]. Under basal conditions, NRF2 is continuously ubiquitinated by the KEAP1-CUL3 E3 ubiquitin ligase complex and targeted for proteasomal degradation, maintaining low cellular levels with a short half-life of approximately 10-30 minutes [50].
During oxidative stress, specific cysteine residues (C273 and C288) in KEAP1 undergo modification, inactivating its E3 ligase function and stabilizing NRF2 [49]. Stabilized NRF2 translocates to the nucleus, forms heterodimers with sMaf proteins, and binds to Antioxidant Response Elements (ARE; 5'-TGACXXXGC-3') in the regulatory regions of target genes [49] [50]. This activation cascade induces the expression of hundreds of cytoprotective genes involved in glutathione synthesis (Gclc, Gclm), ROS detoxification (Gpx2, Gsts, Txnrd1), NADPH regeneration, and xenobiotic metabolism (Nqo1) [50]. Beyond antioxidant responses, NRF2 regulates diverse cellular processes including autophagy, intermediary metabolism, and proteostasis [50].
Table 1: NRF2 Domain Architecture and Functional Characteristics
| Domain | Amino Acid Region | Key Functional Features | Binding Partners |
|---|---|---|---|
| Neh1 | CNC-bZIP region | DNA binding, sMaf heterodimerization | sMaf proteins |
| Neh2 | N-terminal | KEAP1 binding (DLG/ETGE motifs), ubiquitination | KEAP1 |
| Neh3 | C-terminal | Transactivation | CHD6 |
| Neh4/5 | Central | Transcriptional activation | CBP/p300 |
| Neh6 | Serine-rich | KEAP1-independent degradation | β-TrCP/GSK-3β |
| Neh7 | - | Repression of transcriptional activity | RXRα |
Table 2: Major NRF2 Target Genes and Functional Categories
| Functional Category | Representative Genes | Biological Role |
|---|---|---|
| Glutathione System | Gclc, Gclm, Gsr1, Gpx2 | GSH synthesis, reduction, and utilization |
| Thioredoxin System | Txnrd1, Srxn1, TXN | Protein disulfide reduction |
| Xenobiotic Detoxification | Nqo1, Gsts, Mrps | Phase I/II metabolism, transport |
| NADPH Regeneration | Me1, Pgd, G6pd | NADPH production for antioxidant systems |
| Heme Metabolism | Hmox1 | Heme degradation, antioxidant protection |
NF-κB Signaling Pathway
NF-κB (nuclear factor kappa-light-chain-enhancer of activated B cells) functions as a primary regulator of inflammatory and immune responses. In its canonical activation pathway, NF-κB dimers (typically p50-p65) are sequestered in the cytoplasm by inhibitory IκB proteins [51]. Pro-inflammatory stimuli such as tumor necrosis factor-α (TNF-α), interleukin-1β (IL-1β), and pathogen-associated molecular patterns (PAMPs) activate the IκB kinase (IKK) complex, which phosphorylates IκB proteins, targeting them for ubiquitination and proteasomal degradation [51]. This process releases NF-κB dimers to translocate to the nucleus and activate transcription of genes encoding cytokines (TNF-α, IL-1β, IL-6), chemokines, adhesion molecules, and enzymes involved in inflammation (COX-2) [51].
The ROS-mediated activation of NF-κB occurs through multiple mechanisms, including IKK activation through oxidative modifications and IκB phosphorylation [48]. Importantly, NF-κB and NRF2 pathways exhibit significant crosstalk, with NRF2 activation generally repressing NF-κB signaling and subsequent pro-inflammatory gene expression, thereby creating a negative feedback loop that limits inflammation-induced oxidative stress [51] [48].
HIF-1α Signaling Pathway
Hypoxia-inducible factor-1α (HIF-1α) serves as the master regulator of cellular responses to low oxygen tension (hypoxia). HIF-1α forms a heterodimeric transcription factor with its constitutive partner HIF-1β (ARNT) [47]. Under normoxic conditions, HIF-1α undergoes rapid proteasomal degradation following prolyl hydroxylation by prolyl hydroxylase domain proteins (PHD1-3) and factor-inhibiting HIF-1 (FIH-1) [47]. Hydroxylated HIF-1α is recognized by the von Hippel-Lindau tumor suppressor protein (pVHL), which recruits an E3 ubiquitin ligase complex for degradation [47].
Under hypoxic conditions, PHD and FIH-1 activity decreases due to oxygen substrate limitation, stabilizing HIF-1α [47]. Stabilized HIF-1α translocates to the nucleus, dimerizes with HIF-1β, and binds to hypoxia response elements (HREs; 5'-(A/G)CGTG-3') in target genes [47]. HIF-1α activation promotes the expression of genes involved in angiogenesis (VEGF), glycolytic metabolism (GLUTs, PDK1), erythropoiesis (EPO), and cell survival (BCL-2) [47]. ROS signaling contributes to HIF-1α stabilization through inhibition of PHD activity, creating a direct link between oxidative stress and hypoxic responses [47].
Table 3: Comparative Features of Key Transcriptional Regulators in ROS Signaling
| Feature | NRF2 | NF-κB | HIF-1α |
|---|---|---|---|
| Primary Stimulus | Oxidative/electrophilic stress | Inflammatory cytokines, PAMPs | Hypoxia |
| Key Inhibitor | KEAP1 | IκB | pVHL |
| Degradation Mechanism | KEAP1-CUL3 ubiquitination | IKK-mediated IκB degradation | PHD/pVHL ubiquitination |
| DNA Response Element | ARE (5'-TGACXXXGC-3') | κB site | HRE (5'-(A/G)CGTG-3') |
| Dimerization Partner | sMaf proteins | p50, p52, Rel subunits | HIF-1β (ARNT) |
| Primary Biological Roles | Antioxidant defense, detoxification | Inflammation, immunity, cell survival | Angiogenesis, metabolic adaptation |
Pathway Interplay and Crosstalk
The NRF2, NF-κB, and HIF-1α pathways form an intricate regulatory network with significant functional crosstalk that determines cellular responses to stress signals. Multiple positive and negative feedback loops connect these transcription factors, creating a sophisticated control system for maintaining homeostasis [48].
NRF2-NF-κB Crosstalk: NRF2 and NF-κB generally exhibit antagonistic relationships. NRF2 activation represses NF-κB signaling and subsequent pro-inflammatory gene expression through multiple mechanisms, including enhanced antioxidant capacity that quenches ROS required for NF-κB activation and potential direct protein-protein interactions [51] [48]. Conversely, NF-κB can inhibit NRF2 signaling through competitive binding to transcriptional coactivators like CBP/p300 [48]. This reciprocal inhibition creates a molecular switch that determines whether cells mount primarily antioxidant or inflammatory responses to stress signals.
HIF-NRF2 Interplay: The relationship between HIF-1α and NRF2 is context-dependent and multifaceted. Under hypoxic conditions, HIF-1α can directly activate NRF2 transcription, thereby enhancing antioxidant defenses to manage hypoxia-associated ROS generation [47]. Additionally, mitochondrial ROS produced during hypoxia can stabilize both HIF-1α and NRF2 through inhibition of PHDs and KEAP1, respectively [47]. However, NRF2 can also limit HIF-1α signaling by reducing ROS levels, thereby promoting PHD activity and HIF-1α degradation [47]. This complex regulation allows fine-tuning of hypoxic responses based on cellular redox status.
HIF-NF-κB Interactions: HIF-1α and NF-κB demonstrate cooperative interactions in inflammatory and cancer contexts. HIF-1α stabilization can enhance NF-κB activity through direct protein interactions and synergistic transactivation of shared target genes [51] [48]. In macrophages, HIF-1α promotes polarization toward a pro-inflammatory phenotype and enhances production of cytokines like TNF-α and IL-1β through cooperation with NF-κB [51]. This cooperation establishes a positive feedback loop that amplifies inflammatory responses under hypoxic conditions, such as those found in the tumor microenvironment [47] [48].
Table 4: Experimental Modulators of NRF2, NF-κB, and HIF-1α Pathways
| Pathway | Chemical Activators | Genetic Manipulations | Inhibitors |
|---|---|---|---|
| NRF2/KEAP1 | Sulforaphane, CDDO-Me, Tert-butylhydroquinone | Keap1 knockout, Nrf2 overexpression, CRISPR-mediated Keap1 mutation | ML385, Brusatol, Trigonelline |
| NF-κB | TNF-α, IL-1β, LPS, PMA | IκBα knockout, IKKβ overexpression, RelA/p65 transgenic models | BAY-11-7082, SC-514, Bortezomib |
| HIF-1α | Dimethyloxallylglycine (DMOG), CoCl₂, Deferoxamine | HIF-1α overexpression, Vhl knockout, PHD siRNA | Acriflavine, PX-478, Echinomycin |
Experimental Protocols for Pathway Analysis
NRF2/KEAP1 Interaction Assay
Co-Immunoprecipitation Protocol: To investigate NRF2-KEAP1 interactions under oxidative stress conditions, seed HEK293T cells in 10-cm dishes at 2×10ⶠcells/dish and culture for 24 hours. Treat cells with either vehicle (DMSO) or 10µM sulforaphane for 4 hours. Harvest cells in ice-cold PBS and lyse in IP lysis buffer (25mM Tris-HCl pH 7.4, 150mM NaCl, 1mM EDTA, 1% NP-40, 5% glycerol) supplemented with protease and phosphatase inhibitors. Incubate 500µg of total protein with 2µg of anti-KEAP1 antibody overnight at 4°C with gentle rotation. Add Protein A/G PLUS-Agarose beads and incubate for 2 hours at 4°C. Wash beads four times with lysis buffer, resuspend in 2× Laemmli buffer, and analyze by Western blotting using anti-NRF2 and anti-KEAP1 antibodies [50].
ARE-Luciferase Reporter Assay: Plate HEK293 cells in 24-well plates at 1×10ⵠcells/well. After 24 hours, transfect cells with 200ng of pGL4-ARE-luciferase reporter plasmid and 20ng of pRL-TK Renilla luciferase control vector using lipofection reagent. At 24 hours post-transfection, treat cells with NRF2 activators (sulforaphane, CDDO-Me) or inhibitors (ML385) for 16 hours. Measure firefly and Renilla luciferase activities using dual-luciferase reporter assay system. Normalize ARE-driven firefly luciferase activity to Renilla luciferase activity for transfection efficiency [49].
NF-κB Activation and Nuclear Translocation
Immunofluorescence Staining Protocol: Seed cells on sterile glass coverslips in 12-well plates and culture until 70% confluent. Stimulate cells with 20ng/mL TNF-α for 0, 15, 30, and 60 minutes. Fix cells with 4% paraformaldehyde for 15 minutes at room temperature, permeabilize with 0.1% Triton X-100 for 10 minutes, and block with 5% BSA for 1 hour. Incubate with anti-p65 primary antibody (1:200) overnight at 4°C, followed by Alexa Fluor 488-conjugated secondary antibody (1:500) for 1 hour at room temperature. Mount coverslips with mounting medium containing DAPI and visualize using confocal microscopy. Quantify nuclear translocation by calculating the ratio of nuclear to cytoplasmic fluorescence intensity using ImageJ software [51].
Electrophoretic Mobility Shift Assay (EMSA): Prepare nuclear extracts from treated cells using high-salt extraction buffer. Label double-stranded NF-κB consensus oligonucleotide (5'-AGTTGAGGGGACTTTCCCAGGC-3') with γ-³²P-ATP using T4 polynucleotide kinase. Incubate 5µg of nuclear extract with labeled probe in binding buffer (10mM Tris-HCl pH 7.5, 50mM NaCl, 1mM DTT, 1mM EDTA, 5% glycerol) for 20 minutes at room temperature. For competition assays, include 100-fold excess unlabeled probe. For supershift assays, pre-incubate extracts with anti-p65 or anti-p50 antibodies. Separate protein-DNA complexes on 6% non-denaturing polyacrylamide gel in 0.5× TBE buffer at 100V for 2-3 hours. Dry gel and expose to phosphorimager screen overnight [51].
HIF-1α Stabilization and Transcriptional Activity
Hypoxia Mimetic Treatment and Western Blot: Culture cells in normoxic conditions (21% O₂, 5% CO₂) until 80% confluent. Treat cells with 100µM cobalt chloride (CoCl₂) or 1mM dimethyloxallylglycine (DMOG) for 4-16 hours to chemically mimic hypoxia. Prepare whole-cell extracts using RIPA buffer with protease inhibitors. Separate 30-50µg of protein by SDS-PAGE and transfer to PVDF membrane. Block membrane with 5% non-fat milk and incubate with anti-HIF-1α primary antibody (1:1000) overnight at 4°C. After washing, incubate with HRP-conjugated secondary antibody (1:5000) for 1 hour at room temperature. Develop blots using enhanced chemiluminescence substrate. Use anti-β-actin antibody as loading control [47].
Chromatin Immunoprecipitation (ChIP) Assay: Cross-link proteins to DNA by adding 1% formaldehyde directly to cell culture medium for 10 minutes at room temperature. Quench cross-linking with 125mM glycine for 5 minutes. Harvest cells and lyse in ChIP lysis buffer. Sonicate chromatin to shear DNA fragments between 200-500bp. Pre-clear lysate with Protein A/G beads for 1 hour at 4°C. Immunoprecipitate 100µg of chromatin with 2µg of anti-HIF-1α antibody or control IgG overnight at 4°C. Capture immune complexes with Protein A/G beads, then wash sequentially with low salt, high salt, and LiCl wash buffers. Elute chromatin and reverse cross-links at 65°C overnight. Purify DNA and analyze target gene promoters (VEGF, GLUT1) by quantitative PCR using specific primers [47].
The Scientist's Toolkit: Research Reagent Solutions
Table 5: Essential Research Reagents for Pathway Investigation
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| NRF2 Activators | Sulforaphane, CDDO-Me, Tert-butylhydroquinone | Induce ARE-driven gene expression, oxidative stress response studies | Dose-dependent effects; CDDO-Me has clinical relevance |
| KEAP1 Inhibitors | BRD4770, CPUY192018 | Disrupt NRF2-KEAP1 interaction, study NRF2 stabilization | Selectivity over other protein-protein interactions |
| NF-κB Inducers | TNF-α, IL-1β, LPS, PMA | Activate canonical NF-κB signaling, inflammation models | Timing critical for nuclear translocation studies |
| IKK Inhibitors | BAY-11-7082, SC-514, TPCA-1 | Block NF-κB activation, anti-inflammatory mechanisms | Off-target effects on other kinases possible |
| HIF Stabilizers | DMOG, CoClâ‚‚, Deferoxamine | Mimic hypoxia, study HIF target genes | Distinct mechanisms (PHD inhibition vs. iron chelation) |
| HIF Inhibitors | Acriflavine, PX-478, Echinomycin | Block HIF-1α dimerization/DNA binding, cancer models | Variable specificity for HIF-1α vs. HIF-2α |
| Antioxidant Enzymes | SOD, Catalase, GSH | Modulate ROS levels, validate redox mechanisms | Cell permeability considerations |
| ROS Indicators | Hâ‚‚DCFDA, MitoSOX, DHE | Quantify intracellular/mitochondrial ROS | Specificity for different ROS types varies |
| Pathway Reporters | ARE-luciferase, NF-κB-luciferase, HRE-luciferase | Monitor pathway activation in real-time | Normalization with constitutive controls essential |
| KBD4466 | KBD4466, MF:C24H23F3N6O, MW:468.5 g/mol | Chemical Reagent | Bench Chemicals |
| Iminostilbene-d10 | Iminostilbene-d10, MF:C14H11N, MW:203.30 g/mol | Chemical Reagent | Bench Chemicals |
Pathway Visualization Diagrams
Diagram 1: NRF2/KEAP1 Pathway Mechanism. This diagram illustrates the dual regulation of NRF2 under basal and oxidative stress conditions, highlighting the transition from proteasomal degradation to transcriptional activation of antioxidant response element (ARE)-driven genes.
Diagram 2: NF-κB Activation Pathway. This visualization depicts the canonical NF-κB signaling cascade, from inflammatory stimulus recognition to IκB degradation and subsequent activation of pro-inflammatory gene transcription.
Diagram 3: HIF-1α Regulation by Oxygen. This diagram contrasts HIF-1α regulation under normoxic and hypoxic conditions, demonstrating the oxygen-dependent switch between degradation and transcriptional activation.
Diagram 4: Pathway Crosstalk in ROS Signaling. This integrated network visualization illustrates the complex interactions between NRF2, NF-κB, and HIF-1α pathways, highlighting both antagonistic and cooperative relationships in response to various cellular stressors.
Reactive oxygen species (ROS) are increasingly recognized not merely as damaging agents but as crucial signaling molecules that regulate fundamental cellular processes through oxidative post-translational modifications (Oxi-PTMs) [1] [7]. The sulfur-containing amino acid cysteine serves as a primary sensor for redox changes due to its high susceptibility to oxidation, with cysteine thiols acting as molecular switches that modulate protein function, stability, and interactions in response to fluctuating ROS levels [52] [53] [54]. Proteomic and redoxomic profiling represents a powerful analytical approach for comprehensively identifying these oxidation-sensitive protein targets on a global scale, providing critical insights into redox signaling mechanisms in both physiological and pathological contexts [52] [54]. Within the broader thesis of ROS signaling mechanisms research, this technical guide outlines current methodologies, key findings, and practical applications for identifying and validating redox-sensitive proteins across biological systems.
Quantitative Approaches in Redox Proteomics
Mass Spectrometry-Based Methodologies
Modern redox proteomics employs sophisticated mass spectrometry (MS) techniques coupled with selective thiol-labeling strategies to quantitatively map redox-sensitive cysteine residues at proteome-wide scales. The sequential iodoTMT (tandem mass tag) labeling approach enables precise, site-specific quantification of reversible cysteine modifications in complex biological samples [52]. This method involves blocking reduced protein thiols with isobaric iodoacetyl-TMT reagents, selectively reducing reversibly oxidized thiols (e.g., disulfides, sulfenic acids), and labeling these newly reduced thiols with a different TMT reagent for subsequent enrichment and quantification via LC-MS/MS [52]. Similarly, the OxICAT (isotope-coded affinity tag) technology combines differential thiol trapping with isotope coding to determine the in vivo oxidation percentage of individual cysteine residues [54]. These approaches have enabled the identification and quantification of thousands of redox-sensitive cysteine sites, revealing the extensive scope of redox regulation across cellular proteomes.
Key Quantitative Findings from Redox Profiling Studies
Table 1: Summary of Major Redox Proteomics Studies and Their Findings
| Study System | Profiling Method | Cysteine Sites Identified | Key Findings | Reference |
|---|---|---|---|---|
| Mouse fetal & adult HSPCs | Sequential iodoTMT | 4,438 cysteines (1,850 proteins) | Fetal HSPCs showed higher oxidation susceptibility; redox changes in metabolic & protein homeostasis proteins during leukemogenesis | [52] |
| S. cerevisiae (yeast) | OxICAT | 6,277 cysteine peptides (2,733 proteins) | >93% of thiols reduced under baseline; mitochondrial ROS regulate translation via redox switches | [54] |
| Diverse immune cells | Single-cell mass cytometry (SN-ROP) | 33 ROS-related proteins simultaneously | Cell-type-specific redox patterns; dynamic redox shifts in CD8+ T cells post-stimulation | [55] |
Table 2: Oxidation Levels of Protein Functional Classes in Steady-State Conditions
| Functional Category | Representative Proteins | Typical Oxidation Range | Biological Significance |
|---|---|---|---|
| Metabolic enzymes | GAPDH, Triosephosphate isomerase | 15-30% | Regulation of metabolic flux in response to ROS |
| Translation machinery | Ribosomal proteins, Initiation factors | 15-30% | Global control of protein synthesis |
| Antioxidant systems | Sod1, Peroxiredoxins | 60-100% | Functional disulfide formation; high activity state |
| Zinc-binding proteins | Metalloproteases, Transcription factors | 15-30% | Zinc release as redox regulatory mechanism |
Experimental Protocols for Redox Proteomics
Cell Preparation and Lysis Under Redox-Preserving Conditions
Proper sample preparation is critical for preserving the in vivo redox state of protein thiols during analysis. The following protocol outlines the essential steps for redox proteomics sample preparation:
Rapid inactivation of metabolism: Immediately quench cell metabolism by adding cell pellets directly to ice-cold 10-15% trichloroacetic acid (TCA) or by rapid freezing in liquid nitrogen [54]. TCA denatures proteins and acidifies the environment, effectively "freezing" the redox state by inhibiting cellular oxidoreductases.
Cell lysis under denaturing conditions: Lyse TCA-precipitated cells in a buffer containing 6-8 M urea or 2% SDS, 50-100 mM Tris-HCl (pH 8.0-8.5), and protease inhibitors. The strong denaturants prevent artificial thiol-disulfide exchange during sample processing [52] [54].
Blocking reduced thiols: Add a thiol-blocking reagent such as 20-40 mM iodoacetamide or N-ethylmaleimide to covalently alkylate reduced cysteine residues, preventing their oxidation during subsequent steps. Incubate for 1 hour in the dark at room temperature [52].
Enrichment and Quantification of Redox-Sensitive Cysteines
Following initial sample preparation, the specific workflow for enriching and quantifying oxidized cysteine residues proceeds as follows:
Selective reduction of oxidized thiols: After removing excess alkylating reagent, add a selective reducing agent (e.g., 10-20 mM ascorbate for reversibly oxidized cysteines or 5-10 mM DTT for disulfides) to specifically reduce the oxidized cysteine populations of interest [52].
Tagging of newly reduced thiols: Label the newly reduced thiols with a distinct isotope-coded or isobaric tag (e.g., ICAT reagents, TMT variants) for subsequent quantification. For iodoTMT, use 0.5-1 mM reagent and incubate for 2 hours in the dark [52].
Affinity enrichment and MS analysis: Capture tagged peptides using affinity purification (e.g., anti-TMT resin), then analyze by nanoLC-MS/MS. Quantify the relative abundance of redox forms using the reporter ion intensities for isobaric tags or the heavy/light ratios for isotopic labeling [52] [54].
Visualization of Redox Proteomics Workflows and Signaling Pathways
Experimental Workflow for Comprehensive Redox Profiling
Redox Proteomics Experimental Workflow
Cysteine Oxidation States and Modification Types
Cysteine Oxidation States and Modifications
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Redox Proteomics Studies
| Reagent Category | Specific Examples | Function & Application |
|---|---|---|
| Thiol-blocking reagents | Iodoacetamide, N-ethylmaleimide, Methyl methanethiosulfonate | Alkylate reduced cysteine thiols to prevent post-lysis oxidation |
| Isotope-coded tags | ICAT reagents, iodoTMT, OxICAT | Differential labeling of reduced vs. oxidized thiol populations for MS quantification |
| Selective reducing agents | Ascorbate, Arsenite, DTT, TCEP | Specific reduction of particular oxidized cysteine forms (e.g., disulfides, sulfenic acids) |
| Affinity purification | Anti-TMT resin, Streptavidin beads, Thiopropyl sepharose | Enrichment of tagged cysteine-containing peptides from complex mixtures |
| ROS detection probes | DCFDA, DHE, MitoSOX, roGFP | Measurement of intracellular ROS levels and redox potential |
| Antioxidant enzymes | Catalase, Superoxide dismutase, Peroxiredoxins | Tools for modulating ROS levels in experimental systems |
| OPBP-1 | OPBP-1, MF:C64H92N20O19S, MW:1477.6 g/mol | Chemical Reagent |
| UM-164 | UM-164, MF:C30H31F3N8O3S, MW:640.7 g/mol | Chemical Reagent |
Biological Implications of Redox-Sensitive Protein Targets
Regulation of Hematopoietic Development and Leukemogenesis
Redox proteomic analyses of fetal and adult hematopoietic stem and progenitor cells (HSPCs) have revealed distinct redox landscapes that contribute to their differential cellular behaviors [52]. Fetal HSPCs demonstrate higher susceptibility to thiol oxidation compared to their adult counterparts, with 174 peptides (from 153 unique proteins) showing significantly higher oxidation levels in fetal cells [52]. These redox-sensitive proteins are prominently involved in metabolic pathways and protein homeostasis, suggesting that developmental differences in redox regulation may underlie the enhanced proliferative and translational capacity of fetal HSPCs. During MLL-ENL leukemogenesis, additional oxidation changes occur in mitochondrial respiration and protein homeostasis pathways in fetal HSPCs, pinpointing potential targetable redox-sensitive proteins in in utero-initiated leukemia [52].
Mitochondrial ROS Regulation of Global Translation
Comprehensive redox profiling in yeast has demonstrated that mitochondria-derived ROS serve as signaling molecules that reversibly control global protein synthesis through oxidation of specific translation machinery components [54]. Under conditions of mitochondrial dysfunction, increased ROS production leads to oxidative modification of cysteine residues in ribosomal proteins, translation initiation factors, and aminoacyl-tRNA synthetases, effectively attenuating global translation rates as an adaptive response to metabolic stress [54]. This mechanism represents a conserved pathway for crosstalk between mitochondrial status and the biosynthetic capacity of the cell, with potential implications for understanding pathologies associated with mitochondrial dysfunction.
Single-Cell Redox Network Profiling in Immune Function
Recent advances in single-cell mass cytometry have enabled high-dimensional profiling of redox signaling networks at single-cell resolution through the Signaling Network under Redox Stress Profiling (SN-ROP) approach [55]. This technology simultaneously quantifies 33 ROS-related proteins, including transporters, enzymes, oxidative stress products, and associated signaling pathways, revealing cell-type-specific redox patterns and dynamic redox shifts during immune activation [55]. Application of SN-ROP to CD8+ T cells following antigen stimulation has uncovered coordinated redox network remodeling that supports T cell effector functions, while distinct redox profiles in CAR-T cells correlate with persistence and therapeutic efficacy [55].
