Redox Signaling in Inflammation and Disease: Molecular Mechanisms, Therapeutic Targeting, and Clinical Translation
This article provides a comprehensive analysis of redox signaling's dual role in physiological homeostasis and the pathogenesis of chronic diseases.
Redox Signaling in Inflammation and Disease: Molecular Mechanisms, Therapeutic Targeting, and Clinical Translation
Abstract
This article provides a comprehensive analysis of redox signaling's dual role in physiological homeostasis and the pathogenesis of chronic diseases. It explores the molecular foundations of redox imbalance, detailing how oxidative and reductive stress regulate immune responses, inflammatory pathways, and contribute to neurological, cardiovascular, and metabolic disorders. For researchers and drug development professionals, we examine cutting-edge methodological approaches for targeting redox-sensitive pathways, troubleshoot past failures of antioxidant therapies, and validate emerging biomarkers and Nrf2-focused strategies through comparative analysis of preclinical and clinical data. The synthesis offers a roadmap for developing precision medicine interventions that restore redox balance in inflammatory diseases.
The Molecular Landscape of Redox Signaling in Immune Regulation and Inflammation
Redox homeostasis, the delicate equilibrium between oxidative and reductive processes within biological systems, serves as a fundamental regulator of cellular function and signaling. While oxidative stress has been extensively studied for decades, emerging research reveals that reductive stress (RS)—the pathological overabundance of reducing equivalents—represents an equally critical disruption of redox balance with profound implications for inflammatory diseases and metabolic disorders. This technical review examines the molecular mechanisms governing redox homeostasis, detailing how bidirectional deviations contribute to disease pathogenesis through dysregulated immune responses, mitochondrial dysfunction, and impaired cellular signaling. We provide comprehensive experimental frameworks and quantitative assessments to equip researchers with methodologies for investigating both oxidative and reductive stress, emphasizing their interplay in chronic inflammation. The synthesized data and protocols presented herein aim to facilitate advanced research and therapeutic development targeting redox-based pathways in human disease.
Redox biology encompasses the complex network of reduction-oxidation reactions that underlie fundamental cellular processes, from energy metabolism to signal transduction. The term "redox" originates from the combination of "reduction" and "oxidation," describing chemical processes involving electron transfer between reactants [1]. Redox homeostasis represents the maintenance of optimal nucleophilic tone through continuous signaling for the production and elimination of electrophiles and nucleophiles [2]. This dynamic balance is not a static state but rather a continuously regulated process essential for healthy physiological functioning.
The clinical significance of redox homeostasis extends across numerous disease states. In cardiovascular diseases, dysregulated redox signaling facilitates persistent reactive oxygen species (ROS) generation that drives pathological feedback loops, contributing to an estimated increase in global cardiovascular deaths from 20.5 million in 2025 to approximately 35.6 million by 2050 [3]. Similarly, in chronic inflammatory conditions, redox imbalance creates a synergistic pathogenic loop that sustains inflammation through continuous activation of immune cells and pro-inflammatory signaling pathways [4]. The field of Quantitative Redox Biology has emerged to address the need for absolute quantitative information on all redox-active compounds, thermodynamic parameters, and kinetic data necessary to model these complex biological systems [5].
Traditional research has predominantly focused on oxidative stress, characterized by excessive reactive oxygen species (ROS) and reactive nitrogen species (RNS) that overwhelm antioxidant defenses. However, robust evidence now highlights that reductive stress—the pathological shift toward an excessively reduced cellular state—plays an equally critical role in disease pathogenesis, particularly in metabolic and cardiovascular disorders [6] [7]. This review examines both extremes of the redox spectrum, their interconnected roles in inflammatory pathways, and the experimental approaches essential for their investigation.
Fundamental Concepts and Definitions
The Redox Spectrum: From Oxidative to Reductive Stress
The redox state of a cell exists on a spectrum, with oxidative stress and reductive stress representing opposing pathological extremes that disrupt normal physiological signaling:
Oxidative Stress (OS): A state characterized by an overproduction of reactive oxygen species (ROS) and reactive nitrogen species (RNS) that overwhelms antioxidant defenses, leading to potential damage to cellular components such as lipids, proteins, and DNA [4]. ROS include superoxide anions (O₂•â»), hydrogen peroxide (Hâ‚‚Oâ‚‚), and hydroxyl radicals (•OH), while RNS encompass nitric oxide (NO•) and peroxynitrite (ONOOâ») [4] [3].
Reductive Stress (RS): "A shift in the cellular redox balance towards a more reduced state, characterized by an excess of endogenous reductants (such as NADH, NADPH, and GSH) over their oxidized counterparts (NAD+, NADP+, and GSSG)" [7]. This excessively reduced state disrupts normal redox signaling, impairs mitochondrial function, and triggers endoplasmic reticulum stress [6].
Redox Homeostasis: The maintenance of nucleophilic tone through continuous feedback mechanisms that preserve the balance between oxidants and nucleophiles, representing the optimal physiological steady state for cellular function [2].
Quantitative Redox Principles
The field of Quantitative Redox Biology emphasizes precise measurement of redox parameters to enable accurate comparison across experimental systems. A fundamental quantitative relationship is described by the Nernst equation for the GSSG/2GSH couple, the major cellular redox buffer:
Where Eₕc represents the half-cell reduction potential. This equation demonstrates why absolute concentrations matter—a cell with 10 mM GSH requires a [GSH]/[GSSG] ratio of only 16.6 to achieve an Eₕc of -228 mV, while a cell with 1 mM GSH requires a ratio of 166 to achieve the same potential [5]. This quantitative approach reveals that the biological state of cells (proliferation, quiescence, differentiation, or cell death) correlates with specific redox environments, with proliferating cells exhibiting a more reduced state than differentiated cells [5].
Table 1: Characteristic Redox Environments Across Biological States
| Biological State | GSH/GSSG Ratio | Reduction Potential (Eâ‚•c) | Cellular Conditions |
|---|---|---|---|
| Proliferation | High (≥166:1 in low GSH cells) | More reduced (-228 mV or lower) | Associated with superoxide signaling |
| Quiescence | Moderate | Intermediate (-228 to -200 mV) | Associated with hydrogen peroxide signaling |
| Differentiation | Lower than proliferating state | More oxidized | Stable functional state |
| Apoptosis | Significantly decreased | Oxidized (-180 to -150 mV) | Initiates programmed cell death |
| Necrosis | Drastically decreased | Highly oxidized | Results from severe oxidation |
Molecular Mechanisms of Redox Imbalance
Oxidative Stress in Inflammation
Oxidative stress represents a key pathogenic element in the pathophysiology of chronic inflammatory diseases, establishing a synergistic relationship that creates a pathogenic loop sustaining chronic inflammation [4]. This dynamic has been extensively documented in atherosclerosis, neurodegeneration, non-alcoholic steatohepatitis, inflammatory bowel diseases, and rheumatoid arthritis [4].
The molecular mechanisms through which OS drives inflammation include:
NF-κB Activation: ROS activate IκB kinase (IKK), leading to phosphorylation and proteasomal degradation of IκB proteins, which frees NF-κB to translocate to the nucleus and promote transcription of pro-inflammatory genes encoding cytokines, adhesion molecules, and enzymes like COX-2 and iNOS [4].
MAPK Pathway Activation: ROS inhibit MAPK phosphatases by oxidizing their catalytic cysteine residues, thereby prolonging MAPK signaling, particularly the p38 MAPK branch, which stabilizes mRNAs of inflammatory mediators and modulates chromatin accessibility [4].
Inflammasome Activation: ROS are essential for activating the NOD-like receptor family pyrin domain containing 3 (NLRP3) inflammasome, a multiprotein complex responsible for cleaving pro-caspase-1 into its active form, which subsequently activates interleukin (IL)-1β and IL-18, key cytokines in inflammatory propagation [4].
The major cellular sources of ROS include mitochondrial complexes I and III of the electron transport chain, NADPH oxidases (NOX1-5, DUOX1/2), uncoupled nitric oxide synthase (NOS) isoforms, xanthine oxidase, and enzymes involved in endoplasmic reticulum oxidative protein folding [4] [3].
Reductive Stress in Metabolic and Inflammatory Disorders
Reductive stress has emerged as a critical pathway in metabolic disorders induced by overnutrition, with significant implications for cardiovascular health [6] [7]. The pathological mechanisms of RS include:
Mitochondrial Dysfunction: Excessive NADH accumulation disrupts mitochondrial function by impairing the electron transport chain, leading to decreased ATP production and paradoxically increased production of reactive oxygen species [7].
Endoplasmic Reticulum Stress: An excess of reductive equivalents in the ER hampers proper protein folding by disrupting disulfide bond formation, triggering the unfolded protein response (UPR), which can lead to insulin resistance and compromised cellular homeostasis [7].
Paradoxical Pro-inflammatory Effects: While traditionally viewed as opposing oxidative stress, chronic reductive stress can paradoxically sustain inflammatory responses by altering redox-sensitive signaling pathways, including modulation of NF-κB activity, thereby contributing to disease progression in autoimmune, cardiovascular, and neuroinflammatory disorders [4].
Antioxidant Exacerbation: Excessive antioxidant supplementation can further shift the redox balance toward reductive stress, potentially undermining the beneficial effects of exercise, impairing cardiovascular health, and aggravating metabolic disorders, particularly in obese individuals [7].
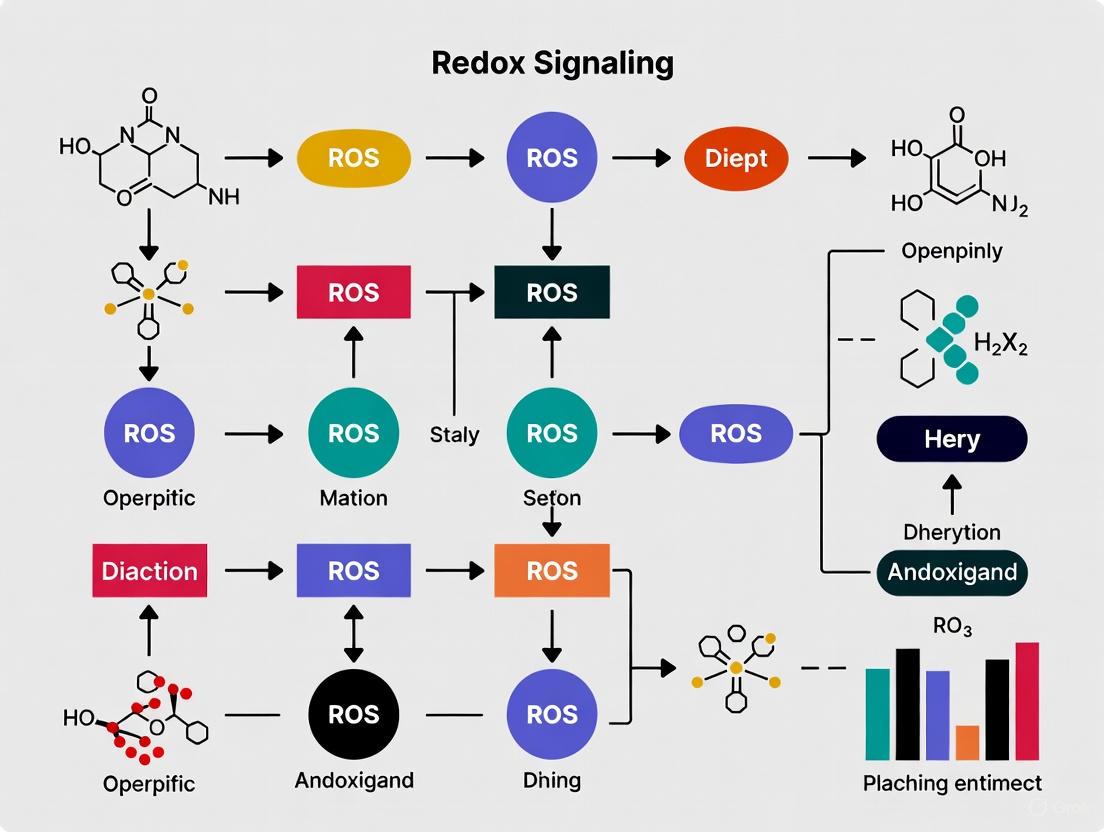
The following diagram illustrates the key signaling pathways and pathological consequences of both oxidative and reductive stress:
Figure 1: Signaling Pathways in Oxidative and Reductive Stress
Experimental Approaches and Assessment Methodologies
Quantitative Assessment of Redox States
Accurate measurement of redox parameters requires standardized quantitative approaches. The following methodologies provide comprehensive assessment of redox status:
Glutathione Homeostasis Quantification:
- Sample Preparation: Deproteinize cell lysates or tissue homogenates using metaphosphoric acid or perchloric acid
- GSH Measurement: Derivatize with monobromobimane followed by HPLC separation with fluorescence detection
- GSSG Measurement: Mask GSH with 2-vinylpyridine before derivatization and HPLC analysis
- Calculation: Apply Nernst equation to determine reduction potential (Eâ‚•c) using absolute concentrations [5]
NAD(H) and NADP(H) Redox Couples:
- Enzyme Cycling Assays: Utilize specific dehydrogenases coupled to colorimetric or fluorescent reporters
- Separation Methods: HPLC or LC-MS for direct quantification of oxidized and reduced forms
- Critical Ratios: Calculate NADH/NAD+ and NADPH/NADP+ ratios as indicators of reductive stress [6] [7]
Redox-Sensitive GFP (roGFP) Imaging:
- Genetically encoded sensors targeted to specific cellular compartments
- Ratiometric fluorescence measurements for quantitative assessment
- Real-time monitoring of redox dynamics in living cells [5]
Table 2: Comprehensive Redox Assessment Parameters and Methodologies
| Parameter | Methodology | Physiological Range | Pathological Indicators |
|---|---|---|---|
| GSH/GSSG Ratio | HPLC with fluorescence detection | 166:1 (in 1 mM GSH cells) for Eâ‚•c -228 mV | Decreased in OS (<100:1); Increased in RS (>300:1) |
| NADH/NAD+ Ratio | Enzyme cycling assays or LC-MS | Varies by compartment | >0.01 in cytoplasm indicates RS |
| NADPH/NADP+ Ratio | Enzyme cycling assays or LC-MS | ~100:1 in cytoplasm | Significant elevation in RS |
| Hâ‚‚Oâ‚‚ Steady-State | roGFP or HyPer probes | 1-10 nM in cytoplasm | Elevated in OS (>100 nM) |
| Protein Sulfenylation | Dimedone-based probes | Baseline tissue-specific modifications | Widespread increase in OS |
| Mitochondrial Membrane Potential | TMRM or JC-1 staining | Cell type dependent | Hyperpolarization in RS |
Induction Models for Redox Studies
Experimental Models of Reductive Stress:
- Pharmacological Induction: Treatment with compounds like sulforaphane or glutathione ethyl ester (GEE) to boost cellular reducing capacity [6]
- Genetic Models: Expression of human R120G mutant αB-crystallin (hR120G cryAB) known to induce reductive stress [6]
- Metabolic Loading: High-glucose conditions or fatty acid oversupply to increase reducing equivalent generation [7]
Experimental Models of Oxidative Stress:
- Pharmacological Induction: Treatment with paraquat, menadione, or buthionine sulfoximine (BSO) [1]
- Genetic Models: Knockdown of antioxidant enzymes (SOD, GPx, catalase) [5]
- Physiological Stimuli: Hypoxia-reoxygenation, cytokine stimulation, or NOX activation [4]
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Redox Biology Investigations
| Reagent/Category | Specific Examples | Research Application | Mechanistic Basis |
|---|---|---|---|
| ROS Inducers | Paraquat, Menadione, BSO | Experimental OS models | Generate superoxide or deplete GSH |
| RS Inducers | GSH ethyl ester (GEE), NAC, Sulforaphane | Experimental RS models | Boost cellular reducing capacity |
| NADH Modulators | NR (Nicotinamide riboside) | Manipulate NADH/NAD+ ratio | Precursor for NAD+ biosynthesis |
| Mitochondrial Probes | TMRM, JC-1, MitoSOX | Assess membrane potential and mtROS | Potential-sensitive distribution |
| Genetic Tools | shRNA against SOD, NOX isoforms, roGFP constructs | Targeted pathway manipulation | Specific pathway modulation |
| Redox Biosensors | roGFP, HyPer, Grx1-roGFP | Quantitative live-cell imaging | Ratiometric redox measurement |
| Thiol Status Assays | Monobromobimane, DTNB | Quantify thiol oxidation | Thiol-reactive compounds |
| Antioxidant Enzymes | Recombinant SOD, CAT, GPx | Supplemental antioxidant defense | Scavenge specific ROS |
| 1,2-O-Cyclohexylidene-myo-inositol | 1,2-O-Cyclohexylidene-myo-inositol, MF:C12H20O6, MW:260.28 g/mol | Chemical Reagent | Bench Chemicals |
| 2-Fluorophenylboronic acid | 2-Fluorophenylboronic Acid | High Purity RUO | 2-Fluorophenylboronic acid for Suzuki cross-coupling. High purity, for research use only (RUO). Not for human or veterinary use. | Bench Chemicals |
Research Gaps and Future Directions
The emerging recognition of reductive stress as a significant pathological state has revealed several critical research gaps that warrant investigation:
Threshold Determination: Precise quantitative thresholds for pathological reductive stress across different tissue types and disease states remain undefined [4] [5].
Dual-Role Proteins: The context-dependent functions of factors like Nrf2, which can exhibit both protective and potentially detrimental effects depending on the duration and intensity of activation, require clarification [4] [1].
Spatiotemporal Dynamics: Advanced technologies are needed to resolve redox dynamics with high spatial and temporal resolution to understand compartment-specific redox regulation [3] [5].
Antioxidant Therapy Refinement: The paradoxical effects of antioxidant interventions, which may exacerbate reductive stress in certain contexts, necessitate the development of more precise, targeted approaches that consider the bidirectional nature of redox dysregulation [4] [7] [1].
Future research should prioritize the development of disease-specific redox profiling and biomarker panels that can distinguish between oxidative and reductive stress components in clinical samples, enabling personalized redox-based therapeutics.
Redox homeostasis represents a critical determinant of cellular health, with both oxidative and reductive stress contributing significantly to inflammatory pathogenesis and metabolic disorders. The traditional antioxidant-centric view of redox balance requires expansion to incorporate the emerging understanding of reductive stress as a distinct pathological entity. Comprehensive investigation of redox processes demands rigorous quantitative approaches, precise compartment-specific assessment, and integrated analysis of the interconnected networks that maintain redox equilibrium. The experimental frameworks and methodological tools presented in this review provide a foundation for advancing research in redox biology, with particular relevance for understanding inflammatory disease mechanisms and developing targeted therapeutic interventions that restore redox homeostasis without inducing pathological extremes in either direction.
Redox signaling represents a fundamental regulatory mechanism in cellular biology, governing processes from metabolism to gene expression. The term "redox" originates from "reduction" and "oxidation," describing chemical processes involving electron transfer between reactants [1]. Within physiological systems, reactive oxygen species (ROS), reactive nitrogen species (RNS), and reactive sulfur species (RSS) function as crucial signaling mediators, maintaining cellular homeostasis at low concentrations but driving pathological processes when dysregulated [8] [3] [1]. The delicate balance between oxidative and reductive forces constitutes redox homeostasis, where disruption—termed oxidative stress or reductive stress—forms a common pathway in the pathogenesis of diverse inflammatory, cardiovascular, neurodegenerative, and metabolic diseases [4] [1]. This review comprehensively examines the dual nature of key reactive species, their signaling mechanisms, measurement methodologies, and therapeutic targeting within inflammation and disease research contexts.
Classification and Properties of Key Reactive Species
Reactive Oxygen Species (ROS)
ROS are oxygen-containing molecules characterized by highly reactive unpaired electrons [9]. They are broadly categorized into radical and non-radical species, generated endogenously as metabolic byproducts and exogenously from environmental exposures [10] [9].
Table 1: Major Reactive Oxygen Species (ROS)
| Category | Species | Chemical Formula | Reactivity | Primary Sources |
|---|---|---|---|---|
| Radical ROS | Superoxide anion | O₂•⻠| Moderate | Mitochondrial ETC, NADPH oxidases |
| Hydroxyl radical | •OH | Very high | Fenton reaction | |
| Alkoxyl radical | RO• | High | Lipid peroxidation | |
| Peroxyl radical | ROO• | High | Lipid peroxidation | |
| Non-radical ROS | Hydrogen peroxide | Hâ‚‚Oâ‚‚ | Moderate | Superoxide dismutation |
| Singlet oxygen | ¹O₂ | High | Photosensitization reactions | |
| Hypochlorous acid | HOCl | High | Myeloperoxidase activity | |
| Ozone | O₃ | High | Exogenous source |
Reactive Nitrogen Species (RNS)
RNS are nitrogen-containing radicals and non-radicals derived primarily from nitric oxide (NO•) and its reaction products [3] [9]. Nitric oxide, synthesized by nitric oxide synthases (NOS), plays vital roles in vascular regulation, neurotransmission, and immune responses [9].
Table 2: Major Reactive Nitrogen Species (RNS)
| Category | Species | Chemical Formula | Reactivity | Primary Sources |
|---|---|---|---|---|
| Free Radical RNS | Nitric oxide | NO• | Moderate | NOS enzymes |
| Nitrogen dioxide | NO₂• | High | Peroxynitrite decomposition | |
| Non-radical RNS | Peroxynitrite | ONOO⻠| Very high | NO• + O₂•⻠reaction |
| Nitrous acid | HNOâ‚‚ | Moderate | Acidification of nitrite | |
| Nitroxyl anion | NOâ» | Moderate | NO metabolism | |
| Dinitrogen trioxide | N₂O₃ | High | NO• + NO₂• reaction |
Reactive Sulfur Species (RSS)
RSS represent a rapidly emerging class of redox regulators, with hydrogen sulfide (Hâ‚‚S) serving as a key signaling molecule [3]. RSS participate in protein post-translational modifications, particularly S-sulfhydration, which regulates numerous cellular processes including metabolism, mitochondrial function, vasodilation, and inflammatory responses [3]. The Hâ‚‚S donor, S-propyl-L-cysteine, demonstrates cardioprotective effects by improving mitochondrial dysfunction via S-sulfhydration of Ca²âº/calmodulin-dependent protein kinase II in heart failure models [3].
Compartmentalization of Reactive Species Production
Reactive species generation exhibits distinct subcellular compartmentalization, with specific organelles contributing differentially to the cellular redox landscape [8]. Mitochondria constitute the primary source of endogenous ROS, accounting for approximately 90% of cellular ROS production during oxidative phosphorylation [8]. Complexes I and III of the electron transport chain represent major sites of superoxide generation [3]. Additional significant sources include NADPH oxidases (NOX family enzymes) dedicated to regulated ROS production [8] [11], endoplasmic reticulum oxidative protein folding [4], peroxisomal fatty acid oxidation [8], and cytoplasmic enzymatic reactions involving xanthine oxidase and cytochrome P450 systems [8] [9].
Enzymatic Systems for Reactive Species Generation
The NADPH oxidase (NOX) family comprises seven homologs (NOX1-5, DUOX1/2) that catalyze superoxide production by transferring electrons from NADPH to molecular oxygen [3] [11]. These enzymes differ in tissue distribution, activation mechanisms, and biological functions, with NOX2 originally identified in phagocytes for microbial killing [11]. Nitric oxide synthases (NOS) generate NO• through oxidation of L-arginine, with three isoforms mediating neuronal signaling (nNOS), vascular regulation (eNOS), and inflammatory responses (iNOS) [9]. Xanthine oxidase produces superoxide during purine metabolism [4], while mitochondrial electron transport chain complexes generate ROS as byproducts of aerobic respiration [8] [3].
Diagram 1: Cellular Sources of Reactive Species. ROS are generated through multiple cellular compartments including mitochondrial electron transport, NADPH oxidase enzymes, endoplasmic reticulum protein folding, and peroxisomal metabolism.
Molecular Targets and Signaling Pathways
Redox-Sensitive Signaling Cascades
Reactive species function as signaling mediators through reversible oxidation of critical cysteine residues in target proteins, altering their structure, activity, and interaction networks [1]. Major redox-sensitive pathways include:
The NF-κB pathway represents a primary inflammatory signaling cascade regulated by ROS [4]. Under basal conditions, NF-κB dimers remain sequestered in the cytoplasm by inhibitory IκB proteins. ROS activate IκB kinase (IKK), leading to IκB phosphorylation and degradation, thereby releasing NF-κB for nuclear translocation and pro-inflammatory gene transcription [4]. Additionally, ROS inhibit MAPK phosphatases by oxidizing catalytic cysteine residues, prolonging MAPK signaling including JNK, p38, and ERK pathways that regulate inflammation, stress responses, and cell survival [4].
The Nrf2/KEAP1 axis constitutes a central antioxidant response system [4] [1]. Under homeostatic conditions, Nrf2 remains bound to KEAP1, targeting it for ubiquitination and degradation. Oxidative modification of critical cysteine residues on KEAP1 enables Nrf2 stabilization and nuclear translocation, where it induces expression of cytoprotective genes including heme oxygenase-1 (HO-1), NAD(P)H quinone dehydrogenase 1 (NQO1), and glutamate-cysteine ligase catalytic subunit (GCLC) [4].
Hypoxia-inducible factor-1α (HIF-1α) represents another redox-sensitive transcription factor that coordinates cellular adaptation to low oxygen tension [8] [4]. ROS stabilize HIF-1α by inhibiting prolyl hydroxylase domain-containing proteins (PHDs), enabling its dimerization with HIF-1β and transcription of genes promoting angiogenesis, metabolic adaptation, and cell survival [8].
Diagram 2: Redox-Sensitive Signaling Pathways. ROS activate multiple signaling cascades including NF-κB (inflammatory genes), Nrf2 (antioxidant genes), and MAPK (cell growth/differentiation genes).
Biomolecular Damage and Pathological Consequences
At elevated concentrations, reactive species inflict macromolecular damage through irreversible oxidation, contributing to cellular dysfunction and disease pathogenesis [12] [9]. Lipid peroxidation represents a particularly destructive process wherein ROS attack polyunsaturated fatty acids in cell membranes, initiating chain reactions that generate reactive aldehydes including malondialdehyde (MDA) and 4-hydroxynonenal (4-HNE) [9]. These products form adducts with proteins and DNA, impairing their function and propagating oxidative damage [9]. Protein oxidation modifies amino acid side chains (particularly cysteine and methionine), forms protein-protein crosslinks, and fragments peptide chains, leading to loss of enzymatic activity, disrupted signaling, and structural protein degradation [13] [9]. DNA damage includes base modifications (e.g., 8-hydroxy-2'-deoxyguanosine), strand breaks, and crosslinking, resulting in mutations, genomic instability, and aberrant gene expression [9].
Table 3: Biomarkers of Oxidative Stress and Damage
| Target | Biomarker | Detection Methods | Significance |
|---|---|---|---|
| Lipids | Malondialdehyde (MDA) | TBARS assay, HPLC, GC-MS | Lipid peroxidation end product |
| 4-Hydroxynonenal (4-HNE) | HPLC, GC-MS/MS, immunoassays | Reactive aldehyde, protein adduct formation | |
| Fâ‚‚-isoprostanes | GC-MS, LC-MS, immunoassays | Gold standard for lipid peroxidation | |
| Proteins | Protein carbonyls | HPLC, immunoassays, Western blot | Protein oxidation marker |
| 3-Nitrotyrosine | LC/GC with various detectors, immunoassays | Protein nitration marker | |
| Advanced Oxidation Protein Products (AOPP) | Colorimetric assays, GC-MS | Protein damage in inflammatory diseases | |
| DNA | 8-OHdG | HPLC-EC, LC-MS, GC-MS, immunoassays | Oxidative DNA damage marker |
| 5-Hydroxymethyluracil | GC-MS | DNA oxidation product | |
| Overall Status | Total Antioxidant Capacity | Various colorimetric assays | Integrated antioxidant defense assessment |
Physiological Roles in Cellular Signaling
At low, physiological concentrations, reactive species function as crucial signaling mediators in numerous cellular processes [8]. ROS regulate cell proliferation and differentiation through reversible oxidation of protein tyrosine phosphatases and receptor tyrosine kinases, modulating growth factor signaling cascades [8]. The MAPK/ERK, PTK/PTP, and PI3K-AKT-mTOR pathways represent key redox-sensitive signaling networks controlling cell growth, survival, and metabolism [8]. In the immune system, ROS production by NADPH oxidase (NOX2) in phagocytes enables microbial killing through the respiratory burst, while simultaneously regulating immune cell activation and inflammatory responses [4] [11]. Reactive species also mediate apoptotic signaling, with mitochondrial ROS participating in intrinsic pathway activation and caspase regulation [14]. Vascular tone regulation involves NO•-mediated vasodilation and ROS modulation of endothelial signaling, while neuronal communication utilizes NO• as a neurotransmitter and ROS in synaptic plasticity [3] [9].
Pathological Implications in Disease
Oxidative Stress in Chronic Inflammation
Oxidative stress and chronic inflammation form a self-perpetuating cycle that drives disease pathogenesis across multiple organ systems [4] [11]. In cardiovascular diseases, ROS contribute to endothelial dysfunction, leukocyte recruitment, foam cell formation, and vascular remodeling in atherosclerosis [3] [11]. Myocardial infarction and heart failure involve ROS-mediated mitochondrial dysfunction, impaired contractility, and adverse remodeling [3]. Neurodegenerative disorders including Alzheimer's and Parkinson's diseases feature oxidative damage to neurons, protein misfolding, and mitochondrial dysfunction that promote neuronal loss [13] [9]. Respiratory diseases such as COPD, asthma, and ARDS involve oxidative injury to lung epithelium, barrier dysfunction, and persistent inflammation [8] [13]. Autoimmune and metabolic disorders including rheumatoid arthritis, inflammatory bowel disease, and diabetes mellitus demonstrate sustained ROS production that amplifies tissue damage and dysfunction [8] [4].
The Emerging Concept of Reductive Stress
Recent evidence indicates that not only oxidative stress but also reductive stress (RS)—characterized by excessive reducing equivalents including NADH, NADPH, and reduced glutathione (GSH)—can disrupt redox homeostasis and contribute to disease [4]. RS arises from overactive antioxidant systems or metabolic alterations that increase reducing capacity, potentially impairing disulfide bond formation, altering redox-sensitive signaling, and compromising mitochondrial function [4]. Chronic reductive stress associates with certain cardiomyopathies, neurodegenerative disorders, and metabolic syndromes, demonstrating the importance of balanced redox regulation rather than simply maximizing antioxidant capacity [4].
Methodologies for Detection and Measurement
Experimental Approaches for Reactive Species Detection
Accurate measurement of reactive species and oxidative damage presents methodological challenges due to their reactivity, short half-lives, and low physiological concentrations [12]. Direct detection approaches include electron spin resonance (ESR) spectroscopy for free radical identification and quantification, while fluorescent probes (e.g., DCFH-DA, DHE) enable cellular imaging of ROS with spatial and temporal resolution [12]. Chemiluminescence-based assays utilizing luminol or lucigenin provide sensitive detection of extracellular ROS production, particularly in immune cells [11]. Indirect assessment through oxidative damage biomarkers offers more stable analytical targets, with mass spectrometry-based methods (GC-MS, LC-MS/MS) providing gold-standard quantification of isoprostanes, 8-OHdG, and protein carbonyls [12]. Immunoassays enable high-throughput measurement of various oxidative stress markers in clinical and research settings [12].
Table 4: Research Reagent Solutions for Redox Biology
| Reagent Category | Specific Examples | Function/Application | Key Features |
|---|---|---|---|
| Fluorescent Probes | DCFH-DA, DHE, MitoSOX | Cellular ROS detection | Site-specific (mitochondrial), redox-sensitive fluorescence |
| Chemical Scavengers | N-acetylcysteine, Tempol | Direct ROS quenching | Membrane-permeable antioxidants |
| Enzyme Inhibitors | Apocynin, VAS2870 | NADPH oxidase inhibition | Specific targeting of ROS sources |
| Genetic Tools | siRNA, CRISPR/Cas9 | Knockdown/knockout of redox enzymes | Targeted manipulation of specific pathways |
| Activity Assays | Amplex Red, cytochrome c reduction | Enzymatic activity measurement | Quantification of NOX, XO, antioxidant enzymes |
| Antibody-based Reagents | Anti-3-nitrotyrosine, anti-HNE | Detection of oxidative modifications | Specific recognition of oxidized biomolecules |
Protocol for Measuring Lipid Peroxidation via TBARS Assay
The thiobarbituric acid reactive substances (TBARS) assay represents a widely used method for assessing lipid peroxidation in biological samples [12]:
- Sample Preparation: Homogenize tissue samples or collect cell lysates in phosphate-buffered saline containing butylated hydroxytoluene (0.01%) to prevent artificial oxidation during processing.
- Reaction Mixture: Combine 100μL sample with 200μL of 8.1% sodium dodecyl sulfate, 1.5mL of 20% acetic acid (pH 3.5), and 1.5mL of 0.8% thiobarbituric acid.
- Incubation: Heat mixture at 95°C for 60 minutes, then cool on ice for 10 minutes.
- Extraction: Add 1mL of distilled water and 5mL of n-butanol:pyridine (15:1 v/v) mixture, vortex vigorously, and centrifuge at 1,500×g for 10 minutes.
- Measurement: Collect the organic layer and measure absorbance at 532nm against MDA standards (typically 1-20μM). Express results as nmol MDA equivalents per mg protein.
Protocol for Assessing Protein Carbonylation via DNPH Assay
Protein carbonylation serves as a reliable marker of protein oxidation [12]:
- Protein Precipitation: Add 20% trichloroacetic acid (TCA) to sample (1:1 v/v), incubate on ice for 10 minutes, and centrifuge at 15,000×g for 5 minutes.
- Derivatization: Resuspend protein pellet in 500μL of 10mM 2,4-dinitrophenylhydrazine (DNPH) in 2M HCl (for sample) or 2M HCl alone (for blank control). Incubate for 60 minutes at room temperature with vortexing every 15 minutes.
- Precipitation and Washing: Precipitate protein with 20% TCA, wash pellet three times with 1mL ethanol:ethyl acetate (1:1 v/v) to remove free DNPH.
- Solubilization: Dissolve final pellet in 500-1000μL of 6M guanidine hydrochloride (pH 2.3) by incubating at 37°C for 30 minutes with occasional vortexing.
- Measurement: Measure absorbance at 370nm and calculate carbonyl content using molar extinction coefficient of 22,000 Mâ»Â¹cmâ»Â¹. Normalize to protein concentration.
Therapeutic Implications and Targeting Strategies
Antioxidant-Based Therapeutic Approaches
Traditional antioxidant strategies have focused on direct ROS scavenging using compounds such as vitamin C, vitamin E, N-acetylcysteine, and SOD mimetics [9] [1]. However, clinical trials with broad-spectrum antioxidants have yielded largely disappointing results, attributed to lack of specificity, inability to target relevant ROS sources, and disruption of physiological redox signaling [3] [1]. This has prompted development of more targeted approaches including NOX isoform-specific inhibitors that block pathological ROS production at its source [11], Nrf2 activators that boost endogenous antioxidant defenses [4] [1], and mitochondria-targeted antioxidants (e.g., MitoQ) that concentrate antioxidant capacity at major ROS generation sites [3].
Emerging Redox-Based Therapeutics
Contemporary drug development recognizes the need for nuanced redox modulation rather than blanket antioxidant suppression [1]. Emerging strategies include small molecule inhibitors targeting specific cysteine residues in redox-sensitive proteins [1], modulators of redox-sensitive transcription factors with contextual activity [4], and redox-based combination therapies that exploit oxidative vulnerabilities in specific disease states [3]. The bidirectional nature of redox imbalance necessitates therapeutic approaches that can address both oxidative and reductive stress depending on disease context [4]. Future directions include development of disease-specific redox biomarkers for patient stratification, smart antioxidants with activatable specificity, and nanoparticle-based delivery systems for targeted redox modulation [13] [1].
Diagram 3: Therapeutic Strategies for Redox Imbalance. Approaches include traditional antioxidants, targeted inhibitors of specific ROS sources, NRF2 activators boosting endogenous defenses, and mitochondrial-targeted antioxidants.
ROS, RNS, and RSS function as crucial signaling mediators in physiological processes while simultaneously driving pathological mechanisms when dysregulated. The dual nature of these reactive species necessitates precise homeostatic control rather than simple elimination. Future research directions should focus on spatiotemporal regulation of specific reactive species, development of targeted redox-based therapeutics, identification of clinically relevant redox biomarkers, and understanding of inter-organ communication in systemic redox regulation. As methodological advances enable more precise monitoring and manipulation of redox processes, the therapeutic targeting of reactive species promises novel interventions for inflammatory, cardiovascular, neurodegenerative, and metabolic diseases.
Redox imbalance, a state of disrupted equilibrium between oxidant production and antioxidant defenses, is a pivotal regulator of inflammatory processes and the pathogenesis of numerous diseases [4]. While physiological levels of reactive oxygen species (ROS) and reactive nitrogen species (RNS) function as crucial signaling molecules, their dysregulation contributes to a spectrum of pathologies including cardiovascular, neurodegenerative, and autoimmune disorders [4] [15] [16]. This technical guide examines three principal cellular sources of redox imbalance: mitochondria, NADPH oxidase (NOX) enzymes, and the endoplasmic reticulum (ER). Understanding the distinct mechanisms, interplay, and experimental approaches for investigating these sources is fundamental for developing targeted therapeutic strategies in inflammation-related disease research.
Mitochondria: The Metabolic Powerhouse as a Redox Signal Integrator
Mechanisms of Mitochondrial ROS Production
Mitochondria are fundamental organelles responsible for cellular bioenergetics, but他们也 represent a major endogenous source of ROS [17]. The electron transport chain (ETC) is the primary site for mitochondrial ROS generation, with complex I (NADH dehydrogenase) and complex III (ubiquinol-cytochrome c oxidoreductase) identified as the most significant contributors [17]. Under normal physiological conditions, an estimated 1-2% of molecular oxygen consumed by mitochondria undergoes incomplete reduction, leading to the formation of superoxide anion (O₂•â») [17]. At complex I, O₂•⻠is produced primarily through the electron transfer to Oâ‚‚ during flavin mononucleotide semiquinone autoxidation. At complex III, O₂•⻠generation occurs via the ubiquinone cycle, where the semiubiquinone intermediate donates an electron to molecular oxygen [17]. The highly reactive O₂•⻠is rapidly converted to the more stable hydrogen peroxide (Hâ‚‚Oâ‚‚) by manganese superoxide dismutase (MnSOD/SOD2) in the mitochondrial matrix. Hâ‚‚Oâ‚‚, being membrane-permeable, can diffuse throughout the cell and function as a redox signaling molecule [4] [17].
Beyond the ETC, several other mitochondrial enzymes contribute to ROS production, including α-ketoglutarate dehydrogenase, pyruvate dehydrogenase, and enzymes involved in fatty acid β-oxidation [17]. Under pathophysiological conditions such as hypoxia, metabolic overload, or mitochondrial DNA damage, electron leakage increases substantially, leading to excessive ROS production that overwhelms antioxidant defenses and promotes oxidative damage [17] [18].
Redox Signaling and Pathophysiological Consequences
Mitochondrial ROS function as important signaling molecules that regulate various cellular processes, including inflammatory responses, hypoxic signaling, and apoptosis [17]. However, chronic mitochondrial ROS overproduction disrupts redox-sensitive signaling pathways, particularly through the oxidation of critical cysteine residues in regulatory proteins [17]. In cardiovascular diseases, mitochondrial ROS contribute to endothelial dysfunction by reducing nitric oxide (NO) bioavailability through the formation of peroxynitrite (ONOOâ»), a potent oxidant and nitrating agent [15] [16]. In the context of intervertebral disc degeneration, mitochondrial dysfunction and ROS overproduction promote inflammatory cytokine production, extracellular matrix degradation, and cellular senescence [18]. Furthermore, mitochondrial ROS can activate the NLRP3 inflammasome, leading to the maturation and secretion of pro-inflammatory cytokines such as IL-1β and IL-18 [4].
Table 1: Key Sites of Mitochondrial ROS Production and Their Characteristics
| Site/Enzyme | Primary ROS | Subcellular Location | Regulatory Factors |
|---|---|---|---|
| Complex I | O₂•⻠| Mitochondrial matrix | High NADH/NAD+ ratio, reverse electron transport |
| Complex III | O₂•⻠| Mitochondrial intermembrane space | Antimycin A, ubiquinone pool redox state |
| α-Ketoglutarate dehydrogenase | O₂•⻠| Mitochondrial matrix | Substrate availability, Ca²⺠|
| Pyruvate dehydrogenase | O₂•⻠| Mitochondrial matrix | Pyruvate concentration, phosphorylation status |
| Fatty acid β-oxidation | H₂O₂ | Mitochondrial matrix | Fatty acid load, carnitine levels |
NADPH Oxidases: Purpose-Built ROS-Generating Enzymes
NOX Enzyme Family Structure and Function
The NADPH oxidase (NOX) family represents the only known enzyme family dedicated solely to deliberate ROS generation [19] [20]. Unlike mitochondrial ROS production, which occurs as a byproduct of metabolism, NOX enzymes catalyze the controlled reduction of molecular oxygen to generate O₂•⻠and/or H₂O₂ for specific signaling purposes [19]. The NOX family comprises seven members: Nox1-5 and Duox1-2, each with distinct tissue distribution, regulatory mechanisms, and subcellular localization [19]. All NOX isoforms share a common core structure consisting of six transmembrane domains containing two heme groups, and cytosolic C-terminal domains that bind FAD and NADPH [19] [20]. Electrons are transferred from NADPH through FAD and the heme groups to molecular oxygen, resulting in superoxide production [20].
Nox2 (originally identified as gp91phox) is highly expressed in phagocytic cells where it generates antimicrobial ROS, but it is also present in vascular cells including endothelial and smooth muscle cells [19]. Nox4, predominantly expressed in the kidney and vasculature, differs from other isoforms by producing H₂O₂ rather than O₂•⻠under most conditions [19]. Interestingly, subcellular localization studies of endogenous Nox4 in human endothelial cells show predominant nuclear localization, suggesting specific roles in nuclear redox signaling, though overexpression studies often show endoplasmic reticulum localization [19].
Regulation and Pathological Roles of NOX Enzymes
NOX enzyme activity is tightly regulated through multiple mechanisms, including transcriptional control, post-translational modifications, and interactions with regulatory subunits [19]. The vascular endothelium predominantly expresses Nox2 and Nox4, with Nox4 demonstrating constitutive activity while Nox2 requires activation by stimuli such as cytokines, growth factors, hyperoxia, and hypoxia [19]. In cardiovascular pathologies, angiotensin II significantly upregulates Nox1 expression in vascular smooth muscle cells, contributing to hypertension and vascular remodeling [19] [16].
NOX-derived ROS play critical roles in inflammatory signaling through the activation of redox-sensitive transcription factors including NF-κB and AP-1, which subsequently induce expression of adhesion molecules, cytokines, and chemokines that perpetuate inflammatory cascades [4] [19]. In chronic inflammatory diseases such as atherosclerosis, sustained NOX activation contributes to endothelial dysfunction, LDL oxidation, and monocyte recruitment [15] [16]. The development of isoform-specific NOX inhibitors represents an active area of therapeutic research for inflammatory and cardiovascular diseases [19] [16].
Diagram 1: NOX Enzyme Activation and Downstream Signaling
Endoplasmic Reticulum: Protein Folding and Redox Crossroads
ER Stress and Redox Imbalance
The endoplasmic reticulum (ER) is a crucial organelle for protein synthesis, folding, and post-translational modifications [21] [22]. The ER lumen maintains a unique oxidizing environment necessary for disulfide bond formation, a process catalyzed by protein disulfide isomerase (PDI) and ER oxidoreductase 1 (Ero1) [21]. During oxidative protein folding, electrons are transferred from cysteine thiols in substrate proteins through PDI and Ero1 to molecular oxygen, generating H₂O₂ as a byproduct [21] [18]. Under physiological conditions, this ROS production is minimal, but during ER stress – triggered by accumulation of unfolded/misfolded proteins – dysregulated disulfide bond formation leads to excessive ROS generation [21] [22].
ER stress activates an adaptive signaling network called the unfolded protein response (UPR), primarily through three transmembrane sensors: IRE1α, PERK, and ATF6 [21] [22]. Under normal conditions, these sensors are maintained in an inactive state through association with the ER chaperone BiP/GRP78. The accumulation of unfolded proteins causes BiP dissociation, leading to sensor activation [22]. Persistent or severe ER stress that cannot be resolved by the UPR transitions from adaptive to pro-apoptotic signaling, contributing to various pathological states [21] [22].
ER-Mitochondrial Crosstalk in Redox Signaling
A critical aspect of ER-related redox imbalance involves interorganellar crosstalk, particularly with mitochondria at specialized contact sites called mitochondria-associated ER membranes (MAMs) [21] [22]. Under ER stress conditions, calcium (Ca²âº) release from the ER leads to subsequent mitochondrial Ca²⺠uptake, which can stimulate mitochondrial ROS production [21] [18]. This creates a vicious cycle where ER stress-induced ROS promotes mitochondrial ROS, which further exacerbates ER stress [22]. Additionally, the UPR transducer IRE1α can activate JNK and NF-κB signaling pathways through interaction with TRAF2, thereby linking ER stress to inflammatory responses [22]. The transcription factor CHOP, induced during prolonged ER stress, downregulates antioxidant defenses and promotes oxidative damage [21] [22].
Table 2: Endoplasmic Reticulum Stress Sensors and Their Redox Functions
| UPR Sensor | Activation Mechanism | Redox-Related Functions | Outcomes |
|---|---|---|---|
| IRE1α | Dimerization, trans-autophosphorylation, RNase activation | XBP1 splicing, RIDD, JNK activation via TRAF2 | ER biogenesis, ERAD, apoptosis |
| PERK | Oligomerization, eIF2α phosphorylation | ATF4 and CHOP induction, antioxidant regulation | Translational attenuation, oxidative cell death |
| ATF6 | Golgi trafficking, proteolytic cleavage | Chaperone induction (BiP, GRP94) | Enhanced folding capacity, ER quality control |
Integrated Experimental Approaches for Studying Redox Imbalance
Methodologies for Source-Specific ROS Detection
Accurate measurement of ROS from specific cellular sources requires sophisticated experimental approaches. The following protocols represent current best practices for investigating redox imbalance in research settings:
Protocol 1: Mitochondrial Superoxide Measurement using MitoSOX Red
- Principle: MitoSOX Red reagent is a fluorogenic dye selectively targeted to mitochondria that exhibits fluorescence upon oxidation by superoxide.
- Procedure:
- Culture cells in appropriate growth medium and apply experimental treatments.
- Load cells with 2-5 μM MitoSOX Red in buffer for 15-30 minutes at 37°C.
- Wash cells with warm buffer to remove excess dye.
- Acquire fluorescence using flow cytometry (excitation/emission: 510/580 nm) or fluorescence microscopy.
- Validation: Include controls with mitochondrial inhibitors (e.g., rotenone for complex I, antimycin A for complex III) and antioxidants (e.g., Mito-TEMPO).
- Applications: Assessment of mitochondrial ROS in response to inflammatory stimuli, metabolic challenges, or pharmacological interventions [17] [18].
Protocol 2: NOX Activity Assay using Lucigenin-Enhanced Chemiluminescence
- Principle: Lucigenin undergoes redox cycling, producing light emission in the presence of superoxide anion.
- Procedure:
- Prepare membrane fractions from tissues or cells via differential centrifugation.
- Add NADPH (100 μM) as substrate to initiate the reaction.
- Measure chemiluminescence in the presence of lucigenin (5 μM) using a luminometer.
- Specificity Controls: Include inhibitors such as diphenyleneiodonium (DPI) or apocynin, and validate using cells deficient in specific NOX isoforms.
- Normalize results to protein concentration.
- Applications: Quantification of NOX activity in vascular tissues, immune cells, and disease models [19].
Protocol 3: ER Stress and ROS Detection using ER-Targeted HyPer Sensor
- Principle: The HyPer sensor is a genetically encoded fluorescent probe sensitive to Hâ‚‚Oâ‚‚ that can be targeted to the ER lumen.
- Procedure:
- Transfect cells with ER-HyPer plasmid using appropriate transfection methods.
- After 24-48 hours, treat cells with ER stress inducers (e.g., tunicamycin, thapsigargin).
- Measure fluorescence ratio (excitation: 420 nm/500 nm, emission: 516 nm) using fluorescence microscopy or plate readers.
- Parallel Assessment: Combine with UPR reporter assays (e.g., XBP1 splicing, CHOP expression) to correlate ER stress with redox changes.
- Applications: Investigation of ER redox dynamics during protein misfolding, nutrient stress, and inflammatory signaling [21] [22].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Investigating Cellular Redox Imbalance
| Reagent/Tool | Specific Target/Function | Research Application | Considerations |
|---|---|---|---|
| MitoTEMPO | Mitochondrial superoxide | Scavenges mitochondrial O₂•⻠| Cell-permeable, mitochondrial-targeted |
| Apocynin | NOX2 assembly inhibitor | Suppresses NOX2-derived ROS | Requires metabolic activation; specificity limitations |
| 4-PBA | Chemical chaperone | Attenuates ER stress | May affect multiple folding pathways |
| MitoSOX Red | Mitochondrial superoxide | Detection and quantification | Specificity requires validation with inhibitors |
| DHE (Dihydroethidium) | Cellular superoxide | Histochemical detection | Oxidized products intercalate with DNA |
| Lucigenin | Superoxide anion | Chemiluminescence-based NOX activity assay | Redox cycling may artifactually increase signal |
| ER-Tracker dyes | Endoplasmic reticulum | Live-cell ER labeling | Compatible with other fluorescent probes |
| HyPer sensors | Hâ‚‚Oâ‚‚ | Genetically encoded redox sensing | Ratiometric measurement enables quantification |
| 1,2-Dioleoyl-Sn-Glycerol | 1,2-Dioleoyl-Sn-Glycerol, CAS:24529-88-2, MF:C39H72O5, MW:621.0 g/mol | Chemical Reagent | Bench Chemicals |
| N-Isobutyryl-D-cysteine | N-Isobutyryl-D-cysteine, CAS:124529-07-3, MF:C7H13NO3S, MW:191.25 g/mol | Chemical Reagent | Bench Chemicals |
Diagram 2: Experimental Workflow for Investigating Cellular Redox Imbalance
The intricate interplay between mitochondrial, NOX-derived, and ER-generated ROS creates a complex redox signaling network that profoundly influences inflammatory responses and disease pathogenesis [4] [22]. Rather than functioning in isolation, these cellular compartments engage in cross-talk that amplifies redox imbalances under pathological conditions [21] [18] [22]. Future research directions should focus on developing more precise tools for real-time monitoring of compartment-specific ROS, elucidating the spatiotemporal dynamics of redox signaling, and identifying source-specific inhibitors with therapeutic potential. The integration of redox proteomics, genetically encoded biosensors, and systems biology approaches will provide unprecedented insights into how coordinated redox regulation from these diverse cellular sources orchestrates both physiological signaling and pathological inflammation in human disease.
