Redox Homeodynamics vs. Homeostasis: A Paradigm Shift for Precision Medicine and Drug Discovery
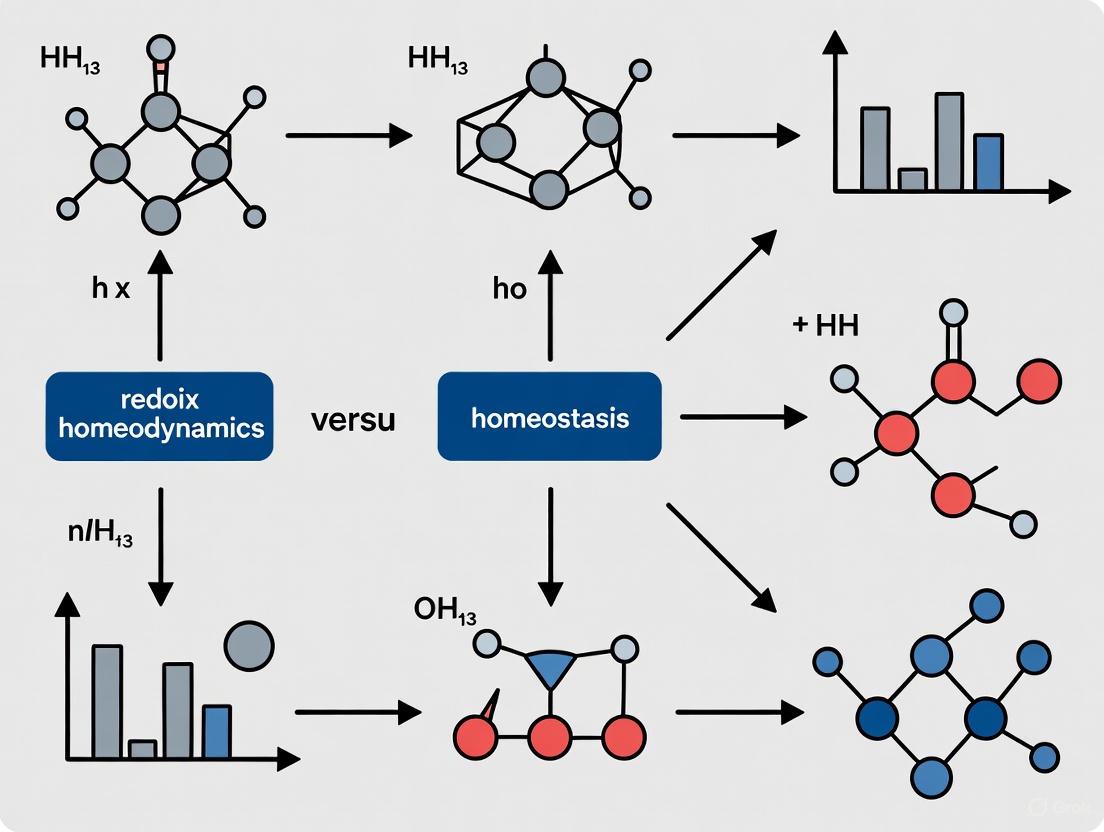
This article explores the critical paradigm shift from the static concept of redox homeostasis to the dynamic model of redox homeodynamics.
Redox Homeodynamics vs. Homeostasis: A Paradigm Shift for Precision Medicine and Drug Discovery
Abstract
This article explores the critical paradigm shift from the static concept of redox homeostasis to the dynamic model of redox homeodynamics. Tailored for researchers and drug development professionals, it delves into the foundational principles of this continuous, adaptive process and its disruption in disease states. The content covers advanced methodologies for quantifying redox states, analyzes the pitfalls of broad-spectrum antioxidants, and proposes strategies for targeted therapeutic intervention. Finally, it validates the homeodynamics framework through its application in precision medicine, offering a comparative analysis of its advantages over the traditional homeostasis model for developing novel, context-specific treatments for cancer, cardiovascular, and neurodegenerative diseases.
From Static Balance to Dynamic Control: Deconstructing Redox Homeodynamics
Within redox biology, a paradigm shift is occurring from a classical view of static maintenance of balance toward a modern understanding of continuous adaptation. This whitepaper delineates the conceptual and operational distinctions between redox homeostasis, defined as the dynamic equilibrium maintaining reducing and oxidizing (redox) reactions within a narrow, optimal range, and redox homeodynamics, which describes the continuous adaptive process that transiently expands or contracts the homeostatic range in response to sub-toxic signaling events. For researchers and drug development professionals, appreciating this distinction is critical for designing targeted therapeutic strategies that either maintain equilibrium or harness adaptive responses.
The concept of homeostasis, originating from Claude Bernard's "milieu intérieur" and later coined by Walter Cannon, has long been a cornerstone of physiology, describing the maintenance of nearly constant internal conditions [1] [2]. In the context of redox biology, redox homeostasis has been traditionally understood as the dynamic balance between pro-oxidants (electrophiles) and antioxidants (nucleophiles) within the cell [3] [4]. This balance is crucial for normal cellular function, as reactive oxygen and nitrogen species (ROS/RNS) are not merely harmful byproducts but also essential signaling molecules [5] [4].
However, emerging research underscores that biological systems do not merely defend a fixed setpoint. Instead, they demonstrate homeodynamics—a continuous adaptive capacity that allows for transient changes in the homeostatic range itself. This adaptive process, sometimes termed Adaptive Homeostasis, enables organisms to adjust their functional stability in response to mild, non-damaging stimuli, such as dietary components, exercise, or low levels of chemical agents [2]. This whitepaper explores the technical definitions, mechanisms, and experimental distinctions between these two interconnected concepts, providing a framework for their application in biomedical research and therapeutic development.
Redox Homeostasis: A Dynamic Equilibrium
Core Definition and Characteristics
Redox Homeostasis is the dynamic equilibrium process that maintains the balance between reducing and oxidizing reactions within a cell, preserving the optimum redox steady state [5] [4]. It is a highly responsive system that continuously senses and realigns metabolic activities to restore redox balance following perturbations. The key characteristics of the redox homeostasis model are:
- Dynamic Equilibrium: The system maintains a "nucleophilic tone" through continuous feedback mechanisms, not a static, fixed state [3] [4].
- Narrow Optimal Range: The goal of the system is to confine redox potentials to a strict, favorable range for cellular function [1].
- Reactive Restoration: The system operates primarily through feedback loops that react to changes and disturbances, forcing the variable back into its normal range [1].
Molecular Mechanisms and Signaling Pathways
The maintenance of redox homeostasis involves a complex network of enzymatic and non-enzymatic systems. Reactive Oxygen Species (ROS), such as superoxide radical (●O2⁻) and hydrogen peroxide (H₂O₂), are generated as byproducts of metabolism and by dedicated enzymes like NADPH oxidases [5]. At controlled levels, these molecules act as crucial secondary messengers in redox signaling.
A central regulator is the Keap1-Nrf2-ARE pathway, the master regulator of the cellular antioxidant response [3] [5] [4]. Under basal conditions, the cytosolic protein Keap1 targets the transcription factor Nrf2 for proteasomal degradation. Upon an increase in oxidative or electrophilic stress, this degradation is halted, allowing Nrf2 to translocate to the nucleus, dimerize with small Maf proteins, and bind to the Antioxidant Response Element (ARE), activating the transcription of a battery of cytoprotective genes. These genes include NAD(P)H:quinone oxidoreductase 1 (NQO1), heme oxygenase-1 (HO-1), and enzymes involved in glutathione synthesis [5] [4].
The following diagram illustrates the core Keap1-Nrf2 signaling pathway that maintains redox homeostasis:
Redox Signaling Mechanisms: Redox signaling occurs largely through reversible redox post-translational modifications (rPTMs) of specific cysteine thiolates (-SH) in target proteins [5] [4]. Oxidation by H₂O₂ can form sulfenic acid (-SOH), which can lead to disulfide bond (-S-S-) formation. These modifications are readily reversed by disulfide reductase enzymes like thioredoxin (Trx) and glutaredoxin (Grx), ensuring the transient nature of the signal. This reversible oxidation can regulate the activity of key signaling proteins, such as inhibiting Protein Tyrosine Phosphatases (PTPs), thereby potentiating kinase signaling [5].
Redox Homeodynamics: A Continuous Adaptive Process
Core Definition and Characteristics
Redox Homeodynamics (or Adaptive Homeostasis) is the transient expansion or contraction of the homeostatic range in response to exposure to sub-toxic, non-damaging, signaling molecules or events, or the removal of such molecules or events [2]. This concept moves beyond maintaining a fixed range to encompass the biological capacity for adaptation. Its key characteristics are:
- Adaptive Capacity: The system's setpoint or range of "normal" capacity can be adjusted based on environmental cues or previous exposures [2].
- Transient Nature: The expansion or contraction of the homeostatic range is not permanent but is calibrated to the duration and intensity of the stimulus.
- Anticipatory Potential: Unlike classic reactive homeostasis, homeodynamics can involve feedforward mechanisms that pre-emptively adjust system capacity in anticipation of a challenge [1] [2].
This concept is distinct from related terms like allostasis (maintaining stability through change) and hormesis (a biphasic dose response to toxins), though there is some conceptual overlap. Adaptive homeostasis specifically refers to responses to mild, non-damaging stimuli and involves changes to the normal capacity of systems [2].
Molecular Basis of Adaptation
The mechanisms underlying redox homeodynamics often involve the same molecular players as homeostasis, such as the Nrf2 pathway, but their activity is modulated to reset the system's operational range. For instance, a mild electrophilic stress might not only activate Nrf2 to restore the immediate redox balance but also prime the system for a subsequent challenge by maintaining a slightly elevated level of antioxidant enzymes, thereby transiently expanding the homeostatic range [3] [2].
The following diagram contrasts the classical homeostatic response with the adaptive homeodynamic response:
Para-hormesis: This is a key concept in homeodynamics, where certain natural dietary compounds (phytochemicals) can activate stress-response pathways like Nrf2 without causing significant damage, thereby mimicking the effect of endogenously produced electrophiles and contributing to long-term health by favoring the maintenance of an adapted homeostatic state [3] [4].
Experimental Distinction: Methodologies and Assessment
Distinguishing between homeostasis and homeodynamics in a research setting requires carefully designed experiments that measure not only the immediate response to a stressor but also the kinetics of recovery and the subsequent capacity of the system to handle a second challenge.
Quantitative Assessment of Redox States
A variety of techniques are employed to quantify the redox state of cells and tissues, providing data to differentiate static imbalance from dynamic adaptation.
Table 1: Key Analytical Methods for Assessing Redox Homeostasis and Homeodynamics
| Method | Measured Parameter | Technical Insight | Application in Concept Discrimination |
|---|---|---|---|
| Redox-Sensitive GFP (roGFP) | Dynamic, real-time changes in glutathione redox potential (EGSSG/2GSH) [5]. | Genetically encoded sensor allowing compartment-specific monitoring in live cells. | Tracks real-time recovery kinetics after a perturbation; slower recovery suggests impaired homeostasis. |
| LC-MS/MS for Oxidized Lipids | Levels of specific lipid peroxidation products (e.g., 4-hydroxynonenal (HNE), malondialdehyde (MDA)) [6] [4]. | Provides a sensitive and specific measure of oxidative damage to membranes. | High sustained levels indicate failed homeostasis; a primed system in homeodynamics may show a blunted response to a second, similar challenge. |
| Western Blot for rPTMs | Detection of specific redox post-translational modifications (e.g., cysteine sulfenylation, nitrosylation) [5] [4]. | Uses specific antibodies to detect modified proteins; can assess signaling activity. | Identifies activation of specific pathways (e.g., Nrf2) and their return to baseline, differentiating transient signaling (homeodynamics) from chronic activation (stress). |
| qPCR/Western for Nrf2 Target Genes | mRNA or protein levels of HO-1, NQO1, GSTs, etc. [5] [4]. | Measures the transcriptional output of a key redox regulatory pathway. | A transient increase indicates successful adaptation (homeodynamics), while a persistent elevation may indicate chronic oxidative stress overwhelming homeostasis. |
Protocol for Differentiating Homeostasis from Homeodynamics
The following experimental workflow is designed to probe the adaptive capacity of a biological system, thereby distinguishing a homeodynamic response.
Protocol Title: Sequential Challenge Assay to Quantify Adaptive Redox Homeodynamics.
Objective: To determine if a mild, sub-toxic preconditioning stimulus expands the homeostatic range and confers enhanced protection against a subsequent toxic challenge.
Cell Culture & Preconditioning:
- Use a relevant cell line (e.g., primary hepatocytes, neuronal cells).
- Test Group: Treat with a mild, sub-toxic dose of a redox-active compound (e.g., 10-50 µM sulforaphane, a known Nrf2 inducer) for 6-12 hours.
- Control Group: Treat with vehicle only (e.g., DMSO < 0.1%).
- Washout: Remove the medium, wash cells with PBS, and add fresh compound-free medium for a 6-24 hour "recovery" period. This step is crucial for observing adaptation beyond the immediate stress response.
Toxic Challenge:
- Expose both Preconditioned and Control cells to a standardized oxidative insult (e.g., 200-500 µM H₂O₂ or 50-100 µM tert-butyl hydroperoxide (tBHP)) for a defined period (e.g., 2-6 hours).
Endpoint Analysis (Post-Challenge):
- Cell Viability: Measure using MTT or Calcein-AM assay. A significantly higher viability in the Preconditioned group indicates successful adaptation.
- Redox Status: Quantify using roGFP imaging or by measuring the GSH/GSSG ratio via enzymatic recycling assays. A more reduced state in Preconditioned cells suggests an enhanced antioxidant capacity.
- Molecular Markers: Analyze by qPCR/Western blot for Nrf2 target genes (HO-1, NQO1). The Preconditioned group may show a more rapid or robust induction of these genes upon challenge.
Interpretation: A system operating only with classical homeostasis will return to its original baseline after the preconditioning washout and will be equally susceptible to the toxic challenge as the control. A system demonstrating homeodynamics will retain a "memory" of the preconditioning, evident as an expanded homeostatic range that provides greater resilience to the subsequent challenge.
The following diagram outlines this experimental workflow:
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Redox Homeostasis and Homeodynamics Research
| Reagent / Assay Kit | Primary Function | Application in Redox Research |
|---|---|---|
| CellROX / MitoSOX Probes | Fluorescent detection of general cellular and mitochondrial superoxide, respectively. | Qualitative/quantitative assessment of ROS production during stress and adaptation. |
| GSH/GSSG Ratio Detection Kit | Enzymatic quantification of reduced (GSH) and oxidized (GSSG) glutathione. | A cornerstone assay for defining the central redox couple and overall cellular redox state. |
| roGFP Plasmids | Genetically encoded biosensor for real-time, compartment-specific redox monitoring. | Gold standard for dynamic, non-disruptive tracking of redox potential fluctuations. |
| Sulforaphane | Natural compound that acts as a potent Nrf2 activator by modifying Keap1 cysteine residues. | Standard tool for preconditioning experiments to induce an adaptive homeodynamic response. |
| Anti-Nrf2 & Anti-Keap1 Antibodies | Protein detection and localization via Western Blot, Immunoprecipitation, or Immunofluorescence. | Essential for monitoring the status and activity of the key Nrf2-Keap1 signaling axis. |
| N-Acetylcysteine (NAC) | Precursor for glutathione synthesis and a direct antioxidant/redox modulator. | Commonly used to test the necessity of redox changes in a observed phenotype or signaling event. |
| Recombinant Thioredoxin (Trx) | Key disulfide reductase enzyme that reverses oxidative protein modifications. | Used to demonstrate the reversibility of redox signaling and its functional consequences. |
The distinction between redox homeostasis and redox homeodynamics is more than semantic; it represents a fundamental shift in how researchers conceptualize the interaction between organisms and their environment. The classical model of homeostasis describes the elegant machinery that maintains stability, while the homeodynamics model explains the plasticity that confers resilience and facilitates survival in a fluctuating environment.
For drug development, this distinction is critically important. Therapeutic strategies aimed at crudely suppressing all ROS with high-dose antioxidants have largely failed in clinical trials, and in some cases, have been harmful [6] [5]. This failure can be understood through the lens of homeodynamics: such approaches likely disrupt essential redox signaling and impair the body's innate adaptive responses. The future lies in precision redox medicine, which involves:
- Modulation, Not Blunt Inhibition: Developing therapeutics that fine-tune redox signaling rather than ablating it [6].
- Context-Specific Strategies: Applying pro-oxidant therapies in contexts like cancer, where disrupting the heightened redox homeostasis of tumor cells is desirable, and using targeted Nrf2 activators for chronic degenerative diseases [6] [7].
- Temporal Control: Timing interventions to work with the body's natural adaptive rhythms, potentially using preconditioning (homeodynamic) strategies to protect against anticipated insults, such as the cardiotoxic effects of chemotherapy [6].
Ultimately, embracing the concept of redox homeodynamics will enable scientists and clinicians to develop more sophisticated and effective interventions that support the body's inherent capacity for adaptive, healthy living.
Redox signaling represents a fundamental regulatory mechanism in cellular biology, governing processes from proliferation and differentiation to programmed cell death. This whitepaper examines the core molecular players in redox signaling—reactive oxygen species (ROS), reactive nitrogen species (RNS), glutathione (GSH), thioredoxin (Trx), and NADPH systems—through the conceptual framework of redox homeodynamics rather than static homeostasis. Unlike the traditional homeostasis concept which implies a stable equilibrium, homeodynamics better reflects the dynamic, adaptive nature of redox regulation where systems maintain functional integrity through continuous flux and interaction between oxidizing and reducing species [8] [5]. This dynamic interplay enables precise spatiotemporal control of cellular signaling networks, with disruption leading to pathological conditions including neurodegenerative diseases, cardiovascular disorders, and cancer.
The concept of redox homeodynamics provides a transformative perspective on cellular redox regulation. While homeostasis suggests a return to a fixed set point, homeodynamics acknowledges that living systems maintain stability through continuous activity and adaptation to internal and external challenges [5]. This paradigm is particularly apt for redox biology, where the balance between oxidants and antioxidants is not static but rather a highly responsive, dynamic system that senses changes in redox status and realigns metabolic activities to restore functional balance.
In practical terms, redox homeodynamics involves constant surveillance and adjustment through interconnected systems including glutathione, thioredoxin, NADPH-regenerating systems, and their associated enzymes [5]. Under physiological conditions, nonradical ROS such as hydrogen peroxide (H₂O₂) function as crucial second messengers to modulate redox signaling by orchestrating multiple redox sensors at concentrations ranging from 1-100 nM [8]. However, when redox homeodynamics is disrupted, excessive ROS accumulation—termed oxidative stress—leads to biomolecule damage and subsequent disease pathogenesis [8].
Reactive Oxygen and Nitrogen Species: The Signaling Messengers
ROS Diversity and Characteristics
Reactive oxygen species are not a monolithic entity but rather a diverse group of molecules with distinct chemical properties, reactivities, and biological impacts [9]. The major ROS species include:
Table 1: Key Reactive Oxygen Species in Redox Signaling
| ROS Species | Chemical Formula | Production Sources | Reactivity & Characteristics | Primary Signaling Roles |
|---|---|---|---|---|
| Superoxide anion | O₂•⁻ | Mitochondrial ETC, NOX enzymes, P450 systems | Moderate reactivity; limited membrane permeability; precursor to other ROS | Limited direct signaling; mainly precursor for H₂O₂ and ONOO⁻ |
| Hydrogen peroxide | H₂O₂ | SOD conversion of O₂•⁻, NOX4, DUOX | Moderate reactivity; membrane-diffusible; specific target oxidation | Major redox messenger; oxidizes protein cysteine residues |
| Hydroxyl radical | •OH | Fenton reaction, water radiolysis | Extremely reactive; non-specific; minimal diffusion distance | Not a signaling molecule; causes oxidative damage |
| Singlet oxygen | ¹O₂ | Photosensitization reactions | Highly reactive with organic compounds | Stress signaling; programmed cell death |
The specificity of redox signaling is largely determined by the chemical properties of each ROS. H₂O₂ has emerged as a primary redox signaling mediator due to its relative stability, ability to diffuse across membranes, and selective reactivity with specific protein cysteine residues [8] [9]. In contrast, the hydroxyl radical (•OH) is extremely reactive and immediately removes electrons from any molecule in its path, making it unsuitable for specific signaling but highly destructive to cellular components [10].
Reactive Nitrogen Species
Reactive nitrogen species, particularly nitric oxide (NO•) and its derivatives, represent another crucial class of redox signaling mediators. Peroxynitrite (ONOO⁻), formed from the diffusion-limited reaction between superoxide and nitric oxide, is a strong two-electron oxidant that can modify protein tyrosines to form nitrotyrosines, affecting protein function [10]. The biological activity of RNS depends on the local concentration of its precursor molecules and the specific microenvironment in which it is generated.
The Major Redox Buffering Systems
Glutathione System
Glutathione (GSH) is the most abundant non-protein thiol in cells, functioning as a primary redox buffer, antioxidant, and enzyme cofactor against oxidative stress [11]. This tripeptide (γ-glutamylcysteinylglycine) is synthesized intracellularly via two ATP-dependent reactions catalyzed by γ-glutamylcysteine ligase (GCL) and glutathione synthetase (GS).
The glutathione system maintains redox homeodynamics through several mechanisms:
- Redox Buffering: The GSH/GSSG couple maintains intracellular redox status with a ratio typically >100:1 under physiological conditions, decreasing to 10:1 or less under oxidative stress [11].
- Enzyme Cofactor: GSH serves as an essential cofactor for glutathione peroxidases (GPx) which reduce H₂O₂ and lipid hydroperoxides to water and corresponding alcohols.
- Protein Modification: GSH participates in S-glutathionylation, a reversible post-translational modification that regulates protein function and protects cysteine residues from irreversible oxidation [11].
The brain is particularly vulnerable to GSH depletion due to its high oxygen consumption, abundance of unsaturated fatty acids, and relatively low antioxidant capacity [11]. Neuronal GSH synthesis depends on cysteine uptake through excitatory amino acid carrier 1 (EAAC1), highlighting the tight coupling between redox homeostasis and neuronal function [11].
Thioredoxin System
The thioredoxin system represents another essential redox regulatory network centered on thioredoxin (Trx), a small (12 kDa) multifunctional redox-active protein [12]. The system includes:
- Thioredoxin (Trx): Contains a conserved active-site sequence (-Cys-Gly-Pro-Cys-) that undergoes reversible oxidation/reduction during disulfide reduction.
- Thioredoxin Reductase (TrxR): A NADPH-dependent flavoenzyme that reduces oxidized Trx.
- Peroxiredoxin (Prx): Thioredoxin-dependent peroxidases that reduce H₂O₂, organic hydroperoxides, and peroxynitrite.
Table 2: Thioredoxin Family Proteins and Their Cellular Roles
| Protein | Localization | Key Features | Biological Functions |
|---|---|---|---|
| Trx-1 | Cytosol, nucleus | 12 kDa; can translocate to nucleus upon stimulation | Redox regulation, transcription factor control, apoptosis inhibition |
| Trx-2 | Mitochondria | 18.2 kDa immature protein; mitochondrial targeting sequence | Regulation of mitochondrial apoptosis, cytochrome c release inhibition |
| TRP14 | Cytosol | 14 kDa; reacts with PTEN | Cellular redox regulation, PTEN reactivation |
| Grx-1 | Cytosol, nucleus | Glutathione-dependent; dithiol or monothiol mechanisms | Reduction of protein-GSH mixed disulfides (deglutathionylation) |
The thioredoxin system collaborates with complementary antioxidant systems through overlapping functions. Glutaredoxins (Grx), which are glutathione-dependent thioredoxin family proteins, specialize in reducing protein-glutathione mixed disulfides (deglutathionylation) using glutathione as a reductant [12]. Both systems are essential for embryonic development, as demonstrated by the embryonic lethality observed in Trx-1 and Trx-2 deficient mice [12].