Technical Considerations and Future Perspectives
The field of redox proteomics continues to evolve with emerging technologies that address current limitations. Single-cell redox profiling methods like SN-ROP represent a significant advancement beyond bulk measurements, enabling the characterization of redox heterogeneity within cell populations and its functional consequences [55]. Additionally, the integration of redox proteomics with other omics approaches (transcriptomics, metabolomics) provides more comprehensive understanding of redox regulation in biological systems. Future methodological developments will likely focus on improving spatial resolution for subcellular redox compartmentalization, temporal resolution for capturing dynamic redox changes, and expansion to other oxidative modifications beyond cysteine oxidation. As these technologies mature, their application to disease models and therapeutic development will continue to illuminate the complex role of redox signaling in health and disease, potentially identifying novel therapeutic targets for conditions characterized by redox dysregulation.
High-Throughput Screening Platforms for Redox-Active Compound Discovery
Reactive oxygen species (ROS) homeostasis represents a fundamental physiological process wherein cells dynamically regulate their ROS levels to ensure survival and execute diverse biological functions [1]. These highly reactive molecules, including superoxide anion (•O2–), hydrogen peroxide (H2O2), and hydroxyl radicals (•OH), serve as critical signaling agents while simultaneously posing potential toxic threats when dysregulated [1]. Within the context of ROS signaling mechanisms research, high-throughput screening (HTS) platforms have emerged as indispensable tools for identifying and characterizing redox-active compounds that modulate these delicate biological balances. The discovery of such compounds provides critical insights into redox signaling pathways and creates opportunities for therapeutic interventions in diseases marked by oxidative stress imbalances, including cardiovascular diseases, neurodegenerative disorders, cancers, and metabolic conditions [1] [8].
The integration of HTS methodologies specifically designed for redox-active compound discovery has transformed our ability to systematically investigate ROS signaling mechanisms at scale. These platforms enable researchers to rapidly evaluate thousands of chemical entities for their effects on ROS homeostasis, cellular redox states, and specific oxidative post-translational modifications that regulate protein function [7]. This technical guide examines the core components, experimental protocols, and data management strategies that constitute modern HTS platforms tailored for advancing our understanding of redox biology and identifying novel therapeutic candidates targeting ROS-related pathways.
Core Components of HTS Platforms for Redox Biology
Integrated Robotic and Computational Architecture
Modern HTS platforms for redox-active compound discovery combine automated physical systems with sophisticated computational guidance. The physical layer typically encompasses robotic arms for precise liquid and powder handling, automated incubation systems maintaining constant temperature control, and high-throughput analytical instrumentation such as quantitative NMR (qNMR) or UV-Vis spectroscopy [56]. This automation enables the preparation and analysis of hundreds of samples in parallel, dramatically accelerating the traditionally labor-intensive process of solubility measurement and compound characterization. For instance, one documented automated platform reduced processing time from approximately 525 minutes per sample manually to just 39 minutes per sample—a 13-fold improvement in efficiency [56].
The computational layer incorporates active learning algorithms, particularly Bayesian optimization (BO), which serves as an intelligent guide for the experimental workflow [56]. This algorithm consists of a surrogate model that predicts compound properties based on existing data, and an acquisition function that strategically selects the most promising candidates for subsequent testing. This closed-loop system continuously refines its predictions based on experimental outcomes, enabling the rapid identification of optimal compounds or solvent systems with minimal experimental effort. Research demonstrates that such integrated systems can identify high-performing solvents for redox-active molecules from libraries of thousands of candidates while requiring solubility assessments for fewer than 10% of the total candidates [56].
Specialized Assay Design for Redox Applications
HTS campaigns targeting redox-active compounds require specialized assay designs that capture the dynamic and multifaceted nature of ROS biology. Key considerations include the selection of appropriate detection methods for various ROS species, incorporation of relevant biological models (cell-free, cellular, or enzymatic), and implementation of controls that account for the rapid reactivity and transient nature of many redox species. For cell-based screens, assays may focus on measuring ROS production, assessing changes in antioxidant capacity, or evaluating the activation of redox-sensitive transcription factors like NRF2, which regulates the expression of antioxidant enzymes including superoxide dismutase (SOD), catalase, and glutathione peroxidase (GPx) [8].
Assay formats commonly employed in redox-focused HTS include:
- Binding assays to identify compounds that interact with known redox-sensitive proteins
- Functional cell assays to detect modulators of ROS production or scavenging
- ADMET assays to evaluate absorption, distribution, metabolism, excretion, and toxicity properties of redox-active compounds [57]
The choice of assay format depends on the specific research objectives, whether targeting the discovery of novel antioxidants, pro-oxidants for selective cancer cell toxicity, or modulators of specific ROS signaling pathways.
Integrated HTS Platform Workflow
The following diagram illustrates the seamless integration of high-throughput experimentation with machine learning guidance in a modern HTS platform for redox-active compound discovery:
HTS Platform with Active Learning
This integrated workflow demonstrates the closed-loop operation between experimental and computational components, wherein each cycle of experimentation informs the next round of candidate selection, dramatically accelerating the discovery process for redox-active compounds with desired properties.
Experimental Protocols for Redox-Active Compound Screening
High-Throughput Solubility Determination for ROMs
The solubility of redox-active organic molecules (ROMs) represents a critical parameter in redox flow battery development and pharmacological applications where compound concentration directly influences energy density or therapeutic efficacy [56]. The following protocol details the 'excess solute' method for thermodynamic solubility measurement, adapted for high-throughput implementation:
Materials Required:
- Robotic liquid handling system with powder dispensing capability
- Temperature-controlled incubation chambers
- Quantitative NMR (qNMR) system or alternative analytical instrumentation
- Redox-active molecule of interest (e.g., 2,1,3-benzothiadiazole)
- Solvent library (single solvents and binary mixtures)
Procedure:
- Sample Preparation: Utilize a robotic arm to dispense solid ROM (typically 5-10 mg) into individual vials followed by automated addition of solvents (typically 0.5-1 mL) from the library [56].
- Equilibration: Transfer the prepared samples to temperature-controlled incubation chambers maintained at 20°C with continuous agitation for 8 hours to ensure thermodynamic equilibrium is reached [56].
- Liquid Sampling: After equilibration, automatically transfer saturated solutions to analysis vessels (e.g., NMR tubes), ensuring no solid transfer occurs.
- Concentration Determination: Analyze samples using qNMR spectroscopy, comparing signal intensities between solvent and analyte to determine molar solubility (mol Lâ»Â¹) [56].
- Data Processing: Automate the conversion of spectral data to solubility values, with incorporation of control samples (e.g., 2 M and saturated solutions in ACN) in each batch to ensure data quality and reproducibility [56].
Validation Metrics: The protocol should yield reproducibility with relative standard deviation of less than 5% for control samples across multiple batches [56].
Cell-Based ROS Modulation Screening
For biological applications, screening for compounds that modulate ROS levels or signaling requires different methodological approaches:
Materials Required:
- Cell culture system relevant to research focus (primary cells or cell lines)
- ROS-sensitive fluorescent probes (e.g., H2DCFDA, MitoSOX Red)
- Microplate readers capable of fluorescence detection
- Automated liquid handlers for cell culture and compound addition
- Positive control compounds (e.g., menadione for ROS induction, N-acetylcysteine for ROS reduction)
Procedure:
- Cell Preparation: Seed cells in 96- or 384-well plates at optimized density and culture until 70-80% confluency.
- Compound Treatment: Using automated liquid handling, add test compounds across a range of concentrations, including appropriate positive and negative controls.
- ROS Detection: At predetermined time points, incubate cells with ROS-sensitive fluorescent probes according to established protocols, ensuring consistent incubation conditions.
- Signal Measurement: Quantify fluorescence using appropriate microplate reader settings with maintained temperature at 37°C and CO₂ control if possible.
- Data Analysis: Normalize signals to vehicle controls and calculate fold-changes in ROS production relative to baseline.
Validation Metrics: Assay quality should be monitored through Z'-factor calculations (>0.5 indicates robust assay), coefficient of variation, and signal-to-background ratios consistent with HTS standards.
Quantitative Performance Data
The table below summarizes key performance metrics from documented HTS platforms applied to redox-active material discovery:
Table 1: HTS Platform Performance Metrics
| Platform Component | Performance Metric | Reported Value | Experimental Context |
|---|---|---|---|
| Throughput Capacity | Samples per batch | 42+ samples simultaneously | BTZ solubility screening [56] |
| Time Efficiency | Processing time per sample | ~39 minutes | Automated 'excess solute' method [56] |
| Time Efficiency Comparison | Manual processing time per sample | ~525 minutes | Traditional 'excess solute' method [56] |
| Computational Efficiency | Search space reduction | >90% (testing <10% of library) | Bayesian optimization with 2000+ solvent library [56] |
| Solubility Achievement | Maximum BTZ solubility | >6.20 M | Binary solvent mixtures with 1,4-dioxane [56] |
| Data Quality | Control sample reproducibility | <5% RSD | qNMR measurements across batches [56] |
These quantitative benchmarks demonstrate the significant advantages of integrated HTS platforms over traditional manual approaches, particularly in accelerating the discovery process while maintaining data quality and reproducibility.
ROS Signaling Mechanisms in Cellular Context
To fully appreciate the biological relevance of HTS for redox-active compounds, understanding ROS signaling mechanisms is essential. The following diagram illustrates key ROS signaling pathways and their cellular impacts:
ROS Signaling Pathways and Cellular Outcomes
This diagram highlights how ROS generated from various cellular sources can modify specific cellular targets through oxidative post-translational modifications (Oxi-PTMs), leading to diverse cellular outcomes. HTS platforms aim to identify compounds that can selectively modulate these pathways to achieve therapeutic benefits.
The Scientist's Toolkit: Essential Research Reagents and Materials
The table below catalogues essential reagents, materials, and computational tools required for implementing HTS platforms for redox-active compound discovery:
Table 2: Essential Research Reagents and Materials for HTS in Redox Biology
| Category | Specific Examples | Function/Application | Reference Source |
|---|---|---|---|
| Redox-Active Molecules | 2,1,3-benzothiadiazole (BTZ) | Model ROM for solubility and performance screening | [56] |
| Organic Solvents | Acetonitrile (ACN), 1,4-dioxane | Single solvents and binary mixtures for solubility enhancement | [56] |
| Analytical Instruments | qNMR, UV-Vis spectroscopy | Quantitative solubility measurement and compound characterization | [56] |
| Automation Equipment | Robotic liquid handlers, powder dispensers | High-throughput sample preparation and processing | [56] |
| Cell Culture Reagents | ROS-sensitive fluorescent probes (H2DCFDA, MitoSOX) | Detection of intracellular ROS in cell-based assays | [8] |
| Data Repositories | PubChem, ChEMBL, BindingDB | Sources of HTS data and compound bioactivity information | [57] |
| Computational Tools | Bayesian optimization algorithms, Tanaguru Contrast-Finder | Active learning guidance and accessibility-compliant visualization | [56] |
| Selnoflast calcium | Selnoflast calcium, MF:C20H27CaN3O3S, MW:429.6 g/mol | Chemical Reagent | Bench Chemicals |
| Rac1 inhibitor W56 tfa | Rac1 inhibitor W56 tfa, MF:C76H118F3N19O25S, MW:1786.9 g/mol | Chemical Reagent | Bench Chemicals |
This toolkit represents the core components necessary for establishing a robust HTS platform targeting redox-active compounds. The selection of specific reagents and instruments should be guided by the particular research objectives, whether focused on energy storage materials or pharmacologically active compounds.
Data Management and Public Repositories
Effective management of HTS data represents a critical component of modern redox-active compound discovery campaigns. Public repositories such as PubChem provide essential infrastructure for storing, sharing, and accessing large-scale screening data [57]. As of 2015, PubChem housed over 60 million unique chemical structures and 1 million biological assays from more than 350 contributors [57]. These resources enable researchers to leverage existing HTS data to inform experimental design and avoid duplication of effort.
Key considerations for HTS data management include:
- Standardized Formats: Utilization of consistent data formats (e.g., CSV, ASN, JSON) facilitates data sharing and integration across platforms [57].
- Structured Metadata: Comprehensive documentation of experimental conditions (temperature, equilibrium time, measurement technique) is essential for data interpretation and reproducibility [56].
- Programmatic Access: Implementation of REST-style interfaces such as PubChem's PUG-REST enables automated data retrieval for large compound sets [57].
- Quality Metrics: Incorporation of control samples and calculation of reproducibility measures (e.g., relative standard deviation) ensures data reliability [56].
Proper attention to data management practices enhances the value of HTS campaigns and contributes to the growing body of publicly available information on redox-active compounds and their biological activities.
High-throughput screening platforms represent transformative tools for advancing our understanding of redox signaling mechanisms and accelerating the discovery of redox-active compounds with therapeutic potential. The integration of automated experimental systems with active learning algorithms creates efficient, closed-loop workflows that dramatically reduce the time and resources required to identify promising candidates from vast chemical libraries. These platforms have demonstrated remarkable success in specific applications such as solubility optimization for redox-active molecules in energy storage, with comparable potential for pharmacological compound discovery.
As ROS signaling research continues to elucidate the complex roles of reactive oxygen species in health and disease, HTS technologies will play an increasingly vital role in translating mechanistic insights into targeted interventions. The ongoing development of more sophisticated screening assays, computational guidance systems, and data management infrastructure will further enhance our ability to discover and optimize compounds that selectively modulate redox pathways for therapeutic benefit.
Overcoming ROS Targeting Challenges: Specificity, Resistance, and Therapeutic Windows
Reactive oxygen species (ROS) function as critical signaling molecules in numerous biological processes, yet their dysregulation contributes to the pathogenesis of various diseases, including cancer [58]. The "Specificity Paradox" refers to the fundamental challenge in redox biology of achieving selective modulation of distinct ROS-mediated pathways without triggering global antioxidant effects that disrupt essential redox homeostasis. This paradox presents a significant obstacle in developing effective redox-based therapies, as broad-spectrum antioxidants often fail to account for the nuanced, context-dependent roles of ROS in cellular signaling [8] [59]. While oxidative stress occurs when ROS production overwhelms detoxification capacity, physiological ROS levels act as crucial second messengers in proliferation, differentiation, and survival pathways [34]. The therapeutic goal has therefore shifted from non-specific ROS scavenging to precision interventions that target pathological ROS sources or signaling nodes while preserving physiological redox signaling [8]. This whitepaper examines the molecular basis of this paradox and outlines emerging strategies to achieve selective ROS modulation for therapeutic applications.
Cellular redox homeostasis maintains a delicate balance between ROS generation and elimination. Understanding the compartmentalization and specificity of these systems is foundational to addressing the specificity paradox.
ROS encompass diverse molecules with varying reactivity, half-lives, and biological targets. The primary ROS sources contribute differently to redox signaling and stress [60].
Table 1: Primary Intracellular ROS Sources and Their Characteristics
| ROS Source | Subcellular Location | Primary ROS Produced | Biological Functions | Regulation in Disease |
|---|---|---|---|---|
| Mitochondrial ETC | Mitochondria (Complexes I & III) | O₂•â», Hâ‚‚Oâ‚‚ | Energy metabolism, hypoxia signaling | Hyperactive in cancer; increased electron leakage [58] [34] |
| NADPH Oxidases (NOX) | Plasma membrane, ER, peroxisomes | O₂•⻠(NOX1-3), H₂O₂ (NOX4, DUOX) | Cell signaling, growth factor response | Oncogene activation (e.g., RAS); sustained activation [58] [59] |
| Endoplasmic Reticulum | ER lumen | Hâ‚‚Oâ‚‚ | Protein folding (disulfide bond formation) | ER stress; unfolded protein response [58] |
| Peroxisomes | Peroxisomal matrix | Hâ‚‚Oâ‚‚ | Fatty acid oxidation | Altered metabolism in cancer [34] [60] |
The Antioxidant Defense Network
Cells maintain sophisticated, multi-layered antioxidant systems that work in concert to regulate ROS levels. The specificity and subcellular localization of these components create discrete redox environments [34] [8].
Table 2: Major Cellular Antioxidant Systems
| Antioxidant System | Key Components | Specific Function | Subcellular Localization |
|---|---|---|---|
| Enzymatic First Line | Superoxide dismutase (SOD), Catalase (CAT), Glutathione peroxidase (GPx) | Converts O₂•⻠to H₂O₂ (SOD); decomposes H₂O₂ to H₂O/O₂ (CAT, GPx) | Cytosol, mitochondria, extracellular space [34] [8] |
| Redox Buffer Systems | Glutathione (GSH)/GSSG, Thioredoxin (Trx)/Trx reductase | Maintains reduction potential; reduces disulfides | Cytosol, mitochondria, nucleus [58] [8] |
| Master Regulator | NRF2-Keap1 axis | Transcriptional control of antioxidant genes | Cytosol (Keap1), nucleus (NRF2) [58] |
| Non-Enzymatic Scavengers | Vitamin C, Vitamin E | Direct ROS neutralization; regenerates other antioxidants | Aqueous (vitamin C), lipid (vitamin E) compartments [34] |
The NRF2-Keap1 axis represents the master regulator of the antioxidant response. Under basal conditions, Keap1 targets NRF2 for proteasomal degradation. During oxidative stress, specific cysteine sensors in Keap1 are modified, leading to NRF2 stabilization, nuclear translocation, and activation of antioxidant gene expression [58]. This system exemplifies the specificity possible in antioxidant responses, as different ROS species and levels activate distinct patterns of gene expression.
Molecular Mechanisms of the Specificity Paradox
Spatial and Temporal Dimensions of ROS Signaling
The signaling specificity of ROS is governed by their spatiotemporal dynamics. The same ROS molecule can produce different effects based on its subcellular origin, concentration, and duration of exposure [59].
- Spatial Compartmentalization: Mitochondrial ROS (mtROS) and NOX-derived ROS activate distinct signaling pathways despite potentially identical chemical identities. mtROS preferentially influence hypoxic signaling and apoptosis, while NOX-derived ROS often amplify growth factor signaling [60] [59].
- Temporal Dynamics: Acute versus chronic ROS exposure produces fundamentally different outcomes. Low-level, pulsatile ROS activates signaling pathways like PI3K/AKT and MAPK/ERK that promote cell survival and proliferation. Sustained ROS elevation triggers oxidative damage to lipids, proteins, and DNA, leading to senescence or death [59].
- Concentration Dependence: The biphasic nature of ROS responses creates a narrow therapeutic window. The threshold for transitioning from physiological signaling to pathological stress varies by cell type, metabolic state, and genetic background [58] [59].
Limitations of Conventional Antioxidant Approaches
Broad-spectrum antioxidants face inherent limitations due to their inability to distinguish between pathological and physiological ROS. Clinical trials of non-specific antioxidants like vitamin E and N-acetylcysteine (NAC) have yielded disappointing results, sometimes even worsening outcomes [8]. This failure stems from several factors:
- Disruption of Redox Signaling: Global antioxidant administration indiscriminately quenches both pathological and physiological ROS pools, interfering with normal redox signaling [8].
- Lack of Target Engagement Specificity: Conventional antioxidants react chemically with ROS based on reactivity rather than biological context, lacking the compartmental specificity of native antioxidant enzymes [60].
- Compensatory Mechanisms: Chronic antioxidant exposure can trigger feedback upregulation of endogenous ROS production or downregulation of antioxidant defenses, mitigating long-term efficacy [58].
Diagram 1: Specificity Paradox in ROS Modulation
Experimental Approaches for Specific ROS Modulation
Advanced ROS Detection and Quantification Methods
Precise ROS measurement is prerequisite for targeted modulation. Advanced techniques now enable specific detection of distinct ROS species with subcellular resolution [60].
Table 3: Advanced Methodologies for Specific ROS Detection
| Method/Technique | ROS Detected | Specificity Features | Applications in Research | Limitations |
|---|---|---|---|---|
| EPR/ESR Spectroscopy | Multiple specific radicals | Identifies radical species; can differentiate mitochondrial vs global ROS | in vivo ROS discrimination; mitochondrial ROS tracking [61] | Requires specialized equipment; technical complexity |
| Redox-Sensitive GFP Probes (e.g., HyPer) | Hâ‚‚Oâ‚‚ | Genetically encoded; compartment-specific targeting | Real-time Hâ‚‚Oâ‚‚ dynamics in subcellular locales [59] | Limited to transfectable cells; potential pH interference |
| Chemical Probes (e.g., MitoSOX) | Mitochondrial O₂•⻠| Chemical targeting to mitochondria | Selective detection of mtROS in live cells [60] | Specificity concerns; potential artifacts |
| LC-MS Oxidized Metabolites | Lipid peroxidation products | Specific molecular fingerprints of oxidative damage | Biomarker discovery; ferroptosis detection [60] | Endpoint measurement only |
Experimental Protocol: Discriminating Mitochondrial vs. Global ROS Using EPR
Electron paramagnetic resonance (EPR) spectroscopy represents a gold standard for specific ROS detection. The following protocol enables non-invasive discrimination between mitochondrial and global ROS production in solid tumors [61]:
Principle: EPR utilizes spin probes with different subcellular localization and ROS sensitivity. Mitochondria-targeted probes (e.g., mitoTEMPO) versus cell-permeable probes (e.g., 3-carbamoyl-proxyl) enable compartment-specific ROS assessment.
Procedure:
- Animal Model Preparation: Establish solid tumor xenografts in appropriate immunocompromised mice (e.g., 5-7 weeks post-inoculation).
- Spin Probe Administration: Inject mice intravenously with either:
- Mitochondria-targeted probe: mitoTEMPO (5 mg/kg in saline)
- Global ROS probe: 3-carbamoyl-proxyl (7.5 mg/kg in saline)
- In Vivo EPR Measurement:
- Anesthetize animals (isoflurane/oxygen mixture)
- Position tumor in EPR resonator cavity
- Acquire spectra at X-band (9.5 GHz) with modulation amplitude 2 G, microwave power 20 mW
- Measure signal intensity decay over 30-60 minutes
- Data Analysis:
- Calculate ROS-dependent signal decay rates for each probe
- Compare mitochondrial vs. global ROS production rates
- Normalize to tumor volume and perfusion status
Key Controls:
- Include non-tumor bearing controls for baseline ROS levels
- Validate mitochondrial specificity with rotenone (Complex I inhibitor)
- Confirm ROS dependence with NAC pre-treatment
This methodology enables direct comparison of compartmental ROS production in living systems, providing critical insights for targeted therapeutic development.
Strategic Approaches to Overcome the Specificity Paradox
Source-Directed Therapeutic Interventions
Rather than targeting ROS generally, emerging strategies focus on inhibiting specific ROS sources or activating localized ROS production in pathological cells.
- NOX Isoform-Specific Inhibitors: Development of small molecules that selectively target specific NOX isoforms (e.g., NOX4 vs NOX2) overcomes the redundancy and pleiotropy of pan-NOX inhibition [59].
- Mitochondrial ROS Modulators: Compounds like mitoQ and SkQ1 selectively accumulate in mitochondria, enabling compartment-specific antioxidant effects while preserving cytosolic redox signaling [8].
- Pro-oxidant Therapies: Agents like high-dose vitamin C and arsenic trioxide (ATO) exploit the already elevated ROS state in cancer cells, further increasing ROS to lethal levels through Fenton chemistry and specific enzyme inhibition [58].
Targeting ROS Signaling Nodes and Antioxidant Adaptations
An alternative approach focuses on disrupting cancer-specific adaptations to oxidative stress rather than ROS directly.
- NRF2 Pathway Inhibition: Cancer cells with heightened NRF2 activity become dependent on this antioxidant pathway. Inhibitors like brusatol or ML385 specifically target NRF2, disabling this adaptation and restoring sensitivity to endogenous ROS [58].
- Ferroptosis Induction: Inhibition of the glutathione system via cysteine uptake inhibitors (sulfasalazine, erastin) or direct GPX4 inhibition triggers iron-dependent lipid peroxidation and cell death, selectively targeting tumors with high iron metabolism [58].
- Thioredoxin System Targeting: Auranofin irreversibly inhibits thioredoxin reductase (TrxR), disrupting this key antioxidant system and selectively killing cells dependent on Trx activity [58].
Diagram 2: Strategic Approaches to Specific ROS Modulation
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for Specific ROS Modulation Studies
| Reagent/Category | Specific Function | Key Applications | Considerations for Use |
|---|---|---|---|
| MitoTEMPO | Mitochondria-targeted SOD mimetic | Specific mitochondrial O₂•⻠scavenging; controls for mtROS effects | Validate mitochondrial localization; assess effects on energy metabolism [61] |
| NOX Isoform Inhibitors (e.g., GKT137831 for NOX1/4) | Selective inhibition of specific NOX isoforms | Dissecting NOX vs mitochondrial ROS signaling; therapeutic development | Verify isoform specificity; monitor compensatory mechanisms [59] |
| Brusatol/ML385 | NRF2 pathway inhibitors | Targeting antioxidant adaptation; chemosensitization | Monitor NRF2 target gene expression; assess toxicity in normal cells [58] |
| Erastin/RSL3 | Ferroptosis inducers (system xcâ»/GPX4 inhibition) | Selective killing of high-iron or mesenchymal cells | Confirm lipid peroxidation; test iron chelator rescue [58] |
| HyPer Family Probes | Genetically encoded Hâ‚‚Oâ‚‚ sensors | Compartment-specific Hâ‚‚Oâ‚‚ dynamics; real-time signaling studies | Control for pH effects; optimize expression levels [59] |
| Auranofin | Thioredoxin reductase inhibitor | Targeting Trx antioxidant system; combination therapies | Assess TrxR activity inhibition; monitor glutathione compensation [58] |
Overcoming the specificity paradox in ROS modulation requires a paradigm shift from broad antioxidant approaches to precision redox medicine. Success hinges on understanding and leveraging the spatiotemporal specificity inherent to native redox signaling systems. Future progress will depend on developing increasingly sophisticated tools for compartment-specific ROS detection and intervention, enabling researchers to dissect the nuanced roles of distinct ROS in health and disease. The strategic approaches outlined—including source-directed therapies, signaling node targeting, and spatiotemporal control—represent promising pathways toward resolving this fundamental challenge in redox biology. As these technologies mature, they will pave the way for truly selective redox-based therapeutics that manipulate pathological ROS signaling while preserving essential physiological functions.