The cellular response to oxidative stress is orchestrated by a complex network of redox-sensitive signaling pathways. Key nodes within this network—NF-κB, MAPK, Nrf2, and the NLRP3 inflammasome—integrate oxidative cues to direct critical cellular decisions regarding inflammation, survival, and programmed cell death. This whitepaper provides an in-depth analysis of the molecular architecture, activation mechanisms, and intricate crosstalk between these pathways. Framed within the context of inflammation and disease pathogenesis, this review synthesizes current mechanistic understanding and presents structured experimental data, detailed methodologies, and essential research tools to aid investigators in navigating this dynamic field. The overarching thesis posits that a systems-level understanding of this redox-sensitive signaling interactome is fundamental to developing novel therapeutics for chronic inflammatory, metabolic, and neurodegenerative diseases.
Redox signaling acts as a critical mediator in the dynamic interactions between organisms and their external environment, profoundly influencing both the onset and progression of various diseases [1]. Under physiological conditions, a delicate balance exists between the generation of reactive oxygen species (ROS) and the activity of antioxidant systems, a state known as redox homeostasis [1]. ROS, including superoxide (O₂•â»), hydrogen peroxide (Hâ‚‚Oâ‚‚), and hydroxyl radicals (•OH), are now recognized not merely as toxic byproducts but as crucial signaling molecules that maintain physiological functions—a process termed redox biology [23] [24].
The principle of hormesis governs the cellular response to ROS; low levels activate signaling pathways to initiate biological processes, while high levels cause damage to DNA, proteins, and lipids, leading to oxidative stress and pathology [24]. A critical mechanism of redox signaling involves the oxidation of cysteine residues within proteins. Hâ‚‚Oâ‚‚ can oxidize the thiolate anion (Cys-Sâ») to sulfenic acid (Cys-SOH), causing allosteric changes that alter protein function. This modification is reversible via disulfide reductases like thioredoxin (Trx) and glutaredoxin (Grx), making it a potent signal transduction mechanism [24].
Disruption of redox homeostasis is a hallmark of numerous chronic diseases, including cardiovascular disorders, neurodegeneration, diabetes, and cancer [25] [4]. This imbalance can manifest as either oxidative stress (OS), characterized by an overabundance of ROS, or its less-appreciated counterpart, reductive stress (RS), marked by an excess of reducing equivalents like NADH, NADPH, and reduced glutathione (GSH) [4]. Both extremes disrupt redox-sensitive signaling and contribute to inflammatory pathogenesis. This review dissects the core redox-sensitive signaling nodes—NF-κB, MAPK, Nrf2, and the NLRP3 inflammasome—that translate oxidative cues into inflammatory responses, providing a mechanistic framework for understanding disease progression and identifying therapeutic opportunities.
Molecular Mechanisms of Redox-Sensitive Signaling Nodes
The NF-κB Pathway
NF-κB is a master regulator of inflammation and a key redox-sensitive transcription factor. The NF-κB family comprises five members: p50, p52, RelA (p65), c-Rel, and RelB, which form various homo- and heterodimers [26]. The most common dimer, p65-p50, is sequestered in the cytoplasm by inhibitory IκB proteins in unstimulated cells.
- Activation Mechanism: The canonical pathway is triggered by pro-inflammatory stimuli like TNF-α or IL-1. This leads to the activation of the IκB kinase (IKK) complex, consisting of IKKα, IKKβ, and the regulatory subunit NEMO (IKKγ) [26]. IKK phosphorylates IκBα, targeting it for ubiquitination and proteasomal degradation. This liberates the p65-p50 dimer, allowing its nuclear translocation and binding to κB motifs in the promoter regions of target genes, leading to the expression of cytokines (e.g., TNF-α, IL-6), chemokines, adhesion molecules, and enzymes like COX-2 and iNOS [4] [26].
- Redox Regulation: ROS are potent activators of NF-κB. The IKK complex is redox-sensitive, and ROS can inhibit MAPK phosphatases by oxidizing their catalytic cysteine residues, indirectly prolonging kinase signaling that feeds into NF-κB activation [4]. Furthermore, the activity of other kinases upstream of IKK, such as AKT, can be modulated by ROS.
Table 1: Key Components of the NF-κB Signaling Pathway
| Component | Function | Redox Sensitivity |
|---|---|---|
| IKK Complex (IKKα/IKKβ/NEMO) | Phosphorylates IκB, leading to its degradation | Activation is enhanced by ROS |
| IκBα | Inhibitory protein that sequesters NF-κB in cytosol | Target for degradation upon pathway activation |
| p65 (RelA) | Transcription factor subunit with transactivation domain | DNA binding can be modulated by redox state |
| p50 | Transcription factor subunit for DNA binding | Forms the DNA-binding core of the heterodimer |
| NEMO (IKKγ) | Regulatory subunit essential for canonical signaling | Scaffold protein; crucial for complex assembly |
The MAPK Pathway
The Mitogen-Activated Protein Kinase (MAPK) pathways are a family of serine/threonine kinases that transduce extracellular signals into intracellular responses. Key branches include ERK1/2, JNK, and p38 MAPK.
- Activation Mechanism: MAPKs are activated through a three-tiered kinase cascade: MAPK Kinase Kinases (MAP3Ks) phosphorylate and activate MAPK Kinases (MAP2Ks), which in turn phosphorylate the MAPKs on threonine and tyrosine residues. Activated MAPKs then phosphorylate a wide range of substrates, including transcription factors, other kinases, and cytoskeletal proteins [4].
- Redox Regulation: MAPKs are major effectors of oxidative stress. ROS directly inhibit MAPK phosphatases (MKPs) by oxidizing a critical catalytic cysteine residue, leading to sustained MAPK activation [4]. The p38 and JNK pathways are particularly responsive to stress stimuli, including oxidative stress, and play significant roles in regulating apoptosis, cytokine production, and differentiation.
The Nrf2-Keap1 Pathway
The transcription factor Nrf2 (Nuclear factor erythroid 2-related factor 2) is the master regulator of the cellular antioxidant response, coordinating the expression of over 250 cytoprotective genes [26] [27].
- Canonical Regulation by Keap1: Under basal conditions, Nrf2 is continuously ubiquitinated and targeted for proteasomal degradation by its negative regulator, Keap1, which acts as a substrate adaptor for a Cullin 3 (Cul3)-based E3 ubiquitin ligase complex [26] [27]. Keap1 is a highly redox-sensitive sensor protein containing multiple critical cysteine residues.
- Activation Mechanism: Upon exposure to oxidative stress or electrophiles, specific cysteine residues in Keap1 are modified. This causes a conformational change that inactivates the E3 ligase complex, allowing newly synthesized Nrf2 to accumulate and translocate to the nucleus [26] [27]. In the nucleus, Nrf2 forms a heterodimer with a small Maf protein and binds to the Antioxidant Response Element (ARE) in the promoter regions of its target genes.
- Non-Canonical Activation: Nrf2 can also be activated independently of Keap1 cysteine modification. The autophagy adapter protein p62/SQSTM1 can compete with Nrf2 for binding to Keap1, sequestering Keap1 into aggregates and facilitating Nrf2 stabilization [26] [27].
Table 2: Key Components of the Nrf2-Keap1 Signaling Pathway
| Component | Function | Redox Sensitivity |
|---|---|---|
| Nrf2 | Master regulator transcription factor for antioxidant genes | Stabilized upon oxidative stress |
| Keap1 | Cysteine-rich sensor protein; negative regulator of Nrf2 | Directly modified by ROS/electrophiles |
| Cul3/Rbx1 | E3 ubiquitin ligase complex for Nrf2 ubiquitination | Constitutively active in complex with Keap1 |
| ARE | DNA promoter element (5'-TGACnnnGC-3') | Binding site for Nrf2-Maf heterodimer |
| Target Genes | HO-1, NQO1, GCLC, GPX, TXNRD1 |
Execute antioxidant and detoxification functions |
The NLRP3 Inflammasome
The NLRP3 inflammasome is a multiprotein complex that serves as a central platform for the activation of caspase-1 and the maturation of the pro-inflammatory cytokines IL-1β and IL-18, as well as the induction of a lytic form of cell death called pyroptosis [27] [28].
- Structure and Activation: The complex consists of a sensor (NLRP3), an adaptor (ASC), and an effector (caspase-1) [28]. Its activation typically requires a two-step process: a priming signal (e.g., through TLR4-NF-κB) upregulates the expression of NLRP3 and pro-IL-1β, and an activation signal triggers complex assembly.
- Redox Regulation: ROS are a well-established trigger for NLRP3 activation [27] [28]. Multiple sources of ROS, including mitochondrial ROS, NOX-derived ROS, and ER stress-induced ROS, can promote inflammasome assembly. The specific molecular mechanism by which ROS activates NLRP3 is still under investigation but may involve direct oxidation of NLRP3 or associated proteins, or indirect effects via the oxidation of cellular components like mitochondrial DNA or cardiolipin, which can then be released as DAMPs.
Pathway Crosstalk: An Integrated Redox Signaling Network
The redox-sensitive pathways do not operate in isolation but form a dense, interconnected network characterized by extensive crosstalk, which can be either antagonistic or synergistic.
The Antagonistic Nrf2-NF-κB Crosstalk
A prime example of pathway crosstalk is the predominantly antagonistic relationship between Nrf2 and NF-κB [26] [29]. This occurs at multiple levels:
- Competition for Transcriptional Coactivators: Both Nrf2 and NF-κB require the coactivator CBP (CREB-binding protein) for efficient gene transcription. They compete for binding to limited pools of CBP, such that activation of one pathway can sequester CBP and suppress the other [29].
- Direct Transcriptional Regulation: Nrf2 can directly suppress the expression of pro-inflammatory cytokines like IL-6 and IL-1β, thereby dampening the NF-κB-driven inflammatory response [27].
- Redox-Mediated Inhibition: By enhancing the expression of antioxidant and detoxifying enzymes, Nrf2 reduces intracellular ROS levels, which can diminish ROS-dependent activation of NF-κB and MAPK pathways [4] [26].
This reciprocal inhibition suggests that the cellular response to stress is channeled towards either a pro-survival, antioxidant program (Nrf2) or a pro-inflammatory, immune-activating program (NF-κB).
Nrf2 and the Inflammasome
Nrf2-activating compounds have been shown to inhibit NLRP3 inflammasome activation and subsequent inflammation [27]. The mechanisms are multifaceted and may involve:
- Reduction of ROS: As a primary activator of NLRP3, reducing cellular ROS via Nrf2 is a key inhibitory mechanism.
- Upregulation of Heme Oxygenase-1 (HO-1): The Nrf2 target gene HO-1 has potent anti-inflammatory effects, including the generation of carbon monoxide and bilirubin, which can suppress inflammasome activity.
- Modulation of Autophagy: Nrf2 can influence autophagic flux, which is crucial for clearing damaged mitochondria (a source of NLRP3-activating DAMPs) and potentially degrading inflammasome components.
MAPK as a Common Integrator
The MAPK pathways, particularly p38 and JNK, are activated by a wide array of stimuli, including ROS and inflammatory cytokines. They serve as integrators that can feed into both NF-κB and NLRP3 activation. For instance, MAPK signaling can enhance NF-κB transcriptional activity and is involved in the priming step of NLRP3 inflammasome activation by upregulating NLRP3 expression [4].
The following diagram illustrates the core crosstalk and regulatory relationships between these key pathways:
Experimental Analysis of Redox Signaling
Studying redox-sensitive pathways requires a combination of molecular biology, biochemical, and cell imaging techniques to assess pathway activation, protein modifications, and functional outcomes.
Key Methodologies
1. Assessing Nrf2 Pathway Activation
- Western Blotting: Measure protein levels of Nrf2 in nuclear vs. cytoplasmic fractions. Assess Keap1 degradation and levels of key target proteins (e.g., NQO1, HO-1).
- Quantitative PCR (qPCR): Quantify mRNA levels of Nrf2 target genes (e.g.,
NQO1,HMOX1,GCLM). A significant upregulation indicates pathway activation. - ARE-Luciferase Reporter Assay: Cells are transfected with a plasmid containing an ARE promoter sequence driving luciferase expression. Increased luminescence upon treatment indicates Nrf2-mediated transcriptional activation.
- Immunofluorescence: Visualize the translocation of Nrf2 from the cytoplasm to the nucleus using specific antibodies.
2. Detecting NF-κB and MAPK Activation
- Phospho-Specific Western Blotting: The gold standard. Use antibodies against:
- NF-κB pathway: Phospho-IκBα (Ser32/36), Phospho-IKKα/β (Ser176/180), Phospho-p65 (Ser536).
- MAPK pathway: Phospho-p44/42 (Thr202/Tyr204) for ERK, Phospho-SAPK/JNK (Thr183/Tyr185), Phospho-p38 MAPK (Thr180/Tyr182).
- Electrophoretic Mobility Shift Assay (EMSA): To assess NF-κB DNA-binding activity in nuclear extracts (less common now due to advanced Western blotting).
- ELISA-based Transcription Factor Activity Assays: Commercial kits are available to quantify the DNA-binding activity of NF-κB or Nrf2 from nuclear extracts.
3. Measuring NLRP3 Inflammasome Activation
- Caspase-1 Activity Assay: Use fluorogenic substrates (e.g., YVAD-AFC) to measure caspase-1 enzymatic activity in cell lysates.
- Western Blotting for IL-1β and IL-18: Detect the cleaved, mature forms (p17 for IL-1β) in cell culture supernatants. Also, assess pro-IL-1β levels in lysates (priming readout).
- ASC Speck Formation Assay: Use immunofluorescence microscopy to visualize the large, micron-sized ASC oligomers that form upon inflammasome assembly.
4. Monitoring Redox State
- ROS-Sensitive Dyes: Cell-permeable fluorogenic probes like Hâ‚‚DCFDA (for general ROS), MitoSOX Red (for mitochondrial superoxide), and DHE (for superoxide).
- GSH/GSSG Ratio: Measured using enzymatic recycling assays or HPLC to quantify the cellular reduced-to-oxidized glutathione ratio, a key indicator of redox balance.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Studying Redox-Sensitive Pathways
| Reagent / Assay | Function / Target | Example Use Case |
|---|---|---|
| Sulforaphane | Natural isothiocyanate; canonical Nrf2 activator via Keap1 cysteine modification | Positive control for Nrf2 pathway induction; studying antioxidant responses [27]. |
| tert-Butylhydroquinone (tBHQ) | Synthetic phenolic antioxidant; potent Nrf2 inducer | Used in vitro to activate Nrf2 and study ARE-driven gene expression. |
| ML385 | Small molecule inhibitor that blocks Nrf2 binding to ARE | Validating the dependency of an observed effect on Nrf2 transcriptional activity. |
| TNF-α | Pro-inflammatory cytokine; potent activator of NF-κB canonical pathway | Standard stimulus for inducing NF-κB-dependent inflammation in cellular models. |
| Bay 11-7082 | Inhibitor of IκBα phosphorylation | Confirming NF-κB involvement in a signaling process. |
| LPS (Lipopolysaccharide) | TLR4 agonist; provides priming signal for NLRP3 inflammasome | Used in combination with a second signal (e.g., ATP, nigericin) to activate NLRP3 [28]. |
| MCC950 | Potent and selective small molecule inhibitor of NLRP3 | Determining the specific role of the NLRP3 inflammasome in a pathological model [28]. |
| Hâ‚‚DCFDA | Cell-permeable dye, fluoresces upon oxidation by broad-spectrum ROS | General measurement of intracellular oxidative stress. |
| MitoSOX Red | Mitochondria-targeted dye sensitive to superoxide | Specific detection of mitochondrial ROS, a key activator of NLRP3. |
| ARE-Luciferase Reporter | Plasmid for monitoring Nrf2 transcriptional activity | High-throughput screening for Nrf2 activators/inhibitors. |
| 3,7-Dimethyluric Acid | 3,7-Dimethyluric Acid, CAS:13087-49-5, MF:C7H8N4O3, MW:196.16 g/mol | Chemical Reagent |
| 3,6-Dibromopyridazine | 3,6-Dibromopyridazine, CAS:17973-86-3, MF:C4H2Br2N2, MW:237.88 g/mol | Chemical Reagent |
The experimental workflow below outlines a typical strategy for dissecting the role of these pathways in a cellular model of oxidative stress and inflammation:
The redox-sensitive signaling nodes NF-κB, MAPK, Nrf2, and the NLRP3 inflammasome form an intricate regulatory network that dictates cellular fate in response to oxidative challenge. The antagonistic relationship between the pro-survival Nrf2 pathway and the pro-inflammatory NF-κB and NLRP3 pathways suggests a cellular "switch" that determines the balance between cytoprotection and inflammation. Dysregulation of this balance is a cornerstone of pathogenesis in a wide array of chronic diseases.
Future research will benefit from a more dynamic and quantitative approach. Single-cell analysis techniques will reveal heterogeneity in pathway activation within cell populations. Advanced redox proteomics will allow for the systematic identification of specific cysteine residues modified under different stress conditions, providing a more precise map of the redox signaling network. Furthermore, the emerging concept of reductive stress and its impact on inflammation warrants deeper investigation [4].
From a therapeutic perspective, the crosstalk between these pathways offers both challenges and opportunities. While broad-spectrum antioxidants have shown limited clinical success, targeting specific nodes of the redox network holds greater promise. For example, the development of specific Nrf2 activators or KEAP1 inhibitors is a vibrant area of research for combating diseases driven by oxidative stress. Conversely, inhibiting the NLRP3 inflammasome with specific agents like MCC950 is being explored for inflammatory diseases [28]. A nuanced, systems-level understanding of this redox interactome will be essential for designing next-generation therapeutics that can precisely modulate the inflammatory response in a myriad of human diseases.
Redox signaling, the process by which reactive oxygen species (ROS) and other redox-active molecules modulate cellular functions, serves as a fundamental regulatory mechanism in inflammation and immunity [30]. This whitepaper examines how redox pathways precisely control key immune processes, particularly macrophage polarization and neutrophil extracellular trap (NET) formation (NETosis), alongside cytokine production, within the broader context of inflammatory diseases and therapeutic development. The bidirectional nature of redox signaling is critical to its function, with physiological levels of ROS acting as signaling messengers while excessive or sustained production leads to oxidative stress and pathological inflammation [4] [31] [3]. A sophisticated antioxidant system, including the NRF2 pathway, maintains this delicate balance [1]. Understanding these mechanisms provides crucial insights for developing targeted therapies for conditions ranging from cardiovascular and metabolic diseases to cancer and autoimmune disorders [1] [32] [3].
Redox Regulation of Macrophage Polarization and Function
Molecular Mechanisms of Redox Signaling in Macrophages
Macrophages exhibit remarkable functional plasticity, dynamically shifting their polarization state in response to microenvironmental cues. Redox signaling plays a pivotal role in directing these phenotypic changes through several molecular mechanisms:
Redox-Sensitive Transcription Factors: NF-κB represents the most well-characterized redox-dependent pathway in macrophages [4] [31]. ROS promote the phosphorylation and degradation of IκB proteins, enabling NF-κB nuclear translocation and transcription of pro-inflammatory genes including TNF-α, IL-1β, and IL-6 [4]. The NRF2-Keap1 system functions as a complementary protective axis, where ROS modify specific cysteine residues on Keap1, leading to NRF2 stabilization and nuclear translocation to induce antioxidant gene expression [4] [1]. The HIF-1α pathway is additionally activated under hypoxic conditions, driving expression of glycolytic enzymes and pro-inflammatory mediators [31].
Cysteine Oxidation in Signaling Proteins: Redox signaling primarily operates through the reversible oxidation of cysteine thiols (-SH) to sulfenic acid (-SOH) in target proteins [33] [30]. This modification significantly alters protein structure, activity, and localization. Key signaling nodes affected include protein kinases (PKA, PKC, CaMKII), receptor tyrosine kinases, and phosphatases [31] [30]. The specificity of these modifications is governed by kinetic parameters and subcellular localization, ensuring precise signal transduction [33].
Metabolic Reprogramming: Distinct macrophage polarization states exhibit characteristic metabolic profiles. M1 macrophages primarily utilize glycolysis, while M2 macrophages rely more on oxidative phosphorylation [31] [34]. Mitochondrial ROS (mtROS) generated from complexes I and III of the electron transport chain activate the NLRP3 inflammasome and promote IL-1β and IL-18 secretion [4] [31]. NOX-derived ROS additionally influence metabolic enzyme activity, creating feedback loops that sustain polarization states [31].
Table 1: Primary ROS Sources in Macrophage Polarization and Signaling
| ROS Source | Subcellular Location | Primary ROS | Role in Macrophage Function |
|---|---|---|---|
| NOX2 | Plasma membrane, phagosomal membrane | O₂•â», Hâ‚‚Oâ‚‚ | Microbial killing, pro-inflammatory polarization, cytokine production |
| Mitochondrial ETC | Mitochondrial matrix, inner membrane | O₂•â», Hâ‚‚Oâ‚‚ | Inflammasome activation, HIF-1α stabilization, metabolic reprogramming |
| NOX4 | Various intracellular membranes | Hâ‚‚Oâ‚‚ | Host defense against specific pathogens, cell death in response to oxLDL |
| p66Shc | Mitochondrial intermembrane space | Hâ‚‚Oâ‚‚ | Pro-apoptotic signaling, mitochondrial dysfunction |
Experimental Approaches for Studying Redox Signaling in Macrophages
Investigating redox mechanisms in macrophage biology requires specialized methodologies that capture the dynamic and compartmentalized nature of these processes:
Genetically Encoded Redox Probes: Modern approaches employ fluorescent protein-based probes (e.g., roGFP, HyPer) targeted to specific subcellular compartments (mitochondria, cytosol, phagosomal space) [30]. These tools enable real-time, compartment-specific measurements of Hâ‚‚Oâ‚‚ and glutathione redox potential in live cells with high spatiotemporal resolution [30]. For example, HyPer targeted to the mitochondrial matrix can reveal mtROS bursts following TLR4 activation.
Pharmacological Modulation of ROS Pathways: Specific inhibitors and activators help delineate contributions from distinct ROS sources:
- NOX inhibition: Diphenyleneiodonium (DPI) and apocynin (though with specificity limitations)
- Mitochondrial ROS scavenging: MitoTEMPO (mitochondria-targeted antioxidant)
- Xanthine oxidase inhibition: Allopurinol
- NRF2 pathway activation: Sulforaphane
Gene Silencing and Knockout Models: CRISPR/Cas9-mediated knockout or siRNA knockdown of specific ROS-generating enzymes (NOX isoforms, mitochondrial complexes) or antioxidant proteins (NRF2, SOD, GPX) enables determination of their specific contributions to macrophage polarization and function [34].
Redox Control of Neutrophil NETosis
Molecular Pathways of NET Formation
Neutrophil extracellular traps (NETs) are web-like structures composed of decondensed chromatin decorated with antimicrobial proteins that neutrophils expel to immobilize and neutralize pathogens [32]. Redox signaling plays a fundamental role in regulating multiple NETosis pathways:
NADPH Oxidase-Dependent NETosis: The classical pathway of NET formation requires assembly and activation of NOX2 at the plasma membrane, generating superoxide that is dismutated to Hâ‚‚Oâ‚‚ [31] [32]. Myeloperoxidase (MPO) then utilizes Hâ‚‚Oâ‚‚ to produce hypochlorous acid (HOCl), a potent oxidant that activates neutrophil elastase and MPO itself [31] [32]. These proteases translocate to the nucleus, where they degrade histones and promote chromatin decondensation, a prerequisite for NET release [32].
NADPH Oxidase-Independent Pathways: Certain stimuli, including calcium ionophores and uric acid crystals, can trigger NETosis through mitochondrial ROS (mtROS) production rather than NOX2 activation [32]. In this pathway, mtROS directly promote chromatin decondensation and NET release, demonstrating the versatility of redox signaling in regulating this process [32].
Redox Regulation of Cell Death Mechanisms: NETosis intersects with various cell death pathways. The interplay between ROS and the kinases RIPK1 and RIPK3 can promote necroptosis, which in neutrophils can be associated with NET release [32]. Additionally, metabolic reprogramming toward glycolysis provides both energy and biosynthetic precursors necessary for NET formation, with several glycolytic enzymes physically associating with NOX2 to potentially facilitate its activation [31].
Table 2: Redox-Dependent Mediators of NETosis and Their Functions
| Mediator | Source/Type | Role in NETosis | Key Interactions |
|---|---|---|---|
| NOX2 | Enzyme complex | Generates O₂•â»/Hâ‚‚Oâ‚‚ for MPO activation and downstream signaling | Required for classical NETosis; assembles with cytoskeletal elements |
| Myeloperoxidase (MPO) | Heme enzyme | Produces HOCl from Hâ‚‚Oâ‚‚; processes and activates proteases | Activates neutrophil elastase; synergizes with NE in histone degradation |
| Mitochondrial ROS | Mitochondrial ETC | Promotes chromatin decondensation in NOX-independent NETosis | Alternative pathway when NOX2 is deficient or inhibited |
| Neutrophil Elastase (NE) | Serine protease | Cleaves histones and nuclear proteins to decondense chromatin | Activated by MPO-generated oxidants; translocates to nucleus |
| PAD4 | Enzyme | Citrullinates histones to reduce DNA-histone binding | Can be activated by redox conditions; promotes chromatin decondensation |
Methodologies for NETosis Research
Investigating the redox aspects of NETosis requires complementary approaches that quantify NET formation while directly measuring associated redox changes:
NET Quantification Methods:
- Fluorescence Microscopy: Cells are stained with DNA-binding dyes (Sytox Green, DAPI) and neutrophil-specific markers (anti-MPO, anti-neutrophil elastase) to visualize and quantify NET structures. High-content imaging systems enable automated quantification.
- Circulating NET Marker Detection: ELISA-based measurements of MPO-DNA complexes or citrullinated histone H3 (CitH3) in plasma or supernatants provide quantitative NETosis data.
- DNase-Based NET Disruption: Treatment with exogenous DNase I following stimulation degrades NET structures, serving as both a experimental tool and therapeutic approach [32].
Redox Measurements During NETosis:
- Chemiluminescence Detection: Luminol and lucigenin amplification systems enable sensitive detection of ROS production during NET induction.
- Flow Cytometry with Redox-Sensitive Dyes: DCFH-DA (for general ROS), MitoSOX Red (for mtROS), and Amplex Red (for Hâ‚‚Oâ‚‚) allow quantification of ROS production in individual neutrophils.
- Inhibitor Studies: Pharmacological inhibition of NOX (DPI), MPO (ABAH), or mitochondrial ROS (MitoTEMPO) helps delineate specific ROS contributions.
Redox Control of Cytokine Networks
Cytokine production represents a critical endpoint of redox signaling in immune cells, with ROS directly and indirectly regulating both synthesis and secretion of these inflammatory mediators:
Transcription Factor Regulation: As previously discussed, redox-sensitive transcription factors including NF-κB, AP-1, and HIF-1α control the expression of numerous cytokines (TNF-α, IL-1β, IL-6, IL-8/CXCL8) and chemokines [4] [31]. The thiol-disulfide status of critical cysteine residues in these proteins determines their DNA-binding affinity and transcriptional activity [4] [30].
Inflammasome Activation: ROS, particularly mtROS, serve as potent activators of the NLRP3 inflammasome, leading to caspase-1-dependent processing and secretion of IL-1β and IL-18 [4] [31]. This mechanism connects redox signaling to the maturation of key cytokines central to inflammatory responses.
Cytokine-Chemokine Networks: Redox signaling creates feed-forward loops that amplify inflammatory responses. For example, TNF-α can stimulate ROS production from multiple sources, which in turn activates NF-κB to further enhance TNF-α expression [4] [31]. In β-cells under ER stress, macrophage-derived TNF-α induces Cxcl8 expression, recruiting neutrophils to sites of inflammation [35].
Table 3: Redox Regulation of Key Inflammatory Mediators
| Cytokine/Chemokine | Primary Cell Sources | Redox-Sensitive Transcription Factors | Functional Role in Inflammation |
|---|---|---|---|
| TNF-α | Macrophages, monocytes, T cells | NF-κB, AP-1 | Pro-inflammatory cytokine; activates endothelial cells; promotes leukocyte recruitment |
| IL-1β | Macrophages, monocytes, dendritic cells | NF-κB, NLRP3 inflammasome | Pyrogenic cytokine; activates fibroblasts and endothelial cells; promotes leukocyte activation |
| IL-6 | Macrophages, fibroblasts, endothelial cells | NF-κB, AP-1 | Pro-inflammatory cytokine; induces acute phase proteins; promotes B cell differentiation |
| IL-8/CXCL8 | Macrophages, neutrophils, endothelial cells | NF-κB, AP-1, HIF-1α | Neutrophil chemotaxis and activation; angiogenesis |
| IL-4 | T cells, mast cells, macrophages | STAT6 (indirect redox effects) | M2 macrophage polarization; anti-inflammatory responses; tissue repair |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Studying Redox Signaling in Immunology
| Reagent/Category | Specific Examples | Primary Research Application | Key Considerations |
|---|---|---|---|
| ROS Inhibitors | Diphenyleneiodonium (DPI), Apocynin, VAS2870 | Inhibition of NADPH oxidase activity | DPI lacks specificity (inhibits other flavoproteins); specificity varies by compound |
| Mitochondrial ROS Modulators | MitoTEMPO, MitoQ, Rotenone, Antimycin A | Scavenging or generation of mtROS | MitoTEMPO is mitochondria-targeted SOD mimetic; Rotenone/Antimycin inhibit ETC complexes |
| Antioxidant Enzymes | PEG-SOD, PEG-Catalase, Exogenous Thioredoxin | Scavenging specific ROS in extracellular space | Cell-impermeable; useful for extracellular ROS effects; PEGylation extends half-life |
| Redox-Sensitive Probes | DCFH-DA, MitoSOX Red, Amplex Red, roGFP, HyPer | Detection and quantification of specific ROS | Specificity varies (DCFH-DA detects various ROS); genetically encoded probes allow compartment-specific measurement |
| NETosis Inducers/Inhibitors | PMA, Ionomycin, ML171 (NOX2 inhibitor), DNase I | Induction or inhibition of NET formation | PMA is potent NOX2 activator; DNase I degrades existing NETs |
| Cytokine Measurement | ELISA, Luminex, ELISA-based MPO-DNA complexes | Quantification of cytokines and NET markers | MPO-DNA complexes are specific NET markers; multiplex assays enable cytokine profiling |
| Genetic Manipulation Tools | CRISPR/Cas9, siRNA, shRNA | Knockdown/knockout of redox-related genes | Enables cell-specific manipulation; in vivo models available for many redox enzymes |
| 4-(2-Acetoxyacetyl)phenyl acetate | 4-(2-Acetoxyacetyl)phenyl acetate, CAS:42528-99-4, MF:C12H12O5, MW:236.22 g/mol | Chemical Reagent | Bench Chemicals |
| Ergosta-4,6,8(14),22-Tetraen-3-One | Ergosta-4,6,8(14),22-tetraen-3-one|High-Purity | Bench Chemicals |
Therapeutic Implications and Future Directions
The intricate involvement of redox signaling in immunomodulation presents both challenges and opportunities for therapeutic intervention:
Context-Dependent Therapeutic Strategies: The dual roles of ROS as both signaling molecules and damaging agents necessitate precisely targeted approaches rather than broad antioxidant strategies [1] [3]. Future therapeutics should aim to modulate specific ROS sources or redox-sensitive pathways in a spatiotemporally controlled manner [1] [3].
Promising Therapeutic Targets:
- NOX Isoform-Specific Inhibitors: Developing compounds that selectively target specific NOX isoforms could attenuate pathological inflammation while preserving antimicrobial defense [3] [34].
- NLRP3 Inflammasome Regulators: Compounds that specifically modulate NLRP3 activation or downstream signaling could control IL-1β and IL-18 production in inflammatory diseases [4] [31].
- NET-Targeting Therapies: DNase I administration, which degrades NETs, has shown promise in preclinical models of autoimmune diseases, thrombosis, and cancer [32]. More specific approaches targeting NET formation without compromising neutrophil antimicrobial functions are under development [32].
Emerging Research Frontiers:
- Redoxomics: Comprehensive profiling of redox-sensitive protein modifications in specific immune cell types during activation and polarization [1] [30].
- Single-Cell Redox Analysis: Developing methods to measure redox states in individual immune cells within complex tissue environments [30].
- Metabolic-Redox Imaging: Simultaneous visualization of metabolic and redox changes in real-time in living immune cells [31] [34].
The evolving understanding of immunomodulation by redox signaling continues to reveal novel therapeutic opportunities for inflammatory diseases, cancer, and immune disorders. The development of sophisticated tools to precisely measure and manipulate redox processes in specific immune cell populations and subcellular compartments will drive future advances in this rapidly progressing field.
Redox signaling, a fundamental biological process involving the transfer of electrons in chemical reactions, exemplifies a dualistic nature in health and disease [1]. Under physiological conditions, reactive oxygen species (ROS) and reactive nitrogen species (RNS) function as crucial signaling molecules, regulating immune function, metabolic pathways, and cellular homeostasis [3] [36]. This delicate balance is maintained by sophisticated antioxidant systems, including the NRF2 pathway and enzymes like superoxide dismutase (SOD) and glutathione peroxidase (GPx) [1] [37]. However, dysregulation of this equilibrium leads to a state of oxidative stress, characterized by the overproduction of ROS/RNS that overwhelms antioxidant defenses, resulting in molecular damage and sustained activation of inflammatory pathways such as NF-κB [4] [38]. This review explores the intricate mechanisms of bidirectional redox control, detailing its role in physiological signaling versus its contribution to pathological damage across chronic diseases. We further provide a comprehensive toolkit for researchers, including standardized experimental protocols, key reagent solutions, and data visualization frameworks to advance the study of redox biology in inflammation and therapeutic development.
The term "redox" originates from the combination of "reduction" and "oxidation," describing chemical processes involving electron transfer between reactants [1]. These reactions are fundamental to energy acquisition in biological systems, primarily through oxidative respiration in mitochondria [1]. The redox state of a cell is determined by the delicate equilibrium between pro-oxidant species (ROS, RNS) and antioxidant defenses [37]. Physiological redox signaling occurs when low to moderate levels of reactive species function as signaling molecules, modulating essential processes including immune cell activation, vascular tone, and metabolic adaptation [3] [36]. Conversely, pathological oxidative stress arises from a disruption in this homeostasis, where excessive ROS/RNS production leads to oxidative damage of lipids, proteins, and DNA, driving the pathogenesis of chronic diseases [4] [37].
The interplay between oxidative stress and inflammation forms a self-amplifying vicious cycle in numerous pathologies [38]. ROS activate key inflammatory transcription factors like NF-κB, which in turn upregulates the expression of pro-inflammatory cytokines and enzymes that generate additional ROS [4] [38]. This nexus is critically implicated in a wide spectrum of conditions, including cardiovascular diseases, neurodegenerative disorders, diabetes, cancer, and autoimmune conditions [4] [1] [3]. Understanding the precise mechanisms that differentiate beneficial redox signaling from harmful oxidative damage is paramount for developing targeted therapeutic interventions that can disrupt this cycle without compromising essential redox-dependent functions.
Molecular Mechanisms of Bidirectional Redox Control
Reactive species are generated from both endogenous and exogenous sources and play context-dependent roles. Key reactive species and their primary sources are summarized below.
Table 1: Key Reactive Species and Antioxidants in Redox Biology
| Reactive Species/Antioxidants | Primary Production Source / Location | Primary Role/Reaction |
|---|---|---|
| Superoxide (O₂•â») | Mitochondrial ETC (Complexes I & III), NADPH oxidases (NOX) [4] [3] | One-electron reduction of Oâ‚‚; dismutates to Hâ‚‚Oâ‚‚ [25] |
| Hydrogen Peroxide (Hâ‚‚Oâ‚‚) | Product of SOD-mediated dismutation [25] | Diffusible signaling oxidant; detoxified by catalase/GPx [4] [25] |
| Hydroxyl Radical (•OH) | Generated from Hâ‚‚Oâ‚‚ via Fenton reaction (Fe²âº) [4] [25] | Highly reactive; causes severe damage to lipids, proteins, DNA [4] |
| Nitric Oxide (NO) | Nitric oxide synthases (eNOS, iNOS, nNOS) [4] [25] | Radical gasotransmitter; reacts with O₂•⻠to form peroxynitrite [4] |
| Peroxynitrite (ONOOâ») | Reaction between NO• and O₂•⻠[4] [25] | Potent oxidant/nitrating agent; modifies proteins and lipids [4] |
| Antioxidant Enzymes (SOD, Catalase, GPX) | SOD1 (cytosol), SOD2 (mitochondria), Catalase (peroxisomes) [1] [25] | SOD: 2 O₂•⻠+ 2H⺠→ H₂O₂ + O₂; Catalase/GPX: H₂O₂ → H₂O [1] [25] |
At low concentrations, Hâ‚‚Oâ‚‚ acts as a key signaling molecule, modulating pathways critical for cell proliferation, differentiation, and immune response [3]. Its membrane-permeable nature allows it to propagate oxidative signals [4]. However, high concentrations of Hâ‚‚Oâ‚‚ and other ROS like the hydroxyl radical lead to irreversible damage, initiating lipid peroxidation chains, oxidizing methionine and cysteine residues in proteins, and causing DNA strand breaks [4] [25].
Key Redox-Sensitive Signaling Pathways
The cellular response to reactive species is mediated by redox-sensitive signaling pathways. The interplay between the pro-inflammatory NF-κB pathway and the cytoprotective NRF2 pathway is a central paradigm in bidirectional redox control.
Figure 1: The interplay between the NF-κB and NRF2 pathways in redox signaling. Oxidative stress activates the pro-inflammatory NF-κB pathway while simultaneously inducing the cytoprotective NRF2 pathway. These pathways engage in reciprocal regulation, with NF-κB potentially suppressing NRF2 and vice versa, forming a critical regulatory node between inflammation and antioxidant defense [4] [1] [38].
NF-κB Pathway: This is a primary pro-inflammatory pathway activated by ROS. In the cytoplasm, NF-κB is sequestered by its inhibitory protein, IκB. ROS activate the IκB kinase (IKK) complex, leading to IκB phosphorylation and degradation. This allows NF-κB dimers (e.g., p65/p50) to translocate to the nucleus and induce the transcription of genes encoding pro-inflammatory cytokines (TNF-α, IL-1β, IL-6), adhesion molecules, and enzymes like COX-2 and iNOS, which further amplify ROS production [4] [38].
NRF2 Pathway: This is the master regulator of the antioxidant response. Under basal conditions, NRF2 is bound to its repressor, Keap1, and targeted for proteasomal degradation. Oxidative stress modifies critical cysteine residues on Keap1, leading to NRF2 stabilization and nuclear translocation. In the nucleus, NRF2 binds to Antioxidant Response Elements (AREs), driving the expression of a battery of cytoprotective genes, including heme oxygenase-1 (HO-1), NAD(P)H quinone dehydrogenase 1 (NQO1), and glutathione-synthesizing enzymes [1] [38]. NRF2 activation not only mitigates oxidative damage but also exerts anti-inflammatory effects by suppressing NF-κB signaling [4] [38].
The crosstalk between these pathways is critical; they compete for transcriptional co-activators like CREB-binding protein (CBP), and their mutual antagonism helps determine cellular fate in response to redox challenges [38].
Experimental Approaches in Redox Biology
Assessing Redox Status and Oxidative Damage
Accurate measurement of oxidative stress biomarkers is essential for diagnosing redox imbalance and evaluating therapeutic interventions. The following table summarizes key biomarkers and their measurement techniques.
Table 2: Biomarkers of Oxidative Stress and Damage
| Biomarker Category | Specific Biomarker | Detection Method | Biological Significance |
|---|---|---|---|
| Lipid Peroxidation | Malondialdehyde (MDA) | Thiobarbituric Acid-Reactive Substances (TBARS) assay [37] | End-product of lipid peroxidation; indicates oxidative damage to cell membranes [37] |
| F2-isoprostanes | Gas or Liquid Chromatography-Mass Spectrometry (GC/MS, LC-MS/MS) [37] | Stable, specific end-products of arachidonic acid peroxidation; gold standard for in vivo oxidative stress [37] | |
| Protein Oxidation | Protein Carbonyls | Derivatization with DNPH followed by spectrophotometry or immunoblotting [37] | Formation of carbonyl groups on protein side-chains; marker of irreversible protein oxidation [37] |
| DNA Oxidation | 8-Hydroxy-2'-deoxyguanosine (8-OHdG) | HPLC-ECD, HPLC-MS/MS, or ELISA [37] | Oxidized guanine nucleoside; biomarker for oxidative DNA damage; linked to mutagenesis [37] |
| Direct ROS Detection | Intracellular ROS (e.g., O₂•â», Hâ‚‚Oâ‚‚) | Electron Paramagnetic Resonance (EPR) with spin trapping; fluorescent probes (e.g., DCFH-DA) [37] | Allows dynamic, direct quantification of specific ROS in biological tissues and cells [37] |
The Scientist's Toolkit: Research Reagent Solutions
A range of chemical probes, inhibitors, and activators is essential for manipulating and studying redox pathways in vitro and in vivo.
Table 3: Key Research Reagents for Redox Biology
| Reagent / Tool | Category | Primary Function / Mechanism | Example Application |
|---|---|---|---|
| DCFH-DA | Fluorescent Probe | Cell-permeable dye oxidized by ROS to fluorescent DCF; measures general intracellular ROS [37] | Quantifying ROS bursts in immune cells (e.g., macrophages) upon stimulation [37] |
| MitoSOX Red | Mitochondria-targeted Probe | selectively targets mitochondria and is oxidized by superoxide; measures mtROS [3] | Assessing mitochondrial superoxide production in endothelial dysfunction [3] |
| MitoQ | Mitochondria-targeted Antioxidant | Ubiquinone derivative conjugated to TPP⺠cation; accumulates in mitochondria and reduces oxidative damage [37] | Investigating role of mtROS in models of hypertension and metabolic disease [37] |
| sulforaphane | NRF2 Activator | Natural compound that modifies Keap1 cysteine residues, stabilizing NRF2 and inducing ARE-driven gene expression [1] [38] | Enhancing antioxidant defenses in cellular models of oxidative stress [38] |
| NOX Inhibitors | Enzyme Inhibitor | e.g., GKT136901, VAS2870; selectively inhibit specific NADPH oxidase isoforms to block specific ROS sources [3] [37] | Dissecting the contribution of NOX-derived ROS vs. mitochondrial ROS in disease models [3] |
| NADPH Oxidase Assay Kit | Activity Assay | Measures superoxide production by NOX enzymes via luminescence or colorimetry | Determining NOX activation in cell lysates or tissue homogenates |
| 2-Bromo-5-hydroxybenzaldehyde | 2-Bromo-5-hydroxybenzaldehyde, CAS:1761-61-1, MF:C7H5BrO2, MW:201.02 g/mol | Chemical Reagent | Bench Chemicals |
| 2-Amino-5-chlorobenzophenone-d5 | 2-Amino-5-chlorobenzophenone-d5, CAS:65854-72-0, MF:C13H10ClNO, MW:236.71 g/mol | Chemical Reagent | Bench Chemicals |
Detailed Experimental Protocol: Evaluating NRF2 Activation and NF-κB Inhibition by a Plant Polyphenol
The following workflow provides a standardized method for investigating the dual antioxidant and anti-inflammatory effects of a candidate compound, such as the plant-derived polyphenol curcumin.
Figure 2: Experimental workflow for evaluating a compound's effect on NRF2 activation and NF-κB inhibition. This integrated protocol assesses key redox and inflammatory endpoints in a cellular model, such as LPS-stimulated macrophages [38] [37].
Protocol Steps:
Cell Culture and Treatment:
- Culture relevant cell lines (e.g., RAW264.7 macrophages or primary human macrophages) in appropriate media.
- Pre-treat cells with a range of concentrations of the test compound (e.g., curcumin at 5, 10, 20 µM) for 2 hours. Include a control group with vehicle (e.g., DMSO <0.1%).
- Stimulate cells with LPS (100 ng/mL) for 24 hours to induce an inflammatory response and oxidative stress.
Protein Extraction and Analysis:
- Harvest cells and separate nuclear and cytoplasmic fractions using a commercial kit.
- Perform Western blot analysis on the fractions.
- Probe for: NRF2 in the nuclear fraction (activation marker); NQO1 and HO-1 in total lysates (NRF2 target genes); IκBα in total lysates (degrades upon NF-κB activation); and NF-κB p65 in the nuclear fraction (translocation marker) [38].
RNA Analysis:
- Extract total RNA from treated cells.
- Perform quantitative RT-PCR (qRT-PCR) to measure mRNA levels of pro-inflammatory cytokines (TNF-α, IL-6, IL-1β) and NRF2-target antioxidant genes (HO-1, NQO1, GCLM) [38].
Functional Assays:
- Intracellular ROS: Seed cells in a black-walled plate. After treatment, load cells with DCFH-DA (10 µM) for 30 minutes. Measure fluorescence (Ex/Em: 485/535 nm) using a microplate reader [37].
- Glutathione Status: Use a commercial GSH/GSSG assay kit to measure the ratio of reduced to oxidized glutathione, a key indicator of cellular redox state [4] [37].
Pathophysiological Implications and Therapeutic Translation
Redox Dysregulation in Chronic Disease
The bidirectional nature of redox control is evident in its contribution to the pathogenesis of numerous chronic diseases. Dysregulation manifests as either sustained oxidative stress or, notably, reductive stress (RS), a condition marked by an overabundance of reducing equivalents like NADH, NADPH, and GSH, which can paradoxically impair immune defense and disrupt signaling [4].
- Cardiovascular Diseases (CVDs): Redox imbalance is a central driver of endothelial dysfunction, vascular inflammation, and cardiac remodeling. Mitochondrial dysfunction and NOX activation lead to excess ROS, which promotes VSMC proliferation, activates MMPs, and triggers inflammasome activation, contributing to atherosclerosis and heart failure [3].
- Neurodegenerative Disorders: Oxidative stress is a hallmark of Alzheimer's and Parkinson's diseases. ROS contribute to protein misfolding (e.g., Aβ and tau aggregation), mitochondrial dysfunction in neurons, and neuroinflammation via activation of microglial NF-κB and NLRP3 inflammasome [4] [1].
- Metabolic Syndromes (Diabetes & Hypertension): In diabetes, hyperglycemia-induced ROS via the polyol pathway, AGE/RAGE interaction, and PKC activation damages pancreatic β-cells and promotes insulin resistance [37]. In hypertension, angiotensin II-induced NOX activation produces superoxide, which quenches nitric oxide (NO), reducing vasodilation and increasing blood pressure [37].
- Osteoporosis and Cartilage Damage: In bone aging, ROS and inflammation synergize to disrupt bone homeostasis. TNF-α and IL-1β stimulate osteoclast differentiation via the RANKL/RANK/NF-κB axis while inhibiting osteoblast activity, leading to net bone loss [39] [40].
Emerging Therapeutic Strategies
The failure of broad-spectrum antioxidants in many clinical trials underscores the need for targeted, nuanced approaches that respect the physiological roles of ROS [38] [3] [37].
- NRF2 Activators: Synthetic and natural compounds (e.g, sulforaphane, bardoxolone methyl) that stabilize NRF2 offer a promising strategy to boost the endogenous antioxidant response and indirectly suppress inflammation [1] [38] [37].
- NOX Isoform-Specific Inhibitors: Unlike non-specific antioxidants, inhibitors targeting specific NOX isoforms (e.g., GKT136901 for NOX1/4) aim to block the primary source of pathological ROS without disrupting redox signaling from other sources [3] [37].
- Mitochondria-Targeted Antioxidants: Compounds like MitoQ and SkQ1 are engineered to accumulate within mitochondria, the primary source of ROS, offering superior efficacy in protecting against mtROS-induced damage in preclinical models of CVD and metabolic disease [3] [37].
- Redox Nanomedicine: Nanoparticles can be designed to deliver antioxidants (e.g., NRF2 activators, SOD mimetics) specifically to diseased tissues, such as atherosclerotic plaques or inflamed joints, improving efficacy and reducing off-target effects [38] [37].
- Modulating Reductive Stress: Emerging understanding of RS suggests that therapeutic interventions may need to carefully modulate, rather than universally boost, reducing equivalents to restore true redox homeostasis [4].
The duality of redox control—as both a vital physiological regulator and a potent mediator of pathology—presents a complex yet targetable axis in modern biomedicine. The interplay between oxidative stress, reductive stress, and inflammatory pathways like NF-κB and NRF2 creates a dynamic system that determines cellular and organismal health. Future research must focus on developing more sophisticated tools to measure and manipulate redox states with spatial and temporal precision, moving beyond the simplistic "antioxidant" paradigm. The integration of detailed molecular protocols, standardized biomarker assessment, and targeted therapeutic designs, as outlined in this review, provides a roadmap for advancing this field. Success in translating redox biology into clinical applications will depend on a nuanced understanding of this bidirectional control, ultimately enabling the development of personalized therapies that can correct specific redox imbalances across a spectrum of inflammatory diseases.
Advanced Methodologies and Therapeutic Applications for Targeting Redox Pathways
Redox imbalance plays a pivotal role in the regulation of inflammation, influencing both the onset and progression of various inflammatory conditions [41]. The concept of redox balance represents the equilibrium between oxidative and reductive forces within the cellular environment, with deviations toward either extreme contributing to disease pathogenesis [41]. While the pro-inflammatory role of oxidative stress (OS) has been extensively documented, emerging evidence highlights the significance of reductive stress (RS)—a condition marked by excessive reducing equivalents such as NADH, NADPH, and reduced glutathione (GSH) [41]. This dynamic interplay between oxidative and reductive stress modulates immune cell function, inflammatory signaling pathways, and ultimately contributes to chronic inflammatory diseases including autoimmune disorders, cardiovascular conditions, and neuroinflammatory ailments [41].
Reactive oxygen species (ROS) and reactive nitrogen species (RNS) function as crucial signaling molecules in innate immunity, integrating with antioxidant systems to regulate phagocyte metabolism, migration, phagocytosis, and intercellular communication [36]. The redox signaling landscape has expanded to include reactive sulfur species (RSS), which together with ROS and RNS form sophisticated networks that control immune homeostasis and inflammatory resolution [36]. Understanding these complex redox dynamics requires precise biomarkers that can detect subtle imbalances before they manifest as pathological inflammation, driving the search for novel biomarkers spanning from traditional lipid peroxidation products to specific microRNAs that offer enhanced specificity and diagnostic potential.
Traditional Lipid Peroxidation Biomarkers
Lipid peroxidation represents a primary consequence of oxidative stress in inflammatory conditions, generating a variety of breakdown products that serve as reliable biomarkers for assessing redox imbalance. These traditional biomarkers have been extensively validated across numerous inflammatory diseases and remain fundamental to redox research.
Table 1: Traditional Lipid Peroxidation and Protein Oxidation Biomarkers
| Biomarker | Chemical Nature | Detection Method | Inflammatory Context |
|---|---|---|---|
| Malondialdehyde (MDA) | Lipid peroxidation product | Thiobarbituric acid reactive substances (TBARS) assay | Elevated in psoriasis, atopic dermatitis, and IBD [42] [43] |
| Advanced Oxidation Protein Products (AOPP) | Oxidized protein compounds | Spectrophotometry (Witko-Sarsat method) | Increased in inflammatory skin diseases and gastrointestinal inflammation [42] [43] |
| 8-hydroxy-2'-deoxyguanosine (8-OHdG) | Oxidized DNA product | ELISA, LC-MS | Elevated in psoriasis and atopic dermatitis urine samples [42] |
| 4-hydroxynonenal (4-HNE) | Lipid peroxidation aldehyde | Immunohistochemistry, LC-MS | Protein adducts formed during inflammatory tissue damage |
Malondialdehyde (MDA), a prominent lipid peroxidation product, has demonstrated significant diagnostic utility in inflammatory conditions. Comparative studies between psoriasis and atopic dermatitis patients reveal that while MDA levels are elevated in both conditions compared to healthy controls, they do not significantly differ between these two inflammatory skin diseases, suggesting MDA represents a general marker of inflammatory oxidative stress rather than a disease-specific indicator [42]. In inflammatory bowel disease (IBD), meta-analyses have confirmed that MDA levels effectively differentiate between active and inactive Crohn's disease, highlighting its value as a monitoring biomarker for disease flares [43].