NADPH: The Central Reductant
NADPH serves as the central electron donor for redox homeodynamics, providing reducing equivalents for:
- Regeneration of reduced glutathione via glutathione reductase
- Reduction of thioredoxin via thioredoxin reductase
- Direct antioxidant function through NADPH-quinone oxidoreductase
- NADPH oxidase (NOX)-dependent ROS generation for signaling
The NADPH/NADP⁺ ratio is tightly regulated through the pentose phosphate pathway, malic enzyme, and NADP⁺-dependent isocitrate dehydrogenase, creating direct links between cellular metabolic status and redox homeodynamics [11].
Redox Signaling Mechanisms and Molecular Targets
Cysteine Oxidation as a Central Mechanism
Redox signaling primarily occurs through specific, reversible oxidation of cysteine residues in target proteins [5]. The sulfur atom in cysteine undergoes a range of oxidative modifications that function as molecular switches:
Figure 1: Cysteine Oxidation States in Redox Signaling
The reactivity of cysteine residues toward H₂O₂ varies widely, with rate constants ranging from <1 M⁻¹s⁻¹ for non-reactive cysteines to >10⁵ M⁻¹s⁻¹ for specialized peroxidatic cysteines in peroxiredoxins and other redox sensors. This differential reactivity provides specificity to redox signaling [5].
Recent research has revealed that per/polysulfidation of cysteine residues (formation of Cys-SSH or Cys-SnSH) may protect against irreversible oxidation during severe oxidative stress. When persulfidated cysteines are overoxidized, they form cysteine-persulfinic/sulfonic acids (Cys-S-SO₂H/SO₃H) that retain a reducible disulfide bond, allowing enzyme repair by thioredoxin or glutaredoxin systems [5].
Redox-Sensitive Signaling Pathways
Multiple major signaling pathways are regulated by redox mechanisms through reversible cysteine modifications:
Keap1-Nrf2 Pathway: The primary cellular defense against oxidative stress. Under basal conditions, Nrf2 is bound by Keap1 and targeted for proteasomal degradation. Oxidative modification of specific cysteine residues in Keap1 (Cys151, Cys273, Cys288) disrupts this interaction, allowing Nrf2 translocation to the nucleus where it activates antioxidant response element (ARE)-containing genes [8] [5].
NF-κB Pathway: Redox regulation of NF-κB occurs at multiple levels, including IKK activation, IκB degradation, and NF-κB DNA binding. The pathway is differentially regulated by various ROS, with H₂O₂ often activating and higher ROS levels potentially inhibiting NF-κB signaling [13].
Other Pathways: Additional redox-sensitive pathways include HIF-1α (stabilized under hypoxia), FOXO transcription factors (activated by oxidative stress to enhance antioxidant expression), and p53 (regulated by redox modifications that affect its DNA binding and transcriptional activity) [13].
Experimental Approaches in Redox Biology
Methodological Framework
Investigating redox signaling requires careful experimental design and interpretation. The following checklist provides key considerations for establishing a role for specific ROS in biological processes [9]:
- Identify the specific ROS responsible rather than using "ROS" as a generic term
- Verify chemical plausibility of the proposed reactions
- Confirm appropriate localization and concentration of the ROS or antioxidant
- Demonstrate functional impact of altering ROS levels or oxidative modifications
Figure 2: Experimental Workflow for Redox Signaling Studies
Critical Reagents and Methodologies
Table 3: Essential Research Reagents for Redox Signaling Studies
| Reagent Category | Specific Examples | Function & Application | Important Considerations |
|---|---|---|---|
| ROS Probes | Genetically encoded HyPer, roGFP; DCFH-DA, DHE | Dynamic, compartment-specific ROS measurement; general oxidative stress assessment | Specificity varies (HyPer for H₂O₂; roGFP for redox potential); artifacts common with chemical probes |
| ROS Modulators | NOX inhibitors (apocynin, VAS2870); SOD mimetics; Catalase | Modulate specific ROS pathways; test functional involvement | Verify specificity and efficacy; SOD mimetics often have lower activity than endogenous SOD |
| Thiol Modifiers | N-ethylmaleimide (NEM), iodoacetamide (IAM) | Alkylate free thiols to preserve redox state during sample processing | Use appropriate controls; ensure complete alkylation |
| Antioxidants | N-acetylcysteine (NAC), Tempol, Vitamin E | Test antioxidant effects; modulate redox state | NAC acts mainly as cysteine precursor, not direct H₂O₂ scavenger; multiple effects possible |
| Redox Biosensors | Biotin-switch techniques, redox Western blotting | Detect specific protein modifications (S-nitrosylation, glutathionylation) | Multiple controls needed; potential false positives |
| Genetic Tools | siRNA/shRNA, CRISPR/Cas9, transgenic animals | Modulate expression of redox system components | Consider compensation and developmental effects |
Recent advances in genetically encoded fluorescent redox probes allow dynamic, real-time measurements of defined redox species with subcellular compartment resolution in intact living cells [10]. These tools have revolutionized our understanding of redox homeodynamics by enabling researchers to monitor spatiotemporal patterns of redox signaling rather than static snapshots.
When using pharmacological tools, careful interpretation is essential. For example, N-acetylcysteine (NAC) is widely described as an antioxidant but directly scavenges H₂O₂ very slowly; many of its effects likely result from increasing cellular thiol levels or reducing disulfide bridges in cell surface receptors [9]. Similarly, the biological activity of SOD mimetics should be verified to significantly increase total SOD activity above endogenous levels before concluding that superoxide depletion mediates observed effects [9].
Pathophysiological Implications and Therapeutic Perspectives
Disruption of redox homeodynamics contributes to numerous pathological conditions. In neurodegenerative diseases such as Alzheimer's and Parkinson's, oxidative damage accumulates due to the brain's high oxygen consumption, abundance of oxidizable substrates, and relatively weak antioxidant defenses [11] [13]. In the cardiovascular system, NADPH oxidase-derived ROS contribute to endothelial dysfunction, hypertension, and atherosclerosis [13]. Cancers often display altered redox regulation, with increased ROS production driving proliferation while adaptive upregulation of antioxidant systems promotes survival [8].
Therapeutic strategies targeting redox systems include:
- Nrf2 Activators: Compounds that promote Nrf2 dissociation from Keap1 to enhance antioxidant gene expression
- NOX Inhibitors: Specific inhibitors of pathological ROS production
- Mitochondria-Targeted Antioxidants: Compounds like MitoQ that accumulate in mitochondria
- Redox Modulators: Agents that selectively increase ROS in cancer cells to exceed toxic thresholds
The dual role of ROS as both signaling molecules and damaging agents creates therapeutic challenges, as global antioxidant supplementation may disrupt beneficial redox signaling while attempting to reduce oxidative damage [5]. Future therapeutic approaches will likely require precise spatiotemporal modulation of specific redox pathways rather than general antioxidant approaches.
The molecular players in redox signaling—ROS, RNS, GSH, thioredoxin, and NADPH systems—function within an integrated framework of redox homeodynamics that maintains functional stability through dynamic interactions and continuous adjustment. Understanding the specific roles, compartmentalization, and regulatory relationships among these systems provides crucial insights into both physiological regulation and pathological mechanisms. Future research emphasizing spatiotemporal resolution of redox processes and their integration with other signaling networks will advance both fundamental understanding and therapeutic applications of redox biology.
The concept of redox homeostasis as a simple, static balance has evolved into the more dynamic paradigm of redox homeodynamics, which portrays redox regulation as a continuous, adaptive signaling process. Central to this framework is the "Redox Code," a set of principles governing how specific, reversible chemical modifications on cysteine residues transduce cellular signals to regulate metabolism, gene expression, and cell fate. This whitepaper delves into the molecular machinery of thiol-based redox switches, focusing on the mechanisms of reversible cysteine oxidative post-translational modifications (PTMs) and their role in health and disease. We provide a detailed examination of the core signaling mechanisms, supported by summarized quantitative data, experimental protocols for key assays, and visualizations of critical pathways. Furthermore, we explore the therapeutic implications of targeting the redox code, offering a toolkit for researchers and drug developers aiming to intervene in pathologies driven by redox dysregulation, from cancer to neurodegenerative diseases.
The traditional view of redox homeostasis as a simple steady-state balance between oxidants and antioxidants has been refined by the concept of redox homeodynamics. This modern paradigm emphasizes that the redox state is not a static set-point to be maintained, but a dynamic, actively signaling interface that continuously adapts to metabolic and environmental challenges [14] [3]. This dynamic equilibrium, or nucleophilic tone, is preserved through continuous feedback signaling for the production and elimination of electrophiles and nucleophiles [3].
Underpinning this redox homeodynamics is the Redox Code, a set of principles that includes the regulation of NADH and NADPH systems in metabolism and the dynamic control of thiol switches in the redox proteome [15]. The code is written primarily through the chemistry of cysteine thiols, which act as molecular sensors and transducers. The redox-sensitive proteome, or redoxome, with its network of cysteine-sensitive proteins—the cysteinet—serves as the hardware upon which this code is executed [16]. These proteins are fundamental for maintaining cellular redox balance and controlling signaling in response to changes in the redox environment. Understanding this code is paramount, as its dysregulation is a hallmark of a wide array of diseases, including cancer, neurodegenerative disorders, and metabolic syndromes [15] [16].
The Molecular Basis of the Redox Code: Cysteine Chemistry and Compartmentalization
Cysteine as a Redox-Sensitive Molecular Switch
The sulfur atom of a cysteine residue is uniquely versatile in its chemistry. Its thiol (-SH) side chain can undergo a wide spectrum of reversible oxidative post-translational modifications, making it an ideal molecular switch analogous to phosphorylation [17]. The reactivity of a specific cysteine is dictated by its local protein microenvironment. A key determinant is its acidity (pKa); cysteines with a low pKa (4–5) exist as a reactive thiolate anion (S-) at physiological pH, making them uniquely susceptible to oxidation compared to cysteines with a typical pKa of 8.5 [18] [17].
The following table summarizes the major reversible cysteine modifications involved in redox signaling:
Table 1: Major Reversible Cysteine Oxidative Post-Translational Modifications
| Modification | Inducing Species | Chemical Designation | Key Regulatory Enzymes |
|---|---|---|---|
| S-Nitrosylation [18] | NO, S-nitrosothiols | SNO | GSNO Reductase [18] |
| S-Glutathionylation [18] | ROS, reactive intermediates | PSSG | Glutaredoxin (Grx) [18] |
| Disulfide Bond [19] | ROS | S-S | Thioredoxin (Trx), Protein Disulfide Isomerase (PDI) [18] |
| Sulfenic Acid [19] | H₂O₂ | SOH | Peroxiredoxins, subsequent reactions |
| S-Sulfhydration [17] | H₂S derivatives | SSH | Not Specified |
| Sulfinic Acid [18] | ROS | SO₂H | Sulfiredoxin (ATP-dependent) [18] |
These modifications function as molecular switches that can drastically alter protein function, location, and interaction partners. Distinct modifications can lead to unique functional outcomes, allowing a single cysteine to process different redox signals into specific cellular responses [18]. For instance, sulfenic acid formation in protein tyrosine phosphatases (PTPs) leads to their inactivation, thereby promoting phosphorylation-dependent signaling cascades [19].
Compartmentalization of Redox Potential
A critical feature of redox homeodynamics is the stark compartmentalization of the redox potential within the cell. This compartmentalization ensures that redox signals are spatially constrained, adding specificity to the redox code.
Table 2: Redox Compartmentalization in Eukaryotic Cells
| Cellular Compartment | Redox Environment (Eh GSSG) | Key Characteristics and Players |
|---|---|---|
| Cytosol / Nucleus [17] | Highly Reducing (-150 to -200 mV) | Reduced by GSH, Grx, Trx. Disulfide formation is unfavorable. |
| Mitochondria [17] | Highly Reducing (-150 to -200 mV) | Major source of ROS (e.g., Complex I, III). High GSH and Trx2. |
| Endoplasmic Reticulum [17] | Oxidizing (-170 to -185 mV) | Specialized for disulfide bond formation via Ero1, PDI, QSOX. |
| Extracellular Space [17] | Oxidizing (-80 to -150 mV) | More oxidizing milieu, stable disulfide bonds. |
This compartmentalization dictates the type of redox modifications that can occur. The cytosol and nucleus are optimized for transient, reversible signaling modifications like S-nitrosylation and S-glutathionylation, whereas the ER is specialized for the formation of structural disulfide bonds in secretory and membrane proteins [17].
Figure 1: The Cysteine Redox Switch Network. Cysteine thiols, particularly in their reactive thiolate form (S⁻), can be oxidized by various reactive species to form different reversible post-translational modifications. A network of specific reductase enzymes returns the oxidized cysteine to its reduced state, completing the catalytic cycle that forms the basis of redox signaling. Key: RNS, Reactive Nitrogen Species; GSSG, Oxidized Glutathione; ROS, Reactive Oxygen Species; Trx, Thioredoxin; Grx, Glutaredoxin; GSNOR, S-Nitrosoglutathione Reductase; PDI, Protein Disulfide Isomerase. Adapted from [18] [16] [17].
Physiological and Pathophysiological Roles of Thiol Switches
Regulation of Signal Transduction Pathways
Redox signaling via cysteine switches is a main feature of signal transduction downstream of a vast array of receptors, including receptor tyrosine kinases (RTKs), G-protein coupled receptors (GPCRs), and cytokine receptors [18] [19]. A classic example is the reversible inactivation of Protein Tyrosine Phosphatases (PTPs). The catalytic cysteine of PTPs has a low pKa and is highly susceptible to oxidation by H₂O₂ generated in response to growth factor stimulation. Formation of sulfenic acid reversibly inactivates the phosphatase, thereby prolonging the phosphorylation and activation of kinase signaling cascades [19]. This mechanism ensures that physiological levels of H₂O₂ act as a second messenger to amplify mitogenic signals.
Another key regulatory mechanism involves the redox-dependent switch of Peroxiredoxins (Prx). These major antioxidant enzymes can shift from acting as peroxidases to functioning as molecular chaperones upon overoxidation. This functional switch, triggered by high levels of H₂O₂, allows localized H₂O₂ accumulation to facilitate signaling to proteins like the transcription factor HIF1α while simultaneously preparing the cell to handle stress-induced protein unfolding [19].
Mitochondrial Redox Signaling
Mitochondria are critical hubs for redox signaling, with several physiological processes being initiated by a transient redox burst from the electron transport chain (ETC) [20]. Key mechanisms of elevated superoxide/H₂O₂ production include:
- Reverse Electron Transport (RET): Driven by succinate accumulation, leading to superoxide production at Complex I, which signals in contexts like hypoxia-reperfusion and thermogenesis [20].
- Cytochrome c retardation: Slowing of electron flow at Complex III, a key mechanism for initiating HIF1α stabilization during hypoxia [20].
- Fatty acid oxidation: Electron transfer flavoprotein: coenzyme Q oxidoreductase (ETFQOR) generates superoxide during elevated fatty acid oxidation, which can stimulate insulin secretion [20].
This mitochondrial redox signal is then relayed, often via peroxiredoxins, to specific extramitochondrial targets, enabling processes such as the regulation of transcription factors (e.g., HIF1α, PGC1α), immune cell activation, and metabolic adaptation [20].
Redox Dysregulation in Disease
Dysregulation of the redox code is implicated in the pathogenesis of numerous diseases. In neurodegenerative diseases such as Amyotrophic Lateral Sclerosis (ALS), Alzheimer's, and Parkinson's, redox dysregulation and oxidative stress lead to aberrant cysteine PTMs on key proteins. This can result in protein misfolding, aggregation, and neuronal dysfunction, forming a "cysteinet" that drives pathology [16]. For example, S-nitrosylation of protein disulfide isomerase (PDI) can inhibit its chaperone activity, contributing to the accumulation of misfolded proteins [16].
In cancer, redox signaling promotes tumor progression and metastasis. For instance, knockdown of the antioxidant enzyme GPx2 in a breast cancer model creates a redox signal that stabilizes HIF1α. This, in turn, activates the transcription factor p63, driving a hybrid epithelial/mesenchymal (E/M) phenotype and metabolic reprogramming towards oxidative phosphorylation (OXPHOS), ultimately facilitating metastasis [21]. This highlights how targeted redox dysregulation can orchestrate complex phenotypic and metabolic switches in cancer.
Experimental Approaches and Methodologies
Studying the redox code requires a specialized set of tools to detect, quantify, and manipulate specific cysteine modifications and their functional consequences.
The Scientist's Toolkit: Key Research Reagents and Methods
Table 3: Essential Reagents and Methods for Redox Biology Research
| Reagent / Method | Function / Target | Key Application Notes |
|---|---|---|
| Biotin-Switch Assay [18] | Specific detection of S-nitrosylation (SNO). | Proteins are initially blocked, SNO bonds are selectively reduced (e.g., with ascorbate), and newly freed thiols are biotinylated for pull-down. |
| Dimedone & Probes [19] | Chemical probes that specifically trap sulfenic acids (SOH). | Allows for direct labeling and detection of this often transient intermediate. Critical for studying PTP and kinase regulation. |
| Antibodies vs. Oxidized Cys | Immunodetection of specific PTMs (e.g., SO₂H, SNO). | Commercially available antibodies enable Western blot and IHC detection, though specificity must be validated. |
| Redox-Sensitive GFP (roGFP) [15] | Real-time, live-cell measurement of redox potential. | Genetically encoded sensor that ratiometrically reports the glutathione redox potential (Eh) in specific cellular compartments. |
| MS-based Redox Proteomics [18] [16] | Global, unbiased mapping of cysteine oxidation states. | Involves blocking free thiols, reducing specific PTMs, and labeling newly freed thiols with isotopic tags for mass spectrometry (MS) identification/quantification. |
| siRNA/CRISPR for Redox Enzymes [21] | Functional studies of redox regulators (e.g., GPx2, Trx, GSNOR). | Used to dissect the role of specific enzymes in controlling redox signaling nodes in disease models like cancer. |
Detailed Experimental Protocol: Mapping the Redox Proteome
For researchers aiming to conduct a global analysis of the "cysteinet," the following workflow, based on modern mass spectrometry (MS) approaches, is considered a gold standard.
Objective: To identify and quantify reversible cysteine oxidation events across the proteome in response to a specific stimulus (e.g., H₂O₂, growth factors).
Workflow:
Cell Lysis with Alkylation: Rapidly lyse cells in a buffer containing a strong alkylating agent (e.g., Iodoacetamide, IAM; or N-ethylmaleimide, NEM) to block all free, reduced thiols. This "caps" the basal reduced state of cysteines and prevents post-lysis oxidation artifacts.
PTM-Specific Reduction: Divide the lysate. In one sample, treat with a reagent that selectively reduces the PTM of interest. For example:
- S-nitrosylation: Use ascorbate/copper to selectively reduce S-NO bonds to free thiols.
- Disulfides/S-glutathionylation: Use a specific reducing agent like Tris(2-carboxyethyl)phosphine (TCEP) or DTT.
- Sulfenic Acid: Use a probe-labeled dimedone derivative that has been conjugated to a tag like biotin after the initial trapping step.
Tagging of Newly Freed Thiols: After the selective reduction step, the newly exposed thiols, which represent previously oxidized cysteines, are labeled with a distinct isotopic tag. The most common method is using IodoTMT or similar tandem mass tag (TMT) reagents that enable multiplexed quantification.
Combination, Digestion, and Enrichment: Combine the differentially labeled samples. Digest the proteins with trypsin. Enrich for the tagged, previously oxidized peptides using anti-TMT antibodies or streptavidin beads (if a biotin-based method was used in step 2).
Liquid Chromatography-Mass Spectrometry (LC-MS/MS): Analyze the enriched peptides by LC-MS/MS. The isotopic tags allow for precise relative quantification of the oxidation level of specific cysteine sites across different experimental conditions.
Data Analysis: Use bioinformatic tools to identify the proteins and specific cysteine residues that showed significant changes in oxidation, mapping them onto pathways and functional networks.
Figure 2: Experimental Workflow for Redox Proteomics. This diagram outlines the key steps for a quantitative mass spectrometry-based experiment to map specific cysteine oxidative post-translational modifications (PTMs) across the proteome, such as the biotin-switch technique and related methods. LC-MS/MS, Liquid Chromatography-Tandem Mass Spectrometry; IAM, Iodoacetamide; SNO, S-Nitrosylation. Adapted from [18] [16].
Therapeutic Targeting of the Redox Code
The intricate role of redox signaling in disease makes it an attractive therapeutic arena. Strategies are moving beyond broad-spectrum antioxidants to targeted approaches that aim to reset specific dysregulated nodes in the redox network.
Current and Emerging Therapeutic Strategies
Small Molecule Inhibitors: Emerging therapies focus on developing small molecule inhibitors that target specific cysteine residues in redox-sensitive proteins. These compounds have demonstrated promising outcomes in preclinical models, setting the stage for forthcoming clinical trials [15]. For example, targeting the redox-sensitive transcription factor NRF2, the "master regulator" of the antioxidant response, is a active area of research for cancer and inflammatory diseases [15].
Modulating Redox-Sensitive Nodes in Cancer: The example of GPx2 in breast cancer provides a mechanistic basis for therapeutic intervention. In this context, GPx2 loss creates a dependency on HIF1α signaling for metastasis. Experimental Approach: To validate this, researchers can treat GPx2-knockdown tumor-bearing mice with a HIF1α inhibitor like echinomycin. The protocol involves monitoring tumor growth and quantifying lung metastases, with results demonstrating that HIF1α loss or GPx2 overexpression reverses the metastatic phenotype [21]. This confirms HIF1α as a druggable target in this specific redox-context.
Challenges and Precision Medicine: The failure of broad-spectrum antioxidants in complex diseases underscores the need for precision. The therapeutic goal is not global antioxidant suppression but the precise re-establishment of redox balance in specific cellular compartments or pathways [15] [3]. This requires a deep, context-specific understanding of redox signaling in each disease.
Figure 3: Targeting a Redox Signaling Pathway in Breast Cancer Metastasis. This pathway, elucidated through single-cell transcriptomics, shows how knockdown of Glutathione Peroxidase 2 (GPx2) creates a redox signal that stabilizes HIF1α, activating p63 and driving a metastatic hybrid epithelial/mesenchymal (E/M) state. The diagram highlights two successful therapeutic intervention points: HIF1α inhibition and GPx2 overexpression, both of which suppress metastasis in experimental models [21].
The framework of redox homeodynamics has revolutionized our understanding of redox biology, positioning it as a dynamic, information-rich signaling system rather than merely a battle against oxidative damage. The Redox Code, executed through reversible cysteine modifications, represents a fundamental language of cellular communication that integrates metabolic status, environmental cues, and transcriptional responses. The experimental and therapeutic landscape in redox biology is rapidly advancing, driven by sophisticated proteomic tools and a more nuanced understanding of context-specific redox signaling. The future of targeting the redox code lies in the development of precise, mechanism-based therapeutics that can modulate specific thiol switches to restore physiological redox homeodynamics in a wide range of human diseases.
Within cellular biology, the conceptual framework is evolving from static redox homeostasis toward redox homeodynamics, emphasizing the dynamic, adaptive, and signaling roles of redox processes. This whitepaper elucidates how the Nrf2-Keap1 pathway and PGC-1α function as central sensors and effectors within this paradigm. Nrf2 orchestrates a rapid, inducible antioxidant response, while PGC-1α governs mitochondrial biogenesis and function, ensuring long-term metabolic adaptation. Critically, these systems are not isolated; they engage in extensive crosstalk, forming a resilient regulatory network that maintains cellular integrity in the face of metabolic and oxidative challenges. Understanding this intricate interplay provides a sophisticated foundation for novel therapeutic strategies in drug development targeting age-related diseases, metabolic disorders, and cancer.