Reactive Oxygen Species (ROS) are a group of oxygen-containing, highly reactive molecules that function as a double-edged sword in cancer biology. At physiological levels, ROS act as critical signaling molecules regulating cellular metabolism, differentiation, and survival [1]. Under pathological accumulation, however, ROS cause macromolecular damage, leading to oxidative stress, genetic instability, and cell death [62] [1]. Tumor cells exploit this duality by activating sophisticated adaptive mechanisms to maintain ROS levels within a pro-tumorigenic window—sufficient to drive mutagenesis and proliferation but insufficient to trigger cell death. Central to this adaptation is the transcriptional activation of the Nuclear factor erythroid 2-related factor 2 (NRF2), a master regulator of cellular redox homeostasis [63] [64].
This whitepaper, framed within broader research on ROS signaling mechanisms, delineates the pivotal role of constitutive NRF2 activation as a cornerstone of tumor resistance. We provide an in-depth analysis of how NRF2-driven metabolic reprogramming, immune evasion, and adaptive survival pathways confer resilience to anticancer therapies. The content is structured to equip researchers and drug development professionals with a detailed mechanistic understanding, supported by summarized quantitative data, experimental protocols, and visualizations of the core signaling pathways.
Molecular Mechanisms of NRF2 Pathway Activation in Cancer
Canonical Regulation of NRF2
Under homeostatic conditions, NRF2 protein levels are kept low through its interaction with the KEAP1-CUL3 E3 ubiquitin ligase complex, which targets NRF2 for proteasomal degradation. This complex functions as a cellular sensor for oxidative and electrophilic stress. KEAP1, an obligate homodimer, contains reactive cysteine residues that are modified by ROS or other stressors. This modification suppresses the KEAP1-CUL3 complex's ability to degrade NRF2 [63]. Consequently, newly synthesized NRF2 accumulates, translocates to the nucleus, and heterodimerizes with small Maf (sMAF) proteins. This complex then binds to the Antioxidant Response Element (ARE), also known as the CNC-sMaf binding element (CsMBE), in the promoters of its target genes, initiating their transcription [63]. These genes govern four interconnected cellular processes: the antioxidant response, drug detoxification, cellular metabolism, and inflammation [63].
Mechanisms of Constitutive NRF2 Activation in Malignancy
In multiple cancer types, this carefully regulated system is subverted, leading to constitutive NRF2 activation and a malignant phenotype. The mechanisms underlying this hyperactivation are diverse, as summarized below and illustrated in Figure 1.
- Somatic Mutations: Gain-of-function mutations in
NFE2L2(the gene encoding NRF2) and loss-of-function mutations inKEAP1orCUL3are frequently observed in cancers associated with carcinogen exposure, such as non-small cell lung cancer (NSCLC) [63]. Mutations in theDLGexandETGEmotifs of NRF2 impair its binding to the KEAP1 homodimer, preventing its degradation [63] [64]. - Epigenetic and Post-transcriptional Regulation: Dysregulation of miRNAs that target both NRF2 and KEAP1 (redox miRs) can promote carcinogenesis and therapy resistance [63]. Furthermore, a novel lactylation-driven pathway has been identified in hepatocellular carcinoma (HCC), where ZNF207-driven lactylation of PRDX1 promotes its nuclear translocation and subsequent NRF2 activation, contributing to ferroptosis evasion and drug resistance [65].
- Oncogenic Signaling Pathways: Commonly dysregulated cancer pathways, including
BRAF,RAS-RAF-MAPK,Myc, andp53, have been associated with NRF2 activation, integrating antioxidant responses with pro-growth signals [63].
The following diagram illustrates the core regulatory circuit of NRF2 and its dysregulation in cancer.
Figure 1. NRF2 Regulatory Circuit and Dysregulation in Cancer. The core pathway shows KEAP1-CUL3-mediated degradation of NRF2 under normal conditions, inhibited by oxidative stress. Cancer cells hijack this through KEAP1/NRF2 mutations, oncogenic signaling, or lactylation, leading to constitutive NRF2 activation and target gene expression. Abbreviations: ARE, Antioxidant Response Element; CsMBE, CNC-sMaf Binding Element.
Metabolic Adaptation to Oxidative Stress
Metabolic Reprogramming Through NRF2
Constitutive NRF2 activation drives a comprehensive metabolic rewiring that enhances the antioxidant capacity and anabolic processes of cancer cells. A key redox proteomics study on 70 human NSCLC tissues and matched healthy counterparts revealed that tumors adapt to higher intracellular oxidative stress by increasing glutathione (GSH) biosynthesis [66]. This reinforces the primary intracellular antioxidative defense system. The study quantitatively identified differentially oxidized cysteine residues, with top hits being Cys156 of caveolin-1 (CAV1) and Cys240 of RACK1, both interactors with potent oncogenes [66].
A critical finding was the potentially redox-dependent hampering of the glyoxalase system, the main route for detoxifying methylglyoxal (MG), a reactive glycolytic byproduct and precursor of advanced glycation end-products (AGEs). Despite this compromised detoxification capacity, tumors do not accumulate AGEs. The study proposed a metabolic adaptation wherein tumors increase GAPDH activity to reduce MG production at its source, thereby preventing AGE formation despite reduced glyoxalase function [66]. This highlights a sophisticated re-routing of glucose metabolism to simultaneously manage oxidative and carbonyl stress.
Quantitative Redox Profiling in Human Lung Cancer
The table below summarizes key quantitative findings from the redox proteomics and biochemical analysis of human NSCLC tissues compared to healthy lung tissue [66].
Table 1: Redox and Metabolic Alterations in Human NSCLC Tissue
| Parameter | Finding in Tumor vs. Healthy Tissue | Implication |
|---|---|---|
| Global Redox State | 170 cysteine residues significantly differentially oxidized; median Cys~red~/Cys~ox~ ratio clustered around 1. | Redox ratios are tightly controlled; specific, significant changes occur against a stable background. |
| Top Oxidized Cysteine | Caveolin-1 (CAV1) Cys156: significantly more oxidized in tumor. | Displaces and activates proto-oncogene SRC, promoting oncogenic signaling. |
| Antioxidant Enzyme Abundance | SOD1/SOD2 (Cytosolic/Mitochondrial): Increased in tumor.SOD3 (Extracellular): Decreased in tumor. | Tumors reinforce intracellular over extracellular antioxidant defense. |
| Hemoglobin Subunits | Prominent reduction in abundance in tumor tissue. | Reflects poorer vascularization and oxygen availability in the tumor microenvironment (TME). |
| Glyoxalase System | Compromised by oxidation and downregulation. | Reduced capacity to detoxify methylglyoxal (MG). |
| Advanced Glycation End-products (AGEs) | Not accumulated despite impaired glyoxalase function. | Suggests metabolic adaptation (e.g., via GAPDH) to reduce MG production. |
NRF2-Mediated Remodeling of the Tumor Microenvironment and Immunosuppression
Suppression of Immune Cell Infiltration
A critical consequence of NRF2 activation in cancer cells is the profound suppression of the anti-tumor immune response. Clinical observations linking NRF2 hyperactivation to an immunosuppressive tumor microenvironment have been validated using a syngeneic mouse model with 3LL lung cancer-derived cells. In this model, KEAP1 gene deletion (leading to NRF2 hyperactivation) resulted in a marked decrease in overall immune cell infiltration, with CD45-positive leukocyte fractions dropping from approximately 30% in wild-type tumors to less than 10% in KEAP1-KO tumors [67]. This pan-immune suppression affected a broad range of cells, including NK cells, B cells, macrophages, neutrophils, and dendritic cells (DCs). Crucially, the concomitant deletion of NRF2 in the KEAP1-deleted background restored immune cell infiltration, providing direct genetic evidence that NRF2 activation is the causal factor in provoking this "cold" tumor phenotype [67].
Mechanisms of Immune Evasion
The mechanisms underlying NRF2-driven immunosuppression are multifaceted. By orchestrating a robust antioxidant and detoxification response, NRF2-active cancer cells can resist the cytotoxic ROS and reactive nitrogen species produced by innate immune effector cells like phagocytes and NK cells, which are vital for anti-tumor activity [63]. Furthermore, NRF2 activation in tumor-associated macrophages (TAMs) has been shown to drive metabolic reprogramming towards an immunosuppressive M2-like phenotype, which in turn can stabilize an epithelial-to-mesenchymal transition (EMT) in malignant cells and promote treatment resistance [63]. The overall effect is the generation of an immune-privileged niche where cancer cells are protected from elimination.
The following diagram synthesizes the interplay between NRF2 activation, metabolic adaptation, and the resulting tumor resistance and immune evasion.
Figure 2. Integrated View of NRF2-Driven Tumor Resistance. Constitutive NRF2 activation transcriptionally upregulates a network of genes involved in antioxidant defense, detoxification, metabolism, and cell survival. This network collectively confers resistance to therapy, protects against ferroptosis, and establishes an immunosuppressive tumor microenvironment, leading to a cold tumor phenotype. TAM: Tumor-Associated Macrophage.
Experimental Models and Methodologies for Investigating NRF2
A Syngeneic Mouse Model of NRF2-Activated Lung Cancer
To conclusively determine the impact of NRF2 activation on the tumor immune microenvironment, researchers established a syngeneic transplant model using the 3LL (Lewis lung carcinoma) cell line in immunocompetent C57BL/6 mice [67]. The detailed experimental workflow is outlined below.
Table 2: Key Experimental Protocol for Syngeneic Mouse Model [67]
| Step | Methodology Description | Key Outcome/Validation |
|---|---|---|
| 1. Cell Line Engineering | KEAP1-KO: CRISPR-Cas9-mediated deletion of Keap1 gene in 3LL cells.NRF2 Rescue: Concomitant Keap1 and Nrf2 gene deletion in 3LL cells. |
Sequencing confirmed homozygous frameshift mutations. Immunoblot confirmed KEAP1 loss and NRF2/NQO1 protein accumulation. qPCR confirmed upregulation of Nqo1 and Gsta4 mRNAs. |
| 2. Tumor Transplantation | Bilaterally transplant KEAP1-KO and WT 3LL cells into right and left flanks of albino C57BL/6 mice. | Allows comparison of tumor growth and immune infiltration in the same host systemic environment. KEAP1-KO tumors showed moderately accelerated growth. |
| 3. Tumor Processing & Analysis | Harvest tumors, dissociate into single-cell suspension, perform red blood cell lysis, and remove debris. | Prepares samples for downstream immune phenotyping. |
| 4. Immune Phenotyping (Flow Cytometry) | Stain cells with antibody panels for immune cell markers:- Pan-leukocyte: CD45- NK cells: NK1.1- B cells: B220- Macrophages: CD11b, F4/80- Neutrophils: CD11b, Ly6G- Dendritic Cells: CD11b, CD11c, MHCII | Revealed a significant decrease in CD45+ cells and all enumerated immune cell populations in KEAP1-KO tumors. Concomitant NRF2 deletion restored immune infiltration. |
The Scientist's Toolkit: Essential Research Reagents
The following table compiles key reagents and models used in the cited studies to investigate NRF2 biology and its role in therapy resistance.
Table 3: Research Reagent Solutions for NRF2 and Oxidative Stress Studies
| Reagent / Model | Function/Application | Key Findings Enabled |
|---|---|---|
| KEAP1-KO 3LL Cell Line (Murine) | Syngeneic model for studying NRF2 activation in an immunocompetent host. | Established causal link between NRF2 activation and suppressed immune cell infiltration [67]. |
| CRISPR/Cas9 Genome-Wide Screening | Identification of critical genes driving drug resistance. | Identified ZNF207 as a central driver of regorafenib resistance in hepatocellular carcinoma [65]. |
| Redox Proteomics with Instant Thiol Quenching | Unbiased analysis of cysteine oxidation in clinical tissue samples. | Mapped the protein thiol oxidation landscape in human NSCLC, revealing adaptation in glutathione and glucose metabolism [66]. |
| Antibodies for Immune Phenotyping (e.g., anti-CD45, anti-NK1.1, anti-F4/80) | Flow cytometric identification and quantification of tumor-infiltrating immune cells. | Quantified the reduction of myeloid, monocytic, NK, and dendritic cells in NRF2-activated tumors [67]. |
| ZNF207-Targeting Reagents (siRNA, CRISPR) | Functional validation of ZNF207's role in NRF2 activation and resistance. | Elucidated the ZNF207-PRDX1 lactylation-NRF2 axis in ferroptosis evasion [65]. |
Therapeutic Implications and Targeting Strategies
The NRF2 pathway presents both a challenge and an opportunity for cancer therapy. Its activation is a common mechanism of resistance to radio-, chemo-, and immunotherapy [63] [64]. Consequently, strategies to inhibit NRF2 or exploit the vulnerabilities of NRF2-addicted cancers are under active investigation.
One approach involves the direct inhibition of NRF2 using small molecules, which can sensitize KEAP1-mutant tumor cells to conventional therapies like cisplatin and gefitinib [64]. An alternative strategy is to target the downstream vulnerabilities created by NRF2 addiction. For instance, the reliance on increased glutathione synthesis creates a dependency on metabolic pathways like glutaminolysis, which can be therapeutically targeted [68] [64]. Furthermore, inducing alternative cell death pathways such as ferroptosis represents a promising strategy, as NRF2 directly upregulates key ferroptosis suppressors like SLC7A11 and GPX4 [63] [65]. Combining NRF2 inhibitors or ferroptosis inducers with standard therapies or immunotherapies holds significant potential to overcome treatment resistance and improve patient outcomes.
Reactive oxygen species (ROS) exhibit a profoundly dualistic role in cancer biology, functioning as both critical promoters of tumorigenesis and potent inducers of cancer cell death. This dichotomy is governed by precise spatiotemporal regulation, where concentration thresholds, subcellular localization, and exposure duration dictate functional outcomes. Moderate ROS levels activate pro-tumorigenic signaling cascades that drive proliferation, metastasis, and angiogenesis, while excessive ROS accumulation triggers oxidative damage, initiating apoptosis, necroptosis, and ferroptosis. This comprehensive review delineates the molecular mechanisms underlying context-dependent ROS effects, focusing on redox-sensitive pathways, metabolic adaptations, and therapeutic interventions. We provide detailed experimental methodologies, quantitative analyses, and visualization tools to guide research and drug development efforts aimed at harnessing ROS biology for cancer therapy.
The "oxygen paradox" describes the fundamental duality wherein oxygen is essential for aerobic life yet generates reactive oxygen species (ROS) that can damage cellular components [69]. In cancer biology, this paradox manifests as concentration-dependent ROS effects that both promote and suppress tumorigenesis. Cancer cells typically exhibit elevated ROS levels due to metabolic reprogramming, oncogenic signaling, and disrupted redox homeostasis [69] [70]. The intracellular ROS concentration creates a therapeutic window: low-to-moderate levels function as signaling messengers that activate oncogenic pathways, while excessive levels induce lethal oxidative damage [69] [71] [70]. This balance is maintained by sophisticated antioxidant systems that cancer cells upregulate to survive under persistent oxidative stress [72].
The spatial and temporal dynamics of ROS production further complicate their biological effects. Compartment-specific ROS generation (mitochondrial versus cytosolic) and exposure duration (acute versus chronic) activate distinct downstream pathways with different cellular outcomes [73]. Understanding these nuanced regulatory mechanisms provides critical insights for developing targeted therapies that either augment or inhibit ROS production based on cancer context and stage.
Molecular Mechanisms of ROS Signaling in Cancer
Concentration-Dependent Effects on Cellular Outcomes
The intracellular concentration of ROS serves as a primary determinant of their biological activity, creating a threshold-based regulatory system that governs cell fate decisions in cancer.
Table 1: Concentration-Dependent Effects of ROS in Cancer Biology
| ROS Level | Intracellular Concentration Range | Primary Cellular Outcomes | Key Activated Pathways |
|---|---|---|---|
| Low/Moderate | ~1.5×10ⵠoxidative hits/day [70] | Proliferation, Survival, Migration | PI3K/Akt, MAPK/ERK, NF-κB |
| High | Exceeds antioxidant capacity | Cell Death, Growth Inhibition | JNK/p38MAPK, Oxidative Damage Response |
| Chronic Elevation | Persistent 2-3 fold increase | Genomic Instability, Therapy Resistance | NRF2, HIF-1α, TGF-β |
At low-to-moderate concentrations, ROS function as secondary messengers in signaling pathways that drive tumor progression. Specifically, physiological Hâ‚‚Oâ‚‚ diffuses via aquaporins to oxidize redox-sensitive cysteine residues in phosphatases and kinases, thereby activating proliferative signaling cascades [74] [70]. The primary molecular targets include:
- Phosphatase inhibition: ROS oxidize catalytic cysteines in protein tyrosine phosphatases (PTPs) and PTEN, relieving constitutive inhibition of growth signaling [70].
- Kinase activation: Multiple receptor tyrosine kinases (RTKs) and downstream effectors including Src family kinases, Ras, and Akt are activated through oxidative modification [70] [73].
- Transcription factor modulation: NF-κB, HIF-1α, and NRF2 are redox-sensitive transcription factors that adjust gene expression profiles to favor survival under oxidative stress [75] [70].
When ROS levels exceed cellular antioxidant capacity, they induce irreversible damage to lipids, proteins, and DNA, triggering programmed cell death pathways. The mechanisms include:
- Lipid peroxidation: ROS attack polyunsaturated fatty acids in cellular membranes, particularly mitochondrial membranes, disrupting integrity and initiating ferroptosis [75] [70].
- Protein carbonylation: Irreversible oxidative modification of proteins alters structure and function, potentially inactivating critical enzymes and structural proteins [71].
- DNA damage: ROS generate 8-oxoguanine and other mutagenic lesions that activate DNA damage response pathways when excessive [71] [70].
Spatial Regulation: Subcellular Compartmentalization of ROS Effects
The biological impact of ROS is profoundly influenced by their subcellular origin and site of action, creating compartment-specific signaling microdomains.
Figure 1: Subcellular Compartmentalization of ROS Signaling. ROS generated from different cellular sources activate distinct downstream pathways with specific functional outcomes.
Mitochondrial ROS primarily originate from electron transport chain complexes I and III, where 1-2% of molecular oxygen undergoes incomplete reduction to superoxide [69] [70]. These ROS are particularly implicated in:
- Metabolic adaptation: Regulation of HIF-1α under hypoxia promotes glycolytic switching (Warburg effect) [69] [75].
- Apoptosis initiation: Excessive mROS induces mitochondrial permeability transition pore opening, cytochrome c release, and intrinsic apoptosis [69] [70].
- Genomic instability: mROS-induced mitochondrial DNA mutations contribute to tumorigenesis and therapy resistance [69].
NADPH oxidase (NOX) complexes at the plasma membrane generate ROS specifically for signaling purposes, creating precise spatial and temporal activation of:
- Proliferation pathways: Localized Hâ‚‚Oâ‚‚ production inactivates PTEN and activates growth factor receptors [76] [77].
- Migration and invasion: NOX4-derived ROS facilitate epithelial-mesenchymal transition (EMT) and matrix remodeling [71] [78].
- Differentiation programs: DUOX enzymes at the plasma membrane regulate differentiation signaling in epithelial tissues [76] [77].
Key ROS-Sensitive Signaling Pathways in Cancer
Multiple oncogenic and tumor suppressive pathways demonstrate redox sensitivity, with ROS serving as critical modulators of their activity states.
Figure 2: Key ROS-Sensitive Signaling Pathways in Cancer. ROS modulate multiple cancer-relevant pathways with predominantly pro-tumorigenic outcomes at moderate levels and anti-tumorigenic effects at high concentrations.
PI3K/Akt Pathway: This critical survival pathway is activated by ROS through multiple mechanisms. Hâ‚‚Oâ‚‚ oxidizes and inactivates PTEN phosphatase, relieving inhibition of PI3K signaling [70] [73]. Additionally, ROS activate Akt directly through oxidative modification, promoting glucose metabolism and suppressing apoptosis [75] [70]. In non-small cell lung cancer, NOX4-generated ROS maintain PI3K/Akt activation, supporting glycolytic metabolism and cell survival [75].
MAPK/ERK Pathway: ROS stimulate sequential activation of Ras, Raf, MEK, and ERK through inhibition of MAPK phosphatases [73]. This pathway drives proliferation and migration in response to growth factors and cellular stress. The duration and magnitude of ROS exposure determine functional outcomes, with transient activation promoting proliferation and sustained activation potentially inducing senescence [70].
NRF2 Antioxidant Response: Under basal conditions, NRF2 is sequestered in the cytoplasm by KEAP1 and targeted for degradation. ROS oxidize critical cysteine residues in KEAP1, disrupting this interaction and allowing NRF2 nuclear translocation [70]. NRF2 then activates transcription of antioxidant genes (SOD, catalase, glutathione peroxidase), enhancing cellular detoxification capacity [70] [72]. Cancer cells frequently exploit this pathway to maintain redox balance despite elevated ROS generation [70].
TGF-β/SMAD Pathway: TGF-β signaling induces NOX4 expression, generating ROS that enhance SMAD2/3 phosphorylation and nuclear translocation [71] [78]. This positive feedback loop promotes epithelial-mesenchymal transition (EMT), facilitating metastasis in breast, lung, and renal cancers [71] [78]. NOX4 knockdown experiments demonstrate significantly reduced metastatic potential in vivo [78].
Mitochondrial Electron Transport Chain
Mitochondria represent the primary source of intracellular ROS, generating approximately 90% of cellular superoxide through oxidative phosphorylation [69]. Key sites of production include:
- Complex I (NADH:ubiquinone oxidoreductase): Superoxide generation occurs primarily at the flavin mononucleotide site, directed toward the mitochondrial matrix [69].
- Complex III (ubiquinol:cytochrome c reductase): The Q cycle in complex III produces superoxide at both the Qo and Qi sites, releasing ROS into both matrix and intermembrane space [69].
Cancer cells exhibit mitochondrial DNA mutations and electron transport chain alterations that enhance ROS production while maintaining energy generation [69]. This adaptation creates a pro-tumorigenic environment while simultaneously increasing vulnerability to oxidative stress-induced cell death.
NADPH Oxidase (NOX) Family Enzymes
The NOX family comprises seven transmembrane enzymes (NOX1-5, DUOX1-2) dedicated to regulated ROS generation [76] [77]. These enzymes utilize NADPH to reduce molecular oxygen, producing superoxide or hydrogen peroxide in a tightly controlled manner.
Table 2: NOX Family Enzymes in Cancer Pathology
| Isoform | Primary ROS | Regulatory Partners | Cancer Associations | Therapeutic Implications |
|---|---|---|---|---|
| NOX1 | O₂•⻠| p22phox, NOXO1, NOXA1, Rac | Colon carcinoma, enhanced proliferation [77] | shRNA knockdown inhibits tumor growth in vivo [77] |
| NOX2 | O₂•⻠| p22phox, p47phox, p67phox, Rac | Breast, colorectal, gastric cancers [77] | siRNA silencing reduces cell viability [77] |
| NOX4 | Hâ‚‚Oâ‚‚ | p22phox, Poldip2 | NSCLC, RCC, pancreatic cancer [75] | EFHD2 inhibition blocks NOX4-mediated cisplatin resistance [75] |
| NOX5 | O₂•⻠| Ca²âº, Hsp90, c-Abl | Prostate cancer, melanoma, leukemia [77] | shRNA suppression inhibits proliferation [77] |
| DUOX1/2 | Hâ‚‚Oâ‚‚ | DUOXA1/2 | Lung, liver cancers (tumor suppressor) [77] | Epigenetic silencing in cancer [77] |
NOX4 demonstrates particularly significant involvement across multiple cancer types. It localizes to various subcellular compartments including plasma membrane, endoplasmic reticulum, mitochondria, and nucleus, allowing site-specific ROS signaling [76] [75]. In renal cell carcinoma, NOX4 regulates HIF-2α nuclear localization and supports glycolytic metabolism through PKM2 stabilization [75]. In NSCLC, NOX4 maintains NRF2-mediated antioxidant defense while simultaneously promoting pro-tumorigenic inflammatory signaling [75].
- Endoplasmic reticulum: Protein folding generates ROS through protein disulfide isomerase and Ero1 oxidase activities [74] [73].
- Peroxisomes: Fatty acid β-oxidation produces H₂O₂ as a byproduct [70].
- Xanthine oxidase: Purine metabolism generates superoxide and Hâ‚‚Oâ‚‚, particularly under hypoxic conditions [73].
- Cytochrome P450 enzymes: Xenobiotic metabolism produces ROS as side products [73].
Experimental Approaches for ROS Research
Methodologies for ROS Detection and Quantification
Accurate ROS measurement presents technical challenges due to their reactivity, short half-lives, and compartmentalized production. Advanced methodologies enable precise spatiotemporal analysis:
Fluorescent Probes and Biosensors
- Genetically encoded biosensors: Redox-sensitive fluorescent proteins (HyPer variants) enable real-time Hâ‚‚Oâ‚‚ monitoring in specific subcellular compartments [73]. Peroxiredoxin-FRET constructs report on localized oxidation states [73].
- Chemical probes: CM-Hâ‚‚DCFDA detects general cellular oxidation but requires careful interpretation due to potential artifacts. MitoSOX Red selectively measures mitochondrial superoxide with confirmation by HPLC [74].