Advanced Oxidation Protein Products (AOPP) have emerged as crucial markers of protein oxidative damage in chronic inflammation. These compounds are detected using the Witko-Sarsat method, which relies on their reaction with glacial acetic acid and potassium iodide [42]. In clinical studies of psoriasis and atopic dermatitis, AOPP levels demonstrate the pervasive protein oxidation that occurs during inflammatory responses, though similar to MDA, they show limited specificity for distinguishing between different inflammatory conditions [42].
Antioxidant Defense System Biomarkers
The antioxidant defense system comprises enzymatic and non-enzymatic components that maintain redox homeostasis. Measurements of these antioxidants provide valuable insights into the compensatory mechanisms activated during inflammatory stress and have emerged as sensitive biomarkers for tracking disease activity.
Table 2: Antioxidant Defense System Biomarkers in Inflammatory Diseases
| Biomarker | Function | Detection Method | Inflammatory Context |
|---|---|---|---|
| Catalase (CAT) | Hâ‚‚Oâ‚‚ decomposition | Spectrophotometric (ammonium molybdate complex) | Higher in atopic dermatitis vs. psoriasis; discriminates between these conditions [42] |
| Superoxide Dismutase (SOD) | Superoxide radical dismutation | Misra and Fridovich method | Altered activity in psoriasis and atopic dermatitis [42] |
| Glutathione Peroxidase (GPx) | Hydroperoxide reduction | NADPH consumption assay | Differentiates active vs. inactive ulcerative colitis [43] |
| Paraoxonase 1 (PON1) | HDL-associated esterase | Arylesterase activity assay | Indicator of disease activity in both Crohn's disease and ulcerative colitis [43] |
| Free Thiols | Redox-active sulfhydryls | Ellman's assay | Reduced in active ulcerative colitis [43] |
| Total Antioxidant Capacity (TAC) | Cumulative antioxidant capacity | Colorimetric assays | Decreased during Crohn's disease flares [43] |
Catalase has demonstrated particular diagnostic value in differentiating between inflammatory conditions. ROC analysis reveals that catalase exhibits good diagnostic accuracy (AUC = 0.719) in discriminating patients with psoriasis versus atopic dermatitis, with a cut-off value of 0.436 U/L providing optimal differentiation [42]. This finding highlights how specific antioxidant enzymes can offer diagnostic specificity beyond general oxidative stress markers.
The diagnostic potential of antioxidant biomarkers extends to gastrointestinal inflammation, where paraoxonase 1, erythrocyte glutathione peroxidase, catalase, albumin, transferrin, and free thiols all demonstrate significant alterations between active and inactive ulcerative colitis [43]. Similarly, meta-analyses confirm that malondialdehyde, paraoxonase 1, catalase, albumin, transferrin, and total antioxidant capacity serve as reliable indicators of Crohn's disease flares [43]. These findings underscore the value of combining multiple antioxidant biomarkers to comprehensively assess inflammatory disease activity.
microRNAs as Novel Redox Biomarkers
The discovery of microRNAs (miRNAs) as regulators of redox signaling has opened new avenues for biomarker development. These small non-coding RNAs (19-22 nucleotides) offer exceptional stability in circulation, tissue-specific expression patterns, and the ability to provide real-time insights into redox regulatory networks [44].
Redox-Sensitive miRNA Signatures
Several miRNA families have emerged as key responders and regulators of cellular redox status, forming sophisticated feedback loops that influence inflammatory pathways:
miR-21, miR-155, and miR-210 represent prominently studied redox-sensitive miRNAs that are selectively packaged into exosomes under oxidative stress conditions through RNA-binding proteins like hnRNPA2B1 and SYNCRIP [44]. These miRNAs operate within a ROS-miRNA-exosome axis that orchestrates intercellular communication within the tumor microenvironment and inflammatory foci [44]. For instance, oxidative stress not only stimulates exosome biogenesis but also influences the selective packaging of these redox-sensitive miRNAs, creating a feed-forward loop that amplifies inflammatory signaling [44].
The functional significance of these miRNAs extends to their ability to modulate key redox-sensitive pathways. Exosomal miR-200c suppresses Nrf2 activation, reducing antioxidant capacity and increasing oxidative stress in recipient cells, thereby sensitizing them to ferroptosis [44]. Similarly, miR-23a-3p inhibits GPX4 expression, promoting ROS accumulation and iron-dependent cell death, which significantly influences cancer progression and inflammatory tissue damage [44]. The identification of "ProteotoxomiRs" - diagnostic and pathologic miRNA signatures for reductive stress-induced proteotoxic heart disease - further highlights the expanding role of miRNAs in detecting specific redox pathologies [45].
miRNA Regulation of Immune Redox Responses
Exosomal miRNAs play a particularly important role in shaping immune responses through redox modulation. miR-155-5p has been shown to promote immune evasion by suppressing antitumor immunity through modulation of PD-L1 expression in macrophages [44]. Meanwhile, miR-21 and miR-146a induce macrophage reprogramming toward an M2 phenotype, reinforcing an immunosuppressive microenvironment in chronic inflammation [44]. These findings position specific miRNAs as both biomarkers and regulators of immune cell function in inflammatory conditions.
The transformative potential of miRNAs as biomarkers stems from their ability to provide dynamic information about redox status while offering superior stability due to their encapsulation in exosomes and other vesicles that protect them from RNase degradation [44]. This stability enables their detection in various biofluids, making them ideal candidates for minimally invasive monitoring of inflammatory activity.
Experimental Protocols for Redox Biomarker Analysis
Lipid Peroxidation Product Quantification
Malondialdehyde (MDA) via TBARS Assay
- Principle: MDA reacts with thiobarbituric acid (TBA) to form a pink chromophore.
- Protocol:
- Add 100 μL serum sample to 500 μL of TBA reagent (0.375% TBA, 15% trichloroacetic acid in 0.25M HCl)
- Heat mixture at 95°C for 30 minutes
- Cool on ice and centrifuge at 10,000 × g for 5 minutes
- Measure absorbance at 532 nm against blank
- Calculate concentration using molar extinction coefficient of 1.56 × 10^5 M^-1cm^-1
- Sample Type: Serum, plasma, or tissue homogenates
- Critical Notes: Avoid iron contamination; include butylated hydroxytoluene (0.01%) to prevent artificial lipid peroxidation during assay [42]
Advanced Oxidation Protein Products (AOPP)
- Principle: AOPP react with potassium iodide in acidic conditions to form colored complexes.
- Protocol:
- Dilute serum 1:5 in phosphate-buffered saline (PBS)
- Add 10 μL glacial acetic acid to 200 μL diluted serum
- Add 20 μL potassium iodide (1.16M)
- Incubate for 2 minutes at room temperature
- Read absorbance at 340 nm against chloramine-T standard curve
- Sample Type: Serum or plasma
- Critical Notes: Freshly prepare potassium iodide solution; measure immediately after mixing [42]
Antioxidant Enzyme Activity Assays
Catalase Activity Measurement
- Principle: Catalase decomposes Hâ‚‚Oâ‚‚, forming a stable complex with ammonium molybdate.
- Protocol:
- Mix 50 μL serum with 1 mL substrate (65 μM H₂O₂ in 60 mM sodium-potassium phosphate buffer, pH 7.4)
- Incubate exactly 1 minute at 37°C
- Add 1 mL ammonium molybdate (32.4 mM in 2M Hâ‚‚SOâ‚„)
- Measure absorbance at 374 nm against blank
- Express activity as U/L based on Hâ‚‚Oâ‚‚ consumption standard curve [42]
- Sample Type: Serum, plasma, or tissue homogenates
- Critical Notes: Strictly control reaction time; prepare Hâ‚‚Oâ‚‚ solution freshly
Superoxide Dismutase (SOD) Activity
- Principle: SOD inhibits autoxidation of epinephrine at alkaline pH.
- Protocol:
- Add 10 μL serum to 970 μL carbonate buffer (0.05M, pH 10.2, 0.1mM EDTA)
- Initiate reaction with 20 μL epinephrine (30mM in 0.05% acetic acid)
- Monitor absorbance at 480 nm for 2-3 minutes
- Calculate activity as units inhibiting 50% of epinephrine autoxidation [42]
- Sample Type: Serum, plasma, or tissue homogenates
- Critical Notes: Perform at 25°C; run blank without sample simultaneously
microRNA Analysis from Biofluids
Exosomal miRNA Isolation and Quantification
- Exosome Isolation:
- Centrifuge serum/plasma at 2,000 × g for 20 minutes to remove cells/debris
- Ultracentrifuge supernatant at 100,000 × g for 70 minutes at 4°C
- Resuspend exosome pellet in PBS for immediate use or storage at -80°C
- miRNA Extraction:
- Add Qiazol lysis reagent to exosome suspension (1:1 ratio)
- Extract RNA using miRNeasy Mini Kit with on-column DNase treatment
- Elute in RNase-free water and quantify using Nanodrop
- Reverse Transcription and qPCR:
- Reverse transcribe using miRNA-specific stem-loop primers
- Perform qPCR with TaqMan miRNA assays
- Normalize to spiked-in cel-miR-39 or stable endogenous controls (miR-16, miR-423)
- Critical Notes: Process plasma within 2 hours of collection; avoid freeze-thaw cycles; verify exosome isolation by electron microscopy or CD63/TSG101 immunoblotting [44]
Redox Signaling Pathways in Inflammation: Visualization
The integration of redox biomarkers into inflammatory signaling networks reveals complex regulatory circuits that drive disease progression. The following diagram illustrates key redox-sensitive pathways in inflammation:
The nuclear factor kappa B (NF-κB) pathway represents a central redox-sensitive signaling cascade in inflammation [41]. ROS promote activation of the IκB kinase (IKK) complex, leading to phosphorylation and proteasomal degradation of IκB, the inhibitory subunit of NF-κB [41]. This liberation allows NF-κB dimers to translocate to the nucleus and activate transcription of pro-inflammatory cytokines, adhesion molecules, and enzymes like COX-2 and iNOS [41]. Simultaneously, the Nrf2-Keap1 pathway functions as a protective antioxidant axis, where oxidative modification of critical cysteine residues on Keap1 leads to stabilization and nuclear translocation of Nrf2, driving expression of cytoprotective genes [41]. Specific miRNAs, including miR-21 and miR-155, form regulatory loops that fine-tune these pathways, creating interconnected networks that determine inflammatory outcomes.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Redox Biomarker Analysis
| Reagent/Category | Specific Examples | Research Function | Application Notes |
|---|---|---|---|
| Oxidative Damage Assay Kits | TBARS Assay Kit (Cayman), OxiSelect AOPP Assay Kit | Quantify lipid peroxidation and protein oxidation | Include antioxidant in lysis buffers to prevent ex vivo oxidation [42] |
| Antioxidant Activity Assays | Catalase Activity Kit (Sigma-Aldrich), Superoxide Dismutase Assay Kit (Cayman) | Measure enzymatic antioxidant capacity | Establish standard curves with purified enzymes for quantification [42] |
| Exosome Isolation Kits | ExoQuick-TC, Total Exosome Isolation Kit | Isulate exosomes from biofluids | Validate isolation efficiency by electron microscopy or nanoparticle tracking [44] |
| miRNA Analysis Platforms | TaqMan Advanced miRNA Assays, miRCURY LNA miRNA PCR System | Detect and quantify specific miRNAs | Use spike-in controls for normalization; verify specificity with inhibition studies [44] |
| Redox-Sensing Probes | CM-H2DCFDA, MitoSOX Red, roGFP | Measure specific ROS in cells | Calibrate for each cell type; consider compartment-specific localization |
| Antibodies for Redox Modifications | Anti-nitrotyrosine, Anti-4-HNE, Anti-8-OHdG | Detect specific oxidative modifications | Optimize antigen retrieval for immunohistochemistry applications |
| 2-Hydroxypalmitic acid | 2-Hydroxypalmitic acid, CAS:2398-34-7, MF:C16H32O3, MW:272.42 g/mol | Chemical Reagent | Bench Chemicals |
| N-Boc-N-methylethylenediamine | N-Boc-N-methylethylenediamine, CAS:121492-06-6, MF:C8H18N2O2, MW:174.24 g/mol | Chemical Reagent | Bench Chemicals |
This toolkit enables comprehensive assessment of redox biomarkers across multiple dimensions, from traditional oxidative damage markers to innovative miRNA signatures. The integration of these reagents into standardized protocols facilitates reproducible research that advances our understanding of redox dynamics in inflammation.
The evolving landscape of redox biomarkers spans from well-established lipid peroxidation products to emerging specific microRNAs, offering increasingly sophisticated tools for monitoring inflammatory diseases. Traditional markers like MDA and AOPP provide robust measurements of oxidative damage, while antioxidant enzymes including catalase and superoxide dismutase reflect compensatory cellular responses [42] [43]. The emergence of miRNA signatures such as miR-21, miR-155, and miR-200c represents a paradigm shift, enabling researchers to detect subtle redox imbalances with enhanced specificity and predictive value [44] [45].
Future research directions will focus on developing integrated biomarker panels that combine traditional oxidative stress markers with miRNA profiles and exosome characteristics to create comprehensive redox signatures. The application of single-cell RNA sequencing and spatial transcriptomics will further resolve cell-type-specific redox responses within inflammatory microenvironments [44]. Additionally, the concept of reductive stress as a pathological entity warrants expanded biomarker development beyond traditional oxidative stress markers [41]. As these novel redox biomarkers undergo validation in larger clinical cohorts, they hold exceptional promise for advancing personalized medicine approaches in inflammatory diseases, enabling earlier diagnosis, precise monitoring of therapeutic responses, and development of targeted interventions that restore redox homeostasis.
The transcription factor nuclear factor erythroid 2-related factor 2 (Nrf2) is recognized as the master regulator of the cellular antioxidant response, governing a genetic program that integrates cellular defense mechanisms against oxidative, metabolic, and inflammatory stress [46] [47]. Under homeostatic conditions, Nrf2 is constitutively targeted for proteasomal degradation by its primary negative regulator, Kelch-like ECH-associated protein 1 (Keap1), which acts as a substrate adaptor for a Cullin 3 (Cul3)-based E3 ubiquitin ligase complex [48] [49]. This system functions as a sensitive redox sensor; upon exposure to reactive oxygen species (ROS) or electrophiles, specific cysteine residues in Keap1 are modified, leading to Nrf2 stabilization, nuclear translocation, and transactivation of over 200 genes containing antioxidant response elements (ARE) in their promoters [47] [48]. The breadth of this regulatory network encompasses genes critical for glutathione synthesis, NADPH production, xenobiotic detoxification, and inflammation resolution, positioning the Keap1-Nrf2 axis as a pivotal therapeutic target for diseases characterized by oxidative stress and inflammation, including neurodegenerative, cardiovascular, metabolic, and autoimmune disorders [46] [50]. This whitepaper provides a comprehensive technical overview of small molecule strategies to activate Nrf2, detailed experimental methodologies for evaluating compound efficacy, and the therapeutic implications of modulating this pathway within the broader context of redox signaling in disease.
Molecular Architecture and Regulatory Mechanisms of the Keap1-Nrf2 System
Structural Domains and Functional Motifs
The functional interplay between Nrf2 and Keap1 is governed by their multi-domain structures:
NRF2 Structure: The human NRF2 protein comprises 605 amino acids with seven highly conserved Nrf2-ECH homology (Neh) domains [48]. The Neh2 domain mediates binding to Keap1 through two critical motifs: a high-affinity ETGE motif and a low-affinity DLG motif, forming the basis of the "hinge and latch" model of Nrf2 regulation [47] [51]. The Neh1 domain contains a basic leucine zipper (bZIP) structure that facilitates heterodimerization with small Maf (sMaf) proteins and subsequent binding to ARE sequences [48]. The transactivation domains Neh4 and Neh5 recruit co-activators like CBP/p300, while Neh6 mediates Keap1-independent degradation via β-TrCP, and Neh7 interacts with RXRα to repress Nrf2 activity [48] [52].
KEAP1 Structure: KEAP1 functions as a homodimer, with each 624-amino acid monomer containing several critical domains [47] [48]. The BTB domain mediates homodimerization and Cul3 binding, the intervening region (IVR) contains redox-sensitive cysteine residues that act as stress sensors, and the Kelch/DGR domain (double glycine repeat) directly binds the ETGE and DLG motifs of Nrf2 [48] [49]. Key cysteine residues—including Cys151 (BTB domain), Cys273, and Cys288 (IVR domain)—undergo modification under oxidative stress, leading to conformational changes that disrupt Nrf2 ubiquitination [48] [51].
The Canonical Activation Pathway
The following diagram illustrates the core regulatory mechanism of the Nrf2-Keap1 pathway under homeostatic and stressed conditions:
Under basal conditions, the Keap1 homodimer sequesters Nrf2 in the cytoplasm via binding to its ETGE and DLG motifs, presenting Nrf2 to the Cul3-RBX1 E3 ubiquitin ligase complex for polyubiquitination and subsequent proteasomal degradation, maintaining low cellular Nrf2 levels [48] [49]. Upon oxidative or electrophilic challenge, specific cysteine sensors (e.g., Cys151, Cys273, Cys288) in Keap1 are modified, inducing conformational changes that disrupt the Keap1-Nrf2 interaction, particularly at the DLG interface ("latch") while potentially retaining ETGE binding ("hinge") [46] [51]. This stabilization allows newly synthesized Nrf2 to accumulate and translocate to the nucleus, where it heterodimerizes with sMaf proteins and binds to ARE sequences, initiating transcription of a cytoprotective gene battery [47] [48].
Small Molecule Activators of Nrf2: Mechanisms and Quantitative Profiling
Electrophilic Inducers
Electrophilic compounds represent the first class of Nrf2 activators identified and include several clinical agents. These molecules typically function by covalently modifying critical cysteine residues within Keap1's sensor architecture.
Table 1: Electrophilic Nrf2 Activators
| Compound | Mechanism of Action | Key Molecular Targets | Clinical/Preclinical Status | Reported ECâ‚…â‚€/ICâ‚…â‚€ |
|---|---|---|---|---|
| Dimethyl Fumarate (DMF) [46] | Modifies Keap1 Cys151; activates Nrf2/ARE pathway | KEAP1 cysteine residues | Approved for multiple sclerosis, psoriasis | N/A |
| Sulforaphane [46] | Modifies Keap1 cysteine residues; induces Nrf2 nuclear accumulation | KEAP1 cysteine residues | Multiple clinical trials ongoing | N/A |
| Bardoxolone Methyl [46] | Modifies Keap1 Cys151; potent Nrf2 inducer | KEAP1 Cys151 | Clinical trials (CKD, pulmonary hypertension) | Submicromolar concentrations |
| CDDO-Im [46] | Highly potent electrophile; modifies multiple Keap1 cysteines | Multiple KEAP1 cysteine residues | Preclinical development | Highly toxic at submicromolar concentrations |
Protein-Protein Interaction (PPI) Inhibitors
A more recent strategy focuses on developing non-covalent, non-electrophilic inhibitors that directly disrupt the Keap1-Nrf2 protein-protein interaction by competitively binding to the Kelch domain of Keap1, thus preventing Nrf2 binding and degradation [46].
Table 2: Keap1-Nrf2 Protein-Protein Interaction Inhibitors
| Compound Class | Mechanism | Key Interactions | Development Status | Reported Káµ¢/ICâ‚…â‚€ |
|---|---|---|---|---|
| Tetrahydroisoquinoline Derivatives [46] | Binds Keap1 Kelch domain; competes with Nrf2 ETGE motif | Keap1 Kelch domain active site | Preclinical optimization | Low micromolar to nanomolar range |
| Fragment-Based Discoveries [46] | Small fragments binding Kelch domain; optimized for potency | Key residues in Keap1 binding pocket | Early preclinical | Micromolar range (fragments) |
| Peptide-based Inhibitors [46] | High-affinity peptides mimicking Nrf2 ETGE motif | Keap1 Kelch domain | Research tools | Nanomolar affinity |
PPI inhibitors offer potential advantages over electrophilic activators, including reduced off-target effects and greater specificity, as they do not react promiscuously with biological nucleophiles [46]. However, challenges remain in achieving optimal pharmacokinetic properties, particularly for central nervous system targets where blood-brain barrier penetration is essential [46] [52].
Experimental Framework for Evaluating Nrf2 Activators
In Vitro Binding and Biochemical Assays
A multi-tiered experimental approach is essential for comprehensive characterization of Nrf2 activators:
Surface Plasmon Resonance (SPR) and Bio-Layer Interferometry (BLI): Label-free techniques for quantifying binding kinetics (KD, kon, koff) between small molecules and the Keap1 Kelch domain, providing direct measurement of binding affinity and mechanism of competition with Nrf2 peptides [46].
Fluorescence Polarization (FP): High-throughput screening method that measures displacement of a fluorescently-labeled Nrf2 peptide from the Keap1 Kelch domain, generating IC50 values for PPI inhibitors [46].
Isothermal Titration Calorimetry (ITC): Gold standard for determining binding thermodynamics (KD, ΔH, ΔS, stoichiometry) by measuring heat changes during molecular interactions, providing mechanistic insights into binding drivers [46].
Cellular Thermal Shift Assay (CETSA): Evaluates target engagement in intact cells by measuring thermal stabilization of Keap1 upon compound binding, confirming cellular target occupancy [46].
Cellular Activity and Functional Assays
ARE-Luciferase Reporter Gene Assays: Engineered cells containing ARE-driven luciferase constructs provide a quantitative measure of Nrf2 pathway activation, with induction EC50 values indicating functional potency [46].
Western Blotting and Immunofluorescence: Measure Nrf2 protein accumulation, nuclear translocation, and expression of downstream targets (HO-1, NQO1, GCLC) under compound treatment, confirming pathway activation [46] [48].
Quantitative PCR (qPCR): Quantifies mRNA expression of canonical Nrf2 target genes (NQO1, HMOX1, GCLM, GCLC) to verify transcriptional activation [48] [53].
Glutathione and ROS Detection Assays: Functional readouts using fluorescent probes (DCFDA, DHE) or enzymatic assays to measure compound effects on cellular redox state and antioxidant capacity [47] [48].
In Vivo Efficacy and ADME Profiling
Animal Disease Models: Compounds are evaluated in preclinical models including myocardial ischemia-reperfusion [53], neurodegenerative models [52], renal inflammation [46], and metabolic disease models to establish proof-of-concept efficacy.
Blood-Brain Barrier Penetration: Critical for neurotherapeutic applications, assessed through parallel artificial membrane permeability assay (PAMPA) and in vivo brain-plasma ratio measurements [46] [52].
Pharmacokinetic Studies: Comprehensive ADME profiling including bioavailability, half-life, clearance, and volume of distribution to establish compound suitability for in vivo applications [46].
The following workflow diagram illustrates a recommended experimental cascade for characterizing novel Nrf2 activators:
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents for Investigating the Keap1-Nrf2 Pathway
| Reagent/Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| Recombinant Proteins | Keap1 Kelch domain, Full-length Nrf2 | In vitro binding assays (SPR, ITC, FP) | Direct binding characterization and competition studies |
| Cell-Based Reporters | ARE-luciferase stable lines (HEK293, HepG2) | High-throughput compound screening | Functional assessment of Nrf2 pathway activation |
| Antibodies | Anti-Nrf2, anti-Keap1, anti-HO-1, anti-NQO1 | Western blot, immunofluorescence, IP | Detection of protein expression, localization, and interactions |
| Animal Models | Nrf2 knockout mice, Keap1 knockdown models | In vivo target validation, efficacy studies | Genetic confirmation of on-target effects and disease modulation |
| Chemical Tools | Sulforaphane, DMF, ML334, compound A | Positive controls, mechanism studies | Benchmarking novel compounds against established chemotypes |
| 1-Boc-4-(aminomethyl)piperidine | 1-Boc-4-(aminomethyl)piperidine, CAS:144222-22-0, MF:C11H22N2O2, MW:214.30 g/mol | Chemical Reagent | Bench Chemicals |
| 5-Bromo-4-chloro-1H-indol-3-yl nonanoate | 5-Bromo-4-chloro-1H-indol-3-yl nonanoate, CAS:133950-77-3, MF:C17H21BrClNO2, MW:386.7 g/mol | Chemical Reagent | Bench Chemicals |
Therapeutic Implications in Redox-Mediated Diseases
The strategic activation of Nrf2 holds therapeutic potential across multiple disease domains characterized by oxidative stress and inflammation:
Neurodegenerative Disorders: In Alzheimer's and Parkinson's disease models, Nrf2 activation mitigates neuroinflammation, reduces protein aggregation, and enhances neuronal resilience [52] [50]. However, blood-brain barrier penetration remains a significant challenge for central nervous system targets [46] [52].
Cardiovascular and Metabolic Diseases: Nrf2 activators like AEOL-10150 demonstrate efficacy in myocardial ischemia-reperfusion injury by preserving mitochondrial function and reducing oxidative damage [53]. In metabolic contexts, Nrf2 influences NADPH production and glutathione regeneration, impacting diabetic complications and nonalcoholic steatohepatitis (NASH) [46] [48].
Cancer and Chemoprevention: The dual role of Nrf2 in cancer presents a complex therapeutic landscape—while activation can prevent carcinogenesis through enhanced detoxification, constitutive activation in established tumors promotes chemoresistance and metabolic adaptation [48] [51].
Autoimmune and Inflammatory Conditions: Dimethyl fumarate's clinical success in multiple sclerosis and psoriasis validates Nrf2 activation as a therapeutic strategy for immune-mediated disorders [46] [50]. Emerging evidence suggests Nrf2 modulates immune cell function and phenotype, particularly in T-cells and macrophages [50].
Challenges and Future Directions in Nrf2-Targeted Therapeutics
Despite significant progress, several challenges persist in the clinical translation of Nrf2-targeted therapies:
Specificity and Off-Target Effects: Electrophilic compounds exhibit promiscuous reactivity with biological nucleophiles beyond Keap1, while PPI inhibitors may disrupt other Kelch-domain interactions [46] [52]. Future efforts should focus on achieving greater selectivity through rational drug design.
Context-Dependent Biology: The protective versus pro-tumorigenic effects of Nrf2 activation require careful contextual consideration, potentially necessitating tissue-specific delivery or transient activation strategies [51].
Alternative Activation Strategies: Emerging approaches include inhibiting the Nrf2 repressor Bach1 to achieve constitutive pathway activation while bypassing Keap1 entirely, and targeted protein degradation strategies to address Nrf2 hyperactivation in cancer [52] [51].
Advanced Delivery Systems: Nanoencapsulation techniques and targeted delivery platforms show promise in enhancing the bioavailability and tissue specificity of Nrf2 activators, particularly for challenging targets like the central nervous system [50].
The continued elucidation of Nrf2 biology across tissues and disease states, coupled with advances in compound design and delivery, positions the Keap1-Nrf2 axis as a compelling target for next-generation therapeutics addressing the fundamental role of redox signaling in human disease.
Reactive oxygen species (ROS) are crucial signaling molecules in physiological processes, but their dysregulation is a hallmark of numerous chronic diseases. The concept of "redox stress" encompasses both oxidative stress (an excess of ROS) and reductive stress (an excess of reducing equivalents), both of which can disrupt cellular homeostasis [4]. Under physiological conditions, cells maintain redox homeostasis through tightly balanced systems including the mitochondrial electron transport chain, NADPH oxidases (NOX), and antioxidant defenses governed by transcription factors like NRF2 [1]. However, in pathological states, this balance is disrupted, leading to sustained ROS production that activates inflammatory pathways, promotes genomic instability, and drives disease progression [1] [38].
The interplay between oxidative stress and inflammation represents a core, self-amplifying mechanism in pathogenesis. ROS activate redox-sensitive transcription factors including nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB), which controls expression of pro-inflammatory cytokines, chemokines, and adhesion molecules [38]. This creates a vicious cycle wherein inflammation enhances ROS generation through immune cell activation, establishing sustained tissue injury [38]. Understanding these mechanisms has revealed new therapeutic opportunities for targeting the specific sources of pathological ROS production rather than deploying broad-spectrum antioxidants, which have largely failed in clinical trials [3] [38].
NOX Family of NADPH Oxidases: Structure, Function, and Isoforms
The NADPH oxidase (NOX) family represents a primary controlled source of cellular ROS, distinct from mitochondrial ROS byproducts. These transmembrane enzymes facilitate the generation of superoxide by transferring a single electron from NADPH to oxygen [3]. All NOX isoforms share conserved structural properties: six transmembrane domains, NADPH binding sites at the COOH terminus, a FAD binding region, and four highly conserved histidines that bind heme [54]. The NOX family comprises seven members: NOX1-5 and DUOX1-2, each with distinct tissue distribution, activation mechanisms, and ROS products [54] [55].
Table 1: NOX Isoforms: Characteristics, Expression, and Roles in Disease
| Isoform | Structural Partners | Primary ROS | Tissue Expression | Pathological Roles |
|---|---|---|---|---|
| NOX1 | p22phox, NOXO1, NOXA1 | O₂•⻠| Colon, vascular smooth muscle, endothelium [54] | Tumor proliferation, angiogenesis, hypertension [54] [55] |
| NOX2 (gp91phox) | p22phox, p47phox, p67phox, p40phox, Rac | O₂•⻠| Phagocytes, vascular cells, cardiomyocytes [54] | Chronic granulomatous disease, immune dysfunction in tumors, cardiovascular disease [54] [3] |
| NOX3 | p22phox, NOXO1 | O₂•⻠| Inner ear, vestibular system [54] | Otoconia formation, hearing loss [54] |
| NOX4 | p22phox, Poldip2 | Hâ‚‚Oâ‚‚ | Kidney, osteoclasts, vascular cells [54] | Fibrosis, tumor survival, metabolic syndrome [54] [55] |
| NOX5 | Ca²âº-binding EF hands (no p22phox) | O₂•⻠| Testis, spleen, lymphocytes, kidney [54] | Cardiovascular disease, inflammation [54] |
| DUOX1/2 | Ca²âº-binding EF hands, peroxidase-like | Hâ‚‚Oâ‚‚ | Thyroid, respiratory, gastrointestinal epithelium [54] | Thyroid hormone synthesis, airway defense [54] |
NOX2, originally identified in phagocytes, represents the prototypical NADPH oxidase and is essential for microbial killing [54]. Its activation requires assembly of multiple subunits: the membrane-bound heterodimer of NOX2 and p22phox, and cytosolic components p47phox (organizer subunit), p67phox (activator subunit), p40phox, and the small GTPase Rac [54]. NOX4 displays constitutive activity and primarily produces hydrogen peroxide (Hâ‚‚Oâ‚‚) rather than superoxide, functioning as an important signaling module in metabolic and fibrotic diseases [54] [55]. NOX5 and DUOX enzymes are uniquely regulated by calcium through EF-hand domains and do not require the classical cytosolic subunits [54].
Mitochondrial ROS Production and Cross-Talk with NOX
Mitochondrial complexes I (NADH:ubiquinone oxidoreductase) and III (ubiquinol:cytochrome c oxidoreductase) constitute the major sites of mitochondrial ROS (mtROS) production within the electron transport chain [3]. These complexes generate superoxide anion (O₂•â») and hydrogen peroxide (Hâ‚‚Oâ‚‚) from molecular oxygen [56] [3]. Additionally, mitochondria-localized proteins including NADPH oxidase-4 (NOX4), p66shc, and monoamine oxidases (MAO-A and MAO-B) contribute to mtROS production [3].
A critical concept in redox biology is the "ROS-induced ROS release" mechanism, which represents a feed-forward amplification pathway between different cellular ROS sources [56]. This cross-talk is particularly significant between NOX enzymes and mitochondria. Studies demonstrate that NOX-derived ROS can stimulate mitochondrial ROS production, and conversely, mtROS can activate NOX enzymes, creating a self-reinforcing cycle that sustains elevated ROS levels under pathological conditions [56] [57]. For instance, in serum withdrawal models, mitochondrial ROS production occurs within minutes, which subsequently activates NOX1 via the PI3K/Rac1 pathway, leading to sustained ROS accumulation and eventual cell death [57].
Table 2: Mitochondrial ROS Sources and Characteristics
| Source | Location | Primary ROS | Activation Triggers | Pathological Significance |
|---|---|---|---|---|
| Complex I | Mitochondrial matrix | O₂•⻠| Reverse electron flow, ischemia-reperfusion [56] [3] | Metabolic syndrome, cardiovascular disease [55] [3] |
| Complex III | Intermembrane space | O₂•⻠| Antimycin A, hypoxia [56] [3] | Angiogenesis, endothelial dysfunction [56] |
| p66Shc | Intermembrane space | Hâ‚‚Oâ‚‚ | Oxidative stress, apoptosis signals [3] | Cardiovascular aging, diabetes complications [3] |
| MAO-A/B | Outer membrane | Hâ‚‚Oâ‚‚ | Substrate availability (amines) [3] | Heart failure, neurodegenerative diseases [3] |
This synergistic relationship between NOX and mitochondrial ROS sources is particularly relevant in the context of metabolic syndrome and cardiovascular diseases, where coordinated ROS production from both sources promotes chronic inflammation, insulin resistance, and endothelial dysfunction [55]. In angiogenesis, the cross-talk between NOX and mitochondria organizes sustained redox signaling essential for VEGF-induced endothelial cell migration and proliferation [56].
NOX Isoform-Specific Inhibitors: Mechanisms and Applications
The development of isoform-specific NOX inhibitors represents a promising approach for targeted antioxidant therapy. Unlike broad-spectrum antioxidants, these compounds aim to selectively disrupt pathological ROS signaling while preserving physiological redox functions.
NOX1-Targeted Inhibitors
NOX1 is implicated in tumor proliferation, invasion, and angiogenesis [54]. The organizer subunit NOXO1 presents a potential target for disrupting NOX1 complex assembly and activity [54]. Experimental approaches include small interfering RNA (siRNA) targeting NOX1 expression and peptide inhibitors that disrupt the interaction between NOX1 and its regulatory subunits [54]. In colon cancer models, NOX1 suppression has been shown to reduce ROS-dependent tumor growth and metastatic potential [54].
NOX2 Inhibition Strategies
NOX2 activation requires precise assembly of multiple cytosolic components with the membrane-bound cytochrome complex [54]. Inhibitors targeting the interaction between p47phox and p22phox disrupt this assembly and prevent NOX2 activation [54]. Apocynin, a naturally occurring methoxy-substituted catechol, requires metabolic activation to inhibit NOX2 by preventing cytosolic subunit translocation [54]. Gp91ds-tat is a chimeric peptide that competitively inhibits the interaction between NOX2 and p47phox, showing efficacy in various vascular disease models [54].
NOX4-Specific Approaches
NOX4 produces Hâ‚‚Oâ‚‚ in a constitutive manner and depends on p22phox for ROS generation [54]. Unlike other NOX isoforms, NOX4 does not require classical cytosolic subunits for activity, complicating targeted inhibition [54]. GKT137831 is one of the first-in-class dual NOX1/4 inhibitors that has progressed to clinical trials for diabetic nephropathy and idiopathic pulmonary fibrosis [54]. NOX4 suppression has demonstrated beneficial effects in reducing fibrotic responses and tumor survival in preclinical models [54].
Emerging NOX5 Inhibitors
NOX5 is regulated by intracellular calcium levels and contains unique N-terminal EF-hand domains [54]. The absence of NOX5 in rodent genomes has complicated preclinical studies, but pharmacological inhibitors targeting the Ca²âº-binding domain or the NADPH-binding site are under development [54]. As NOX5 is implicated in cardiovascular diseases and inflammation, its specific inhibition holds therapeutic promise [54].
Diagram 1: NOX2 activation involves stimulus-induced phosphorylation of p47phox, which triggers translocation of cytosolic subunits to the membrane-bound NOX2/p22phox complex. Rac-GTP binding facilitates full activation and ROS production. Inhibition strategies include Apocynin (prevents subunit translocation), Gp91ds-tat (competitive inhibition), and siRNA approaches (gene silencing).
Mitochondrial-Targeted Therapeutics
Mitochondria-targeted antioxidants represent a significant advancement over conventional antioxidants by specifically delivering active compounds to the mitochondrial matrix, where they can effectively neutralize ROS at their primary source of production.
MitoQ and SS-Peptides
MitoQ is a ubiquitone derivative covalently linked to a triphenylphosphonium (TPP) cation, which enables its accumulation within mitochondria driven by the organelle's strong negative membrane potential [37] [38]. Once inside, MitoQ is reduced by the respiratory chain to its active antioxidant form, which effectively scavenges mitochondrial lipid peroxides [37]. In preclinical models of hypertension and metabolic syndrome, MitoQ has demonstrated efficacy in improving endothelial function and reducing oxidative stress markers [37].
Szeto-Schiller (SS) peptides are alternative mitochondria-targeted antioxidants that concentrate in the inner mitochondrial membrane independent of membrane potential [38]. These peptides typically contain alternating aromatic and basic amino acids that facilitate uptake and target cardiolipin, a phospholipid abundant in mitochondrial membranes [38]. SS-31 (elamipretide) has shown promise in protecting mitochondrial function and reducing ROS in models of ischemia-reperfusion injury and neurodegenerative diseases [38].
Mitochondria-Targeted SOD Mimetics
Manganese-based superoxide dismutase (SOD) mimetics such as MitoSOD and MitoTEMPO are designed to accumulate in mitochondria and catalytically convert superoxide to hydrogen peroxide [38]. These compounds contain TPP cations for mitochondrial targeting coupled to SOD-mimetic metal complexes [38]. In diabetic models, MitoTEMPO has been shown to improve insulin sensitivity and reduce complications including nephropathy through suppression of mtROS [38].
Therapeutic Applications in Disease Models
Mitochondria-targeted therapeutics have demonstrated particular promise in metabolic and cardiovascular diseases. In metabolic syndrome, MitoQ supplementation improved vascular function in resistant hypertension by reducing mtROS and enhancing nitric oxide bioavailability [37]. In diabetes, SS-31 peptides protected against diabetic nephropathy by preserving mitochondrial integrity and reducing oxidative damage in renal tissues [37]. For neurodegenerative diseases, mitochondrial-targeted antioxidants have shown neuroprotective effects by preventing mtROS-induced neuronal death and inflammation [58].
Diagram 2: Mitochondrial ROS production primarily occurs at Complexes I and III of the electron transport chain. mtROS can activate cytosolic NOX enzymes through "ROS-induced ROS release" mechanisms, creating an amplification cycle. Mitochondrial-targeted therapeutics including MitoQ, SS-peptides, and SOD mimetics specifically neutralize mtROS at their source of production.
Experimental Protocols for Redox Therapeutics
Assessing NOX Activity in Cellular Models
Protocol for NOX Activation and Inhibition Assay:
- Cell Culture and Treatment: Plate vascular smooth muscle cells (VSMCs) or endothelial cells at 70% confluence in appropriate growth media. Serum-starve cells for 24 hours to minimize basal activation. Pre-treat with NOX inhibitors (e.g., GKT137831 for NOX1/4, Apocynin for NOX2) at varying concentrations (1-50 μM) for 2 hours before stimulation with agonists such as angiotensin II (100 nM) or platelet-derived growth factor (20 ng/mL) for 30 minutes to 4 hours [54] [55].
ROS Detection: Load cells with 5 μM CM-H2DCFDA or dihydroethidium (DHE) for 30 minutes at 37°C. For specific superoxide detection, use HPLC-based quantification of 2-hydroxyethidium from DHE oxidation [37]. Analyze fluorescence by flow cytometry or fluorescence microscopy with appropriate filters (excitation/emission: 495/529 nm for DCF; 518/605 nm for ethidium) [37].
NOX Subunit Translocation: Fractionate cells into membrane and cytosolic components using differential centrifugation. Confirm purity of fractions with compartment-specific markers (Na+/K+ ATPase for membrane, GAPDH for cytosol). Detect translocation of p47phox (for NOX2) or NOXO1 (for NOX1) via Western blotting [54].
Gene Expression Analysis: Isolate total RNA and perform quantitative RT-PCR for NOX isoforms (NOX1-5, DUOX1-2) using isoform-specific primers. Reference to housekeeping genes (GAPDH, β-actin) [54].
Evaluating Mitochondrial ROS and Function
Protocol for Mitochondrial ROS Assessment and Therapeutic Testing:
- Mitochondrial Isolation: Homogenize tissues or collected cells in ice-cold mitochondrial isolation buffer (250 mM sucrose, 10 mM HEPES, 1 mM EGTA, pH 7.4). Centrifuge at 800 × g for 10 minutes at 4°C to remove nuclei and debris. Collect supernatant and centrifuge at 8,000 × g for 15 minutes to pellet mitochondria. Wash mitochondrial pellet twice and resuspend in isolation buffer [56] [3].
mtROS Measurement: Incubate isolated mitochondria (0.5 mg protein/mL) with 5 μM MitoSOX Red in respiration buffer (125 mM KCl, 10 mM HEPES, 5 mM MgCl2, 2 mM K2HPO4, pH 7.2) at 37°C. Add substrates (5 mM glutamate/5 mM malate for Complex I; 10 mM succinate for Complex II) to initiate respiration. Monitor MitoSOX fluorescence (excitation/emission: 510/580 nm) over time. Include inhibitors (e.g., 2 μM rotenone for Complex I, 10 μM antimycin A for Complex III) to identify ROS sources [56] [3].
Therapeutic Testing: Pre-incubate mitochondria with targeted antioxidants (MitoQ: 0.1-5 μM; SS-31: 0.1-10 μM; MitoTEMPO: 1-50 μM) for 15 minutes before adding substrates. Include untreated and vehicle controls [37] [38].
Functional Assessment: Measure mitochondrial membrane potential using 0.5 μM JC-1 dye (aggregate/monomer fluorescence ratio) or 100 nM tetramethylrhodamine methyl ester (TMRM). Assess oxygen consumption using a Clark-type electrode or Seahorse analyzer with sequential addition of substrates (malate/glutamate), ADP (1 mM), oligomycin (1 μg/mL), FCCP (1-4 μM), and antimycin A (2 μM) [56] [3].
In Vivo Models for Therapeutic Efficacy
Protocol for Animal Studies of NOX and Mitochondrial Inhibition:
- Animal Models: Utilize appropriate disease models: angiotensin II-infused mice (150-500 ng/kg/min for 2-4 weeks) for hypertension; db/db or high-fat diet-fed mice for metabolic syndrome; streptozotocin-induced diabetic mice for diabetes complications [37] [55].
Therapeutic Administration: Administer NOX inhibitors (GKT137831: 10-40 mg/kg/day orally) or mitochondrial-targeted antioxidants (MitoQ: 100-500 μM in drinking water; SS-31: 1-10 mg/kg/day IP) for 2-8 weeks based on disease model [37] [55].
Tissue Collection and Analysis: Euthanize animals and collect tissues (vessels, heart, kidney, liver). Snap-freeze portions for molecular studies, preserve portions in formalin for histology, and freshly isolate mitochondria from other portions [37] [55].
Outcome Measures: Assess blood pressure (tail-cuff or telemetry), glucose tolerance (IPGTT), and insulin tolerance (ITT). Measure oxidative stress markers: tissue malondialdehyde (MDA) by TBARS assay, protein carbonyls by DNPH method, 8-OHdG by ELISA for DNA oxidation [37]. Evaluate target engagement by measuring specific NOX isoform expression (Western blot, qPCR) and mitochondrial function (isolated mitochondria) [37] [55].
The Scientist's Toolkit: Research Reagents and Methodologies
Table 3: Essential Research Reagents for Redox Therapeutics Development
| Reagent/Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| NOX Inhibitors | GKT137831 (NOX1/4), Apocynin (NOX2), Gp91ds-tat (NOX2) | Isoform-specific targeting, mechanism studies [54] | Selectivity verification, off-target effects, species specificity |
| Mitochondrial-Targeted Antioxidants | MitoQ, SS-31 (Elamipretide), MitoTEMPO, MitoSOD | mtROS scavenging, mitochondrial function assessment [37] [38] | Membrane potential dependence, accumulation kinetics, effects on respiration |
| ROS Detection Probes | CM-H2DCFDA (general ROS), DHE (superoxide), MitoSOX Red (mtROS) | Quantifying ROS production, compartment-specific detection [37] | Specificity limitations, photostability, appropriate controls |
| Genetic Tools | siRNA/shRNA (NOX knockdown), CRISPR/Cas9 (NOX knockout), transgenic animals | Target validation, pathway analysis [54] | Isoform compensation, complete vs partial knockdown |
| Biomarker Assays | MDA-TBARS (lipid peroxidation), DNPH-protein carbonyls (protein oxidation), 8-OHdG-ELISA (DNA damage) [37] | Therapeutic efficacy assessment, oxidative damage quantification | Sample processing standardization, assay validation |
| Mitochondrial Function Assays | Seahorse Analyzer (respiration), JC-1/TMRM (membrane potential), Amplex Red (Hâ‚‚Oâ‚‚ production) [56] [3] | Mitochondrial bioenergetics assessment, therapeutic mechanism studies | Substrate optimization, appropriate normalization |
| Methyl 3-aminopyridine-4-carboxylate | Methyl 3-aminopyridine-4-carboxylate, CAS:55279-30-6, MF:C7H8N2O2, MW:152.15 g/mol | Chemical Reagent | Bench Chemicals |
| Benzyltributylammonium chloride | Benzyltributylammonium chloride, CAS:23616-79-7, MF:C19H34N.Cl, MW:311.9 g/mol | Chemical Reagent | Bench Chemicals |
Diagram 3: Systematic experimental workflow for developing redox therapeutics, progressing from target identification through validation, compound screening, efficacy assessment, and translational development, incorporating appropriate methodologies at each stage.
The targeted inhibition of ROS at its source represents a paradigm shift from non-specific antioxidant approaches toward precision redox medicine. NOX isoform-specific inhibitors and mitochondrial-targeted therapeutics offer the potential to disrupt pathological ROS signaling while preserving physiological redox functions. The continued development of these targeted strategies requires addressing several key challenges: improving isoform selectivity for NOX inhibitors, optimizing mitochondrial delivery efficiency, understanding tissue-specific differences in ROS signaling, and developing better biomarkers to assess target engagement and efficacy in clinical trials [1] [38].
Future directions in the field include the development of dual-targeting approaches that simultaneously address NOX and mitochondrial ROS sources, given their functional cross-talk in disease processes [56] [57]. Additionally, personalized approaches considering genetic polymorphisms in redox regulatory genes (such as NRF2 and KEAP1) may enhance therapeutic efficacy [37] [1]. As our understanding of the spatial and temporal dynamics of ROS signaling improves, next-generation therapeutics will likely incorporate sophisticated targeting mechanisms and combinatorial strategies to more effectively restore redox balance in chronic inflammatory diseases, cancer, and metabolic disorders [1] [38].
The perception of reactive oxygen species (ROS) has evolved from agents of cellular damage to secondary messengers that modify signaling proteins in both physiology and disease states, particularly in the context of inflammation [59]. Central to this regulatory mechanism are cysteine residues, which constitute 1–2% of the mammalian proteome and undergo versatile oxidative post-translational modifications (Ox-PTMs) that function as molecular switches to control protein function [60] [59]. These modifications enable a spatio-temporal control to signaling as redox-sensitive proteins traffic between subcellular compartments with different redox environments [59]. The unique chemistry of the sulfur-containing side chain allows cysteine thiol groups to participate in a diverse range of oxidative modifications, making them ideal sensors of cellular redox status and transducers of redox signals in inflammatory pathways [61] [62].
Cysteine residues play structural and regulatory roles as part of proteins or glutathione, contributing to maintain redox homeostasis and regulate signaling within and amongst cells [60]. The facile chemistry of cysteine stems from the electronic structure of its thiol group, which enables multiple oxidation states (from -2 to +6) leading to an array of redox modifications with distinct chemical properties that contribute to signaling specificity [59]. This malleable chemistry confers unique capabilities to cysteine residues for sensing and transducing signaling by modifying the structure and function of proteins, particularly in the regulation of innate immune responses and inflammatory processes [63] [36].
Fundamental Chemistry of Cysteine Oxidative Modifications
Determinants of Cysteine Reactivity
The reactivity of cysteine residues toward oxidants and electrophiles is strongly influenced by their microenvironment within the protein structure. Enzymes with active-site cysteine residues typically rely on the thiolate (deprotonated) form of the cysteine for activity, and reactivity toward substrates (and oxidants) is therefore enhanced by a microenvironment that perturbs the normally high pKa (~8.5) of cysteine thiols to a value at or lower than neutral pH [61]. In the case of the disulfide-bond oxidoreductase DsbA, the pKa drops as low as 3.5 [61]. Thus, although the vast majority of cysteine residues within cytoplasmic proteins are in the protonated form at physiological pH, the small subset within enzyme catalytic or regulatory sites are largely or fully ionized due to their low pKa values [61]. Aside from shifts in pKa, additional features that enhance reactivity include the presence of acid-base catalysts and specialized substrate-docking sites [61].
Cysteine reactivity is also context-specific because the acid dissociation constant (pKa) of a cysteine residue's thiol varies widely in proteins (pKa 3–9) depending on many factors including local pH, redox environment, proximity to metal centers and positively charged residues, and solvent access [59]. The local microenvironment affects protein thiol nucleophilicity which promotes spatially distinct, redox-mediated signaling [59]. This compartmentalization adds a temporal control to redox regulation as different intrinsic rates of formation, diffusibility and stability of ROS in various subcellular compartments influence modification dynamics [59].
Types of Cysteine Oxidative Post-Translational Modifications
Thiol groups in proteins can undergo both one- and two-electron chemistry to generate more oxidized products [61]. With one-electron oxidation, thiol groups are converted to thiyl radicals (R-S•), species that can participate in free radical chain reactions and can go on to form various oxidized species [61]. These species also have the potential to react directly with another radical, NO•, to form S-nitrosylated thiol groups and can participate in oxygen-dependent pathways that produce superoxide [61]. Thiolate reactions with H₂O₂, organic hydroperoxides, and peroxynitrite are two-electron processes that form the reactive oxidation product cysteine sulfenic acid, a metastable intermediate that is readily transformed into other oxidative products such as disulfide bonds (with other protein cysteines or glutathione) and sulfenamides [61].