The traditional view of redox homeostasis implies a static equilibrium in the balance between oxidants and antioxidants. However, contemporary research underscores that redox processes are inherently dynamic, acting as continuous signaling mechanisms that can be smoothly modulated to support physiological functions and adaptive responses [3]. This dynamic equilibrium, or redox homeodynamics, involves constant feedback to preserve nucleophilic tone, which is essential for a healthy physiological state [3]. Within this framework, electrophiles and reactive oxygen species (ROS) are not merely damaging agents but serve as specific molecular messengers in cellular signaling [22]. A key feature of homeodynamics is hormesis, where mild stress triggers adaptive beneficial responses, and parahormesis, where certain nutritional phytochemicals mimic these effects by activating pathways like Nrf2 to support homeostasis [3]. This paper explores the Nrf2-Keap1 pathway and PGC-1α as quintessential sensors and effectors within the paradigm of redox homeodynamics.
The Nrf2-Keap1 Pathway: A Sensor for Electrophilic Stress
Molecular Regulation of the Nrf2-Keap1 Axis
The Nrf2-Keap1 system is a primary cellular defense mechanism against electrophilic stress and oxidative challenge. Under basal conditions, Nrf2 is continuously ubiquitinated and targeted for proteasomal degradation by its negative regulator, Keap1, a substrate adaptor for a Cullin 3-based E3 ubiquitin ligase complex [23]. Keap1 is a cysteine-rich protein that acts as a sensitive redox sensor. Upon exposure to oxidants or electrophiles, specific cysteine residues in Keap1 are modified, leading to a conformational change that inhibits its E3 ligase activity [23]. This results in Nrf2 stabilization, its translocation to the nucleus, and heterodimerization with small MAF (sMAF) proteins. The heterodimer binds to the Antioxidant Response Element (ARE), activating the transcription of a vast network of over 200 genes involved in antioxidant defense, detoxification, and NADPH regeneration [24] [23]. The system is designed for rapid activation and deactivation, ensuring a dynamic and responsive defense.
Experimental Analysis of the Nrf2 Pathway
Studying the Nrf2 pathway requires methodologies to assess its activation, downstream effects, and functional outcomes. Key experimental approaches are summarized in the table below.
Table 1: Key Experimental Methodologies for Investigating the Nrf2-Keap1 Pathway
| Methodology | Key Objective | Example Application & Findings |
|---|---|---|
| Quantitative Proteomics | Identify oxidative modifications on protein cysteine residues. | Revealed redox changes in 403 proteins in AZA-resistant leukemic cells, implicating the SQSTM1-KEAP1-NRF2 pathway in drug resistance [25]. |
| ARE-Luciferase Reporter Assay | Measure Nrf2 transcriptional activity. | Used in vitro and in vivo to screen for Nrf2 activators (e.g., sulforaphane) and quantify pathway induction [23]. |
| GSH/GSSG Ratio Measurement | Assess the cellular redox state. | Flow cytometry revealed a more oxidized state and higher GSH in 5-azacytidine (AZA)-resistant MDS/AML cells [25]. |
| Keap1 Inhibitor Studies | Functionally validate Nrf2 dependence. | KEAP1 inhibition re-sensitized AZA-resistant cells to treatment and improved survival in mouse xenograft models [25]. |
| ChIP-Seq (Chromatin Immunoprecipitation) | Map genome-wide Nrf2 binding sites. | Identifies direct Nrf2 target genes and ARE locations in specific cell types [24]. |
Figure 1: The Nrf2-Keap1 Signaling Pathway. Under basal conditions, Keap1 targets Nrf2 for degradation. Oxidative stress modifies Keap1 cysteine residues, leading to Nrf2 stabilization, nuclear translocation, and activation of cytoprotective gene expression.
PGC-1α: A Master Regulator of Mitochondrial and Redox Homeodynamics
PGC-1α as an Integrative Coactivator
PGC-1α is a transcriptional coactivator identified as a master regulator of mitochondrial biogenesis and function [26]. It does not bind DNA directly but serves as a modular scaffolding platform, interacting with and coactivating a wide range of transcription factors in response to environmental and intracellular cues [27] [26]. Through its interactions with nuclear respiratory factors (NRF1 and NRF2), and ERRα, PGC-1α drives the expression of nuclear-encoded mitochondrial genes, including those for the electron transport chain (ETC), and key factors like TFAM, which is essential for mitochondrial DNA transcription and replication [28]. Consequently, PGC-1α is a central effector for enhancing oxidative phosphorylation (OXPHOS) and cellular energy capacity.
Regulation of PGC-1α Expression and Activity
PGC-1α is regulated at multiple levels, allowing for precise control over its activity:
- Transcriptional Regulation: Key upstream transcription factors include CREB (activated by cAMP/PKA signaling in response to glucagon or cold), MEF2, and ATF2 (activated by p38 MAPK signaling) [27] [28]. Intracellular calcium influx, such as during muscle contraction, activates CaMKIV, which also promotes PGC-1α expression via CREB [28].
- Post-Translational Modifications: These critically fine-tune PGC-1α's activity and stability. Key activating modifications include phosphorylation by p38 MAPK and AMPK, and deacetylation by SIRT1 in low-energy states (high NAD+ levels) [27] [28]. Conversely, acetylation by GCN5 and phosphorylation by AKT or GSK3β inhibit PGC-1α or promote its degradation [27] [28].
Table 2: Key Regulatory Inputs and Modifications of PGC-1α
| Regulator | Effect on PGC-1α | Physiological Context |
|---|---|---|
| CREB | Increased transcription | Fasting, cold exposure, exercise [28]. |
| p38 MAPK | Increased transcription and phosphorylation (activation) | Cellular stress, exercise [27] [28]. |
| AMPK | Phosphorylation (activation) | Low energy status (high AMP/ATP ratio) [28]. |
| SIRT1 | Deacetylation (activation) | Low energy status (high NAD+), fasting [27]. |
| AKT/GSK3β | Phosphorylation (inhibition/degradation) | Insulin signaling [27]. |
| NF-κB | Repressed expression and activity | Inflammation [26]. |
PGC-1α in Redox Metabolism
Beyond its role in mitochondrial biogenesis, PGC-1α is a pivotal regulator of the cellular antioxidant response. It directly controls the expression of major mitochondrial and cytosolic antioxidant enzymes, including manganese superoxide dismutase (MnSOD/SOD2), catalase, peroxiredoxin 3/5, uncoupling protein 2 (UCP2), and thioredoxin 2 [27]. By enhancing the mitochondrial membrane potential and OXPHOS, PGC-1α can also influence the primary site of ROS generation. Therefore, PGC-1α acts as a key node, dynamically coordinating energy production with the capacity to manage its potentially harmful redox byproducts, a core principle of homeodynamics.
Interplay and Crosstalk between Nrf2 and PGC-1α Signaling
The relationship between Nrf2 and PGC-1α is a quintessential example of homeodynamic crosstalk. Rather than operating in isolation, these pathways form a regulatory loop that ensures a coordinated adaptation to metabolic and oxidative demands [28].
- PGC-1α as a Downstream Effector of Nrf2: Nrf2 activation can promote mitochondrial biogenesis by upregulating the expression of NRF1 (a nuclear respiratory factor), which is a key binding partner for PGC-1α [28]. This creates a direct molecular link from the antioxidant response to the enhancement of mitochondrial capacity.
- Nrf2 as a Target of PGC-1α-Regulated Metabolism: Conversely, the metabolic shifts driven by PGC-1α influence the redox environment. Increased mitochondrial flux can elevate ROS production, which in turn can serve as a signaling molecule to activate the Nrf2 pathway [28]. This creates a feedback loop where an increase in metabolic capacity is matched by an enhanced antioxidant capability.
- Shared Upstream Regulators: Both pathways are influenced by common sensors of cellular energy and stress. For instance, AMPK not only activates PGC-1α but can also phosphorylate and activate Nrf2 [23]. Similarly, p38 MAPK signaling positively regulates both factors [27] [23].
This intricate crosstalk underscores the system's robustness, allowing the cell to mount a unified and adaptive response to maintain homeodynamics.
Figure 2: Crosstalk between the Nrf2 and PGC-1α Pathways. Shared upstream regulators like AMPK and p38 MAPK coregulate Nrf2 and PGC-1α. Nrf2 can promote mitochondrial biogenesis via NRF1, while PGC-1α-driven metabolism can generate ROS signals that feedback to activate Nrf2.
The Scientist's Toolkit: Key Research Reagents and Models
Table 3: Essential Research Reagents and Models for Studying Redox Homeodynamics
| Reagent / Model | Function/Application | Key Examples & Notes |
|---|---|---|
| KEAP1 Inhibitors | Pharmacologically disrupt Nrf2-Keap1 interaction to study Nrf2 activation. | e.g., ML334, RTA-408; used to re-sensitize AZA-resistant cancer cells [25]. |
| Nrf2 Activators | Induce the antioxidant response pathway. | Sulforaphane, CDDO-Me; used to study cytoprotection and potential in metabolic diseases [23]. |
| SIRT1 Activators | Mimic low-energy state to activate PGC-1α via deacetylation. | Resveratrol, SRT1720; important for studying mitochondrial adaptation and energy metabolism [27]. |
| PGC-1α Expression Constructs | Overexpress or knock down PGC-1α to determine its functional role. | Adenoviral or lentiviral vectors for gain/loss-of-function studies in vitro and in vivo [26]. |
| ARE-Luciferase Reporter | Quantify Nrf2 transcriptional activity in high-throughput screens. | Cell lines stably transfected with ARE-driven luciferase construct [23]. |
| AZA-Resistant Cell Lines | Model of acquired chemoresistance linked to redox reset. | MDS/AML OCI-M2 clones with altered KEAP1-NRF2 signaling and redox state [25]. |
| CdX Mouse Models | In vivo validation of pathway mechanisms and therapeutic efficacy. | Immunodeficient mice transplanted with AZA-R cells to test KEAP1 inhibitor efficacy [25]. |
The Nrf2-Keap1 pathway and PGC-1α are master regulators that epitomize the concept of redox homeodynamics. Their roles as sensors and effectors, their multi-layered regulation, and their extensive crosstalk create a dynamic and resilient network that allows the cell to adapt to a constantly changing environment. Moving forward, several key areas will shape future research and therapeutic development:
- Targeting Pathway Crosstalk: Therapeutic strategies should consider the interconnected nature of these pathways. For example, in inflammatory diseases where NF-κB suppresses PGC-1α [26], combined activation of PGC-1α and Nrf2 may offer synergistic benefits.
- Overcoming Drug Resistance: The discovery that AZA resistance in MDS/AML is mediated by a redox reset involving KEAP1-NRF2 [25] opens new avenues for combination therapies, using KEAP1 inhibitors to re-sensitize tumors to existing drugs.
- Precision Modulation: A major challenge is achieving tissue- and context-specific modulation. The development of more targeted activators and a deeper understanding of the differential regulation of PGC-1α splice variants [26] will be crucial for minimizing off-target effects.
In conclusion, framing these regulatory systems within the dynamic concept of homeodynamics provides a more powerful and accurate model for understanding cellular resilience, aging, and disease pathogenesis, ultimately guiding the development of next-generation therapeutics.
Redox homeostasis, the delicate balance between reactive oxygen species (ROS) production and elimination, is fundamental to cellular health. This whitepaper explores the concept of redox homeodynamics—the dynamic, adaptive nature of redox regulation—and its critical shift toward redox dyshomeostasis in pathological states. We provide a technical analysis of how the loss of redox control drives pathogenesis in cardiovascular diseases (CVD), neurodegenerative disorders (NDDs), and neoplastic diseases through shared yet context-specific mechanisms. By integrating current research findings, structured quantitative data, detailed experimental methodologies, and visual signaling pathways, this guide serves as a comprehensive resource for researchers and drug development professionals targeting redox-based therapeutic strategies.
The traditional concept of redox homeostasis implies a static equilibrium, whereas contemporary understanding emphasizes redox homeodynamics—a dynamic, adaptive interplay between pro-oxidant generation and antioxidant defense that maintains functional stability in biological systems [15]. This sophisticated regulatory network ensures that reactive oxygen species (ROS), once considered merely toxic metabolic byproducts, can function as crucial redox signaling molecules at physiological concentrations [29] [30].
Redox dyshomeostasis occurs when this dynamic balance is disrupted, leading to either oxidative stress (excess ROS) or reductive stress (excess antioxidants) [29] [31]. This imbalance triggers molecular damage and aberrant signaling, establishing a common pathological foundation across diverse disease states. The dual nature of ROS as both signaling molecules and damaging agents creates a context-dependent therapeutic challenge [29] [31]. In the transition from homeodynamics to dyshomeostasis, several core mechanisms are repeatedly engaged:
- Mitochondrial dysfunction leading to altered ROS production
- Dysregulated NRF2 signaling, a master regulator of antioxidant response
- Altered redox-sensitive pathways (NF-κB, MAPK)
- Epigenetic modifications and post-translational changes to proteins [15]
The following sections detail how these mechanisms manifest in cardiovascular, neurodegenerative, and neoplastic diseases, providing a comparative framework for understanding disease-specific and shared therapeutic targets.
Redox Dyshomeostasis in Cardiovascular Diseases
In the cardiovascular system, redox homeodynamics is precisely regulated, with ROS serving as vital signaling molecules for normal vascular function. The shift toward dyshomeostasis involves hyperactivation of oxidant sources and impaired antioxidant defense, contributing fundamentally to endothelial dysfunction, atherosclerosis, and cardiac remodeling.
Molecular Mechanisms and Pathological Consequences
Table 1: Major ROS Sources and Their Roles in Cardiovascular Pathology
| ROS Source | Localization | Primary ROS | Cardiovascular Pathological Role |
|---|---|---|---|
| NADPH Oxidases (Nox) | Vascular cell membranes | Superoxide (O₂•⁻) | Primary signaling ROS source; activated by AngII, TNF-α; drives hypertrophy & endothelial dysfunction [30] |
| Mitochondrial ETC | Mitochondrial inner membrane | Superoxide (O₂•⁻) | Electron leak during oxidative phosphorylation; enhanced in cardiac hypertrophy & I/R injury [32] [30] |
| Uncoupled eNOS | Endothelium | Superoxide (O₂•⁻) | Tetrahydrobiopterin deficiency converts eNOS from •NO to O₂•⁻ production; promotes atherosclerosis [30] |
| Xanthine Oxidase | Cytoplasm | Superoxide (O₂•⁻), H₂O₂ | Purine metabolism; contributes to endothelial dysfunction and heart failure [30] |
Mitochondrial sirtuins (SIRT3, SIRT4, SIRT5) function as crucial redox sensors in CVD, linking cellular metabolic status to oxidative stress responses. These NAD+-dependent enzymes are dysregulated under nutrient excess, creating a vicious cycle of mitochondrial dysfunction and ROS production [32]. SIRT3 in particular regulates key antioxidant pathways by deacetylating and activating mitochondrial enzymes like superoxide dismutase 2 (SOD2) [32].
ROS directly impact cardiovascular function through redox-sensitive post-translational modifications of cysteine thiols in proteins critical for contractility, calcium handling, and signaling. Key modifications include:
- S-glutathionylation: Reversible disulfide formation between glutathione and protein thiols regulating proteins like sarcoplasmic/endoplasmic reticulum Ca²⁺ ATPase (SERCA) and ryanodine receptors [30]
- S-nitrosylation: •NO-dependent modification regulating caspase activity and apoptosis [30]
- Sulfenic acid formation: Initial oxidation product that can progress to irreversible oxidation [30]
Experimental Assessment Methodologies
Protocol 1: Measuring Mitochondrial ROS Production in Cardiac Tissue
- Tissue Preparation: Fresh cardiac tissue (50-100mg) minced in ice-cold mitochondrial isolation buffer (250mM sucrose, 10mM HEPES, 1mM EGTA, pH 7.4)
- Mitochondrial Isolation: Differential centrifugation at 4°C: 800g for 10min (discard pellet), 10,000g for 10min (mitochondrial pellet)
- ROS Detection: Resuspend mitochondria in respiration buffer with 5μM MitoSOX Red; incubate 15min at 37°C
- Stimuli Testing: Add substrates (succinate/glutamate) with/without inhibitors (antimycin A/rotetone)
- Quantification: Measure fluorescence (excitation/emission: 510/580nm) and normalize to mitochondrial protein content [32] [30]
Protocol 2: Assessing Vascular Redox Status via NADPH Oxidase Activity
- Vessel Homogenization: Pulverize frozen vessels under liquid N₂, homogenize in lysis buffer with protease inhibitors
- Membrane Fraction Isolation: Centrifuge at 100,000g for 45min at 4°C
- Activity Assay: Incubate membrane fraction with NADPH (100μM), lucigenin (5μM) in assay buffer
- Kinetic Measurement: Monitor chemiluminescence for 30min; specificity confirmed with diphenyleneiodonium (DPI) inhibition
- Normalization: Express activity as relative light units/min/mg protein [30]
Redox Dyshomeostasis in Neurodegenerative Diseases
The brain's high metabolic rate and lipid-rich environment make it particularly vulnerable to redox dyshomeostasis. In neurodegenerative diseases, a gradual shift from adaptive redox signaling to chronic oxidative damage drives neuronal loss through distinct yet overlapping mechanisms.
Mechanisms of Oxidative Vulnerability
Table 2: Redox Dysregulation in Major Neurodegenerative Diseases
| Disease | Primary Redox Features | Key Affected Pathways | Oxidative Biomarkers |
|---|---|---|---|
| Alzheimer's Disease | Mitochondrial dysfunction, ER stress, impaired Nrf2 signaling, heme dysregulation [33] [34] | GSK3β-Nrf2 interaction, p38 MAPK, NF-κB | Increased protein & lipid oxidation in brain tissue, 4-hydroxynonenal [29] [35] |
| Parkinson's Disease | Mitochondrial complex I deficiency, dopamine oxidation, diminished Nrf2 activity [33] | DJ-1/PARK7, PINK1/Parkin, Nrf2-ARE | Protein carbonyls, lipid peroxidation in substantia nigra [33] [35] |
| Amyotrophic Lateral Sclerosis | SOD1 mutations, excessive NOX activity, disrupted RSS signaling [33] | TDP-43 pathology, ER stress, NF-κB | Elevated CSF 8-OHdG, nitrotyrosine modifications [33] |
The NRF2-KEAP1 pathway is particularly critical in NDDs, with declining Nrf2 activity observed in aging brains and neurodegenerative conditions [29] [35]. This master regulator coordinates the expression of over 250 cytoprotective genes; its impairment leaves neurons vulnerable to oxidative insults. The GSK3β enzyme serves as a key endogenous negative regulator of Nrf2, providing a mechanistic link between insulin signaling, autophagy, and redox homeostasis [35].
Post-translational modifications fine-tune redox regulation in the brain through several mechanisms:
- S-sulfhydration: Modification by hydrogen sulfide that can protect against oxidative damage [33]
- CoAlation: Covalent modification by coenzyme A that protects cysteine residues from overoxidation, particularly relevant to tau protein in Alzheimer's disease [35]
- m6A RNA methylation: Redox-sensitive epigenetic modification regulating spinal cord injury responses [35]
Experimental Assessment Methodologies
Protocol 3: Assessing Mitochondrial Function in Neuronal Cultures
- Cell Culture: Primary neurons (DIV 10-14) or neuronal cell lines cultured in neurobasal medium with B27 supplement
- Staining: Load cells with 5μM MitoTracker Red CMXRos and 2μM MitoSOX Red in HBSS for 30min at 37°C
- Treatment: Apply disease-relevant stressors (e.g., Aβ oligomers for AD models, rotenone for PD models)
- Imaging: Confocal microscopy with 579nm excitation/599nm emission (MitoTracker) and 510nm excitation/580nm emission (MitoSOX)
- Analysis: Quantify mitochondrial morphology, membrane potential, and ROS production using ImageJ plugins [33] [36]
Protocol 4: Measuring Protein Oxidation in Brain Tissue
- Tissue Homogenization: Homogenize brain regions in RIPA buffer with protease/phosphatase inhibitors
- Protein Carbonyl Detection: Derivatize with 2,4-dinitrophenylhydrazine (DNPH) for 45min at room temperature
- Detection: Separate by SDS-PAGE, transfer to PVDF, incubate with anti-DNP antibody (1:1000)
- Quantification: Normalize to total protein loaded; express as % increase over control [33]
- Alternative Method: For specific proteins, immunoprecipitate target first, then detect carbonyls
Redox Dyshomeostasis in Neoplastic Diseases
Cancer cells exploit redox homeodynamics to support proliferation, survival, and treatment resistance. The "redox adaptation" phenomenon enables neoplastic cells to maintain pro-tumorigenic ROS levels while avoiding cytotoxicity, representing a fundamental shift from physiological redox regulation.
Oncogenic Redox Rewiring
Table 3: Redox Features Across Cancer Hallmarks
| Cancer Hallmark | Redox Regulation | Key Molecular Players | Therapeutic Implications |
|---|---|---|---|
| Sustained Proliferation | Moderate ROS promote growth signaling; reductive stress in some cancers [31] | Growth factor receptors, PI3K/Akt, MAPK | Antioxidants may promote or inhibit depending on context [31] |
| Resisting Cell Death | Upregulated antioxidant systems prevent ROS-mediated apoptosis [31] [37] | Nrf2, Bcl-2, GPX4, GSH | Pro-oxidant therapies to overwhelm defenses [37] |
| Metabolic Reprogramming | ROS regulate HIF-1α, promote glycolysis; metabolic enzymes produce ROS [31] | PKM2, IDH, HIF-1α | Targeting metabolic antioxidant generation (NADPH) [31] |
| Therapy Resistance | Enhanced antioxidant capacity; redox-regulated drug efflux [37] | Nrf2, MRP1, BCRP, MDR1 | Inhibiting antioxidant systems or targeting specific cysteine residues [37] |
The NRF2 pathway demonstrates context-dependent duality in cancer: it prevents carcinogenesis during initiation but promotes tumor progression and therapy resistance once cancer is established [31]. Cancer cells frequently exhibit NRF2 hyperactivation through various mechanisms, including KEAP1 mutations, disrupting the KEAP1-NRF2 interaction, and increased NRF2 transcription [31]. This leads to constitutive expression of antioxidant and detoxification genes that protect cancer cells from oxidative stress and chemotherapeutic agents.
Cancer cells develop multiple redox-dependent resistance mechanisms:
- Altered drug efflux: ROS modify cysteine residues in ABC transporters (MDR1, MRP1, BCRP), affecting their conformation and function [37]
- Enhanced DNA repair: Redox regulation of DNA repair proteins like ATM allows cancer cells to withstand genotoxic stress [15]
- Maintained stemness: CSCs utilize sophisticated antioxidant systems (elevated SOD2, Nrf2 activation) to maintain low ROS and resist therapy [29]
- Metabolic adaptation: Increased pentose phosphate pathway flux generates NADPH to support antioxidant systems [29] [31]
Experimental Assessment Methodologies
Protocol 5: Evaluating NRF2 Activation and Antioxidant Response
- Cell Treatment: Treat cancer cells with NRF2 inducers (sulforaphane, CDDO-Me) or chemotherapeutic agents
- Nuclear/Cytoplasmic Fractionation: Use commercial kits to separate fractions; verify purity with Lamin B1 (nuclear) and GAPDH (cytosolic)
- Western Blotting: Probe with anti-NRF2 antibody (1:1000); quantify nuclear:cytoplasmic ratio
- Gene Expression: Extract RNA, reverse transcribe, perform qPCR for NRF2 targets (NQO1, HO-1, GCLC)
- ARE Reporter Assay: Transfert cells with ARE-luciferase construct; measure luminescence after treatments [31] [37]
Protocol 6: Measuring Glutathione Dynamics in Cancer Cells
- Cell Lysis: Lyse cells in ice-cold PBS with 1% Triton X-100, 0.6% sulfosalicylic acid
- GSH/GSSG Separation: Use commercial GSH/GSSG extraction kits to acidify and stabilize thiols
- Derivatization: Incubate with o-phthalaldehyde (for GSH) or N-ethylmaleimide followed by NaOH (for GSSG)
- Detection: Fluorescence measurement (excitation/emission: 350nm/420nm)
- Calculation: Generate standard curves for GSH and GSSG; calculate GSH:GSSG ratio [31] [37]
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents for Redox Biology Research
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| ROS Detection Probes | MitoSOX Red, H₂DCFDA, Amplex Red | Specific detection of mitochondrial superoxide, general cellular ROS, and extracellular H₂O₂ | Concentration optimization crucial; validate with appropriate controls [33] [30] |
| Antioxidant Response Assays | ARE-luciferase reporters, NRF2 antibodies, KEAP1 mutants | Monitor NRF2 pathway activation, protein localization, and interaction studies | Include both nuclear and cytoplasmic fractions for localization studies [31] [15] |
| Thiol Modification Tools | Biotin-switch assays, dimedone-based probes, mass spectrometry | Detect specific oxidative PTMs: S-nitrosylation, sulfenic acids, comprehensive redox proteomics | Preserve labile modifications during sample preparation [33] [30] |
| Mitochondrial Function Assays | Seahorse XF Analyzer kits, JC-1, MitoTracker | Measure OCR, ECAR, membrane potential, and mass | Correlate with ROS measurements for comprehensive assessment [32] [30] |
| Genetic Manipulation Tools | NRF2 siRNA/shRNA, NOX isoform inhibitors, SOD mimetics | Pathway perturbation studies, target validation | Consider compensatory mechanisms in knockout models [31] [37] |
The transition from redox homeodynamics to dyshomeostasis represents a fundamental pathological shift across cardiovascular, neurodegenerative, and neoplastic diseases. While the specific manifestations differ, shared mechanisms include mitochondrial dysfunction, dysregulated NRF2 signaling, and altered redox-sensitive pathways. The intricate duality of ROS—as both essential signaling molecules and damaging agents—demands precisely targeted therapeutic approaches rather than broad antioxidant interventions. Future research must focus on developing disease-specific redox modulators that account for the dynamic, context-dependent nature of redox biology, with particular attention to the timing of intervention and personalized redox profiling. The integrated experimental approaches and comparative analysis presented here provide a framework for advancing these therapeutic strategies.