Protocol: Mitochondrial Superoxide Measurement Using MitoSOX Red
- Culture cells in appropriate medium to 70-80% confluence
- Prepare 5µM MitoSOX Red working solution in pre-warmed buffer
- Incubate cells for 10-15 minutes at 37°C protected from light
- Wash gently three times with warm buffer to remove excess probe
- Analyze immediately by flow cytometry (excitation/emission: 510/580nm) or confocal microscopy
- Include controls with mitochondrial uncouplers (FCCP) and antioxidants (MitoTEMPO) to verify specificity
Electron Paramagnetic Resonance (EPR) Spectroscopy
- Employ spin traps such as DMPO (5,5-dimethyl-1-pyrroline N-oxide) to stabilize and detect short-lived radical species
- Provides quantitative data on specific ROS types with minimal perturbation to biological systems
- Requires specialized instrumentation but offers high specificity and sensitivity
Genetic Manipulation of ROS Pathways
Genetic approaches enable precise dissection of ROS-generating and scavenging systems:
NOX Isoform Knockdown Studies
- shRNA-mediated knockdown: Lentiviral transduction with NOX4-targeting shRNA (sequence: 5'-CCGGGCTCGAGTGGAATA...-3') in 4T1 breast cancer cells significantly reduced pulmonary metastasis in syngeneic mouse models [78].
- Validation requirements: Measure target protein reduction by Western blot, ROS production by specific assays, and functional outcomes (migration, invasion, proliferation).
Antioxidant Enzyme Modulation
- CRISPR/Cas9 knockout: SOD2 deletion enhances mitochondrial ROS sensitivity, while GPX4 knockout induces ferroptosis.
- Overexpression studies: NRF2 transfection increases antioxidant capacity and chemoresistance, mimicking adaptive responses in tumors.
Pharmacological Modulation of ROS Levels
Small molecule inhibitors and activators provide tools for acute ROS manipulation with therapeutic potential:
Table 3: Pharmacological Modulators of ROS Pathways
| Compound | Molecular Target | Mechanism of Action | Experimental Applications |
|---|---|---|---|
| Schisandrin B | NOX4 inhibitor | Direct enzyme inhibition (IC₅₀ = 9.3µM) [78] | Suppresses TGF-β-induced migration and metastasis in vivo |
| Apocynin | NOX1/2 inhibitor | Prevents p47phox translocation and complex assembly [77] | Reduces angiogenesis in xenograft models |
| DPI (Diphenyleneiodonium) | Flavoprotein inhibitor | Broad-spectrum inhibition of NOXs and other flavoenzymes [77] | Used for proof-of-concept studies of ROS involvement |
| Auranofin | Thioredoxin reductase inhibitor | Increases oxidized thioredoxin, enhancing oxidative stress [70] | Induces cancer cell death in combination with other agents |
| Elesclomol | Mitochondrial ROS inducer | Copper ionophore that increases electron transport chain leakage [70] | Phase II/III trials in melanoma, promotes oxidative stress-induced apoptosis |
Therapeutic Implications and Research Reagent Toolkit
Research Reagent Solutions for ROS Studies
Table 4: Essential Research Reagents for ROS Signaling Investigation
| Reagent Category | Specific Examples | Research Applications | Technical Considerations |
|---|---|---|---|
| ROS Detection | MitoSOX Red, CM-Hâ‚‚DCFDA, HyPer biosensors | Spatial and temporal ROS measurement | Validate with appropriate controls for specificity |
| NOX Inhibitors | Schisandrin B, GKT137831, Apocynin | Target validation studies | Assess isoform selectivity and off-target effects |
| Genetic Tools | NOX isoform shRNAs, CRISPR/Cas9 systems | Mechanistic studies of specific ROS sources | Confirm knockdown/knockout efficiency at protein level |
| Antioxidant Enzymes | PEG-SOD, PEG-catalase, MitoTEMPO | Scavenging specific ROS types | Consider membrane permeability and subcellular targeting |
| Oxidative Stress Inducers | Piperlongumine, Auranofin, Elesclomol | Testing ROS-mediated cytotoxicity | Titrate concentration to achieve desired effect level |
Therapeutic Strategies Targeting ROS Biology
ROS-Augmentation Approaches
- Pro-oxidant therapies: Compounds like piperlongumine and β-phenethyl isothiocyanate increase ROS beyond the toxicity threshold, selectively targeting cancer cells with already elevated basal ROS [70].
- Radiotherapy enhancement: Pharmacological ascorbate (high-dose vitamin C) generates Hâ‚‚Oâ‚‚ in tumor microenvironment, augmenting radiation-induced DNA damage [70].
- Metabolic vulnerability exploitation: Inhibition of NADPH-generating pathways (pentose phosphate pathway, folate metabolism) depletes antioxidant capacity, sensitizing to endogenous ROS [72].
ROS-Mitigation Approaches
- NOX isoform inhibition: Selective NOX1/4 inhibitors (GKT137831) block pro-tumorigenic signaling in pancreatic and renal cancers [77] [75].
- Inflammation-targeted antioxidants: Specific ROS scavengers in tumor microenvironment may suppress metastasis-initiating niches without protecting cancer cells.
- NRF2 pathway modulation: Brusatol inhibits NRF2 and sensitizes resistant tumors to conventional therapies [70].
Synthetic Lethality Strategies
- Glutathione depletion: Buthionine sulfoximine (BSO) inhibits γ-glutamylcysteine synthetase, creating vulnerability to ROS-inducing agents [72].
- Thioredoxin inhibition: Auranofin targets thioredoxin reductase, disrupting redox balance in combination with standard chemotherapy [70].
- Glucose transport inhibition: Blocking GLUT1 sensitizes cancer cells to oxidative stress by limiting NADPH production through pentose phosphate pathway [72].
The context-dependent effects of ROS in cancer represent both a challenge and opportunity for therapeutic development. The precise navigation of pro-tumorigenic versus anti-tumorigenic signaling requires sophisticated understanding of concentration thresholds, spatial organization, and temporal dynamics. Future research should focus on:
- Developing more precise tools for compartment-specific ROS modulation
- Identifying biomarkers that predict therapeutic response to ROS-targeting agents
- Optimizing combination strategies that exploit redox vulnerabilities while minimizing normal tissue toxicity
- Exploring immunomodulatory effects of ROS manipulation in tumor microenvironment
The dual nature of ROS in cancer biology continues to provide fascinating insights into cellular adaptation mechanisms while offering promising avenues for therapeutic intervention. As our tools for measuring and manipulating ROS become increasingly sophisticated, so too will our ability to harness this fundamental biological process for cancer treatment.
Reactive oxygen species (ROS) homeostasis represents a fundamental biological process wherein cells dynamically regulate intracellular ROS levels to ensure survival and execute physiological functions. ROS encompass a collection of highly reactive molecules, including both free radicals such as superoxide anion (•O2–) and hydroxyl radical (•OH), and non-radicals like hydrogen peroxide (H2O2) [1]. These molecules serve as critical signaling agents at physiological levels but transform into potential toxic agents when their concentrations exceed the cellular buffering capacity [1] [79]. This dual nature of ROS is dramatically exploited in the context of cancer therapy, where a state of "redox paradox" exists—heightened ROS levels act as pro-tumorigenic factors yet also present anti-tumorigenic opportunities when elevated beyond a toxic threshold [58].
The therapeutic challenge lies in precisely navigating this paradoxical landscape. While cancer cells exhibit elevated baseline ROS levels due to heightened metabolic activity and oncogenic signaling, they simultaneously develop reinforced antioxidant systems to maintain redox homeostasis [58] [80]. This adaptation creates a vulnerable dependency that can be therapeutically exploited. The conceptual foundation of optimizing therapeutic indices in strategies targeting ROS hinges on selectively pushing malignant cells beyond their redox tolerance threshold while preserving or even protecting normal tissue [79]. Achieving this balance requires deep understanding of ROS signaling mechanisms, sophisticated therapeutic approaches, and robust experimental methodologies to evaluate efficacy and safety.
ROS Biology and Signaling Mechanisms
ROS are generated through multiple interconnected cellular systems, each contributing differentially to the overall redox landscape. The major ROS species include superoxide anion (•O2–), the primary initial product of ROS typically produced from electron leakage in the mitochondrial respiratory chain; hydrogen peroxide (H2O2), a relatively stable molecule serving as an important signaling molecule; and hydroxyl radical (•OH), an extremely reactive radical generated through Fenton and Haber-Weiss reactions [1]. Additional ROS include hydroperoxyl radicals (HO₂•), peroxyl radicals (RO₂•), alkoxyl radicals (RO•), and carbonate radical anions (CO₃•−) [1].
The principal cellular sources of ROS include:
- Mitochondrial respiratory chain: Complexes I, II, and III of the electron transport chain are significant sources of •O2– during oxidative phosphorylation [58] [79].
- NADPH oxidase (NOX) family: Transmembrane enzymes dedicated to ROS generation that utilize NADPH to reduce O2, directly or indirectly producing H2O2 [1] [58].
- Endoplasmic reticulum: Contributes to ROS production during protein folding through oxidative protein folding reactions and ER-associated degradation pathways [58].
- Peroxisomes: Generate ROS during metabolic oxidation reactions [79].
In cancer cells, these sources are often hyperactive, creating an intrinsically pro-oxidant environment that, while supporting proliferation, also creates vulnerability to further oxidative insult [58] [80].
Antioxidant Defense Systems
To counteract persistent ROS generation, cells employ sophisticated, multi-layered antioxidant defense systems. The cornerstone is the NRF2-KEAP1 pathway, where under basal conditions, NRF2 is sequestered by KEAP1 and targeted for proteasomal degradation. Upon oxidative stress, KEAP1 cysteine residues undergo oxidation, releasing NRF2 to translocate to the nucleus and activate antioxidant response elements (AREs), driving expression of detoxifying and antioxidant enzymes [58] [80]. These enzymes include:
- Superoxide dismutase (SOD): Catalyzes the conversion of •O2– into oxygen and H2O2 [79].
- Catalase (CAT): Converts H2O2 into H2O and oxygen [79].
- Glutathione (GSH) system: Utilizes glutathione as a key non-enzymatic antioxidant and cofactor for GPX enzymes [58] [80].
- Thioredoxin (TXN) system: Comprising thioredoxin and thioredoxin reductase, maintains protein thiol homeostasis [58].
Cancer cells frequently exhibit constitutive activation of NRF2, either through mutation or epigenetic alteration, establishing a hyperactive antioxidant shield that represents a key mechanism of redox adaptation [58] [80]. Simultaneously, they may upregulate the BACH1 transcription factor, which competes with NRF2 for ARE binding sites and suppresses antioxidant gene expression under specific conditions, particularly facilitating metastasis when antioxidants are administered [81] [80].
Table 1: Major Reactive Oxygen Species and Their Characteristics
| ROS Species | Chemical Symbol | Reactivity | Primary Cellular Sources | Biological Roles |
|---|---|---|---|---|
| Superoxide anion | •O2– | Moderate | Mitochondrial ETC, NOX enzymes | Initial ROS product, signaling precursor |
| Hydrogen peroxide | H2O2 | Mild | NOX enzymes, peroxisomes | Key signaling molecule, substrate for •OH |
| Hydroxyl radical | •OH | Extreme | Fenton reaction, Haber-Weiss | Extreme damage to macromolecules |
| Hydroperoxyl radical | HO₂• | High | Protonation of •O2– | Lipid peroxidation initiation |
| Peroxyl radical | RO₂• | Moderate | Lipid peroxidation chain reactions | Membrane damage propagation |
| Alkoxyl radical | RO• | High | Decomposition of RO₂• | Protein and DNA oxidation |
Therapeutic Strategies Exploiting the Redox Paradox
Pro-Oxidant Therapies for Selective Cytotoxicity
Pro-oxidant therapies aim to overwhelm the adapted antioxidant defenses of cancer cells, pushing ROS levels beyond the toxic threshold to induce oxidative cell death. These approaches leverage the inherently elevated ROS state of malignant cells, exploiting their reduced buffer capacity compared to normal counterparts [58] [79]. Key pro-oxidant strategies include:
High-dose vitamin C (ascorbic acid): At pharmacological concentrations, vitamin C can generate H2O2 through auto-oxidation, exhibiting selective toxicity toward cancer cells [58]. The differential sensitivity arises from cancer cells' frequently diminished capacity to efficiently catabolize H2O2 due to altered metabolic and antioxidant enzyme profiles.
Arsenic trioxide (ATO): Demonstrated efficacy in promyelocytic leukemia by inducing severe oxidative stress and targeting specific oncoproteins for degradation [58]. ATO directly inhibits antioxidant enzymes and promotes mitochondrial ROS production.
Redox-active metal complexes: Manganese porphyrins and other metal-based compounds catalyze superoxide dismutation while simultaneously generating secondary ROS, creating a dual oxidative stress that can overwhelm adaptive responses [58]. These complexes leverage the differential redox state of normal versus cancer cells.
Ferroptosis inducers: Compounds like erastin and sulfasalazine inhibit system Xc– cysteine uptake, depleting glutathione and disabling GPX4 activity, leading to iron-dependent lipid peroxidation and cell death [58] [79]. This approach bypasses classical apoptosis resistance mechanisms.
Inhibiting Antioxidant Defense Systems
An alternative to directly increasing ROS production is disabling the antioxidant systems that cancer cells depend on for survival. This approach targets the "addiction" to rewired redox homeostasis [58]:
NRF2 inhibitors: Compounds such as Brusatol and ML385 disrupt the core antioxidant response by preventing NRF2-mediated transcription, sensitizing cancer cells to endogenous and therapy-induced oxidative stress [58].
Glutathione system disruption: Buthionine sulfoximine (BSO) inhibits γ-glutamylcysteine synthetase, the rate-limiting enzyme in glutathione synthesis, depleting this critical antioxidant and sensitizing tumors to oxidative challenges [80].
Thioredoxin system inhibition: Auranofin, a repurposed anti-rheumatic drug, irreversibly inhibits thioredoxin reductase (TrxR), disrupting redox balance and inducing apoptosis in cancer cells [58].
SOD targeting: Emerging approaches aim to inhibit SOD1, which is often overexpressed in tumors and drives oncogene-induced proliferation [79].
Normal Tissue Protection Strategies
While selectively increasing oxidative stress in malignancies, parallel strategies must protect normal tissues from collateral damage. Effective approaches include:
Selective delivery systems: Nanoparticle-based platforms enable tumor-specific delivery of pro-oxidant agents, minimizing exposure to healthy tissues [80] [82]. These systems leverage enhanced permeability and retention (EPR) effects or tumor-specific targeting ligands.
Temporal exploitation of differential repair capacity: Normal tissues often possess more robust DNA repair and protein quality control systems than malignant cells. Timing pro-oxidant therapies to exploit these differences can widen the therapeutic window [8].
NRF2 activation in normal tissues: Pharmacological activation of NRF2 using non-electrophilic activators in normal tissues can precondition these tissues against oxidative damage without similarly protecting tumors, particularly those with mutant KEAP1 or NRF2 [8] [82].
Mitochondria-targeted antioxidants: Compounds like MitoQ and MitoTEMPO accumulate specifically in mitochondria, protecting normal tissues from oxidative damage without interfering with pro-oxidant cytotoxicity in tumors [81] [82].
Table 2: Pro-Oxidant Agents and Their Mechanisms of Action
| Therapeutic Agent | Class | Primary Mechanism | Cancer Types with Demonstrated Efficacy | Clinical Status |
|---|---|---|---|---|
| High-dose vitamin C | Redox-active vitamin | Generates H2O2, depletes glutathione | Pancreatic, ovarian, glioblastoma | Phase I/II trials |
| Arsenic trioxide (ATO) | Metal compound | Inhibits antioxidant enzymes, induces mitochondrial ROS | Acute promyelocytic leukemia | FDA-approved |
| Erastin | Small molecule | Inhibits system Xc–, induces ferroptosis | Various solid tumors | Preclinical |
| Auranofin | Gold complex | Inhibits thioredoxin reductase | Chronic lymphocytic leukemia, ovarian | Repurposed in trials |
| Manganese porphyrins | Metal complex | SOD mimetic and pro-oxidant | Glioblastoma, pancreatic | Early clinical trials |
| Piperlongumine | Natural product | Increases ROS, depletes glutathione | Multiple solid tumors | Preclinical |
Experimental Models and Methodologies
In Vitro Assessment of ROS and Cytotoxicity
Robust evaluation of redox-targeting therapies requires multifaceted experimental approaches. Key methodologies for in vitro assessment include:
ROS Detection Protocols:
- DCFDA assay: Cells are loaded with 2',7'-dichlorofluorescin diacetate (10-20 μM) for 30-60 minutes at 37°C. After washing, the fluorescence intensity (excitation/emission: 485/535 nm) is measured over time following treatment. This assay primarily detects intracellular H2O2 and hydroxyl-like species [79].
- MitoSOX Red staining: Specifically detects mitochondrial superoxide. Cells are incubated with MitoSOX Red (5 μM) for 10-30 minutes at 37°C, washed, and fluorescence (excitation/emission: 510/580 nm) is measured. This is critical for evaluating mitochondrial-specific ROS production [79].
- CellROX assays: Cell-permeable dyes that exhibit fluorescence upon oxidation by ROS, available in different colors for multiplexing with other probes.
Cell Viability and Death Mechanism Assessment:
- Clonogenic survival assays: The gold standard for measuring long-term reproductive viability following treatment. Cells are seeded at low density, treated, and allowed to form colonies for 7-14 days before staining and counting [81].
- MTT/XTT assays: Measure metabolic activity as a surrogate for viability based on mitochondrial reductase activity.
- Annexin V/PI staining: Flow cytometry-based method to distinguish apoptosis (Annexin V+/PI– early; Annexin V+/PI+ late) from necrosis (Annexin V–/PI+).
- LDH release assays: Quantify plasma membrane integrity as an indicator of necrotic cell death.
Oxidative Lipid Damage Assessment:
- C11-BODIPY 581/591 assay: This fluorescent probe shifts from red to green upon oxidation by lipid peroxyl radicals, enabling quantification of lipid peroxidation, a key marker of ferroptosis, via flow cytometry or fluorescence microscopy [79].
- Malondialdehyde (MDA) measurement: Using thiobarbituric acid reactive substances (TBARS) assay to quantify end-products of lipid peroxidation.
Antioxidant Capacity Evaluation:
- GSH/GSSG ratio: Measured using commercial kits based on enzymatic recycling or liquid chromatography-mass spectrometry, providing insight into the cellular redox buffer capacity [58] [79].
- Antioxidant enzyme activity assays: Spectrophotometric measurements of SOD, catalase, GPX, and GR activities in cell lysates under optimized substrate conditions.
In Vivo Models and Therapeutic Efficacy Assessment
Translation of redox-modulating therapies requires appropriate in vivo models that recapitulate the tumor microenvironment and systemic responses:
Genetically Engineered Mouse Models (GEMMs):
- KRAS-driven lung cancer models: Enable evaluation of antioxidant and pro-oxidant therapies in autochthonous tumors with intact tumor microenvironments. These models have demonstrated that antioxidants can accelerate tumor progression in certain genetic contexts [81].
- MYC-driven lymphoma models: Have shown tumor-suppressive effects of antioxidants, highlighting the context-dependence of redox therapies [81].
- TRP53 knockout models: Used to evaluate how p53 status influences response to oxidative stress-inducing agents [81].
Human Tumor Xenografts:
- Subcutaneous or orthotopic implantation of human cancer cell lines or patient-derived xenografts (PDXs) in immunocompromised mice. PDXs better maintain the original tumor's characteristics and are valuable for assessing patient-specific responses.
Metastasis Models:
- Tail vein injection models for lung metastasis or spontaneous metastasis from orthotopic implants. These are particularly relevant given evidence that antioxidants can promote metastasis through BACH1 stabilization and metabolic reprogramming in some contexts [81] [80].
Therapeutic Efficacy Metrics:
- Tumor volume measurements: Regular caliper measurements for subcutaneous tumors or advanced imaging (MRI, ultrasound) for deep tumors.
- Biomarker analysis: Immunohistochemistry for oxidative damage markers (8-oxo-dG for DNA, 4-HNE for lipids), antioxidant enzyme expression, and cell death markers in tumor tissues.
- Survival studies: Overall survival or progression-free survival as ultimate efficacy endpoints.
Signaling Pathways in Redox Regulation and Therapeutic Targeting
The cellular response to oxidative stress is orchestrated through interconnected signaling networks that represent potential therapeutic targets. Key pathways include:
Figure 1: Key ROS Signaling Pathways and Their Crosstalk in Cancer. This diagram illustrates the major signaling pathways responsive to reactive oxygen species (ROS) and their functional outcomes in cancer cells. The KEAP1-NRF2 pathway activates antioxidant gene expression under oxidative stress. NF-κB promotes cell survival and proliferation, while BACH1 facilitates metastasis through glycolytic reprogramming. HIF-1α is stabilized by ROS and promotes angiogenic responses. Therapeutic pro-oxidant approaches aim to push ROS beyond the toxic threshold to induce cell death.
The NRF2-KEAP1-ARE Pathway
The NRF2-KEAP1 axis represents the master regulator of cellular antioxidant responses. Under basal conditions, KEAP1 functions as a substrate adaptor for a CUL3-based E3 ubiquitin ligase complex, constantly targeting NRF2 for proteasomal degradation [80]. KEAP1 contains multiple reactive cysteine sensors (Cys151, Cys273, Cys288) that undergo modification upon oxidative stress, leading to conformational changes that impair NRF2 ubiquitination [80]. Stabilized NRF2 translocates to the nucleus, heterodimerizes with small MAF proteins, and binds to antioxidant response elements (AREs) in the promoter regions of target genes [8]. These genes encode numerous cytoprotective proteins, including glutathione biosynthesis enzymes (GCLC, GCLM), glutathione S-transferases, NAD(P)H quinone dehydrogenase 1 (NQO1), and heme oxygenase-1 (HO-1) [8] [80].
Therapeutic targeting of this pathway presents a double-edged sword: NRF2 activation in normal tissues can confer protection against therapy-induced damage, while NRF2 inhibition in tumors can sensitize them to oxidative stress. This dichotomy necessitates tissue-specific targeting approaches [8] [80].
NF-κB and Inflammatory Signaling
ROS directly activate the NF-κB pathway, a critical regulator of inflammation and cell survival. ROS stimulate IκB kinase (IKK), leading to phosphorylation and degradation of IκB, the inhibitory subunit that sequesters NF-κB in the cytoplasm [82]. Released NF-κB dimers (primarily p65/p50) translocate to the nucleus and induce expression of pro-inflammatory cytokines (TNF-α, IL-6, IL-1β), chemokines, and anti-apoptotic factors [82]. This creates a feed-forward loop wherein inflammation generates more ROS, and ROS sustain inflammatory signaling. In the context of cancer therapy, NF-κB activation can promote tumor cell survival and resistance to pro-oxidant therapies, making its inhibition an attractive combination strategy [82].
BACH1-Mediated Metabolic Reprogramming
BACH1 represents a redox-sensitive transcription factor that competes with NRF2 for ARE binding. Under mild oxidative stress, BACH1 is stabilized and suppresses antioxidant gene expression [80]. Importantly, BACH1 has emerged as a key mediator of antioxidant-induced metastasis. Antioxidants stabilize BACH1 by reducing free heme levels (heme promotes BACH1 degradation), leading to BACH1-dependent activation of glycolytic genes (HK2, GAPDH) and enhanced glucose uptake and lactate production [81] [80]. This metabolic reprogramming drives glycolysis-dependent metastasis in lung cancer and other malignancies. Consequently, BACH1 inhibition represents a promising approach to block the metastasis-promoting effects of antioxidants while maintaining their potential protective benefits [80].
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 3: Essential Research Reagents for Redox Biology Studies
| Reagent/Category | Specific Examples | Primary Research Application | Key Considerations |
|---|---|---|---|
| ROS detection probes | DCFDA, MitoSOX Red, CellROX, H2DCFDA | Quantifying intracellular and compartment-specific ROS levels | Selectivity for specific ROS species, potential auto-oxidation, photostability |
| Antioxidant enzyme inhibitors | BSO (GCL inhibitor), Auranofin (TrxR inhibitor), Brusatol (NRF2 inhibitor) | Disabling specific antioxidant pathways | Specificity, off-target effects, cytotoxicity in normal cells |
| Pro-oxidant compounds | Erastin, RSL3, Arsenic trioxide, High-dose vitamin C | Inducing oxidative stress and cell death | Selectivity for cancer cells, therapeutic window, combination potential |
| Genetic manipulation tools | NRF2 siRNA/shRNA, BACH1 overexpression plasmids, CRISPR/Cas9 systems | Modulating expression of redox regulators | Efficiency of delivery, complete knockdown/overexpression, compensatory mechanisms |
| Cell death inhibitors | Ferrostatin-1 (ferroptosis), Z-VAD-FMK (apoptosis), Necrostatin-1 (necroptosis) | Determining mechanism of cell death | Specificity at working concentration, effect on baseline viability |
| Animal models | GEMMs (KRAS, MYC), PDX models, Metastasis models | In vivo validation of therapeutic efficacy | Tumor microenvironment representation, metastatic potential, immunocompetence |
| Biomarker detection antibodies | Anti-8-oxo-dG, Anti-4-HNE, Anti-phospho-H2AX, Anti-HO-1 | Assessing oxidative damage and stress responses in tissues | Antibody specificity, appropriate controls, quantification method |
The strategic manipulation of redox balance represents a promising approach for cancer therapy, but its successful implementation requires navigating complex biological paradoxes. The divergent responses of different cancer types—and even different cellular compartments within tumors—to both pro-oxidant and antioxidant interventions highlight the critical importance of context [81]. Future advances in this field will likely emerge from several key areas:
First, personalized redox profiling of tumors will enable matching specific therapeutic approaches to individual tumor characteristics. This includes comprehensive assessment of antioxidant enzyme expression, NRF2/BACH1 status, metabolic dependencies, and ROS buffering capacity [80]. Such profiling could predict which tumors are vulnerable to pro-oxidant therapies versus those that might respond to antioxidant disruption.