Table 1: Major Types of Cysteine Oxidative Post-Translational Modifications
| Modification Type | Chemical Formula | Inducing Species | Reversibility | Functional Impact |
|---|---|---|---|---|
| S-sulfenylation | Cys-SOH | Hâ‚‚Oâ‚‚, ROS | Reversible | Intermediate for other modifications; regulatory switch |
| S-nitrosylation | Cys-SNO | NO, RNS | Reversible | Cardioprotection; regulates inflammation |
| Persulfidation | Cys-SSH | Hâ‚‚S, RSS | Reversible | Vasorelaxation; ER stress response |
| S-glutathionylation | Cys-SSG | ROS, GSSG | Reversible | Protection from over-oxidation; regulatory |
| Disulfide bond | Cys-S-S-Cys | Oxidation | Reversible | Structural stability; regulatory switches |
| Sulfinic acid | Cys-SOâ‚‚H | Hâ‚‚Oâ‚‚ | Reversible (Prxs) / Irreversible | Activates some enzymes (e.g., MMPs) |
| Sulfonic acid | Cys-SO₃H | H₂O₂ | Irreversible | Protein degradation/inactivation |
Sulfenic acids are also intermediates in the formation of more extensively oxidized and generally irreversible oxidative and nitrosative products (i.e., sulfinic acids, sulfinamides, sulfonic acids, and sulfonamides) [61]. Myeloperoxidase-generated oxidants such as hypohalous acids (hypochlorous acid and hypobromous acid) and N-chloramines also produce sulfenic acids and other reversibly or irreversibly oxidized products of cysteine residues [61]. While sulfenic acid, sulfenamide, S-nitrosothiol, and disulfide products are readily reduced to thiols by the prominent thioredoxin- and glutathione-dependent redox systems, sulfinamides and sulfonamides are characterized as crosslinks that are resistant to such reduction [61]. Sulfinic acids in one family of proteins, the peroxiredoxins (Prxs), can be repaired through an ATP-dependent process catalyzed by sulfiredoxins, but are likely to be irreversibly oxidized products in most proteins [61]. There is no known biological repair pathway for sulfonic acids [61].
Cysteine Redox Switches in Inflammation and Immunity
Redox Regulation of Innate Immune Cells
Redox signaling plays a central role in regulating macrophage and neutrophil function, integrating reactive oxygen species (ROS), reactive nitrogen species (RNS), and reactive sulfur species (RSS) to modulate innate immune responses [63] [36]. Reactive species modulate diverse cellular processes in phagocytes, including differentiation, metabolic adaptation, cytokine production, and cell death [63]. Antioxidant systems, including the glutathione and thioredoxin systems, play essential roles in maintaining redox balance, counteracting excessive oxidants, and preserving immune cell function [63]. Oxidative post-translational modifications of proteins, mainly on cysteine and methionine residues, act as redox switches that regulate innate immune cell function [63].
Dynamic redox modifications critically influence phagocyte metabolism, migration, phagocytosis, survival and communication with neighboring immune and non-immune cells, thereby controlling the response to infection as well as initiation and resolution of inflammation [63]. Additionally, other oxidized mediators, such as oxidized mitochondrial DNA and oxidized lipids, contribute to immune regulation and its dysregulation in inflammatory diseases [63]. Thus, redox signaling is tightly linked to both immune homeostasis and pathological inflammation [63]. This intricate regulation highlights the dual nature of reactive species in immune function - serving as both antimicrobial effector molecules and signaling mediators.
Key Redox-Sensitive Signaling Pathways in Inflammation
The nuclear factor-kappa B (NF-κB) pathway represents one of the most well-characterized redox-dependent inflammatory pathways [41]. NF-κB dimers are physiologically retained in the cytoplasm by IκB proteins, which can undergo phosphorylation and proteasomal degradation in response to OS and pro-inflammatory stimuli by activated IκB kinase (IKK) [41]. This event frees NF-κB to translocate into the nucleus, where it promotes the transcription of pro-inflammatory genes encoding cytokines, adhesion molecules, and enzymes like COX-2 and iNOS [41]. ROS can activate these redox-sensitive transcription factors, which in turn upregulate the expression of pro-inflammatory cytokines, perpetuating the inflammatory cascade [41].
In addition to NF-κB, mitogen-activated protein kinases (MAPKs), including ERK1/2, JNK, and p38 MAPK, are also activated in a redox-sensitive manner [41]. ROS inhibit MAPK phosphatases by oxidizing their catalytic cysteine residues, thereby prolonging MAPK signaling [41]. The p38 MAPK branch plays a key role in stabilizing mRNAs of inflammatory mediators and modulating chromatin accessibility via histone-modifying enzymes [41].
On the other hand, the nuclear factor erythroid 2-related factor 2 (Nrf2)–Keap1 pathway functions as a protective axis [41]. Nrf2 is normally bound to Keap1, which facilitates its ubiquitination and degradation, but oxidative stress modifies critical cysteine residues on Keap1, leading to the stabilization and nuclear translocation of Nrf2 [41]. Once in the nucleus, Nrf2 binds to antioxidant response elements (AREs) and induces the transcription of cytoprotective genes such as heme oxygenase-1 (HO-1), NAD(P)H quinone dehydrogenase 1 (NQO1), and glutamate–cysteine ligase catalytic subunit (GCLC) [41]. Nrf2 activity not only mitigates oxidative damage but also exerts anti-inflammatory effects by modulating macrophage polarization and suppressing NF-κB-driven transcription [41].
Diagram 1: Redox Regulation of Inflammatory Signaling Pathways. This diagram illustrates how reactive oxygen species (ROS) generated in response to inflammatory stimuli activate key signaling pathways including NF-κB, MAPK, and Nrf2, leading to either pro-inflammatory cytokine production or antioxidant responses.
Oxidative Stress and Reductive Stress in Inflammation
The relationship between oxidative stress and inflammation is not merely sequential but synergistic, establishing a pathogenic loop that sustains chronic inflammation [41]. These dynamics have been extensively documented in several pathological conditions, including atherosclerosis, neurodegeneration, non-alcoholic steatohepatitis, inflammatory bowel diseases, and rheumatoid arthritis [41]. Elevated ROS levels influence the redox-sensitive activity of transcription factors that drive the expression of adhesion molecules, cytokines, chemokines, and matrix metalloproteinases (MMPs), thereby amplifying the tissue recruitment of immune cells and sustaining inflammatory circuits [41].
While the pro-inflammatory role of oxidative stress (OS) is well established, the impact of reductive stress (RS)—a condition marked by excessive reducing equivalents such as NADH, NADPH, and reduced glutathione (GSH)—remains underappreciated [41]. RS arises from an overabundance of reducing agents, leading to an excessively reduced cellular state characterized by elevated NADH/NAD+ and NADPH/NADP+ ratios, an increased reduced/oxidized glutathione (GSH/GSSG) ratio, and the persistent activation of antioxidant systems [41]. This imbalance can impair the formation of disulfide bonds in proteins, alter cellular signaling pathways, and compromise mitochondrial function [41]. Chronic RS has been associated with the pathophysiology of various inflammation-related diseases, including certain cardiomyopathies, neurodegenerative disorders, and metabolic syndromes [41].
Thiol-Based Drug Design: Mechanisms and Applications
Molecular Mechanisms of Thiol-Based Drugs
Thiol-based drugs represent a class of therapeutic agents that exploit the redox chemistry of cysteine residues to achieve their pharmacological effects. These drugs contain at least one functional thiol group that can exist in both protonated (-SH) and deprotonated (-S−) forms, with their reactivity influenced by the pKa of the thiol group [64]. Alkyl thiols are weakly acidic with pKa > 9, with a low fraction of thiolate present at physiologic pH of 7.4 [64]. Thiol compounds with a lower pKa (i.e., approaching 7.4) will have more thiolate species at physiologic conditions and may be more potent in various therapeutic applications [64].
The primary mechanism of action for many thiol-based drugs involves disruption of disulfide bonds in proteins through thiol-disulfide exchange reactions [64] [65]. In the case of N-acetylcysteine (NAC), a thiol-based drug with a free sulfhydryl group (-SH), it breaks the disulfide bonds (S-S) that connect mucin proteins by donating electrons to the thiol groups of mucin monomer cysteine (Cys) residues [65]. This pharmacological effect results in the depolymerization of mucin and a reduction in mucus viscosity, explaining its use as a mucolytic agent [65]. Similar mechanisms are likely involved in the antiviral effects of thiol drugs against viruses like SARS-CoV-2, where they may cleave cystines in the receptor binding domain of the spike glycoprotein to disrupt its binding to ACE2 [64].
Beyond their direct chemical actions, thiol-based drugs also possess potent antioxidant and anti-inflammatory properties [64] [65]. They can scavenge reactive oxygen species (ROS) and interrupt ROS-mediated inflammatory cascades, including pathways for NF-κB activation and cytokine and chemokine production [64]. Some thiol drugs can also inhibit the activity of myeloperoxidase, a mediator of inflammation and oxidative stress [64]. Cysteamine, for example, has an expanded range of anti-inflammatory activities related to the inhibition of transglutaminase 2 and somatostatin [64].
Major Thiol-Based Drugs and Their Therapeutic Applications
Table 2: Therapeutic Thiol-Based Drugs and Their Applications
| Drug Name | Chemical Properties | Primary Mechanisms | Therapeutic Applications |
|---|---|---|---|
| N-acetylcysteine (NAC) | Free sulfhydryl group, pKa ~9.5 | Mucolytic (disrupts disulfide bonds), antioxidant, glutathione precursor | COPD, acetaminophen poisoning, antioxidant therapy |
| Cysteamine | Aminothiol, low pKa | Antioxidant, anti-inflammatory, inhibits transglutaminase 2 and somatostatin | Cystinosis, neurodegenerative diseases, inflammatory conditions |
| Erdosteine | Thiol derivative (metabolized to active form) | Mucolytic, antioxidant, anti-inflammatory | COPD, bronchial inflammation, respiratory infections |
| S-carboxymethyl-L-cysteine (S-CMC) | Thioether carboxylate | Mucolytic, anti-inflammatory | Chronic bronchitis, COPD, respiratory conditions with mucus hypersecretion |
| Amifostine (WR-1065) | Organic thiophosphate (metabolized to thiol) | Cytoprotective, free radical scavenger | Radioprotective agent, reduces toxicity of chemotherapy |
| Bucillamine | Dithiol compound | Antioxidant, anti-inflammatory, immunomodulatory | Rheumatoid arthritis, inflammatory conditions |
Thiol-based drugs are usually given orally, but they may be more effective when administered by inhalation because they can directly act on the airway, a possibility that has several advantages such as reaching the correct anatomical target at high concentrations, thus avoiding drug metabolism by the liver and intestine, and also fast onset, a lower drug dose, and reduced systemic side effects [65]. However, there is little literature on inhaled thiol-based drugs, which is limited in any case to NAC [65]. The recent Global Initiative for Chronic Obstructive Lung Diseases (GOLD 2019) report has listed NAC, S-CMC, and erdosteine as additional therapies to consider in the treatment of COPD because recent data have shown that some of these drugs (erdosteine and NAC) can reduce exacerbations in patients with COPD, even in patients taking inhaled corticosteroids [65].
Antiviral Applications of Thiol-Based Drugs
Emerging research has revealed potential antiviral applications for thiol-based drugs, particularly against SARS-CoV-2. Studies have found that multiple thiol drugs inhibit SARS-2-S binding to ACE2 and virus infection [64]. The most potent drugs were effective in the low millimolar range, and ICâ‚…â‚€ values followed the order of their cystine cleavage rates and lower thiol pKa values [64]. This suggests that the reactive or cystine cleaving form of a thiol is its deprotonated (thiolate) form, and compounds with pKa values approaching physiological pH will have more thiolate species and potentially greater potency [64].
In vivo studies with cysteamine in hamsters infected with SARS-CoV-2 demonstrated that while it did not decrease lung viral infection, it significantly decreased lung neutrophilic inflammation and alveolar hemorrhage [64]. This suggests that the concentration of cysteamine achieved in the lungs with intraperitoneal delivery was insufficient for antiviral effects but sufficient for anti-inflammatory effects [64]. These findings provide rationale for future studies to test if direct (aerosol) delivery of thiol drugs to the airways might also result in antiviral effects [64].
Experimental Approaches and Research Methodologies
Detection and Characterization of Cysteine Ox-PTMs
Advancing our understanding of cysteine redox switches requires sophisticated methodological approaches for detecting and characterizing various oxidative post-translational modifications. With the increasing study of Hâ‚‚Oâ‚‚ signal transduction, proteomics tools for identifying S-sulfenylation have been implemented and optimized [66]. The initial workflow is to block free thiols in the extracted proteome, reduce oxidized Cys, and finally label the newly formed thiols [66]. However, these indirect proteomic methods can only be used to identify cysteine sulfenic acid (Cys-SOH) in vitro, albeit with some limitations [66].
There are two main methods for identifying S-sulfenylated proteins selectively captured in Arabidopsis thaliana that have broader applications [66]. The first method involves the use of YAP1-based probes that were developed to capture S-sulfenylated proteins, and a YAP1-based hyposulfenylated capture method coupled with a tandem affinity purification tag has been implemented [66]. Approximately 100 S-sulfenylated proteins were identified in early and late oxidative stress reactions using this approach, including 67 that had not been previously identified as being involved in OxiPTMs [66].
The other method involves a chemoselective DYn-2 probe based on alkynyl functionalization, which was developed to enable capturing information on the multiple redox changes of proteins that could not be obtained using previous analysis methods of protein-level capture [66]. DYn-2 marks S-sulfenylated proteins in complete cells [66]. Cell proteins are digested with trypsin, the labeled peptide is combined with azide biotin by a CuAAC reaction, and the peptide is affinity-purified on streptavidin resin, and is ultimately released through the light-splitting action of a biotin linker [66]. The released DYn-2-modified peptide is then analyzed by mass spectrometry-based proteomics [66]. Subsequently, utilizing an enhanced 1-(pent-4-yn-1-yl)-1H-benzo[c][1,2] thiazin-4(3H)-one 2,2-dioxide (BTD)-derived probe, which exhibited superior reactivity compared to the DYn-2 probe, facilitated the comprehensive identification of 1394 proteins susceptible to S-sulfenylation [66]. This achievement represented a substantial enlargement of the known S-sulfenylated proteome, surpassing the previous tally of 200 proteins [66].
Diagram 2: Experimental Workflow for Detecting S-Sulfenylated Proteins. This diagram outlines the key steps in identifying protein S-sulfenylation, from initial sample preparation to mass spectrometry-based analysis.
Assessment of Thiol Drug Efficacy
To explore the antiviral effects of thiol drugs in COVID-19, researchers have employed ACE-2 binding assays and cell entry assays utilizing reporter pseudoviruses and authentic SARS-CoV-2 viruses [64]. These approaches allow for the evaluation of drug potency in the low millimolar range, with ICâ‚…â‚€ values following the order of their cystine cleavage rates and lower thiol pKa values [64]. For in vivo assessment, animal models such as hamsters infected with SARS-CoV-2 can be used to test the effects of thiol drugs on both viral infection and inflammatory parameters [64].
Standardized assays for evaluating the mucolytic activity of thiol drugs include viscometry and rheology measurements of mucus samples, assessment of mucociliary clearance in ex vivo models, and evaluation of sputum properties in clinical studies [65]. For antioxidant effects, measures of oxidative stress markers such as glutathione levels, lipid peroxidation products, protein carbonylation, and DNA oxidation products provide quantitative assessment of drug efficacy [65]. Anti-inflammatory properties can be evaluated through measurement of cytokine production, NF-κB activation assays, and assessment of inflammatory cell infiltration in animal models of inflammation [65].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Studying Cysteine Redox Modifications
| Reagent/Category | Specific Examples | Primary Function | Applications |
|---|---|---|---|
| Thiol-blocking agents | Iodoacetamide, N-ethylmaleimide | Alkylate free thiols to prevent further reactions | Sample preparation for redox proteomics |
| Chemoselective probes | DYn-2, BTD-based probes, YAP1-based probes | Selective labeling of oxidized cysteine species | Detection of specific Ox-PTMs in cells and tissues |
| Reduction systems | DTT, TCEP, glutathione reductase | Reduce disulfide bonds and other reversible Ox-PTMs | Reversibility studies and sample processing |
| Oxidant sources | Hâ‚‚Oâ‚‚, peroxynitrite donors, NO donors | Induce specific oxidative modifications | Controlled oxidation experiments in model systems |
| Affinity purification resins | Streptavidin beads, antibody-conjugated resins | Isolation of labeled proteins/peptides | Enrichment of modified species for proteomics |
| Detection antibodies | Anti-glutathione, anti-nitrotyrosine | Immunological detection of specific Ox-PTMs | Western blot, immunohistochemistry |
| Mass spectrometry standards | Isotope-labeled peptides, TMT/iTRAX reagents | Quantification of modified peptides | Quantitative redox proteomics |
| Cell-permeable ROS sensors | DCFH-DA, MitoSOX, roGFP | Measure intracellular ROS levels | Live-cell imaging and flow cytometry |
| 2,4-Dihydroxyquinoline | 2,4-Quinolinediol (CAS 86-95-3) - High-Purity Research Grade | 2,4-Quinolinediol for research. Explore its role in bacterial pathogenicity and as a key hydroxyquinolone metabolite. For Research Use Only. Not for human use. | Bench Chemicals |
| (2-Aminoethyl)phosphonic acid | (2-Aminoethyl)phosphonic acid, CAS:2041-14-7, MF:C2H8NO3P, MW:125.06 g/mol | Chemical Reagent | Bench Chemicals |
The study of cysteine redox switches and the development of thiol-based therapeutics represent a rapidly advancing frontier in biomedical research, with significant implications for understanding and treating inflammatory diseases. The regulatory functions performed by protein cysteine residues provide a framework for understanding how mutation and/or (in)activation of this key amino acid can cause disease [60]. In many genetic diseases and cancer, mutations can either directly target a cysteine or affect residues that contribute to maintain optimal cysteine pKa, accessibility, and/or reactivity [60].
Future research directions should focus on developing a more comprehensive understanding of the detailed biochemistry and biological roles of cysteine and glutathione in living systems [65]. Additionally, there is a need to enlarge our knowledge about free radicals or ROS to establish clinical therapeutic strategies regarding the use of antioxidant regimens in medicine [65]. For thiol-based drugs specifically, crucial questions remain regarding whether their clinical benefits are related to their mucolytic, antioxidant, anti-inflammatory, or antimicrobial activities, or to all of these properties combined [65].
The emerging concept of reductive stress as a contributor to inflammatory diseases suggests that therapeutic approaches should shift from antioxidant-centric treatments to approaches that consider the bidirectional nature of redox dysregulation [41]. This framework may inform the development of more precise interventions for inflammation-related diseases that target specific redox-sensitive nodes in inflammatory signaling pathways rather than broadly suppressing oxidative processes [41]. As our tools for detecting and quantifying specific cysteine oxidative modifications continue to improve, and as we develop more sophisticated thiol-based therapeutic agents, we move closer to harnessing the full potential of cysteine redox chemistry for treating inflammatory diseases and improving human health.
Redox signaling, encompassing the regulated generation and metabolism of reactive oxygen species (ROS), reactive nitrogen species (RNS), and reactive sulfur species (RSS), forms a critical biochemical layer controlling cellular homeostasis and immune function [63] [36]. In physiological conditions, these reactive molecules act as signaling messengers, modulating processes from vascular tone to insulin signaling [3]. However, dysregulated redox balance drives a cascade of pathological events, including mitochondrial dysfunction, chronic inflammation, and impaired autophagy, which are common threads linking cardiovascular, neurodegenerative, and metabolic diseases [3] [67]. This whitepaper examines disease-specific therapeutic strategies through the lens of redox biology, highlighting how targeting these interconnected pathways offers promising avenues for intervention. The intricate interplay between oxidative stress and inflammatory pathways creates a self-amplifying cycle that accelerates tissue damage across organ systems, making the restoration of redox equilibrium a central goal of modern therapeutic development [63] [3].
Cardiovascular Protection: Targeting Inflammation and Metabolic Pathways
Cardiovascular disease (CVD) management is undergoing a transformative shift beyond conventional lipid-lowering approaches, with new strategies targeting underlying inflammatory and metabolic drivers [68] [3]. Dysregulated redox signaling and subsequent mitochondrial dysfunction are now recognized as central mechanisms in the pathogenesis of atherosclerosis, myocardial infarction, and heart failure [3]. The failure of non-specific antioxidant trials has underscored the necessity for targeted interventions that modulate specific redox-sensitive pathways without disrupting essential ROS-dependent signaling [3].
Table 1: Emerging Cardiovascular Therapeutic Strategies and Mechanisms
| Therapeutic Strategy | Key Molecular Targets | Physiological Effects | Clinical Evidence |
|---|---|---|---|
| GLP-1 Receptor Agonists (e.g., Semaglutide, Tirzepatide) | GLP-1 Receptors | 20% MACE risk reduction; improved endothelial function; cardiac tissue protection [68] | SELECT trial: Cardiovascular benefit in patients with obesity and pre-existing CVD [68] |
| Inflammation Pathway Inhibitors (e.g., Canakinumab) | IL-1β | Reduced cardiovascular events independent of lipid lowering [68] | CANTOS trial: Significant MACE reduction in patients with existing heart disease [68] |
| CRISPR-Based Gene Editing (e.g., Nexigalan ziclumeran) | TTR Gene | Reduces serum transthyretin (89% reduction at 28 days) for ATTR-CM treatment [68] | Phase 1 trial: Promising reduction in TTR levels; Phase 3 MAGNITUDE trial ongoing [68] |
| Small Interfering RNA (siRNA) Therapies (e.g., Patisiran, Vutrisiran) | TTR mRNA | Reduces TTR protein production; slows amyloid fibril accumulation [68] | HELIOS-B: Vutrisiran led to lower risk of death and recurrent cardiovascular events (HR, 0.72) [68] |
The spatiotemporal production of ROS is crucial in determining its pathological impact, with mitochondrial complexes I and III, NADPH oxidases (NOXs), and xanthine oxidase identified as key contributors to redox imbalance [3]. Emerging evidence suggests that modulating immune responses through control of redox-sensitive pathways in myeloid cells, including macrophage polarization and autophagic activity, is crucial for determining the severity and resolution of cardiac and vascular inflammation [3]. Furthermore, the cardioprotective effects of hydrogen sulfide (H2S) and other RSS donors are being explored for their ability to improve mitochondrial function via post-translational modifications such as S-sulfhydration, offering novel therapeutic avenues for heart failure management [3].
Experimental Protocols for Cardiovascular Redox Biology
Protocol 1: Assessing Mitochondrial ROS Production in Cardiac Tissue
- Tissue Preparation: Fresh cardiac tissue samples are homogenized in ice-cold mitochondrial isolation buffer (250 mM sucrose, 10 mM HEPES, 1 mM EGTA, pH 7.4). Mitochondria are isolated via differential centrifugation [3].
- ROS Measurement: Load mitochondria with 5 μM MitoSOX Red dye in respiration buffer (125 mM KCl, 10 mM HEPES, 5 mM MgCl2, 2 mM K2HPO4, pH 7.4). Incubate for 30 minutes at 37°C. Add complex I substrates (5 mM glutamate/5 mM malate) or complex II substrate (5 mM succinate) to initiate ROS production [3].
- Data Acquisition: Monitor fluorescence (excitation/emission: 510/580 nm) using a plate reader or fluorometer. Validate with specific inhibitors (e.g., rotenone for complex I, antimycin A for complex III) [3].
Protocol 2: Evaluating Redox-Sensitive Inflammasome Activation in Macrophages
- Cell Culture: Differentiate THP-1 monocytes to macrophages with 100 nM PMA for 48 hours. Pre-treat with experimental compounds (e.g., NOX inhibitors, ROS scavengers) for 2 hours [63] [3].
- Stimulation: Activate NLRP3 inflammasome with 500 μM ATP for 30 minutes or nigericin (10 μM) for 45 minutes following priming with 100 ng/mL LPS for 3 hours [63].
- Analysis: Measure IL-1β secretion via ELISA. Assess caspase-1 activation using Western blot (anti-caspase-1 antibody). Quantify mitochondrial ROS using MitoSOX Red as above [63] [3].
Research Reagent Solutions for Cardiovascular Investigations
Table 2: Essential Research Reagents for Cardiovascular Redox Studies
| Research Reagent | Function/Application | Key Examples |
|---|---|---|
| MitoSOX Red | Selective detection of mitochondrial superoxide | Validation of mtROS sources using substrate/inhibitor combinations [3] |
| NADPH Oxidase Inhibitors | Target specific ROS sources (e.g., NOX2, NOX4) | VAS2870 (pan-NOX), GKT137831 (NOX1/4); elucidate contribution of cytoROS vs. mtROS [3] |
| H2S Donors | Investigate RSS-mediated cardioprotection | Sodium hydrosulfide (NaHS), S-propyl-L-cysteine; study S-sulfhydration of target proteins like CaMKII [3] |
| SIRT Activators | Modulate sirtuin pathway for mitochondrial biogenesis | Resveratrol, SRT2104; assess impact on endothelial function and autophagy [3] [67] |
Figure 1: Redox Signaling in Cardiovascular Disease Pathogenesis and Intervention. This diagram illustrates how dysregulated redox signaling from multiple sources drives cellular dysfunction in the vasculature, leading to atherosclerosis, and highlights the points of intervention for emerging therapeutic strategies.
Neurodegeneration: Integrated Strategies Against Age-Related Pathology
Neurodegenerative diseases (NDDs) exemplify the consequences of chronic redox imbalance within the complex adaptive system of the aging brain [67]. The risk of developing Alzheimer's disease (AD) increases dramatically with age, from 5% among individuals aged 65-74 to 33% after age 85, creating an urgent need for effective interventions [67]. Aging introduces multiple biological changes that converge on neurodegeneration, including inefficient DNA repair, protein buildup, impaired nutrient sensing, oxidative stress, and mitochondrial dysfunction [67]. In the brain, these processes manifest as excessive activation of immune cells (glia), abnormal neural circuit activity, and accumulation of toxic proteins such as amyloid-beta (Aβ), hyperphosphorylated tau, and α-synuclein (α-syn) [69] [67]. These proteins subsequently trigger neuroinflammation, further exacerbating mitochondrial dysfunction and oxidative stress in a vicious cycle [67].
Advanced molecular imaging techniques, particularly positron emission tomography (PET), have revolutionized our understanding of these pathological processes by providing quantitative tracking of physiological changes over time [69]. PET tracers targeting metabolism, amyloid, tau, neuroinflammation, and neurotransmitter systems provide critical insights into TBI-induced neurodegeneration and serve as biomarkers for therapeutic development [69].
Table 3: PET Imaging Tracers for Tracking Neurodegenerative Pathways
| PET Tracer Category | Specific Tracers | Molecular Targets | Pathophysiological Insights |
|---|---|---|---|
| Metabolic | 18F-fluorodeoxyglucose (FDG) | Regional glucose metabolism | Neuronal viability; patterns of hypometabolism/hypermetabolism post-TBI [69] |
| Proteinopathic | Amyloid tracers (e.g., Pittsburgh compound B), Tau tracers (e.g., Flortaucipir) | Aβ plaques, Neurofibrillary tangles | Protein aggregation and distribution; relationship to cognitive decline [69] |
| Neuroinflammatory | TSPO tracers (e.g., PK11195) | Translocator protein on activated microglia | Chronic neuroinflammatory responses; microglial activation states [69] |
| Neurotransmitter | Various dopamine, serotonin tracers | Dopaminergic, serotonergic systems | Neurotransmitter dysregulation following injury [69] |
Experimental Protocols for Neurodegeneration Research
Protocol 1: PET Imaging for Neuroinflammation Assessment in Rodent Models
- Animal Preparation: Anesthetize animals with isoflurane (2-3% for induction, 1-2% for maintenance). Maintain body temperature at 37°C throughout the procedure [69].
- Radiotracer Injection: Administer 3.7-7.4 MBq of [11C]PK11195 or equivalent TSPO tracer via tail vein. Note exact time and dose for quantitative analysis [69].
- Image Acquisition: Position animal in microPET scanner. Begin 60-minute dynamic acquisition immediately after tracer injection. Follow with CT scan for anatomical co-registration [69].
- Data Analysis: Reconstruct images using ordered-subset expectation maximization (OSEM) algorithm. Define regions of interest (ROIs) using co-registered CT/MRI atlas. Calculate standardized uptake value (SUV) or binding potential (BPND) using reference tissue models [69].
Protocol 2: Assessing Cognitive Outcomes in Preclinical Neurodegeneration Models
- Morris Water Maze Protocol: Conduct over 5-6 days with a pool diameter of 120-150 cm. Perform 4 trials per day with 60-second maximum swim time and 30-minute inter-trial intervals [67].
- Probe Trial: On day 6, remove the platform and record swim paths for 60 seconds. Measure time spent in target quadrant, platform crossings, and latency to first platform crossing [67].
- Data Interpretation: Compare treatment groups using ANOVA with post-hoc testing. Impaired learning manifests as longer escape latencies during training and fewer platform crossings during probe trial [67].
Research Reagent Solutions for Neurodegeneration Studies
Table 4: Essential Research Reagents for Neurodegeneration Investigations
| Research Reagent | Function/Application | Key Examples |
|---|---|---|
| PET Radiotracers | Target-specific molecular imaging | [11C]PK11195 (TSPO), [18F]Flortaucipir (tau), [11C]PIB (Aβ); quantify protein pathology and neuroinflammation in vivo [69] |
| Senolytic Compounds | Selective clearance of senescent cells | Dasatinib + Quercetin (D+Q), Fisetin; assess impact on glial senescence and neuroinflammation [67] |
| mTOR Pathway Modulators | Regulate autophagy and protein clearance | Rapamycin (inhibitor); evaluate enhancement of clearance of aggregated proteins (Aβ, tau) [67] |
| SIRT Activators | Modulate mitochondrial function and stress resistance | Resveratrol, NAD+ precursors; investigate impact on neuronal resilience and cognitive function [67] |
Figure 2: Integrated Anti-Aging Strategy for Neurodegeneration. This diagram illustrates how fundamental aging processes drive brain pathology through interconnected pathways, and highlights how multi-targeted therapeutic interventions can disrupt this cycle to prevent neuronal loss.
Metabolic Disorders: Systemic Approaches for Multiorgan Health
Metabolic disorders represent a cascade of interrelated conditions driven by sustained positive energy balance, ectopic fat storage, and resultant insulin resistance and systemic inflammation [70]. The European Atherosclerosis Society (EAS) has recently proposed a clinical staging framework that conceptualizes systemic metabolic disorders as a progressive multisystem condition, with stages ranging from metabolic abnormalities without organ damage (Stage 1) to late-stage organ disease (Stage 3) [70]. Analysis of the UK Biobank population revealed that 58% exhibit Stage 1 and a further 19% exhibit Stage 2 systemic metabolic disorders, with Stage 2 conferring a 49% increase in all-cause mortality after adjustment for age and sex [70]. This underscores the critical importance of early intervention before irreversible organ damage occurs.
The pathophysiology of metabolic disorders is intimately connected with redox imbalance, as nutrient excess promotes mitochondrial overload and excessive ROS production in metabolic tissues, initiating inflammatory cascades that further disrupt metabolic homeostasis [3] [70]. The interplay between oxidative stress and inflammation creates a self-reinforcing cycle that accelerates disease progression across multiple organs, including liver, pancreas, heart, and kidneys [71] [3]. This understanding has prompted a shift toward therapeutic strategies that target the systemic nature of metabolic dysregulation rather than individual disease manifestations.
Table 5: Clinical Staging and Management of Systemic Metabolic Disorders
| Disease Stage | Clinical Criteria | Recommended Management Strategies | Therapeutic Goals |
|---|---|---|---|
| Stage 1: Early Metabolic Abnormalities | Excess adiposity + ≥1 metabolic risk factor (e.g., elevated triglycerides, blood pressure, fasting glucose) without organ damage [70] | Lifestyle modification (cornerstone); consider GLP-1 RAs for multiple risk factors [70] | Prevent progression to organ damage; reduce multiple metabolic risk factors [70] |
| Stage 2: Early Organ Damage | Stage 1 criteria + evidence of subclinical organ damage (e.g., fatty liver, microalbuminuria, diastolic dysfunction) [70] | Intensive lifestyle intervention; pharmacotherapy for individual disorders; GLP-1 RAs for multi-organ benefit [70] | Halt progression of organ damage; reverse early pathological changes [70] |
| Stage 3: Late-Stage Organ Disease | Stage 2 criteria + established organ disease (e.g., type 2 diabetes, ASCVD, heart failure, CKD) [70] | Comprehensive multi-system pharmacotherapy; metabolic surgery in severe cases [70] | Manage established disease; prevent complications and further multi-organ injury [70] |
Experimental Protocols for Metabolic Research
Protocol 1: Assessing Systemic Insulin Sensitivity In Vivo
- Animal Preparation: House mice/rats on standardized diet. Fast animals for 5-6 hours (rodents) or overnight (larger species) with free access to water [72].
- Insulin Tolerance Test (ITT): Measure baseline blood glucose (time 0). Administer human regular insulin (0.75 U/kg for mice, 0.5 U/kg for rats) via intraperitoneal injection. Collect blood samples at 15, 30, 60, and 120 minutes post-injection for glucose measurement [72].
- Data Analysis: Calculate area under the curve (AUC) for glucose during ITT. Express results as percentage of baseline glucose or rate of glucose disappearance (Kitt) [72].
Protocol 2: Evaluating Oxidative Stress in Metabolic Tissues
- Tissue Collection: Rapidly harvest tissues (liver, skeletal muscle, adipose) and freeze in liquid N2. Store at -80°C until analysis [3].
- Lipid Peroxidation Assay (MDA-TBA Adduct): Homogenize 100 mg tissue in 1 mL RIPA buffer containing BHT (0.01%). Centrifuge at 10,000 × g for 10 minutes at 4°C. Incubate 200 μL supernatant with 600 μL TBA reagent (0.375% TBA, 15% TCA, 0.25 N HCl) for 15 minutes at 95°C [3].
- Measurement: Cool samples and measure fluorescence (excitation/emission: 532/553 nm). Calculate malondialdehyde (MDA) equivalents using tetraethoxypropane standard curve. Normalize to protein content [3].
Research Reagent Solutions for Metabolic Studies
Table 6: Essential Research Reagents for Metabolic Disorder Investigations
| Research Reagent | Function/Application | Key Examples |
|---|---|---|
| GLP-1 Receptor Agonists | Investigate pleiotropic benefits beyond glucose control | Semaglutide, Tirzepatide; study effects on hepatic steatosis, cardiovascular function, and renal protection [68] [70] |
| SGLT2 Inhibitors | Target renal glucose reabsorption | Empagliflozin, Dapagliflozin; explore mechanisms of renoprotection and hemodynamic benefits [71] |
| Metabolic Cage Systems | Comprehensive energy balance assessment | Simultaneous measurement of O2 consumption, CO2 production, food/water intake, locomotor activity; calculate RER and energy expenditure [70] |
| Antibody Panels for Flow Cytometry | Immune-metabolic profiling in metabolic tissues | Anti-F4/80 (macrophages), CD11c (M1), CD206 (M2); assess adipose tissue inflammation and macrophage polarization [63] [3] |
Figure 3: Progressive Staging of Systemic Metabolic Disorders. This diagram illustrates the pathophysiological cascade from initial energy imbalance through to end-organ disease, aligned with the clinical staging framework proposed by the European Atherosclerosis Society. The progression from Stage 1 to Stage 3 highlights the importance of early intervention to prevent irreversible multi-organ damage.
The traditional view of oxidative stress as merely a detrimental state to be neutralized by broad-spectrum antioxidants has undergone a fundamental revision. Precision redox represents a paradigm shift in redox biology and medicine, emphasizing that redox status must be considered in the context of specific species, locations, timing, levels, and molecular targets rather than as a global cellular condition [73]. This approach recognizes that reactive oxygen and nitrogen species (ROS/RNS) function as crucial signaling molecules in physiological processes, and their dysregulation—in both oxidative and reductive directions—can drive disease pathogenesis [4] [1]. The failure of numerous clinical trials using non-specific antioxidants underscores the limitations of the traditional approach and highlights the necessity for precision strategies that account for the complex, context-dependent nature of redox signaling [73] [3].
Within inflammation and disease research, precision redox medicine offers a framework for understanding how redox imbalances manifest differently across tissues, cellular compartments, and disease stages. The emerging understanding of reductive stress (RS)—a condition marked by excessive reducing equivalents—as potentially detrimental as oxidative stress (OS) further illustrates the complexity of redox homeostasis [4]. This in-depth technical guide examines the core principles, methodologies, and therapeutic applications of precision redox medicine, providing researchers and drug development professionals with the tools necessary to advance this transformative field.
Fundamental Principles of Precision Redox
The "5R" Framework of Precision Redox
The precision redox framework is built upon the "5R" principle, which provides a systematic approach for investigating and targeting redox processes in health and disease [73]:
- Right Species: Reactive species exhibit diverse chemical properties and biological activities. The major ROS/RNS species include hydrogen peroxide (Hâ‚‚Oâ‚‚), hydroxyl radicals (·OH), superoxide radicals (Oâ‚‚â»), nitric oxide (NO), and peroxynitrite (ONOOâ»), each with distinct signaling and damaging potential [73] [74].
- Right Place: Redox status varies significantly between subcellular compartments. Mitochondria maintain a relatively reduced environment (-300 mV for GSH/GSSG), while the endoplasmic reticulum exhibits a more oxidized state (-150 mV) [73].
- Right Time: Redox status demonstrates dynamic fluctuations across circadian cycles, cell division phases, and disease progression timelines [73].
- Right Level: Physiological ROS/RNS concentrations mediate essential signaling functions, while pathological deviations in either direction disrupt homeostasis [4] [1].
- Right Target: Specific cysteine residues and other redox-sensitive motifs in proteins serve as molecular switches that regulate function through post-translational modifications [36] [1].
Spatiotemporal Regulation of Redox Status
Cellular redox status is precisely regulated across spatial and temporal dimensions, creating specialized microenvironments that influence protein function and signaling pathways. The table below summarizes key aspects of redox compartmentalization:
Table 1: Subcellular Compartmentalization of Redox Indicators
| Cellular Compartment | Redox Potential (Eh) | Key Redox Couples/Proteins | Physiological Significance |
|---|---|---|---|
| Mitochondria | -300 mV | GSH/GSSG, Trx2 | Energy metabolism, apoptosis regulation |
| Cytoplasm | -220 to -260 mV | GSH/GSSG, Trx1 | General cellular signaling, proliferation |
| Nucleus | -300 mV | Trx1(-SH)â‚‚/SS | Gene expression, DNA repair |
| Endoplasmic Reticulum | -150 mV | Ero1, PDI | Oxidative protein folding, quality control |
| Lysosome | -240 mV | GSH/GSSG | Macromolecular degradation |
| Cell Membrane | -130 to -153 mV | GSH/GSSG | Receptor signaling, transport |
Temporal regulation of redox processes occurs across multiple timescales. Circadian oscillations in H₂O₂ levels have been observed in mouse liver, with relatively oxidized states during active phases and reduced states during resting phases [73]. The cell cycle demonstrates periodic redox changes, with the NADPH/NADP⺠ratio significantly increasing during cell division [73]. Throughout the aging process, redox changes occur in a compartment-specific manner, with the cytosol and mitochondria becoming more oxidized while the endoplasmic reticulum shifts toward a more reductive state in Caenorhabditis elegans [73].
Redox Signaling in Inflammation and Disease
Redox signaling plays a central role in regulating immune responses and inflammation. The transcription factor NF-κB represents a well-characterized redox-sensitive pathway that is activated by ROS and promotes the expression of pro-inflammatory cytokines, adhesion molecules, and enzymes like COX-2 and iNOS [4]. Concurrently, the Nrf2-Keap1 pathway functions as a critical protective mechanism that is activated by oxidative stress and induces the expression of cytoprotective genes including heme oxygenase-1 (HO-1) and NAD(P)H quinone dehydrogenase 1 (NQO1) [4] [1].
The dual nature of redox signaling is particularly evident in inflammation, where moderate ROS production facilitates pathogen clearance and immune activation, while excessive or sustained ROS production leads to tissue damage and chronic inflammation [4] [36]. Emerging evidence indicates that reductive stress can similarly disrupt immune function, illustrating the detrimental potential of deviations in either direction from redox homeostasis [4].
Methodological Approaches for Precision Redox Research
Advanced Analytical Techniques
Mass spectrometry (MS) has emerged as a powerful tool for precision redox research, enabling comprehensive analysis of redox biomarkers and modifications [75]. Key MS applications include:
- Redox proteomics: Identification and quantification of specific oxidative protein modifications including carbonylation, S-nitrosylation, S-glutathionylation, and sulfenic acid formation on cysteine residues [75] [76].
- Lipid peroxidation products: Measurement of specific biomarkers including F2-isoprostanes, 4-hydroxynonenal (4-HNE), and malondialdehyde (MDA) with high sensitivity and specificity [74] [75].
- DNA damage markers: Quantification of 8-oxo-2'-deoxyguanosine (8-oxo-dG) and other oxidative DNA lesions [74] [75].
- Redox metabolites: Analysis of GSH/GSSG, Cys/CySS, NADPH/NADPâº, and other redox couples using liquid chromatography-mass spectrometry (LC-MS) platforms [75].
Table 2: Mass Spectrometry Approaches for Redox Biomarker Analysis
| Analyte Category | Specific Biomarkers | MS Platform | Clinical/Research Utility |
|---|---|---|---|
| Protein oxidation | Carbonylated proteins, nitrotyrosine, sulfenic acids | LC-MS/MS, redox proteomics | Assessment of oxidative damage to functional proteins |
| Lipid peroxidation | 4-HNE, F2-isoprostanes, MDA | GC-MS, LC-MS/MS | Indicator of membrane oxidative damage |
| DNA/RNA oxidation | 8-oxo-dG, 8-OHdG | LC-MS/MS, HPLC-ECD | Genotoxic stress evaluation |
| Redox couples | GSH/GSSG, Cys/CySS, NADPH/NADP⺠| LC-MS/MS, CE-MS | Cellular redox capacity assessment |
| Metabolic profiling | TCA cycle intermediates, pentose phosphate pathway metabolites | LC-MS, GC-MS | Redox metabolism flux analysis |
Genetically Encoded Redox Probes
Genetically encoded fluorescent probes represent another essential methodology for precision redox research, enabling real-time monitoring of redox dynamics in specific cellular compartments [73] [75]. Examples include:
- HyPer family probes: Hâ‚‚Oâ‚‚-specific sensors that can be targeted to various subcellular locations [73].
- roGFP-based probes: Redox-sensitive GFP variants that monitor glutathione redox potential (Eh) and can be fused with glutaredoxin or other redox-active proteins for specificity [75].
- NADH/NADPH sensors: Such as SoNar and iNAP for monitoring NADâº/NADH and NADPâº/NADPH ratios [73].
These tools have revealed compartment-specific redox changes during physiological processes and disease progression, providing critical insights that would be obscured by global redox measurements [73].
Multi-Omics Integration and Artificial Intelligence
The integration of multiple analytical approaches through multi-omics strategies provides a systems-level understanding of redox regulation [74]. Combining redox proteomics with transcriptomic, metabolomic, and epigenetic datasets enables the identification of redox-regulated networks in specific pathological contexts [74] [1].
Artificial intelligence and machine learning approaches are being leveraged to analyze complex redox datasets, identify biomarker patterns, and predict patient-specific responses to redox-targeted therapies [74]. These computational approaches facilitate the transition from population-based to personalized redox medicine by accounting for individual variations in redox homeostasis [74].
Experimental Workflows and Research Reagents
Comprehensive Workflow for Precision Redox Analysis
The following diagram illustrates an integrated experimental workflow for precision redox analysis, incorporating multiple methodological approaches:
Diagram 1: Precision Redox Analysis Workflow. This integrated approach combines subcellular fractionation, advanced mass spectrometry, live-cell imaging with genetically encoded probes, multi-omics integration, and artificial intelligence to generate comprehensive redox profiles.
Research Reagent Solutions for Precision Redox
Table 3: Essential Research Reagents for Precision Redox Investigations
| Reagent Category | Specific Examples | Function/Application |
|---|---|---|
| Genetically encoded redox probes | HyPer, roGFP, Grx1-roGFP | Compartment-specific real-time monitoring of Hâ‚‚Oâ‚‚ and glutathione redox potential |
| Small-molecule fluorescent probes | MitoSOX, DCFH-DA, H2DCFDA | Detection of specific ROS in cellular compartments |
| Mitochondria-targeted antioxidants | MitoQ, SS-31 | Selective mitigation of mitochondrial oxidative stress |
| NRF2 activators | Dimethyl fumarate, sulforaphane | Pharmacological enhancement of antioxidant response element-mediated gene expression |
| NOX inhibitors | GKT137831, apocynin | Specific targeting of NADPH oxidase-derived ROS production |
| Redox biosensors | glutaredoxin-1, thioredoxin biosensors | Monitoring specific redox enzyme activities and dynamics |
| CRISPR/Cas9 tools | SOD1/2 KO, GPx1 correction | Genetic manipulation of specific antioxidant defense elements |
| Nanoparticle delivery systems | Antioxidant-loaded nanoparticles | Targeted delivery of redox modulators to specific tissues or cell types |
Detailed Protocol: Compartment-Specific Redox Assessment
Objective: Comprehensive evaluation of redox status across subcellular compartments in cultured cells under inflammatory stimulation.
Methodology:
Cell Culture and Stimulation:
- Culture appropriate cell model (e.g., primary macrophages, endothelial cells)
- Stimulate with inflammatory agents (e.g., LPS, TNF-α) for defined timepoints
- Include controls with specific ROS inhibitors (e.g., NOX inhibitors, mitochondrial ROS scavengers)
Subcellular Fractionation:
- Perform differential centrifugation to isolate nuclear, mitochondrial, cytoplasmic, and microsomal fractions
- Verify fraction purity using compartment-specific markers (e.g., TOM20 for mitochondria, Lamin B1 for nucleus)
- Process fractions immediately for redox analysis
Redox Parameter Assessment:
- GSH/GSSG ratios: Determine using LC-MS/MS or commercial kits adapted for small sample volumes
- Redox potential calculation: Compute Eh using Nernst equation with measured GSH/GSSG ratios
- Protein carbonylation: Detect using DNPH-based methods or redox proteomics
- Lipid peroxidation: Quantify 4-HNE and F2-isoprostanes using LC-MS/MS
- Enzymatic activities: Measure SOD, catalase, GPx, and GR activities in each fraction
Live-Cell Imaging:
- Transfect with compartment-targeted redox probes (e.g., mito-roGFP, nuclear HyPer)
- Perform time-lapse imaging during inflammatory stimulation
- Quantify fluorescence ratios to determine dynamic redox changes
Data Integration and Analysis:
- Correlate compartment-specific redox changes with functional outcomes
- Identify critical redox thresholds for pathological transitions
- Validate key findings using genetic or pharmacological interventions
This protocol enables researchers to obtain a comprehensive, compartment-resolved understanding of redox dynamics in inflammatory models, facilitating the identification of precise therapeutic targets [73] [75].
Signaling Pathways in Redox-Mediated Inflammation
The following diagram illustrates key redox-sensitive signaling pathways in inflammation, highlighting potential targets for precision interventions:
Diagram 2: Redox-Sensitive Inflammatory Signaling. Reactive species activate pro-inflammatory pathways including NF-κB and NLRP3 inflammasome, while simultaneously triggering protective NRF2-mediated antioxidant responses that facilitate inflammation resolution.
Therapeutic Applications and Clinical Translation
Precision Redox Therapeutics
The precision redox approach has generated several targeted therapeutic strategies with promising clinical potential:
- Mitochondria-targeted antioxidants: Compounds such as MitoQ and SS-31 (elamipretide) selectively accumulate in mitochondria, protecting against mitochondrial oxidative damage while preserving redox signaling in other compartments [74] [3].
- NRF2 activators: Agents like dimethyl fumarate (approved for multiple sclerosis) and synthetic triterpenoids enhance the antioxidant response in a regulated manner, providing cytoprotection in neurodegenerative and inflammatory conditions [74] [1].
- NOX inhibitors: Isoform-specific NADPH oxidase inhibitors (e.g., GKT137831) target specific ROS sources without disrupting physiological redox signaling [4] [1].
- Sulfur-based therapeutics: Hydrogen sulfide (Hâ‚‚S) donors and other reactive sulfur species modulators target specific sulfhydration pathways with potential benefits in cardiovascular diseases [3].
Disease-Specific Applications
Neurodegenerative Diseases: Precision redox approaches are particularly relevant in conditions like Alzheimer's disease, Parkinson's disease, and amyotrophic lateral sclerosis, where oxidative damage contributes to pathogenesis but previous antioxidant trials have largely failed [74]. Current strategies focus on targeting specific oxidative processes (e.g., lipid peroxidation in ferroptosis) and delivering antioxidants to vulnerable neuronal populations [74].
Cardiovascular Diseases: Redox signaling contributes to cardiovascular pathophysiology through multiple mechanisms including endothelial dysfunction, vascular inflammation, and mitochondrial dysfunction in cardiomyocytes [3]. Precision approaches aim to target specific ROS sources (e.g., NOX isoforms, mitochondrial complex I) while preserving physiological NO signaling [3].
Cancer: The dual role of ROS in cancer—promoting tumor progression at moderate levels while triggering cell death at high levels—creates opportunities for precision interventions [73] [1]. Strategies include pro-oxidant therapies for certain cancer types and antioxidant approaches for others, based on the specific redox vulnerabilities of each tumor [73].
Clinical Trial Considerations
Successful translation of precision redox therapies requires attention to several key factors:
- Patient stratification: Identification of biomarkers that predict response to specific redox-targeted therapies [73] [74].
- Dosing and timing: Optimization of intervention timing based on disease stage and circadian redox rhythms [73].
- Combination therapies: Rational design of drug combinations that target multiple redox nodes simultaneously [74] [1].
- Biomarker development: Validation of redox biomarkers for patient selection and treatment monitoring [75].
Precision redox medicine represents a fundamental advancement in our approach to understanding and targeting redox processes in inflammation and disease. By accounting for the spatial, temporal, and contextual specificity of redox signaling, this framework enables the development of targeted interventions that preserve physiological redox functions while correcting pathological imbalances. The integration of advanced analytical methodologies, multi-omics datasets, and computational approaches will continue to drive innovation in this field, ultimately enabling personalized redox medicine tailored to individual patient profiles and specific disease contexts. As these strategies mature, precision redox approaches hold significant promise for transforming the treatment of inflammatory, neurodegenerative, cardiovascular, and neoplastic diseases.
Troubleshooting Antioxidant Therapies and Optimizing Redox-Based Interventions
The hypothesis that broad-spectrum antioxidants could combat chronic diseases by neutralizing reactive oxygen species (ROS) was once a cornerstone of therapeutic optimism. However, the consistent failure of large-scale clinical trials has necessitated a paradigm shift in redox biology. This review delves into the mechanistic failures of non-specific antioxidant therapies, moving beyond the simplistic "oxidants are bad, antioxidants are good" dogma. We analyze how an incomplete understanding of redox signaling—particularly the dual roles of ROS as both damaging agents and crucial signaling molecules—has led to these clinical disappointments. By integrating recent advances in redox biology, we outline a more nuanced framework for therapeutic development, emphasizing targeted delivery, context-specific actions, and the critical balance of the redox landscape.
The oxidative stress theory of disease, which posits that an imbalance between reactive oxygen species (ROS) and antioxidant defenses drives pathology, provided a compelling and simple rationale for antioxidant therapy [25] [77]. This led to immense commercial and clinical interest in broad-spectrum antioxidants like vitamins C and E, and β-carotene. The initial premise was straightforward: supplementing the body's defenses with exogenous antioxidants should mitigate oxidative damage, thereby preventing or treating a myriad of conditions from cancer to cardiovascular disease [77] [78].
However, this intuitive approach has yielded largely negative or even harmful results in well-controlled clinical trials. The failure of these interventions highlights a critical conceptual flaw: the failure to account for the complex physiological roles of ROS in redox signaling and control [24] [79]. ROS are not merely toxic byproducts; they are essential signaling molecules that regulate key processes including growth factor signaling, immune response, and genomic stability [1] [24]. This whitepaper analyzes the mechanistic reasons behind these clinical failures and re-frames the discussion within the modern understanding of redox biology in inflammation and disease.