Quantifying the Flux: Biomarkers and Models for Assessing Redox Homeodynamics
The conceptual framework for understanding the biological redox environment has evolved significantly from a static notion of redox homeostasis to a dynamic, adaptive model of redox homeodynamics [3]. This paradigm shift acknowledges that redox states are not fixed but are continuously modulated within a physiological range, facilitating crucial signaling processes. The redox code constitutes a set of principles that govern how redox reactions organize biological systems, involving the compartmentalized management of NADPH systems, dynamic thiol switches, and structured oxidant production [15]. Under physiological conditions, reactive oxygen species (ROS) and reactive nitrogen species (RNS) generated by mitochondrial respiration, NADPH oxidases (NOX), and other systems function as signaling molecules that regulate processes from cell proliferation to immune response [15] [38]. The balance between oxidant generation and the antioxidant system—comprising enzymes like superoxide dismutase (SOD), catalase (CAT), glutathione peroxidase (GPx), and glutathione reductase (GR), as well as non-enzymatic antioxidants like glutathione (GSH)—maintains this dynamic equilibrium [15] [39].
When this delicate balance is disrupted, oxidative stress occurs, leading to molecular damage that propagates disease pathogenesis. Oxidative stress is implicated in a vast spectrum of pathological conditions, including COVID-19 severity [40] [41], neurodegenerative diseases [42] [38], cardiovascular disorders [43], and metabolic syndromes. The measurement of specific systemic redox biomarkers—particularly protein carbonyls, the GSH/GSSG ratio, and key antioxidant enzyme activities—provides critical insights into oxidative damage levels, redox regulation capacity, and disease progression. These biomarkers serve not only as diagnostic tools but also as prognostic indicators and potential targets for therapeutic intervention within the framework of precision medicine [41] [43].
Core Biomarker Systems: Mechanisms and Physiological Significance
Protein Carbonyls as Biomarkers of Protein Oxidation
Protein carbonyls represent a stable and widespread marker of protein oxidation formed through multiple mechanisms: direct metal-catalyzed oxidation of side chains (especially lysine, arginine, proline, and threonine), cleavage by the α-amylase pathway, or secondary reaction with reactive carbonyl derivatives from lipid peroxidation (e.g., 4-hydroxynonenal (4-HNE) and malondialdehyde (MDA)) [41]. Their accumulation indicates irreversible oxidative damage to proteins, often leading to loss of enzymatic function, protein aggregation, and impaired cellular function. In COVID-19 patients, elevated levels of protein oxidation markers, including advanced glycation end products (AGEs) and advanced oxidation protein products (AOPP), strongly correlate with disease severity, with AGEs demonstrating exceptional diagnostic power (AUC=0.997) for differentiating patients from healthy controls [41].
The GSH/GSSG Ratio: A Central Metabolic Redox Couple
The glutathione system constitutes one of the most crucial redox buffers in biological systems. Reduced glutathione (GSH), a tripeptide thiol, serves as a primary non-enzymatic antioxidant, directly neutralizing ROS and acting as an essential cofactor for glutathione peroxidase (GPx) and glutathione S-transferase (GST). During its antioxidant function, GSH is oxidized to glutathione disulfide (GSSG). The GSH/GSSG ratio thus provides a sensitive indicator of the cellular redox state, with a decreased ratio signifying oxidative stress [40] [39]. Research has consistently demonstrated that COVID-19 patients exhibit significantly depleted GSH levels alongside elevated GSSG, indicating a compromised antioxidant capacity that correlates with increased mortality risk (p=0.008) and more severe disease progression [40]. Furthermore, genetic polymorphisms in glutathione metabolism enzymes (e.g., GST) can influence individual susceptibility to severe outcomes from oxidative stress conditions [44].
Antioxidant Enzyme Activities: The First Line of Defense
The major enzymatic antioxidants work in concert to neutralize reactive species and maintain redox homeodynamics:
- Superoxide Dismutase (SOD): Catalyzes the dismutation of superoxide anion (O₂•⁻) to hydrogen peroxide (H₂O₂) and oxygen. The three isoforms are compartmentalized: SOD1 (Cu/Zn-SOD) in the cytosol and mitochondrial intermembrane space, SOD2 (Mn-SOD) in the mitochondrial matrix, and SOD3 (EC-SOD) in the extracellular space [38].
- Catalase (CAT): Located primarily in peroxisomes, it catalyzes the conversion of H₂O₂ to water and oxygen, serving as a high-capacity H₂O₂ removal system [41].
- Glutathione Peroxidase (GPx): Utilizes GSH to reduce H₂O₂ and lipid hydroperoxides to water and corresponding alcohols, thereby preventing lipid peroxidation chain reactions [15].
- Glutathione Reductase (GR): Regenerates GSH from GSSG using NADPH as a reducing equivalent, maintaining the reduced glutathione pool essential for antioxidant defense [41].
In pathological states, the activities of these enzymes are characteristically altered. For instance, COVID-19 patients demonstrate significantly increased GR and GST activity alongside decreased total antioxidant capacity (TAC), reflecting a compensatory, yet insufficient, response to heightened oxidative stress [40] [41].
Table 1: Major Systemic Redox Biomarkers and Their Clinical Significance
| Biomarker Category | Specific Marker | Physiological Role | Alteration in Disease | Associated Conditions |
|---|---|---|---|---|
| Protein Oxidation | Protein Carbonyls | Irreversible protein modification | ↑ Significantly increased | COVID-19 severity [41], Neurodegeneration [38] |
| AGEs | Protein adducts from glycoxidation | ↑ Significantly increased | COVID-19 (AUC=0.997) [41], Diabetes | |
| AOPP | Chlorinated protein products | ↑ Significantly increased | COVID-19, Chronic inflammation [41] | |
| Thiol Redox State | GSH/GSSG Ratio | Major redox buffer ratio | ↓ Decreased | COVID-19 mortality (p=0.008) [40] |
| Reduced GSH | Primary non-enzymatic antioxidant | ↓ Depleted | Severe COVID-19 [40], Aging | |
| GSSG | Oxidized glutathione | ↑ Increased | COVID-19 [40] | |
| Antioxidant Enzymes | SOD | Superoxide radical dismutation | ↓ Decreased/Inconsistent | Neurodegeneration, COVID-19 [44] |
| Catalase | H₂O₂ decomposition | ↓ Decreased/Inconsistent | COVID-19 [41] | |
| GPx | H₂O₂ & lipid peroxide reduction | ↓ Decreased | COVID-19 severity [44] | |
| GR | GSSG reduction to GSH | ↑ Increased | COVID-19 [41] | |
| GST | Xenobiotic detoxification | ↑ Increased | COVID-19 (p=0.046) [40] | |
| Lipid Peroxidation | MDA (Malondialdehyde) | Lipid peroxidation end product | ↑ Significantly increased | COVID-19, CVD [41] [43] |
| 4-HNE (4-Hydroxynonenal) | Reactive aldehyde from lipid peroxidation | ↑ Significantly increased | COVID-19, Neurodegeneration [41] [38] |
Quantitative Biomarker Profiles in Human Studies
The quantitative assessment of redox biomarkers across patient populations provides compelling evidence for their clinical relevance and diagnostic utility. The following table synthesizes key findings from recent clinical studies, particularly in COVID-19, where comprehensive redox profiling has been conducted.
Table 2: Quantitative Redox Biomarker Alterations in Clinical Studies
| Study Population | GSH (μM) | GSSG (μM) | GSH/GSSG Ratio | SOD Activity | GR Activity | GPx Activity | MDA (μM) | Protein Carbonyls (nmol/mg protein) |
|---|---|---|---|---|---|---|---|---|
| Healthy Controls | ~2000-5000 [39] | Maintained low | High (Homeodynamic range) | Normal | Normal | Normal | Low | Low (< baseline) |
| COVID-19 Patients | ↓ Significant decrease (p<0.001) [40] | ↑ Increased | ↓ Disrupted | Inconsistent findings [44] | ↑ Significantly increased (p<0.0001) [41] | ↓ Decreased in severe cases [44] | ↑ Significantly elevated (p<0.0001) [41] | ↑ AGEs, AOPP significantly elevated (p<0.0001) [41] |
| COVID-19 Convalescents | Recovering | Recovering | Partially restored | - | Higher than patients (p<0.0001) [41] | - | ↓ Reduced but still elevated vs controls (p<0.0001) [41] | ↑ AGEs remain elevated (AUC=1.000) [41] |
| Neurodegenerative Disease | ↓ Depleted | ↑ Increased | ↓ Decreased | ↓ Often reduced | Altered | ↓ Reduced | ↑ Elevated in CSF/serum [42] [38] | ↑ Elevated in brain tissue/plasma [38] |
| Cardiovascular Disease | ↓ Depleted | ↑ Increased | ↓ Decreased | ↓ Reduced in heart failure | Altered | ↓ Reduced | ↑ Elevated in serum [43] | ↑ Protein oxidation products increased |
Experimental Protocols for Redox Biomarker Assessment
Spectrophotometric Measurement of GSH and GSSG
Principle: This method exploits the reaction of GSH with 5,5'-dithio-bis-(2-nitrobenzoic acid) (DTNB, Ellman's reagent) to produce 2-nitro-5-thiobenzoic acid (TNB), which can be measured spectrophotometrically at 412 nm. For separate GSH/GSSG quantification, GSSG is measured after derivatization of GSH with 2-vinylpyridine [40] [41].
Detailed Protocol:
- Sample Preparation: Collect venous blood in EDTA tubes. Centrifuge at 4000 × g for 10 minutes at 4°C to separate plasma and erythrocytes. Erythrocytes are lysed for intracellular measurement. Precipitate proteins with 5-10% metaphosphoric acid or perchloric acid, then centrifuge to obtain deproteinized supernatant [41].
- Total Glutathione (GSH+GSSG) Assay:
- Prepare reaction mixture: 0.1 M phosphate buffer (pH 7.4), 1 mM EDTA, 0.3 mM DTNB, 0.4 U/mL GR, 0.2 mM NADPH.
- Add deproteinized sample to the reaction mixture.
- Monitor absorbance at 412 nm for 3-5 minutes. The rate of TNB formation is proportional to total glutathione concentration.
- Calculate concentration using a standard curve of GSH (0-40 μM).
- GSSG-Specific Assay:
- Incubate deproteinized supernatant with 2-vinylpyridine (0.5-2%) for 1 hour to derivative GSH.
- Proceed with the DTNB assay as above. The measured glutathione represents GSSG content.
- GSH Calculation: Subtract GSSG value from total glutathione and multiply by 2 to obtain GSH concentration.
- Quality Control: Run samples in duplicate, include internal controls, and standardize to total protein content (determined by BCA assay) [41].
DNPH-Based Spectrophotometric Assay for Protein Carbonyls
Principle: Protein carbonyl groups react with 2,4-dinitrophenylhydrazine (DNPH) to form stable dinitrophenylhydrazone derivatives, which can be quantified by spectrophotometry at 370-375 nm [41] [38].
Detailed Protocol:
- Protein Precipitation: Aliquot serum or plasma samples (100-200 μL) into two tubes. Precipitate proteins with 20% trichloroacetic acid (TCA, final concentration 10%) and centrifuge at 10,000 × g for 5 minutes.
- Derivatization:
- Resuspend one pellet in 500 μL of 0.2% (w/v) DNPH in 2M HCl.
- Resuspend the second pellet (control) in 500 μL of 2M HCl only.
- Incubate both tubes in the dark for 1 hour with intermittent vortexing.
- Washing: Precipitate proteins with 10% TCA, wash pellet 3 times with ethanol:ethyl acetate (1:1 v/v) to remove free DNPH.
- Solubilization and Measurement: Dissolve final pellet in 500-1000 μL of 6M guanidine hydrochloride (pH 2.3) with gentle shaking at 37°C for 15 minutes. Centrifuge to remove insoluble material.
- Spectrophotometric Analysis: Measure absorbance of the DNPH-treated sample against the HCl control at 370-375 nm.
- Calculation: Use the molar extinction coefficient of 22,000 M⁻¹cm⁻¹ to calculate carbonyl content. Express results as nmol carbonyl groups per mg of total protein [41].
Enzymatic Activity Assays for Antioxidant Enzymes
Glutathione Reductase (GR) Activity:
- Principle: GR catalyzes the reduction of GSSG to GSH using NADPH, which is oxidized to NADP⁺. The decrease in absorbance of NADPH at 340 nm is monitored.
- Protocol: Prepare reaction mixture: 0.1 M potassium phosphate buffer (pH 7.4), 1 mM EDTA, 1 mM GSSG, 0.1 mM NADPH. Add sample and monitor absorbance at 340 nm for 3-5 minutes. One unit of activity is defined as the amount of enzyme that oxidizes 1 μmol NADPH per minute [41].
Superoxide Dismutase (SOD) Activity:
- Principle: SOD inhibits the autoxidation of adrenaline to adrenochrome at alkaline pH, measured at 480 nm.
- Protocol: Add sample to 0.05 M carbonate buffer (pH 10.2) with 0.1 mM EDTA. Initiate reaction with 0.3 mM adrenaline. Monitor increase in absorbance at 480 nm for 3-4 minutes. One unit is defined as the amount of enzyme causing 50% inhibition of adrenaline autoxidation [41].
Catalase (CAT) Activity:
- Principle: CAT decomposes H₂O₂, which can be monitored by the decrease in absorbance at 240 nm.
- Protocol: Add sample to 50 mM phosphate buffer (pH 7.0) containing 10-20 mM H₂O₂. Monitor decrease in absorbance at 240 nm for 1-2 minutes. Calculate activity using the molar extinction coefficient of 43.6 M⁻¹cm⁻¹ [41].
Redox Signaling Pathways and Experimental Workflows
Redox Homeodynamics Signaling Network
Redox Homeodynamics Signaling Network: This diagram illustrates the core regulatory circuit maintaining redox balance. Oxidative triggers modify KEAP1, leading to NRF2 release and translocation to the nucleus. NRF2 binds to the Antioxidant Response Element (ARE), activating transcription of antioxidant genes. The resulting antioxidant proteins neutralize oxidants, completing the feedback loop that maintains redox homeodynamics [15].
Systemic Redox Biomarker Analysis Workflow
Systemic Redox Biomarker Analysis Workflow: This workflow outlines the standardized procedure for comprehensive redox profiling. Blood collection is followed by appropriate sample processing for different biomarker classes. Protein carbonyls are measured in plasma/serum, glutathione species require deproteinized extracts, and enzyme activities are typically determined in erythrocyte lysates. Data integration from all assays provides a complete assessment of systemic redox status [40] [41].
Biomarker Interrelationships in Disease Pathogenesis
Biomarker Interrelationships in Disease Pathogenesis: This diagram illustrates the vicious cycle of oxidative damage in disease. Initial oxidative stress simultaneously elevates multiple biomarkers of damage (protein carbonyls, lipid peroxides) while depleting protective systems (GSH). The resulting tissue damage triggers inflammation, which generates further oxidative stress, creating a self-perpetuating cycle that drives disease progression [41] [38] [43].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Redox Biomarker Analysis
| Reagent/Material | Application | Function | Example Specifications |
|---|---|---|---|
| DTNB (Ellman's Reagent) | GSH/GSSG assay | Thiol-reactive compound forming colored TNB | ≥99% purity, in ethanol or DMSO [41] |
| NADPH | GR assay, Total glutathione assay | Enzymatic cofactor for reduction reactions | ≥97% purity, lyophilized powder [41] |
| 2,4-Dinitrophenylhydrazine (DNPH) | Protein carbonyl assay | Derivatization of carbonyl groups | ~200 mM in 2M HCl, protect from light [41] |
| Guanidine HCl | Protein carbonyl assay | Protein denaturant for carbonyl solubilization | ≥99% purity, 6M solution [41] |
| 2-Vinylpyridine | GSSG-specific assay | Derivatization of GSH for selective GSSG measurement | ≥95% purity, under nitrogen atmosphere [41] |
| Glutathione Reductase (Enzyme) | Total glutathione assay | Enzymatic recycling of GSSG to GSH | ≥100 U/mg protein from yeast or human [41] |
| Superoxide Dismutase Standard | SOD activity assay | Reference enzyme for standardization | Human erythrocyte SOD, ≥3,000 U/mg [41] |
| Catalase Standard | CAT activity assay | Reference enzyme for standardization | Bovine liver catalase, ≥30,000 U/mg [41] |
| BCA Protein Assay Kit | All assays | Total protein quantification for normalization | Compatible with guanidine HCl [41] |
| EDTA-containing Tubes | Blood collection | Chelates metals to prevent artificial oxidation | Lavender-top K3 EDTA tubes [40] |
| Proteinase Inhibitors | Sample preparation | Prevents protein degradation during processing | Complete protease inhibitor cocktails [40] |
The comprehensive assessment of systemic redox biomarkers—protein carbonyls, GSH/GSSG ratio, and antioxidant enzyme activities—provides powerful insights into the disruption of redox homeodynamics across numerous pathological conditions. The quantitative data and standardized methodologies presented herein establish robust frameworks for investigating oxidative stress mechanisms in human disease. As we advance into the era of precision medicine, integrating these biomarker panels with multi-omics approaches and clinical parameters will enable unprecedented patient stratification and targeted therapeutic interventions. Future directions will likely focus on establishing standardized reference ranges, developing point-of-care testing platforms, and validating redox biomarker-guided treatments that can restore the delicate balance of redox homeodynamics for improved clinical outcomes.
This technical guide explores the critical roles of the transcription factors Nuclear Factor Erythroid 2–Related Factor 2 (Nrf2) and Peroxisome Proliferator-Activated Receptor Gamma Coactivator 1-Alpha (PGC-1α) as biomarkers for assessing redox stress. Moving beyond the classical concept of static redox homeostasis, we frame their function within the modern paradigm of redox homeodynamics—a dynamic, adaptive process essential for cellular health. The document provides an in-depth analysis of the signaling pathways governed by these biomarkers, summarizes quantitative approaches for their measurement, and offers detailed experimental protocols. Aimed at researchers and drug development professionals, this review also includes key visualization tools and a catalog of essential research reagents to facilitate the investigation of Nrf2 and PGC-1α in the context of redox-related diseases.
The traditional view of redox homeostasis implies a static steady-state balance between reactive oxygen species (ROS) and antioxidants. However, contemporary understanding emphasizes redox homeodynamics, which recognizes the continuous, dynamic flux and adaptive reprogramming of redox systems to maintain stability [14] [45]. This dynamic equilibrium is maintained through constant redox sensing, signal transduction, and subsequent activation of cellular stress responses [45].
Within this framework, transcriptional biomarkers serve as crucial indicators of a cell's redox status and adaptive capacity. Among these, Nrf2 and PGC-1α have emerged as master regulators that orchestrate the expression of vast gene networks in response to redox challenges [46] [28]. Their coordinated action allows the cell to fine-tune its antioxidant defenses, manage inflammatory responses, and regulate mitochondrial biogenesis and function, making them indispensable sensors of redox homeodynamics.
Molecular Foundations of Nrf2 and PGC-1α
The Nrf2 Signaling Pathway
Nrf2 is a transcription factor belonging to the Cap'n'Collar (CNC) subfamily of basic leucine zipper (bZip) proteins. It is the principal regulator of cytoprotective gene expression in response to oxidative and electrophilic stress [47].
- Regulation by Keap1: Under basal conditions, Nrf2 is sequestered in the cytoplasm by its repressor protein, Kelch-like ECH-associated protein 1 (Keap1). Keap1 acts as a substrate adaptor for a Cullin 3 (CUL3)-based E3 ubiquitin ligase complex, which continuously targets Nrf2 for proteasomal degradation, thereby maintaining low cellular levels of Nrf2 [46] [48].
- Activation by Stress: Upon oxidative stress, specific cysteine residues within Keap1 become modified, leading to a conformational change that disrupts its ability to target Nrf2 for degradation. This results in Nrf2 stabilization and accumulation [46].
- Nuclear Translocation and ARE Binding: Stabilized Nrf2 translocates to the nucleus, where it heterodimerizes with small musculoaponeurotic fibrosarcoma (sMaf) proteins. The heterodimer binds to the Antioxidant Response Element (ARE)—a specific DNA sequence—in the promoter regions of its target genes, initiating their transcription [46] [48].
- Target Genes: Nrf2 activation leads to the upregulation of a vast array of genes involved in:
- Antioxidant Defense: Heme oxygenase-1 (HO-1), NAD(P)H quinone dehydrogenase 1 (NQO1), glutamate-cysteine ligase catalytic (GCLC) and modifier (GCLM) subunits [46] [49].
- Detoxification: Glutathione S-transferases (GSTs) [49].
- Proteostasis: Proteasome subunits [48].
- Iron Metabolism: Ferritin heavy and light chains [48].
The PGC-1α Signaling Pathway
PGC-1α is a transcriptional coactivator that serves as a master regulator of mitochondrial biogenesis and energy metabolism, acting as a central node integrating multiple signaling pathways [28].
- Transcriptional Regulation: The PPARGC1A gene encoding PGC-1α is regulated by several transcription factors. cAMP Response Element-Binding Protein (CREB) is a major activator, particularly in response to β-adrenergic signaling and increased cAMP levels. Myocyte Enhancer Factor 2 (MEF2) and Activating Transcription Factor 2 (ATF2), activated by p38 MAPK, also drive PGC-1α expression [28].
- Post-Translational Modifications: The activity and stability of PGC-1α are heavily regulated by post-translational modifications:
- Activation: AMP-activated protein kinase (AMPK) and p38 MAPK phosphorylate PGC-1α, enhancing its transcriptional activity. Furthermore, deacetylation by the NAD+-dependent deacetylase SIRT1 activates PGC-1α, linking its function to cellular energy status [28].
- Inhibition: Acetylation by GCN5 and phosphorylation by Glycogen Synthase Kinase 3β (GSK3β) inhibit PGC-1α and promote its degradation [28].
- Downstream Functions: Activated PGC-1α co-activates several transcription factors, including:
- Nuclear Respiratory Factor 1 (NRF1) and Nuclear Respiratory Factor 2 (NRF2/GABP): These factors control the expression of nuclear-encoded mitochondrial proteins and key components of the mitochondrial transcription and replication machinery, such as Transcription Factor A, Mitochondrial (TFAM) [28].