Second, advanced delivery systems including nanoparticle platforms and tumor-targeting modalities will enhance the therapeutic index by maximizing drug delivery to malignant tissues while minimizing exposure to normal organs [80] [82]. These systems could be further refined to respond to tumor-specific microenvironments such as low pH or specific enzyme activities.
Third, rational combination therapies that pair pro-oxidant agents with complementary mechanisms—such as inhibitors of specific antioxidant pathways or drugs that disrupt redox adaptation mechanisms—will likely yield synergistic effects [58] [79]. The growing understanding of ferroptosis and other oxidative cell death pathways provides additional combinatorial opportunities.
Finally, temporal control of therapy through chronotherapeutic approaches or triggered release systems may exploit fluctuations in redox homeostasis that occur through circadian rhythms or in response to specific stimuli [8]. As our understanding of redox biology deepens, so too will our ability to precisely manipulate this fundamental biological process for therapeutic benefit while minimizing collateral damage to normal tissues.
Delivery and Pharmacokinetic Challenges for Redox-Directed Therapeutics
Reactive oxygen species (ROS) are a collection of oxygen-containing, highly reactive molecules that serve as critical signaling entities in normal cellular physiology but also contribute to disease pathogenesis when dysregulated [1]. Redox-directed therapeutics represent a novel class of pharmacological agents designed to modulate cellular redox homeostasis through direct or indirect alteration of ROS generation, signaling, and turnover [83]. The therapeutic strategy is twofold: either to suppress pathologically elevated ROS using antioxidant approaches or to increase ROS beyond the oxidative stress threshold of cancer cells to induce cytotoxic effects [84]. This field has transitioned from bench to bedside, with several agents now in advanced clinical development [83] [85].
The intricate interplay between redox signaling and inflammation lies at the core of numerous pathologies, ranging from chronic inflammatory disorders to cancer [86]. Redox dysregulation originating from metabolic alterations and dependence on mitogenic and survival signaling through ROS represents a specific vulnerability of malignant cells that can be selectively targeted by redox chemotherapeutics [83]. However, the development of these agents faces unique pharmacological challenges, particularly in delivery and pharmacokinetic optimization, which must be addressed to realize their full clinical potential.
ROS Biology and Signaling Mechanisms
Categories of Reactive Oxygen Species
ROS encompass both free radicals and non-radical molecules with varying reactivity, half-lives, and biological functions [1]:
- Superoxide anion (•Oâ‚‚â»): The main initial ROS product, primarily generated through electron leakage in the mitochondrial respiratory chain and stored in mitochondria during cellular diffusion [1]. It possesses strong oxidative properties and serves as a precursor to other ROS.
- Hydrogen peroxide (Hâ‚‚Oâ‚‚): A relatively stable non-radical ROS molecule primarily produced intracellularly through enzymatic reactions, notably by NADPH oxidase (NOX) family enzymes [1]. It serves as an important signaling molecule at physiological concentrations.
- Hydroxyl radical (•OH): An extremely reactive radical primarily generated through Fenton and Haber-Weiss reactions, especially in iron-rich areas such as mitochondria and lysosomes [1]. Its high reactivity limits diffusion but enables significant damage to macromolecules.
- Other significant ROS: Include hydroperoxyl radicals (HO₂•), peroxyl radicals (RO₂•), alkoxyl radicals (RO•), carbonate radical anion (CO₃•â»), and singlet oxygen (¹Oâ‚‚) [1].
ROS Homeostasis and Signaling
ROS homeostasis relies on the dynamic equilibrium of intracellular redox reactions, enabling cells to adapt to changing conditions such as hypoxia, hyperoxia, and oxidative stress [1]. This balance is maintained through sophisticated regulatory mechanisms:
- ROS production systems: Mitochondrial electron transport chain, NADPH oxidases (NOX), xanthine oxidoreductase, and enzymes involved in arachidonic acid metabolism [87].
- Antioxidant defense systems: Include enzymatic components such as superoxide dismutase (SOD), catalase (CAT), glutathione peroxidase (GPX), and glutathione reductase (GR), as well as non-enzymatic small molecule scavengers such as vitamins C and E [87].
At physiological levels, ROS function as signaling molecules through oxidative post-translational modifications (Oxi-PTMs) of proteins, particularly targeting cysteine and methionine residues [7]. These modifications act as molecular switches that precisely regulate protein function by adjusting structure, charge distribution, stability, and interaction capabilities [7]. The thiol group of cysteine residues serves as one of the most sensitive targets for ROS signaling-induced PTMs, with modifications including S-sulfenylation, S-glutathionylation, and disulfide bond formation [7].
ROS Signaling Pathways in Disease
Redox signaling plays a pathogenic role in various diseases, particularly cancer. ROS contribute to carcinogenesis by modulating multiple signaling pathways including NF-κB, MAPK, PI3K/AKT, and p53, thereby promoting inflammation, increasing genomic instability, and shaping a tumor-promoting microenvironment [84]. In breast cancer, ROS metabolic imbalance plays a key role in occurrence, development, and treatment resistance [87]. NOX4 serves as the predominant NADPH oxidase enzyme in breast cancer, facilitating oxidative stress regulation and promoting metastasis through lymphangiogenesis [87].
Table 1: Major Reactive Oxygen Species and Their Characteristics
| ROS Species | Chemical Nature | Reactivity | Primary Sources | Biological Roles |
|---|---|---|---|---|
| Superoxide anion (•Oâ‚‚â») | Free radical | High | Mitochondrial ETC, NOX | Signaling, precursor to other ROS |
| Hydrogen peroxide (Hâ‚‚Oâ‚‚) | Non-radical | Moderate | NOX, peroxisomes | Redox signaling, immune response |
| Hydroxyl radical (•OH) | Free radical | Very high | Fenton reaction | Macromolecular damage |
| Singlet oxygen (¹O₂) | Excited state | High | Photosensitization | Cell signaling, damage |
| Peroxyl radicals (RO₂•) | Free radical | Moderate | Lipid peroxidation | Membrane damage |
Pharmacodynamic Aspects of Redox Therapeutics
Therapeutic Strategies Targeting ROS
Redox-directed therapeutics can be categorized into four primary mechanistic classes [85]:
- Activators of endogenous antioxidant defense systems: These include NRF2 activators such as dimethyl fumarate (DMF), bardoxolone methyl, and sulforaphane, which enhance the expression of antioxidant response element (ARE)-regulated genes [85].
- Inhibitors of ROS formation: Target enzymatic sources of disease-relevant ROS, including NOX inhibitors, xanthine oxidase inhibitors, and monoamine oxidase inhibitors [85].
- Inhibitors of ROS toxification: Includes compounds that inhibit peroxidases such as myeloperoxidase [85].
- Compounds that allow functional repair of ROS-induced damage: Such as the functional repair of oxidatively damaged soluble guanylate cyclase (sGC) [85].
Redox Programmed Cell Death Induction
A significant therapeutic strategy involves increasing ROS beyond cellular tolerance thresholds to trigger various forms of programmed cell death. In breast cancer, ROS are critical inducers of multiple cell death pathways [87]:
- Apoptosis: The classic programmed cell death pathway
- Pyroptosis: Inflammatory programmed cell death
- Ferroptosis: Iron-dependent cell death driven by lipid peroxidation
- Cuproptosis: Copper-dependent cell death
- Disulfidptosis: Disulfide stress-induced death
- PANoptosis: An integrated form of cell death encompassing apoptosis, pyroptosis, and necroptosis [87]
The pleiotropic action of many redox chemotherapeutics that involves simultaneous modulation of multiple redox-sensitive targets can overcome cancer cell drug resistance originating from redundancy of oncogenic signaling and rapid mutation [83].
Pharmacokinetic Challenges in Redox Therapeutics
Absorption and Bioavailability Hurdles
The development of anticancer redox chemotherapeutics faces significant pharmacokinetic challenges [83]. Unfavorable pharmacokinetics, unexpected off-target activity, and systemic toxicity not predicted from simple cell culture and short-term murine xenograft models pose serious obstacles during later stages of development [83]. Many redox-active compounds contain chemically reactive pharmacophores that display potential for uncontrolled reactivity and untargeted cytotoxicity, complicating their administration and distribution [83].
Distribution and Targeting Limitations
Achieving selective distribution to disease sites remains a fundamental challenge. Traditional small molecule redox modulators often lack tissue specificity, leading to off-target effects on physiological ROS signaling. This is particularly problematic as ROS serve essential functions in normal cellular processes, including regulation of extracellular matrix, control of vasomotor activity, involvement in innate immune response, and promotion of cell differentiation, proliferation, and migration [85].
Metabolism and Elimination Issues
Redox-active compounds often undergo complex metabolic transformations that can alter their therapeutic activity or generate reactive metabolites contributing to toxicity. The electrophilic nature of many redox modulators leads to rapid conjugation with glutathione and subsequent elimination, reducing their therapeutic half-life and efficacy [85].
Table 2: Major Pharmacokinetic Challenges and Potential Solutions
| PK Challenge | Impact on Therapy | Potential Solutions |
|---|---|---|
| Poor bioavailability | Limited systemic exposure | Nanoformulations, prodrug approaches |
| Lack of targeting | Off-target effects, toxicity | Active targeting ligands, stimuli-responsive release |
| Rapid clearance | Short half-life, reduced efficacy | PEGylation, sustained release systems |
| Metabolic instability | Generation of inactive/toxic metabolites | Structural optimization, delivery systems |
| Tissue penetration barriers | Limited access to target sites | Permeation enhancers, nanocarriers |
Advanced Delivery Systems for Redox Therapeutics
Redox-Responsive Nanoassemblies
Carrier-free nanoassemblies composed of small-molecule drugs or prodrugs have emerged as a promising platform for cancer therapy [88]. These systems retain the advantages of traditional nanomedicines while offering distinct benefits, including simple fabrication, high drug loading (>50%), and the elimination of carrier-related toxicity [88]. In particular, prodrug-based nanoassemblies integrate the precision of prodrug design with the efficiency of nanoscale delivery, representing a paradigm shift in drug development [88].
Recent advances have demonstrated that strategic incorporation of redox-sensitive disulfide bonds with different π-π stacking interactions in the prodrug structure effectively optimizes the delivery-release balance in vivo, ensuring both potent antitumor efficacy and reduced systemic toxicity [88]. For example, position-specific disulfide-bridged doxorubicin prodrugs (FAD, FBD, FGD) spontaneously self-assembled into stable carrier-free nanoassemblies that demonstrated improved tumor accumulation and redox-responsive drug release [88].
Targeted Delivery Approaches
Active targeting strategies enhance the specificity of redox therapeutic delivery. Mannose-functionalized nanoparticles (MnCNPs) can specifically target mannose receptors (CD206) predominantly found on tumor-associated macrophages (TAMs) and certain cancer cells [89]. This approach offers a means to reprogram TAMs toward an anti-tumor phenotype or selectively deliver anticancer agents to the tumor site [89].
The development of MnCNPs represents a convergence of multiple disciplines, including biochemistry, materials science, and oncology. The synthesis and functionalization of these nanoparticles require precise control to achieve optimal performance, with various techniques such as emulsion-based methods, self-assembly, and layer-by-layer deposition employed to fabricate MnCNPs with desirable characteristics [89].
Stimuli-Responsive Release Systems
Smart delivery systems that respond to tumor-specific microenvironmental cues enable controlled drug release at disease sites. Tumor-specific activation is enabled by the abnormal chemical milieu of tumors, such as elevated levels of ROS and glutathione (GSH) [88]. Researchers have engineered cleavable linkers—such as disulfide bonds—that respond to these cues and trigger drug release within tumors [88].
Beyond accelerating drug release, certain linkers also enhance the self-assembly of prodrugs by strengthening intermolecular interactions [88]. These insights have broadened the functional scope of chemical linkers in prodrug-based delivery and sparked growing interest in the design of novel linker chemistries.
Figure 1: Redox-Responsive Prodrug Nanoassembly Delivery Pathway
Experimental Models and Methodologies
Synthesis of Redox-Responsive Prodrugs
The development of position-specific disulfide-bridged DOX prodrugs follows a standardized three-step protocol [88]:
- Activation of dithiodiacids: Dithiodiacids (2 mmol) are reacted with acetic anhydride (5 mL) at 25°C for 2 h under N₂, followed by toluene-assisted drying.
- Fmoc conjugation: The intermediates are coupled with Fmoc (2 mmol) and DMAP (0.2 mmol) in dichloromethane (10 mL) at 25°C for 12 h, purified by silica column chromatography (CH₂Cl₂:MeOH, 500:1).
- DOX conjugation: The Fmoc intermediates (0.5 mmol) are conjugated with DOX·HCl (0.5 mmol) using HBTU/DIPEA in DMF (10 mL) at 30°C for 48 h.
- Purification: All products are purified by preparative high-performance liquid chromatography (HPLC, acetonitrile:water, 70:30) with yields >50% and characterized by mass spectrometry (MS) and NMR [88].
Preparation and Characterization of Nanoassemblies
Prodrug-based nanoassemblies are synthesized using a standardized nanoprecipitation protocol [88]:
- Preparation: Individual prodrugs (1 mg) are initially dissolved in a 1:1 (v/v) THF/ethanol cosolvent system (200 μL total volume). This organic solution is then rapidly injected into deionized water (1 mL) under continuous magnetic stirring.
- Characterization: Comprehensive characterization includes self-assembly kinetics, redox-responsive drug release profiles, physicochemical stability, cellular uptake efficiency, in vivo pharmacokinetics, and antitumor efficacy in tumor-bearing mouse models [88].
Analytical Methods for Redox Biology
Advanced analytical techniques are essential for evaluating redox biology and therapeutic effects:
- Mass spectrometry: HR-ESI-MS in positive ion mode with scanning range m/z 100-1500, drying temperature 300°C, capillary voltage 3.5 kV, and collision energy 20-40 eV [88].
- NMR characterization: ¹H NMR (400/600 MHz, DMSO-d₆ with 0.03% TMS) at 25°C, analyzing chemical shifts, peak patterns, and integration ratios with acquisition parameters of 32-64 scans, 12 ppm spectral width, and 2 s relaxation delay [88].
- Biological evaluation: Cellular uptake efficiency, in vivo pharmacokinetics, and antitumor efficacy in tumor-bearing mouse models [88].
Table 3: Key Research Reagent Solutions for Redox Therapeutics Development
| Reagent/Category | Function/Application | Specific Examples |
|---|---|---|
| Disulfide linkers | Redox-responsive cleavage | α, β, γ-positioned disulfide linkages |
| Fmoc moieties | Enhance π-π stacking for self-assembly | Fluorenylmethoxycarbonyl |
| Coupling reagents | Prodrug synthesis | HBTU, DIPEA, DMAP |
| Characterization tools | Structural confirmation | HR-ESI-MS, NMR |
| Cell culture models | In vitro efficacy testing | MCF-7, 4T1 breast cancer cells |
| Animal models | In vivo pharmacokinetics/efficacy | Tumor-bearing mouse models |
Quantitative Assessment of Delivery Systems
Pharmacokinetic Performance Metrics
Comprehensive pharmacokinetic evaluation is essential for assessing the performance of redox-directed delivery systems. Studies on disulfide-bridged doxorubicin prodrug nanoassemblies demonstrated remarkable improvements in key pharmacokinetic parameters [88]:
- Tumor accumulation: FBD NAs achieved 101.7-fold greater tumor accumulation (AUC) than DiR Sol controls [88].
- Antitumor efficacy: In 4T1 tumor-bearing models, FBD NAs displayed potent antitumor efficacy, yielding a final mean tumor volume of 518.06 ± 54.76 mm³ that was statistically significantly smaller than all comparator groups (p < 0.001 by ANOVA at a 99% confidence interval) [88].
- Systemic toxicity: Optimal redox-responsive release kinetics maintained minimal systemic toxicity while ensuring therapeutic efficacy [88].
Structure-Activity Relationships
Strategic molecular design significantly impacts delivery system performance. Systematic characterization revealed that π-conjugated disulfide bond positioning dictates prodrug self-assembly and inversely regulates reductive drug release relative to carbon spacer length [88]. The FBD NAs with specific disulfide bond positioning demonstrated optimal redox-responsive release kinetics, highlighting the importance of molecular engineering in balancing delivery and release properties.
Figure 2: Structure-Function Relationship in Redox Prodrug Design
The field of redox-directed therapeutics continues to evolve with several promising directions emerging. Future advancements will likely focus on personalized redox medicine that depends on careful patient selection based on genotypic and phenotypic profiling that matches the individual patient with a specific redox intervention [83]. The complexity and variability of redox dysregulation in tumors depends on tumor type and progressional stage, localization, and prior chemotherapeutic exposure, necessitating tailored therapeutic approaches [83].
Combination therapies represent another promising direction. Many developmental redox therapeutics have shown a potentiating effect on pharmacodynamic activity of other anticancer agents and radiation [83]. The integration of redox therapeutics with immunotherapy, conventional chemotherapy, and targeted agents may yield synergistic benefits while mitigating resistance mechanisms.
From a technological perspective, the convergence of redox biology with advanced delivery platforms such as multifunctional nanoparticles, stimuli-responsive systems, and carrier-free nanoassemblies will address current pharmacokinetic limitations [88] [89]. Further optimization of linker chemistries, self-assembly mechanisms, and targeting strategies will enhance the therapeutic index of redox-directed therapeutics.
As the field advances, the translation of redox-directed therapeutics will require coordinated efforts from academia and industry scientists to achieve unambiguous validation through proof-of-principle studies, potentially leading toward a new era of redox medicine [85]. With the availability of optimized compounds and validated biomarkers, redox-directed therapeutics are poised to make significant contributions to cancer treatment and other oxidative stress-related pathologies.
Evaluating ROS-Targeting Therapies: Preclinical Models to Clinical Trial Insights
Reactive oxygen species (ROS) are oxygen-derived, chemically reactive molecules that function as central regulators of cellular physiology and pathology. The current paradigm in redox biology recognizes their fundamental duality: at low or physiological concentrations, ROS act as crucial signaling molecules governing processes from cell proliferation to differentiation, while at high concentrations, they induce oxidative stress, leading to damage of cellular macromolecules and pathology [4] [90] [91]. This delicate balance places ROS-modulating agents—both pro-oxidants and antioxidants—at the forefront of therapeutic development for conditions ranging from cancer to neurodegenerative diseases.
The signaling function of ROS is primarily mediated through precise, reversible modifications of specific protein targets. Key among these are the oxidation of cysteine thiolate anions (Cys-S-) within catalytic sites of phosphatases like PTP1B and PTEN, which leads to their transient inactivation and sustained activation of growth factor signaling pathways [4]. Hydrogen peroxide (Hâ‚‚Oâ‚‚), a relatively stable ROS, serves as the primary secondary messenger in these processes due to its ability to selectively oxidize target proteins and its diffusibility across membranes [4]. This redox signaling occurs within specific cellular compartments, with production sources including NADPH oxidases (NOX) at the plasma membrane and electron leakage from mitochondrial complexes I and III [4] [90].
When ROS production overwhelms cellular antioxidant defenses, oxidative stress ensues. This state is characterized by irreversible oxidative modifications to lipids, proteins, and DNA, leading to loss of function, membrane disruption, and genomic instability [91] [41]. The hydroxyl radical (•OH), generated via Fenton reactions involving transition metals like iron and copper, is particularly damaging due to its extreme reactivity and non-selective attack on biomolecules [17] [91]. This oxidative damage establishes a vicious cycle of cellular dysfunction that underpins numerous pathological states, creating therapeutic opportunities for both pro-oxidant and antioxidant approaches depending on the disease context.
Molecular Mechanisms of ROS Activity and Cellular Sensing
Table 1: Primary Reactive Oxygen Species: Sources, Reactivity, and Biological Impact
| ROS Species | Primary Production Sources | Reactivity & Selectivity | Primary Biological Consequences |
|---|---|---|---|
| Superoxide (O₂•â») | Mitochondrial ETC (Complex I & III), NADPH oxidases (NOX), xanthine oxidase [17] [90] | Moderate reactivity; targets iron-sulfur cluster proteins [4] | Signaling initiation; precursor for other ROS; oxidative damage to Fe-S proteins |
| Hydrogen Peroxide (Hâ‚‚Oâ‚‚) | SOD-catalyzed dismutation of O₂•â», peroxisomal oxidases, NOX [17] [4] | Selective, diffusible; oxidizes cysteine thiolates in specific proteins [4] | Primary redox signaling molecule; reversible phosphatase inactivation; cellular proliferation |
| Hydroxyl Radical (•OH) | Fenton reaction (Hâ‚‚Oâ‚‚ + Fe²âº/Cuâº), Haber-Weiss reaction [17] [91] | Extreme reactivity; non-selective; attacks all biomolecules [91] | Lipid peroxidation; DNA strand breaks; protein carbonylation; irreversible oxidative damage |
| Peroxynitrite (ONOOâ») | Reaction between O₂•⻠and NO• [17] [91] | Potent oxidant/nitrating agent; moderate selectivity [17] | Protein tyrosine nitration; lipid peroxidation; contributes to inflammatory tissue damage |
Cellular Sensing and Signaling Pathways
ROS modulate cellular function through several evolutionarily conserved signaling pathways. The transcription factor Nuclear factor erythroid 2-related factor 2 (Nrf2) serves as the master regulator of the antioxidant response. Under basal conditions, Nrf2 is sequestered in the cytoplasm by its inhibitor Keap1 and targeted for proteasomal degradation. During oxidative stress, specific cysteine residues in Keap1 are oxidized, causing conformational changes that release Nrf2, allowing its translocation to the nucleus where it activates the Antioxidant Response Element (ARE)-mediated transcription of numerous antioxidant and cytoprotective genes [17] [41].
Simultaneously, ROS activate pro-inflammatory signaling through the Nuclear Factor-kappa B (NF-κB) pathway. Multiple mechanisms underlie ROS-induced NF-κB activation, including IκB kinase (IKK) activation through oxidation and inhibition of its regulatory phosphatases [4]. NF-κB translocation to the nucleus initiates transcription of inflammatory cytokines, adhesion molecules, and enzymes that further amplify the oxidative and inflammatory response—a key connection in chronic inflammatory diseases [17].
Mitogen-activated protein kinase (MAPK) pathways, including JNK, p38, and ERK, represent another major signaling cascade regulated by ROS. These pathways are activated through oxidative inhibition of their respective phosphatases and direct oxidation of pathway components, influencing cell fate decisions including proliferation, differentiation, and apoptosis [41]. The specific cellular outcome of MAPK activation depends on the intensity and duration of the oxidative stimulus, as well as the cellular context.
Figure 1: Core ROS Signaling Pathways. ROS, particularly Hâ‚‚Oâ‚‚, activate adaptive and inflammatory responses through oxidation of specific sensor proteins including Keap1 and protein tyrosine phosphatases (PTPs).
Pro-Oxidant Agents: Mechanisms and Research Applications
Direct Oxidizing Agents and Experimental Induction
Pro-oxidant agents increase intracellular ROS levels either through direct generation of reactive species or by interfering with cellular antioxidant systems. A primary method for experimental ROS induction involves inhibition of the electron transport chain (ETC). Compounds such as rotenone (Complex I inhibitor) and antimycin A (Complex III inhibitor) induce significant superoxide production by increasing electron leakage at these sites [90]. Similarly, pharmacological agents like menadione undergo redox cycling, generating O₂•⻠while depleting cellular reducing equivalents like NADPH.
Transition metal complexes, particularly those containing copper and iron, represent another important class of pro-oxidant agents. These metals catalyze Fenton and Haber-Weiss reactions that convert less reactive H₂O₂ into highly damaging •OH radicals [91]. Recent research has identified a novel copper-dependent cell death pathway termed cuproptosis, wherein copper directly binds to lipoylated enzymes in the tricarboxylic acid (TCA) cycle, leading to protein aggregation and proteotoxic stress [92]. This discovery has opened new avenues for pro-oxidant cancer therapies targeting copper homeostasis.
Research Protocols for Pro-Oxidant Studies
Protocol 1: Induction of Mitochondrial ROS Production
- Reagents: Rotenone (Complex I inhibitor, 100-500 nM), Antimycin A (Complex III inhibitor, 1-10 µM), DCFH-DA (5-10 µM for detection)
- Procedure: Seed cells in appropriate culture plates and allow to adhere overnight. Replace medium with fresh containing rotenone or antimycin A at determined concentrations. Incubate for 2-24 hours depending on experimental requirements. For detection, load cells with DCFH-DA in serum-free medium for 30 minutes, wash with PBS, and measure fluorescence (Ex/Em: 485/535 nm) [4] [90].
- Validation: Confirm ROS induction using multiple probes; assess mitochondrial membrane potential with TMRE or JC-1; measure cytotoxicity via MTT or LDH release assays.
Protocol 2: Copper-Induced Pro-Oxidant Stress and Cuproptosis
- Reagents: Copper chloride (CuCl₂, 10-100 µM), Elesclomol (copper ionophore, 100-500 nM), NAC (antioxidant control, 1-5 mM)
- Procedure: Prepare copper solutions fresh in serum-free medium. Treat cells with CuClâ‚‚ alone or in combination with elesclomol for 4-48 hours. For rescue experiments, pre-treat with NAC for 2 hours before copper addition. Assess cell viability using resazurin reduction assay; measure protein aggregation via immunoblotting for lipoylated DLAT; detect ROS using CellROX Green [92].