Mechanistic Foundations: Why Simple Neutralization Fails
The Dual Nature of ROS: Redox Signaling vs. Oxidative Damage
The fundamental failure of broad-spectrum antioxidants lies in their inability to distinguish between pathological oxidative stress and physiological redox signaling.
- Redox Signaling (Eustress): At low, physiological concentrations (typically in the nanomolar range), specific ROS like H₂O₂ act as precise second messengers [24]. A key mechanism involves the reversible oxidation of critical cysteine residues in target proteins, such as protein tyrosine phosphatases (PTPs) and the transcription factor NF-κB, thereby altering their activity and propagating signals for cell growth, differentiation, and immune response [1] [24]. This state is often termed eustress [79].
- Oxidative Damage (Distress): At high concentrations, ROS cause random damage to lipids, proteins, and DNA, a state of distress that leads to cellular dysfunction and death [25] [78]. Broad-spectrum antioxidants non-discriminately quench both signaling and damaging ROS, disrupting essential physiological pathways while attempting to curb pathological damage [24].
Table 1: Key Reactive Oxygen Species and Their Dual Roles
| ROS Molecule | Primary Physiological Role (Signaling) | Pathological Role (Damage) |
|---|---|---|
| Superoxide (O₂•â») | Precursor for Hâ‚‚Oâ‚‚ generation [78] | Inactivates iron-sulfur cluster proteins; precursor to more reactive species [24] |
| Hydrogen Peroxide (Hâ‚‚Oâ‚‚) | Reversible oxidation of cysteine thiols in signaling proteins (e.g., PTPs) [24] | Can be converted to highly damaging hydroxyl radicals via Fenton reaction [25] [79] |
| Hydroxyl Radical (•OH) | Minimal to no signaling function | Indiscriminate damage to all biomolecules; major contributor to cytotoxicity [25] [78] |
Disruption of Physiological Redox Circuits
The cellular redox environment is a tightly regulated network, not a simple battlefield. Key transcription factors like NF-κB (pro-inflammatory) and NRF2 (anti-inflammatory/cytoprotective) are exquisitely sensitive to the redox state [25] [4].
- NF-κB Pathway: ROS can activate the IκB kinase (IKK) complex, leading to the degradation of IκB and the translocation of NF-κB to the nucleus, where it drives the expression of pro-inflammatory cytokines and enzymes [4]. While chronic NF-κB activation is pathogenic, its transient activity is essential for proper immune function. Non-specific antioxidant suppression can thus impair necessary inflammatory responses [4].
- NRF2-KEAP1 Pathway: Under basal conditions, NRF2 is bound to KEAP1 and targeted for degradation. Oxidative modification of KEAP1 cysteine residues frees NRF2, allowing it to translocate to the nucleus and activate the transcription of a battery of antioxidant and cytoprotective genes [25] [4]. By globally lowering ROS, broad-spectrum antioxidants can paradoxically dampen this endogenous, adaptive antioxidant response [1].
Diagram 1: Redox-sensitive signaling pathways. ROS directly oxidize and inhibit KEAP1, leading to NRF2 activation and antioxidant gene transcription. Concurrently, ROS activate IKK, leading to NF-κB activation and pro-inflammatory gene expression. Broad-spectrum antioxidants non-specifically quench the ROS signal, disrupting both pathways.
The Emergence of Reductive Stress
An often-overlooked consequence of excessive antioxidant use is the induction of reductive stress [4] [77]. This condition is characterized by an overabundance of reducing equivalents (e.g., high NADH/NADâº, NADPH/NADPâº, and GSH/GSSG ratios), which can paradoxically impair cellular function.
- Impact on Immune Function: Sustained reductive stress can compromise the immune system's ability to mount an effective oxidative burst, a critical mechanism for pathogen clearance by neutrophils and macrophages [4].
- Signaling Impairment: An overly reduced environment can disrupt the normal formation of disulfide bonds in proteins, alter the activity of redox-sensitive transcription factors, and contribute to the progression of diseases such as cardiomyopathies and metabolic syndromes [4] [77].
Clinical Evidence: Lessons from Failed Trials
The theoretical pitfalls of broad-spectrum antioxidants have been starkly realized in several major clinical trials. The outcomes not only demonstrated a lack of efficacy but also revealed significant harm in certain populations.
Table 2: Summary of Major Clinical Trial Failures with Broad-Spectrum Antioxidants
| Trial (Acronym) | Intervention | Target Population | Primary Outcome | Key Finding & Implication |
|---|---|---|---|---|
| ATBC (1994) | β-carotene, Vitamin E | 29,133 male smokers | Lung cancer incidence | 18% increase in lung cancer risk with β-carotene [77]. Demonstrated that context (smoking) is critical. |
| CARET (1996) | β-carotene, Retinyl palmitate | Smokers, asbestos workers | Lung cancer incidence | 28% increase in lung cancer incidence and 17% increase in mortality; trial halted early [77]. |
| Physicians' Health Study | β-carotene | Male physicians | Cancer & CVD incidence | No significant benefit or harm in a low-risk population [77]. Highlighted population-specific effects. |
| HOPE / HOPE-TOO | Vitamin E | High-risk CVD patients | Cardiovascular events | No reduction in cancer incidence, CV events, or mortality; trend towards increased heart failure [3]. |
| GPx1 Mimic (Ebselen) Trials | Ebselen | Stroke, other conditions | Neurological recovery | Lack of efficacy due to poor bioavailability and failure to hit critical molecular targets [1]. |
Case Study: The Failure of β-Carotene in Smokers
The ATBC and CARET trials represent the most alarming examples of antioxidant failure. The proposed mechanism for harm involves the pro-oxidant behavior of β-carotene in the unique, pro-oxidant microenvironment of the smoker's lung [77]. Under high oxygen tension and in the presence of high levels of other radicals (e.g., from cigarette smoke), β-carotene can oxidize and generate reactive oxidative products that themselves damage DNA and lipids. Furthermore, by quenching ROS non-specifically, β-carotene may have interfered with ROS-dependent apoptosis, allowing damaged, pre-cancerous cells to proliferate [24].
New Frontiers: Moving Beyond Broad-Spectrum Approaches
The consistent failures of the past demand a more sophisticated, targeted approach to redox medicine. Current research is focused on strategies that respect the complexity of redox networks.
Targeting the Source: Specific ROS-Generating Enzymes
Instead of neutralizing all ROS, new therapies aim to inhibit specific, pathologically relevant sources of ROS. For example, highly specific inhibitors of Nox2 or Nox4 isoforms of NADPH oxidase are being explored for conditions like fibrosis and hypertension where these enzymes are known to be major drivers of pathology [1] [3]. This approach leaves ROS from other sources (e.g., mitochondrial signaling ROS) intact.
Boosting Endogenous Defenses: NRF2 Activators
Pharmacological activation of the NRF2 pathway represents a "smarter" antioxidant strategy. Instead of directly scavenging ROS, NRF2 activators (such as sulforaphane) enhance the cell's own, elegantly regulated antioxidant defense systems [25] [4]. This allows for a coordinated, amplified response that is integrated into the cell's natural homeostasis.
Redox Nanomedicine and Targeted Delivery
A major limitation of traditional antioxidants is their inability to reach the specific subcellular compartment where oxidative stress is occurring. Nanotechnology offers solutions through:
- Nanozymes: Nanomaterials with enzyme-mimicking activities (e.g., cerium oxide nanoparticles that mimic SOD and catalase) that can be engineered for stability and targeted delivery [79].
- Targeted Delivery Systems: Liposomal or polymer-based nanoparticles can be designed to deliver antioxidant agents (e.g., catalase) specifically to mitochondria or other organelles, maximizing therapeutic impact while minimizing systemic disruption [78] [79].
Diagram 2: The paradigm shift in redox therapeutics, from global suppression to precision medicine.
The Scientist's Toolkit: Key Reagents and Methodologies
Table 3: Essential Research Reagents for Advanced Redox Biology Studies
| Reagent / Tool Category | Specific Examples | Primary Function in Research |
|---|---|---|
| Specific Enzyme Inhibitors | GKT137831 (Nox1/Nox4 inhibitor), Apocynin (Nox inhibitor) | To dissect the contribution of specific enzymatic ROS sources to disease pathways without causing global antioxidant effects [3]. |
| NRF2 Pathway Modulators | Sulforaphane, CDDO-Me (synthetic triterpenoid) | To pharmacologically activate the endogenous antioxidant response element (ARE)-driven gene battery in a controlled manner [25] [4]. |
| Genetically Encoded Redox Probes | roGFP (redox-sensitive GFP), HyPer (Hâ‚‚Oâ‚‚ sensor) | To provide real-time, compartment-specific (e.g., mitochondrial matrix, cytosol) measurement of redox states (e.g., GSH/GSSG ratio, Hâ‚‚Oâ‚‚ levels) in live cells [80]. |
| Single-Cell Profiling Technologies | Signaling Network under Redox Stress Profiling (SN-ROP) via mass cytometry [80] | To simultaneously quantify >30 redox-related proteins (ROS transporters, enzymes, oxidative damage products) and signaling pathways at single-cell resolution, revealing heterogeneity in redox responses [80]. |
| Nanozymes | Cerium oxide (CeO₂) nanoparticles, Mn₃O₄ nanoparticles (SOD/CAT mimics) | To develop stable, multifunctional enzyme mimics for probing redox mechanisms and as potential therapeutic candidates with enhanced catalytic properties [79]. |
| Methyl 3,3-dimethoxypropionate | Methyl 3,3-dimethoxypropionate, CAS:7424-91-1, MF:C6H12O4, MW:148.16 g/mol | Chemical Reagent |
| 1-(Azetidin-3-yl)piperidine | 1-(Azetidin-3-yl)piperidine, CAS:138022-86-3, MF:C8H16N2, MW:140.23 g/mol | Chemical Reagent |
Experimental Protocol: Single-Cell Redox Signaling Network Profiling (SN-ROP)
The SN-ROP platform [80] represents a cutting-edge methodology for moving beyond bulk ROS measurements.
- Cell Preparation and Barcoding: Expose diverse cell types (e.g., immune cells, endothelial cells) to varying doses and durations of redox stressors (e.g., Hâ‚‚Oâ‚‚). Use a fluorescent cell barcoding technique to pool multiple experimental conditions.
- Staining with Mass Cytometry Antibody Panel: Stain the pooled cell sample with a metal-tagged antibody panel targeting ~30-40 key redox proteins. This includes:
- ROS-related transporters (e.g., aquaporins).
- ROS-generating and scavenging enzymes (e.g., NOX subunits, SOD, Catalase, GPX).
- Oxidative damage markers (e.g., protein sulfonation).
- Key signaling nodes (e.g., pNF-κB, pAKT, pERK, NRF2).
- Data Acquisition and Analysis: Analyze cells by mass cytometry (CyTOF). Use dimensionality reduction (e.g., UMAP) and clustering algorithms to deconvolute the single-cell data and identify distinct redox states and signaling network adaptations in response to stress.
The history of broad-spectrum antioxidants is a powerful lesson in translational medicine, demonstrating that therapeutic strategies must be built on a deep, nuanced understanding of fundamental biology. The failure of these interventions is not a repudiation of the role of oxidative stress in disease, but rather a confirmation that ROS function within a complex, tightly regulated redox signaling network. The path forward lies in precision redox medicine—developing therapies that target specific ROS sources, modulate endogenous defense pathways with temporal and spatial control, and are tailored to the individual's genetic and disease context. By learning from these failures, the field is now poised to develop a new generation of sophisticated, effective redox-based therapeutics.
Redox signaling, the biological process mediated by reactive oxygen species (ROS) and reactive nitrogen species (RNS), functions as a crucial cellular communication system that regulates immune responses, tissue repair, and metabolic balance [81]. Under physiological conditions, ROS generated by mitochondrial oxidative respiration, endoplasmic reticulum, and NADPH oxidases (NOX) are effectively neutralized by NRF2-mediated antioxidant responses, which elevate the synthesis of superoxide dismutase (SOD), catalase, and key molecules like nicotinamide adenine dinucleotide phosphate (NADPH) and glutathione (GSH) to maintain cellular redox homeostasis [1]. This delicate balance is essential for normal cellular function, as ROS serve as vital signaling molecules that modulate transcription factors such as NF-κB and Nrf2, and influence pathways like MAPK and PI3K/Akt, which are critical for neuronal survival, adaptation, and inflammatory regulation [82].
The therapeutic challenge emerges when well-intentioned antioxidant interventions disrupt this precise equilibrium. Reductive stress occurs when excessive antioxidant capacity overwhelms physiologically beneficial ROS signaling, creating an imbalance that can be as pathologically disruptive as oxidative stress [6]. This condition represents a fundamental bidirectional challenge in redox medicine: while oxidative stress results from excessive ROS production that overwhelms antioxidant defenses, reductive stress occurs when antioxidant interventions excessively suppress ROS, disrupting essential redox signaling networks. In metabolic disorders induced by overnutrition, this reductive stress emerges as a key pathological pathway, disrupting mitochondrial function, promoting endoplasmic reticulum (ER) stress, and ultimately contributing to disease progression [6]. The central paradox facing researchers and drug development professionals is that aggressive antioxidant therapies designed to mitigate oxidative damage in chronic inflammatory conditions may inadvertently induce harmful reductive stress, creating new pathological cascades while attempting to resolve others.
Molecular Mechanisms: From Oxidative to Reductive Stress
The Physiological Roles of ROS in Cellular Signaling
Reactive oxygen species, particularly hydrogen peroxide (H2O2), function as secondary messengers in multiple signaling cascades. At physiological levels, ROS modulate critical cellular processes including synaptic plasticity, neurogenesis, circadian rhythm regulation, immune function, and vascular tone [82] [9]. The mitochondrial electron transport chain represents a primary endogenous source of ROS, where approximately 1-3% of electrons leak during oxidative phosphorylation, leading to the partial reduction of oxygen and formation of superoxide radicals (O2•−) [25]. These radicals are subsequently converted to H2O2 by superoxide dismutase (SOD), which then functions as a signaling molecule at low concentrations [9]. Specific enzymatic systems, particularly the NADPH oxidase (NOX) family, also generate ROS in a regulated manner for signaling purposes rather than as mere metabolic byproducts [1].
The redox code governs how thiols, highly reactive constituents in protein residues, serve as crucial agents in the transduction of redox signals [1]. Influenced by ROS, thiols participate in reversible oxidative reactions including formation of disulfide bonds (S-S), S-glutathionylation (SSG), S-nitrosylation (SNO), and S-sulfenylation (SOH). These oxidative modifications of cysteine can be reverted to the free thiol state (-SH) by specific reductants, enabling them to modulate protein structure and functionality, subsequently affecting cellular physiological processes [1]. This sophisticated regulatory system allows cells to respond dynamically to environmental changes while maintaining redox homeostasis.
The Transition to Reductive Stress
Reductive stress develops when overzealous antioxidant therapy disrupts these essential signaling mechanisms. The pathological transition occurs through several interconnected mechanisms:
- Disruption of physiological ROS signaling: Excessive antioxidant activity suppresses ROS below their physiological concentrations, impairing essential signaling pathways that depend on redox-sensitive transcription factors like NRF2, NF-κB, and HIF-1α [6].
- Mitochondrial dysfunction: Under reductive conditions, the mitochondrial electron transport chain becomes over-reduced, leading to reverse electron transport and increased ROS production at complex I, paradoxically generating oxidative damage despite the antioxidant-rich environment [6].
- Impaired protein folding: The endoplasmic reticulum maintains an oxidative environment necessary for disulfide bond formation in secretory and membrane proteins. Reductive stress disrupts this environment, causing ER stress and activating the unfolded protein response (UPR) [6].
- Altered metabolic flux: Reductive stress promotes glycolytic flux while inhibiting the tricarboxylic acid (TCA) cycle, creating metabolic imbalances that further exacerbate cellular dysfunction [6].
The resulting pathological state demonstrates the bidirectional nature of redox imbalance, where both excessive oxidation and excessive reduction can drive disease processes through distinct yet interconnected molecular mechanisms.
Biomarkers and Detection: Quantifying Reductive Stress in Research Models
Established Biomarkers for Redox Imbalance
Detecting and quantifying reductive stress requires monitoring specific biochemical parameters that reflect the cellular redox state. The table below summarizes key biomarkers used to identify reductive stress in experimental models:
Table 1: Biomarkers for Detecting Reductive Stress in Experimental Systems
| Biomarker Category | Specific Marker | Normal Function | Change in Reductive Stress | Detection Method |
|---|---|---|---|---|
| Redox Couples | GSH/GSSG ratio | Cellular antioxidant capacity | Significantly increased | HPLC, enzymatic assays |
| NADPH/NADP+ ratio | Electron donor for antioxidant systems | Markedly elevated | Mass spectrometry | |
| Reduced/Oxidized Trx | Protein disulfide reduction | Increased reduced form | Western blot, ELISA | |
| ROS Signaling Molecules | H2O2 concentration | Secondary messenger | Abnormally low | Amplex Red, fluorescent probes |
| Superoxide (O2•−) | Signaling molecule | Suppressed | Lucigenin, DHE staining | |
| Protein Modifications | S-glutathionylation | Reversible protein regulation | Abnormal patterns | Proteomics, mass spectrometry |
| Sulfenic acid formation | Redox sensing | Decreased | Dimedone-based probes | |
| Metabolic Indicators | Lactate/pyruvate ratio | Glycolytic flux | Increased | Metabolomics, enzymatic assays |
| Mitochondrial membrane potential (ΔΨm) | Proton gradient for ATP synthesis | Hyperpolarized | JC-1, TMRM staining |
These biomarkers provide researchers with quantitative tools to assess the redox state of experimental systems and identify the transition from physiological redox balance to pathological reductive stress. The GSH/GSSG ratio is particularly informative, as glutathione represents one of the most abundant cellular thiol antioxidants and its redox couple is highly sensitive to both oxidative and reductive imbalances [1] [9].
Advanced Detection Methodologies
Several specialized protocols enable precise measurement of reductive stress parameters:
Protocol 1: Comprehensive Redox Status Assessment
- Sample Preparation: Harvest cells or tissue samples under anaerobic conditions to prevent artificial oxidation. Use potassium phosphate buffer (50 mM, pH 7.4) containing 1 mM EDTA and protease inhibitors.
- GSH/GSSG Quantification: Derivatize with 2-vinylpyridine for GSSG measurement without derivatization for total glutathione. Use glutathione reductase recycling assay with 5,5'-dithio-bis(2-nitrobenzoic acid) (DTNB) at 412 nm.
- NADPH/NADP+ Analysis: Extract with hot ethanol, then measure using enzymatic cycling assays with glucose-6-phosphate dehydrogenase and phenazine ethosulfate.
- Protein Thiol Status: Label with monobromobimane followed by SDS-PAGE separation and fluorescence detection.
Protocol 2: Mitochondrial Redox Function Assessment
- Isolate Mitochondria: Differential centrifugation in sucrose-based media (250 mM sucrose, 10 mM HEPES, 1 mM EGTA, pH 7.4).
- Measure Membrane Potential: Use tetramethylrhodamine methyl ester (TMRM) at 20 nM with fluorescence detection at 573 nm excitation/625 nm emission.
- Assess ROS Production: Monitor H2O2 production with Amplex Red (10 μM) and horseradish peroxidase (0.1 U/mL) at 563 nm excitation/587 nm emission in the presence of complex I or II substrates.
- Determine Electron Transport Chain Redox State: Monitor absorbance changes of cytochromes using dual-wavelength spectrophotometry (550-540 nm for cytochrome c, 605-630 nm for cytochrome a/a3).
These methodologies enable researchers to precisely quantify the degree of reductive stress in experimental systems and evaluate the potential off-target effects of antioxidant therapies.
Experimental Models and Methodologies for Studying Reductive Stress
In Vitro Induction and Assessment
Table 2: Experimental Models for Reductive Stress Research
| Model System | Induction Method | Key Parameters | Advantages | Limitations |
|---|---|---|---|---|
| Cardiomyocytes | N-acetylcysteine (0.5-5 mM), GSH ethyl ester (1-10 mM) | Contractility, mitochondrial function, apoptosis markers | High clinical relevance, well-characterized | May not reflect tissue complexity |
| Hepatic Cells | Sulforaphane (1-20 μM), α-lipoic acid (0.1-2 mM) | Lipid accumulation, ER stress markers, insulin signaling | Strong metabolic relevance | Variable response between cell types |
| Neuronal Cultures | High-dose vitamin E (50-200 μM), coenzyme Q10 (5-50 μM) | Neurite outgrowth, synaptic function, oxidative markers | Relevant for neurodegenerative disease | Difficult to maintain long-term cultures |
| Animal Models | Transgenic NRF2 overexpression, high-dose antioxidant diets | Tissue function, behavioral outcomes, organ pathology | Whole-organism physiology | Complex interplay of systems |
| Human Studies | High-dose antioxidant supplementation (e.g., vitamin C/E) | Biomarker changes, subtle functional declines | Direct clinical relevance | Ethical limitations, confounding factors |
Controlled induction of reductive stress in cellular models typically involves administration of reducing agents at supraphysiological concentrations. N-acetylcysteine (NAC), a precursor to glutathione, is commonly used at 0.5-5 mM concentrations to create a reductive environment. Similarly, glutathione ethyl ester (1-10 mM), which readily crosses cell membranes, can directly elevate intracellular GSH levels [6]. These models demonstrate that reductive stress impairs cellular function through multiple pathways, including disruption of mitochondrial energy production, induction of ER stress, and promotion of metabolic dysfunction.
In Vivo Modeling Approaches
Animal models of reductive stress have been developed using both genetic and pharmacological approaches:
Protocol 3: Murine Model of Diet-Induced Reductive Stress
- Animals: C57BL/6J mice (8-10 weeks old)
- Intervention: High-fat diet (60% kcal from fat) supplemented with N-acetylcysteine (1 g/L in drinking water) and vitamin E (2,000 IU/kg diet) for 12-16 weeks
- Monitoring: Weekly body weight, fasting blood glucose biweekly, glucose and insulin tolerance tests at 4-week intervals
- Tissue Collection: Harvest liver, heart, adipose tissue under isoflurane anesthesia. Snap-freeze in liquid N2 or preserve in formalin for histology
- Endpoint Analyses: Hepatic triglyceride content, mitochondrial respiration in permeabilized muscle fibers, glutathione levels in tissues, RNA sequencing for pathway analysis
Protocol 4: Acute Reductive Stress in Isolated Perfused Heart
- Heart Isolation: Anesthetize rat with sodium pentobarbital (50 mg/kg i.p.), excise heart, and cannulate aorta for Langendorff perfusion
- Perfusion Conditions: Krebs-Henseleit buffer (37°C, pH 7.4) gassed with 95% O2/5% CO2
- Reductive Stress Induction: Infuse GSH ethyl ester (10 mM) or dithiothreitol (DTT, 1-5 mM) for 20 minutes
- Functional Assessment: Measure left ventricular developed pressure, +dP/dt, -dP/dt, coronary flow rate
- Metabolic Analysis: Freeze-clamp heart at conclusion for assessment of GSH/GSSG, protein carbonylation, and S-glutathionylation patterns
These experimental approaches enable systematic investigation of reductive stress pathophysiology and provide platforms for evaluating potential therapeutic interventions.
Pathway Visualization: Molecular Mechanisms of Reductive Stress
The following diagram illustrates the key molecular pathways through which overly aggressive antioxidant therapy induces harmful reductive stress:
Diagram Title: Reductive Stress Pathways from Excessive Antioxidants
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Research Reagent Solutions for Reductive Stress Investigation
| Reagent Category | Specific Examples | Concentration Range | Mechanism of Action | Research Applications |
|---|---|---|---|---|
| Reductive Stress Inducers | N-acetylcysteine (NAC) | 0.5-5 mM | Glutathione precursor, thiol donor | Establishing reductive stress models |
| Glutathione ethyl ester | 1-10 mM | Membrane-permeable GSH analog | Rapid intracellular glutathione elevation | |
| Dithiothreitol (DTT) | 1-5 mM | Thiol-based reducing agent | Acute reductive challenge in vitro | |
| Sulforaphane | 1-20 μM | NRF2 pathway activator | Chronic induction of antioxidant genes | |
| Redox Biosensors | roGFP | N/A (genetically encoded) | Redox-sensitive green fluorescent protein | Real-time monitoring of glutathione redox potential |
| HyPer | N/A (genetically encoded) | H2O2-specific biosensor | Detection of hydrogen peroxide dynamics | |
| MitoSOX Red | 5 μM | Mitochondrial superoxide indicator | Selective detection of mitochondrial O2•− | |
| JC-1 dye | 2-5 μM | Mitochondrial membrane potential sensor | Assessment of mitochondrial polarization | |
| Analytical Tools | Monobromobimane | 100 μM | Thiol-specific alkylating agent | Protein thiol status quantification |
| Anti-glutathione antibody | Dilution-dependent | Detection of protein S-glutathionylation | Western blot, immunocytochemistry | |
| Mass spectrometry kits | N/A | Comprehensive redox proteomics | System-wide analysis of redox modifications | |
| 2,3,8-Tri-O-methylellagic acid | 2,3,8-Tri-O-methylellagic acid, CAS:1617-49-8, MF:C17H12O8, MW:344.3 g/mol | Chemical Reagent | Bench Chemicals |
This toolkit enables researchers to induce, measure, and analyze reductive stress in experimental systems. The combination of chemical inducers with genetically encoded biosensors provides particularly powerful approaches for real-time monitoring of redox dynamics in living cells and tissues.
Strategic Approaches for Balanced Redox-Targeted Therapeutics
Context-Dependent Antioxidant Interventions
Modern redox medicine requires a nuanced approach that respects the bidirectional nature of redox balance. Several strategic approaches show promise for avoiding reductive stress while effectively targeting oxidative damage:
Temporally-Controlled Antioxidant Delivery
- Rationale: Redox needs fluctuate diurnally and in response to physiological challenges
- Implementation: Chronotherapeutic administration aligned with circadian ROS fluctuations
- Experimental Evidence: Timed NRF2 activator administration shows improved efficacy with reduced side effects
Compartment-Specific Targeting
- Mitochondria-Targeted Antioxidants: Compounds like MitoQ and SkQ1 accumulate in mitochondria, preventing systemic reductive stress while addressing localized oxidative damage [83]
- NOX Isoform-Specific Inhibitors: Selective targeting of pathological ROS sources (e.g., NOX2 in inflammation) while preserving physiological ROS signaling from other sources
NRF2 Activity Modulators Rather Than Direct Antioxidants
- Approach: Compounds that moderately enhance endogenous antioxidant capacity without creating immediate reductive environments
- Examples: Bardoxolone methyl analogs that provide controlled NRF2 activation without complete pathway saturation
Experimental Workflow for Evaluating Reductive Stress Risk
The following diagram outlines a systematic approach for assessing the reductive stress potential of novel antioxidant therapies during preclinical development:
Diagram Title: Reductive Stress Risk Assessment Workflow
This systematic workflow enables researchers to identify reductive stress liabilities early in therapeutic development, guiding dose optimization and formulation strategies to maintain physiological redox balance while achieving therapeutic efficacy.
The bidirectional challenge of avoiding harmful reductive stress while effectively mitigating oxidative damage represents a critical frontier in redox biology and therapeutic development. The evidence from multiple disease models indicates that the traditional "more antioxidants are better" paradigm requires fundamental reassessment. Future advances will depend on developing sophisticated delivery systems that target antioxidants to specific cellular compartments, personalizing interventions based on individual redox profiles, and designing dynamic therapies that adapt to changing redox needs. By embracing the complexity of redox signaling and respecting the delicate balance between oxidation and reduction, researchers and drug developers can create a new generation of redox-based therapeutics that avoid the pitfalls of reductive stress while effectively addressing the oxidative components of inflammatory and degenerative diseases.
The field of redox signaling has established the critical role of reactive oxygen and nitrogen species (ROS/RNS) in driving inflammatory pathways and disease progression [3]. However, therapeutic intervention faces a fundamental challenge: achieving sufficient drug concentrations at specific diseased sites while minimizing systemic exposure and side effects. Conventional antioxidants have demonstrated limited clinical efficacy, primarily due to poor bioavailability, inadequate tissue specificity, and rapid systemic clearance [84] [3].
Nanotechnology has emerged as a transformative solution to these limitations, offering sophisticated platforms for enhancing therapeutic delivery. Nanoparticles possess tunable physicochemical properties that enable passive targeting through pathological tissue characteristics and active targeting through surface-modified ligands [85] [86]. Within the context of redox-mediated inflammatory diseases, these approaches allow for precise modulation of oxidative stress at its source, potentially disrupting the vicious cycle of inflammation and tissue damage without compromising physiological redox signaling [84] [87].
This technical guide examines current nanotechnology approaches for optimizing delivery and specificity, with particular emphasis on applications in redox-based therapeutics. We provide structured data on nanomaterial systems, detailed experimental methodologies, and visualization of key concepts to support research and development in this advancing field.
Nanoparticle Design Parameters for Enhanced Delivery
The delivery efficiency of nanomedicines to target tissues is governed by a series of design parameters that must be strategically optimized. These factors influence circulatory half-life, tissue extravasation, and cellular uptake.
Core Physicochemical Properties
Size: Nanoparticle dimension critically determines biodistribution and clearance pathways. Particles below 10 nm typically undergo rapid renal clearance, while those exceeding 400 nm are often sequestered by the reticuloendothelial system (RES). Optimal tumor accumulation via the Enhanced Permeability and Retention (EPR) effect generally occurs within the 10-200 nm range, with specific studies indicating particularly efficient tumor deposition for liposomes between 90-200 nm [85]. Responsive systems that undergo size reduction after tissue entry can enhance both extravasation and tissue penetration [85].
Surface Charge: Charge characteristics influence colloidal stability, protein adsorption, and cellular interactions. Negatively charged nanoparticles typically exhibit prolonged circulation times due to reduced opsonization and RES uptake [85]. Cationic surfaces, while promoting stronger interactions with anionic cell membranes and enhanced cellular internalization, often suffer from accelerated blood clearance due to plasma protein adsorption and aggregation [85]. Surface functionalization with hydrophilic polymers like polyethylene glycol (PEG) can mitigate rapid clearance regardless of core charge [85].
Shape: Non-spherical architectures demonstrate distinct advantages in margination, adhesion, and vascular extravasation. Rod-shaped nanoparticles exhibit hydrodynamic properties that enhance endothelial transmigration, while disk-shaped variants demonstrate superior adhesion probabilities in laminar flow environments [85]. Cylindrical micellar structures have shown extended systemic circulation (approximately 24-hour elimination half-lives) and 1.4- to 2.3-fold greater tumor accumulation compared to spherical equivalents [85].
Targeting Moieties and Surface Functionalization
Active targeting represents a paradigm beyond passive accumulation, employing surface-bound ligands to recognize and bind specific molecular markers on target cells. Common targeting approaches include:
- Antibody-mediated targeting: Monoclonal antibodies or fragments targeting disease-specific surface antigens
- Ligand-receptor targeting: Peptides, vitamins, or carbohydrates targeting upregulated receptors (e.g., folate, transferrin)
- Aptamer-based targeting: Nucleic acid or peptide aptamers with high affinity for molecular targets
These targeting strategies enhance cellular internalization through receptor-mediated endocytosis and improve tissue specificity, particularly important in diseases with heterogeneous EPR effects [85] [86].
Table 1: Nanoparticle Design Parameters and Their Biological Implications
| Parameter | Optimal Range | Biological Impact | Considerations |
|---|---|---|---|
| Size | 10-200 nm | • <10 nm: Renal clearance• 90-200 nm: Enhanced tumor accumulation• >400 nm: RES sequestration | Tumor-dependent vascular pore sizes; Stimuli-responsive size switching enhances penetration |
| Surface Charge | Slightly negative to neutral | • Cationic: Enhanced cellular uptake but rapid clearance• Anionic: Prolonged circulation• Neutral: Reduced opsonization | PEGylation reduces RES recognition; Charge-reversal systems respond to microenvironment |
| Shape | Rod, disk, cylindrical | • Spherical: Laminar flow dynamics• Rod: Enhanced endothelial transmigration• Disk: Superior margination and adhesion | Anisotropic structures improve pharmacokinetics; High-aspect-ratio micelles show 2.3× greater tumor deposition |
Tissue-Targeting Mechanisms in Redox Pathology
Passive Targeting Approaches
Passive targeting capitalizes on the unique pathological features of diseased tissues to achieve selective nanoparticle accumulation. The most extensively studied mechanism is the Enhanced Permeability and Retention (EPR) effect, predominant in tumors and inflammatory sites.
The EPR effect arises from two key abnormalities: (1) hypervasculature with enhanced endothelial permeability due to malformed, fenestrated blood vessels, and (2) impaired lymphatic drainage that reduces nanoparticle clearance from the tissue [85]. This combination enables nanoparticles to extravasate and accumulate preferentially in diseased tissues.
However, several physiological barriers limit the efficiency of passive targeting. Elevated interstitial fluid pressure (IFP) resulting from vascular leakage and poor lymphatic function can impede nanoparticle distribution once extravasated [85]. Additionally, dense extracellular matrix (ECM) rich in collagen, elastin, and hyaluronic acid creates a physical barrier to nanoparticle penetration, particularly for larger or highly charged particles that may interact electrostatically with matrix components [85].
Table 2: Passive Targeting Strategies and Implementation Approaches
| Strategy | Mechanism | Implementation Methods | Therapeutic Context |
|---|---|---|---|
| EPR Exploitation | Leverages leaky vasculature and impaired lymphatic drainage | Size optimization (10-200 nm); Surface charge modulation; Prolonged circulation | Solid tumors; Chronic inflammatory conditions [85] |
| TME Modulation | Remodels pathological barriers to improve delivery | ECM-degrading enzymes (hyaluronidase, collagenase); Vascular normalization agents | Dense stroma tumors; Fibrotic diseases [85] |
| Stimuli-Responsive Size Switching | Size reduction after tissue entry enhances penetration | pH-sensitive linkers; Enzyme-cleavable coatings; Photothermal size transition | Deep tissue penetration; Heterogeneous tumors [85] |
Active Targeting Strategies
Active targeting employs molecular recognition to achieve precise delivery to specific cell types or tissues. In redox pathology, this approach can direct therapeutics to cell populations experiencing elevated oxidative stress or expressing inflammation-specific markers.
Key targeting opportunities in inflammatory and redox-related conditions include:
- Endothelial markers: Vascular cell adhesion molecules (VCAM-1, ICAM-1) upregulated at inflammatory sites
- Immune cell receptors: Targeting specific macrophage subsets (M1/M2) or neutrophil populations
- Oxidative stress markers: Surface proteins modified by lipid peroxidation or specific receptors activated under oxidative conditions
- Metabolic markers: Transporters and receptors overexpressed in metabolically active inflammatory cells
Biomimetic approaches represent an advanced form of active targeting, utilizing natural membranes (e.g., from red blood cells, leukocytes, or cancer cells) or exosomes to confer enhanced immune evasion and homing capabilities [86] [87]. These systems retain source cell surface proteins and recognition molecules, enabling sophisticated biological targeting mechanisms.
Diagram 1: Active targeting mechanisms for redox pathology
Experimental Protocols for Targeting Validation
Synthesis of Tissue-Targeted Nanoparticles
Protocol: Preparation of Ligand-Functionalized Polymeric Nanoparticles for Redox Targeting
Materials:
- Biodegradable polymer (PLGA, PLA, or chitosan)
- Carbodiimide crosslinkers (EDC/NHS) for covalent conjugation
- Targeting ligand (antibody fragment, peptide, or aptamer)
- Therapeutic agent (antioxidant enzyme mimic, ROS-scavenger, or anti-inflammatory drug)
- Organic solvent (acetone, DMSO, or ethyl acetate)
- Aqueous surfactant solution (PVA, poloxamer)
Procedure:
- Nanoparticle Formation: Prepare blank nanoparticles using either single or double emulsion method. For drug-loaded systems, dissolve both polymer and therapeutic agent in organic phase before emulsification.
- Surface Functionalization:
- Activate carboxylic acid groups on nanoparticle surface using EDC/NHS chemistry (2-hour incubation in MES buffer, pH 6.0)
- Purify activated nanoparticles by centrifugation (15,000 × g, 15 minutes)
- Resuspend in coupling buffer (PBS, pH 7.4) containing targeting ligand (0.5-2 mg/mL)
- Incubate with gentle mixing for 4-12 hours at 4°C
- Purification: Remove unreacted ligands by gel filtration chromatography or extensive dialysis against PBS.
- Characterization: Determine particle size (dynamic light scattering), surface charge (zeta potential), and ligand density (BCA assay, fluorescence quantification, or ELISA).
Quality Control:
- Confirm ligand integrity after conjugation (SDS-PAGE, Western blot, or activity assay)
- Verify targeting functionality through receptor binding assays
- Determine drug loading efficiency and release kinetics
In Vitro Targeting Validation
Protocol: Cell-Specific Binding and Uptake Assay
Materials:
- Target cells (disease-relevant cell type)
- Control cells (non-target cell type)
- Fluorescently labeled targeted and non-targeted nanoparticles
- Flow cytometer or confocal microscopy system
- Cell culture reagents and buffers
Procedure:
- Cell Culture: Maintain target and control cells in appropriate media. Seed cells in 12-well plates (1×10^5 cells/well) 24 hours before experiment.
- Binding Competition: Pre-treat target cells with free targeting ligand (10-100× concentration) for 30 minutes to block receptors.
- Nanoparticle Incubation: Add fluorescent nanoparticles (50-200 μg/mL) to all wells and incubate for 1-4 hours at either 4°C (binding only) or 37°C (binding + internalization).
- Analysis:
- For flow cytometry: Trypsinize cells, wash, and resuspend in PBS containing 1% FBS. Analyze minimum 10,000 events per sample.
- For confocal microscopy: Fix cells with 4% PFA, stain nuclei and membrane, and image using appropriate filters.
Data Interpretation:
- Specific binding = (Target cell signal - Control cell signal)
- Receptor-mediated uptake = Difference between blocked and unblocked target cells
- Specificity index = (Target cell uptake)/(Control cell uptake)
In Vivo Biodistribution and Efficacy Studies
Protocol: Quantitative Biodistribution in Disease Models
Materials:
- Animal model of disease (e.g., inflammatory, cancer, or autoimmune model)
- Radiolabeled or fluorescently labeled nanoparticles (targeted and non-targeted)
- Imaging system (IVIS, PET/CT, or fluorescence imager)
- Tissue homogenization equipment
- Analytical methods (gamma counter, HPLC, or fluorescence plate reader)
Procedure:
- Dosing: Administer nanoparticles via appropriate route (IV, IP, or oral) at therapeutic dose.
- Time Points: Euthanize animals at multiple time points (1, 4, 12, 24, 48 hours) post-administration (n=5-6 per group).
- Tissue Collection: Harvest target tissues, clearance organs (liver, spleen, kidneys), and blood. Weigh all tissues immediately after collection.
- Sample Processing:
- For radiolabeled nanoparticles: Count tissue radioactivity using gamma counter and calculate % injected dose per gram (%ID/g)
- For fluorescent nanoparticles: Homogenize tissues, extract fluorescence, and quantify against standard curve
- Data Analysis:
- Calculate targeting index = (AUCtarget tissue targeted NPs)/(AUCtarget tissue non-targeted NPs)
- Determine selectivity ratio = (AUCtarget tissue)/(AUCnon-target tissue)
Efficacy Correlations:
- Correlate biodistribution data with therapeutic outcomes
- Assess target engagement through pharmacological markers
- Evaluate reduction in oxidative stress markers in target tissues
Nanotechnology Platforms for Redox Modulation
Various nanomaterial platforms have been engineered to address redox imbalances in inflammatory diseases, each with unique mechanisms and applications.
Inorganic Nanozymes and Antioxidant Systems
Inorganic nanoparticles with enzyme-mimetic properties represent a breakthrough in redox therapeutics. These "nanozymes" catalytically neutralize reactive species while offering superior stability compared to natural enzymes.
Cerium Oxide Nanoparticles: Exhibit mixed valence states (Ce³âº/Ceâ´âº) that enable catalytic scavenging of superoxide anions and hydrogen peroxide through auto-regeneration [84]. Applications demonstrated in acute kidney injury and neurodegenerative models.
Manganese-Based Nanomaterials: Mimic both superoxide dismutase (SOD) and catalase activities, providing cascade antioxidant protection [84]. Particularly valuable in inflammatory conditions with mitochondrial dysfunction.
Selenium Nanoparticles: Exhibit glutathione peroxidase (GPx)-like activity, especially effective against lipid peroxides [88]. Selenium incorporation enhances activity of endogenous antioxidant systems.
Organic Nanocarriers for Redox Cargo Delivery
Organic platforms provide versatile vehicles for delivering conventional antioxidants, enzymes, or gene therapies to target tissues.
Liposomes: Spherical phospholipid bilayers capable of encapsulating both hydrophilic (in aqueous core) and hydrophobic (within membrane) antioxidants. Surface modification with targeting ligands enhances specificity [86] [89].
Polymeric Nanoparticles: Biodegradable polymers (PLGA, chitosan) offer controlled release kinetics and excellent cargo protection. Chitosan-based systems particularly valuable for mucosal delivery due to permeation-enhancing properties [86].
Biomimetic Nanocarriers: Natural membrane-coated systems (erythrocyte, leukocyte, or platelet membranes) provide enhanced immune evasion and intrinsic targeting capabilities [86] [87]. Exosome-based systems enable natural intercellular communication and cargo delivery.
Table 3: Nanotechnology Platforms for Redox Targeting Applications
| Platform | Key Components | Mechanism of Action | Targeting Applications |
|---|---|---|---|
| Inorganic Nanozymes | Cerium oxide, Manganese, Selenium | Catalytic ROS scavenging; Enzyme mimicry (SOD, catalase, GPx) | Acute kidney injury [84]; Neuroinflammation; Cardiovascular ischemia |
| Polymeric NPs | PLGA, Chitosan, Dendrimers | Controlled release; Cargo protection; Surface functionalization | Inflammatory bowel disease [84]; Multiple sclerosis [84]; Periodontitis [84] |
| Lipid-Based Systems | Liposomes, Solid lipid NPs | Membrane fluidity; Fusion with cells; Versatile encapsulation | Acute myocardial infarction [89]; Cancer therapy [86] |
| Biomimetic Systems | Cell membranes, Exosomes | Immune evasion; Natural targeting ligands; Biological communication | Immune-mediated diseases [87]; Complex inflammatory conditions |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Nanotechnology Targeting Studies
| Reagent/Category | Function | Example Applications |
|---|---|---|
| Biodegradable Polymers | Nanoparticle matrix; Controlled release | PLGA (synthetic), Chitosan (natural) for drug encapsulation and sustained delivery [86] |
| Crosslinking Reagents | Surface ligand conjugation; Stabilization | EDC/NHS chemistry for covalent attachment of targeting moieties to nanoparticle surface |
| Targeting Ligands | Specific molecular recognition | Antibodies/fragments, peptides (RGD), aptamers for active targeting [85] [86] |
| Fluorescent Probes | Tracking and quantification | DIR, Cy dyes, quantum dots for in vivo imaging and biodistribution studies |
| ROS-Sensitive Materials | Redox-responsive release | Thioketal polymers, phenylboronic acid derivatives for triggered drug release in oxidative environments [87] |
| Characterization Tools | Physicochemical analysis | DLS (size), Zeta potentiometer (charge), HPLC (drug loading), TEM (morphology) |
Diagram 2: Nanotechnology platform selection for redox targeting
The strategic integration of nanotechnology with tissue-targeting approaches represents a paradigm shift in addressing redox dysregulation in inflammatory diseases. The multi-parameter optimization of nanoparticle design—encompassing size, charge, shape, and surface functionality—enables researchers to overcome the biological barriers that have limited conventional antioxidant therapies.
Future advancements in this field will likely focus on several key areas: (1) development of increasingly sophisticated stimuli-responsive systems that activate only within specific redox environments, (2) integration of artificial intelligence and computational modeling to accelerate nanomaterial design and predict in vivo behavior, and (3) advancement of personalized targeting approaches based on individual patient disease signatures.
As these technologies mature, the translation of targeted nanotherapies from preclinical models to clinical application will require rigorous attention to manufacturing scalability, long-term safety evaluation, and regulatory considerations. The systematic approach outlined in this guide provides a foundation for developing the next generation of redox-targeted therapeutics with enhanced specificity and efficacy.
Overcoming Compensatory Mechanisms and Pathway Redundancy in Redox Networks
Redox signaling is a fundamental regulatory process in biology, involving the transfer of electrons that modifies the structure and function of biomolecules. In physiological conditions, cells maintain redox homeostasis through a delicate balance between oxidant generation and antioxidant capacity [90] [91]. This equilibrium is governed by sophisticated networks characterized by significant pathway redundancy and compensatory mechanisms that ensure system stability despite fluctuating metabolic demands or transient stressors. However, in pathological states, these same adaptive systems present a formidable challenge for therapeutic intervention, as targeted inhibition of single pathways often triggers compensatory activation of alternative circuits that restore redox balance and confer treatment resistance [1] [92].
The clinical implications of redox network robustness are particularly evident in chronic diseases involving inflammatory components, including cancer, neurodegenerative disorders, and cardiovascular conditions [90] [93] [94]. In cancer biology, therapeutic targeting of oncogenic signaling pathways frequently engages feedback loops that restore proliferative signals and promote survival. Similarly, in neurodegenerative diseases, the multifaceted nature of oxidative damage and the brain's layered antioxidant defenses have complicated the development of effective neuroprotective strategies [94]. This whitepaper examines the molecular architecture of redox compensation mechanisms and provides technical guidance for developing strategies that overcome these adaptive responses in disease contexts.
Core Compensatory Circuits in Redox Signaling Networks
Major Redox Buffering Systems and Their Interconnections
Cellular redox homeostasis is maintained through several interconnected buffering systems that demonstrate functional redundancy. The principal antioxidant systems include the glutathione (GSH) system, the thioredoxin (Trx) system, and the NRF2-mediated antioxidant response [1] [92]. These systems work in concert to regulate reactive oxygen species (ROS) levels, but when one system is compromised, others frequently undergo compensatory upregulation.
The thioredoxin system, comprising thioredoxin (Trx), thioredoxin reductase (TrxR), and NADPH, represents a particularly robust compensatory circuit. TrxR is a selenoprotein that reduces oxidized Trx using NADPH as an electron donor, and this system plays crucial roles in regulating transcription factor activity, protein folding, and sulfur metabolism. When TrxR is inhibited, cells often upregulate glutathione-dependent pathways to maintain redox balance, thereby circumventing the therapeutic effects of TrxR-targeted agents [92]. Similarly, the NRF2 transcription factor serves as a master regulator of antioxidant gene expression, controlling the production of enzymes including NAD(P)H quinone dehydrogenase 1 (NQO1), glutathione peroxidase 4 (GPX4), and peroxiredoxin 1 (PRDX1) [1].
Table 1: Major Compensatory Antioxidant Systems in Mammalian Cells
| System Component | Primary Function | Compensatory Partners | Cellular Localization |
|---|---|---|---|
| Thioredoxin (Trx) | Protein disulfide reduction | Glutathione system | Cytosol, mitochondria, nucleus |
| Thioredoxin Reductase (TrxR) | Reduction of oxidized Trx using NADPH | Glutathione reductase | Cytosol, mitochondria |
| Glutathione (GSH) | Direct ROS scavenging, enzyme cofactor | Thioredoxin system | Cytosol, mitochondria, nucleus |
| NRF2 | Transcriptional activation of antioxidant genes | FOXO, HIF-1α signaling | Nucleus (when activated) |
| Superoxide Dismutase (SOD) | Superoxide dismutation to Hâ‚‚Oâ‚‚ | Catalase, GPx | Cytosol (SOD1), mitochondria (SOD2) |
| Peroxiredoxin (Prx) | Peroxide reduction | GPx, Catalase | Throughout cell |
Quantitative Assessment of Compensatory Activation
Evidence for compensatory pathway activation comes from rigorous experimental models. In a systematic investigation of combination therapy targeting redox adaptation, researchers demonstrated that mTOR inhibition alone increased TrxR expression and activity in cancer cells. Specifically, treatment with everolimus (5 μM, 24h) resulted in a 2.3-fold increase in TrxR activity in HCT116 colorectal carcinoma cells, while auranofin (a TrxR inhibitor) monotherapy induced adaptive upregulation of mTOR signaling pathway components [92]. This reciprocal compensation maintained viability despite significant individual pathway inhibition, with monotherapies achieving only 15-30% reduction in cell viability compared to 75-85% reduction with coordinated pathway blockade [92].
Similar compensatory dynamics are observed in neurological disorders. In models of ischemic stroke, inhibition of mitochondrial ROS sources leads to increased activity of NADPH oxidases, particularly NOX2 and NOX4 isoforms, highlighting the challenges in targeting single enzymatic ROS generators in complex neurological conditions [95].
Experimental Approaches for Mapping Redox Compensation
Methodologies for Quantifying Redox Pathway Interactions
Comprehensive Redox State Assessment
Protocol: Multiparameter Redox Status Analysis
- Intracellular ROS Measurement: Cells are stained with 10 μM 2,7-dichlorofluorescein diacetate (DCFH-DA) for 30 minutes at 37°C before collection. Fluorescence intensity is quantified via flow cytometry (excitation 488 nm, emission 525 nm) to assess general oxidative stress [92].
- Antioxidant Enzyme Activity Profiling:
- TrxR Activity: Measured using endpoint insulin reduction assay. Cell lysates are incubated with insulin and NADPH, and TrxR activity is determined by monitoring NADPH consumption at 340 nm [92].
- SOD Activity: Employed using xanthine oxidase-cytochrome c method, measuring superoxide-mediated cytochrome c reduction inhibition.
- GPx Activity: Quantified by NADPH consumption monitoring in the presence of glutathione reductase, GSH, and cumene hydroperoxide.
- GSH/GSSG Ratio: Determined using the Tietze enzymatic recycling method with slight modifications, providing insight into the glutathione system redox status.
Pathway Activation Mapping
Protocol: Compensatory Signaling Analysis
- Western Blot for Adaptive Signaling: Cells are treated with targeted inhibitors (e.g., mTOR or TrxR inhibitors) for 2-24 hours. Lysates are probed for phosphorylation of mTOR pathway components (p-S6K, p-4E-BP1), NRF2 stabilization, and stress kinases (p-JNK, p-p38) [92].
- Autophagy Flux Monitoring: A tandem mRFP-GFP-tagged LC3 lentivirus system is employed. Autophagic flux is quantified by fluorescence microscopy, counting red-only puncta (autolysosomes) versus yellow puncta (autophagosomes) [92].
- Gene Expression Profiling: RNA sequencing or qRT-PCR analysis of NRF2 target genes (NQO1, HO-1, GCLM), glutathione synthesis enzymes, and xenobiotic metabolism genes to identify compensatory transcriptional programs.
Advanced Computational Modeling of Redox Networks
The complexity of redox signaling networks necessitates computational approaches to predict compensatory behaviors. The "redox code" concept provides a framework for understanding how NADH/NAD+, NADPH/NADP+, GSH/GSSG, and other redox couples integrate to determine cellular responses [1] [95]. Computational models can simulate network behavior under various perturbation scenarios, identifying critical nodes where intervention is most likely to overcome compensation.