- Estrogen-Related Receptors (ERRs) and Peroxisome Proliferator-Activated Receptors (PPARs): These regulate fatty acid oxidation and oxidative phosphorylation [28].
Nrf2 and PGC-1α Crosstalk
Emerging evidence indicates significant crosstalk between the Nrf2 and PGC-1α pathways, forming a coordinated defense network. Some studies suggest that Nrf2 can directly influence the expression of PPARGC1A (PGC-1α), while PGC-1α may also contribute to the regulation of certain antioxidant genes [28]. This interaction creates a positive feedback loop that amplifies the mitochondrial antioxidant response, ensuring that increased energy production is matched with enhanced ROS detoxification capacity [28]. This crosstalk exemplifies the integrative nature of redox homeodynamics.
The following diagram illustrates the core signaling pathways and key regulatory interactions for Nrf2 and PGC-1α.
Quantitative Biomarker Profiles in Disease States
The expression and activity of Nrf2 and PGC-1α are dynamically altered in various pathological conditions, reflecting the underlying redox stress. The following tables summarize key quantitative findings from clinical and preclinical studies.
Table 1: Biomarker Alterations in Neurodegenerative Diseases
| Disease Model | Nrf2 Level/Activity | PGC-1α Level/Activity | Observed Molecular Consequences | Citation |
|---|---|---|---|---|
| Parkinson's Disease (PD) Human Monocytes | Decreased with disease burden | Decreased with disease burden | Increased inflammation (IL-6, IL-1β); Mitochondrial dysregulation [50] | |
| PD Post-Mortem Brain Tissue | Reduced NRF2 binding activity in Substantia Nigra | N/A | Loss of dopaminergic neurons; Increased oxidative damage [48] | |
| Alzheimer's Disease (AD) Models | Dysregulated | Implicated in dysfunction | Elevated oxidative stress; Impaired mitochondrial function [46] [47] | |
| Ischemic Preconditioning (Model of neuroprotection) | Activated | Associated with pathway | Enhanced antioxidant defense; Improved mitochondrial function & neuronal survival [46] |
Table 2: Experimental Model Findings Highlighting Nrf2/PGC-1α Interdependence
| Experimental Context | Nrf1/Nrf2 Status | PGC-1α & Mitochondrial Status | Key Findings | Citation |
|---|---|---|---|---|
| Nrf1α-/- Cells (HepG2) | Nrf1 knocked out; Nrf2 hyperactive | Glycolysis enhanced; Mitochondrial ETC impaired & ROS increased | Loss of Nrf1 caused severe oxidative stress not rescued by Nrf2; Demonstrates Nrf1's vital role in mitochondrial homeostasis [49] | |
| Nrf2-/- Models | Nrf2 knocked out | Impaired mitochondrial biogenesis | Confirms Nrf2's role in regulating basal levels of mitochondrial proteins and antioxidants [28] | |
| SIRT1 Modulation | Interacts with & deacetylates Nrf2 | Activated by SIRT1 via deacetylation | SIRT1-Nrf2 crosstalk enhances antioxidant response and mitochondrial function [46] |
Experimental Protocols for Biomarker Assessment
This section provides detailed methodologies for evaluating Nrf2 and PGC-1α activity and downstream effects in cellular and animal models.
Protocol: Assessing Nrf2 Nuclear Translocation by Immunofluorescence
Objective: To visualize and quantify the stress-induced translocation of Nrf2 from the cytoplasm to the nucleus.
Cell Seeding and Treatment:
- Seed cells (e.g., SH-SY5Y, PC12) on sterile, poly-L-lysine-coated glass coverslips in a culture plate.
- Allow cells to adhere overnight (~70% confluence).
- Treat cells with an Nrf2 inducer (e.g., 10-50 µM Sulforaphane (SFN), 10-50 µM Dimethyl Fumarate (DMF)) or a vehicle control (DMSO) for a predetermined time (e.g., 2-6 hours).
Fixation and Permeabilization:
- Aspirate media and wash cells gently with 1X Phosphate Buffered Saline (PBS).
- Fix cells with 4% paraformaldehyde in PBS for 15 minutes at room temperature.
- Wash 3x with PBS.
- Permeabilize cells with 0.1% Triton X-100 in PBS for 10 minutes.
- Wash 3x with PBS.
Blocking and Immunostaining:
- Incubate cells in blocking buffer (e.g., 5% Normal Goat Serum in PBS) for 1 hour to reduce non-specific binding.
- Incubate with primary antibody against Nrf2 (e.g., Rabbit anti-Nrf2) diluted in blocking buffer overnight at 4°C.
- Wash 3x with PBS.
- Incubate with a fluorophore-conjugated secondary antibody (e.g., Alexa Fluor 488 Goat Anti-Rabbit IgG) and a nuclear counterstain (e.g., DAPI) for 1 hour at room temperature in the dark.
- Wash 3x with PBS.
Mounting and Imaging:
- Mount coverslips onto glass slides using an anti-fade mounting medium.
- Acquire high-resolution images using a confocal or fluorescence microscope.
- Quantification: Using image analysis software (e.g., ImageJ), calculate the nuclear-to-cytoplasmic fluorescence ratio of Nrf2 signal for at least 50 cells per condition. A significant increase in this ratio indicates Nrf2 activation.
Protocol: Measuring ARE-Dependent Gene Expression via qRT-PCR
Objective: To quantitatively measure the mRNA levels of classic Nrf2 target genes as a functional readout of its transcriptional activity.
RNA Extraction:
- Lyse control or treated cells in TRIzol reagent or using a commercial column-based RNA extraction kit.
- Treat samples with DNase I to remove genomic DNA contamination.
- Quantify RNA concentration and purity using a spectrophotometer.
cDNA Synthesis:
- Reverse transcribe 0.5-1 µg of total RNA into cDNA using a Reverse Transcription kit with random hexamers and/or oligo(dT) primers.
Quantitative Real-Time PCR (qRT-PCR):
- Prepare PCR reactions containing cDNA template, SYBR Green Master Mix, and gene-specific forward and reverse primers.
- Key Target Genes: HMOX1 (HO-1), NQO1, GCLC.
- Reference Genes: ACTB (β-Actin), GAPDH, HPRT1.
- Run the reaction in a real-time PCR cycler with the following typical cycling conditions: 95°C for 10 min (initial denaturation), followed by 40 cycles of 95°C for 15 sec and 60°C for 1 min.
- Perform all reactions in technical triplicates.
Data Analysis:
- Calculate the cycle threshold (Ct) values for each reaction.
- Normalize the Ct of the target gene to the Ct of the reference gene(s) (∆Ct).
- Calculate the fold change in gene expression relative to the control group using the 2^(-∆∆Ct) method.
Protocol: Evaluating Mitochondrial Biogenesis via PGC-1α Activity
Objective: To assess PGC-1α function by measuring the expression of its downstream effector, TFAM, and mitochondrial DNA (mtDNA) content.
Protein Analysis of TFAM:
- Extract total protein from cells or tissue homogenates.
- Perform Western blotting using antibodies against TFAM and a loading control (e.g., Vinculin, COX IV).
- Quantify band intensity to determine TFAM protein levels.
mtDNA Quantification by qPCR:
- Extract total DNA (nuclear and mitochondrial) from samples.
- Design qPCR primers to amplify a conserved region of the mitochondrial genome (e.g., MT-ND1) and a single-copy nuclear gene (e.g., 18S rRNA or β-globin).
- Perform qPCR on both mitochondrial and nuclear targets using the same DNA sample.
- The relative mtDNA copy number is calculated as the ratio of the mitochondrial gene signal to the nuclear gene signal (mtDNA/nDNA).
The workflow for this multi-faceted assessment is summarized below.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for Investigating Nrf2 and PGC-1α Pathways
| Reagent Category | Specific Examples | Function & Application in Research | Key Considerations |
|---|---|---|---|
| NRF2 Inducers | Sulforaphane (SFN), Dimethyl Fumarate (DMF), CDDO-Me (Bardoxolone methyl) | Activate Nrf2 by modifying KEAP1 cysteine residues. Used to study antioxidant responses and potential therapeutics. | Specificity; high concentrations may have off-target effects. DMF is an approved drug for MS. |
| PGC-1α Activators | Resveratrol (activates SIRT1), AICAR (AMPK activator), Bezafibrate (PPAR pan-agonist) | Indirectly activate PGC-1α via upstream kinases (AMPK) or deacetylases (SIRT1). Used to induce mitochondrial biogenesis. | Resveratrol has multiple cellular targets. Effects are often context and dose-dependent. |
| Genetic Tools | siRNA/shRNA (for NFE2L2, PPARGC1A, KEAP1), CRISPR/Cas9 Knockout Cells (e.g., Nrf2-/-), Overexpression Plasmids | To knock down or knock out genes to study loss-of-function phenotypes, or overexpress to study gain-of-function. | Essential for establishing causal relationships. Validation of knockout efficiency is critical. |
| Key Antibodies | Anti-Nrf2 (for WB, IF, ChIP), Anti-PGC-1α, Anti-Keap1, Anti-HO-1, Anti-NQO1, Anti-TFAM | For protein quantification (Western Blot), cellular localization (Immunofluorescence), and binding studies (ChIP). | Check species reactivity and application-specific validation. |
| Cell Lines | SH-SY5Y (human neuroblastoma), PC12 (rat pheochromocytoma), HepG2 (human hepatoma), Primary Neurons/Astrocytes | Model systems for studying redox biology in neurologically relevant and other contexts. | Primary cells are more physiologically relevant but have limited lifespan. |
| Animal Models | Nfe2l2-/- (Nrf2 knockout) mice, Ppargc1a-/- (PGC-1α knockout) mice, Toxin-induced models (e.g., MPTP for PD) | In vivo models for studying the systemic role of these pathways in disease and protection. | Nrf2-/- mice are viable but more susceptible to oxidative stress. |
The integration of Nrf2 and PGC-1α as transcriptional biomarkers provides a powerful, multi-faceted lens through which to assess the dynamic state of cellular redox signaling. Their coordinated analysis moves research beyond a simple snapshot of oxidative damage and towards a functional understanding of the cell's adaptive capacity. The experimental frameworks and tools detailed in this guide will aid researchers in quantifying these biomarkers accurately.
Future research must focus on several key areas:
- Dynamic Imaging: Developing and utilizing genetically encoded biosensors to monitor Nrf2 and PGC-1α activity in real-time within living cells and organisms.
- Cell-Type Specificity: Understanding how the crosstalk between these pathways differs across various cell types in complex tissues, particularly the brain.
- Therapeutic Translation: Designing and testing novel therapeutics or lifestyle interventions that can precisely modulate this Nrf2/PGC-1α axis to restore redox homeodynamics in chronic diseases like Parkinson's, Alzheimer's, and metabolic disorders.
By leveraging Nrf2 and PGC-1α as indicators, scientists can decode the complex language of redox stress, paving the way for innovative strategies to diagnose, monitor, and treat a wide spectrum of redox-related diseases.
The traditional view of redox homeostasis—a static steady-state balance between oxidants and antioxidants—is being superseded by the more dynamic concept of redox homeodynamics [51]. This paradigm shift recognizes that redox processes are part of a continuous, adaptive signaling system that can be smoothly modulated rather than merely switched on or off [3]. Biological systems maintain a "nucleophilic tone" through continuous feedback mechanisms that preserve physiological function despite constant challenges [3]. This fine-tuned equilibrium involves specific reactive oxygen species (ROS), particularly hydrogen peroxide (H2O2), which at low concentrations (1–10 nM) act as fundamental coordinators of cell signaling—a state termed oxidative eustress ("good stress") [52]. Only when this dynamic balance is overwhelmed does oxidative distress occur, leading to potential damage [52]. The principles governing this biological redox organization are collectively termed the 'redox code' [51], which requires advanced analytical technologies to decipher its complexity. Understanding these dynamics is crucial, as dysregulation is associated with ageing and numerous diseases, including cardiological and neurodegenerative conditions, and cancer [51].
Advanced Proteomic Techniques for Redox Mapping
Cysteine-Reactive Phosphate Tag (CPT) Technology
Comprehensive analysis of the cysteine redox proteome in living tissues has represented a major technical challenge in redox biology. The Cysteine-reactive Phosphate Tag (CPT) technology represents a transformative advancement, enabling comprehensive and quantitative mapping of reversible cysteine oxidation across the proteome [53]. This method addresses a critical gap: while redox regulation of protein cysteines is implicated in vast arrays of tissue-specific processes, most previous methods failed to measure percent cysteine modification (site occupancy), which is essential for identifying functionally significant regulatory nodes [53].
The CPT workflow involves several critical steps: (1) derivatization of the entire cysteine proteome under denaturing conditions using a reagent containing a non-hydrolyzable phosphate moiety, an iodoacetamide-based cysteine alkylating warhead, and a tunable hydrophobic linker; (2) proteolytic digestion followed by enzymatic removal of endogenous phosphorylation; (3) highly selective enrichment (>99%) of CPT-derivatized cysteine-containing peptides using Immobilized Metal Affinity Chromatography (IMAC); and (4) quantitative analysis via Tandem Mass Tag (TMT)-multiplexed mass spectrometry [53]. This approach allows for simultaneous analysis of five biological replicates in a single experiment, reporting percentage reversible cysteine modification while controlling for changes in protein abundance [53].
The power of this methodology is demonstrated by the Oximouse project, which established a comprehensive and quantitative landscape of the mouse cysteine redox proteome in vivo [53]. This compendium quantified approximately 171,000 individual cysteine sites across ten mouse tissues in young and old mice, corresponding to ~34,000 unique sites across ~9,400 proteins [53]. Remarkably, the oxidation state of over 98% of these sites had not been previously quantified in their corresponding tissues, representing an order-of-magnitude improvement in coverage compared to previous stoichiometric technologies [53].
Oximouse Compendium: Key Findings and Implications
The Oximouse dataset revealed several fundamental paradigms of physiological redox signaling. It established that tissues contain cysteine redox networks that are tissue-selective and underlie tissue-specific biology [53]. This finding is particularly significant as it helps explain how tissues control distinct physiological processes despite sharing substantially overlapping transcriptomes and proteomes.
Unexpectedly, the data demonstrated that aged tissues do not display a global increase in protein oxidation, as previously hypothesized. Instead, a fundamental remodeling of cysteine oxidation networks occurs across all aged tissues, with many of these networks mapping to established disease-relevant protein families [53]. This remodeling represents a systemic molecular basis for the long-proposed links between redox dysregulation and tissue aging.
The dataset also proposed a common mechanism for encoding redox sensitivity through electrostatic gating, where local electrostatic environments control cysteine reactivity [53]. This provides a potential explanatory framework for why specific cysteine residues undergo extensive regulatory oxidation while others do not.
Table 1: Key Quantitative Findings from the Oximouse Compendium
| Parameter | Finding | Significance |
|---|---|---|
| Coverage | ~171,000 cysteine sites quantified across 10 tissues; ~34,000 unique sites on ~9,400 proteins | Over an order of magnitude improvement in coverage vs. previous technologies |
| Tissue Specificity | Tissue-selective cysteine redox networks identified | Explains how specialized physiology emerges from shared proteomes |
| Aging Effect | Network remodeling rather than global oxidation increase | Challenges traditional views of oxidative stress in aging |
| Redox Sensitivity | Electrostatic gating as a mechanism for encoding sensitivity | Provides molecular principles for predicting regulatory cysteine residues |
Complementary Redox Proteomic Methods
Beyond CPT technology, other innovative methods have emerged to address different aspects of redox proteomic analysis. Redox lipidomics and adductomics focus on analyzing oxidized lipids and their covalent adducts with proteins [54]. This is particularly important because lipid peroxidation products can form adducts with cysteine, histidine, and lysine residues, potentially disrupting protein function or creating new signaling modalities [54].
For more accessible, targeted analyses, high-throughput immunoassays have been developed, including the Antibody-Linked Oxi-State Assay (ALISA) and RedoxiFluor assays [52]. These techniques utilize fluorescent-conjugated reporters to label reversibly oxidized thiols in a microplate format, making redox assessment more accessible to laboratories without specialized mass spectrometry capabilities. For instance, ALISA has been successfully used to quantify reversible thiol oxidation in human erythocyte PP2A following maximal exercise [52].
Metabolomic and Imaging Approaches in Redox Biology
Redox Lipidomics and Metabolomics
The field of redox lipidomics has advanced significantly to characterize oxidized lipids that function as active regulators of cellular and physiological functions [54]. Imbalances in controlled production of oxidized lipids have been associated with various types of cell death, immune responses, and chronic inflammation [54]. Advanced mass spectrometry approaches now enable comprehensive analysis of diverse oxidized lipid species, including oxysterols, eicosanoids, and other oxygenated polyunsaturated fatty acids [54].
These methodologies have revealed that oxidized lipids are not merely damage markers but play specific regulatory roles. For example, enzymatic and non-enzymatic oxidation pathways produce distinct stereoisomers with different biological activities, requiring enantioselective analytical methods for proper characterization [54]. The analysis of nitrated lipid derivatives has also gained prominence, as these species are recognized as important mediators in inflammatory processes [54].
Quantitative Redox Imaging
Imaging approaches provide spatial resolution of redox processes within tissues and cells. Dynamic Nuclear Polarization Magnetic Resonance Imaging (DNP-MRI) has been employed with nitroxyl radicals such as tempol as chemical dosimeters to visualize X-ray exposure via redox reactions [55]. In this system, gel phantoms containing glutathione and paramagnetic tempol radical enable monitoring of deposited X-ray irradiation through redox-mediated changes in tempol concentration, which can be quantified via DNP-MRI signal intensity [55].
For live-cell imaging, ratiometric fluorescent reporters such as reduction-oxidation-sensitive Green Fluorescent Protein (roGFP) allow redox imaging with high spatiotemporal resolution [56]. These genetically encoded sensors can be targeted to specific organelles, enabling compartment-specific redox measurements, and can be combined with probes for other physiological parameters for multi-dimensional imaging [56]. Specialized software solutions have been developed to process the large datasets generated by these imaging approaches, providing tools for multi-channel ratio imaging, pixel-population statistics, and object-based ratio analysis [56].
Experimental Protocols and Methodologies
Detailed CPT Experimental Protocol
Tissue Preparation:
- Harvest tissues from experimental models (e.g., C57BL/6J mice) and immediately snap-freeze in liquid nitrogen to preserve in vivo redox states.
- Homogenize tissues under denaturing conditions (e.g., 4% SDS buffer) with complete inhibition of proteolytic and redox enzyme activities.
- Clarify lysates by centrifugation (16,000 × g, 10 min) and quantify protein concentration.
CPT Derivatization:
- Reduce samples with TCEP (1 mM, 10 min, 55°C) to reduce all reversible oxidations.
- Alkylate with CPT reagent (2 mM, 20 min, room temperature in darkness) to derivative all reduced cysteine thiols.
- Remove excess CPT using protein precipitation or spin columns.
Sample Processing for MS:
- Digest proteins with sequencing-grade trypsin/Lys-C (1:50 w/w, 37°C, overnight).
- Dephosphorylate endogenous phosphopeptides using alkaline phosphatase (2 h, 37°C).
- Enrich CPT-labeled peptides using IMAC (Fe³⁺ or Ti⁴⁺-loaded) with >99% specificity.
- Label with TMT reagents (6-plex or 11-plex) according to manufacturer's protocols.
- Pool labeled samples and clean up via C18 solid-phase extraction.
LC-MS/MS Analysis:
- Separate peptides using nano-LC (C18 column, 75 μm × 25 cm, 2 μm particles) with a 120-min gradient (3-30% acetonitrile in 0.1% formic acid).
- Analyze using Orbitrap mass spectrometer (MS1: 120,000 resolution; MS2: 50,000 resolution).
- Fragment peptides using higher-energy collisional dissociation (HCD).
Data Processing:
- Identify peptides and proteins using search engines (MaxQuant, Proteome Discoverer) against appropriate databases.
- Quantify percentage reversible oxidation using TMT reporter ion intensities.
- Normalize data across samples and perform statistical analysis for differential oxidation.
Table 2: Research Reagent Solutions for Redox Proteomics
| Reagent/Tool | Function | Application Notes |
|---|---|---|
| CPT Reagents | Derivatization of cysteine thiols with phosphate tags for IMAC enrichment | Tunable hydrophobicity minimizes peptide loss; enables >72,000 unique cysteine peptide identifications |
| TMT Multiplex Kits | Isobaric labeling for simultaneous quantification of multiple samples | Enables 5-11 plex experiments; controls for protein abundance changes |
| IMAC Materials | Immobilized metal affinity chromatography for phosphopeptide enrichment | >99% enrichment selectivity for CPT-derivatized peptides |
| roGFP Sensors | Genetically encoded redox sensors for live-cell imaging | Ratiometric measurement independent of probe concentration; targetable to organelles |
| ALISA Kits | Microplate-based assessment of specific protein thiol oxidation | Accessible for labs without MS capabilities; validated in human erythrocytes |
The advanced analytical techniques described herein—particularly the CPT-based proteomics embodied in the Oximouse compendium—provide unprecedented insights into the dynamic landscape of redox regulation [53]. These approaches have fundamentally altered our understanding of redox biology, revealing that aging involves specific remodeling of cysteine oxidation networks rather than global oxidative damage, and demonstrating that tissues maintain specialized redox networks that underlie their physiological specificity [53].
The emerging framework of redox homeodynamics provides a more nuanced understanding of how biological systems dynamically maintain redox balance through continuous signaling and feedback mechanisms [51] [3]. This perspective recognizes that electrophiles and nucleophiles are not intrinsically harmful or protective but function as complementary components of a dynamic signaling system that maintains physiological function [3].
Future developments in redox research will likely focus on several key areas: (1) increasing spatial and temporal resolution of redox measurements; (2) integrating multi-omics approaches to connect redox changes to functional outcomes; (3) developing standardized methodologies for clinical translation; and (4) advancing computational models to predict redox network behavior. The concept of the exposome—the cumulative measure of environmental influences and biological responses throughout the lifespan—highlights the importance of understanding how lifelong exposures are communicated to cells through redox signals [51].
As these technologies mature and become more accessible, they will guide novel redox medicine approaches aimed at preventing and treating diseases associated with disturbed redox regulation [51] [52]. By moving beyond simplistic oxidative stress paradigms and embracing the complexity of redox homeodynamics, researchers can develop more targeted interventions that maintain or restore the delicate redox balance essential for health.
The conceptual framework for understanding redox biology in preclinical models has undergone a fundamental shift from the classical concept of redox homeostasis to the more dynamic redox homeodynamics [45]. Homeostasis implies a static, steady-state balance between oxidants and antioxidants, an approach that fails to capture the complex, fluctuating nature of biological redox systems. In contrast, redox homeodynamics recognizes that living systems maintain health through continuous dynamic adjustments, characterized by spatiotemporal redox fluctuations and sophisticated communication networks that allow for adaptive responses to internal and external stimuli [45]. This paradigm shift has profound implications for preclinical model development, as it necessitates approaches that can capture these dynamic redox processes rather than merely measuring static redox states.
The principles of biological redox organization are encapsulated in the "redox code" – a set of organizational principles governing how redox reactions are integrated across biological systems [45]. This code encompasses: (1) the organization of bioenergetics through NADH and NADPH systems operating near equilibrium with metabolic fuels; (2) the linkage of macromolecular structure and function through kinetically controlled sulfur switches in the redox proteome; (3) activation-deactivation cycles of H2O2 production that support spatiotemporal signaling; and (4) redox networks that form adaptive systems from microcompartments to cellular organization [45]. Understanding this code is essential for developing preclinical models that accurately recapitulate human redox biology in health and disease.
Redox Homeodynamics in Physiological and Pathological Processes
Fundamental Mechanisms and Signaling Pathways
Redox homeodynamics operates through sophisticated signaling mechanisms where reactive oxygen species (ROS), particularly hydrogen peroxide (H2O2), function as signaling messengers at physiological concentrations while causing damage at elevated levels [45]. The primary molecular mechanisms involve reversible oxidative modifications of protein cysteine thiols, which act as redox switches to control protein function and cellular signaling pathways [15]. These modifications include disulfide bond formation, S-glutathionylation, S-nitrosylation, and S-sulfenylation, all of which can be reversed by specific cellular reductants [15].