- Validation: Confirm copper dependency using copper chelators (tetrathiomolybdate); assess specific cuproptosis markers including loss of Fe-S cluster proteins.
Antioxidant Agents: Classification and Mechanistic Actions
Endogenous Antioxidant Systems
Table 2: Classification of Antioxidant Systems and Their Mechanisms of Action
| Antioxidant Category | Key Components | Mechanism of Action | Research Applications |
|---|---|---|---|
| Enzymatic Antioxidants | Superoxide dismutase (SOD1/2), Catalase, Glutathione peroxidase (GPX), Peroxiredoxins [17] [91] | Catalytic removal of ROS; SOD converts O₂•⻠to H₂O₂; catalase/GPX reduce H₂O₂ to H₂O [91] | Gene overexpression/knockdown studies; activity assays; biomarker development |
| Non-Enzymatic Endogenous | Glutathione (GSH), α-Lipoic acid, Coenzyme Q10, Melatonin [91] [41] | Direct free radical scavenging; regeneration of other antioxidants; metal chelation [41] | GSH depletion models (BSO); supplementation studies; redox status monitoring |
| Dietary/Nutraceutical | Vitamin C, Vitamin E, Polyphenols (curcumin, resveratrol), Carotenoids, Flavonoids [17] [91] | Direct electron donation; chain-breaking antioxidant activity; activation of Nrf2 pathway [17] | Bioavailability studies; pre-treatment models; structure-activity relationship studies |
The cellular antioxidant system operates through multiple tiers of defense. The first line includes enzymatic antioxidants like superoxide dismutase (SOD), which exists in distinct isoforms compartmentalized to different cellular locations. SOD1 is primarily cytosolic and in the mitochondrial intermembrane space, while SOD2 is localized to the mitochondrial matrix [4]. These enzymes catalyze the dismutation of superoxide to hydrogen peroxide, which is subsequently degraded by catalase in peroxisomes or glutathione peroxidases throughout the cell [91].
The tripeptide glutathione (GSH) represents the most abundant non-enzymatic antioxidant and serves as a central hub in cellular redox homeostasis. GSH directly scavenges reactive species and serves as an essential cofactor for glutathione peroxidases and glutathione transferases. The ratio of reduced (GSH) to oxidized (GSSG) glutathione is a key indicator of cellular redox status, with shifts toward oxidation indicating oxidative stress [4]. The NADPH-dependent enzyme glutathione reductase maintains GSH levels by reducing GSSG, linking antioxidant defense to cellular metabolic status.
Exogenous Antioxidants and Research Protocols
Natural polyphenols such as curcumin, resveratrol, and quercetin represent important research tools for modulating redox signaling. These compounds exhibit multifaceted mechanisms including direct free radical scavenging, metal ion chelation, and activation of the Nrf2 antioxidant pathway [17]. Their effects are often biphasic, with lower concentrations potentially exhibiting pro-oxidant effects that activate adaptive stress responses, while higher concentrations provide direct antioxidant activity.
Protocol 3: Evaluation of Antioxidant Efficacy in Cell Culture
- Reagents: N-acetylcysteine (NAC, 1-5 mM), water-soluble vitamin E analog (Trolox, 50-200 µM), polyphenol of interest (e.g., curcumin, resveratrol; concentration varies by compound)
- Procedure: Pre-treat cells with antioxidant for 2-24 hours before oxidative challenge (e.g., H₂O₂, 100-500 µM; menadione, 25-100 µM). Include vehicle and oxidative stress-only controls. Measure ROS production using fluorescent probes (DCFH-DA, CellROX Green/Orange); assess cell viability via MTT, resazurin, or colony formation assays; examine oxidative damage markers (protein carbonylation, 8-OHdG, lipid peroxidation products) [17] [91].
- Validation: Confirm antioxidant activity in cell-free systems (ORAC, TEAC assays); demonstrate target engagement for Nrf2 activators via nuclear translocation or ARE-reporter assays.
Protocol 4: Assessing Nrf2 Pathway Activation
- Reagents: SFN (sulforaphane, 1-10 µM), tert-butylhydroquinone (tBHQ, 10-50 µM), Nrf2 siRNA/antibodies, ARE-luciferase reporter
- Procedure: Treat cells with Nrf2 activator for 6-24 hours. For nuclear translocation studies, perform subcellular fractionation or immunofluorescence staining. For transcriptional activity, transfert cells with ARE-luciferase reporter construct and measure luciferase activity. Assess downstream targets via qPCR (NQO1, HO-1, GCLC) or western blot [17] [41].
- Validation: Use Nrf2 genetic knockdown (siRNA) to confirm specificity; measure antioxidant response element binding via EMSA.
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 3: Essential Research Reagents for ROS Studies
| Research Tool Category | Specific Reagents | Primary Research Application | Key Considerations & Limitations |
|---|---|---|---|
| ROS Detection Probes | DCFH-DA, CellROX Green/Orange, MitoSOX Red, DHE [90] [91] | Specific detection of general ROS (DCFH-DA), mitochondrial superoxide (MitoSOX), cellular superoxide (DHE) | Artifact potential (photooxidation, non-specific oxidation); proper probe selection for specific ROS |
| Oxidative Damage Markers | Anti-8-OHdG, anti-nitrotyrosine, anti-4-HNE, TBARS assay kits [91] | Detection of oxidative DNA damage (8-OHdG), protein nitration (nitrotyrosine), lipid peroxidation (4-HNE, MDA) | Specificity validation; appropriate controls for immunohistochemistry/ELISA |
| Genetic Manipulation Tools | Nrf2 siRNA/CRISPR, SOD overexpression vectors, NOX expression constructs, ARE-luciferase reporters [17] [4] | Pathway dissection; establish causal relationships; monitor pathway activation | Off-target effects (RNAi); compensatory mechanisms; cell-type specific responses |
| Enzyme Activity Assays | SOD activity kits, catalase activity assays, GSH/GSSG detection kits [91] [41] | Quantify antioxidant enzyme function; measure redox status (GSH/GSSG ratio) | Sample preparation critical (avoid oxidation); tissue/cell-specific normalization |
| Pro-Oxidant Inducers | Rotenone, antimycin A, menadione, copper chloride, elesclomol [4] [92] | Induce mitochondrial ROS, redox cycling, copper-mediated oxidative stress | Concentration optimization critical; monitor cytotoxicity timelines |
Experimental Design Considerations and Integrated Workflow
Designing robust experiments to evaluate ROS-modulating agents requires careful consideration of several critical factors. First, the cellular context significantly influences outcomes—cancer cells often exist under elevated basal ROS and may respond differently to pro-oxidants than non-transformed cells [4]. Second, concentration and timing parameters are crucial, as many ROS modulators exhibit biphasic or hormetic effects [4]. Third, compartmentalization of ROS production and signaling must be considered through use of targeted probes and expression systems.
Figure 2: Experimental Workflow for ROS Modulator Studies. A systematic approach to evaluating pro-oxidant and antioxidant agents, emphasizing appropriate model selection, multi-modal detection, and mechanistic validation.
A comprehensive assessment of ROS-modulating agents should integrate multiple detection methodologies to overcome limitations of individual approaches. Fluorescent probes provide real-time, live-cell monitoring capabilities but require careful controls for artifacts. Biochemical assays measuring oxidative damage markers (8-OHdG, protein carbonylation, lipid peroxidation products) offer more specific but static assessments of oxidative stress [91]. Genetic approaches, including pathway-specific reporters and gene manipulation, establish mechanistic links between ROS changes and functional outcomes.
Functional outcomes should be assessed through context-appropriate endpoints. In cancer models, pro-oxidant efficacy may be measured through apoptosis assays, clonogenic survival, and in vivo tumor growth inhibition [4] [92]. For antioxidant applications in neurodegenerative or inflammatory disease models, appropriate endpoints include viability assays, inflammatory cytokine production, and markers of cellular senescence [93] [94]. Combining these approaches provides a comprehensive understanding of ROS modulator mechanisms and potential therapeutic utility.
The comparative analysis of pro-oxidant and antioxidant agents reveals a complex landscape of redox modulation with significant research and therapeutic implications. Pro-oxidant approaches offer promising strategies in oncology, where elevated basal ROS levels create vulnerability to further oxidative insult, while antioxidant interventions hold potential for conditions driven by chronic oxidative stress including neurodegenerative, inflammatory, and metabolic diseases [17] [4] [92].
Future research directions will likely focus on developing more specific targeting strategies, including tissue-specific delivery systems and agents that selectively modulate ROS in specific cellular compartments. The emerging understanding of distinct ROS-mediated cell death pathways such as cuproptosis provides new therapeutic targets [92]. Additionally, personalized approaches considering individual genetic variations in antioxidant pathways and redox homeostasis may enhance therapeutic efficacy while minimizing off-target effects.
The successful translation of ROS-modulating strategies will depend on sophisticated experimental design that acknowledges the dual nature of ROS in cellular physiology and pathology. Researchers must carefully consider context, concentration, and compartmentalization when designing studies and interpreting results. As our understanding of redox biology continues to evolve, so too will our ability to precisely manipulate these pathways for research and therapeutic benefit.
In vivo models are indispensable tools for validating reactive oxygen species (ROS) signaling mechanisms and their implications in disease pathogenesis and therapeutic development. While in silico predictions and in vitro assays provide initial insights, the complex interplay of ROS within living organisms—including pharmacokinetics, tissue remodeling, and systemic effects—can only be fully assessed in animal models [95]. ROS function as crucial signaling molecules that regulate cellular processes such as proliferation, differentiation, and cell death, but they also contribute to oxidative stress and tissue damage when homeostasis is disrupted [1]. The dual nature of ROS in physiological signaling and pathological processes necessitates research models that can faithfully recapitulate this balance in a whole-organism context.
Murine models, particularly mice and rats, offer physiological similarities to humans that make them preferred systems for investigating ROS signaling pathways. Researchers leverage everything from conventional rodent models to sophisticated genetically engineered systems and patient-derived xenografts to explore ROS dynamics in health and disease. The selection of an appropriate in vivo model depends on the specific research question, whether it involves target identification, validation of ROS-mediated mechanisms, or preclinical assessment of antioxidant or pro-oxidant therapies [95]. This technical guide provides a comprehensive overview of the core in vivo models used in ROS research, with detailed methodologies and applications tailored for researchers and drug development professionals.
Murine Models in Research: Fundamentals and Applications
Physiological and Genetic Similarities
Murine models show significant physiological similarities to humans and share approximately 99% of conserved genomic regions, making them invaluable for studying conserved ROS signaling pathways and their biological effects [96]. Their miniature size, affordability, and handling ease provide practical advantages over larger animal models [96]. Additionally, mice genes can be readily manipulated to create specific disease models, and tissue sections are accessible for detailed histopathological examination of ROS-mediated damage [96].
Different mouse strains exhibit varying susceptibility to oxidative stress and related pathologies, enabling researchers to select models based on their specific research needs. For example, BALB/c mice are widely used in research involving oxidative stress and are resistant to cerebral malaria, making them suitable for studying systemic rather than neurological oxidative damage [96]. C3H/HeJ mice represent an immunocompetent inbred strain susceptible to various challenges, while AKR/J mice display resistance to cerebral malaria due to deficiency in complement component C5 [96]. These strain-specific characteristics must be considered when designing experiments related to ROS signaling.
Rodent Plasmodium Species for ROS Studies
The table below summarizes rodent Plasmodium species and their applications in ROS research:
Table 1: Rodent Plasmodium Species for Modeling ROS-Related Pathologies
| Plasmodium Species | Pathology Model | Research Applications | ROS Implications |
|---|---|---|---|
| P. berghei ANKA | Severe malaria, cerebral malaria | Models for P. falciparum infection, severe malaria [96] | Oxidative burst in cerebral tissue, endothelial dysfunction |
| P. yoelii 17XL | Lethal infection | Models for severe malaria [96] | Systemic oxidative stress, organ damage |
| P. yoelii 17XNL | Non-lethal infection | Malaria vaccine development [96] | Protective immune responses involving ROS signaling |
| P. chabaudi | Human malaria pathology and immunology | General malaria pathology studies [96] | Inflammation-related oxidative stress |
Genetically Engineered Models (GEMs) for Targeted ROS Research
Design Principles and Generation Methods
Genetically Engineered Models (GEMs) are specifically designed to replicate human disease biology by inserting, deleting, or altering specific genes using techniques such as CRISPR/Cas9, traditional transgenesis, or targeted gene knockouts [97]. These models provide essential in vivo systems to study the genetic basis of ROS-related diseases, evaluate drug efficacy, and explore biological functions in a controlled environment that cell cultures and in vitro studies cannot fully replicate [97].
The various genetic modifications possible include knockout models where a gene is completely disabled to study loss-of-function effects; knock-in models where specific mutations or reporter genes are inserted into the genome; humanized models where human genes or immune components are introduced to better mimic human biology; and conditional models where gene expression is controlled spatially or temporally using inducible systems [97]. Each approach offers distinct advantages for ROS signaling research, particularly for studying spatially and temporally regulated oxidative processes.
Applications in ROS Signaling Research
GEMs enable researchers to investigate specific ROS signaling pathways and their role in disease pathogenesis. For example, the rasH2 mouse model carries a human HRAS transgene that increases susceptibility to carcinogenesis, making it valuable for studying ROS-mediated DNA damage and tumor development [97]. Transgenic mice expressing chimeric human HLA molecules represent unique in vivo experimental models for evaluating human immune system function, including ROS-dependent immune responses commonly used in vaccine and immuno-oncology research [97].
NOG (CIEA NOG mouse) portfolio models provide a versatile super immunodeficient platform that offers advantages over standard nude and scid strains, particularly for engraftment of challenging cell lines, patient-derived xenografts, and immune system humanization [97]. These models enable researchers to study human-specific ROS signaling pathways in an in vivo context, bridging the gap between conventional rodent models and human clinical applications.
Patient-Derived Xenograft (PDX) Models
Establishment and Engraftment Techniques
Patient-Derived Xenograft (PDX) models are established by transplanting fresh tumor tissue resected from human cancer into immunocompromised mice [98]. The tumor pieces can be implanted subcutaneously, orthotopically, or heterotopically into locations such as the intracapsular fat pad, the anterior compartment of the eye, or under the renal capsule [98]. Orthotopic implantation (engraftment into the same tissue origin) generally better preserves the tumor microenvironment and associated ROS signaling dynamics.
The establishment time varies by tumor type, ranging from a few days to several months. When the tumor reaches 1-2cm³ (first generation, designated P1), it can be segmented and reimplanted for passage, with establishment time typically stabilizing at 40-50 days with subsequent passages [98]. To avoid engraftment rejection, PDX models require immunocompromised mice such as athymic nude mice, severe combined immunodeficiency (SCID) mice, non-obese diabetic-severe combined immunodeficiency (NOD-SCID) mice, or further optimized strains [98].
Advantages for ROS Signaling Research
PDX models excel in recapitulating the spatial structure of original tumors and maintaining intratumor heterogeneity, which is crucial for studying ROS gradients and their differential effects on various tumor subpopulations [98]. These models retain the genomic features of patient tumors across different stages, subtypes, and treatment backgrounds, preserving patient-specific ROS regulatory mechanisms [98].
PDX models also provide a platform for studying therapy-induced changes in ROS homeostasis. They show similar responses to chemotherapy in corresponding patients and have been used to identify HER-2 inhibitors for treating cetuximab-resistant patients [98]. The "mouse hospital" concept—in vivo drug testing in models that recapitulate different cancer subtypes before clinical trials—leverages PDX models to predict therapeutic responses and identify biomarkers of drug sensitivity and resistance [98].
Experimental Design for In Vivo Validation Studies
Key Considerations for Study Design
Proper experimental design is crucial for generating meaningful data from in vivo ROS studies. The intention of the study defines how its design will differ for in vivo target identification versus drug and/or target validation [95]. For target identification, an exploratory approach may require only two groups (with and without specific intervention), while target validation studies need appropriate control groups for all types of manipulation [95].
Inclusion and exclusion criteria must be defined for all animal studies involving disease models. For example, if testing a compound in an inducible model, each individual animal should meet the disease criteria before inclusion in the study [95]. In spontaneous models, researchers should exclude animals that do not exhibit the expected phenotype—for instance, approximately 10% of db/db mice may not show elevated blood glucose levels and should be excluded from diabetes-related studies [95].
Species and Strain Selection
Mice are generally preferred when gene knockout technology is used, while rats are better suited for most solid-organ transplantation models due to technical reasons related to surgical procedures [95]. Some disease models are restricted to specific species; for example, anti-Thy1.1 nephropathy or Heymann nephritis are restricted to rats because mice lack the disease-specific antigens [95].
The rationale for selecting the particular species, strain, gender, and age of animals must be provided, and these should be accessible to the scientific community [95]. Strain-specific characteristics can significantly influence ROS responses, and these variations must be considered when designing experiments and interpreting results.
Advanced Methodologies for ROS Detection and Monitoring
Single-Cell Signaling Network under Redox Stress Profiling (SN-ROP)
The SN-ROP method utilizes multi-parameter, single-cell mass cytometry to map redox-associated signaling networks within individual cells [55]. This approach involves comprehensive screening of antibodies targeting redox-related proteins to identify those suitable for single-cell profiling, enabling researchers to trace key redox dynamics involved in cellular activation and identify significant alterations within ROS networks [55].
SN-ROP quantifies ROS transporters, pivotal ROS-generating and ROS-scavenging enzymes and their regulatory modifications, products of prolonged oxidative stress, and the transcription factors and signaling molecules that drive specific redox programs [55]. This method has been validated against mass spectrometry-based quantitative proteome datasets, showing notable concordance between the techniques [55].
Application and Validation
SN-ROP has been applied to analyze various immune cell types, including CAR-T cells and immune cells from patients with conditions such as chronic hemodialysis and hepatocellular carcinoma [55]. The method can distinguish unique redox patterns across different cell types, with markers such as Ref/APE1 primarily associated with T and B cells, while NNT and PCYXL are significantly enriched in neutrophils [55].
Machine learning algorithms trained with SN-ROP profiles from healthy donors have demonstrated prediction accuracies exceeding 95% for six main immune subsets based on redox features alone, confirming that the method accurately detects redox patterns associated with cell lineage [55]. This high-resolution platform provides new insights into immune regulation and disease pathophysiology through redox signaling adaptations.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions for In Vivo ROS Studies
| Reagent/Model | Function/Application | Specific Use in ROS Research |
|---|---|---|
| NOG (CIEA NOG mouse) | Super immunodeficient model for engraftment | Human immune system reconstitution for studying human-specific ROS signaling [97] |
| rasH2 Mouse Model | Carries human HRAS transgene for carcinogenesis studies | Short-term carcinogenicity testing of compounds involving ROS-mediated DNA damage [97] |
| Transgenic HLA Mice | Express human HLA molecules | Vaccine and immuno-oncology research involving ROS-dependent antigen presentation [97] |
| Antibody Panels for SN-ROP | Single-cell redox network profiling | Simultaneous quantification of 33+ ROS-related proteins for systems-level redox analysis [55] |
| Cryopreserved GEMs | Preservation and distribution of genetically engineered models | Maintain genetic integrity of specialized ROS models; provide perpetual use rights [97] |
In vivo models, including murine models, genetically engineered systems, and patient-derived xenografts, provide indispensable platforms for validating ROS signaling mechanisms and developing therapeutic interventions. Each model system offers distinct advantages and limitations that must be carefully considered in experimental design. The integration of advanced technologies such as single-cell redox profiling and genetically humanized models continues to enhance the translational relevance of these systems. By selecting appropriate models and implementing rigorous experimental designs, researchers can generate clinically relevant insights into ROS homeostasis and its therapeutic manipulation across diverse disease contexts.
Visual Appendix
Workflow for Establishing and Applying PDX Models in ROS Research
Strategic Selection Framework for In Vivo ROS Models
The clinical trial landscapes for cancer and neurodegenerative diseases are undergoing a transformative shift, increasingly informed by our growing understanding of molecular signaling pathways, including reactive oxygen species (ROS) homeostasis. This review synthesizes key recent outcomes from 2024-2025, highlighting a movement towards precision medicine, novel therapeutic modalities, and innovative trial designs. In cancer, breakthroughs include targeted therapies, antibody-drug conjugates, and mRNA-based platforms showing significant efficacy. Concurrently, neurodegenerative disease research is advancing with targeted protein inhibitors, stem cell therapies, and genetically-defined interventions. The integration of ROS signaling mechanisms into our understanding of both therapeutic efficacy and disease pathophysiology provides a unifying framework for interpreting these advances and designing future interventions. This report details these outcomes, provides associated experimental methodologies, and outlines essential research tools for continued progress.
The clinical translation of basic scientific discoveries is accelerating, driven by a deeper comprehension of disease pathophysiology. The year 2025 has been marked by significant findings in both oncology and neurodegeneration, two fields facing the complex challenges of disease heterogeneity and treatment resistance. A critical mechanistic element underlying many recent advances is the role of reactive oxygen species (ROS) signaling. ROS, a collection of highly reactive oxygen-containing molecules, function as critical signaling entities and potential toxic agents at the cellular level [1]. The dynamic equilibrium of ROS homeostasis is essential for normal cellular function, including processes like proliferation, differentiation, and metabolism [1] [41]. Dysregulation of this balance impairs cellular and organismal physiology, contributing to the pathogenesis of a wide spectrum of diseases, including cancer and neurodegenerative disorders [1]. This review will frame recent clinical trial outcomes within this context, examining how new therapies implicitly or explicitly modulate these fundamental pathways to achieve clinical benefit.
Recent Therapeutic Advances in Cancer Clinical Trials
The cancer clinical trial landscape in 2025 is characterized by the refinement of targeted therapies and the emergence of novel platform technologies. The following table summarizes pivotal recent trials and their outcomes.
Table 1: Key Cancer Clinical Trial Outcomes in 2024-2025
| Trial Name / Therapy | Cancer Type | Phase | Key Intervention | Primary Outcome |
|---|---|---|---|---|
| EMBER-4 [99] | Early-stage, high-risk ER+/HER2- breast cancer | Phase 3 | Imlunestrant (oral SERD) | (Based on EMBER-3: 38% reduction in progression alone; 43% with abemaciclib) |
| DESTINY-Breast06 [99] | HER2-low/Ultralow HR+ metastatic breast cancer | Phase 3 | Trastuzumab Deruxtecan (T-DXd) | Significantly improved progression-free & overall survival vs. physician's choice chemo |
| INAVO120 [99] | HR+/HER2- metastatic breast cancer (PIK3CA-mutated) | Phase 3 | Inavolisib + palbociclib + fulvestrant | Median PFS: 15 months vs. 7 months (placebo combo) |
| BNT142 [100] | CLDN6-positive solid tumors (testicular, ovarian, etc.) | Phase 1/2 | Lipid nanoparticle-encapsulated mRNA encoding bispecific antibody | Manageable safety profile & promising anti-tumor activity at higher doses |
| Thyroid Combo Therapy [100] | BRAF V600E Anaplastic Thyroid Cancer | Phase 2 | Neoadjuvant Dabrafenib + Trametinib + Pembrolizumab (DTP) | 67% with no residual cancer post-surgery; 69% 2-year overall survival |
| VLS-1488 [100] | Cancers with chromosomal instability | Phase 1/2 | Oral KIF18A inhibitor | Generally safe, tolerable; showed anti-tumor activity in heavily pre-treated patients |
| Pivekimab Sunirine [100] | Blastic Plasmacytoid Dendritic Cell Neoplasm (BPDCN) | Phase 2 | Anti-CD123 antibody-drug conjugate | High, durable composite complete remission responses |
Detailed Experimental Protocol: mRNA-Encoded Bispecific Antibody (BNT142)
Objective: To assess the safety, tolerability, and preliminary efficacy of BNT142, a lipid nanoparticle (LNP)-encapsulated mRNA that encodes the anti-CLDN6/CD3 bispecific antibody RiboMab02.1, in patients with CLDN6-positive advanced solid tumors [100].
Methodology:
- Trial Design: First-in-human, Phase I/II, multi-center, open-label study with a dose-escalation and dose-expansion phase.
- Intervention: Participants receive intravenous infusions of BNT142 weekly. The dose-escalation phase employs a "3+3" design across seven predefined dose levels to determine the maximum tolerated dose (MTD) and recommended Phase II dose (RP2D).
- Primary Endpoints:
- Incidence of dose-limiting toxicities (DLTs).
- Incidence and severity of adverse events (AEs).
- Objective Response Rate (ORR) per RECIST v1.1.
- Key Biomarkers/Imaging: CLDN6 tumor expression is confirmed via immunohistochemistry (IHC) of tumor tissue. Tumor response is assessed radiologically via CT or MRI scans at predefined intervals.
This trial represents a novel therapeutic paradigm where the patient's own body is used as a "bioreactor" to produce a potent anti-cancer bispecific antibody, bypassing complex recombinant protein manufacturing and leveraging the transient yet potent expression enabled by mRNA technology.
Recent Therapeutic Advances in Neurodegenerative Disease Clinical Trials
Neurodegenerative disease trials are increasingly focusing on genetically-stratified populations and disease-modifying therapies, moving beyond symptomatic management. The NIH is currently funding 495 clinical trials for Alzheimer's and related dementias, including 68 testing promising drug candidates [101].