Table 2: Experimental Models for Studying Redox Compensation
| Model System | Key Measurable Parameters | Advantages | Limitations |
|---|---|---|---|
| Cancer Cell Lines (HCT116, SGC-7901) | CI values for drug combinations, ROS flux, antioxidant enzyme activities | High throughput, genetically tractable | May not reflect tissue context |
| Primary Cell Cultures | Cell-type specific compensation patterns | More physiologically relevant | Limited lifespan in culture |
| Xenograft Models | Tumor growth inhibition, toxicity assessment, biomarker analysis | In vivo context, therapeutic assessment | Species differences in redox regulation |
| Ischemic Stroke Models | Infarct volume, lipid peroxidation products, mitochondrial function | Clinically relevant pathophysiology | Technical complexity, ethical considerations |
Strategic Approaches to Overcome Redox Compensation
Rational Combination Therapies
Simultaneous targeting of complementary redox systems has demonstrated significant promise in overcoming compensatory resistance mechanisms. The combination of mTOR and TrxR inhibitors represents a paradigmatic example of this approach. Mechanistically, mTOR inhibitors (e.g., everolimus) increase ROS production but simultaneously trigger compensatory upregulation of TrxR. Concurrent administration of TrxR inhibitors (e.g., auranofin) blocks this adaptive response, leading to irreversible oxidative stress and cell death [92].
In preclinical models, this combination yielded dramatic synergistic effects. The combination index (CI) for auranofin + everolimus was approximately 0.3 in HCT116 xenograft models, indicating strong synergy [92]. This coordinated targeting approach suppressed tumor growth by >80% compared to monotherapies, without significant toxicity signs [92]. The molecular mechanisms driving this synergy involve coordinated induction of oxidative stress, autophagy, endoplasmic reticulum (ER) stress, and JNK pathway activation [92].
Similar principles apply in neurological contexts. In ischemic stroke, where multiple simultaneous ROS sources (mitochondrial RET, NOX enzymes, xanthine oxidase) contribute to injury, combinatorial approaches targeting different generators show enhanced efficacy compared to single-source inhibition [95].
Temporal Sequencing of Interventions
An alternative to simultaneous combination therapy involves precisely timed sequential inhibition based on the kinetics of compensatory pathway activation. This approach requires detailed understanding of the temporal patterns of adaptive responses. For instance, in the mTOR/TrxR model, TrxR upregulation occurs within 4-8 hours of mTOR inhibition, suggesting that administration of TrxR inhibitors within this window may preempt establishment of compensation [92].
In ischemic stroke, the concept of temporal sequencing is particularly relevant, with different ROS sources predominating at various phases of injury. Reverse electron transport (RET) at mitochondrial complex I generates a massive ROS burst within seconds of reperfusion, while ferroptosis contributes to cell death hours later [95]. This temporal hierarchy creates opportunities for staged interventions targeting early and delayed injury mechanisms sequentially.
Visualization of Key Redox Networks and Experimental Workflows
Redox Compensation Circuitry in Disease
Experimental Workflow for Evaluating Redox Compensation
The Scientist's Toolkit: Essential Research Reagents and Models
Table 3: Key Research Reagent Solutions for Redox Compensation Studies
| Reagent/Category | Specific Examples | Primary Research Application | Considerations for Use |
|---|---|---|---|
| TrxR Inhibitors | Auranofin, D9, Shikonin | Block thioredoxin system, test compensatory mechanisms | Monitor GSH system upregulation; potential off-target effects |
| mTOR Inhibitors | Everolimus, Rapamycin, AZD8055 | Inhibit mTOR signaling, induce metabolic stress | Triggers multiple compensatory pathways; dose optimization critical |
| ROS Detection Probes | DCFH-DA, MitoSOX, DHE | Quantify general or site-specific ROS production | Consider compartmentalization; validate specificity |
| Antioxidant Enzyme Activity Assays | Insulin reduction (TrxR), XO-cytochrome c (SOD) | Measure activity of specific antioxidant systems | Normalize to protein content; control for assay interference |
| NRF2 Activators/Inhibitors | Sulforaphane, ML385 | Modulate antioxidant transcriptional responses | Useful for validating NRF2 role in compensation |
| GSH System Modulators | BSO, GSH-MEE | Deplete or augment glutathione system | Monitor viability effects; consider temporal aspects |
| Combination Index Analysis Software | CompuSyn, Chalice | Quantify synergistic, additive, or antagonistic drug interactions | Use multiple effect levels for robust CI calculation |
| Xenograft Models | HCT116, SGC-7901 cell lines | In vivo validation of combination efficacy | Monitor toxicity; assess biomarker modulation |
Overcoming compensatory mechanisms and pathway redundancy in redox networks represents a formidable but surmountable challenge in therapeutic development for inflammatory diseases and cancer. The strategic integration of rational combination therapies, temporal sequencing approaches, and comprehensive network analysis enables researchers to anticipate and circumvent adaptive resistance mechanisms. As our understanding of the "redox code" deepens through advanced computational modeling and multi-omics integration, the precision of redox-directed therapies will continue to improve, offering new opportunities for effective intervention in complex diseases characterized by redox dysregulation [1] [95] [94]. The experimental frameworks and technical approaches outlined in this whitepaper provide a roadmap for systematically addressing the challenges of redundancy and compensation in redox networks, ultimately facilitating the development of more durable and effective therapeutic strategies.
Redox signaling, the process by which reactive oxygen species (ROS) and reactive nitrogen species (RNS) function as signaling molecules, is a critical mediator in the dynamic interactions between organisms and their external environment, profoundly influencing both the onset and progression of various diseases [96]. Under physiological conditions, a delicate redox homeostasis is maintained where oxidative free radicals generated by the mitochondrial oxidative respiratory chain, endoplasmic reticulum, and NADPH oxidases are effectively neutralized by endogenous antioxidant responses [96]. The nuclear factor erythroid 2-related factor 2 (NRF2) serves as the master regulator of antioxidant gene expression, elevating the synthesis of superoxide dismutase (SOD), catalase, and key molecules like nicotinamide adenine dinucleotide phosphate (NADPH) and glutathione (GSH) to maintain cellular redox balance [96] [4].
Disruption of this finely tuned equilibrium is closely linked to the pathogenesis of a wide range of inflammatory and metabolic diseases [96] [4] [97]. The relationship between oxidative stress and inflammation is not merely sequential but synergistic, establishing a pathogenic loop that sustains chronic inflammation in conditions including atherosclerosis, neurodegeneration, metabolic syndrome, fibromyalgia, and autoimmune disorders [4] [98] [97]. Recent advances have broadened our understanding of the molecular mechanisms underpinning this dysregulation, highlighting the pivotal roles of genomic instability, epigenetic modifications, protein degradation, and metabolic reprogramming [96]. These findings provide a foundation for exploring redox regulation as a mechanistic basis for improving therapeutic strategies, particularly through optimized timing and dosing of interventions aimed at re-establishing redox balance [96] [37].
Redox Dynamics and Pathological Transitions
The Bidirectional Nature of Redox Imbalance
The traditional view of redox imbalance has predominantly focused on oxidative stress (OS), characterized by an overproduction of ROS and RNS that overwhelms antioxidant defenses, leading to damage of cellular components [4]. However, emerging evidence underscores the equally significant, yet often overlooked, role of reductive stress (RS)—a condition where an excess of reducing equivalents (NADH, NADPH, GSH) disrupts redox homeostasis [4]. This bidirectional perspective is crucial for understanding therapeutic windows, as both oxidative and reductive extremes can contribute to inflammatory pathogenesis.
Redox imbalance plays a pivotal role in regulating inflammation, influencing both the onset and progression of various inflammatory conditions [4]. The dynamic interplay between OS and RS acts as interconnected modulators of immune function, where OS activates inflammatory pathways through redox-sensitive transcription factors like nuclear factor-kappa B (NF-κB), while chronic RS can paradoxically impair immune defense, alter redox-sensitive signaling, and contribute to disease progression [4]. This bidirectional imbalance establishes a pathological continuum that evolves throughout disease progression, creating distinct intervention windows that require specific therapeutic approaches [4] [37].
Molecular Mechanisms of Redox Signaling in Inflammation
At the molecular level, redox signaling influences inflammatory processes through several key mechanisms:
- NF-κB Activation: ROS can activate the IκB kinase (IKK), leading to phosphorylation and degradation of IκB proteins, which frees NF-κB to translocate into the nucleus and promote transcription of pro-inflammatory genes encoding cytokines, adhesion molecules, and enzymes like cyclooxygenase-2 (COX-2) and inducible nitric oxide synthase (iNOS) [4].
- Inflammasome Activation: ROS are essential for the activation of the NOD-like receptor family pyrin domain containing 3 (NLRP3) inflammasome, a multiprotein complex responsible for cleaving pro-caspase-1 into its active form, which in turn activates interleukin (IL)-1β and IL-18, key cytokines in inflammatory propagation [4].
- Mitogen-Activated Protein Kinase (MAPK) Signaling: ROS inhibit MAPK phosphatases by oxidizing their catalytic cysteine residues, thereby prolonging MAPK signaling [4]. The p38 MAPK branch plays a key role in stabilizing mRNAs of inflammatory mediators and modulating chromatin accessibility via histone-modifying enzymes [4].
- Nrf2-Keap1 Pathway: Under oxidative stress, critical cysteine residues on Keap1 are modified, leading to stabilization and nuclear translocation of Nrf2, which binds to antioxidant response elements (AREs) and induces transcription of cytoprotective genes [4]. Nrf2 activity not only mitigates oxidative damage but also exerts anti-inflammatory effects by modulating macrophage polarization and suppressing NF-κB-driven transcription [4] [99].
Table 1: Key Redox-Sensitive Signaling Pathways in Inflammatory Diseases
| Pathway | Redox Regulation | Inflammatory Outcome | Disease Associations |
|---|---|---|---|
| NF-κB | ROS activate IKK complex | Increased pro-inflammatory cytokine production (TNF-α, IL-6, IL-1β) | Atherosclerosis, Rheumatoid Arthritis, IBD [4] |
| NLRP3 Inflammasome | ROS trigger assembly and activation | Caspase-1 activation, IL-1β and IL-18 maturation | Gout, Type 2 Diabetes, Fibromyalgia [4] [98] |
| Nrf2-Keap1 | Oxidized Keap1 releases Nrf2 | Antioxidant gene expression (HO-1, NQO1, GCLC) | COPD, Diabetic Complications [4] [37] |
| MAPK | ROS inhibit MAPK phosphatases | Sustained inflammatory signaling | Neuroinflammation, Metabolic Syndrome [4] |
Temporal Considerations in Redox-Targeted Interventions
Disease Stage-Specific Redox Profiles
The therapeutic window for redox-targeted interventions is highly dependent on disease stage, as the redox environment evolves throughout pathological progression. Early in inflammatory diseases, compensated oxidative stress typically occurs, where adaptive responses such as Nrf2 activation partially counteract ROS increases [37]. During this phase, low-level ROS may even function as signaling molecules that activate protective mechanisms [96] [4]. As diseases progress to established chronic conditions, decompensated oxidative stress develops, characterized by sustained ROS production that overwhelms antioxidant defenses, leading to macromolecular damage and tissue injury [37]. In advanced disease stages, reductive stress may emerge as a maladaptive response or as a consequence of excessive antioxidant therapy, creating a different pathological environment that requires distinct therapeutic approaches [4].
In hypertension and diabetes mellitus, oxidative stress serves as both an instigator and amplifier of cardiometabolic dysfunction [37]. Early in diabetes, hyperglycemia-induced ROS production worsens beta-cell failure and insulin resistance through pathways such as the AGE-RAGE signaling, protein kinase C (PKC) activation, and the polyol pathway [37]. In established disease, chronic oxidative stress accelerates endothelial dysfunction, insulin resistance, and end-organ damage, thereby perpetuating disease progression [37]. The transition from early to late disease stages is marked by shifts in oxidant-antioxidant balance that create different therapeutic requirements at each phase [37].
Chronobiological Influences on Redox Homeostasis
Emerging evidence suggests that redox homeostasis exhibits circadian oscillations that influence both disease susceptibility and treatment efficacy. The timing of antioxidant administration relative to these biological rhythms may significantly impact therapeutic outcomes, though this area remains underexplored in clinical studies [37]. Mitochondrial function, ROS production, and antioxidant enzyme activities all demonstrate circadian patterns that align with metabolic cycles [91]. Understanding these temporal dynamics is essential for optimizing dosing schedules to align with periods of peak oxidative stress or maximal antioxidant capacity.
In conditions like fibromyalgia, symptoms often exhibit diurnal variations, with pain and fatigue frequently worsening at specific times of day [98]. These clinical patterns may reflect underlying circadian redox fluctuations, suggesting that chronotherapeutic approaches—adjusting treatment timing to biological rhythms—could enhance efficacy of redox-targeted interventions [98]. Future research should prioritize mapping these circadian redox patterns in different inflammatory conditions to identify optimal intervention windows.
Table 2: Disease Stage-Specific Redox Profiles and Intervention Strategies
| Disease Stage | Redox Status | Key Biomarkers | Recommended Intervention Strategy |
|---|---|---|---|
| Early/Preclinical | Compensated Oxidative Stress | Mild increases in Hâ‚‚Oâ‚‚, early Nrf2 activation | Low-dose Nrf2 activators, Lifestyle interventions [37] |
| Established Chronic Disease | Decompensated Oxidative Stress | Elevated MDA, 8-OHdG, F2-isoprostanes | Targeted antioxidants, Combination therapies [37] [100] |
| Advanced Disease with Complications | Mixed Oxidative-Reductive Stress | Simultaneous oxidative damage and elevated GSH/GSSG ratio | Balanced redox modulators, Personalized dosing [4] [37] |
| Treatment-Resistant Disease | Complex Redox Remodeling | Altered mitochondrial function, NOX upregulation | Mitochondria-targeted antioxidants, NOX inhibitors [37] |
Dosing Strategies for Redox-Targeted Therapies
Principles of Redox Pharmacology
Conventional dosing approaches for antioxidants have largely failed in clinical trials, highlighting the need for more sophisticated redox pharmacology principles [96] [4] [37]. The bidirectional nature of redox signaling necessitates a departure from traditional "more is better" antioxidant approaches, as excessive reduction can be equally problematic as excessive oxidation [4]. Several key principles should guide dosing strategies for redox-targeted therapies:
- Hormetic Response: Many redox-active compounds exhibit biphasic dose responses, where low doses activate adaptive stress response pathways (e.g., Nrf2) that enhance cellular resilience, while high doses may cause toxicity or disrupt redox signaling [96] [4]. Effective dosing must identify the therapeutic range that maximizes adaptive signaling without causing reductive stress [4].
- Context-Specific Dosing: Optimal dosing varies significantly based on disease stage, tissue environment, and individual redox status [96] [37]. For instance, dosing requirements differ substantially between conditions primarily driven by oxidative stress (e.g., paraquat poisoning) versus those with complex, multifactorial etiologies (e.g., cancer, neurodegenerative diseases) [96].
- Combination Approaches: Given the complexity of redox networks, synergistic combinations of agents targeting different aspects of redox balance often show greater efficacy than single agents [101] [37]. These combinations must be carefully balanced to avoid over-correction toward reductive stress [4].
Biomarker-Guided Dose Optimization
The development of validated redox biomarkers is essential for guiding dose optimization in both research and clinical practice [37] [100]. Different biomarkers provide information about various aspects of redox homeostasis and oxidative damage:
- Lipid Peroxidation: Malondialdehyde (MDA) measured via Thiobarbituric Acid-Reactive Substances (TBARS) assay and F2-isoprostanes quantified by chromatography-mass spectrometry provide specific measures of oxidative damage to lipids [37].
- DNA Oxidation: 8-hydroxy-2'-deoxyguanosine (8-OHdG) is a well-established biomarker of DNA oxidation, with levels quantified using high-performance liquid chromatography (HPLC) coupled with electrochemical or mass spectrometry detection [37] [100].
- Protein Oxidation: Protein carbonyl groups serve as reliable biomarkers of protein oxidation, typically detected through derivatization with 2,4-dinitrophenylhydrazine (DNPH) and spectrophotometric quantification [37].
- Antioxidant Capacity: Measurements of superoxide dismutase (SOD), catalase, glutathione peroxidase (GPx) activities, and reduced-to-oxidized glutathione ratios (GSH/GSSG) provide information about antioxidant defense status [37].
The Oxidative Balance Score (OBS) has emerged as a comprehensive assessment tool that quantifies the balance between dietary and lifestyle-derived antioxidants and pro-oxidants [37]. Higher OBS values demonstrate significant inverse relationships with chronic kidney disease risk and serum uric acid levels, highlighting its potential utility in guiding dietary and therapeutic interventions [37].
Experimental Protocols for Evaluating Timing and Dosing
Comprehensive Redox Status Assessment
Objective: To evaluate dynamic changes in redox homeostasis following therapeutic interventions at different disease stages and dosing regimens.
Materials and Methods:
- Sample Collection: Collect tissue, blood, and urine samples at multiple timepoints (0, 2, 6, 12, 24 hours post-intervention) to capture dynamic changes [37] [100].
- Oxidative Damage Markers:
- Lipid Peroxidation: Measure MDA using TBARS assay and F2-isoprostanes via gas or liquid chromatography-mass-mass spectrometry (HPLC/MS-MS) [37].
- DNA Oxidation: Quantify 8-OHdG using high-performance liquid chromatography with electrochemical detection (HPLC-ECD) or ELISA [37] [100].
- Protein Oxidation: Assess protein carbonyl content through derivatization with DNPH and spectrophotometric quantification at 370-375 nm [37].
- Antioxidant Defense Capacity:
- Redox Signaling Molecules:
Data Analysis: Establish temporal patterns of redox parameter changes and identify optimal sampling timepoints that best reflect therapeutic effects. Determine correlation between redox biomarker modulation and functional outcomes.
Time-Staged Therapeutic Intervention Protocol
Objective: To determine optimal intervention windows by administering redox-targeted therapies at different disease stages.
Experimental Design:
- Animal Model: Utilize established disease models (e.g., Freund's complete adjuvant-induced arthritis for inflammatory diseases, high-fat diet/streptozotocin models for diabetes) [101] [37].
- Intervention Groups:
- Prophylactic: Initiate treatment before disease induction
- Early Intervention: Begin treatment at first signs of pathology
- Established Disease: Start treatment after full disease manifestation
- Advanced Disease: Administer treatment during complication phase
- Dosing Regimens: For each timing group, test multiple dosing strategies:
- Low-dose continuous
- High-dose pulsed
- Dose-escalation
- Combination therapy
Assessment Parameters:
- Clinical Outcomes: Disease-specific clinical scores (e.g., arthritic score, pain sensitivity, metabolic parameters) [101] [98].
- Biomarker Monitoring: Comprehensive redox status assessment as described in Protocol 5.1.
- Tissue Analysis: Histopathological evaluation of target tissues and molecular analyses (Western blot, PCR, immunohistochemistry) of redox and inflammatory pathways [101].
Statistical Analysis: Compare efficacy across timing and dosing groups using appropriate statistical methods. Identify critical windows where interventions provide maximal benefit.
Visualization of Redox Signaling Pathways and Therapeutic Targets
Redox Signaling in Inflammation and Therapeutic Modulation
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 3: Key Research Reagent Solutions for Redox Timing and Dosing Studies
| Reagent/Category | Specific Examples | Research Application | Timing/Dosing Considerations |
|---|---|---|---|
| NRF2 Activators | Sulforaphane, Bardoxolone methyl, Dimethyl fumarate | Modulate antioxidant response element signaling | Early intervention; low-dose for priming, high-dose for established disease [4] [99] |
| NOX Inhibitors | GKT137831, Apocynin, VAS2870 | Target specific NADPH oxidase isoforms | Prophylactic or early disease; continuous dosing required [4] [37] |
| Mitochondria-Targeted Antioxidants | MitoQ, SkQ1, SS-31 | Accumulate in mitochondria to reduce mitochondrial ROS | Established disease with mitochondrial dysfunction; requires precise dosing to avoid reductive stress [37] |
| Redox Biosensors | roGFP, HyPer, Grx1-roGFP2 | Real-time monitoring of redox dynamics in live cells | Critical for timing studies; enables temporal mapping of redox changes [37] |
| Oxidative Stress Biomarkers | 8-OHdG ELISA kits, MDA assay kits, Protein carbonyl assays | Quantify oxidative damage to biomolecules | Guide dosing adjustments; establish therapeutic windows [37] [100] |
| Thiol Modulators | N-acetylcysteine, Glutathione, Diselenides | Modify redox status of protein cysteine residues | Biphasic dosing; context-dependent effects [4] [97] |
The optimization of timing and dosing considerations for redox-targeted interventions represents a critical frontier in inflammatory disease therapeutics. The complex, bidirectional nature of redox signaling demands a sophisticated approach that moves beyond conventional antioxidant strategies toward temporally precise and dose-optimized interventions [96] [4]. Future advances will require the development of more precise assessment methods for redox homeostasis, the judicious selection of oxidative modulators based on disease characteristics, the rationalization of delivery systems, and the creation of precise interventions that consider various factors to achieve optimal modulation [91].
Key priorities for future research include:
- Developing real-time redox monitoring technologies that can guide therapeutic timing in individual patients [37]
- Establishing stage-specific treatment algorithms based on comprehensive redox phenotyping [37]
- Exploring chronotherapeutic approaches that align with circadian redox rhythms [98] [37]
- Validating personalized dosing strategies through biomarker-guided clinical trials [37] [100]
The integration of these advanced approaches with lifestyle modifications that support redox balance, such as Mediterranean or DASH diets rich in polyphenols, represents a comprehensive strategy for addressing redox dysregulation across the spectrum of inflammatory diseases [37]. As our understanding of redox dynamics continues to evolve, so too will our ability to intervene with precisely timed and dosed therapies that restore homeostasis while respecting the complex signaling functions of redox molecules.
The intricate role of redox signaling in cellular homeostasis presents a unique therapeutic paradox in oncology. Reactive oxygen species (ROS) function as critical signaling molecules in cancer biology, promoting proliferation, angiogenesis, and metastasis at controlled levels while inducing lethal damage when exceeding the cell's buffering capacity [102]. To survive under chronic oxidative stress, cancer cells become dependent on a hyperactive antioxidant shield, primarily orchestrated by the NRF2, glutathione (GSH), and thioredoxin (Trx) systems [102]. This rewired redox state creates a therapeutically exploitable vulnerability, wherein pharmacologically tipping the redox balance beyond the threshold of tolerance offers a rational approach to eliminate malignant cells [102]. The strategic combination of redox modulators with conventional treatments represents a novel frontier in targeted cancer therapy, leveraging cancer-specific redox adaptations to overcome drug resistance and improve therapeutic outcomes.
Redox Signaling Foundations in Cancer Biology
The Dual Nature of ROS in Malignancy
The "Redox Paradox" describes the complex interplay where ROS simultaneously drives and can be used to combat malignancy [102]. In cancer cells, heightened ROS levels act as pro-tumorigenic factors through multiple mechanisms:
- Oncogenic Signaling Enhancement: Elevated ROS, particularly Hâ‚‚Oâ‚‚, promote proliferation through oxidative inactivation of tumor-suppressor phosphatases such as PTEN, which drives the PI3K/AKT/mTOR pathway [102].
- Metabolic Adaptation: Cancer cells exhibit increased ROS production through heightened metabolic activity, mitochondrial dysfunction, and NADPH oxidase (NOX) enzyme activation [102].
- Survival Dependence: To thrive amidst self-inflicted oxidative stress, cancers engineer powerful antioxidant defenses, creating a precarious balance that can be therapeutically exploited [102].
Master Regulators of Cancer Redox Homeostasis
Cancer cells co-opt fundamental cellular defense systems to maintain their malignant redox state:
- NRF2-KEAP1 Axis: The cornerstone of cellular antioxidant response, NRF2 under basal conditions is bound by KEAP1 and targeted for degradation. Under oxidative stress, KEAP1 cysteine modifications release NRF2, allowing nuclear translocation and transcription of cytoprotective genes [103].
- Glutathione System: This tripeptide thiol (GSH) constitutes one of the primary cellular redox buffers, with cancer cells frequently maintaining elevated GSH levels to counteract persistent oxidative stress [102].
- Thioredoxin System: Comprising thioredoxin (Trx), thioredoxin reductase (TrxR), and NADPH, this system regulates protein dithiol-disulfide balance and serves as a backup when GSH systems are compromised [102].
Diagram 1: NRF2-mediated antioxidant response in cancer cells. ROS oxidize KEAP1, releasing NRF2 to activate antioxidant gene expression, promoting survival.
Strategic Combination Approaches
Overcoming Therapy-Induced Senescence (TIS)
Cellular senescence, particularly therapy-induced senescence (TIS), has emerged as a pivotal contributor to tumor drug resistance. Senescent cells in the tumor microenvironment acquire a highly active secretome termed the senescence-associated secretory phenotype (SASP), which includes growth factors, chemokines, cytokines, and proteases that significantly reshape the TME, enabling cancer cells to evade immune destruction [104]. Redox signaling networks are deeply intertwined with this process, creating a redox-senescence feedback loop that drives tumor adaptation under therapeutic pressure [104].
Combination Strategy: Redox modulators can be strategically combined with senescence-inducing chemotherapies to target the resulting senescent cell population. This approach utilizes two sequential mechanisms:
- Conventional chemotherapies (e.g., cisplatin, doxorubicin) induce DNA damage and initiate senescence through p53 activation and CDK inhibitor transactivation [104].
- Redox-directed agents then selectively eliminate senescent cells by exploiting their altered redox state, characterized by elevated ROS and SASP amplification [104].
Experimental evidence demonstrates that redox-balanced combination strategies can reinforce DNA damage-induced senescence while preventing the pro-tumorigenic effects of SASP, ultimately restraining tumor relapse [104].
Targeting NRF2-Mediated Defense Mechanisms
Hyperactivation of the NRF2-mediated antioxidant response represents a common resistance mechanism across multiple cancer types. Cancer cells exploit this pathway to enhance detoxification and combat therapy-induced oxidative stress [102] [103].
Combination Strategy: NRF2 inhibitors paired with ROS-generating therapies.
Table 1: NRF2-Targeting Combination Approaches
| NRF2 Inhibitor | Combination Therapy | Mechanism of Action | Experimental Evidence |
|---|---|---|---|
| Brusatol | Cisplatin, Doxorubicin | Global protein synthesis inhibition, depleting NRF2 levels | Potentiates cytotoxicity in lung, pancreatic cancer models |
| ML385 | Radiotherapy | Binds NRF2 directly, preventing ARE binding | Enhances radiation sensitivity in lung cancer models |
| OK-1 | 5-FU, Oxaliplatin | Disrupts NRF2-MafG association | Shows efficacy in colorectal cancer models |
This approach is particularly effective because inhibiting the master antioxidant regulator disrupts the core antioxidant response, leaving cancer cells vulnerable to ROS-generating conventional therapies [102].
Inducing Ferroptosis for Selective Cell Death
Ferroptosis is an iron-dependent form of cell death characterized by impaired glutathione metabolism, lipid peroxidation, and mitochondrial failure [105]. This non-apoptotic cell death pathway can be harnessed to eliminate cancer cells that resist conventional apoptosis [102].
Combination Strategy: Glutathione system disruptors with standard chemotherapies.
- Cysteine Uptake Inhibitors: Sulfasalazine or erastin potently induce ferroptosis by blocking system Xcâ» cysteine/glutamate antiporter, depleting GSH reserves [102].
- GPX4 Inhibition: Direct targeting of glutathione peroxidase 4, the key enzyme preventing lipid peroxidation, synergizes with chemotherapy in resistant populations [102].
- GSH Synthesis Inhibitors: Buthionine sulfoximine (BSO) inhibits γ-glutamylcysteine synthetase, depleting cellular GSH and sensitizing to platinum-based therapies [102].
This approach capitalizes on the differential iron metabolism in cancer cells, which frequently exhibit iron overload, making them particularly susceptible to ferroptosis induction [106].
Pro-Oxidant Therapies to Overwarm Defenses
Pro-oxidant therapies aim to overwhelm cellular antioxidant defenses, creating lethal oxidative stress selectively in cancer cells [102].
Table 2: Pro-Oxidant Redox Modulators in Combination Therapy
| Pro-Oxidant Agent | Combination Partner | Mechanism | Tumor Selectivity Basis |
|---|---|---|---|
| High-Dose Vitamin C (Ascorbic acid) | Gemcitabine, Paclitaxel | Generates Hâ‚‚Oâ‚‚ via auto-oxidation | Cancer cells' decreased catalase activity |
| Arsenic Trioxide (ATO) | All-trans retinoic acid (APL) | Mitochondrial ROS generation, TrxR inhibition | Differential redox state in malignant vs. normal cells |
| Manganese Porphyrins | Radiotherapy | SOD mimetic, indirect Nrf2-mediated effects | Exploits altered redox signaling in cancer cells |
| Auranofin | Proteasome inhibitors | Thioredoxin reductase (TrxR) inhibition | Cancer cells' dependence on Trx system |
Extensive preclinical data and ongoing clinical trials support the concept that reliance on redox adaptation represents a cancer-selective vulnerability that can be leveraged through these combination approaches [102].
Experimental Protocols and Methodologies
Assessing Redox-Modulator Efficacy in 3D Culture Models
Objective: Evaluate the combined effects of redox modulators with conventional chemotherapies using physiologically relevant 3D cancer models.
Materials and Methods:
- Cell Culture: Establish liver cancer 3D spheroids using Huh7 or HepG2 cells in low-attachment plates with appropriate media [106].
- Treatment Protocol:
- Allow spheroid formation over 5-7 days until 200-300μm diameter
- Pre-treat with redox modulators (IITK4003, ECâ‚…â‚€ ~340 nM) for 24h [106]
- Add conventional chemotherapeutic (e.g., sorafenib, cisplatin) at clinically relevant concentrations
- Continue co-incubation for 72-96h
- Assessment Endpoints:
- Viability Metrics: ATP-based luminescence, resazurin reduction
- Redox Status: MitoSOX Red for mitochondrial superoxide, CellROX for general ROS
- Lipid Peroxidation: C11-BODIPYâµâ¸Â¹/âµâ¹Â¹ staining via flow cytometry
- GSH/GSSG Ratio: GSH-Glo Glutathione Assay
- Apoptosis Markers: Caspase-3/7 activity, Annexin V/propidium iodide staining [106]
Interpretation: Effective combinations demonstrate significant reduction in spheroid viability with enhanced oxidative stress markers compared to monotherapies, indicating synergistic activity [106].
Evaluating Therapy-Induced Senescence with Redox Modulation
Objective: Characterize the impact of redox modulation on senescence-associated secretory phenotype (SASP) and drug resistance.
Materials and Methods:
- Senescence Induction: Treat cancer cells (e.g., MCF-7, A549) with sublethal doses of doxorubicin (100-250 nM) or radiation (2-5 Gy) for 48h [104].
- Senescence Validation:
- SA-β-gal Staining: Detect activity at pH 6.0 using X-gal substrate [104]
- Lamin B1 Depletion: Western blot analysis of nuclear envelope protein
- DNA Damage Foci: Immunofluorescence for γH2AX (DNA double-strand breaks)
- Redox Modulation: Apply NRF2 inhibitors (ML385, 5-10μM) or pro-oxidants (ATO, 1-5μM) to senescent populations [104].
- SASP Analysis:
- Cytokine Profiling: ELISA for IL-6, IL-8, IL-1β in conditioned media
- Transcriptional Analysis: qRT-PCR for SASP factor genes
- Functional Assays: Co-culture with naïve cancer cells to assess paracrine pro-survival effects [104]
Interpretation: Successful redox intervention suppresses SASP factors and abolishes the protective paracrine effects on treatment-naïve cancer cells, indicating disruption of the senescence-mediated resistance pathway [104].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Redox Combination Studies
| Reagent/Category | Specific Examples | Primary Function | Application Notes |
|---|---|---|---|
| NRF2 Pathway Modulators | Brusatol, ML385, Omaveloxolone | Inhibit or activate NRF2-mediated transcription | ML385 shows greater specificity for NRF2-DNA binding disruption |
| GSH System Modulators | Erastin, BSO, Sulfasalazine | Deplete glutathione or inhibit synthesis | Erastin induces ferroptosis via system Xcâ» inhibition |
| Thioredoxin Inhibitors | Auranofin, PX-12 | Inhibit thioredoxin reductase | Auranofin shows irreversible TrxR inhibition |
| Pro-Oxidant Compounds | High-dose vitamin C, ATO, MitoTEMPO | Generate ROS in specific compartments | Consider compartment-specific activity (e.g., MitoTEMPO for mitochondria) |
| ROS Detection Probes | MitoSOX Red, CellROX, H2DCFDA | Detect specific ROS types and localization | MitoSOX specifically detects mitochondrial superoxide |
| Cell Death Assays | C11-BODIPYâµâ¸Â¹/âµâ¹Â¹, Annexin V, Caspase-3/7 | Distinguish apoptosis vs. ferroptosis | C11-BODIPY essential for detecting lipid peroxidation in ferroptosis |
| Senescence Assays | SA-β-gal staining, Lamin B1 IHC, SASP cytokine arrays | Identify and characterize senescent cells | SA-β-gal at pH 6.0 remains gold standard for detection |
Diagram 2: Strategic combination of redox modulators with therapy-induced senescence. Redox modulation inhibits SASP and potentiates apoptosis to overcome resistance.
The strategic integration of redox modulators with conventional cancer therapies represents a paradigm shift in oncology, moving beyond non-specific cytotoxic approaches to precision targeting of cancer-specific vulnerabilities. The accumulating preclinical evidence demonstrates that targeting the redox adaptation of cancer cells can effectively overcome resistance mechanisms, eliminate protective senescent populations, and induce synergistic cell death through multiple modalities including apoptosis and ferroptosis [102] [104] [106].
Future directions in this field will likely focus on biomarker-driven patient selection, as tumors with specific genetic alterations (KEAP1 mutations, NRF2 amplifications) or metabolic features (iron overload, elevated ROS) may demonstrate heightened sensitivity to specific redox modulation strategies [1]. Additionally, advances in drug delivery technologies, including polymeric nanoparticles, liposomes, and biomimetic nanoparticles, may overcome current limitations in the pharmacokinetics and tumor specificity of redox modulators, enhancing their therapeutic index and clinical potential [103].
As our understanding of redox biology deepens, the strategic combination of redox modulators with conventional treatments holds significant promise for transforming cancer therapy outcomes, particularly for resistant and aggressive malignancies where current options remain limited.
Validation of Redox Targets and Comparative Analysis Across Disease Models
Redox imbalance, characterized by the disruption of the physiological equilibrium between oxidative and reductive processes, is a hallmark of numerous non-communicable diseases (NCDs) [107]. This whitepaper examines the shared and unique mechanisms of redox dysregulation across three major disease categories: neurodegenerative, cardiovascular, and autoimmune disorders. The nuclear factor erythroid 2-like factor 2 (NRF2) pathway serves as a master regulator of cellular defense against oxidative damage, orchestrating the expression of hundreds of cytoprotective genes [107] [1]. Conversely, the pro-inflammatory nuclear factor-kappa B (NF-κB) pathway is often activated by oxidative stress, creating a complex interplay that influences disease pathogenesis [4]. Understanding these redox mechanisms provides crucial insights for diagnostic, prognostic, and therapeutic strategies in inflammatory diseases.
Core Redox Signaling Pathways in Disease
The NRF2-KEAP1 Antioxidant System
The NRF2-KEAP1 pathway represents the primary cellular defense mechanism against oxidative stress. Under basal conditions, NRF2 is bound to its negative regulator KEAP1, which targets it for ubiquitination and proteasomal degradation [4]. During oxidative stress, reactive oxygen species (ROS) modify critical cysteine residues on KEAP1, leading to NRF2 stabilization and nuclear translocation [4]. In the nucleus, NRF2 binds to antioxidant response elements (AREs), activating the transcription of cytoprotective genes including those involved in glutathione synthesis, quinone reduction, and thioredoxin regeneration [107].
NF-κB Inflammatory Signaling
Oxidative stress activates redox-sensitive transcription factors, with NF-κB representing the most well-characterized pathway [4]. ROS inhibit MAPK phosphatases by oxidizing their catalytic cysteine residues, prolonging MAPK signaling and promoting NF-κB activation [4]. Activated NF-κB translocates to the nucleus and drives the expression of pro-inflammatory cytokines, adhesion molecules, and enzymes such as cyclooxygenase-2 (COX-2) and inducible nitric oxide synthase (iNOS) [4]. This establishes a pathogenic loop wherein oxidative stress promotes inflammation, which in turn generates additional ROS.
Redox Cross-Regulation Between NRF2 and NF-κB
NRF2 and NF-κB pathways engage in complex cross-regulation. NRF2 activation not only mitigates oxidative damage but also exerts anti-inflammatory effects by suppressing NF-κB-driven transcription [4]. This interplay creates a dynamic balance where the relative activation of these pathways significantly influences disease progression and therapeutic outcomes across different pathological contexts.
Quantitative Biomarker Profiles Across Disease Categories
Analysis of NRF2-regulated biomarkers in accessible human samples, particularly peripheral blood mononuclear cells (PBMCs), reveals distinct redox profiles across neurodegenerative, cardiovascular, and autoimmune diseases.
Table 1: NRF2 Biomarker Expression Profiles Across Disease Categories
| Disease Category | GCLC/GCLM | HMOX1 | NQO1 | SRXN1 | TXNRD1 | Primary Redox State |
|---|---|---|---|---|---|---|
| Neurodegenerative | ↓ | ↑↑ | ↓ | ↑ | ↓ | Chronic Oxidative Stress |
| Cardiovascular | ↑ | ↑↑↑ | ↑ | ↑↑ | ↑ | Cyclical OS/RS Shifts |
| Autoimmune | ↓↓ | ↑ | ↓↓ | → | ↓↓ | Severe Oxidative Stress |
Table 2: Systemic Redox Indicators in Major Specific Diseases
| Specific Disease | NRF2 Pathway Activity | GSH/GSSG Ratio | NF-κB Activation | Clinical Correlation |
|---|---|---|---|---|
| Alzheimer's Disease | Impaired | Severely Decreased | ↑↑↑ | Correlates with cognitive decline |
| Atherosclerosis | Compensatory Increase | Moderately Decreased | ↑↑ | Associated with plaque vulnerability |
| Rheumatoid Arthritis | Severely Impaired | Severely Decreased | ↑↑↑ | Correlates with disease activity and joint damage |
| Parkinson's Disease | Impaired | Decreased | ↑↑ | Associated with dopaminergic neuron loss |
| Coronary Artery Disease | Adaptive Increase | Mildly Decreased | ↑↑ | Predicts cardiovascular events |
| Systemic Lupus Erythematosus | Impaired | Severely Decreased | ↑↑↑ | Correlates with multi-organ involvement |
Experimental Methodologies for Redox Pathology Assessment
Biomarker Quantification in Accessible Biosamples
PBMC Isolation and Gene Expression Analysis:
- Collect peripheral blood in EDTA-containing tubes and separate PBMCs via density gradient centrifugation within 2 hours of collection [107].
- Extract total RNA using column-based methods and quantify NRF2 target genes (GCLC, GCLM, HMOX1, NQO1, SRXN1, TXNRD1) via RT-qPCR with TBP or RPL41 as reference genes [107].
- Express results as normalized transcripts per million (nTPM) for cross-study comparisons [107].
Protein-Level Assessment:
- For protein quantification, prepare PBMC lysates using RIPA buffer containing protease and phosphatase inhibitors.
- Measure NRF2 target proteins via enzyme-linked immunosorbent assay (ELISA) with standardized kits, reporting concentrations as pg/mg total protein [107].
- For extracellular vesicles, precipitate from plasma using polymer-based methods and analyze cargo for tissue-derived redox indicators [107].
Functional Redox Status Assessment
Glutathione Homeostasis Assay:
- Deproteinize fresh PBMCs or plasma with acid precipitation followed by neutralization.
- Quantify reduced (GSH) and oxidized (GSSG) glutathione using fluorometric assays with ortho-phthalaldehyde.
- Calculate GSH/GSSG ratio as a primary indicator of cellular redox environment [4] [1].
Oxidative Stress Markers:
- Measure lipid peroxidation via malondialdehyde (MDA) quantification using thiobarbituric acid reactive substances (TBARS) assay.
- Detect protein carbonylation through derivatization with 2,4-dinitrophenylhydrazine (DNPH) and spectrophotometric analysis.
- Assess DNA oxidation by quantifying 8-hydroxy-2'-deoxyguanosine (8-OHdG) in urine or plasma using ELISA [1].
Signaling Pathway Visualization
Diagram 1: Core Redox Signaling in Disease
Comparative Mechanistic Analysis
Shared Pathogenic Mechanisms
Chronic Oxidative Stress: All three disease categories demonstrate persistent redox imbalance with elevated ROS from mitochondrial dysfunction, NADPH oxidase activation, and endoplasmic reticulum stress [4] [1]. This oxidative environment promotes damage to lipids, proteins, and DNA while activating inflammatory cascades through redox-sensitive transcription factors [1].
NRF2 Dysfunction: Despite varying expression patterns, all three disease categories exhibit altered NRF2 signaling. In neurodegenerative diseases, age-related decline in NRF2 responsiveness creates vulnerability to oxidative damage [107]. Autoimmune diseases show impaired NRF2 activation despite severe oxidative stress, while cardiovascular diseases demonstrate cyclical NRF2 activation attempting to compensate for hemodynamic stress [107].
Inflammasome Activation: ROS are essential for activation of the NLRP3 inflammasome, which processes pro-inflammatory cytokines IL-1β and IL-18, perpetuating inflammatory cascades across all three disease categories [4].
Unique Pathogenic Mechanisms
Neurodegenerative Diseases: Feature selective vulnerability of specific neuronal populations to redox imbalance, with protein misfolding and aggregation creating additional oxidative burden. Blood-brain barrier dysfunction limits peripheral antioxidant access to affected regions [107].
Cardiovascular Diseases: Demonstrate oscillatory redox states with hemodynamic fluctuations, where reductive stress during reperfusion phases can be equally damaging [4]. Vascular-specific oxidative enzymes (NOX isoforms) contribute to localized redox dysregulation [4].
Autoimmune Diseases: Exhibit severe glutathione depletion and impaired thioredoxin system function, creating a self-perpetuating cycle of oxidative damage and autoantigen modification [107] [36].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Redox Pathology Studies
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| NRF2 Activators | Sulforaphane, Broccoli Sprout Homogenate, tRES-HESP | Experimental NRF2 pathway induction to assess therapeutic potential |
| NRF2 Inhibitors | ML385, Brusatol | Mechanistic studies to determine NRF2-dependent effects |
| Oxidative Stress Inducers | Hâ‚‚Oâ‚‚, tert-Butyl hydroperoxide, Acrolein | In vitro modeling of oxidative stress conditions |
| Antioxidant Enzymes | Recombinant SOD, Catalase, Thioredoxin | Assessment of exogenous antioxidant protection |
| Detection Kits | GSH/GSSG Assay, Lipid Peroxidation Assay, Protein Carbonylation Kit | Quantitative measurement of oxidative damage markers |
| NRF2 Biomarker Antibodies | Anti-HMOX1, Anti-NQO1, Anti-TXNRD1 | Protein-level quantification of NRF2 target expression |
| Gene Expression Assays | RT-qPCR primers/probes for GCLC, GCLM, SRXN1 | Transcriptional profiling of NRF2 pathway activity |
Experimental Workflow for Comparative Redox Assessment
Diagram 2: Redox Pathology Workflow
Comparative redox pathology reveals both conserved and distinct mechanisms across neurodegenerative, cardiovascular, and autoimmune diseases. The NRF2 biomarker panel (GCLC, GCLM, HMOX1, NQO1, SRXN1, TXNRD1) provides a robust framework for assessing redox status in accessible biosamples, enabling clinical translation for diagnosis, prognosis, and therapeutic monitoring. Future research should focus on tissue-specific redox adaptations, the dynamic interplay between oxidative and reductive stress, and development of targeted therapies that restore physiological redox balance without disrupting essential redox signaling.
Redox imbalance plays a pivotal role in the regulation of inflammation, influencing both the onset and progression of various pathological conditions [4]. Within this framework, specific biomarkers of oxidative stress have emerged as critical tools for understanding disease mechanisms and assessing therapeutic interventions. 3-Nitrotyrosine, 8-iso-prostaglandin F2α (8-iso-PGF2α), and 4-hydroxy-2-nonenal (4-HNE) represent three clinically significant biomarkers that provide distinct yet complementary information about oxidative damage pathways. 3-Nitrotyrosine serves as a specific marker for protein nitration mediated by reactive nitrogen species, particularly peroxynitrite [108]. 8-iso-PGF2α, one of the most well-established biomarkers of oxidative stress, reflects free radical-mediated lipid peroxidation [109] [110]. Meanwhile, 4-HNE represents a reactive aldehyde produced during the peroxidation of ω-6 polyunsaturated fatty acids, which can form adducts with proteins and DNA, contributing to cellular dysfunction in chronic diseases [111]. The accurate measurement of these biomarkers requires sophisticated analytical approaches, and their levels correlate with disease severity across numerous pathological conditions, positioning them as valuable tools for both research and clinical applications in the context of inflammation and redox biology.
Biomarker Origins and Pathophysiological Significance
3-Nitrotyrosine is formed primarily through the reaction of tyrosine residues with reactive nitrogen species, particularly peroxynitrite (ONOOâ»), a powerful oxidant generated from the reaction of nitric oxide (NO•) with superoxide anion (O₂•â») [108]. This modification represents a specific protein footprint of nitrative stress and can profoundly alter protein function, affecting cellular signaling cascades [108]. Its detection has been instrumental in linking nitrative stress to various inflammatory conditions.
8-iso-PGF2α is generated via non-enzymatic, free radical-initiated peroxidation of arachidonic acid, making it a reliable marker of lipid peroxidation [109] [112]. Although it can also be produced through enzymatic pathways involving prostaglandin-endoperoxide synthases (PGHS), the chemical peroxidation pathway dominates in humans, accounting for >99% of its formation in human plasma [110]. This biomarker has been extensively validated in numerous clinical studies and is often regarded as a "gold standard" for assessing oxidative stress in vivo.
4-HNE is a lipid peroxidation product derived from the oxidation of ω-6 polyunsaturated fatty acids [111]. As a reactive carbonyl species (RCS), it exerts both signaling functions at low concentrations and cytotoxic effects at elevated levels. 4-HNE readily forms adducts with proteins, DNA, and phospholipids, amplifying oxidative damage and contributing to the pathogenesis of various diseases, including diabetic complications [111]. Its dual role as both a marker and mediator of oxidative stress makes it particularly significant in chronic inflammatory conditions.
Table 1: Biomarker Characteristics and Pathophysiological Significance
| Biomarker | Formation Pathway | Primary Matrix | Biological Significance | Key Pathological Associations |
|---|---|---|---|---|
| 3-Nitrotyrosine | Tyrosine nitration by reactive nitrogen species (e.g., peroxynitrite) | Tissue proteins, plasma, urine | Marker of nitrative stress; alters protein function and signaling | Cardiovascular disease, neurodegenerative disorders, inflammatory conditions |
| 8-iso-PGF2α | Free radical-mediated peroxidation of arachidonic acid | Urine, plasma, tissues | Gold standard biomarker of lipid peroxidation; correlates with oxidative stress severity | Smoking-related diseases, cardiovascular disorders, diabetes, asthma |
| 4-HNE | Peroxidation of ω-6 polyunsaturated fatty acids | Tissues, blood, cells, urine | Reactive carbonyl species; forms protein/DNA adducts; signaling molecule | Diabetic complications, cardiovascular diseases, neurodegenerative disorders |
Analytical Methodologies and Techniques
The accurate quantification of oxidative stress biomarkers requires highly specific and sensitive analytical methods due to their low concentrations in biological matrices and the presence of numerous structurally similar compounds.
3-Nitrotyrosine Analysis: Early methods for 3-nitrotyrosine detection relied on immunochemical techniques such as immunohistochemistry, ELISA, and Western blotting [108]. While these methods offer accessibility and are useful for spatial localization in tissues, they may lack the specificity and precision required for absolute quantification. High-performance liquid chromatography (HPLC) with various detection systems, including UV and electrochemical detection, provides improved specificity with limits of detection reaching approximately 20 fmol per injection [108]. However, the most definitive methods employ mass spectrometry. Gas chromatography-mass spectrometry (GC-MS) and liquid chromatography-tandem mass spectrometry (LC-MS/MS) offer superior sensitivity and specificity, enabling precise quantification even in complex biological samples like plasma and urine [113] [108]. These advanced techniques also facilitate the localization of nitrotyrosine residues within specific peptide sequences, providing insights into functional consequences.
8-iso-PGF2α Analysis: The analysis of 8-iso-PGF2α presents particular challenges due to the presence of numerous F2-isoprostane isomers with identical mass and similar fragmentation patterns [109]. Early GC-MS methods required extensive sample preparation, including two solid-phase extraction steps, TLC purification, and chemical derivatization [112]. Contemporary approaches favor LC-MS/MS with a single solid-phase extraction cleanup step, significantly improving throughput while maintaining accuracy [109] [112]. A critical analytical consideration is the chromatographic separation of 8-iso-PGF2α from its isomers, particularly in urine samples where multiple isomers coexist [109]. Methods utilizing isocratic or rapid gradient elution (e.g., 9-minute run times) with tandem mass spectrometry detection have been successfully developed, monitoring the transition m/z 353→193 for 8-iso-PGF2α and m/z 357→197 for the deuterated internal standard (8-iso-PGF2α-d4) [109] [112]. While enzyme immunoassays (EIA) offer high throughput, they may overestimate concentrations due to cross-reactivity with other isoprostane isomers, highlighting the importance of mass spectrometry-based methods for accurate quantification [109] [112].
4-HNE Analysis: The analysis of 4-HNE is complicated by its reactivity, volatility, polarity, and instability in biological systems [111]. Methods detect either the free aldehyde or its adducts with macromolecules. Free 4-HNE can be measured directly in tissues, plasma, or urine using techniques such as LC-MS/MS or GC-MS, often requiring derivatization to enhance stability and detectability [111]. Alternatively, 4-HNE-protein adducts are frequently detected immunohistochemically or using ELISA, providing information about tissue-specific damage [111]. However, these adduct measurements can underestimate true formation due to proteolytic degradation. Novel approaches including electrochemical sensors and nanotechnology-based platforms are emerging for real-time monitoring of 4-HNE levels in biological systems [111].
Table 2: Comparison of Key Analytical Techniques for Biomarker Quantification
| Biomarker | Primary Analytical Methods | Key Analytical Considerations | Sensitivity/LOD | Sample Preparation Requirements |
|---|---|---|---|---|
| 3-Nitrotyrosine | Immunoassays, HPLC-UV/ECD, GC-MS, LC-MS/MS | Specificity for protein-bound vs. free form; sample hydrolysis for total measurement | 20 fmol (HPLC-ECD) [108] | Protein precipitation, hydrolysis, solid-phase extraction |
| 8-iso-PGF2α | GC-MS, LC-MS/MS, ELISA | Chromatographic separation from isomers (e.g., 15(R)-PGF2α, 11β-PGF2α) essential for specificity | 53 pg/mL (LC-MS/MS) [109] | Solid-phase extraction (single step for LC-MS/MS) |
| 4-HNE | LC-MS/MS, GC-MS, ELISA, Immunohistochemistry | Distinction between free and protein-adducted forms; chemical instability during processing | Varies by method; adduct detection less quantitative | Derivatization for MS methods; protein extraction for adduct detection |
Experimental Protocols and Workflows
Protocol for Urinary 8-iso-PGF2α Quantification by LC-MS/MS
The following protocol, adapted from validated methods, details the quantification of urinary 8-iso-PGF2α using liquid chromatography-tandem mass spectrometry [109] [112].