Key transcription factors such as NF-κB and Nrf2 serve as critical sensors and effectors of redox signaling [15] [57]. Under oxidative conditions, NF-κB activates pro-inflammatory gene expression, while Nrf2 dissociates from its inhibitor Keap1 and translocates to the nucleus to activate antioxidant response elements (AREs), driving the expression of cytoprotective genes including heme oxygenase-1 (HO-1) and NAD(P)H quinone dehydrogenase 1 (NQO1) [57]. The interplay between these pathways represents a crucial regulatory node in maintaining redox homeodynamics.
The Exposome and Redox Communication
The exposome – the cumulative measure of environmental influences and associated biological responses throughout the lifespan – communicates with cells primarily through redox signals [58] [45]. Environmental factors including nutrition, chemicals, physical factors, microorganisms, and lifestyle factors continuously modulate redox homeodynamics, influencing disease risk and progression [58]. Preclinical models must therefore incorporate relevant exposomal factors to accurately model human disease, moving beyond genetic manipulation alone to include environmental exposures that disrupt redox networks.
Intercellular and interorgan redox communication occurs through multiple mechanisms, including: (1) transport of H2O2 through peroxiporins; (2) direct movement of oxidants between cells via gap junctions; (3) transmission through the extracellular space; and (4) communication via extracellular vesicles [45]. These communication pathways enable coordinated tissue responses to redox challenges and represent critical components for inclusion in sophisticated preclinical models.
Quantitative Redox Proteomics in Preclinical Models
Experimental Workflow for Redox Proteomic Analysis
Comprehensive assessment of redox homeodynamics in preclinical models requires sophisticated proteomic approaches. The following workflow, adapted from studies of hematopoietic stem and progenitor cells (HSPCs), demonstrates a robust methodology for quantifying redox modifications [59]:
Table 1: Key Steps in Redox Proteomics Workflow
| Step | Procedure | Key Considerations |
|---|---|---|
| Cell Isolation | FACS purification of target cells (e.g., Lineage− Sca-1+ c-Kit+ [LSK] for HSPCs) | Maintain physiological conditions during processing; minimize atmospheric oxygen exposure |
| Thiol Blocking | Sequential labelling with iodoTMT reagents | Use isobaric tags for multiplexing; irreversible covalent modification of reduced cysteine sulfhydryls |
| Reduction and Enrichment | Selective reduction of oxidized thiols followed by affinity enrichment | Achieve >87% enrichment efficiency; maintain specificity for cysteine residues |
| Mass Spectrometry | NanoLC-MS3 analysis on 20μg protein samples | Use high-resolution instrumentation; implement MS3 for improved quantification |
| Data Analysis | Identification and quantification of cysteine oxidation sites | Map to known modification databases; implement stringent false discovery rates |
This approach has enabled the identification of 4,438 unique cysteine sites across 1,850 unique protein groups from just 400,000 primary cells, demonstrating the sensitivity achievable with current methodologies [59].
Comparative Redox Profiling Across Developmental Stages
Application of redox proteomics to fetal versus adult HSPCs has revealed striking differences in redox homeodynamics. Quantitative analysis demonstrated that 227 cysteine sites showed significantly different oxidation states between fetal and adult cells, with the majority (174 peptides) being more highly oxidized in fetal HSPCs [59]. This differential oxidation pattern correlates with the distinct functional properties of fetal HSPCs, which display higher proliferative capacity, translation rates, and metabolic demands compared to their adult counterparts [59].
Table 2: Comparative Redox Profiles in Developmental HSPC Models
| Parameter | Fetal HSPCs | Adult HSPCs |
|---|---|---|
| Median Peptide Oxidation | 9-16% | <9% |
| Highly Oxidized Peptides (>70%) | Lower percentage | Higher percentage |
| Cysteines Forming Disulfides | Median 78% oxidation | Median 95% oxidation |
| Proteins with Redox-sensitive Cysteines | Enriched in metabolism and protein homeostasis | Distinct functional clusters |
| Antioxidant Enzyme Levels | Significantly lower | Higher expression |
These findings highlight the importance of selecting appropriate developmental stages in preclinical modeling, as redox regulation differs substantially across the lifespan.
Modeling Redox Dysregulation in Disease States
Neurological and Metabolic Disorders
The α-ketoglutarate dehydrogenase complex (KGDHc) represents a critical redox-sensitive node in mitochondrial metabolism and serves as an important focus for preclinical modeling of neurological and metabolic disorders [60]. KGDHc exhibits dual roles in redox regulation: (1) it senses redox environment changes through reversible oxidation of vicinal lipoic acid thiols on its DLST (E2) subunit, and (2) it generates mitochondrial H2O2 (mtH2O2) through its dihydrolipoamide dehydrogenase (DLD; E3) subunit [60]. Under pathological conditions, KGDHc can become a potent source of oxidative distress, contributing to disease pathogenesis.
Preclinical models targeting KGDHc have revealed that hyper-generation of mtH2O2 by this enzyme complex drives pathology in conditions including non-alcoholic fatty liver disease (NAFLD), neurodegenerative diseases, and inflammation [60]. Experimental approaches using selective KGDHc inhibitors such as 2-keto-3-methylvaleric acid (KMV), valproic acid, carboxyethyl succinyl phosphonate (CESP), and triethyl succinyl phosphonate (TESP) have demonstrated that targeted inhibition of KGDHc-derived ROS can alleviate disease phenotypes [60]. These findings highlight the value of enzyme-specific redox modulation rather than broad-spectrum antioxidant approaches.
Cardiovascular Diseases
Redox homeodynamics plays a fundamental role in cardiovascular physiology and disease pathogenesis [61]. ROS and reactive nitrogen species (RNS) regulate vascular tone, myocardial function, metabolic adaptation, and cell growth under physiological conditions, while dysregulation contributes to endothelial dysfunction, inflammation, fibrosis, and cell death in cardiovascular diseases [61].
Preclinical models of cardiovascular disease must account for redox-sensitive ion channels that coordinate cardiac action potentials. Under oxidative stress conditions, redox modifications commonly reduce potassium currents while enhancing sodium and calcium influx, disrupting cardiac rhythm and promoting arrhythmias [61]. Experimental models demonstrate that oxidizing agents reduce repolarizing currents, while reducing systems can restore normal channel activity, providing a mechanistic basis for targeted therapeutic interventions.
Cancer Models
Cancer cells typically exhibit elevated ROS levels coupled with enhanced antioxidant capacity, creating a redox resilience phenotype that supports proliferation while maintaining viability [15] [62]. Preclinical cancer models must therefore capture this reconfigured redox homeodynamics rather than simply quantifying oxidative stress levels.
The bone marrow microenvironment presents a particularly instructive system for studying redox regulation in cancer, with hypoxic osteoblastic niches (1-2% oxygen) that maintain hematopoietic stem cell quiescence, and more oxygenated vascular niches that promote differentiation [62]. This physiological redox gradient is disrupted in hematological malignancies, making it a critical factor in preclinical modeling. Thiol-active agents that modulate this gradient have shown effects on hematopoietic proliferation and differentiation, suggesting opportunities for therapeutic intervention [62].
Advanced Methodologies for Assessing Redox Homeodynamics
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Redox Homeodynamics Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Thiol-labeling Reagents | IodoTMT, Iodoacetyl tags | Covalent labeling of reduced cysteine thiols for quantification |
| ROS-generating Enzyme Inhibitors | S1QELs, S3QELs | Site-specific inhibition of electron leaks from mitochondrial complexes I and III |
| KGDHc Inhibitors | KMV, Valproic acid, CESP, TESP | Targeted inhibition of KGDHc-derived ROS production |
| Redox-sensitive Fluorescent Probes | DCFH-DA, MitoSOX, roGFP | Detection and quantification of specific ROS in live cells |
| Antioxidant Enzyme Assays | SOD, CAT, GPx activity kits | Quantification of enzymatic antioxidant capacity |
| Thiol Status Assays | GSH/GSSG ratio, Glutathione disulfide reductase | Assessment of cellular reduction potential |
| Mass Spectrometry Tags | TMT, iTRAQ, Dimethyl labeling | Multiplexed quantification of protein expression and modifications |
Detection Methods for Redox Analysis
Multiple methodologies have been developed to quantify different aspects of redox homeodynamics:
Free Radical Scavenging Kinetics:
- ORAC (Oxygen Radical Antioxidant Capacity): Measures kinetics of oxidative fluorescence decay using AAPH-generated peroxyl radicals [63]
- TRAP (Total Radical-trapping Antioxidant Parameter): Quantifies antioxidant capacity by delay in fluorescence decay [63]
- TOSC (Total Oxidant Scavenging Capacity): Measures inhibition of KMBA oxidation to ethylene [63]
Chemiluminescence-based Methods:
- Chemiluminescence Quenching: Measures attenuation of chemiluminescence from reactions between ROS and specific probes (luminol, lucigenin) [63]
- Photochemiluminescence: Specifically quantifies superoxide radical scavenging capacity [63]
These methods provide complementary information about different aspects of redox homeodynamics, from specific ROS production to overall antioxidant capacity.
Experimental Protocols for Key Assessments
Protocol 1: Redox Proteomics Using Sequential IodoTMT Labelling
This protocol enables comprehensive identification of reversible cysteine modifications in limited cell samples [59]:
Cell Preparation and Lysis:
- FACS-sort 400,000-500,000 target cells (approximately 20μg protein)
- Lyse in appropriate buffer containing protease inhibitors without thiol-blocking agents
- Centrifuge at 16,000×g for 15 minutes at 4°C and collect supernatant
Free Thiol Blocking:
- Incubate with iodoTMT reagent (1:50 ratio) in the dark for 1 hour at room temperature
- Remove excess reagent using desalting columns or protein precipitation
Reduction of Oxidized Thiols and Enrichment:
- Reduce reversibly oxidized cysteines with DTT (5mM, 30 minutes, room temperature)
- Label newly reduced thiols with a different iodoTMT isomer
- Capture TMT-labeled peptides using anti-TMT resin
Mass Spectrometric Analysis:
- Perform nanoLC-MS3 analysis on Orbitrap Fusion Lumos or similar instrumentation
- Use MS3 for TMT quantification to minimize ratio compression
- Search data against appropriate database with cysteine modifications specified
Protocol 2: Assessment of Mitochondrial Redox Regulation
This protocol focuses on evaluating KGDHc-dependent ROS production [60]:
Mitochondrial Isolation:
- Isolate mitochondria from target tissue (liver, brain, muscle) using differential centrifugation
- Confirm mitochondrial integrity and function via oxygen consumption assays
Targeted Inhibition:
- Pre-incubate with specific inhibitors: S1QELs (complex I), S3QELs (complex III), or KGDHc inhibitors (KMV, valproic acid)
- Include appropriate vehicle controls for each inhibitor condition
ROS Measurement:
- Assess H2O2 production using Amplex Red/horseradish peroxidase assay
- Measure fluorescence (excitation/emission: 571/585nm) continuously for 30-60 minutes
- Normalize results to mitochondrial protein content or citrate synthase activity
Functional Assessment:
- Measure oxygen consumption rates using Seahorse XF Analyzer or similar platform
- Assess membrane potential using JC-1 or TMRM dyes
- Correlate ROS production with metabolic function under different substrate conditions
Visualization of Redox Signaling Pathways and Experimental Workflows
Redox Signaling Pathway Integration
Diagram 1: Redox Signaling Pathway Integration. This diagram illustrates the integrated cellular response to redox signals, from initial stimulus through cysteine modifications to functional outcomes with feedback mechanisms.
Redox Proteomics Workflow
Diagram 2: Redox Proteomics Workflow. This experimental workflow details the sequential labeling approach for comprehensive identification of reversible cysteine oxidation states in limited cell samples.
Implications for Drug Discovery and Development
Targeting Redox-Sensitive Pathways
The reconceptualization of redox biology from homeostasis to homeodynamics has profound implications for drug discovery. Rather than broadly suppressing ROS with antioxidants, successful strategies now focus on targeted modulation of specific redox-sensitive nodes [15]. Examples include:
- Small molecule inhibitors targeting specific cysteine residues in redox-sensitive proteins
- Modulators of antioxidant transcription factors such as Nrf2
- Enzyme-specific inhibitors that prevent pathological ROS generation without disrupting physiological signaling
- Redox-based combination therapies that exploit oxidative vulnerabilities in cancer cells
Clinical development of compounds like Telintra (Ezatiostat HCl), a GST P1-1 inhibitor that modulates JNK signaling, demonstrates the therapeutic potential of targeted redox modulation [62]. Similarly, the recognition that different GSTP polymorphic variants significantly influence drug response highlights the importance of pharmacogenetic considerations in redox-targeted therapies [62].
Preclinical Model Optimization
Effective integration of redox homeodynamics in drug screening requires optimization of preclinical models:
Incorporation of Relevant Exposomal Factors: Models should include environmental exposures that influence redox homeodynamics through the exposome [58] [45]
Assessment of Bidirectional Redox Dysregulation: Models must capture both oxidative and reductive stress, as both extremes disrupt homeodynamics [57]
Spatiotemporal Monitoring: Advanced imaging and sensing technologies should capture dynamic redox changes rather than single timepoint measurements
Tissue-specific Modeling: Recognition that different tissues maintain distinct redox landscapes requiring specialized model development
These approaches will enable more accurate prediction of clinical efficacy and safety for redox-modulating therapeutics.
The integration of redox homeodynamics into preclinical models represents a paradigm shift in disease modeling and drug screening. Moving beyond static homeostasis to dynamic, network-based understanding of redox regulation enables more accurate recapitulation of human physiology and pathology. The experimental approaches and methodologies outlined herein provide a framework for developing preclinical models that capture the complexity of redox communication across biological scales, from molecular switches to interorgan signaling. As these models continue to evolve, they will undoubtedly accelerate the development of targeted therapies that restore redox homeodynamics in diverse disease contexts.
The conceptual framework for understanding redox biology in clinical applications is evolving from a static homeostasis to a dynamic homeodynamics model. Redox homeostasis traditionally refers to the maintenance of a balanced physiological state between oxidants and antioxidants [64]. In contrast, the homeodynamics concept recognizes redox states as a dynamic, adaptive interface that continuously responds to metabolic demands, circadian rhythms, and environmental exposures [15] [64]. This paradigm shift is critical for precision medicine trials, as it acknowledges that redox profiles are not fixed but represent a systems-level regulatory network that varies between individuals and within the same individual over time.
The failure of broad-spectrum antioxidant therapies in complex diseases underscores the limitations of the homeostasis model [15] [38]. A homeodynamics perspective reveals why non-targeted antioxidant approaches have largely failed—they disrupt delicate redox signaling networks that use reactive species as specific molecular messengers [64]. Precision medicine trials must therefore move beyond simplistic oxidative stress measurements toward multidimensional redox profiling that captures the dynamic signaling capacity of redox networks and an individual's adaptive response capabilities.
Redox Biomarkers for Patient Stratification
Classification and Measurement of Redox Biomarkers
Comprehensive redox profiling requires measuring multiple biomarker classes that reflect different aspects of redox homeodynamics. The table below summarizes key biomarkers with established clinical relevance.
Table 1: Key Redox Biomarkers for Patient Stratification
| Biomarker Category | Specific Biomarkers | Biological Significance | Measurement Techniques |
|---|---|---|---|
| Protein Oxidation | Protein carbonyls [65] | Irreversible protein damage; valuable pre/post-surgery | Spectrophotometric, immunochemical methods |
| Antioxidant Enzymes | Glutathione peroxidase (GPx) [65], Catalase [65], Superoxide dismutase (SOD) [66] [15] | Primary defense against ROS; indicates antioxidant capacity | Spectrophotometric activity assays |
| Transcription Factors | PGC-1α [65], NRF2 [66] [15] | Master regulators of antioxidant response | Immunochemical methods, ELISA |
| Lipid Peroxidation | Malondialdehyde (MDA), 4-hydroxynonenal (4-HNE), F2-isoprostanes [38] | Membrane damage; neuroinflammation in neurodegeneration | LC-MS, immunoassays |
| DNA/RNA Oxidation | 8-hydroxy-2'-deoxyguanosine (8-OHdG) [38] | Oxidative nucleic acid damage; genomic instability | HPLC-EC, LC-MS, immunoassays |
| Thiol Homeostasis | Serum free thiols (R-SH) [67] | Redox control capacity; predictive in cardiovascular diseases | Spectrophotometric methods |
Analytical Approaches for Redox Biomarker Assessment
Modern redox profiling employs integrated multi-platform approaches to capture system-wide dynamics. Spectrophotometric methods provide robust measurement of antioxidant enzyme activities like glutathione peroxidase and catalase, offering clinical practicality for rapid assessment [65]. Immunochemical techniques (ELISA, Western blot) enable precise quantification of specific oxidized proteins (e.g., protein carbonyls) and transcription factors (e.g., PGC-1α) with high sensitivity [65].
Advanced mass spectrometry-based platforms (LC-MS, HPLC-EC) offer unparalleled specificity for detecting lipid peroxidation products (4-HNE, F2-isoprostanes) and DNA damage markers (8-OHdG), capturing the molecular diversity of oxidative modifications [38]. The emerging integration of redox proteomics allows comprehensive mapping of cysteine oxidative modifications (S-sulfenylation, S-nitrosylation, S-glutathionylation) that function as critical redox switches in signaling networks [15].
Redox Signaling Pathways and Stratification Logic
Core Redox Signaling Networks
The NRF2-antioxidant response element (ARE) pathway serves as the primary cellular defense mechanism against oxidative stress. Under basal conditions, NRF2 is bound to KEAP1 in the cytoplasm and targeted for proteasomal degradation. Upon oxidative challenge, specific KEAP1 cysteine residues undergo modification, leading to NRF2 stabilization and nuclear translocation. In the nucleus, NRF2 heterodimerizes with small MAF proteins and activates transcription of over 200 antioxidant and detoxification genes, including SOD, catalase, GPx, and glutathione S-transferases [66] [15].
The PGC-1α pathway integrates redox regulation with mitochondrial biogenesis and metabolic adaptation. PGC-1α activation induces mitochondrial gene expression, enhancing respiratory capacity while simultaneously upregulating antioxidant defenses, including SOD2 and TRX-dependent peroxidases. This coordinated response maintains redox balance during increased energy demand [65].
Diagram: Redox Homeodynamics Regulation Network
Diagram 1: Redox homeodynamics involves multiple coordinated pathways that maintain a dynamic balance.
Technical Implementation: Methodologies and Reagents
Experimental Protocols for Redox Profiling
Comprehensive Redox Biomarker Panel Protocol
Sample Collection and Preparation: Collect blood samples in EDTA-containing Vacutainers, separate plasma within 30 minutes by centrifugation at 2,500 × g for 15 minutes at 4°C. For serum, allow blood to clot for 30 minutes before centrifugation. Aliquot and store at -80°C. For tissue samples, flash-freeze in liquid nitrogen and store at -80°C until analysis [65].
Protein Oxidation Assessment: Measure protein carbonyl content using the 2,4-dinitrophenylhydrazine (DNPH) method. Briefly, precipitate 50 μL plasma proteins with 500 μL 20% trichloroacetic acid (TCA), react with 500 μL 10 mM DNPH in 2M HCl for 1 hour in darkness, with parallel HCl-only controls. Wash pellets three times with ethanol:ethyl acetate (1:1), dissolve in 6M guanidine hydrochloride, and measure absorbance at 370 nm. Calculate carbonyl content using ε = 22,000 M⁻¹cm⁻¹ [65].
Antioxidant Enzyme Activity Profiling:
- Glutathione peroxidase (GPx): Monitor NADPH oxidation at 340 nm in reaction mixture containing 50 mM potassium phosphate buffer (pH 7.0), 1 mM EDTA, 1 mM NaN₃, 0.2 mM NADPH, 1 U/mL glutathione reductase, 1 mM GSH, and 0.1 mM H₂O₂ [65].
- Catalase: Measure H₂O₂ decomposition at 240 nm (ε = 43.6 M⁻¹cm⁻¹) in 50 mM phosphate buffer (pH 7.0) with 10 mM H₂O₂ [65].
- Superoxide dismutase (SOD): Use xanthine oxidase-cytochrome c system, monitoring reduction at 550 nm in 50 mM potassium phosphate buffer (pH 7.8) with 0.1 mM EDTA, 0.1 mM xanthine, 10 μM cytochrome c [15].
Thiol Homeostasis Assessment: Determine free thiol groups using Ellman's reagent (5,5'-dithiobis-2-nitrobenzoic acid, DTNB). Mix 20 μL plasma with 200 μL 0.1M phosphate buffer (pH 8.0) and 10 μL 10 mM DTNB. Incubate 30 minutes at room temperature, measure absorbance at 412 nm. Calculate thiol concentration using ε = 14,150 M⁻¹cm⁻¹ and standard GSH curve [67].
Transcriptional Regulator Quantification Protocol
PGC-1α and NRF2 Measurement: Use commercial ELISA kits with pre-coated plates. For PGC-1α, lyse cells in RIPA buffer with protease inhibitors, centrifuge at 14,000 × g for 15 minutes. Dilute samples in provided buffer, add to wells, incubate 2 hours at room temperature. After washing, add detection antibody, incubate 1 hour, then HRP-conjugated secondary antibody for 1 hour. Develop with TMB substrate, stop with sulfuric acid, measure at 450 nm [65].
NRF2 Nuclear Translocation Assay: Separate nuclear and cytoplasmic fractions using commercial kits. Confirm fraction purity with LDH (cytosol) and lamin B1 (nuclear) markers. Quantify NRF2 in both fractions via Western blot or ELISA to calculate nuclear:cytoplasmic ratio as activation index [15].
Research Reagent Solutions
Table 2: Essential Research Reagents for Redox Profiling
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Antibody-Based Reagents | Anti-protein carbonyl antibodies [65], Anti-PGC-1α ELISA kits [65], Anti-NRF2 antibodies [15] | Quantification of oxidized proteins and transcription factors |
| Enzyme Activity Assay Kits | Glutathione peroxidase assay kits [65], Catalase activity assays [65], Superoxide dismutase kits [15] | Standardized measurement of antioxidant enzyme activities |
| Chemical Detection Reagents | 2,4-dinitrophenylhydrazine (DNPH) [65], Ellman's reagent (DTNB) [67], Thiobarbituric acid (TBA) [38] | Colorimetric/fluorometric detection of specific oxidative modifications |
| Small Molecule Modulators | NRF2 activators (sulforaphane, dimethyl fumarate) [38], Mitochondria-targeted antioxidants (MitoQ, SS-31) [38] | Experimental validation of redox pathways and therapeutic targeting |
Clinical Translation and Trial Design
Stratification Algorithms for Specific Disease Contexts
Cardiovascular Surgery Stratification
In cardiopulmonary bypass (CPB) patients, a validated stratification algorithm incorporates protein carbonyls (>3.5 nmol/mg protein, high-risk), glutathione peroxidase activity (<40 U/L, high-risk), and PGC-1α levels (<2.5 ng/mL, high-risk). Patients with ≥2 high-risk markers demonstrate 4.8-fold increased complication risk and require targeted antioxidant protocols [65]. The receiver operating characteristic (ROC) analysis supports protein carbonyl as valuable in both preoperative (p = 0.009) and postoperative (p = 0.013) periods, while glutathione peroxidase shows particular value postoperatively (p = 0.000) [65].
Neurodegenerative Disease Stratification
For Alzheimer's and Parkinson's trials, stratification incorporates multi-omic redox profiling: lipid peroxidation markers (4-HNE, F2-isoprostanes), oxidized nucleosides (8-OHdG), and specific protein modifications (carbonylated tau, nitrated α-synuclein). Machine learning algorithms integrate these biomarkers with clinical scores to identify patient subgroups most likely to respond to mitochondrial-targeted therapies [38].