Table 2: Key Neurodegenerative Disease Clinical Trial Outcomes in 2024-2025
| Trial Name / Therapy | Disease | Phase | Key Intervention | Primary Outcome / Goal |
|---|---|---|---|---|
| OlympiA [99] | High-risk, HER2- breast cancer with BRCA1/2 mutations | Phase 3 | Olaparib (PARP inhibitor) | 28% reduction in risk of death; significant improvement in overall survival |
| CT1812 [101] | Alzheimer's Disease (AD) / Dementia with Lewy Bodies (DLB) | Phase 2B | Small molecule (displaces toxic amyloid & alpha-synuclein aggregates) | Recruiting; evaluating efficacy to improve cognitive function |
| PSP Platform Trial [101] | Progressive Supranuclear Palsy (PSP) | Platform | Testing ≥3 different therapies under a single master protocol | Aims to expedite therapeutic assessment for this rare dementia |
| Levetiracetam Repurposing [101] | Alzheimer's Disease / Mild Cognitive Impairment | Phase 2 | Antiepileptic drug (levetiracetam) | May slow brain atrophy in APOE ε4 non-carriers |
| TNBC Vaccine Study [99] | Triple-Negative Breast Cancer (TNBC) | Phase 1 | α-lactalbumin vaccine (+/- pembrolizumab) | Safe, well-tolerated; >70% immune response; Phase 2 planned (neoadjuvant) |
| PPMI Study [102] | Parkinson's Disease (PD) | Observational | Longitudinal deep phenotyping | Establishing biomarkers for PD progression |
| iPS Cell Therapy [102] | Parkinson's Disease | Phase I/II | Transplantation of iPS cell-derived dopaminergic progenitors | Evaluating safety and efficacy of cell replacement therapy |
| PTC518 [102] | Huntington's Disease (HD) | Phase 2 | Small molecule (targeting HTT mRNA) | Evaluating safety and pharmacodynamic effects |
Detailed Experimental Protocol: Stem Cell Transplantation for Parkinson's Disease
Objective: To evaluate the safety and efficacy of transplanting human induced pluripotent stem cell (iPS cell)-derived dopaminergic progenitors (CT1-DAP001) into the corpus striatum of patients with Parkinson's disease [102].
Methodology:
- Trial Design: Phase I/II, open-label, surgical intervention study.
- Participant Selection: Patients aged 40-75 with a confirmed diagnosis of idiopathic Parkinson's disease, responsive to levodopa but with worsening motor symptoms.
- Intervention: Under stereotactic guidance, the investigational product (CT1-DAP001) is bilaterally injected into the putamen, a key component of the dorsal striatum. Immunosuppression is administered peri- and post-operatively to prevent graft rejection.
- Primary Endpoints:
- Safety: Incidence and severity of adverse events, including tumors (teratoma formation) and graft-induced dyskinesias.
- Efficacy: Change from baseline in the MDS-UPDRS (Movement Disorder Society-Unified Parkinson's Disease Rating Scale) Part III motor score in the practically defined "OFF" medication state at 1-2 years post-transplantation.
- Key Biomarkers/Imaging: Dopaminergic graft survival and integration are assessed longitudinally using dopamine transporter (DaT) SPECT imaging. Functional MRI and detailed neuropsychological testing are also performed.
This protocol represents a cutting-edge approach aimed at restoring lost neural circuitry, moving beyond pharmacologic dopamine replacement to a potentially restorative therapy.
Methodological Innovations and the Role of ROS Signaling
A critical trend across both fields is the move towards precision medicine and more efficient trial designs. This is particularly vital in neurodegenerative diseases, where the traditional "one-size-fits-all" approach has repeatedly failed [103]. Innovations include Multi-Arm, Multi-Stage (MAMS) platform trials, which allow for the simultaneous evaluation of multiple therapies against a shared control group, and the strategic use of master protocols for patient selection, data management, and logistics [101] [103].
ROS Signaling as a Connecting Framework
The pathophysiology of both cancer and neurodegeneration is intimately linked with dysregulated ROS homeostasis [1] [41]. At low concentrations, ROS act as signaling molecules regulating proliferation, differentiation, and metabolism. However, excessive ROS causes oxidative damage to lipids, proteins, and DNA, contributing to disease.
- In Cancer, elevated ROS can promote tumorigenesis and genomic instability, but cancer cells also experience higher intrinsic ROS levels, making them vulnerable to further oxidative stress induced by chemotherapeutics or radiation [1] [41].
- In Neurodegeneration, oxidative stress is a hallmark, with excessive ROS leading to neuronal damage and death. Key sources include mitochondrial dysfunction and protein aggregates (e.g., amyloid-beta, alpha-synuclein) that can disrupt cellular redox balance [101] [1].
Several therapies in development directly or indirectly engage these pathways. For instance, the small molecule CT1812 is designed to displace toxic protein aggregates at synapses, which are known to induce oxidative stress and neurotoxicity [101]. Furthermore, the exploration of senolytic drugs in conditions like ALS aims to clear senescent glial cells that release ROS and other factors accelerating disease progression [104].
The diagram below illustrates the dual role of ROS in cell fate and how therapeutic interventions can target this balance.
Diagram: ROS in Cell Fate and Therapy. ROS have a dual role: at low levels, they promote cell survival and signaling; at high levels, they cause damage and cell death. Therapeutics can aim to either restore ROS homeostasis (antioxidant strategies) or push cancer cells beyond their redox capacity (pro-oxidant strategies).
The Scientist's Toolkit: Essential Research Reagents and Materials
Advancing the field requires a suite of specialized reagents and tools. The following table details key materials essential for research in this domain.
Table 3: Key Research Reagent Solutions for ROS and Disease Mechanism Studies
| Reagent / Material | Function / Application | Key Characteristics |
|---|---|---|
| siRNA/shRNA Libraries [103] | Gene silencing to validate therapeutic targets (e.g., KIF18A, CLDN6). | Enables high-throughput loss-of-function screens to assess gene dependency. |
| Recombinant Proteins (e.g., CLDN6, Alpha-synuclein) [100] | Target protein for antibody characterization, binding assays, and structural studies. | High purity and correct post-translational modifications are critical for functional studies. |
| Lipid Nanoparticles (LNPs) [100] | Delivery vehicle for nucleic acid-based therapeutics (e.g., mRNA, ASOs). | Formulated for stability, tissue tropism, and efficient intracellular delivery. |
| Antisense Oligonucleotides (ASOs) [103] | Modulate splicing or reduce expression of disease-causing genes (e.g., HTT, C9orf72). | Chemically modified (e.g., 2'-O-methoxyethyl) to enhance stability and binding affinity. |
| Induced Pluripotent Stem Cells (iPSCs) [102] | Disease modeling and source for cell replacement therapies (e.g., dopaminergic neurons). | Can be derived from patients to create genetically relevant in vitro models. |
| ROS-Sensitive Fluorescent Dyes (e.g., H2DCFDA, MitoSOX) [1] [41] | Detect and quantify specific intracellular ROS (general ROS, mitochondrial superoxide). | Cell-permeable probes that become fluorescent upon oxidation, measurable by flow cytometry or microscopy. |
| Phospho-Specific Antibodies (p-MAPK, p-AKT, etc.) [41] | Interrogate activation status of ROS-influenced signaling pathways (MAPK, PI3K/AKT). | Validated for use in Western blot, IHC, and immunofluorescence to monitor pathway activity. |
| CRISPR-Cas9 Gene Editing Systems [103] | Generate isogenic cell lines with specific mutations (e.g., PIK3CA, BRCA1) or knock-in reporters. | Enables precise genetic manipulation to establish causal relationships. |
The experimental workflow for developing and validating these therapies often follows a path from in vitro models to in vivo studies and finally to clinical trials, with ROS measurements integrated throughout.
Diagram: Therapeutic Development Workflow. The path from target identification to clinical trials, highlighting points where ROS analysis (dashed lines) is integrated to understand mechanism, efficacy, and toxicity.
Reactive oxygen species (ROS) homeostasis represents a fundamental biological process wherein cells dynamically regulate their ROS levels to ensure survival and proper physiological function. These highly reactive molecules serve as both critical signaling mediators and potential toxic agents, playing a dual role in cellular physiology and pathology [1]. Under physiological conditions, oxidative free radicals generated by the mitochondrial oxidative respiratory chain, endoplasmic reticulum, and NADPH oxidases are effectively neutralized by NRF2-mediated antioxidant responses, which elevate the synthesis of superoxide dismutase (SOD), catalase, and key molecules like nicotinamide adenine dinucleotide phosphate (NADPH) and glutathione (GSH) [8]. This delicate balance maintains cellular redox homeostasis, but its disruption is intimately linked to disease pathogenesis across multiple organ systems [1] [8].
The concept of "oxidative stress" was formally defined in 1985 as a cellular imbalance between oxidants and reductants, leading to the differentiation of eustress and distress to describe oxidative stress states under physiological and pathological conditions [8]. While traditionally viewed as toxic metabolic by-products, ROS are now recognized as similar to other modification modes that can affect molecular signaling pathways through redox modification, thereby influencing various biological activities [8]. This signaling function occurs primarily through oxidative post-translational modifications (Oxi-PTMs) of proteins, particularly on cysteine and methionine residues, which act as molecular switches that precisely regulate protein function by adjusting structure, charge distribution, stability, and interaction capabilities [7].
In the context of biomarker development, understanding these ROS signaling mechanisms provides the foundational rationale for selecting specific oxidative stress markers that reflect underlying pathophysiological processes rather than merely representing epiphenomena. This technical guide explores the validation of these markers for stratifying patients across various disease states, with particular emphasis on methodological considerations, clinical correlations, and integration into existing risk assessment frameworks.
Key Oxidative Stress Biomarkers: Measurement and Significance
Classification of Reactive Oxygen Species
ROS encompass a diverse collection of oxidative molecules with varying biological functions and chemical reactivities. Understanding this classification is essential for selecting appropriate biomarkers for specific clinical contexts [1]:
Free Radicals: These include superoxide anion (•Oâ‚‚â»), hydroperoxyl radicals (HO₂•), hydroxyl radical (•OH), peroxyl radicals (RO₂•), alkoxyl radicals (RO•), and carbonate radical anion (CO₃•â»). The superoxide anion represents the main initial ROS product, typically generated from electron leakage in the mitochondrial respiratory chain and stored in mitochondria during cellular diffusion [1]. It possesses strong oxidative properties and can react with reductive substances or biomolecules within the cell, thereby regulating redox reactions and influencing the expression of intracellular signaling molecules [1].
Non-radicals: This category includes hydrogen peroxide (H₂O₂), ozone (O₃), singlet oxygen (¹O₂), hypochlorous acid (HOCl), hypobromous acid (HOBr), lipid peroxides (LOOH), and hypothiocyanous acid (HOSCN) [1]. H₂O₂ serves as an important signaling molecule primarily produced intracellularly through enzymatic reactions, notably by NADPH oxidase (NOX) family enzymes which are key dedicated generators of ROS [1].
Table 1: Major Reactive Oxygen Species and Their Characteristics
| ROS Category | Specific Type | Chemical Formula | Primary Sources | Biological Significance |
|---|---|---|---|---|
| Free Radicals | Superoxide anion | •O₂⻠| Mitochondrial electron transport, NADPH oxidases | Primary initial ROS product; converted to H₂O₂ by SOD |
| Hydroxyl radical | •OH | Fenton reaction, Haber-Weiss reaction | Extremely reactive; causes DNA strand breaks, lipid peroxidation | |
| Alkoxyl radicals | RO• | Decomposition of lipid peroxides | Propagates lipid peroxidation chain reactions | |
| Non-radicals | Hydrogen peroxide | Hâ‚‚Oâ‚‚ | Superoxide dismutation, NOX enzymes | Signaling molecule; relatively stable; diffusible |
| Lipid peroxides | LOOH | Peroxidation of unsaturated lipids | Membrane damage; source of secondary ROS | |
| Singlet oxygen | ¹O₂ | Photosensitization reactions | Oxidizes proteins, lipids; role in light-stress responses |
Established Biomarkers of Oxidative Damage and Antioxidant Capacity
Validated oxidative stress biomarkers for patient stratification can be categorized into markers of oxidative damage and markers of antioxidant capacity:
Oxidative Damage Markers: Malondialdehyde (MDA) and protein carbonyl (PCO) content represent well-validated markers of lipid and protein oxidation, respectively. In acute myocardial infarction (AMI) patients, significantly elevated levels of both MDA (p < 0.001) and PCO (p < 0.001) have been observed compared to controls, with strong positive correlations to clinical risk scores (SYNTAX and ACEF) [105]. Bootstrap validation has revealed that MDA and PCO demonstrate consistent stability across analyses, making them among the most reliable oxidative stress biomarkers [105].
Antioxidant Capacity Markers: The glutathione system components—including reduced glutathione (GSH), glutathione S-transferase (GST), glutathione reductase (GR), and glutathione peroxidase (GPx)—along with total sulfhydryl (TSH) groups represent crucial elements of the cellular antioxidant defense system. AMI patients exhibit significantly lower antioxidant parameters (TSH, GST, GR, GPx, and GSH; all p < 0.001) than controls [105]. The reliability of these markers varies, with GST demonstrating consistent stability across patient subgroups, while GPx and GSH show subtype-specific patterns with lower reliability, particularly in NSTEMI patients [105].
Composite Indices: The oxidative stress index (OSI), calculated based on the ratio between diacron-reactive oxygen metabolites (d-ROMs) and biological antioxidant potential (BAP), provides an integrated assessment of redox status. In long COVID patients, median OSI values were 2.0 [IQR: 1.7-2.5], with significantly higher levels in females (2.3 vs. 1.8) and positive correlations with age and body mass index [106]. Optimal OSI cut-off values were determined to be 1.32 for distinguishing long COVID from healthy controls and 1.92 for identifying brain fog among patients with long COVID [106].
Table 2: Established Oxidative Stress Biomarkers and Measurement Methodologies
| Biomarker | Biological Significance | Measurement Techniques | Clinical Correlations |
|---|---|---|---|
| Malondialdehyde (MDA) | Lipid peroxidation end product | Spectrophotometry, HPLC | Strong correlation with SYNTAX (R=0.72) and ACEF scores in AMI [105] |
| Protein Carbonyl (PCO) | Protein oxidation marker | Spectrophotometry, DNPH assay | Independent predictor of SYNTAX score in multivariate analysis [105] |
| Reduced Glutathione (GSH) | Major cellular antioxidant | Spectrophotometry, HPLC | Significantly reduced in AMI patients (p < 0.001) [105] |
| Glutathione S-transferase (GST) | Phase II detoxification enzyme | Spectrophotometric activity assays | Consistent stability in bootstrap validation; reliable across patient subgroups [105] |
| d-ROMs | Total reactive oxygen metabolites | Spectrophotometric assay using N,N-diethyl-p-phenylenediamine | Significantly elevated in long COVID (534 CARR U) with gender differences (580 vs 462 in females vs males) [106] |
| Biological Antioxidant Potential (BAP) | Total antioxidant capacity | Spectrophotometric ferric reduction assay | Negatively correlates with age and BMI in long COVID patients [106] |
| Oxidative Stress Index (OSI) | Integrated redox status | Calculated ratio (d-ROMs/BAP) | Cut-off 1.32 for long COVID detection; 1.92 for brain fog identification [106] |
Experimental Protocols for Biomarker Validation
Spectrophotometric Assay Protocols
Malondialdehyde (MDA) Quantification via TBARS Assay: The thiobarbituric acid reactive substances (TBARS) assay represents one of the most widely employed methods for assessing lipid peroxidation through malondialdehyde measurement. The protocol involves: (1) Preparation of serum or plasma samples by combining 100μL of biological sample with 200μL of sodium dodecyl sulfate (8.1%) solution; (2) Addition of 750μL of thiobarbituric acid (0.8%) and 750μL of acetic acid solution (20%, pH 3.5); (3) Incubation at 95°C for 60 minutes; (4) Cooling on ice for 10 minutes followed by centrifugation at 10,000g for 15 minutes; (5) Measurement of absorbance at 532nm against appropriate blanks and standards. Calculations are performed using the molar extinction coefficient for MDA-thiobarbituric acid complex (ε = 1.56 × 10âµ Mâ»Â¹cmâ»Â¹) [105].
Glutathione S-transferase (GST) Activity Assay: GST activity is determined by measuring the conjugation of glutathione with 1-chloro-2,4-dinitrobenzene (CDNB). The assay protocol includes: (1) Preparation of reaction mixture containing 100mM potassium phosphate buffer (pH 6.5), 1mM glutathione, and 1mM CDNB; (2) Addition of 50μL of serum or tissue homogenate to initiate the reaction; (3) Continuous monitoring of absorbance increase at 340nm for 3 minutes at 25°C; (4) Calculation of enzyme activity using the extinction coefficient for CDNB conjugate (ε = 9.6 mMâ»Â¹cmâ»Â¹). One unit of GST activity is defined as the amount of enzyme catalyzing the conjugation of 1μmol of CDNB with GSH per minute under specified conditions [105].
Integrated Oxidative Stress Assessment Protocol
d-ROMs and BAP Testing for OSI Calculation: The simultaneous measurement of diacron-reactive oxygen metabolites (d-ROMs) and biological antioxidant potential (BAP) provides an integrated assessment of oxidative stress status: (1) For d-ROMs testing, serum samples are incubated with an acidic buffer (pH 4.8) to liberates hydroperoxides from proteins; (2) Released hydroperoxides undergo Fenton reaction to produce alkoxyl and peroxyl radicals, which oxidize N,N-diethyl-p-phenylenediamine to generate a pink chromogen measured photometrically at 505nm; (3) Results are expressed in Carratelli Units (1 CARR U = 0.08 mg H₂O₂/dL); (4) For BAP testing, serum is added to a colored solution containing ferric chloride and a thiocyanate derivative; (5) The reduction of ferric ions to ferrous ions by serum antioxidants causes decolorization measured at 505nm; (6) The oxidative stress index (OSI) is calculated as: OSI = C × (d-ROMs/BAP), where C is a standardization coefficient set to make the mean OSI of healthy controls equal to 1.0 [106].
Analytical Approaches for Biomarker Validation
Statistical Validation Methods
Robust statistical approaches are essential for establishing the clinical validity of oxidative stress biomarkers:
Bootstrap Resampling: This technique involves repeatedly sampling with replacement from the original dataset to evaluate the stability and reliability of biomarker associations. In AMI research, bootstrap validation revealed a hierarchy of biomarker reliability, with MDA, PCO, and GST demonstrating consistent stability across all analyses, whereas GPx and GSH showed subtype-specific patterns with lower reliability, especially in NSTEMI patients [105].
Multivariate Regression Analysis: This approach identifies independent predictors of clinical outcomes while controlling for potential confounders. In a study of AMI patients, multivariate analysis identified age, MDA, PCO, GST, GR, and GSH as independent predictors of SYNTAX score (R² = 0.78), while only age and eGFR predicted ACEF score (R² = 0.65) [105].
Correlation Analysis: Pearson correlation examines linear relationships between oxidative stress markers and clinical risk scores. Strong positive correlations were observed between SYNTAX and ACEF scores in both STEMI (R = 0.72, 95% CI: 0.65-0.78) and NSTEMI groups (R = 0.69, 95% CI: 0.61-0.76) [105]. MDA and PCO showed strong positive correlations with both scoring systems across all patient groups.
Clinical Stratification Applications
Oxidative stress biomarkers demonstrate significant potential for patient stratification across various clinical contexts:
Cardiovascular Risk Stratification: In acute myocardial infarction, oxidative stress biomarkers show strong associations with established risk scoring systems. The integration of validated oxidative stress biomarkers into existing scoring systems may help refine prognostic accuracy and guide personalized treatment strategies for AMI patients [105].
Long COVID Subphenotyping: Oxidative stress markers effectively distinguish clinical subgroups within long COVID populations. Patients reporting brain fog exhibited significantly higher OSI levels (2.2 vs. 1.8), particularly among females (d-ROMs: 625.6 vs. 513.0; OSI: 2.4 vs. 2.0) [106]. These markers may serve as indicators for the presence or prediction of psycho-neurological symptoms associated with long COVID in a gender-dependent manner.
Therapeutic Monitoring: The responsiveness of oxidative stress biomarkers to interventions makes them promising tools for tracking treatment efficacy. While antioxidant-based therapies have shown early promise in conditions where oxidative stress plays a primary pathological role, their efficacy in diseases characterized by complex, multifactorial etiologies remains controversial [8].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Oxidative Stress Biomarker Studies
| Research Reagent | Specific Function | Application Examples | Technical Considerations |
|---|---|---|---|
| N,N-diethyl-p-phenylenediamine | Chromogenic substrate for hydroperoxides | d-ROMs test for total oxidative stress | Reacts with alkoxyl/peroxyl radicals to form pink chromogen measured at 505nm [106] |
| Thiobarbituric acid (TBA) | Reacts with MDA to form fluorescent adduct | TBARS assay for lipid peroxidation | Heating at 95°C for 60 minutes required; specificity improved with HPLC separation [105] |
| 1-chloro-2,4-dinitrobenzene (CDNB) | Electrophilic substrate for GST | Glutathione S-transferase activity assay | Conjugation with GSH monitored at 340nm; requires GSH as co-substrate [105] |
| 5,5'-dithio-bis-(2-nitrobenzoic acid) (DTNB) | Thiol-reactive compound (Ellman's reagent) | Total sulfhydryl group quantification | Reacts with thiols to form yellow 5-thio-2-nitrobenzoic acid measured at 412nm [105] |
| Ferric chloride/thiocyanate derivative | Oxidant solution for antioxidant capacity | BAP test for total antioxidant potential | Serum antioxidants cause decolorization measured at 505nm [106] |
| 2,4-dinitrophenylhydrazine (DNPH) | Reacts with protein carbonyl groups | Protein carbonyl content assay | Forms hydrazone derivatives measured at 370nm; protein precipitation required pre-measurement [105] |
ROS Signaling Pathways: Molecular Mechanisms
Diagram 1: ROS Signaling Pathways and Cellular Consequences. This diagram illustrates the major pathways of reactive oxygen species generation from mitochondrial and enzymatic sources, their interconversion through enzymatic and chemical reactions, and their dual roles in cellular signaling and oxidative damage. Key nodes highlight specific ROS molecules and their cellular impacts, with color coding distinguishing different functional categories.
The molecular mechanisms of ROS signaling involve complex pathways that regulate cellular responses:
ROS Generation and Conversion: Superoxide anion (•Oâ‚‚â») serves as the primary ROS generated through mitochondrial electron transport and NADPH oxidase activity. Superoxide dismutase (SOD) converts •Oâ‚‚â» to hydrogen peroxide (Hâ‚‚Oâ‚‚), which functions as a key signaling molecule due to its relative stability and membrane permeability [1] [8]. In the presence of transition metal ions (particularly Fe²âº), Hâ‚‚Oâ‚‚ can undergo the Fenton reaction to generate the highly toxic hydroxyl radical (•OH), which causes significant biomolecular damage [1].
Redox Signaling Mechanisms: At physiological levels, Hâ‚‚Oâ‚‚ serves as a secondary messenger in redox signaling, primarily through oxidative post-translational modifications (Ox-PTMs) of cysteine residues in target proteins [8] [7]. These modifications include disulfide bond formation, S-glutathionylation, S-nitrosylation, and S-sulfenylation, which act as molecular switches that regulate protein function, localization, and interactions [7]. Specifically, S-glutathionylation represents a reversible post-translational modification that serves as a dynamic regulatory mechanism under oxidative stress conditions, enabling precise modulation of protein functions such as enzymatic activity, protein stability, and molecular interactions [7].
Transcriptional Regulation: ROS-induced redox signaling frequently regulates target gene expression through modification of transcription factors. Redox-sensitive transcription factors undergo oxidative modifications as a result of Hâ‚‚Oâ‚‚-mediated oxidation, further regulating the expression of target genes and thus enhancing cellular adaptation to stress conditions [7]. The NRF2 pathway represents the master regulator of antioxidant responses, activating the expression of antioxidative enzyme genes including NQO1, GPX4, TXN, and PRDX1 when activated under oxidative stress conditions [8].
Biomarker Validation Workflow
Diagram 2: Oxidative Stress Biomarker Validation Workflow. This diagram outlines the sequential stages in developing and validating oxidative stress biomarkers for clinical application, from initial selection based on pathway relevance through analytical validation to clinical implementation. The process emphasizes standardized protocols and statistical rigor throughout development.
The validation of oxidative stress biomarkers for patient stratification represents a promising frontier in precision medicine, particularly for conditions with heterogeneous clinical presentations and treatment responses. The strong correlations observed between specific oxidative stress markers and established clinical risk scores, combined with their potential for revealing underlying pathophysiological mechanisms, position these biomarkers as valuable tools for enhancing risk prediction and therapeutic targeting. Future directions should focus on standardizing measurement protocols across laboratories, establishing disease-specific reference ranges, and validating cut-off values for clinical decision-making in diverse patient populations. Furthermore, prospective studies examining the temporal dynamics of these biomarkers in response to therapeutic interventions will be essential for establishing their utility in guiding personalized treatment approaches across the spectrum of oxidative stress-related disorders.
The assessment of therapeutic efficacy across traditionally distinct disease classes represents a paradigm shift in modern drug development. This whitepaper examines the shared molecular underpinnings of cancer, cardiovascular, and neurodegenerative diseases, with a specific focus on reactive oxygen species (ROS) signaling mechanisms as a unifying element. By integrating quantitative data from disparate disease models and presenting standardized experimental protocols, we provide a framework for researchers to evaluate therapeutic interventions across disease boundaries. The identification of conserved pathways, particularly those regulated by redox balance, creates unprecedented opportunities for drug repurposing and the development of novel pan-therapeutic agents that target shared pathophysiological processes.
The traditional siloed approach to drug development has yielded diminishing returns, particularly for complex chronic diseases. Cross-disease efficacy assessment emerges as an innovative strategy that leverages shared pathophysiological mechanisms across different organ systems and disease classes [107]. Growing evidence indicates that cancer, cardiovascular diseases, and neurodegenerative disorders share convergent molecular processes despite their distinct clinical manifestations [107] [108]. These shared pathways include protein misfolding and aggregation, chronic inflammation, and critically, dysregulated ROS signaling [107] [1] [108].