Sample Preparation:
- Thaw frozen urine samples and centrifuge at 3,500 × g for 3 minutes to remove particulates.
- Aliquot 2.5 mL of clear urine into a clean tube and add 2 mL of 50 mM Tris-HCl buffer (pH 6.00 ± 0.05).
- Add 10 ng of surrogate standard (8-iso-PGF2α-d4) and 750 μL of methanol to precipitate proteins.
- Condition Strata-X AW SPE cartridges (60 mg/3 mL) sequentially with 2 mL methanol containing 2% formic acid followed by 2 mL water.
- Load the prepared urine sample onto the conditioned SPE cartridge.
- Wash sequentially with 2 mL water, 4 mL of 25% methanol in water, and 2 mL 100% acetonitrile.
- Dry the cartridge under vacuum for 15-30 seconds between wash steps.
- Elute analytes with 3 × 1 mL methanol, combining eluents into a single tube.
- Evaporate the combined eluents to dryness under a gentle stream of nitrogen.
- Reconstitute the dry residue in 50 μL of mobile phase (2 mM aqueous ammonium acetate/acetonitrile/methanol, 81:18:1, v/v/v) and centrifuge prior to LC-MS/MS analysis.
LC-MS/MS Analysis:
- Chromatography: Use a reversed-phase C18 column (e.g., Shim-Pack XR-ODS, 2×50 mm, 2.2 μm) maintained at 45°C. Apply isocratic elution with mobile phase (2 mM aqueous ammonium acetate/acetonitrile/methanol, 81:18:1, v/v/v) at a flow rate of 0.45 mL/min. Total run time is approximately 9 minutes.
- Mass Spectrometry: Operate the mass spectrometer in negative ion electrospray ionization mode. Monitor the transitions m/z 353 → 193 for 8-iso-PGF2α and m/z 357 → 197 for the internal standard (8-iso-PGF2α-d4). Optimize source parameters as follows: source temperature 500°C; spray voltage -4200 V; declustering potential -90 V; collision energy -36 eV.
Validation Parameters:
- Assay validation should establish linearity, accuracy, precision, recovery, and stability. The limit of quantification (LOQ) for this method is typically 178 pg/mL, with a limit of detection (LOD) of 53 pg/mL [109]. Normalize urinary concentrations to creatinine to account for dilution variations.
General Workflow for Biomarker Analysis in Biological Samples
The following diagram illustrates the generalized experimental workflow for biomarker analysis, from sample collection to data interpretation:
Diagram 1: Generalized Experimental Workflow for Oxidative Stress Biomarker Analysis
Redox Signaling Pathways and Biomarker Interrelationships
Biomarkers in the Context of Redox Signaling and Inflammation
Oxidative stress represents an imbalance between the production of reactive oxygen/nitrogen species (ROS/RNS) and antioxidant defenses, leading to molecular damage and dysregulated redox signaling [4]. This imbalance activates key inflammatory pathways, establishing a pathogenic loop that sustains chronic inflammation in conditions such as atherosclerosis, neurodegeneration, and metabolic diseases [4] [3].
Reactive oxygen species, including superoxide anion (O₂•â»), hydrogen peroxide (Hâ‚‚Oâ‚‚), and hydroxyl radicals (•OH), are generated through multiple cellular sources. Mitochondrial electron transport chain complexes I and III represent primary endogenous sources, while NADPH oxidases (NOX), uncoupled nitric oxide synthase (NOS), and xanthine oxidase contribute significantly to cellular ROS production [4] [3]. Simultaneously, reactive nitrogen species such as nitric oxide (NO•) and peroxynitrite (ONOOâ») are formed through enzymatic and chemical pathways. Peroxynitrite, in particular, is a potent nitrating agent that modifies tyrosine residues to form 3-nitrotyrosine [108].
These reactive species function as important signaling molecules that activate redox-sensitive transcription factors including nuclear factor-kappa B (NF-κB), which coordinates the expression of pro-inflammatory cytokines, adhesion molecules, and enzymes such as cyclooxygenase-2 (COX-2) and inducible nitric oxide synthase (iNOS) [4]. This inflammatory response further amplifies ROS/RNS production, creating a vicious cycle of oxidative damage and inflammation.
Lipid peroxidation represents a major consequence of oxidative stress, particularly targeting polyunsaturated fatty acids in cellular membranes. The non-enzymatic peroxidation of arachidonic acid generates F2-isoprostanes including 8-iso-PGF2α, while peroxidation of ω-6 polyunsaturated fatty acids produces reactive aldehydes such as 4-HNE [111] [110]. These biomarkers not only serve as indicators of oxidative damage but also actively contribute to pathology by modifying cellular proteins, DNA, and signaling molecules.
The following diagram illustrates the interconnected pathways linking reactive species formation, biomarker generation, and inflammatory signaling:
Diagram 2: Redox Signaling Pathways Connecting Oxidative Stress, Biomarker Formation, and Inflammation
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful analysis of oxidative stress biomarkers requires specific reagents, standards, and materials. The following table details essential components for a comprehensive research toolkit:
Table 3: Essential Research Reagents and Materials for Biomarker Analysis
| Reagent/Material | Function/Purpose | Application Examples | Key Considerations |
|---|---|---|---|
| Analytical Standards | Quantification, method calibration, quality control | 8-iso-PGF2α, 3-nitrotyrosine, 4-HNE, and their deuterated internal standards | Purity verification; stable isotope-labeled internal standards essential for MS quantification |
| Solid-Phase Extraction (SPE) Cartridges | Sample cleanup, analyte concentration, matrix component removal | Strata-X AW, C18, mixed-mode cartridges | Select appropriate chemistry based on analyte properties; optimize conditioning and elution solvents |
| Chromatography Columns | Analytical separation of biomarkers from interfering compounds | Reversed-phase C18 columns (e.g., 2.1 × 50 mm, 1.8-2.2 μm) | Column chemistry and particle size affect resolution of isomers (critical for 8-iso-PGF2α) |
| Mass Spectrometry Solvents | Mobile phase preparation, sample reconstitution | LC-MS grade water, acetonitrile, methanol, ammonium acetate | High-purity solvents essential to minimize background noise and ion suppression |
| Antibodies (for immunoassays) | Detection and quantification via antigen-antibody interaction | Polyclonal/monoclonal antibodies for 3-NT, 4-HNE-adducts, 8-iso-PGF2α | Validate specificity; check cross-reactivity with similar structures (e.g., isoprostane isomers) |
| Protein Hydrolysis Reagents | Release of protein-bound biomarkers for total quantification | Acid hydrolysis (e.g., 6M HCl) for 3-nitrotyrosine | Optimize time/temperature to avoid analyte degradation; use antioxidant protection when needed |
| Derivatization Reagents | Enhance volatility and detectability for GC-MS analysis | Pentafluorobenzyl bromide, BSTFA + 1% TMCS for F2-isoprostanes | Complete derivatization essential for sensitivity; moisture control critical |
Clinical Correlations and Research Applications
Biomarker Levels in Health and Disease
Quantification of 3-nitrotyrosine, 8-iso-PGF2α, and 4-HNE across various pathological conditions has revealed consistent elevations associated with disease severity, progression, and therapeutic outcomes.
8-iso-PGF2α Clinical Correlations: Urinary 8-iso-PGF2α concentrations in healthy individuals typically range from 180 to 500 pg/mg creatinine, with established reference intervals for both adult and pediatric populations (<0.5 ng/mg creatinine in children) [112]. Significantly elevated levels have been documented in numerous conditions, including heavy smoking (approximately 2-3 fold increases), cardiovascular diseases, type 2 diabetes, Alzheimer's disease, and asthma [109] [112]. Interventions such as antioxidant supplementation, smoking cessation, and anti-inflammatory treatments have demonstrated measurable reductions in 8-iso-PGF2α levels, supporting its utility as a pharmacodynamic biomarker [112]. The interpretation of 8-iso-PGF2α levels requires consideration of potential enzymatic contributions, particularly in inflammatory conditions where prostaglandin-endoperoxide synthases (PGHS) are induced. The ratio of 8-iso-PGF2α to prostaglandin F2α (PGF2α) can distinguish enzymatic from chemical lipid peroxidation, providing more specific information about oxidative stress mechanisms [110].
3-Nitrotyrosine Clinical Correlations: Elevated 3-nitrotyrosine levels have been documented in atherosclerosis, neurodegenerative diseases (Alzheimer's and Parkinson's), acute lung injury, and septic shock [108]. In cardiovascular disease, 3-nitrotyrosine accumulation in vessel walls correlates with endothelial dysfunction and disease progression. In neurodegenerative conditions, increased nitrotyrosine immunoreactivity in affected brain regions suggests a role for nitrative stress in disease pathogenesis. The detection of 3-nitrotyrosine in biological fluids like plasma and urine provides a systemic measure of nitrative stress, while tissue immunohistochemistry offers spatial information about protein nitration patterns.
4-HNE Clinical Correlations: 4-HNE and its protein adducts are significantly elevated in diabetes and its complications, with studies reporting approximately 2.5-fold increases in testicular tissue of type 1 diabetic mice and elevated plasma levels (6.7-7.5 ng/mg protein) in diabetic rats compared to controls [111]. In human studies, 4-HNE adducts accumulate in diabetic tissues including retina, kidney, and heart, correlating with the severity of diabetic complications such as retinopathy, nephropathy, and cardiomyopathy [111]. Beyond diabetes, 4-HNE elevations have been documented in cardiovascular diseases, neurodegenerative disorders, non-alcoholic fatty liver disease, and various cancer types, reflecting its broad involvement in oxidative stress-related pathologies.
Applications in Drug Development and Therapeutic Monitoring
These biomarkers play increasingly important roles in pharmaceutical research and development, particularly for compounds targeting oxidative stress pathways.
Target Engagement and Mechanism Validation: For antioxidants and redox-modulating therapies, reduction in 8-iso-PGF2α, 3-nitrotyrosine, or 4-HNE levels provides direct evidence of target engagement and biological activity [112]. This application is particularly valuable during early-phase clinical trials to establish proof-of-concept and determine optimal dosing regimens.
Stratification of Patient Populations: Baseline biomarker levels may help identify patient subgroups most likely to benefit from antioxidant or anti-inflammatory therapies. For instance, patients with elevated 8-iso-PGF2α or 4-HNE levels might represent target populations for interventions targeting specific oxidative pathways.
Safety Assessment: Monitoring these biomarkers can reveal off-target oxidative effects of pharmaceutical compounds, providing early indicators of potential toxicity mechanisms related to oxidative stress.
COVID-19 Applications: Recent research has demonstrated the prognostic value of oxidative stress biomarkers in COVID-19, with elevations in 8-iso-PGF2α, 3-nitrotyrosine (measured as nitrotyrosine), and 4-HNE associated with disease severity, intensive care admission, and mortality [114]. These biomarkers have helped elucidate the role of oxidative stress in the hyperinflammatory response and tissue damage characteristic of severe SARS-CoV-2 infection.
The validation and precise quantification of 3-nitrotyrosine, 8-iso-PGF2α, and 4-HNE provide powerful approaches for investigating redox signaling in inflammatory diseases and beyond. Liquid chromatography-tandem mass spectrometry has emerged as the methodology of choice for accurate quantification of these biomarkers, offering the specificity, sensitivity, and throughput required for both research and clinical applications. The integration of these biomarker measurements with understanding of their roles in redox biology creates a robust framework for elucidating disease mechanisms, evaluating therapeutic interventions, and advancing personalized medicine approaches for oxidative stress-related disorders. As analytical technologies continue to evolve and our understanding of redox biology deepens, these biomarkers will undoubtedly remain essential tools for unraveling the complex relationships between oxidative stress, inflammation, and human disease.
The cellular redox state, governed by the delicate balance between reactive oxygen species (ROS) production and elimination, is a fundamental regulator of signaling pathways influencing inflammation, cell survival, and metabolism. Under physiological conditions, ROS generated by mitochondrial oxidative respiration, endoplasmic reticulum, and NADPH oxidases (NOX) are effectively neutralized by NRF2-mediated antioxidant responses, maintaining cellular redox homeostasis [1]. Disruption of this finely tuned equilibrium is a common hallmark across numerous chronic diseases, including neurodegenerative, cardiovascular, metabolic, and autoimmune disorders [115] [116] [117]. This imbalance creates a pathogenic feedback loop wherein oxidative stress promotes chronic inflammation, and inflammatory mediators further stimulate ROS production [118].
Two central players in redox regulation have emerged as promising therapeutic targets: Nuclear factor erythroid 2-related factor 2 (NRF2), the master regulator of antioxidant responses, and NADPH oxidases (NOX), dedicated enzymatic complexes responsible for controlled ROS generation. The transcription factor NRF2 coordinates the expression of approximately 250 genes containing antioxidant response elements (ARE) in their promoters, including those encoding superoxide dismutase (SOD), catalase, glutathione peroxidase (GPx), and heme oxygenase-1 (HO-1) [115] [116]. Conversely, the NOX family of enzymes, comprising NOX1-5 and DUOX1-2, are transmembrane proteins that catalyze the production of superoxide or hydrogen peroxide, serving as key signaling molecules and microbicidal agents [54].
The interplay between these systems creates a complex redox signaling network. Evidence indicates that NOX-derived ROS can activate NRF2, which in turn transcriptionally represses NOX components, forming a critical negative feedback loop [119]. In pathological states, this reciprocal regulation is disrupted, leading to sustained oxidative stress and chronic inflammation. This whitepaper provides a comprehensive cross-disease analysis of pharmacological strategies targeting NRF2 activation and NOX inhibition in preclinical models, evaluating their therapeutic potential, mechanistic insights, and translational challenges.
Molecular Mechanisms of NRF2 and NOX Signaling
NRF2 Regulation and Activation Pathways
NRF2 is a cap'n'collar (CNC) basic-region leucine zipper (bZIP) transcription factor comprising seven highly conserved NRF2-ECH homology (Neh) domains [117]. The Neh2 domain mediates interaction with its primary negative regulator, Kelch-like ECH-associated protein 1 (KEAP1), while Neh1 facilitates heterodimerization with small Maf proteins (sMaf). Under homeostatic conditions, NRF2 is continuously ubiquitinated by the KEAP1-CUL3-RBX1 E3 ligase complex and targeted for proteasomal degradation, maintaining low basal levels [115] [118].
The "hinge-and-latch" model elucidates the activation mechanism wherein KEAP1 homodimer binds NRF2 via high-affinity ETGE (hinge) and low-affinity DLG (latch) motifs [117]. Cellular stressors modify specific cysteine residues in KEAP1 (notably C151, C273, and C288), inducing conformational changes that disrupt DLG binding, impair NRF2 ubiquitination, and stabilize the protein [115]. Stabilized NRF2 translocates to the nucleus, forms heterodimers with sMaf proteins, and binds to ARE/EpRE sequences, initiating transcription of cytoprotective genes encompassing antioxidant enzymes, detoxification proteins, and metabolic regulators [120].
Alternative regulatory mechanisms include glycogen synthase kinase-3β (GSK-3β)-mediated phosphorylation of the Neh6 domain, promoting β-TrCP-dependent degradation, and epigenetic regulation by microRNAs (e.g., miR-200a, miR-141) that target KEAP1 mRNA [117] [120]. Oncogenic signaling through KRAS, BRAF, and MYC can also transcriptionally upregulate NRF2, particularly in cancer contexts [120].
NOX Family Structure and Function
The NOX family represents the only known enzyme family dedicated solely to ROS generation, functioning as transmembrane electron transporters that reduce oxygen to superoxide or hydrogen peroxide using NADPH as an electron donor [54]. All NOX isoforms share conserved structural features: six transmembrane domains, NADPH and FAD binding sites at the C-terminus, and four heme-binding histidines. NOX1-3 require the membrane-bound subunit p22phox for stabilization and activity, while NOX4 generates hydrogen peroxide constitutively when associated with p22phox [54]. NOX5 and DUOX enzymes contain N-terminal calcium-binding EF-hand domains, rendering them calcium-sensitive [54].
Table 1: NOX Family Isoforms: Expression Patterns and Regulatory Mechanisms
| Isoform | Primary Tissue Distribution | ROS Produced | Key Regulatory Subunits | Activation Mechanisms |
|---|---|---|---|---|
| NOX1 | Colon, vascular smooth muscle, endothelium | Superoxide (O₂•â») | p22phox, NOXO1, NOXA1, Rac | Constitutively active with NOXO1/NOXA1; cytokine-inducible |
| NOX2 | Phagocytes, microglia, endothelium | Superoxide (O₂•â») | p22phox, p47phox, p67phox, p40phox, Rac | Activated by phagocytosis, cytokines, DAMPs/PAMPs |
| NOX3 | Inner ear, vestibular system | Superoxide (O₂•â») | p22phox | Constitutively active; regulated by NOXO1 |
| NOX4 | Kidney, vasculature, osteoclasts | Hydrogen Peroxide (Hâ‚‚Oâ‚‚) | p22phox, Poldip2 | Constitutively active; hypoxia-inducible |
| NOX5 | Testis, spleen, lymphocytes | Superoxide (O₂•â») | Ca²âº/Calmodulin (EF-hands) | Calcium-dependent activation |
| DUOX1/2 | Thyroid, respiratory, gastrointestinal epithelia | Hydrogen Peroxide (Hâ‚‚Oâ‚‚) | DUOXA1/DUOXA2 | Calcium-dependent; regulated by maturation factors |
NOX-derived ROS function as signaling molecules through several mechanisms: reversible oxidation of cysteine thiols in protein phosphatases and kinases; activation of redox-sensitive transcription factors (NF-κB, AP-1); and modulation of calcium signaling channels [54]. In pathological contexts, excessive NOX activation contributes to oxidative damage, chronic inflammation, and disease progression across multiple organ systems.
Figure 1: NRF2 Activation Pathway and Antioxidant Response. Under basal conditions, NRF2 is ubiquitinated by the KEAP1-CUL3 complex and degraded. Oxidative stress modifies KEAP1 cysteines, stabilizing NRF2, which translocates to the nucleus, forms heterodimers with sMaf proteins, and activates antioxidant gene expression, restoring redox homeostasis.
Preclinical Efficacy of NRF2 Activators
Classification and Mechanisms of NRF2 Activators
NRF2 activators are categorized based on their mechanisms of action: electrophilic inducers that modify KEAP1 cysteine residues, protein-protein interaction (PPI) inhibitors that disrupt KEAP1-NRF2 binding, and multi-target drugs that activate NRF2 alongside other pathways [115]. Electrophilic compounds represent the most extensively studied class, with several advancing to clinical trials.
Table 2: Selected NRF2 Activators in Preclinical and Clinical Development
| Compound | Class | Mechanism of Action | Preclinical Disease Models | Key Efficacy Findings |
|---|---|---|---|---|
| Bardoxolone-methyl (CDDO-Me) | Synthetic triterpenoid | Electrophilic modification of KEAP1-Cys151 | Diabetic nephropathy, CKD, pulmonary hypertension, cancer | Improved renal function, reduced inflammation, attenuated vascular remodeling [115] |
| Dimethyl Fumarate (DMF) | Fumaric acid ester | Electrophilic modification of KEAP1-Cys151 | Multiple sclerosis, psoriasis, glioblastoma, osteoarthritis | Enhanced antioxidant capacity, reduced neuroinflammation, chondroprotection [115] [119] |
| RTA-408 (Omaveloxolone) | Synthetic triterpenoid | Electrophilic modification of KEAP1-Cys151 | Friedreich's ataxia, mitochondrial myopathy, melanoma | Improved mitochondrial function, reduced oxidative damage [115] |
| Sulforaphane | Isothiocyanate (natural) | Electrophilic modification of KEAP1 cysteine residues | Neurodegeneration, cancer, metabolic syndrome | Induced phase II enzymes, reduced inflammation, ameliorated insulin resistance [117] [74] |
Cross-Disease Efficacy Analysis
Neurodegenerative Diseases: In Alzheimer's disease models, dimethyl fumarate reduced neuroinflammation and oxidative stress markers, including lipid peroxidation products (4-HNE, F2-isoprostanes) and DNA damage marker 8-OHdG [74]. Sulforaphane demonstrated efficacy in Parkinson's models by upregulating glutathione synthesis and protecting dopaminergic neurons against oxidative damage [74]. In amyotrophic lateral sclerosis (ALS), NRF2 activation mitigated mitochondrial dysfunction and reduced protein misfolding through enhanced proteasomal clearance [74].
Metabolic and Cardiovascular Diseases: Bardoxolone-methyl improved renal function and attenuated histopathological damage in diabetic nephropathy models through NRF2-mediated suppression of pro-inflammatory cytokines and fibrotic markers [115] [83]. In pulmonary hypertension, it reversed vascular remodeling by restoring redox balance and decreasing pulmonary arterial smooth muscle proliferation [115]. NRF2 activation also ameliorated endothelial dysfunction in atherosclerosis models by reducing NOX activity and improving nitric oxide bioavailability [83].
Inflammatory and Autoimmune Diseases: In multiple sclerosis models (experimental autoimmune encephalomyelitis), dimethyl fumarate suppressed CNS inflammation, reduced demyelination, and decreased lymphocyte infiltration through NRF2-dependent mechanisms [115]. In inflammatory bowel disease models, NRF2 activators ameliorated colitis by enhancing HO-1 expression and reducing epithelial barrier dysfunction [117]. In osteoarthritis, NRF2 activation with DMF counteracted NOX1-mediated oxidative stress, prevented chondrocyte ferroptosis, and reduced extracellular matrix degradation [119].
Cancer Chemoprevention: NRF2 activators have demonstrated chemopreventive efficacy in carcinogen-induced models of colon, breast, and lung cancer through enhanced detoxification of electrophilic carcinogens and reduced DNA damage [120]. However, the dual role of NRF2 in cancer necessitates caution, as constitutive activation in established tumors promotes progression and therapy resistance [115] [120].
Preclinical Efficacy of NOX Inhibitors
NOX Isoform-Selective Inhibitors
The development of isoform-selective NOX inhibitors has advanced significantly, enabling more precise targeting of disease-relevant NOX isoforms while minimizing off-target effects.
Table 3: NOX Inhibitors in Preclinical Development
| Compound | Target Specificity | Mechanism of Action | Preclinical Disease Models | Key Efficacy Findings |
|---|---|---|---|---|
| GKT136901 | NOX1/4 preferential | Inhibits enzyme activity | Diabetic nephropathy, pulmonary fibrosis, stroke | Reduced fibrosis, improved renal function, attenuated blood-brain barrier disruption [54] |
| GKT831 (Setanaxib) | NOX4/1 preferential | Inhibits enzyme activity | Liver fibrosis, primary biliary cholangitis | Reduced inflammation and fibrosis, improved portal hypertension [54] |
| ML171 | NOX1-selective | Inhibits enzyme activity | Colitis, vascular inflammation | Ameliorated intestinal inflammation, improved endothelial function [54] |
| NOX2ds-tat | NOX2-selective | Peptide inhibitor targeting p47phox binding | Neuroinflammation, ischemia-reperfusion | Reduced microglial activation, attenuated neuronal death, improved outcomes post-ischemia [54] [74] |
Cross-Disease Efficacy Analysis
Cardiovascular and Metabolic Diseases: NOX1/4 inhibition with GKT136901 in diabetic mouse models attenuated endothelial dysfunction, reduced vascular superoxide production, and improved nitric oxide signaling [83] [54]. In hypertension models, NOX1 inhibition normalized blood pressure and reversed vascular remodeling through reduced ROS-mediated hypertrophy and collagen deposition [83]. NOX2 inhibition improved insulin signaling and glucose uptake in models of metabolic syndrome by reducing oxidative stress in skeletal muscle and adipose tissue [54].
Neurological Disorders: NOX2 inhibition with NOX2ds-tat peptide in Alzheimer's models reduced microglial activation and amyloid-β-induced neuroinflammation, preserving cognitive function [74]. In stroke models, NOX4 inhibition attenuated blood-brain barrier disruption and reduced infarct volume by suppressing matrix metalloproteinase activity [54] [74]. NOX inhibition also demonstrated efficacy in Parkinson's models by protecting dopaminergic neurons against oxidative damage [74].
Fibrotic Diseases: NOX4 inhibition attenuated transforming growth factor-β (TGF-β)-induced fibroblast activation and extracellular matrix deposition in models of pulmonary and renal fibrosis [54]. In liver fibrosis models, dual NOX1/4 inhibitors reduced collagen accumulation and improved liver function by suppressing hepatic stellate cell activation [54].
Inflammatory Diseases: NOX1 inhibition ameliorated intestinal inflammation in colitis models by preserving epithelial barrier function and reducing pro-inflammatory cytokine production [54]. In osteoarthritis, NOX1 knockdown experiments demonstrated reduced chondrocyte ferroptosis, decreased matrix metalloproteinase expression, and improved cartilage integrity [119].
Figure 2: NOX Activation Pathway and Inhibitor Mechanisms. Various stimuli trigger NOX complex assembly and activation, leading to ROS production with distinct pathological consequences. NOX inhibitors target specific complex components to disrupt ROS generation and downstream disease processes.
Experimental Methodologies for Preclinical Evaluation
In Vitro Assessment Protocols
NRF2 Activation and Antioxidant Response Evaluation:
- ARE-Luciferase Reporter Assay: Cells transfected with ARE-driven luciferase construct treated with test compounds for 6-24h. Luciferase activity measured using commercial kits and normalized to protein content or constitutive reporters [117].
- Western Blot Analysis of NRF2 and Target Proteins: Nuclear/cytoplasmic fractionation or whole cell lysates collected after 2-8h compound treatment. Antibodies against NRF2, KEAP1, HO-1, NQO1, GST, and γ-GCLC. GAPDH/Lamin B as loading controls [119] [120].
- Immunofluorescence for NRF2 Localization: Cells fixed, permeabilized, stained with anti-NRF2 antibody and fluorescent secondary antibodies. Nuclear translocation quantified by fluorescence intensity ratio (nuclear/cytoplasmic) [118].
- GSH/GSSG Ratio Measurement: Cell pellets extracted with metaphosphoric acid, derivatized with fluorescent probes, and measured via HPLC or commercial kits. Critical indicator of cellular redox status [119].
- Gene Expression Analysis of NRF2 Targets: RNA extracted after 4-12h treatment, qRT-PCR performed for HO-1, NQO1, GCLM, GCLC, TXNRD1 using appropriate reference genes [117].
NOX Activity and Inhibition Assessment:
- Dihydroethidium (DHE) Staining for Superoxide Detection: Cells loaded with 5μM DHE for 30min, fluorescence measured by flow cytometry or fluorescence microscopy. Specificity confirmed with PEG-SOD [54] [119].
- Amplex Red Assay for H₂O₂ Production: Cells incubated with 50μM Amplex Red and 0.1U/mL HRP, H₂O₂ release quantified fluorometrically (excitation/emission: 571/585nm) [54].
- NOX2 Immunoprecipitation and Activity Assay: Membrane fractions immunoprecipitated with anti-NOX2/p22phox antibodies, activity measured by NADPH-dependent superoxide production using cytochrome c reduction or lucigenin chemiluminescence [54].
- siRNA Knockdown Validation: NOX isoform-specific siRNA transfection (48-72h) followed by Western blot confirmation and functional assays to establish isoform-specific effects [119].
In Vivo Disease Models and Evaluation
Metabolic Disease Models:
- Diabetic Nephropathy: db/db mice or streptozotocin-induced diabetic rats treated with compounds for 8-16 weeks. Endpoints: urinary albumin/creatinine ratio, glomerular filtration rate, kidney histology (periodic acid-Schiff staining), fibrosis markers (α-SMA, collagen IV), NRF2 target gene expression in renal cortex [115] [83].
- Hypertension: Angiotensin II-infused or spontaneously hypertensive rats treated 4-8 weeks. Endpoints: blood pressure monitoring (telemetry), vascular reactivity (wire myography), vascular superoxide production (DHE staining), endothelial-dependent vasodilation [83].
Neurodegenerative Disease Models:
- Alzheimer's Models: APP/PS1 transgenic mice treated 3-6 months. Endpoints: Morris water maze, novel object recognition, amyloid-β plaque burden (thioflavin-S), neuroinflammation (Iba1, GFAP immunohistochemistry), lipid peroxidation (4-HNE, MDA), NRF2 activation in brain homogenates [74].
- Parkinson's Models: MPTP or 6-OHDA lesioned mice treated 2-4 weeks. Endpoints: rotarod performance, striatal dopamine levels, tyrosine hydroxylase-positive neurons in substantia nigra, microglial activation, oxidative stress markers [74].
- Osteoarthritis Model: Monosodium iodoacetate (MIA)-induced rat OA model with intra-articular injection. Endpoints: weight-bearing asymmetry, cartilage degradation (OARSI scoring), chondrocyte ferroptosis markers (GPX4, SLC7A11, ACSL4), inflammatory cytokines (IL-1β, TNF-α) in synovial fluid [119].
Inflammatory Disease Models:
- Multiple Sclerosis: Experimental autoimmune encephalomyelitis (EAE) mice treated from immunization through peak disease. Endpoints: clinical scoring, CNS inflammatory infiltration (H&E), demyelination (Luxol fast blue), NRF2 target expression in spinal cord [115].
- Colitis: Dextran sodium sulfate (DSS)-induced colitis mice treated throughout induction. Endpoints: disease activity index, colon length, histopathological scoring, myeloperoxidase activity, inflammatory cytokines [117].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Research Reagents for NRF2 and NOX Research
| Category | Reagent | Specific Example | Application/Function |
|---|---|---|---|
| Cell Lines | Primary chondrocytes | Rat articular chondrocytes | OA pathogenesis, NOX1-mediated ferroptosis studies [119] |
| Brain cell cultures | Primary microglia, astrocytes | Neuroinflammation, NOX2/NRF2 crosstalk [74] | |
| Immortalized lines | HEK293, HepG2, Caco-2 | NRF2 reporter assays, barrier function studies | |
| Animal Models | Neurodegeneration | APP/PS1 mice, MPTP mice | Alzheimer's, Parkinson's therapeutic evaluation [74] |
| Metabolic disease | db/db mice, AngII-infused rats | Diabetic complications, hypertension studies [115] [83] | |
| Inflammation | EAE mice, DSS colitis models | Multiple sclerosis, IBD mechanisms [115] [117] | |
| Antibodies | NRF2 Pathway | Anti-NRF2, KEAP1, HO-1, NQO1 | Western blot, IHC, immunofluorescence [119] |
| NOX Isoforms | Anti-NOX1, NOX2, NOX4, p22phox | Protein expression, localization studies [54] [119] | |
| Oxidative Damage | Anti-4-HNE, 8-OHdG, nitrotyrosine | Oxidative stress biomarker detection [74] | |
| Assay Kits | ROS Detection | DHE, MitoSOX, Amplex Red | Cellular superoxide, mitochondrial ROS, Hâ‚‚O2 measurement [54] [119] |
| Antioxidant Status | GSH/GSSG ratio, SOD activity | Redox balance assessment, antioxidant capacity [119] | |
| Lipid Peroxidation | MDA, F2-isoprostanes kits | Oxidative lipid damage quantification [74] | |
| Inhibitors/Activators | NRF2 Activators | DMF, sulforaphane, CDDO-Me | Pharmacological NRF2 pathway activation [115] [119] |
| NOX Inhibitors | GKT136901, ML171, NOX2ds-tat | Isoform-specific NOX inhibition studies [54] | |
| Ferroptosis Modulators | Erastin, Ferrostatin-1 | Ferroptosis induction/inhibition in OA models [119] |
The comprehensive analysis of NRF2 activators and NOX inhibitors across diverse preclinical models demonstrates their considerable therapeutic potential for diseases unified by oxidative stress and inflammation pathologies. The accumulating evidence supports a targeted, context-dependent approach to redox modulation, recognizing both the cytoprotective benefits of NRF2 activation and the detrimental effects of uncontrolled NOX-derived ROS signaling.
Future research directions should focus on several critical areas: First, the development of tissue-specific and disease-stage-specific delivery systems to maximize therapeutic efficacy while minimizing off-target effects. Second, addressing the dual role of NRF2 in cancer, where transient activation prevents carcinogenesis but constitutive activation promotes tumor progression and therapy resistance [120]. Third, exploring combination therapies targeting both NRF2 and NOX pathways simultaneously, potentially offering synergistic benefits in complex multifactorial diseases. Finally, advancing biomarker-driven patient stratification using oxidative stress markers (F2-isoprostanes, 8-OHdG, protein carbonylation) to identify individuals most likely to respond to redox-targeted therapies [83] [74].
The integration of multi-omics approaches, artificial intelligence-based biomarker discovery, and patient-specific therapeutic interventions represents the promising frontier of precision redox medicine. As our understanding of redox signaling networks deepens, targeted NRF2 activation and NOX inhibition offer transformative potential for treating chronic inflammatory, neurodegenerative, and metabolic diseases that collectively represent a substantial global health burden.
Redox signaling is a fundamental regulator of macrophage function, influencing inflammation, metabolic adaptation, and immune responses. However, significant species-specific differences in redox biology between human and murine macrophages present a critical challenge in translating preclinical findings into effective clinical therapies. This whitepaper provides an in-depth technical analysis of the comparative redox mechanisms in human versus murine macrophage models. We synthesize current evidence on differential production of reactive oxygen and nitrogen species, divergent antioxidant defense mechanisms, and species-specific metabolic reprogramming during polarization. The document offers structured quantitative data, detailed experimental protocols for cross-species redox studies, and essential research tools to bridge the translational gap in inflammation and disease research.
Macrophages are phagocytic innate immune cells that play pivotal roles in immune regulation, tissue homeostasis, and inflammatory responses by interacting with various tissue types and secreting cytokines [121]. Redox signaling, involving the transfer of electrons from nucleophilic to electrophilic molecules, has emerged as an essential regulator of inflammatory macrophages [122]. This signaling modality is driven by reactive oxygen species (ROS), reactive nitrogen species (RNS), and redox-sensitive metabolites that post-translationally modify specific cysteine residues in target proteins [122].
The term "redox" is derived from "reduction" and "oxidation," describing chemical processes involving electron transfer between reactants [1]. In macrophages, redox reactions facilitate critical functions including phagocytic activity, cytokine production, metabolic reprogramming, and polarization into distinct functional phenotypes [121] [122]. Under physiological conditions, oxidative free radicals generated by mitochondrial respiration, endoplasmic reticulum, and NADPH oxidases are effectively neutralized by NRF2-mediated antioxidant responses, maintaining cellular redox homeostasis [1]. Disruption of this equilibrium is closely linked to pathogenesis across diverse diseases, making redox regulation a critical focus for therapeutic development [3] [1].
Comparative Biology of Human and Murine Macrophages
Fundamental Differences in Macrophage Models
Macrophages exhibit considerable heterogeneity based on developmental origin, tissue niche, and species-specific factors. Understanding these differences is essential for appropriate model selection and data interpretation.
Table 1: Comparison of Primary Macrophage Models Across Species
| Characteristic | Human Primary Macrophages | Murine Primary Macrophages (BMDMs) |
|---|---|---|
| Developmental Origin | Mixed embryonic and bone marrow-derived monocytes [121] | Predominantly bone marrow-derived monocytes [121] |
| Self-Renewal Capacity | Limited in monocyte-derived models; tissue-resident macrophages capable of self-renewal [121] | Varies by tissue source; limited in BMDMs [121] |
| Isolation Methodology | Density gradient centrifugation from PBMCs; ethical and logistical challenges [121] | Bone marrow flush from femurs/tibias with erythrocyte lysis [121] [123] |
| Differentiation Timeline | 5-7 days with M-CSF or GM-CSF [121] | 5-7 days with M-CSF or L929-conditioned medium [121] [123] |
| Proliferative Capacity | Terminally differentiated, non-proliferative [121] | Limited proliferative capacity [121] |
| Key Advantages | Direct human relevance; appropriate for translational studies [121] | Genetic manipulation ease; well-characterized polarization models [121] |
Table 2: Immortalized Macrophage Cell Lines Across Species
| Characteristic | Human Cell Lines (THP-1, U-937) | Murine Cell Lines (RAW264.7, J774A.1) |
|---|---|---|
| Origin | Derived from malignancies or viral transformation [121] | Derived from malignancies or viral transformation [121] |
| Proliferation | Rapid growth, unlimited passages [121] | Rapid growth, unlimited passages [121] |
| Genetic Stability | Prone to genotypic/phenotypic drift [121] | Prone to genotypic/phenotypic drift [121] |
| Functional Fidelity | May lack tissue-specific functions [121] | May lack tissue-specific functions [121] |
| Experimental Utility | Large-scale screens; reproducible assays [121] | Large-scale screens; reproducible assays [121] |
| Key Limitations | Genetic drift; altered polarization responses [121] | Genetic drift; altered polarization responses [121] |
Species-Specific Redox Signaling Mechanisms
Significant differences exist between human and murine macrophages in their redox regulatory mechanisms, creating substantial translational challenges.
Reactive Nitrogen Species Production
A well-documented difference between human and murine macrophages lies in their capacity for RNS production. Multiple studies confirm that human macrophages produce less RNS compared to mouse macrophages in response to inflammatory stimuli [3] [122]. This difference primarily stems from differential expression and regulation of inducible nitric oxide synthase (iNOS), which catalyzes nitric oxide (NO) production from arginine [122]. This fundamental disparity has profound implications for studying redox-regulated pathways in inflammation, as RNS function as crucial signaling molecules that regulate heme-containing proteins and iron-sulfur cluster-containing enzymes [122].
Reactive Oxygen Species Generation
Both human and murine macrophages generate ROS primarily through NADPH oxidases (NOX) and mitochondrial electron transport chains [122]. The NOX family of transmembrane enzymes produces cytosolic superoxide (O₂•â») via electron transfer from NADPH to molecular oxygen [122]. In phagocytes, NOX-generated superoxide production creates the "oxidative burst" essential for eliminating invading microorganisms [122]. Mitochondrial ROS (mtROS) predominantly originate from complexes I and III of the electron transport chain, with superoxide converted to hydrogen peroxide (Hâ‚‚Oâ‚‚) by superoxide dismutases (SOD1 and SOD2) [122]. While the core mechanisms are conserved, quantitative differences in ROS production and regulation exist between species, affecting downstream signaling pathways.
Quantitative Data Comparison: Human vs. Murine Macrophage Redox Biology
Table 3: Comparative Redox Signaling Components in Human vs. Murine Macrophages
| Redox Component | Human Macrophages | Murine Macrophages | Functional Implications |
|---|---|---|---|
| RNS Production | Lower output in response to inflammatory stimuli [3] [122] | Higher output; robust iNOS induction [3] [122] | Differential antimicrobial activity; altered signaling through heme proteins [122] |
| ROS Sources | NOX2, mitochondrial ETC complexes I & III [122] | NOX2, mitochondrial ETC complexes I & III [122] | Conserved mechanisms with potential quantitative differences |
| Antioxidant Systems | NRF2-mediated; SOD, catalase, GPX [1] | NRF2-mediated; SOD, catalase, GPX [1] | Generally conserved with potential regulatory differences |
| Metabolic Reprogramming | Glycolysis (M1); OxPhos (M2) [123] | Glycolysis (M1); OxPhos (M2) [123] | Conserved metabolic signatures during polarization |
| Cysteine Redox Modifications | S-glutathionylation, S-nitrosylation, S-sulfenylation [1] | S-glutathionylation, S-nitrosylation, S-sulfenylation [1] | Conserved modification types with potential target specificity |
Experimental Protocols for Cross-Species Redox Studies
Protocol 1: Isolation and Differentiation of Bone Marrow-Derived Macrophages (BMDMs)
This fundamental protocol for generating murine macrophages is adapted from established methodologies [121] [123] and serves as a cornerstone for redox studies.
Materials and Reagents
- Animals: C57BL/6J mice (8-12 weeks old) [123]
- Extraction Medium: High-glucose DMEM supplemented with 10% fetal bovine serum (FBS), 1% penicillin/streptomycin [123]
- Differentiation Medium: High-glucose DMEM supplemented with 20% FBS and 30% L929-conditioned medium (as source of M-CSF) [123]
- Erythrocyte Lysis Buffer: Ammonium-chloride-based solution
- Surgical Instruments: Sterile scissors, forceps, 25-G needles, 5ml syringes [123]
Procedure
- Euthanize mice according to approved institutional protocols [123].
- Extract hind limbs and remove surrounding muscle tissue under sterile conditions [123].
- Cut femur and tibia ends and flush bone marrow with 5ml extraction medium using a 25-G needle [123].
- Create single-cell suspension by passing aspirate through needles of decreasing sizes (18G, 21G, 23G, 25G) [123].
- Perform erythrocyte lysis using ammonium-chloride-based lysis buffer.
- Resuspend cells in differentiation medium at concentration of 10ⶠcells/ml [123].
- Seed cells at 40,000 cells/cm² in appropriate culture vessels [123].
- Differentiate for 7 days with medium refresh on day 3 [123].
- Verify differentiation through morphology (adherent, spindle-shaped cells) and surface marker analysis (F4/80, CD11b) [121].
Protocol 2: Macrophage Polarization and Redox Analysis
This protocol outlines standardized approaches for polarizing macrophages toward M1 and M2 phenotypes and assessing subsequent redox changes.
Polarization Induction
- M1 Polarization: Treat mature BMDMs or human monocyte-derived macrophages with 100ng/ml LPS + 20ng/ml IFN-γ for 24-48 hours [121] [123]
- M2 Polarization: Treat with 20ng/ml IL-4 for 72 hours [121] [123]
Redox Status Assessment
ROS/RNS Detection:
- Use fluorescent probes (Hâ‚‚DCFDA for general ROS, DAF-FM for NO)
- Employ HPLC-based methods for specific ROS/RNS quantification
- Apply redox-sensitive GFP probes for compartment-specific monitoring
Metabolic Phenotyping:
Cysteine Redox Proteomics:
- Utilize resin-assisted capture methods to identify redox-modified cysteines
- Apply mass spectrometry-based approaches for site-specific mapping
Redox Signaling Pathways in Macrophage Polarization
The following diagrams visualize key redox signaling pathways and experimental workflows in macrophage biology.
Diagram 1: Redox Regulation of Macrophage Polarization. Macrophages polarize into pro-inflammatory M1 or anti-inflammatory M2 states in response to environmental stimuli, with distinct redox and metabolic features [123] [122]. M1 polarization driven by LPS and IFN-γ promotes glycolytic metabolism and increased ROS production, while M2 polarization driven by IL-4 enhances oxidative phosphorylation with lower ROS generation [123].
Diagram 2: Experimental Workflow for Cross-Species Redox Comparison. This workflow outlines a standardized approach for comparative studies of redox biology in human versus murine macrophage models, enabling systematic identification of conserved and species-specific mechanisms [121] [123] [122].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for Macrophage Redox Studies
| Reagent Category | Specific Examples | Function & Application | Species Considerations |
|---|---|---|---|
| Polarization Inducers | LPS, IFN-γ, IL-4, IL-13 [121] [123] | Direct macrophage polarization toward M1 or M2 phenotypes | Conserved response; concentration optimization may be needed |
| ROS Detection Probes | Hâ‚‚DCFDA, MitoSOX, Amplex Red | Quantify general ROS, mitochondrial superoxide, and Hâ‚‚Oâ‚‚ | Similar applicability across species with proper controls |
| RNS Detection Probes | DAF-FM, NO-sensitive electrodes | Measure nitric oxide production | Critical for species comparison due to differential iNOS expression [3] [122] |
| Metabolic Inhibitors | Rotenone (Complex I), Antimycin A (Complex III), 2-DG (glycolysis) | Dissect metabolic contributions to redox signaling | Similar mitochondrial targets; potential efficacy differences |
| Cysteine Redox Tools | Iodoacetamide, N-ethylmaleimide, biotin-conjugated thiol reagents | Identify and characterize cysteine redox modifications | Conserved chemistry; target availability may vary |
| Antioxidant Compounds | N-acetylcysteine, Tempol, mito-TEMPO | Modulate redox status and test functional implications | Similar mechanisms; species-specific efficacy possible |
| Cytokine Analysis | ELISA, Luminex, ELISA-based cytokine arrays | Quantify inflammatory secretome | Antibody cross-reactivity limitations for multi-species studies |
The comparative analysis of redox biology in human versus murine macrophages reveals both conserved mechanisms and critical species-specific differences that significantly impact translational research. The most prominent distinction lies in RNS production, with human macrophages generating substantially lower levels than their murine counterparts [3] [122]. This disparity necessitates careful interpretation of data from murine models, particularly for conditions where nitric oxide signaling plays a central role.
Future research should prioritize the development of standardized cross-species experimental frameworks that systematically account for these differences. Advanced humanized mouse models, improved human macrophage differentiation protocols, and multi-omics approaches will enhance our understanding of species-specific redox regulation. Furthermore, the growing recognition of redox-sensitive metabolites as key regulators of macrophage function presents new opportunities for therapeutic intervention [122].
Bridging the species gap in macrophage redox biology requires continued refinement of experimental models, validation of findings across multiple systems, and cautious interpretation of murine data in the human context. By addressing these challenges, researchers can better leverage the strengths of both human and murine systems to advance our understanding of redox biology in inflammation and disease.
The therapeutic targeting of redox signaling represents a transformative frontier in the management of chronic inflammation, cancer, neurodegenerative, and cardiovascular diseases. This systematic review synthesizes the current landscape of clinical trials investigating redox-targeted interventions, evaluating their mechanistic rationales, clinical outcomes, and methodological approaches. Despite strong preclinical evidence, the translation of redox therapies has been challenged by the dual nature of reactive oxygen species (ROS) as both signaling molecules and damaging agents, the context-dependent outcomes of antioxidant versus pro-oxidant strategies, and patient heterogeneity. Recent trials have shifted from broad-spectrum antioxidants toward precision approaches including NRF2 activators, mitochondria-targeted compounds, pro-oxidant therapies for cancer, and senolytics. This review provides a critical analysis of completed and ongoing clinical investigations, detailed experimental methodologies, and emerging research tools, framed within the broader thesis that understanding redox signaling networks is essential for developing effective therapeutic interventions for inflammatory diseases and beyond.
Redox signaling acts as a critical mediator in the dynamic interactions between organisms and their external environment, profoundly influencing both the onset and progression of various diseases [1]. The term "redox" encompasses reduction-oxidation reactions involving the transfer of electrons between reactants in chemical reactions, fundamental processes underlying cellular energy production and signaling networks [3]. Under physiological conditions, oxidative free radicals generated by the mitochondrial oxidative respiratory chain, endoplasmic reticulum, and NADPH oxidases are effectively neutralized by NRF2-mediated antioxidant responses, maintaining cellular redox homeostasis [1].
The relationship between oxidative stress (OS) and inflammation is not merely sequential but synergistic, establishing a pathogenic loop that sustains chronic inflammation [4]. Elevated ROS levels influence the redox-sensitive activity of transcription factors such as NF-κB, which drives the expression of adhesion molecules, cytokines, chemokines, and matrix metalloproteinases, thereby amplifying tissue recruitment of immune cells and sustaining inflammatory circuits [4]. These dynamics have been extensively documented in several pathological conditions, including atherosclerosis, neurodegeneration, non-alcoholic steatohepatitis, inflammatory bowel diseases, and rheumatoid arthritis [4].
Emerging evidence underscores the equally significant, yet often overlooked, role of reductive stress (RS)—a condition where an excess of reducing equivalents disrupts redox homeostasis—in modulating inflammatory responses and contributing to various pathologies [4]. This bidirectional nature of redox dysregulation necessitates a nuanced therapeutic approach that moves beyond simple antioxidant supplementation toward strategies that restore precise redox balance within specific cellular compartments [4] [3].
Table 1: Key Reactive Species in Redox Signaling and Their Sources
| Reactive Species | Type | Primary Sources | Cellular Targets |
|---|---|---|---|
| Superoxide (O₂•â») | ROS | Mitochondrial ETC complexes I & III, NOX enzymes | Proteins, iron-sulfur clusters |
| Hydrogen Peroxide (Hâ‚‚Oâ‚‚) | ROS | SOD-catalyzed dismutation of O₂•â», NOX4 | Redox-sensitive cysteine residues |
| Hydroxyl Radical (•OH) | ROS | Fenton reaction (Hâ‚‚Oâ‚‚ + Fe²âº) | DNA, lipids, proteins |
| Nitric Oxide (NO•) | RNS | Nitric oxide synthases (NOS) | Guanylate cyclase, mitochondrial complexes |
| Peroxynitrite (ONOOâ») | RNS | Reaction of NO• with O₂•⻠| Tyrosine nitration, mitochondrial damage |
Methodological Framework for Redox Clinical Trials
Search Strategy and Selection Criteria
This review followed a systematic approach to identify relevant clinical trials and preclinical studies. A comprehensive literature search was conducted across multiple electronic databases including PubMed, Scopus, Embase, and ClinicalTrials.gov from inception to January 2025. The search strategy incorporated Medical Subject Headings (MeSH) and keywords related to "redox therapy," "oxidative stress," "clinical trials," "NRF2 activators," "mitochondria-targeted antioxidants," "pro-oxidant therapy," and specific intervention names. Boolean operators (AND, OR) were used to combine search terms.
Studies were included if they met the following criteria: (1) randomized controlled trials (RCTs), phase I-IV clinical trials, or systematic reviews/meta-analyses of redox-targeted interventions; (2) investigations in humans or preclinical models relevant to oxidative stress pathways; (3) interventions specifically targeting redox signaling pathways; and (4) reporting of clinical outcomes, biomarker data, or safety profiles. Exclusion criteria included: (1) case reports with fewer than 10 patients; (2) non-English publications; (3) studies not specifically measuring redox-related parameters; and (4) investigations using only broad-spectrum antioxidants without specific redox targets.
Assessment of Redox Biomarkers
A critical component of redox clinical trials is the accurate measurement of oxidative stress markers and antioxidant capacity. Standardized methodologies have been developed for assessing various redox parameters:
- Lipid peroxidation products: Malondialdehyde (MDA) and 4-hydroxynonenal (4-HNE) measured via thiobarbituric acid reactive substances (TBARS) assay or liquid chromatography-mass spectrometry (LC-MS) [98].
- Protein oxidation: Carbonylated proteins detected using 2,4-dinitrophenylhydrazine (DNPH) derivatization followed by Western blot or ELISA [74].
- DNA damage: 8-hydroxy-2'-deoxyguanosine (8-OHdG) quantified in urine or plasma using ELISA or LC-MS [74].
- Antioxidant enzymes: Superoxide dismutase (SOD), catalase, and glutathione peroxidase (GPx) activities measured via colorimetric or fluorometric assays [1].
- Glutathione status: Reduced (GSH) to oxidized (GSSG) glutathione ratio determined using high-performance liquid chromatography (HPLC) or enzymatic recycling assays [102].
- Transcriptional activators: NRF2 activation assessed through nuclear translocation assays or measurement of downstream targets like NAD(P)H quinone dehydrogenase 1 (NQO1) and heme oxygenase-1 (HO-1) [4] [1].