Diagram: Patient Stratification Workflow
Diagram 2: Comprehensive patient stratification workflow integrates biomarker profiling with computational analysis.
The stratification of patients via redox profiles represents a paradigm shift in precision medicine trials, moving beyond static diagnostic categories to functional redox phenotyping. The integration of dynamic biomarker panels, transcriptional regulators, and advanced computational analytics enables identification of patient subpopulations with shared redox signatures that transcend conventional disease classifications. This approach acknowledges the homeodynamic nature of redox regulation and offers a pathway to meaningfully targeted interventions that restore redox signaling capacity rather than merely suppressing oxidative processes.
Future directions will require developing continuous monitoring technologies, validating standardized redox phenotyping panels across diverse populations, and establishing clinical decision thresholds for redox-targeted therapies. As these tools mature, redox stratification will become an integral component of precision medicine trials across cardiovascular, neurodegenerative, metabolic, and oncological disorders, finally delivering on the therapeutic promise of redox medicine that has remained elusive for decades.
Navigating the Double-Edged Sword: Challenges in Redox-Targeted Therapy
The "antioxidant paradox"—the observation that high-dose antioxidant supplements largely fail to prevent or treat human diseases despite clear evidence implicating reactive oxygen species (ROS) in their pathogenesis—challenges a long-held simplistic view of oxidative stress. This whitepaper reframes this paradox through the lens of redox homeodynamics, a concept that emphasizes the dynamic, context-dependent nature of redox signaling, as opposed to a static homeostasis. We detail the critical dual roles of ROS as both damaging agents and essential signaling molecules, explaining how non-discriminate antioxidant interventions can disrupt adaptive physiological processes, including exercise adaptation, stem cell self-renewal, and immune function. Supported by structured data, experimental protocols, and pathway visualizations, this analysis provides researchers and drug development professionals with a refined framework for targeting redox biology in therapeutic development.
The traditional view of redox biology has been governed by the principle of homeostasis—the idea that biological systems maintain a relatively constant and stable internal environment by eliminating ROS. However, contemporary research necessitates a shift towards the concept of redox homeodynamics [39] [68]. This paradigm recognizes the redox landscape as a dynamic, non-equilibrium state that is precisely regulated in a spatiotemporal manner to support vital biological functions.
The antioxidant paradox emerges directly from this conceptual shift. It describes the contradiction wherein ROS are involved in numerous human diseases, yet large-scale intervention studies with dietary antioxidant supplements have consistently shown little to no preventative or therapeutic benefit [69]. The paradox stems from an outdated belief that all ROS are inherently harmful and that their wholesale elimination is beneficial. In reality, ROS function as crucial redox messengers within a complex network, where their lifetime and signaling specificity are themselves determined by the antioxidant system [39]. This paper will dissect the mechanisms behind this paradox and explore its implications for research and drug discovery.
The Dual Nature of ROS: Damage versus Signaling
Reactive oxygen and nitrogen species exhibit a clear duality in biological systems, acting as both toxic byproducts of metabolism and essential regulators of cellular function.
- The Damaging Potential of ROS: ROS can cause indiscriminate oxidative damage to lipids, proteins, and DNA. The hydroxyl radical (OH•), for instance, is highly reactive and attacks almost all biomolecules [69]. This damage, if persistent, is implicated in the pathogenesis of various chronic diseases and the ageing process [69] [68].
- ROS as Physiological Messengers: In contrast, specific ROS like hydrogen peroxide (H₂O₂) are now recognized as important signaling molecules. They are involved in regulating a myriad of processes, including cell proliferation, immune response, and metabolic adaptation [69] [70]. The signaling function is dependent on the precise subcellular generation of specific ROS and their careful removal by endogenous antioxidants.
Table 1: Key Reactive Species and Their Roles in Physiology and Pathology
| Reactive Species | Primary Sources | Physiological Roles | Pathological Consequences |
|---|---|---|---|
| Superoxide (O₂•⁻) | Mitochondrial ETC, NADPH oxidases | Signal transduction, host defense | Can inactivate enzymes, precursor to more potent ROS |
| Hydrogen Peroxide (H₂O₂) | Dismutation of O₂•⁻, peroxisomes | Redox signaling (e.g., MAPK, NF-κB pathways), immune function | Uncontrolled accumulation leads to oxidative damage |
| Nitric Oxide (NO•) | Nitric oxide synthases (NOS) | Vasodilation, neurotransmission, immune regulation | Reaction with O₂•⁻ forms peroxynitrite (ONOO⁻), a potent oxidant |
| Hydroxyl Radical (OH•) | Fenton reaction (H₂O₂ + Fe²⁺) | Minimal to none; indiscriminately reactive | Significant damage to all biomolecules, lipid peroxidation |
The Core of the Paradox: Mechanisms of Antioxidant Interference
The detrimental effects of high-dose antioxidant supplementation arise from the disruption of specific physiological processes that rely on ROS signaling.
Impairment of Exercise Adaptation
Strenuous exercise generates ROS, which serve as critical signals for inducing beneficial adaptations. Antioxidant supplementation can blunt these adaptive responses [70].
- Mitochondrial Biogenesis: Exercise-induced ROS activate redox-sensitive pathways like NF-κB and MAPK, leading to increased expression of antioxidant enzymes and components of mitochondrial biogenesis, such as PGC-1α. Supplementation with vitamins C and E has been shown to reduce mitochondrial biogenesis [70].
- Insulin Sensitivity and Hypertrophy: ROS generated during muscle contraction are involved in the signaling that improves insulin sensitivity and promotes muscle growth. Exogenous antioxidants can interfere with these signals, hampering performance-enhancing and health-promoting training adaptations [70].
Table 2: Documented Adverse Effects of Antioxidant Supplementation on Exercise Adaptation
| Antioxidant(s) | Study Model | Key Negative Outcome | Reference (from search results) |
|---|---|---|---|
| Vitamin C (1g/d) | 8-week cycling training | Reduced mitochondrial biogenesis | [70] |
| Vitamin C + E | 11-week training program | Reduced mitochondrial biogenesis | [70] |
| Vitamin C + E | Sprint interval training | Blunted training-induced adaptation | [70] |
| Resveratrol | 8-week training program | Blunted cardiovascular health improvements | [70] |
Disruption of Stem Cell Fate and Differentiation
Stem cells reside in specialized "redox niches" characterized by low ROS levels, which are crucial for maintaining self-renewal and pluripotency [71]. A carefully balanced redox state is maintained by scavenger antioxidant enzyme systems and key regulators like FoxO proteins and Nrf2.
- Low ROS for Self-Renewal: Hematopoietic stem cells (HSCs) and neural stem cells (NSCs) require low ROS levels to maintain their stemness and regenerative capacity. Loss of redox regulators like FoxO3 leads to ROS accumulation and HSC defects [71].
- ROS for Differentiation: Conversely, an increase in ROS levels can effectively shut down self-renewal and promote differentiation into specific lineages [71]. Non-discriminate antioxidant use could theoretically disrupt this delicate balance, impairing tissue regeneration and repair.
Inhibition of Immune Defense and Host Protection
ROS are essential components of the innate immune response. Macrophages and neutrophils deliberately produce high levels of ROS via NADPH oxidase (NOX) complexes to destroy invading pathogens [68]. While this is a controlled, beneficial "oxidative burst," systemic high-dose antioxidants could potentially dampen this critical host defense mechanism.
Experimental Evidence and Key Research Models
The paradoxical effects of antioxidants have been robustly demonstrated in both human intervention studies and genetically engineered animal models.
Human Studies: The Failure of Supplementation
Large-scale human trials have consistently failed to show benefits from antioxidant supplementation. The Selenium and Vitamin E Cancer Prevention Trial (SELECT) even found an increased risk of prostate cancer among men taking vitamin E [69]. In the context of exercise, detailed in Table 2, multiple randomized controlled trials demonstrate that vitamins C and E can block positive training adaptations.
Genetic Models: The Phenotype of Antioxidant Enzyme Manipulation
Knockout and overexpression mouse models have been instrumental in revealing the paradoxical roles of antioxidant enzymes. These models show that the effects are complex and context-dependent.
Table 3: Paradoxical Phenotypes in Antioxidant Enzyme Mouse Models
| Gene | Modification | Observed "Paradoxical" Phenotype |
|---|---|---|
| SOD1 | Overexpression | No consistent lifespan extension; some models show reduced function. |
| SOD2 | Knockout | Perinatal lethality, severe metabolic disorders. |
| GPX1 | Overexpression | Promoted high-fat-diet-induced obesity and insulin resistance. |
| GPX1 | Knockout | Showed resistance to high-fat-diet-induced insulin resistance. |
| CAT | Overexpression | No significant healthspan or lifespan benefits reported. |
Adapted from [72]
Detailed Experimental Protocol: Assessing Antioxidant Impact on Exercise Adaptation
To investigate whether an antioxidant compound blunts exercise adaptation, the following clinical research protocol can be employed, based on methodologies cited in [70].
- Objective: To determine the effect of daily oral antioxidant supplementation on exercise-induced mitochondrial biogenesis and performance adaptation.
- Population: Healthy, recreationally active adults (e.g., n=30-40 per group).
- Study Design: Randomized, double-blind, placebo-controlled trial.
- Intervention:
- Experimental Group: Oral dose of the test antioxidant (e.g., 1g Vitamin C + 400 IU Vitamin E) daily.
- Control Group: Matched placebo daily.
- Training Protocol: All participants undergo a supervised endurance training program (e.g., cycling or running at 70-80% VO₂max, 3-4 sessions/week) for 8-12 weeks.
- Primary Outcome Measures:
- Muscle Biopsy Analysis: Pre- and post-intervention biopsies from the vastus lateralis.
- Mitochondrial Content: Measured via citrate synthase activity and mitochondrial DNA copy number.
- Signaling Pathway Activation: Western blot analysis of key proteins (e.g., phospho-AMPK, PGC-1α protein levels).
- Performance Metrics: Maximal oxygen consumption (VO₂max) and time-trial performance.
- Muscle Biopsy Analysis: Pre- and post-intervention biopsies from the vastus lateralis.
- Key Reagent Solutions:
- Citrate Synthase Activity Assay Kit: For spectrophotometric quantification of mitochondrial enzyme activity.
- Primary Antibodies: Anti-PGC-1α, anti-phospho-AMPK, anti-AMPK for Western blotting.
- Real-Time PCR System: For quantification of mitochondrial DNA and relevant nuclear-encoded genes.
The Scientist's Toolkit: Key Research Reagents
Table 4: Essential Research Reagents for Investigating Redox Homeodynamics
| Reagent / Material | Function / Application | Example Use-Case |
|---|---|---|
| H₂DCFDA / CM-H₂DCFDA | Cell-permeable fluorescent probe for detecting general ROS (particularly H₂O₂) in live cells. | Quantifying intracellular ROS flux in cultured stem cells or myotubes under different conditions. |
| MitoSOX Red | Fluorogenic dye that selectively targets mitochondria and is oxidized by superoxide. | Measuring mitochondrial superoxide production in response to exercise-mimetic stimuli. |
| Anti-Nrf2 Antibody | For Western Blot, ELISA, or ChIP to study the activation of this key redox-sensitive transcription factor. | Assessing Nrf2 nuclear translocation after oxidative challenge in the presence/absence of test compounds. |
| SOD, Catalase, GPX Activity Assay Kits | Colorimetric or fluorometric kits to measure the activity of endogenous antioxidant enzymes. | Profiling the antioxidant capacity of tissues from knockout mouse models or supplemented humans. |
| Isoprostane (8-iso-PGF2α) ELISA | Robust mass spectrometry-validated biomarker for lipid peroxidation in vivo. | Accurately measuring oxidative damage in human plasma or urine in clinical trials. |
| siRNA/shRNA for Nrf2, FoxOs | Gene silencing tools to knock down key redox regulators in vitro. | Elucidating the role of specific pathways in maintaining stem cell self-renewal under low ROS. |
Redox Signaling Pathways: A Visual Guide
The following diagrams, generated using Graphviz DOT language, illustrate key signaling pathways discussed in this whitepaper.
Diagram 1: The Nrf2/Keap1 Signaling Pathway in Redox Homeostasis
This diagram depicts the canonical Nrf2-Keap1 pathway. Under basal conditions, Nrf2 is bound by Keap1 and targeted for proteasomal degradation. Oxidative stress modifies critical cysteine residues on Keap1, leading to Nrf2 stabilization, nuclear translocation, and transcription of cytoprotective genes [68].
Diagram 2: The Dual Role of ROS in Exercise Adaptation
This diagram illustrates the exercise-antioxidant paradox. Acute exercise increases ROS, which act as signals to activate pathways leading to beneficial adaptations. The administration of high-dose exogenous antioxidants scavenges these ROS signals, resulting in blunted physiological adaptation [70].
The "antioxidant paradox" is resolved when viewed through the framework of redox homeodynamics. ROS are not merely toxic waste but integral components of a dynamic, information-rich signaling network. The failure of simplistic antioxidant supplementation strategies underscores the need for more sophisticated therapeutic approaches.
Future research and drug development must move beyond global ROS suppression. Promising strategies include:
- Targeting Specific ROS Sources: Developing inhibitors for specific ROS-generating enzymes (e.g., NOX isoforms) implicated in pathological, but not physiological, signaling.
- Enhancing Endogenous Defenses: Identifying compounds that can safely boost the body's own antioxidant systems, such as via mild pro-oxidant or Nrf2-activating strategies that induce a hormetic response [69].
- Spatiotemporal Precision: Designing therapies that target antioxidants to specific cellular compartments or tissues where oxidative damage is paramount, while leaving redox signaling in other compartments intact.
- Exploring Redox-Modulating Metabolites: Investigating endogenous metabolites like betaine, which has been shown to mimic exercise by targeting specific inflammatory pathways like TBK1, without globally scavenging ROS [73] [74].
Understanding the nuanced language of redox biology is essential for developing effective treatments for the many diseases in which ROS play a role. The goal is not to eliminate ROS, but to restore the delicate dynamics of their production and elimination—to manage the balance, not wage a war.
The conceptual framework of redox biology has evolved from a static homeostasis to a dynamic homeodynamics paradigm, recognizing redox states as fluid, adaptive interfaces that mediate cellular responses to internal and external cues. Within this framework, the role of reactive oxygen species (ROS) is fundamentally dualistic. Physiological ROS concentrations, operating within a precise "redox window," are essential for normal cell signaling, proliferation, and immune function [75] [76]. Conversely, a sustained shift beyond this window creates a state of oxidative stress, characterized by redox signaling disruption and macromolecular damage [76] [77]. This whitepaper delineates the context-dependent outcomes of manipulating the redox balance, contrasting pro-oxidant strategies designed to eradicate cancer cells with antioxidant approaches aimed at mitigating oxidative damage in chronic diseases. This dichotomy is central to developing targeted therapeutic interventions in redox medicine, requiring a precise understanding of the distinct redox profiles of different pathological states.
Oxidative Stress Fundamentals: Mechanisms and Biomarkers
Reactive Oxygen Species: Generation and Regulation
Reactive oxygen species are generated from multiple endogenous sources, with the mitochondrial electron transport chain (ETC) and the NADPH oxidase (NOX) family being most significant [78] [79]. In mitochondria, complexes I and III are primary sites of superoxide (O₂•⁻) production due to electron leakage [80]. The NOX family, including NOX1-5 and DUOX1/2, catalyzes the reduction of oxygen to superoxide using NADPH as an electron donor [81] [76]. Additional sources include cytochrome P450 enzymes, xanthine oxidase, and the endoplasmic reticulum [81] [80].
Cellular defense against ROS involves a sophisticated network of enzymatic and non-enzymatic antioxidants. The primary enzymatic defenders include superoxide dismutase (SOD), which catalyzes the dismutation of superoxide to hydrogen peroxide (H₂O₂); catalase (CAT), which converts H₂O₂ to water and oxygen; and the glutathione (GSH) and thioredoxin (Trx) systems, which manage peroxide levels and regulate redox signaling [75] [79]. The transcription factor NRF2 serves as the master regulator of the antioxidant response, activating hundreds of genes that maintain redox homeostasis [81] [79].
Biomarkers of Oxidative Damage
Accurate assessment of oxidative stress is crucial for both research and clinical application. Established biomarkers reflect damage to major biomolecular classes.
Table 1: Key Biomarkers of Oxidative Stress
| Biomolecule Targeted | Biomarker | Significance and Measurement |
|---|---|---|
| Lipids | Malondialdehyde (MDA), 4-Hydroxynonenal (4-HNE) | Stable end products of lipid peroxidation; measured via HPLC, LC-MS/MS, or TBARS assay [75] [77]. |
| DNA | 8-Hydroxy-2'-deoxyguanosine (8-OHdG) | Oxidized guanine nucleoside; a sensitive marker of oxidative DNA damage, measured by ELISA or mass spectrometry [82] [75]. |
| Proteins | Protein Carbonyls | Formed on proline, arginine, lysine side chains; measured via DNPH assay; indicates loss of protein function [77]. |
The Antioxidant Paradigm in Chronic Disease Prevention
In chronic non-communicable diseases, oxidative stress is a well-established driver of pathology, making antioxidant strategies a primary focus. Epidemiological evidence consistently demonstrates an inverse relationship between antioxidant capacity and mortality. The Oxidative Balance Score (OBS) has emerged as a comprehensive tool to quantify this relationship, integrating multiple dietary and lifestyle factors into a single score, where a higher OBS indicates a greater antioxidant status [82] [83].
Table 2: Oxidative Balance Score (OBS) and Mortality Risk from NHANES Studies
| Study Population | OBS Quartile Comparison | All-Cause Mortality Risk (Hazard Ratio) | Cancer-Specific Mortality Risk (Hazard Ratio) |
|---|---|---|---|
| General US Adults (N=37,317) [82] | Highest (Q4) vs. Lowest (Q1) | HR 0.68 (32% lower risk) | HR 0.55 (45% lower risk) |
| Cancer Survivors (N=2,131) [83] | Highest (Q4) vs. Lowest (Q1) | HR 0.60 (40% lower risk) | Significant reduction reported |
This data underscores the protective role of an antioxidant-rich profile, characterized by high intake of nutrients like vitamins C and E, carotenoids, and dietary fiber, and lifestyle factors such as physical activity and non-smoking status [82]. The consistent risk reduction across populations confirms that reinforcing the body's antioxidant defenses is a valid strategy for mitigating the long-term oxidative damage that underlies chronic disease progression.
The Pro-Oxidant Paradigm in Cancer Therapeutics
In contrast to chronic diseases, cancer biology presents a unique "Redox Paradox" [81]. Cancer cells inherently exhibit elevated levels of ROS due to oncogenic signaling, metabolic reprogramming (e.g., Warburg effect), and relative hypoxia [81] [78]. These cells adapt to this chronic oxidative stress by upregulating their antioxidant capacity (e.g., NRF2, GSH), becoming dependent on this heightened defense to survive. This creates a vulnerable "therapeutic window" where further increasing ROS levels can overwhelm their adaptive capacity, pushing them into cell death programs [81] [79]. This rationale underpins pro-oxidant cancer therapy.
Key Signaling Pathways and Molecular Targets
The pro-tumorigenic effects of ROS are mediated through the oxidative inactivation of key regulatory proteins. A critical mechanism involves the oxidation of cysteine residues in the active sites of tumor suppressor phosphatases, such as PTEN [81]. This inactivation leads to the constitutive activation of pro-survival pathways like the PI3K/AKT/mTOR cascade, driving proliferation and survival [81]. Simultaneously, ROS regulate numerous other pathways integral to malignancy, including MAPK/ERK, NF-κB, STAT3, and HIF-1α, which control processes from proliferation to angiogenesis and immune evasion [80] [76].
Diagram 1: ROS signaling in cancer cells
Strategic Targeting of Antioxidant Defenses
The addiction of cancer cells to their rewired redox state reveals key targets for pro-oxidant therapy, focused on disabling their antioxidant shield.
Table 3: Pro-Oxidant Therapeutic Strategies in Cancer
| Therapeutic Target | Mechanism of Action | Example Agents |
|---|---|---|
| Master Regulator NRF2 | Inhibits the master antioxidant response, disabling multiple defense genes [81]. | Brusatol, ML385 [81] |
| Glutathione (GSH) System | Depletes GSH or inhibits its synthesis, inducing ferroptosis [81] [79]. | Sulfasalazine, Erastin, Withaferin A [81] [80] |
| Thioredoxin (Trx) System | Inhibits thioredoxin reductase (TrxR), disrupting redox control and signaling [81] [80]. | Auranofin, PX-12 [81] [80] |
| Direct ROS Induction | Generates high levels of ROS directly, overwhelming defenses [81] [79]. | High-Dose Vitamin C, Arsenic Trioxide (ATO) [81] |
Inducing oxidative cell death, particularly ferroptosis—an iron-dependent form of death driven by overwhelming lipid peroxidation—has emerged as a promising avenue for eliminating aggressive and therapy-resistant cancers [81] [79].
Experimental and Methodological Guide
The Scientist's Toolkit: Core Reagents and Assays
Table 4: Essential Reagents for Redox Biology Research
| Reagent / Assay Kit | Primary Function in Research |
|---|---|
| Cellular ROS Probes (e.g., H₂DCFDA, MitoSOX) | Detect general intracellular or mitochondrial superoxide levels, respectively [79]. |
| GSH/GSSG Assay Kit | Quantify the ratio of reduced glutathione (GSH) to oxidized glutathione (GSSG), a key indicator of cellular redox state [79]. |
| Lipid Peroxidation Assay (MDA/TBARS or C11-BODIPY⁵⁸¹/⁵⁹¹) | Measure end-products of lipid peroxidation, either in cell lysates (MDA) or live cells (C11-BODIPY) [75] [79]. |
| Nrf2 siRNA/inhibitors | Knock down or inhibit NRF2 to study its role in the antioxidant response and sensitize cells to pro-oxidants [81] [79]. |
| Ferroptosis Inducers (e.g., Erastin, RSL3) | Induce ferroptosis by inhibiting system Xc⁻ (Erastin) or directly inhibiting GPX4 (RSL3) [81] [79]. |
Protocol: Assessing Redox Status and Intervention Efficacy
This workflow provides a standardized method for evaluating the effects of redox-modulating compounds.
Title: Combined protocol for redox phenotyping and intervention testing.
Diagram 2: Redox assessment workflow
Detailed Methodology:
Cell Seeding and Treatment:
- Seed appropriate cell models (e.g., cancer cell lines, primary non-malignant cells) in 6-well or 96-well plates.
- After adherence, treat cells with a range of concentrations of the test compound (pro-oxidant or antioxidant) for a defined period (e.g., 24-72 hours). Include vehicle controls.
Intracellular ROS Measurement:
- Harvest trypsinized cells and incubate with H₂DCFDA (5-10 µM) for general ROS or MitoSOX Red (5 µM) for mitochondrial superoxide in serum-free media at 37°C for 30 minutes.
- Wash cells with PBS and analyze fluorescence immediately using a flow cytometer or fluorescence microplate reader.
Antioxidant Capacity Assessment:
- Lyse cells in appropriate buffers. Use a commercial GSH/GSSG Assay Kit to determine the reduced-to-oxidized glutathione ratio, a central redox buffer.
- Measure SOD activity using a tetrazolium-based kit to assess superoxide scavenging capacity.
Oxidative Damage Quantification:
- Lipid Peroxidation: Measure media levels of 8-isoprostane (a stable lipid peroxidation product) via a competitive ELISA kit.
- Protein Oxidation: Quantify protein carbonyls in cell lysates using the DNPH (2,4-dinitrophenylhydrazine) method, followed by spectrophotometric detection.
Functional Outcome Analysis:
- Viability: Perform MTT assay according to standard protocol to assess metabolic activity.
- Cell Death: Stain cells with Annexin V-FITC and Propidium Iodide (PI) and analyze by flow cytometry to distinguish apoptotic and necrotic populations.