ROS homeostasis—the dynamic equilibrium of reactive oxygen species within cells—serves as a critical regulator of cellular fate and function [1]. Under physiological conditions, ROS function as essential signaling molecules; however, when this balance is disrupted, it contributes to disease pathogenesis across multiple organ systems [1] [108] [8]. The dual nature of ROS presents both challenges and opportunities for therapeutic intervention: in cancer, elevated ROS contribute to genomic instability and tumor progression, while in neurodegenerative diseases, ROS accelerate neuronal death and impair cellular repair mechanisms [108]. Understanding these context-dependent roles of ROS is fundamental to cross-disease efficacy assessment.
Shared ROS Signaling Pathways
Core ROS Signaling Mechanisms
ROS encompass a collection of oxidative molecules with various biological functions, primarily including superoxide anion (•Oâ‚‚â»), hydrogen peroxide (Hâ‚‚Oâ‚‚), and hydroxyl radicals (•OH) [1]. These molecules regulate diverse aspects of cell fate through several conserved signaling pathways:
- NF-κB Pathway: A master regulator of inflammatory responses highly sensitive to redox changes [108]. In cancer stem cells (CSCs), constitutively active NF-κB promotes survival, immune evasion, and therapy resistance, while in neurodegenerative diseases, NF-κB activation by ROS contributes to neuroinflammation and neuronal damage [108].
- Nrf2-Keap1 Pathway: Central to cellular defense against oxidative and electrophilic insults [108] [8]. Nrf2 binds to the Antioxidant Response Element (ARE) to induce expression of antioxidant and detoxifying enzymes. This pathway is highly active in CSCs, maintaining redox homeostasis and therapy resistance, while reduced Nrf2 activity in Alzheimer's and Parkinson's diseases leads to oxidative damage [108].
- MAPK Pathway: Redox-sensitive and involved in cellular responses to oxidative stress [108]. ROS activates ERK, JNK, and p38 MAPK in CSCs, promoting self-renewal, survival, and proliferation, while in neurons, ROS-dependent activation of JNK and p38 MAPK is linked to neurodegeneration and apoptosis [108].
The following diagram illustrates the core ROS signaling pathways shared across cancer, cardiovascular, and neurodegenerative diseases:
Disease-Specific Modulation of Shared Pathways
While the core ROS signaling pathways are conserved across disease contexts, their functional outcomes differ based on cell type and disease environment. In cancer stem cells, the Nrf2 pathway is highly active, maintaining redox homeostasis and conferring therapy resistance through upregulation of antioxidant enzymes (GSH, SOD, CAT) and promotion of metabolic adaptation via the pentose phosphate pathway for NADPH production [108]. Conversely, in neurodegenerative diseases, Nrf2 activity declines with age and disease progression, leading to oxidative damage, mitochondrial dysfunction, and neuronal apoptosis [108].
The NF-κB pathway demonstrates similar duality: in CSCs, constitutive NF-κB activation promotes survival through anti-apoptotic gene expression, while in neurodegenerative conditions, chronic NF-κB activation in glial cells exacerbates oxidative stress and neurotoxicity through upregulation of pro-inflammatory cytokines like IL-6 [108]. This paradoxical role of shared pathways underscores the importance of context in cross-disease efficacy assessment and highlights the need for precise therapeutic modulation rather than blanket inhibition or activation.
Quantitative Data Analysis
Comparative ROS Levels and Biomarker Changes
The table below summarizes quantitative measurements of ROS parameters and associated biomarkers across the three disease categories, illustrating both shared and distinct patterns of redox dysregulation.
Table 1: Quantitative Comparison of ROS Parameters Across Disease Contexts
| Parameter | Cancer (CSCs) | Cardiovascular | Neurodegenerative |
|---|---|---|---|
| ROS Levels | Elevated (2-3x normal) [108] | Moderately elevated (1.5-2x normal) [1] | Variable elevation (1.5-3x normal) [108] |
| Primary ROS Source | Mitochondrial ETC, NOX4 [108] [8] | NOX2, XO, mitochondrial leakage [1] | Mitochondrial dysfunction, NOX2 [108] [109] |
| Key Transcription Factors | Nrf2 (↑), NF-κB (↑), HIF-1α (↑) [108] | NF-κB (↑), Nrf2 (↓ in chronic failure) [1] | Nrf2 (↓), NF-κB (↑), p53 (↑) [108] |
| Antioxidant Enzymes | SOD2 (↑), CAT (↑), GPX4 (↑) [108] | SOD1 (↓ in failure), GPX1 (variable) [1] | SOD1/2 (↓), CAT (↓), GPX4 (↓) [108] [109] |
| Oxidative Damage Markers | 8-OHdG (↑), Protein carbonylation (↑) [108] | MDA (↑), oxLDL (↑), Protein carbonylation (↑) [1] | 4-HNE (↑), Protein carbonylation (↑), 8-OHdG (↑) [108] [109] |
| Inflammatory Mediators | IL-6 (↑), TNF-α (↑), COX-2 (↑) [107] [108] | IL-6 (↑), TNF-α (↑), MCP-1 (↑) [1] | IL-1β (↑), IL-6 (↑), TNF-α (↑) [107] [108] |
Therapeutic Response Metrics
The assessment of cross-disease efficacy requires standardized metrics to evaluate therapeutic interventions. The following table provides quantitative benchmarks for evaluating ROS-targeting therapies across disease contexts.
Table 2: Therapeutic Efficacy Metrics for ROS-Targeting Interventions
| Efficacy Metric | Cancer Applications | Cardiovascular Applications | Neurodegenerative Applications |
|---|---|---|---|
| Biomarker Response | >50% reduction in 8-OHdG; >30% increase in GSH/GSSG ratio [108] | >40% reduction in oxLDL; >25% improvement in endothelial function [1] | >30% reduction in protein carbonylation; >20% reduction in lipid peroxidation [108] [109] |
| * Cellular Outcomes* | 20-40% increase in apoptosis of CSCs; >50% reduction in colony formation [108] | >30% reduction in cardiomyocyte apoptosis; >25% improvement in contractility [1] | >25% reduction in neuronal apoptosis; >30% improvement in mitochondrial function [108] [109] |
| Therapeutic Window | Narrow (differential toxicity challenging) [108] | Moderate (context-dependent optimization) [1] | Wide (but delivery challenges to CNS) [108] [109] |
| Treatment Duration for Efficacy | Days to weeks [108] | Weeks to months [1] | Months to years [108] |
| Optimal ROS Modulation | Moderate pro-oxidant shift to target CSCs [108] | Antioxidant support with mild redox signaling preservation [1] | Potent antioxidant support with Nrf2 activation [108] |
Experimental Protocols for Cross-Disease Assessment
Standardized ROS Measurement Protocol
Principle: Accurate quantification of intracellular ROS levels is fundamental to cross-disease efficacy assessment. The protocol below outlines a standardized approach applicable to cellular models from cancer, cardiovascular, and neurodegenerative contexts.
Reagents Required:
- Hâ‚‚DCFDA (2',7'-dichlorodihydrofluorescein diacetate) or CellROX reagents
- PBS (phosphate-buffered saline), calcium and magnesium-free
- Serum-free culture medium
- Antioxidants (e.g., N-acetylcysteine) for positive controls
- Pro-oxidants (e.g., menadione, Hâ‚‚Oâ‚‚) for standardization
- Lysis buffer for normalization (RIPA buffer or similar)
Procedure:
- Cell Preparation: Seed cells at optimized density (typically 1-5×10ⴠcells/well in 96-well plates) and culture for 24 hours to reach 70-80% confluence.
- Staining: Replace medium with serum-free medium containing 5-10 μM H₂DCFDA or recommended concentration of CellROX reagent. Incubate for 30-45 minutes at 37°C protected from light.
- Treatment: Apply test compounds in fresh medium for predetermined time points (typically 2-24 hours).
- Measurement: For fluorescence plate readers, measure fluorescence at Ex/Em 485/535 nm. For flow cytometry, analyze 10,000-50,000 events per sample using appropriate channels.
- Normalization: Normalize ROS measurements to protein content (using BCA assay on parallel wells) or cell number (using DNA content stains or cell counting).
- Controls: Include untreated controls, antioxidant-treated controls (e.g., 1-5 mM NAC), and pro-oxidant stimulated controls (e.g., 100-500 μM H₂O₂ for 30-60 minutes).
Validation Parameters:
- Linear range of detection: Establish using Hâ‚‚Oâ‚‚ standards
- Coefficient of variation: <15% for intra-assay variability
- Z'-factor: >0.5 for high-throughput screening applications
Protein Carbonylation Assessment
Principle: Protein carbonylation serves as a robust marker of irreversible oxidative damage across disease contexts. This protocol adapts the DNPH (2,4-dinitrophenylhydrazine) method for comparative assessment.
Reagents Required:
- DNPH solution (10 mM in 2M HCl)
- Neutralization solution (2M Tris in 30% glycerol)
- Primary antibody: anti-DNP (2,4-dinitrophenol)
- Secondary antibody: HRP-conjugated species-appropriate antibody
- ECL or similar chemiluminescent substrate
Procedure:
- Protein Extraction: Lyse cells in RIPA buffer with protease inhibitors. Centrifuge at 10,000×g for 10 minutes at 4°C.
- Derivatization: Incubate 10-20 μg protein with 0.2 volumes DNPH solution for 20 minutes at room temperature protected from light.
- Neutralization: Add 0.3 volumes neutralization solution.
- Detection: Separate proteins by SDS-PAGE, transfer to PVDF membrane, and detect carbonylated proteins using anti-DNP antibody (1:1000-1:5000 dilution).
- Quantification: Normalize to total protein loaded (using Ponceau S or similar total protein stain).
Cross-Disease Applications:
- Cancer: Assess in cancer stem cells vs. differentiated counterparts
- Cardiovascular: Evaluate in cardiomyocytes under oxidative stress
- Neurodegenerative: Measure in neuronal cultures and brain homogenates
The following diagram illustrates the experimental workflow for cross-disease ROS assessment:
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Cross-Disease ROS Studies
| Reagent Category | Specific Examples | Applications | Cross-Disease Utility |
|---|---|---|---|
| ROS Detection Probes | Hâ‚‚DCFDA, CellROX Green/Orange/Deep Red, MitoSOX Red, Amplex Red [1] [108] | General ROS, mitochondrial superoxide, Hâ‚‚Oâ‚‚ detection | High - standardized protocols across disease models |
| Oxidative Damage Kits | Protein Carbonylation ELISA, 8-OHdG ELISA/EIA, Lipid Hydroperoxide Assay, 4-HNE ELISA [108] | Quantification of oxidative damage to proteins, DNA, lipids | High - direct comparison of oxidative damage burden |
| Antioxidant Enzymes | SOD Activity Kit, Catalase Activity Kit, Glutathione Peroxidase Assay, Total Glutathione Kit [108] [8] | Assessment of antioxidant defense capacity | High - evaluation of compensatory antioxidant responses |
| Pathway Modulators | Nrf2 activators (sulforaphane, bardoxolone), NOX inhibitors (apocynin, GKT137831), NF-κB inhibitors (BAY11-7082) [108] [8] | Pathway-specific manipulation for mechanistic studies | Medium - context-specific effects require optimization |
| Redox-Sensitive Antibodies | Anti-nitrotyrosine, Anti-DNP (protein carbonylation), Anti-phospho-H2AX (DNA damage), Anti-Nrf2, Anti-HO-1 [108] [7] | Detection of oxidative modifications and pathway activation | High - standardized across disease models |
| Genetic Tools | Nrf2 siRNA/shRNA, NOX isoform expression vectors, ARE-luciferase reporters, CRISPR/Cas9 knockout cells [108] [8] | Genetic manipulation of redox pathways | Medium - requires optimization for different cell types |
Visualization of ROS Signaling Networks
The complex interplay between ROS sources, signaling pathways, and functional outcomes across diseases can be visualized as an integrated network. The following comprehensive diagram maps these relationships:
Cross-disease efficacy assessment represents a transformative approach to therapeutic development that leverages shared pathophysiological mechanisms rather than being constrained by traditional disease classification boundaries. The central role of ROS signaling across cancer, cardiovascular, and neurodegenerative diseases provides a compelling rationale for this approach, with conserved pathways offering promising targets for pan-therapeutic interventions. The quantitative frameworks and standardized methodologies presented in this whitepaper provide researchers with tools to systematically evaluate therapeutic efficacy across disease contexts.
Future advances in this field will require development of more sophisticated disease models that capture the complexity of human pathophysiology, enhanced computational methods for integrating multi-omics data across diseases, and innovative clinical trial designs that can efficiently evaluate efficacy across multiple disease indications. As our understanding of shared molecular mechanisms deepens, cross-disease efficacy assessment will increasingly guide strategic decisions in both drug repurposing and novel therapeutic development, ultimately accelerating the delivery of effective treatments to patients across diverse disease areas.
Conclusion
ROS signaling represents a complex, context-dependent network with profound implications for both physiological homeostasis and disease pathogenesis. The dual nature of ROS necessitates precise, targeted therapeutic approaches rather than broad antioxidant interventions. Future research must focus on developing context-specific modulators that account for spatial, temporal, and concentration-dependent ROS effects, alongside validated biomarkers for patient stratification. The integration of redox proteomics, structural biology, and advanced disease models will enable the next generation of ROS-targeted therapies, potentially revolutionizing treatment for cancer, neurodegenerative disorders, and age-related diseases where redox imbalance is a fundamental driver.
References
- 1. ROS homeostasis in cell fate, pathophysiology, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12572517/]
- 2. Reactive oxygen species [https://en.wikipedia.org/wiki/Reactive_oxygen_species]
- 3. ROS: Basic Concepts, Sources, Cellular Signaling, and its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9605829/]
- 4. ROS Function in Redox Signaling and Oxidative Stress - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4055301/]
- 5. Guidelines for measuring reactive oxygen species and ... [https://www.nature.com/articles/s42255-022-00591-z]
- 6. ROSBASE1.0: a comprehensive database of reactive oxygen ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12576790/]
- 7. ROS-induced oxidative post-translational modifications in ... [https://www.sciencedirect.com/science/article/abs/pii/S098194282501068X]
- 8. Redox regulation: mechanisms, biology and therapeutic ... [https://www.nature.com/articles/s41392-024-02095-6]
- 9. Mitochondrial electron transport chain, ROS generation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6559295/]
- 10. Mitochondrial electron transport chain, ROS generation ... [https://pubmed.ncbi.nlm.nih.gov/31115493/]
- 11. NADPH Oxidases (NOX): An Overview from Discovery, ... [https://pubmed.ncbi.nlm.nih.gov/34205998/]
- 12. Targeting ROS production through inhibition of NADPH ... [https://www.nature.com/articles/s41589-023-01457-5]
- 13. Endoplasmic Reticulum Stress and Associated ROS - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4813189/]
- 14. The aftermath of the interplay between the endoplasmic ... [https://www.nature.com/articles/s12276-021-00560-8]
- 15. A Quantitative Method to Monitor Reactive Oxygen Species ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4211297/]
- 16. Quantitative measurements of reactive oxygen species ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2024.1348395/full]
- 17. Exploring the Interplay of Antioxidants, Inflammation, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12469104/]
- 18. First line defence antioxidants-superoxide dismutase (SOD ... [https://www.sciencedirect.com/science/article/pii/S2090506817301550]
- 19. The Applications and Mechanisms of Superoxide Dismutase ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10525108/]
- 20. Dual-Target Insight into Drug Discovery from Natural ... [https://www.mdpi.com/2076-3921/14/11/1364]
- 21. Antioxidant Defense Systems in Plants: Mechanisms ... [https://www.mdpi.com/2075-1729/15/8/1293]
- 22. Induced Oxidative Stress and Inflammation via Nrf2/PINK1 ... [https://www.mdpi.com/2223-7747/14/12/1751]
- 23. Beyond Antioxidants: The Emerging Role of Nrf2 Activation in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12564927/]
- 24. An overview of mechanisms of redox signaling - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4048798/]
- 25. An emerging role for cysteine-mediated redox signaling in aging [https://pmc.ncbi.nlm.nih.gov/articles/PMC12433492/]
- 26. Cysteine thiol-based post-translational modification [https://www.sciencedirect.com/science/article/abs/pii/S1360138522003065]
- 27. The Basics of Thiols and Cysteines in Redox Biology and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4355186/]
- 28. An overview of mechanisms of redox signaling [https://www.sciencedirect.com/science/article/abs/pii/S0022282814000388]
- 29. Oxidative Cysteine Post Translational Modifications Drive ... [https://www.mdpi.com/2076-3921/13/8/883]
- 30. The Expanding Landscape of the Thiol Redox Proteome [https://www.sciencedirect.com/science/article/pii/S153594762033704X]
- 31. Signaling Functions of Reactive Oxygen Species - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4226395/]
- 32. Short Overview of ROS as Cell Function Regulators and Their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6721558/]
- 33. Reactive oxygen species function as signaling molecules ... [https://www.sciencedirect.com/science/article/abs/pii/S1369526622001224]
- 34. Reactive Oxygen Species Signaling and Oxidative Stress [https://pmc.ncbi.nlm.nih.gov/articles/PMC10967436/]
- 35. Physiological Signaling Functions of Reactive Oxygen ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2021.714370/full]
- 36. ROS-activated Michael acceptor prodrug strategy to enhance ... [https://pubs.rsc.org/en/content/articlehtml/2025/sc/d5sc03429a]
- 37. Reactive Oxygen Species Signaling and Oxidative Stress [https://www.mdpi.com/2076-3921/13/3/312]
- 38. Recent advances in electrochemical detection of reactive ... [https://pubs.rsc.org/en/content/articlelanding/2025/an/d4an01533a]
- 39. Nanotechnologies for Reactive Oxygen Species“Turn-On†... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8595313/]
- 40. Special Issue : Probes for Living Cell Detection - Biosensors [https://www.mdpi.com/journal/biosensors/special_issues/ZCOBU00301]
- 41. Reactive oxygen species (ROS): sources, generation ... [https://link.springer.com/article/10.1007/s44371-025-00275-z]
- 42. Revolution of Biotechnology with CRISPR [https://www.nature.com/articles/s12276-025-01452-x]
- 43. News: CMN Weekly (2 May 2025) [https://crisprmedicinenews.com/news/cmn-weekly-2-may-2025-your-weekly-crispr-medicine-news/]
- 44. CRISPR Clinical Trials: A 2025 Update [https://innovativegenomics.org/news/crispr-clinical-trials-2025/]
- 45. Combinatorial CRISPR-Cas9 metabolic screens reveal critical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5819357/]
- 46. A redox-based electrogenetic CRISPR system to connect ... [https://www.nature.com/articles/s41467-020-16249-x]
- 47. Hypoxia, oxidative stress, and the interplay of HIFs and ... [https://www.nature.com/articles/s12276-024-01180-8]
- 48. Understanding chronic inflammation: couplings between ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1558263/full]
- 49. Nrf2 signaling pathway: current status and potential ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10559910/]
- 50. Transcriptional Regulation by Nrf2 - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC6208165/]
- 51. Classification and regulatory interactions of key transcription ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12518327/]
- 52. Quantitative analysis of redox proteome reveals oxidation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9157258/]
- 53. Protein oxidation - Formation mechanisms, detection and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8113053/]
- 54. Quantitative proteomics identifies redox switches for global ... [https://www.nature.com/articles/s41467-017-02694-8]
- 55. Single-cell signaling network profiling during redox stress ... [https://www.nature.com/articles/s41467-025-60727-z]
- 56. An integrated high-throughput robotic platform and active ... [https://www.nature.com/articles/s41467-024-47070-5]
- 57. Accessing the High Throughput Screening Data Landscape [https://pmc.ncbi.nlm.nih.gov/articles/PMC5613246/]
- 58. The Redox Paradox: Cancer's Double-Edged Sword for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12561025/]
- 59. Reactive Oxygen Species: A Double-Edged Sword in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12346646/]
- 60. A guide to reactive oxygen species in tumour hypoxia [https://pmc.ncbi.nlm.nih.gov/articles/PMC12591319/]
- 61. Noninvasive in vivo discrimination between mitochondrial ... [https://www.sciencedirect.com/science/article/pii/S2213231725003842]
- 62. Oxidative stress in cancer: from tumor and ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02375-x]
- 63. NRF2 immunobiology in cancer: implications for ... [https://www.nature.com/articles/s41388-025-03560-4]
- 64. NRF2 activation in cancer and overview of NRF2 small ... [https://pubmed.ncbi.nlm.nih.gov/40815486/]
- 65. ZNF207-Driven PRDX1 Lactylation and NRF2 Activation in ... [https://www.sciencedirect.com/science/article/abs/pii/S1368764625000779]
- 66. Increased antioxidative defense and reduced advanced ... [https://www.nature.com/articles/s41467-025-60326-y]
- 67. NRF2 activation in cancer cells suppresses immune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12483591/]
- 68. Targeting metabolic vulnerabilities, oxidative stress, and ... [https://pubmed.ncbi.nlm.nih.gov/41177183/]
- 69. Reactive Oxygen Species: From Tumorigenesis to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12082284/]
- 70. ROS in cancer therapy: the bright side of the moon [https://www.nature.com/articles/s12276-020-0384-2]
- 71. Interplay of oxidative stress, cellular communication and ... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-023-01398-5]
- 72. NADPH homeostasis in cancer: functions, mechanisms ... [https://www.nature.com/articles/s41392-020-00326-0]
- 73. Reactive Oxygen Species: A Double-Edged Sword in the ... [https://www.mdpi.com/2073-4409/14/15/1207]
- 74. Regulation of anti-tumour effects of Paris polyphylla ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1611911/full]
- 75. NADPH Oxidase 4: A Potential Therapeutic Target of ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2022.884412/full]
- 76. NADPH Oxidases: A Perspective on Reactive Oxygen ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4026372/]
- 77. Inhibiting the Activity of NADPH Oxidase in Cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7370979/]
- 78. Inhibiting cancer metastasis via targeting NAPDH oxidase 4 [https://pubmed.ncbi.nlm.nih.gov/23688500/]
- 79. Oxidative cell death in cancer: mechanisms and ... [https://www.nature.com/articles/s41419-024-06939-5]
- 80. Harnessing Antioxidants in Cancer Therapy [https://www.mdpi.com/2076-3921/14/6/674]
- 81. Effects of antioxidants on cancer progression - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12339922/]
- 82. Therapeutic Strategies Targeting Oxidative Stress and ... [https://www.mdpi.com/2673-6411/5/4/35]
- 83. Redox-Directed Cancer Therapeutics: Molecular Mechanisms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2824519/]
- 84. The role of reactive oxygen species in the pathogenesis ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1662794/full]
- 85. Pharmacology and Clinical Drug Candidates in Redox ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4657508/]
- 86. Pharmacodynamic and Pharmacokinetic Aspects of Redox ... [https://www.frontiersin.org/research-topics/67857/pharmacodynamic-and-pharmacokinetic-aspects-of-redox-signaling-in-inflammation-associated-damage-and-diseasesundefined]
- 87. Targeting the redox-programmed cell death axis in breast ... [https://www.nature.com/articles/s41420-025-02743-y]
- 88. Redox-Responsive π-Conjugated Prodrug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12473931/]
- 89. Mannose directed nanoparticle delivery systems ... [https://www.sciencedirect.com/science/article/abs/pii/S1773224725006860]
- 90. Antioxidants and Reactive Oxygen Species [https://www.mdpi.com/1422-0067/26/15/7520]
- 91. Free radicals and their impact on health and antioxidant ... [https://www.nature.com/articles/s41420-024-02278-8]
- 92. The crosstalk between copper-induced oxidative stress ... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-024-01726-3]
- 93. The crosstalk between oxidative stress and DNA damage ... [https://pubmed.ncbi.nlm.nih.gov/39047850/]
- 94. The crosstalk between oxidative stress and DNA damage ... [https://www.sciencedirect.com/science/article/pii/S0891584924005665]
- 95. Identifying and validating novel targets with in vivo disease ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644607001481]
- 96. The Importance of Murine Models in Determining In Vivo ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11944934/]
- 97. Genetically Engineered Models (GEMs) for Preclinical ... [https://www.taconic.com/products/mouse-rat/gems]
- 98. Patient-derived xenograft models in cancer therapy [https://www.nature.com/articles/s41392-023-01419-2]
- 99. Shining a Spotlight on Promising Clinical Trials in 2025 - Susan G. Komen® [https://www.komen.org/blog/spotlight-on-2025-clinical-trials/]
- 100. 5 emerging cancer therapies presented at ASCO 2025 | MD Anderson Cancer Center [https://www.mdanderson.org/cancerwise/5-emerging-therapies-presented-at-asco-2025.h00-159776445.html]
- 101. 2025 NIH Alzheimer's Disease and Related Dementias ... [https://www.nia.nih.gov/about/2025-nih-dementia-research-progress-report]
- 102. UCSD Neurodegenerative Disease Clinical Trials for 2025 [https://clinicaltrials.ucsd.edu/neurodegenerative-disease]
- 103. Neurodegenerative diseases - Improving clinical trial ... [https://neurotorium.org/next-steps-for-improving-clinical-trial-outcomes-neurodegenerative-disease/]
- 104. Meet the Next Generation of Brain Disease Research [https://www.americanbrainfoundation.org/meet-the-researchers-2025/]
- 105. Associations of oxidative stress biomarkers with SYNTAX ... [https://pubmed.ncbi.nlm.nih.gov/40988253/]
- 106. Clinical Evaluation of Oxidative Stress Markers in Patients ... [https://www.mdpi.com/2076-3921/14/9/1068]
- 107. molecular links of neurodegenerative diseases with cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12532377/]
- 108. Oxidative Stress and Redox Imbalance - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC11988017/]
- 109. Oxidative stress and inflammation in the pathogenesis of ... [https://www.sciencedirect.com/science/article/pii/S2211383524004040]