Redox-Targeted Interventions: Mechanisms and Clinical Applications
NRF2 Activators
The NRF2-Keap1 pathway serves as the master regulator of cellular antioxidant responses, making it a prime therapeutic target. Under basal conditions, NRF2 is bound to Keap1, which facilitates its ubiquitination and degradation. Oxidative stress or pharmacological activators modify critical cysteine residues on Keap1, leading to NRF2 stabilization and nuclear translocation, where it binds to antioxidant response elements (AREs) and induces cytoprotective gene expression [4] [1].
Dimethyl fumarate (Tecfidera) has been approved for multiple sclerosis and demonstrates efficacy in preclinical models of neurodegenerative and inflammatory conditions. It activates NRF2, leading to increased glutathione synthesis and protection against oxidative neuronal damage [74]. Clinical trials have shown reduced disease activity in multiple sclerosis, with decreased inflammatory markers and enhanced antioxidant capacity.
Sulforaphane, derived from cruciferous vegetables, has shown promise in clinical trials for various conditions including autism spectrum disorders, COPD, and cancer prevention. It induces NRF2-mediated gene expression and enhances glutathione biosynthesis, demonstrating protective effects against oxidative damage in the brain and lungs [74].
Table 2: Clinical Trial Landscape of NRF2-Targeted Therapeutics
| Intervention | Mechanism | Disease Target | Trial Phase | Key Findings |
|---|---|---|---|---|
| Dimethyl Fumarate | NRF2 activator, induces ARE genes | Multiple Sclerosis, Psoriasis | Marketed | Reduced relapse rates, increased NQO1 expression, decreased oxidative damage markers |
| Sulforaphane | Isothiocyanate that activates NRF2 | Autism, COPD, Cancer Prevention | Phase II | Improved social responsiveness in autism; enhanced glutathione synthesis; increased antioxidant capacity |
| Bardoxolone Methyl | Synthetic triterpenoid NRF2 inducer | CKD, Pulmonary Hypertension | Phase III | Improved eGFR in CKD patients; pulmonary hemodynamic improvements; side effects include muscle cramps |
| Omaveloxolone | NRF2 activator | Friedreich's Ataxia | Phase III | Improved neurological function; modified NRF2 pathway gene expression |
Mitochondria-Targeted Antioxidants
Mitochondria represent the primary source of endogenous ROS, and their dysfunction is implicated across numerous disease states. Mitochondria-targeted antioxidants represent a sophisticated approach to combat compartment-specific oxidative stress.
MitoQ consists of ubiquinone attached to a triphenylphosphonium cation, facilitating accumulation in the mitochondrial matrix. Clinical trials have investigated MitoQ in Parkinson's disease, non-alcoholic fatty liver disease (NAFLD), and cardiovascular conditions. While some studies show reduced liver inflammation in NAFLD and improved vascular function, results in neurodegenerative diseases have been modest, suggesting timing and patient selection are critical factors [74].
SKQ1 (Visomitin) is a plastoquinone derivative conjugated with a lipophilic cation that accumulates in mitochondria. It has shown promise in dry eye syndrome and age-related inflammatory conditions by mitigating mitochondrial ROS and preventing apoptosis [74].
Elamipretide (SS-31) targets the inner mitochondrial membrane, interacting with cardiolipin to reduce ROS production and improve mitochondrial efficiency. It has been investigated in primary mitochondrial myopathies, heart failure, and renal disease, demonstrating improved exercise tolerance and cardiac function in specific patient populations [3] [74].
Pro-oxidant Therapies in Cancer
The "redox paradox" in cancer describes how ROS simultaneously drive tumorigenesis yet can be harnessed to eliminate malignant cells. Cancer cells exist under chronic oxidative stress and develop dependency on enhanced antioxidant systems, creating a vulnerability to further oxidative insult [102].
High-dose Vitamin C (Ascorbic Acid) acts as a pro-oxidant when administered intravenously at high concentrations, generating hydrogen peroxide selectively in the tumor microenvironment. Clinical trials have investigated its potential in combination with chemotherapy for pancreatic, ovarian, and glioblastoma multiforme, with some studies showing improved quality of life and potential synergy with standard treatments [102].
Auranofin, an FDA-approved anti-rheumatic drug, inhibits thioredoxin reductase (TrxR), a key component of the antioxidant system in cancer cells. It is being repurposed in clinical trials for leukemia, ovarian cancer, and other solid tumors, demonstrating induction of oxidative stress-mediated apoptosis in cancer cells [102].
Arsenic Trioxide (ATO) promotes ROS generation and has shown efficacy in acute promyelocytic leukemia (APL), now serving as standard care. Trials are exploring ATO in other hematological malignancies and solid tumors, with research focusing on its combination with other redox-modulating agents [102].
Brusatol and ML385 represent a newer class of NRF2 inhibitors that block the antioxidant response in cancer cells, increasing their susceptibility to oxidative damage. These are primarily in early-phase clinical development, with preclinical models showing enhanced chemotherapy sensitivity [102].
Glutathione System Modulators
The glutathione (GSH) system represents one of the primary cellular defense mechanisms against oxidative stress. Therapeutic approaches have targeted GSH synthesis, utilization, and regeneration.
N-acetylcysteine (NAC) serves as a precursor for glutathione synthesis and has been extensively studied in paracetamol overdose, COPD, psychiatric disorders, and cardiovascular diseases. While highly effective in acetaminophen toxicity, results in chronic conditions have been mixed, potentially due to timing, dosage, and patient selection issues [1].
Cystine-glutamate exchange inhibitors such as sulfasalazine and erastin inhibit system Xc-, depleting intracellular cysteine and consequently glutathione, leading to ferroptosis—an iron-dependent form of cell death characterized by lipid peroxidation. Early-phase trials are investigating these approaches in glioblastoma and other treatment-resistant cancers [102].
Senolytics and Redox Modulation
Cellular senescence represents a state of permanent growth arrest accompanied by a pro-inflammatory secretory phenotype (SASP). Senescent cells accumulate with age and contribute to tissue dysfunction. Interestingly, senescent cells display altered redox homeostasis, potentially creating therapeutic vulnerabilities.
Redox-targeting senolytics include Fisetin and Quercetin (natural flavonoids with antioxidant and pro-oxidant properties depending on context), Navitoclax (BCL-2 inhibitor that disrupts mitochondrial redox signaling), and A1331852/A1155463 (specific BCL-XL inhibitors). Clinical trials are ongoing for idiopathic pulmonary fibrosis, diabetic kidney disease, and other age-related conditions, with early results showing improved physical function and reduced senescence biomarkers [124] [125].
Figure 1: Redox Signaling Pathways in Inflammation and Therapeutic Targeting. This diagram illustrates the central role of redox imbalance in driving inflammatory pathways through NF-κB activation, NLRP3 inflammasome assembly, and cellular senescence with SASP secretion, ultimately leading to tissue damage and disease. The counterbalancing NRF2 pathway promotes antioxidant gene expression and restoration of redox homeostasis, representing key therapeutic targets.
Detailed Experimental Protocols for Redox-Targeted Interventions
Assessment of NRF2 Pathway Activation
Protocol Objective: To evaluate NRF2 activation and downstream antioxidant response in patient samples or cellular models following interventional administration.
Methodology:
- Nuclear Translocation Assay: Isolate nuclear and cytoplasmic fractions from peripheral blood mononuclear cells (PBMCs) collected at baseline and post-intervention time points (e.g., 4, 24, 48 hours). Perform Western blot analysis using anti-NRF2 antibodies. Calculate nuclear-to-cytoplasmic NRF2 ratio as an indicator of activation.
- Gene Expression Profiling: Extract total RNA from patient PBMCs or tissue biopsies. Conduct quantitative RT-PCR for NRF2 target genes including NQO1, HO-1, GCLC, and GCLM. Normalize expression to housekeeping genes (GAPDH, β-actin).
- ARE-Binding Activity: Perform electrophoretic mobility shift assay (EMSA) using nuclear extracts and biotin-labeled ARE consensus oligonucleotides. Confirm specificity with excess unlabeled competitor oligonucleotides.
- Antioxidant Enzyme Activity: Measure catalytic activities of NRF2-regulated enzymes including NQO1 (using dichlorophenolindophenol reduction assay), GST (using 1-chloro-2,4-dinitrobenzene conjugation), and total glutathione levels (using enzymatic recycling assay with DTNB).
Clinical Application: This protocol has been standardized for trials investigating dimethyl fumarate, bardoxolone methyl, and sulforaphane, providing pharmacodynamic evidence of target engagement [4] [1] [74].
Mitochondrial ROS Measurement in Clinical Trials
Protocol Objective: To quantitatively assess mitochondrial-specific reactive oxygen species production in patient-derived cells following intervention with mitochondria-targeted antioxidants.
Methodology:
- Cell Collection and Processing: Isolate platelets, lymphocytes, or neutrophils from patient blood samples collected in EDTA or heparin tubes at baseline and specified post-treatment intervals.
- Mitochondrial Superoxide Detection: Stain cells with MitoSOX Red (5 μM) for 30 minutes at 37°C. Include positive control (antimycin A, 10 μM) and negative control (MitoTEMPO, 100 μM). Analyze via flow cytometry with excitation/emission at 510/580 nm.
- Mitochondrial Membrane Potential: Assess using JC-1 dye (5 μg/mL) with flow cytometric analysis of red/green fluorescence ratio. Include carbonyl cyanide m-chlorophenyl hydrazone (CCCP, 50 μM) as depolarization control.
- High-Resolution Respirometry: For clinical trials with tissue access (muscle biopsies), perform Oroboros O2k respirometry to assess mitochondrial function parameters including basal respiration, ATP-linked respiration, proton leak, and maximal respiratory capacity.
Clinical Application: This comprehensive mitochondrial assessment protocol has been implemented in trials of MitoQ, elamipretide, and SKQ1, providing direct evidence of mitochondrial target engagement and functional improvement [3] [74].
Ferroptosis Induction Assessment in Cancer Trials
Protocol Objective: To monitor ferroptosis induction in tumor cells or patient samples following pro-oxidant interventions targeting the glutathione system.
Methodology:
- Lipid Peroxidation Measurement:
- Extract lipids from tumor biopsies or patient-derived xenografts at baseline and post-treatment.
- Analyze lipid hydroperoxides using FOX2 assay or C11-BODIPYâµâ¸Â¹/âµâ¹Â¹ fluorescence shift.
- Quantify specific oxidized phospholipid species via LC-MS/MS.
- Glutathione Depletion Assessment:
- Measure intracellular GSH/GSSG ratio using HPLC with electrochemical detection or fluorescent probes (monochlorobimane).
- Confirm system Xc- inhibition via cystine uptake assays with ¹â´C-cystine.
- Morphological Assessment:
- Process tumor biopsies for electron microscopy to identify characteristic mitochondrial features of ferroptosis (reduced size, increased membrane density, absent cristae).
- Cell Death Inhibition Profiling:
- Treat patient-derived organoids with intervention alone or in combination with ferroptosis inhibitors (ferrostatin-1, liproxstatin-1), apoptosis inhibitors (Z-VAD-FMK), and necroptosis inhibitors (necrostatin-1) to confirm ferroptosis as the primary death mechanism.
Clinical Application: This multi-parameter assessment protocol is essential for trials investigating sulfasalazine, erastin, and other ferroptosis-inducing agents, providing mechanistic confirmation of cell death modality [102] [125].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Redox Signaling Investigations
| Reagent/Category | Specific Examples | Research Application | Mechanistic Insight |
|---|---|---|---|
| NRF2 Pathway Modulators | Sulforaphane, Bardoxolone Methyl, ML385 | NRF2 activation/inhibition studies | Keap1 cysteine modification, ARE-driven gene expression |
| Mitochondrial-Targeted Antioxidants | MitoQ, MitoTEMPO, SS-31 | Mitochondrial ROS assessment | Cardiolipin protection, ETC complex regulation |
| GSH System Modulators | BSO, NAC, Erastin, Sorafenib | Glutathione depletion/repletion studies | System Xc- inhibition, GPX4 inactivation, ferroptosis induction |
| ROS/RNS Generators | Menadione, Paraquat, SIN-1 | Controlled oxidative stress induction | Superoxide, Hâ‚‚Oâ‚‚, and peroxynitrite generation |
| Redox-Sensitive Probes | MitoSOX, H2DCFDA, roGFP | Compartment-specific ROS measurement | Mitochondrial matrix, cytosolic, and nuclear redox status |
| Thiol Status Assessment | DTNB, Monobromobimane, IAM | Protein thiol oxidation mapping | Cysteine sulfenylation, glutathionylation, disulfide formation |
Figure 2: Experimental Workflow for Assessing Redox-Targeted Therapies in Clinical Trials. This diagram outlines a comprehensive approach for evaluating redox-targeted interventions, from patient stratification based on redox biomarkers through multi-parameter assessment of target engagement and correlation with clinical outcomes.
Challenges and Future Directions in Redox-Targeted Clinical Trials
The clinical translation of redox-targeted therapies faces several significant challenges that must be addressed in future trial design:
Context-Dependent Outcomes and Patient Stratification
The dual nature of ROS as both signaling molecules and damaging agents creates complex, context-dependent outcomes that have complicated clinical development. Future trials require sophisticated patient stratification strategies based on:
- Baseline redox status using comprehensive biomarker panels
- Genetic polymorphisms in NRF2, glutathione S-transferases, and other redox-related genes
- Disease stage and microenvironment characteristics
- Mitochondrial function parameters assessed through respirometry and imaging
The failure of broad-spectrum antioxidants in large cardiovascular trials highlights the importance of targeting specific redox pathways in appropriately selected patient populations [3].
Compartment-Specific Targeting and Delivery
The subcellular compartmentalization of redox signaling necessitates precision targeting approaches. Future directions include:
- Advanced nanocarriers for organelle-specific delivery of redox modulators
- Mitochondria-targeted pro-oxidants for selective cancer cell elimination
- Dual-acting compounds that simultaneously modulate multiple redox nodes
- Conditionally activated prodrugs that release active redox modulators only in specific microenvironments (e.g., hypoxic tumor regions)
Temporal Dynamics and Dosing Considerations
The temporal dynamics of redox interventions present particular challenges, as demonstrated by the opposing effects of antioxidants in cancer prevention versus treatment. Future strategies must consider:
- Chronotherapeutic approaches aligned with circadian redox fluctuations
- Pulsed versus continuous dosing regimens based on mechanism of action
- Adaptive trial designs that permit dosage adjustments based on real-time redox biomarker monitoring
- Combination strategies that sequence pro-oxidant and antioxidant approaches appropriately
Biomarker Development and Validation
The advancement of redox therapeutics requires robust biomarker development including:
- Integrated redox panels combining oxidative damage markers with antioxidant capacity assessments
- Non-invasive imaging approaches for in vivo redox status monitoring
- Multi-omics integration of redox proteomics, lipidomics, and metabolomics
- Point-of-care devices for rapid assessment of key redox parameters
The clinical trial landscape for redox-targeted interventions has evolved substantially from initial approaches using broad-spectrum antioxidants toward sophisticated strategies that precision-target specific redox nodes. The growing understanding of redox signaling networks in inflammation, cancer, neurodegeneration, and aging has revealed both challenges and opportunities for therapeutic development. Success in this field requires careful consideration of context dependency, compartmentalization, patient stratification, and temporal dynamics. Future clinical trials must incorporate comprehensive biomarker assessments, innovative trial designs, and targeted delivery approaches to fulfill the promise of redox modulation as a therapeutic strategy across the disease spectrum. The integration of multi-omics technologies, artificial intelligence, and patient-specific redox profiling represents the next frontier in the precision targeting of redox signaling for therapeutic benefit.
The intricate interplay between sulfur-based redox signaling and epigenetic modulation represents a transformative frontier in molecular medicine. This in-depth technical guide explores the mechanistic roles of reactive sulfur species (RSS), particularly supersulfides and hydrogen polysulfides, as potent regulators of inflammatory pathways and epigenetic landscapes. Within the broader context of redox signaling in inflammation and disease research, we detail how sulfur catenation chemistry endows these molecules with unique biological activities through specific post-translational modifications, primarily protein persulfidation. This review provides a comprehensive framework for target validation, including detailed methodologies for detecting RSS and profiling epigenetic modifications, alongside critical reagent solutions. The emerging paradigm reveals sophisticated sulfur-mediated mechanisms that integrate metabolic sensing with transcriptional reprogramming, offering novel therapeutic targets for inflammatory diseases, neurological disorders, and cancer. This synthesis aims to equip researchers and drug development professionals with the technical foundation necessary to advance this rapidly evolving field.
Sulfur is the third most abundant mineral in the human body and serves as a fundamental component of redox signaling networks [126]. Beyond its traditional roles in protein structure and metabolism, sulfur exists in diverse chemical species with distinct redox properties that influence cellular function. Recent advances in mass spectrometry-based metabolomics have revealed an extensive landscape of reactive sulfur species (RSS), including supersulfides (characterized by catenated sulfur chains in their structures), hydropersulfides, hydropolysulfides (RSSnH, n > 1), and polysulfides (RSSnR, n > 1) [126]. These species demonstrate enhanced reactivity compared to their monothiol counterparts due to lower pKa values, facilitating more efficient deprotonation and nucleophilic activity under physiological conditions [126].
The conceptual framework of this review positions sulfur-based redox signaling as a critical integrator of metabolic status and epigenetic regulation. The "Redox Code" describes fundamental principles governing how NADH and NADPH systems regulate metabolism, how thiol switches dynamically control the redox proteome, and how H2O2 production cycles respond to environmental changes [1]. This code provides a systems-level understanding of how redox signaling influences cellular phenotype through both genetic and epigenetic mechanisms. Redox balance is not merely a passive indicator of cellular health but an active regulatory system that coordinates adaptation to stress, inflammation, and metabolic changes through precise molecular mechanisms.
Epigenetics, defined as "the structural adaptation of chromosomal regions so as to register, signal or perpetuate altered activity states," provides the mechanistic link between sulfur redox biology and sustained changes in gene expression patterns [127]. The integration of redox signaling with epigenetic modifications creates a sophisticated system for translating environmental and metabolic cues into phenotypic outcomes. This review explores the validated targets emerging at this interface, with particular emphasis on their implications for inflammatory diseases and their therapeutic potential.
Molecular Mechanisms of Sulfur Species in Redox Signaling
Supersulfides and Polysulfides: Unique Chemical Properties
Supersulfides demonstrate unique biological activities attributable to their catenation state—the chain of multiple sulfur atoms that defines their structure [126]. This catenation confers enhanced nucleophilicity and redox potential compared to conventional thiols. For instance, glutathione persulfide (GSSH) exhibits a pKa of 6.9, approximately two orders of magnitude lower than that of glutathione (GSH, pKa 8.9), making GSSH significantly more reactive at physiological pH [126]. This property enables supersulfides to function as more potent antioxidants and redox regulators than their monothiol counterparts.
The enhanced chemical reactivity of supersulfides translates to greater biological potency. Hydrogen polysulfides (H2Sn) have been shown to induce calcium mobilization by activating transient receptor potential A1 (TRPA1) channels with a potency 320 times greater than that of hydrogen sulfide (H2S) [126]. This dramatic difference in potency highlights the critical importance of sulfur catenation in biological signaling and underscores why supersulfides represent a distinct class of signaling molecules rather than mere reservoirs or intermediates in H2S metabolism.
Biosynthetic Pathways for Reactive Sulfur Species
Table 1: Enzymatic Sources of Reactive Sulfur Species
| Enzyme | Cellular Location | Primary Substrates | Sulfur Products | Biological Significance |
|---|---|---|---|---|
| Cystathionine β-synthase (CBS) | Cytosol | Cysteine, Homocysteine | CysSSH, H2S | Highly expressed in central nervous system |
| Cystathionine γ-lyase (CSE) | Cytosol | Cysteine, Homocysteine | CysSSH, H2S | Abundant in cardiovascular system |
| 3-Mercaptopyruvate sulfurtransferase (3-MST) | Mitochondria | 3-Mercaptopyruvate | Protein-bound supersulfides, H2S | Links sulfur metabolism to energy production |
| Cysteinyl-tRNA synthetase (CARS) | Cytosol (CARS1), Mitochondria (CARS2) | Cysteine | CysSSH, tRNA-bound supersulfides | Novel cysteine persulfide synthase; mitochondrial CARS2 critical for supersulfide production |
Supersulfide production occurs through both enzymatic and chemical processes. The transsulfuration pathway enzymes, cystathionine β-synthase (CBS) and cystathionine γ-lyase (CSE), catalyze the conversion of cysteine to cysteine persulfide (CysSSH), which can undergo disproportionation to form oxidized species like cysteine trisulfide while releasing H2S [126]. Similarly, 3-mercaptopyruvate sulfurtransferase generates both low-molecular-weight and protein-bound supersulfides [126]. Notably, studies using triple-knockout mice lacking CBS, CSE, and 3-MST revealed that supersulfide production persists, indicating the existence of compensatory or alternative synthetic pathways [126].
A significant breakthrough in the field came with the identification of cysteinyl-tRNA synthetase (CARS) as a novel cysteine persulfide synthase (CPERS) [126]. This enzyme performs dual enzymatic functions: it catalyzes the formation of tRNA-bound CysSSH adducts for incorporation into proteins, and it synthesizes CysSSH through a pyridoxal phosphate (PLP)-dependent reaction using a second cysteine molecule as the sulfur donor. Genetic evidence supports the critical role of CARS2, the mitochondrial isoform, in supersulfide production, as heterozygous knockout mice show approximately 50% lower supersulfide levels compared to wild-type mice [126].
Protein Persulfidation: A Key Redox Modification
Protein persulfidation (S-sulfhydration) represents a major mechanism through which reactive sulfur species transduce redox signals. This post-translational modification involves the conversion of cysteine thiol groups (-SH) to persulfide groups (-SSH) on target proteins, altering their structure, function, and stability [128]. Early work by Snyder and colleagues introduced this concept, though the mechanism has since been refined to emphasize the role of hydrogen polysulfides (H2Sn) rather than H2S itself in the modification process [128].
Persulfidation exhibits several distinctive features as a redox switch. First, it targets specific cysteine residues with particular microenvironments, especially those that are S-nitrosylated or S-sulfenylated, creating cross-talk between different redox modifications [128]. Second, persulfidation is reversible through the action of reductases like thioredoxin and glutaredoxin, allowing dynamic regulation [1]. Third, this modification can affect diverse protein functions, including enzymatic activity, subcellular localization, protein-protein interactions, and degradation.
Diagram 1: Protein Persulfidation Cycle. Reactive sulfur species mediate the conversion of protein thiols (-SH) to persulfides (-SSH), which can be reversed by cellular reductases like thioredoxin (Trx) and glutaredoxin (Grx).
Epigenetic Regulation by Redox Mechanisms
Metabolic Interfaces Between Redox and Epigenetic Systems
Epigenetic modifications represent a fundamental mechanism for translating multiple signaling inputs, including redox status, into phenotypic outputs. The major epigenetic marks—histone methylation, acetylation, ADP-ribosylation, and DNA methylation—have direct connections to central metabolism through critical redox-sensitive intermediates [127]. Three metabolites in particular serve as key connectors between redox state and epigenetic regulation: NAD+, S-adenosyl methionine (SAM), and 2-oxoglutarate.
S-adenosyl methionine (SAM) serves as the universal methyl donor for histone and DNA methyltransferases. SAM is synthesized from methionine and ATP, with methionine availability being influenced by the redox environment [129]. During methylation reactions, SAM transfers its methyl group to form S-adenosylhomocysteine (SAH), a potent inhibitor of methyltransferases when accumulated. The ratio of SAM to SAH therefore serves as a key indicator of cellular methylation potential, creating a direct link between sulfur amino acid metabolism and epigenetic regulation [127].
NAD+ functions as an essential cofactor for class III histone deacetylases (sirtuins), which catalyze the removal of acetyl groups from histone lysine residues in an NAD+-dependent manner. This reaction generates nicotinamide and O-acetyl-ADP-ribose, directly coupling epigenetic regulation to cellular redox status through the NAD+/NADH ratio [127]. The NAD+ salvage pathway and biosynthesis thus represent potential points of redox control over epigenetic states.
Redox-Sensitive Epigenetic Enzymes
Table 2: Redox-Sensitive Epigenetic Modifying Enzymes
| Enzyme Class | Specific Enzymes | Redox-Sensitive Cofactors/Intermediates | Functional Outcomes |
|---|---|---|---|
| Histone Demethylases | LSD1, JmjC-domain containing demethylases | FAD, 2-oxoglutarate, Fe(II), O2 | H3K4me2/me1 demethylation; responsive to oxygen availability |
| DNA Methyltransferases | DNMT1, DNMT3A/B | SAM, SAH | Methylation potential affected by SAM/SAH ratio |
| Histone Acetyltransferases | p300/CBP, MYST family | Acetyl-CoA | Acetylation linked to metabolic status via acetyl-CoA availability |
| Histone Deacetylases | Sirtuins (SIRT1-7) | NAD+ | Activity directly responsive to NAD+/NADH ratio |
| Ten-Eleven Translocation (TET) Enzymes | TET1-3 | 2-oxoglutarate, Fe(II), O2 | DNA demethylation; sensitive to oxidative stress and hypoxia |
Histone demethylases represent a particularly redox-sensitive class of epigenetic regulators. Lysine-specific demethylase 1 (LSD1), the first identified histone demethylase, requires flavin adenine dinucleotide (FAD) as a cofactor and demethylates histone H3 on lysine 4 or 9 through an amine oxidation process [127]. The Jumonji C (JmjC)-domain containing histone demethylases utilize 2-oxoglutarate, Fe(II), and molecular oxygen to catalyze hydroxylation-based demethylation, making them sensitive to cellular oxygen levels, iron availability, and TCA cycle function [127]. Under conditions of redox imbalance or metabolic stress, the activities of these demethylases can be significantly altered, leading to durable changes in histone methylation patterns.
DNA methyltransferases (DNMTs) transfer methyl groups from SAM to cytosine bases, primarily in CpG dinucleotides. The catalytic activity of DNMTs can be influenced by the SAM/SAH ratio, which fluctuates in response to changes in methionine metabolism and redox status [127]. Additionally, the ten-eleven translocation (TET) family of DNA demethylases, which catalyze the oxidation of 5-methylcytosine to initiate DNA demethylation, require 2-oxoglutarate, Fe(II), and O2, rendering them sensitive to redox conditions and metabolic status [127].
Sulfur-Mediated Persulfidation of Epigenetic Regulators
Emerging evidence indicates that reactive sulfur species can directly modulate epigenetic regulators through persulfidation. This redox modification can alter the catalytic activity, DNA-binding affinity, or protein stability of various epigenetic enzymes and transcription factors. For instance, persulfidation of histone demethylases like LSD1 could potentially regulate their activity by modifying critical cysteine residues near their active sites.
The interplay between sulfur redox biology and epigenetic regulation creates a sophisticated system for maintaining cellular memory of redox states. This integration allows cells to establish stable gene expression patterns in response to transient redox fluctuations, potentially contributing to metabolic programming, inflammatory memory, and adaptation to oxidative stress.
Experimental Approaches for Target Validation
Detection and Quantification of Reactive Sulfur Species
Accurate measurement of reactive sulfur species is fundamental to target validation. Current methodologies include:
Mass Spectrometry-Based Metabolomics: Liquid chromatography coupled with tandem mass spectrometry (LC-MS/MS) enables specific detection and quantification of low-molecular-weight supersulfides including cysteine persulfide (CysSSH), glutathione persulfide (GSSH), and their polysulfides [126]. The protocol involves:
- Rapid sample stabilization using specific blocking agents (e.g., iodoacetamide derivatives) to prevent artificial oxidation or degradation during processing
- Chromatographic separation using reverse-phase or HILIC columns optimized for sulfur compounds
- Multiple reaction monitoring (MRM) for sensitive and specific detection
- Isotope-labeled internal standards (e.g., 34S-cysteine) for precise quantification
Proteomic Mapping of Protein Persulfidation: The biotin switch technique, adapted from S-nitrosylation detection, allows proteome-wide profiling of persulfidated proteins [128]. The detailed protocol includes:
- Blocking free thiols with methyl methanethiosulfonate (MMTS) in HEPES-buffered saline
- Selective reduction of persulfides using specific reducing agents (e.g., DTT or tris(2-carboxyethyl)phosphine)
- Labeling of newly exposed thiols with biotin-HPDP
- Affinity purification using streptavidin beads
- On-bead tryptic digestion and LC-MS/MS analysis for protein identification
Fluorescent Probes for Cellular Imaging: Chemoselective fluorescent probes enable real-time monitoring of H2S and polysulfides in live cells [129]. These probes typically employ specific reactive groups (e.g., azide-based or electrophilic centers) that undergo fluorescence changes upon reaction with sulfur species. Critical validation steps include:
- Specificity testing against other reactive oxygen and nitrogen species
- Subcellular targeting sequences for compartment-specific monitoring
- Rationetric measurements to account for probe concentration variations
Profiling Epigenetic Modifications in Redox Context
Comprehensive epigenetic profiling under different redox conditions requires integrated approaches:
Chromatin Immunoprecipitation Sequencing (ChIP-seq): This technique allows genome-wide mapping of histone modifications and transcription factor binding. For redox studies, key considerations include:
- Rapid cross-linking to capture transient epigenetic states
- Antibody validation for specific histone modifications (H3K4me3, H3K27ac, H3K9me3, etc.)
- Integration with gene expression data from RNA-seq
- Specialized bioinformatics pipelines for differential epigenetic mark analysis
Oxidative Bisulfite Sequencing (oxBS-seq): This method provides quantitative mapping of 5-methylcytosine and 5-hydroxymethylcytosine at single-base resolution, offering unprecedented insight into the redox-sensitive DNA demethylation pathway [127]. The technique involves:
- Parallel bisulfite treatment with and without specific oxidation
- High-throughput sequencing of both libraries
- Computational subtraction to distinguish methylation from hydroxymethylation
CUT&Tag for Redox-Sensitive Epigenetic Profiling: Cleavage Under Targets and Tagmentation (CUT&Tag) offers a sensitive alternative to ChIP-seq with lower cell number requirements, enabling epigenetic profiling in primary cells under defined redox conditions [127].
Diagram 2: Integrated Workflow for Validating Sulfur Redox-Epigenetic Targets. Comprehensive target validation requires multidisciplinary approaches spanning analytical chemistry, epigenomics, and functional genetics.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Sulfur Redox and Epigenetic Studies
| Reagent Category | Specific Examples | Key Applications | Technical Considerations |
|---|---|---|---|
| Supersulfide Donors | GYY4137, DATS, AP39, SG1002 | Physiological RSS delivery; therapeutic potential assessment | Varying release kinetics; compartment-specific targeting |
| Enzyme Inhibitors | AOAA (CBS inhibitor), PAG (CSE inhibitor), ASP9531 (CARS inhibitor) | Pathway dissection; target validation | Specificity validation required; potential off-target effects |
| Epigenetic Chemical Probes | CPI-455 (KDM5 inhibitor), GSK-J4 (KDM6 inhibitor), JQ1 (BET inhibitor) | Epigenetic mechanism studies; therapeutic potential | Cell permeability; target engagement verification |
| Redox Biosensors | roGFP, HyPer, Mrx1-roGFP2 | Real-time redox monitoring in live cells | Calibration for specific compartments; photostability limitations |
| SAM/SAH Modulators | Cycloleucine, adenosine dialdehyde | Methylation potential manipulation | Global effects; pleiotropic consequences |
| Persulfidation Detection Reagents | SSP4, SSP2, biotin-HPDP, dimedone-based probes | Persulfidation mapping and quantification | Specificity validation against other oxidative modifications |
Therapeutic Implications and Future Directions
Inflammatory Diseases
The anti-inflammatory properties of supersulfides represent a promising therapeutic avenue. Supersulfides have been shown to inhibit inflammatory responses by interfering with the NF-κB signaling pathway, a central regulator of immune and inflammatory gene expression [126] [128]. Molecular studies demonstrate that supersulfides can attenuate NF-κB activation by modifying critical cysteine residues in signaling components, potentially through persulfidation. This mechanism disrupts the propagation of pro-inflammatory signals, reducing the production of cytokines, chemokines, and adhesion molecules that drive chronic inflammation.
Beyond NF-κB inhibition, supersulfides influence multiple aspects of the inflammatory cascade. They modulate NLRP3 inflammasome activation, regulate leukocyte adhesion and migration, and promote the resolution phase of inflammation through effects on specialized pro-resolving mediators [126]. The therapeutic potential of supersulfide donors is particularly promising for conditions characterized by chronic, non-resolving inflammation, such as rheumatoid arthritis, inflammatory bowel disease, and atherosclerosis. Current development efforts focus on optimizing donor molecules for tissue-specific delivery and controlled release kinetics to maximize therapeutic efficacy while minimizing off-target effects.
Neurological and Neuropsychiatric Disorders
Sulfur redox pathways play particularly important roles in the central nervous system, where they influence neuronal function, survival, and connectivity. Natural sulfur compounds demonstrate significant potential for managing mental disorders and neurological conditions through multiple mechanisms [130]. Sulfur-containing compounds such as sulforaphane, taurine, and glutathione have shown efficacy in modulating key pathological processes in neurodegenerative diseases:
- Alzheimer's disease: Sulforaphane administration (10-50 mg/kg daily) prevents memory deterioration by enhancing endogenous antioxidant enzymes and reducing neuroinflammation [130]
- Parkinson's disease: Sulfur compounds protect dopaminergic neurons through NRF2 pathway activation and reduction of α-synuclein aggregation
- Depression and anxiety: Sulfur metabolism modulation shows promise for addressing transsulfuration pathway disruptions observed in mood disorders
The therapeutic effects appear to stem from complementary mechanisms including enhanced antioxidant defenses, reduced neuroinflammation, improved endothelial function and cerebral blood flow, and protection against excitotoxicity [130]. Clinical translation requires addressing challenges related to blood-brain barrier penetration, compartment-specific delivery, and long-term safety profiles.
Cancer and Metabolic Diseases
The intersection of sulfur redox biology and epigenetic regulation offers unique opportunities for cancer therapy. Cancer cells frequently exhibit dysregulated sulfur metabolism, with altered expression of CBS, CSE, and other sulfur-metabolizing enzymes [129]. These alterations support redox adaptation, nucleotide synthesis, and epigenetic reprogramming necessary for tumor growth and survival. Strategic inhibition of specific sulfur metabolic enzymes may selectively target cancer cells while sparing normal tissues.
The contextual functionality of sulfur compounds in cancer presents both challenges and opportunities. In tumors such as breast, colorectal, and prostate cancers, H2S may promote tumor growth through pro-angiogenic and anti-apoptotic effects [129]. Conversely, in other contexts, H2S may exert anti-tumor properties by inducing apoptosis and inhibiting proliferation [129]. This dual nature underscores the importance of careful context-specific therapeutic development.
Cardiovascular Diseases
Sulfur species, particularly H2S, demonstrate robust cardiovascular protective effects. These benefits include promotion of endothelial cell function, inhibition of vascular inflammation, vasodilation, and protection against ischemia-reperfusion injury [128] [129]. The cardiovascular system exhibits particular sensitivity to sulfur-based signaling, making it an attractive target for therapeutic intervention. Clinical development of sulfur-based donors for conditions such as myocardial infarction, atherosclerosis, and hypertension is advancing, with several compounds in preclinical and early clinical development.
The integration of sulfur redox biochemistry with epigenetic mechanisms represents a paradigm shift in our understanding of cellular regulation. Supersulfides and related reactive sulfur species function as specialized signaling molecules that transduce redox information into durable changes in gene expression through targeted persulfidation and modulation of epigenetic machinery. The validation of novel targets at this interface provides exciting opportunities for therapeutic intervention in inflammation, neurological disorders, cancer, and metabolic diseases.
Future research directions should focus on developing more specific tools for manipulating individual sulfur species, mapping the precise cysteine residues subject to redox regulation on epigenetic enzymes, and understanding the compartment-specific dynamics of these processes in different disease contexts. As our technical capabilities for monitoring and manipulating these pathways continue to advance, so too will our ability to develop targeted therapies that restore redox and epigenetic balance in disease states. The emerging recognition of sulfur species as central players in the redox-epigenetic axis promises to open new frontiers in molecular medicine and therapeutic development.
Conclusion
The intricate interplay between redox signaling and inflammation represents a fundamental pathway in disease pathogenesis that extends beyond simplistic oxidative damage models. The field is transitioning from non-specific antioxidant approaches to precision targeting of specific redox-sensitive nodes, with Nrf2 activation and NOX inhibition showing particular promise. Future research must prioritize understanding the spatiotemporal dynamics of redox signaling, developing validated biomarker panels for patient stratification, and designing clinical trials that account for the bidirectional nature of redox balance. Success in this arena will require integrated multidisciplinary approaches that leverage genomics, proteomics, and metabolomics to decode individual redox profiles, ultimately enabling personalized therapies that restore physiological redox signaling while preventing pathological imbalance across diverse inflammatory diseases.
References
- 1. Redox regulation: mechanisms, biology and therapeutic ... [https://www.nature.com/articles/s41392-024-02095-6]
- 2. Redox homeostasis: The Golden Mean of healthy living [https://www.sciencedirect.com/science/article/pii/S2213231716300106]
- 3. Dysregulated Redox Signaling and Its Impact on ... [https://www.mdpi.com/2076-3921/14/11/1278]
- 4. Redox Imbalance in Inflammation: The Interplay of Oxidative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12189482/]
- 5. Quantitative Redox Biology: An approach to understanding ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3661692/]
- 6. Reductive stress: The key pathway in metabolic disorders ... [https://www.sciencedirect.com/science/article/pii/S2090123225000311]
- 7. Reductive stress: The key pathway in metabolic disorders ... [https://pubmed.ncbi.nlm.nih.gov/39805424/]
- 8. Reactive Oxygen Species: Drivers of Physiological and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7719303/]
- 9. Free radicals and their impact on health and antioxidant ... [https://www.nature.com/articles/s41420-024-02278-8]
- 10. The Key Roles of ROS and RNS as a Signaling Molecule ... [https://www.mdpi.com/2076-3921/12/2/268]
- 11. Reactive Oxygen Species in Inflammation and Tissue Injury [https://pmc.ncbi.nlm.nih.gov/articles/PMC3929010/]
- 12. sciencedirect.com/topics/veterinary-science-and-veterinary-medicine... [https://www.sciencedirect.com/topics/veterinary-science-and-veterinary-medicine/oxidative-stress-biomarkers]
- 13. Frontiers | Oxidative in the brain–lung crosstalk: cellular and... stress [https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2024.1389454/full]
- 14. : Oxidative and novel therapeutic stress - pmc biomarkers pathways [https://pmc.ncbi.nlm.nih.gov/articles/PMC2827206/]
- 15. Redox imbalance and oxidative stress in cardiovascular ... [https://pubmed.ncbi.nlm.nih.gov/41142692/]
- 16. Redox imbalance and oxidative stress in cardiovascular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12550685/]
- 17. Role of Mitochondria in the Redox Signaling Network and Its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7538663/]
- 18. REDOX Imbalance and Oxidative Stress in the ... [https://www.mdpi.com/2073-4409/14/8/613]
- 19. Redox regulation of Nox proteins - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3001134/]
- 20. Architecture of the NADPH oxidase family of enzymes [https://www.sciencedirect.com/science/article/pii/S2213231722000702]
- 21. Endoplasmic Reticulum Stress and Oxidative Stress in Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4076992/]
- 22. The aftermath of the interplay between the endoplasmic ... [https://www.nature.com/articles/s12276-021-00560-8]
- 23. ROS Function in Redox Signaling and Oxidative Stress [https://www.sciencedirect.com/science/article/pii/S0960982214003261]
- 24. ROS Function in Redox Signaling and Oxidative Stress - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4055301/]
- 25. Exploring the Interplay of Antioxidants, Inflammation, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12469104/]
- 26. Dissecting the Crosstalk Between Nrf2 and NF-κB Response ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8847224/]
- 27. The Crosstalk between Nrf2 and Inflammasomes [https://www.mdpi.com/1422-0067/19/2/562]
- 28. An overview of current research on the modulation ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1634132/full]
- 29. Review Nrf2 signaling pathway: Pivotal roles in inflammation [https://www.sciencedirect.com/science/article/pii/S0925443916302861]
- 30. Redox Signalling - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/redox-signalling]
- 31. ROS signaling in innate immunity via oxidative protein ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10954773/]
- 32. Neutrophil extracellular traps in homeostasis and disease [https://www.nature.com/articles/s41392-024-01933-x]
- 33. An overview of mechanisms of redox signaling - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4048798/]
- 34. Reactive Oxygen Species in Macrophages: Sources and ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.734229/full]
- 35. Macrophages and neutrophils are necessary for ER stress ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9444341/]
- 36. Redox signaling in innate immunity and inflammation [https://www.sciencedirect.com/science/article/pii/S0891584925007555]
- 37. Linking oxidative stress biomarkers to disease progression ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1611842/full]
- 38. Therapeutic Strategies Targeting Oxidative Stress and ... [https://www.mdpi.com/2673-6411/5/4/35]
- 39. From molecular mechanism to plant intervention [https://pmc.ncbi.nlm.nih.gov/articles/PMC12283317/]
- 40. From molecular mechanism to plant intervention [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1634580/full]
- 41. Redox Imbalance in Inflammation: The Interplay of ... [https://www.mdpi.com/2076-3921/14/6/656]
- 42. Comparative Analysis of Redox Homeostasis Biomarkers ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10604746/]
- 43. Oxidative stress-related biomarkers as promising indicators of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11490685/]
- 44. Targeting Redox Signaling Through Exosomal MicroRNA [https://pmc.ncbi.nlm.nih.gov/articles/PMC12108341/]
- 45. Diagnostic and pathologic miRNA signatures for reductive ... [https://www.sciencedirect.com/science/article/pii/S2213231725000382]
- 46. †KEAP protein–protein interaction inhibitors: Design... 1 NRF 2 [https://pmc.ncbi.nlm.nih.gov/articles/PMC10087726/]
- 47. The Anti-Inflammatory and Anti-Oxidant Mechanisms of the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6538222/]
- 48. The NRF2/KEAP1 Axis in the Regulation of Tumor Metabolism [https://pmc.ncbi.nlm.nih.gov/articles/PMC7277620/]
- 49. The Nrf2 antioxidant defense system in intervertebral disc ... [https://www.nature.com/articles/s12276-022-00829-6]
- 50. Regulation of immunomodulatory networks by Nrf2-activation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10877431/]
- 51. Targeting the Keap / 1 in cancer: Nrf mechanisms and... 2 axis molecular [https://link.springer.com/article/10.1007/s10637-025-01578-9]
- 52. Frontiers | Challenges and Limitations of Targeting the... [https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2021.673205/full]
- 53. AEOL- induced and DWORF overexpression mitigate... NRF 2 activation [https://molmed.biomedcentral.com/articles/10.1186/s10020-025-01242-1]
- 54. NOX Family: Regulators of Reactive Oxygen Species Balance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12017260/]
- 55. Coordinated Contribution of NADPH Oxidase [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2021.670076/full]
- 56. Cross-Talk between NADPH Oxidase and Mitochondria: Role ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7466096/]
- 57. Link between Mitochondria and NADPH Oxidase 1 ... [https://www.sciencedirect.com/science/article/pii/S0021925820681777]
- 58. Oxidative stress and inflammation in the pathogenesis of ... [https://www.sciencedirect.com/science/article/pii/S2211383524004040]
- 59. Protein redox chemistry: post-translational cysteine ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2014.00224/full]
- 60. Cysteines as Redox Molecular Switches and Targets of ... [https://www.frontiersin.org/journals/molecular-neuroscience/articles/10.3389/fnmol.2017.00167/full]
- 61. Cysteine-Based Redox Switches in Enzymes - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3064533/]
- 62. Cysteine Oxidative Post-translational Modifications: Emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4340704/]
- 63. Redox signaling in innate immunity and inflammation [https://pubmed.ncbi.nlm.nih.gov/40484207/]
- 64. Exploring antiviral and anti-inflammatory effects of thiol ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9448286/]
- 65. Thiol-Based Drugs in Pulmonary Medicine [https://www.sciencedirect.com/science/article/abs/pii/S0165614719300926]
- 66. Cysteine Thiol-Based Oxidative Post-Translational ... [https://www.mdpi.com/2073-4395/14/12/2757]
- 67. Integrated anti-aging strategy could reduce neurodegeneration [https://www.news-medical.net/news/20250311/Integrated-anti-aging-strategy-could-reduce-neurodegeneration.aspx]
- 68. Cover Story | Transformative Trends in CV Medicine For 2025 [https://www.acc.org/latest-in-cardiology/articles/2025/01/01/42/cover-story-transformative-trends-in-cv-medicine-for-2025]
- 69. Frontiers | From imaging to intervention: emerging potential of PET... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1637243/full]
- 70. Improving the management of systemic metabolic disorders [https://eas-society.org/2025/improving-the-management-of-systemic-metabolic-disorders-a-clinical-staging-system-from-the-european-atherosclerosis-society/]
- 71. New potential therapeutic targets of metabolic disorder- ... [https://pubmed.ncbi.nlm.nih.gov/41139023/]
- 72. Innovative Strategies for Diabetes and Metabolic Disorders [https://www.explorationpub.com/Journals/eemd/Special_Issues/388]
- 73. Precision Redox: The Key for Antioxidant Pharmacology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8080931/]
- 74. The Redox Revolution in Brain Medicine [https://www.mdpi.com/1422-0067/26/15/7498]
- 75. Mass Spectrometry in Advancement of Redox Precision ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9236553/]
- 76. Oxidative Stress Fundamentals [https://www.mdpi.com/2076-3417/15/18/10191]
- 77. More than Just Antioxidants: Redox-Active Components ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9774234/]
- 78. Antioxidants and Reactive Oxygen Species [https://www.mdpi.com/1422-0067/26/15/7520]
- 79. Several lines of antioxidant defense against oxidative stress [https://link.springer.com/article/10.1007/s00204-024-03696-4]
- 80. Single-cell signaling network profiling during redox stress ... [https://www.nature.com/articles/s41467-025-60727-z]
- 81. The Future of Anti- Inflammatory Medicine: Can Redox ... Signaling [https://www.linkedin.com/pulse/future-anti-inflammatory-medicine-can-redox-signaling-harding-jb3ze]
- 82. Unraveling the interplay between sleep, redox metabolism, and aging... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12133771/]
- 83. Linking oxidative stress biomarkers to disease progression ... [https://pubmed.ncbi.nlm.nih.gov/40492113/]
- 84. Applications of Antioxidant Nanoparticles in Immune-Mediated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12466755/]
- 85. Regulation of oxidative stress and inflammation caused by ... [https://cancer-nano.biomedcentral.com/articles/10.1186/s12645-025-00342-1]
- 86. Current advance of nanotechnology in diagnosis and ... [https://www.nature.com/articles/s41392-024-01889-y]
- 87. Advanced Nanomedicines for Treating Refractory ... [https://link.springer.com/article/10.1007/s40820-025-01829-7]
- 88. Targeting the redox-programmed cell death axis in breast ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12500867/]
- 89. Nanoparticle-based drug delivery systems targeting ... [https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2025.1657300/full]
- 90. Redox signaling at the crossroads of human health and disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC8971743/]
- 91. Redox signaling and homeostasis [https://www.sciopen.com/article/10.26599/OSHM.2025.9610003]
- 92. Compensatory combination of mTOR and TrxR inhibitors to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7977446/]
- 93. Redox Signaling, Vascular Function, and Hypertension - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2828811/]
- 94. The Redox Revolution in Brain Medicine: Targeting Oxidative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12347410/]
- 95. Decoding the Redox Code of Ischemic Stroke ... [https://www.mdpi.com/1422-0067/26/22/10835]
- 96. regulation: mechanisms, biology and Redox targets in... therapeutic [https://pmc.ncbi.nlm.nih.gov/articles/PMC11885647/]
- 97. Editorial: Cellular and molecular mechanisms in metabolic ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1580553/full]
- 98. Frontiers | Redox reactions in chronic pain: mechanisms and relevance... [https://www.frontiersin.org/journals/pain-research/articles/10.3389/fpain.2025.1593908/full]
- 99. Regulation of immunomodulatory networks by Nrf2-activation... | CoLab [https://colab.ws/articles/10.1016/j.redox.2024.103077]
- 100. Biomarkers of Oxidative Stress, Systemic Inflammation and ... [https://www.mdpi.com/2077-0383/14/7/2360]
- 101. Quinic acid alleviates inflammatory responses and ... [https://pubmed.ncbi.nlm.nih.gov/41044296]
- 102. The Redox Paradox: Cancer's Double-Edged Sword for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12561025/]
- 103. Delivery strategies to improve the pharmacological efficacy of ... [https://pubs.rsc.org/en/content/articlehtml/2025/md/d5md00571j]
- 104. Harnessing the interaction between redox signaling and ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1639772/full]
- 105. Frontiers | Redox homeostasis and inflammation in fibroblasts of... [https://www.frontiersin.org/journals/molecular-neuroscience/articles/10.3389/fnmol.2025.1571402/full]
- 106. Redox modulator iron complexes trigger intrinsic apoptosis ... [https://www.sciencedirect.com/science/article/pii/S2589004224011210]
- 107. Altered NRF2 signalling in systemic redox imbalance [https://pmc.ncbi.nlm.nih.gov/articles/PMC12554130/]
- 108. Analytical methods for 3-nitrotyrosine as a marker of ... [https://pubmed.ncbi.nlm.nih.gov/10100488/]
- 109. Rapid Quantitative Analysis of 8-iso-PGF2α Using Liquid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2909638/]
- 110. Reinterpreting the Best Biomarker of Oxidative Stress [https://pmc.ncbi.nlm.nih.gov/articles/PMC4441846/]
- 111. 4-Hydroxy-2-nonenal, a lipid peroxidation product, as a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8260649/]
- 112. A sensitive LC-MS/MS method for the quantification of ... [https://www.sciencedirect.com/science/article/abs/pii/S0009898116302790]
- 113. Analysis of 19 urinary biomarkers of oxidative stress ... [https://link.springer.com/article/10.1007/s00216-021-03844-0]
- 114. Antioxidant and oxidative enzymes, genetic variants ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1700263/full]
- 115. Activators and Inhibitors of NRF2: A Review of Their Potential ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6664516/]
- 116. Nrf2 and Oxidative Stress: A General Overview of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9774434/]
- 117. Recent Advances in Understanding Nrf2 Agonism and Its ... [https://www.mdpi.com/1422-0067/23/5/2846]
- 118. An Overview of Nrf2 Signaling Pathway and Its Role in ... [https://www.mdpi.com/1420-3049/25/22/5474]
- 119. NOX1-mediated oxidative stress induces chondrocyte ... [https://www.nature.com/articles/s41598-024-70991-6]
- 120. An update of Nrf2 activators and inhibitors in cancer ... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-022-00906-3]
- 121. Comprehensive review of macrophage models: primary ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1640935/full]
- 122. Redox regulation of macrophages - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11026845/]
- 123. miR-210 promotes the anti-inflammatory phenotype and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12361208/]
- 124. Harnessing the interaction between redox signaling and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12283637/]
- 125. Cancer mortality and senescence: Is redox therapy an option? [https://genesdev.cshlp.org/content/39/15-16/914.full]
- 126. Supersulfide donors and their therapeutic targets in ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1581385/full]
- 127. The Redox Basis of Epigenetic Modifications - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC3118659/]
- 128. Natural Sulfur Compounds in Mineral Waters - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12610360/]
- 129. Sulfide regulation and catabolism in health and disease [https://www.nature.com/articles/s41392-025-02231-w]
- 130. Natural sulfur compounds in mental health and ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1534000/full]