The strategic manipulation of the redox landscape represents a frontier in precision medicine. The critical determinant of therapeutic success lies in accurately diagnosing the underlying redox pathology. In most chronic diseases, characterized by uncontrolled oxidative distress, the therapeutic path involves reinforcing endogenous antioxidant defenses through lifestyle, diet, and potentially, NRF2-activating pharmaceuticals. In stark contrast, for many cancers, the goal is to aggressively disrupt the precarious redox balance of malignant cells, pushing them beyond their buffering capacity into cell death. Future research must focus on developing better biomarkers to classify patients' redox status and creating more targeted agents that can selectively modulate redox pathways in specific cell types. This refined, context-dependent approach will fully realize the potential of redox-based therapies.
The traditional view of redox biology has centered on the concept of homeostasis—the maintenance of a static, reduced cellular environment through broad-spectrum antioxidant systems. However, emerging research reveals that redox regulation follows a more dynamic homeodynamic principle, where controlled fluctuations in reactive oxygen species (ROS) and specific, reversible redox modifications serve as crucial physiological signals [15] [84]. This paradigm shift moves beyond the simplistic "oxidants are bad, antioxidants are good" dichotomy and recognizes that redox processes are precisely regulated in space and time to control cellular function.
This homeodynamic perspective provides the foundation for novel therapeutic strategies that move beyond non-specific ROS scavenging. Instead, they focus on targeting specific redox-sensitive nodes, particularly thiol-based switches in key signaling proteins [85] [86]. Such precision approaches aim to correct pathological redox signaling while preserving beneficial redox regulation, offering new hope for treating cancer, neurodegenerative diseases, metabolic disorders, and other conditions linked to redox dysregulation [87] [15].
Fundamental Mechanisms of Thiol-Based Redox Switches
The Chemistry of Cysteine Oxidation
At the core of redox signaling are the reversible oxidative modifications of cysteine thiols (-SH) in proteins. These modifications function as molecular switches that regulate protein function, localization, and interactions [85]. The reactivity of a specific cysteine toward oxidation depends largely on its local protein microenvironment, which can lower its pKa (typically 8-9) to values where the deprotonated, more nucleophilic thiolate anion (Cys-S-) predominates at physiological pH [85] [84].
Table: Hierarchy of Cysteine Oxidative Modifications and Their Functional Consequences
| Modification | Chemical Structure | Reversibility | Primary Reductase System | Functional Impact |
|---|---|---|---|---|
| Sulfenic acid | Cys-SOH | Fully reversible | Thioredoxin (Trx), Glutaredoxin (Grx) | Allosteric regulation, transient activation |
| Disulfide bond | Cys-S-S-Cys | Fully reversible | Thioredoxin (Trx) | Protein folding, conformational changes |
| S-glutathionylation | Cys-S-SG | Fully reversible | Glutaredoxin (Grx) | Protection from overoxidation, signaling |
| Sulfinic acid | Cys-SO₂H | Reversible (Prx only) | Sulfiredoxin (ATP-dependent) | Regulatory switch (Prx), inactivation |
| Sulfonic acid | Cys-SO₃H | Irreversible | None | Protein damage, degradation |
The initial product of cysteine oxidation is typically sulfenic acid (Cys-SOH), which serves as a crucial intermediate in redox switching [85]. Although sulfenic acids are generally short-lived, some proteins like NADH peroxidase from Streptococcus faecalis and matrix metalloproteinase MMP-7 utilize stable sulfenic acid formations to control their catalytic activity [85]. Most sulfenic acids rapidly react further to form more stable modifications, including disulfide bonds (both intra- and intermolecular), mixed disulfides with glutathione (S-glutathionylation), or cyclic sulfenamides through reaction with nearby backbone nitrogen atoms [85].
Cellular Systems Maintaining Redox Homeodynamics
The reversibility of redox switches is maintained by integrated cellular reductase systems that ensure dynamic responses to changing redox conditions:
- Thioredoxin system: Comprises thioredoxin (Trx), thioredoxin reductase (TrxR), and NADPH. The conserved CXXC motif in Trx directly reduces disulfides and sulfenic acids in client proteins through thiol-disulfide exchange reactions [85].
- Glutaredoxin system: Utilizes glutaredoxin (Grx) and glutathione (GSH) to preferentially reduce S-glutathionylated proteins. Regeneration of reduced GSH from GSSG is maintained by glutathione reductase (GR) at the expense of NADPH [85].
- Sulfiredoxin: A specialized ATP-dependent reductase that specifically reduces the sulfinic acid form of peroxiredoxins, representing a unique reversal pathway for this level of oxidation [85].
These systems work in concert to maintain the homeodynamic balance of the cellular redox environment, allowing for rapid signal transduction while preventing accumulation of irreversible oxidative damage.
Key Redox-Sensitive Signaling Nodes as Therapeutic Targets
Receptor Tyrosine Kinase (RTK) Signaling Pathways
Receptor tyrosine kinases are critical mediators of cellular growth, proliferation, and survival signals, and their regulation exemplifies the importance of redox homeodynamics [87]. Redox control of RTK signaling occurs through several mechanisms:
- Ligand-independent activation via H₂O₂: In chronic lymphocytic leukemia cells, an imbalance between superoxide dismutase 2 (SOD2) and catalase leads to H₂O₂ accumulation, which activates the AXL receptor tyrosine kinase independently of its growth factor ligand, promoting survival through AKT and ERK signaling [87].
- Inactivation of phosphatase counter-regulation: Redox signaling reinforces mitogenic cascades by transiently inactivating protein tyrosine phosphatases (PTPs) through oxidation of their catalytic cysteine residues [84]. PTP1B, which dephosphorylates the epidermal growth factor receptor (EGFR), is inactivated by H₂O₂-mediated sulfenic acid formation, enhancing and prolonging EGFR signaling [84].
- Localized peroxide microdomains: Upon growth factor stimulation, localized pools of peroxiredoxin I (PRXI) associated with cell membranes are phosphorylated and inactivated, allowing controlled accumulation of H₂O₂ specifically at signaling hubs to facilitate phosphatase inhibition while preventing global oxidative stress [84].
These mechanisms are frequently co-opted in cancer, where transformed cells exhibit "redox addiction"—dependence on elevated ROS for maintaining pro-proliferative signaling through pathways like PI3K-AKT and RAS-RAF-MEK-ERK [84]. This creates a therapeutic window where targeting specific redox nodes could disrupt oncogenic signaling while minimizing effects on normal cells.
Metabolic Regulation Through Redox Sensors
Cellular metabolism is intricately connected to redox homeodynamics through multiple sensing mechanisms:
- AMPK signaling: Serves as an energy sensor activated under low ATP conditions. AMPK activation is potentiated by ROS through multiple mechanisms, including direct oxidation of cysteine residues in its regulatory subunits [87].
- mTORC1 pathway: A master regulator of cell growth that is inhibited under oxidative stress conditions, creating a redox-controlled balance between anabolic and catabolic processes [87].
- HIF-1α stabilization: Under hypoxic conditions, mitochondrial ROS production inhibits prolyl hydroxylases (PHDs) that target HIF-1α for proteasomal degradation, leading to HIF-1α stabilization and transcriptional activation of glycolytic enzymes and pro-angiogenic factors [15].
The intersection between redox biology and metabolism creates vulnerabilities in cancer cells, which often display metabolic reprogramming (Warburg effect) accompanied by increased ROS generation. Targeting the redox sensors that control these metabolic adaptations represents a promising therapeutic strategy [15].
Stress Response and Survival Pathways
Multiple stress-responsive transcription factors are regulated through redox-sensitive mechanisms:
- NRF2-KEAP1 system: The primary regulator of antioxidant response elements. Under basal conditions, NRF2 is ubiquitinated by the KEAP1-CUL3 complex and degraded. Oxidative modification of critical cysteine residues in KEAP1 disrupts this complex, allowing NRF2 accumulation and translocation to the nucleus where it activates transcription of antioxidant and detoxification genes [15].
- NF-κB pathway: A key regulator of inflammation and cell survival that is activated by ROS through multiple mechanisms, including IKK activation and IκB degradation [84].
- p53 activation: The tumor suppressor p53 is activated by various stresses including oxidative damage, coordinating cell cycle arrest, DNA repair, or apoptosis depending on signal intensity and context [15].
Table: Key Redox-Sensitive Nodes and Their Therapeutic Implications
| Target Node | Redox Modification | Biological Function | Therapeutic Opportunity |
|---|---|---|---|
| KEAP1-NRF2 | KEAP1 cysteine oxidation | Master regulator of antioxidant response | NRF2 activators for degenerative diseases; KEAP1 stabilizers for cancer |
| PTP1B | Catalytic Cys sulfenylation | Negative regulator of insulin and growth factor signaling | Reversible inhibitors for diabetes; activators for cancer |
| ATM kinase | Disulfide bond formation | DNA damage response, particularly double-strand breaks | Sensitizers for radiotherapy; inhibitors for neurological disorders |
| Peroxiredoxins | Cys overoxidation to sulfinic acid | H₂O2 sensing and scavenging | Prx mimics for oxidative stress; Prx inhibitors for hyperproliferative disorders |
| HSP33 | Disulfide bond formation | Redox-regulated chaperone | Activators for protein aggregation diseases |
Experimental Approaches for Studying Redox Switches
Quantitative Redox Proteomics
Comprehensive identification and quantification of redox-sensitive cysteine residues requires specialized proteomic approaches:
- Oxidation-isotope coded affinity tag (OxICAT): This methodology enables quantitative assessment of cysteine oxidation states in complex biological samples. The protocol involves: 1) Blocking free thiols with N-ethylmaleimide (NEM); 2) Reducing reversibly oxidized thiols with tris(2-carboxyethyl)phosphine (TCEP); 3) Labeling newly reduced thiols with heavy isotopically labeled ICAT reagent; 4) Denaturing proteins and labeling remaining reduced thiols with light ICAT; 5) Performing LC-MS/MS analysis to determine heavy:light ratios and quantify oxidation status [87].
- QTRP (Quantitative Thiol Reactivity Profiling): A gel-free method that utilizes iodoacetyl tandem mass tags (iodoTMT) to quantify cysteine reactivity across multiple samples simultaneously, allowing identification of redox-sensitive cysteines under different physiological conditions [85].
- Dimedone-based probes: Chemical probes that specifically react with sulfenic acids, enabling detection and identification of this transient oxidation intermediate. Modern derivatives include click-compatible alkyne- or azide-containing probes for enrichment and proteomic analysis [85].
Functional Validation of Redox Switches
Once candidate redox-sensitive cysteines are identified, rigorous validation is essential:
- Site-directed mutagenesis: Replacement of redox-sensitive cysteine with serine or alanine to create redox-dead mutants, or with aspartic acid to mimic the charged state of oxidized cysteine. Comparison of wild-type and mutant protein function under oxidizing conditions confirms the functional importance of specific cysteine residues [85].
- In vitro oxidation assays: Purified recombinant proteins are treated with controlled concentrations of oxidants (H₂O₂, HOCl) or physiological oxidant-generating systems, followed by assessment of functional changes (enzyme activity, conformational changes, protein-protein interactions) [85].
- Structural biology approaches: X-ray crystallography and NMR spectroscopy provide atomic-level insight into structural consequences of cysteine oxidation, revealing allosteric mechanisms, disulfide bond formation, and conformational changes [85].
Therapeutic Targeting Strategies
Small Molecule Targeting of Redox-Sensitive Cysteines
The unique chemical properties and microenvironment of redox-sensitive cysteines create opportunities for selective pharmacological targeting:
- Electrophilic compounds: Naturally occurring phytochemicals (sulforaphane, curcumin) and synthetic molecules that modify critical cysteine residues in KEAP1, activating the NRF2 antioxidant response pathway. These compounds work by mimicking the effects of endogenous oxidative modifications [15].
- Allosteric inhibitors: Molecules that exploit oxidized cysteine conformations to achieve selectivity. For example, compounds that stabilize the sulfenic acid form of PTP1B show enhanced specificity compared to active-site directed inhibitors [84].
- Covalent inhibitors: Drugs designed to form reversible covalent bonds with thiolate anions in target proteins, such as inhibitors of mutant KRAS that exploit the enhanced nucleophilicity of cysteine 12 [15].
Context-Dependent Therapeutic Approaches
The therapeutic application of redox modulators must consider the paradoxical roles of ROS in different pathological contexts:
- Cancer: Strategies include: 1) Pro-oxidant therapies that further elevate ROS beyond the toxic threshold in cancer cells (arsenic trioxide, motexafin gadolinium); 2) Inhibitors of antioxidant systems to disrupt redox adaptation (glutathione synthesis inhibitors, thioredoxin reductase inhibitors); 3) Combination approaches where redox modulators sensitize tumors to conventional therapies [15] [84].
- Neurodegenerative diseases: Approaches focus on NRF2 activation to boost antioxidant capacity and inhibition of NOX enzymes to reduce chronic neuroinflammation [15] [88].
- Metabolic diseases: PTP1B inhibitors that target its redox-sensitive cysteine improve insulin sensitivity, while mitochondria-targeted antioxidants (MitoQ) address metabolic syndrome-associated oxidative stress [15].
The Scientist's Toolkit: Essential Reagents and Methodologies
Table: Key Research Reagent Solutions for Redox Biology Studies
| Reagent/Method | Specific Function | Key Applications | Technical Considerations |
|---|---|---|---|
| Dimedone-based probes | Specific detection of sulfenic acids | Identification of sulfenylated proteins in complex samples | Requires optimized fixation; click-chemistry compatible versions available |
| Iodoacetyl TMT | Quantitative thiol reactivity profiling | Parallel quantification of cysteine reactivity across multiple conditions | Critical to maintain consistent protein extraction and labeling conditions |
| NADPH oxidase inhibitors | Selective inhibition of NOX isoforms | Determining contribution of enzymatic vs mitochondrial ROS | Specificity varies (apocynin, VAS2870, GKT136901); confirm with genetic approaches |
| MitoTEMPO/MitoQ | Mitochondria-targeted antioxidants | Distinguishing mitochondrial from other cellular ROS sources | Accumulate in mitochondria 100-1000x over cytosolic concentrations |
| roGFP/Grx1-roGFP | Real-time monitoring of glutathione redox potential | Live-cell imaging of redox dynamics | Requires calibration for quantitative measurements; specific to glutathione redox couple |
| Ahp2-roGFP | Real-time monitoring of H₂O₂ levels | Live-cell H₂O₂ imaging with high temporal resolution | Specifically reacts with H₂O₂, not other ROS; can be targeted to subcellular compartments |
The transition from viewing redox processes through the lens of homeostasis to understanding them as homeodynamic networks represents a fundamental shift with profound therapeutic implications. By mapping the specific nodes within redox-regulated signaling pathways and developing compounds that precisely target pathological redox switches without disrupting physiological signaling, we enter an era of precision redox medicine.
Future progress will depend on developing better tools for monitoring redox dynamics in vivo, creating more specific modulators of redox-sensitive proteins, and establishing biomarkers that can stratify patients based on their specific redox pathophysiology. As our understanding of the redox code continues to deepen, so too will our ability to design therapies that restore physiological redox homeodynamics across a spectrum of diseases.
Redox homeostasis represents a dynamic equilibrium where the production of oxidizing and reducing species is precisely balanced by antioxidant systems, maintaining internal stability essential for normal cellular function [14]. The contemporary concept of redox homeodynamics, however, better captures the fluid, adaptive nature of this system, which continuously adjusts to environmental and metabolic challenges [3]. Within this framework, oxidative stress (OS)—an overabundance of reactive oxygen species (ROS)—has been extensively studied. In contrast, reductive stress (RS) has only recently been recognized as an equally disruptive condition characterized by the excessive accumulation of reducing equivalents, including NADH, NADPH, and reduced glutathione (GSH) [89] [90]. This shift toward a reduced intracellular environment disrupts redox-sensitive signaling, impairs mitochondrial function, and contributes to the pathogenesis of metabolic, cardiovascular, and neoplastic diseases [91] [90].
RS emerges from an imbalance where reductive forces overwhelm oxidative processes, creating a state that paradoxically can lead to increased ROS production through electron leakage from over-reduced electron transport chains [90]. This review explores the molecular mechanisms of RS, its pathophysiological roles, and the experimental and therapeutic strategies targeting this emerging therapeutic axis within the sophisticated paradigm of redox homeodynamics.
Molecular Mechanisms of Reductive Stress
Reductive stress originates from metabolic pathways that generate excessive reducing equivalents, overwhelming the cell's capacity to maintain redox equilibrium. Key sources include:
- Hyperactive Glycolysis and Pentose Phosphate Pathway (PPP): Enhanced glycolytic flux increases NADH production, while a stimulated PPP elevates NADPH levels, a crucial cofactor for regenerating reduced glutathione (GSH) from its oxidized form (GSSG) [90].
- Mitochondrial Dysfunction: Inhibition of the mitochondrial electron transport chain (ETC), whether from genetic mutations, hypoxia, or decreased ATP demand, reduces the oxidation of NADH to NAD+, leading to NADH accumulation [90].
- Excessive Antioxidant Supplementation: High doses of exogenous antioxidants (e.g., vitamins C and E, N-acetylcysteine) can disrupt the physiological redox balance, pushing the system toward a reductive state [90] [75].
- Impaired Oxidation of Reducing Equivalents: Deficiencies in electron acceptors like GSSG and oxidized thioredoxin (TrxSS) prevent the proper dissipation of reducing power, leading to electron leakage and paradoxical ROS formation despite a reduced cellular environment [90].
The Redox Paradox: Pro-Oxidant Effects of a Reducing Environment
A central paradox of RS is its capacity to induce oxidative damage. In a state of RS, the over-reduced NADH/NAD+ pool leads to electron leakage, particularly from mitochondrial Complex I, resulting in superoxide (O₂•⁻) formation [90]. Furthermore, a deficit of oxidized electron acceptors (GSSG, TrxSS) impairs the function of antioxidant enzymes like glutathione peroxidase, allowing H₂O₂ to accumulate [90]. This phenomenon, known as the "antioxidant paradox," explains why elevated levels of antioxidants do not necessarily confer protection and can even exacerbate oxidative damage [90].
core:signaling_pathways
Table 1: Key Redox Couples and Their Compartmentalization in Reductive Stress
| Redox Couple | Physiological Ratio | Redox Potential | Compartment | Change in RS |
|---|---|---|---|---|
| NADH/NAD+ | ~0.01 (Low) | -320 mV | Mitochondria/Cytosol | Significantly Increased |
| NADPH/NADP+ | ~100 (High) | -380 mV | Cytosol | Increased |
| GSH/GSSG | 30:1 to 100:1 | -290 mV | Cytosol | Markedly Increased |
| GSH/GSSG | >100:1 | ≤-300 mV | Mitochondria | Markedly Increased |
| GSH/GSSG | 1:1 to 3:1 | -175 to -185 mV | Endoplasmic Reticulum | Increased (Disrupts folding) |
Pathophysiological Consequences of Reductive Stress
Metabolic Disorders and Cardiovascular Disease
In the context of overnutrition and metabolic syndrome, nutrient excess drives hyperactive glycolysis and TCA cycle activity, generating substantial NADH [91]. This reductive environment disrupts insulin secretion and signaling, contributing to insulin resistance [89] [90]. Reductive stress also exacerbates adipose tissue dysfunction and promotes metabolic inflammation, establishing a vicious cycle that perpetuates metabolic dysregulation [89] [91].
In cardiovascular tissues, RS alters vascular smooth muscle cell function and myocardial metabolism [89]. The over-reduced state impairs calcium handling and compromises mitochondrial quality control, affecting outcomes in ischemia-reperfusion injury and contributing to the pathogenesis of specific cardiomyopathies [89] [57].
Cancer and Inflammation
RS plays a complex, dual role in oncology. Tumors often exploit a reductive environment to support survival and growth. Elevated levels of NADPH and GSH help buffer OS, a common feature of rapidly proliferating cancer cells, and support metabolic reprogramming toward anabolic synthesis [89] [90]. However, excessive RS can trigger proteotoxicity and mitochondrial dysfunction, potentially leading to apoptosis and representing an Achilles' heel that could be therapeutically exploited [89].
In inflammation, the interplay between OS and RS is crucial. While OS is a classic pro-inflammatory trigger, sustained RS can paradoxically impair immune defense, alter redox-sensitive signaling (e.g., NF-κB and Nrf2 pathways), and contribute to the progression of chronic inflammatory diseases [57].
Table 2: Reductive Stress in Disease Pathogenesis
| Disease Category | Key Molecular Mechanisms | Functional Consequences |
|---|---|---|
| Diabetes & Obesity | Disrupted insulin signaling; Adipose tissue macrophage activation; Increased NADH from nutrient flux | Insulin resistance; Systemic inflammation; β-cell dysfunction |
| Cardiovascular Disease | Altered myocardial metabolism; Impaired ETC function; Vascular smooth muscle dysfunction | Ischemia-reperfusion injury; Cardiomyopathy; Reduced contractility |
| Cancer | Buffering of oxidative stress; Metabolic reprogramming; Elevated GSH/GSSG & NADPH/NADP+ ratios | Tumor survival; Chemoresistance; Proteotoxicity (in severe RS) |
| Chronic Inflammation | Altered NF-κB & Nrf2 signaling; Immune cell dysfunction; Paradoxical ROS production | Autoimmunity; Neuroinflammation; Sustained inflammatory response |
Experimental Assessment and Methodologies
Core Analytical Techniques
Quantifying the reductive state of cells and tissues requires a multi-parametric approach, as no single biomarker fully captures RS. The following methodologies form the cornerstone of experimental assessment:
- NAD(H) and NADP(H) Quantification: Liquid chromatography-mass spectrometry (LC-MS/MS) provides the most accurate measurement of these pyridine nucleotides and their ratios (NADH/NAD+ and NADPH/NADP+), which are central to defining RS [89] [90]. Enzymatic cycling assays offer a more accessible alternative.
- Glutathione Status Analysis: The GSH/GSSG ratio is a classic redox indicator. Quantification can be performed via HPLC with electrochemical detection or fluorescent probes like monochlorobimane. A significantly elevated ratio is diagnostic of RS [90].
- Mitochondrial Functional Assays: High-resolution respirometry (e.g., Oroboros O2k) measures the mitochondrial oxygen consumption rate (OCR). In RS, OCR is often suppressed due to ETC inhibition. Concurrent measurement of ROS production (e.g., with MitoSOX) can detect the paradoxical increase in superoxide [91].
- Metabolic Flux Analysis: Using (^{13})C-labeled nutrients (e.g., glucose, glutamine) with LC-MS tracking allows researchers to map the flow of carbon through glycolysis, the PPP, and the TCA cycle, identifying the metabolic sources of excess NADH and NADPH [91] [90].
Perturbation and Intervention Protocols
To experimentally induce or alleviate RS, researchers employ specific reagents and genetic tools:
- RS Induction: Treatment with high-dose reducing agents like 1,4-dithiothreitol (DTT) or N-acetylcysteine (NAC) can artificially create a reductive environment. Genetic models, such as overexpression of glucose-6-phosphate dehydrogenase (G6PD) to stimulate the PPP or specific mutations that inhibit ETC complexes (e.g., in complex I), are also used [91] [90].
- RS Alleviation: The expression of LbNOX, an NADH oxidase from Lactobacillus brevis targeted to the cytosol or mitochondria, effectively oxidizes excess NADH and is a powerful genetic tool to counteract RS [91]. Pharmacological agents like nicotinamide riboside (NR) can enhance NAD+ pools, facilitating NADH oxidation [91].
core:experimental_workflow
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents and Tools for Reductive Stress Research
| Reagent/Tool | Category | Primary Function | Example Application |
|---|---|---|---|
| LbNOX | Genetic Tool | Targeted NADH oxidation; Reduces cytosolic/mitochondrial NADH | Validating causal role of NADH in disease phenotypes [91] |
| Nicotinamide Riboside (NR) | Small Molecule | NAD+ Precursor; Increases NAD+ pool to facilitate NADH oxidation | Testing metabolic benefits of shifting NADH/NAD+ ratio [91] |
| Dithiothreitol (DTT) | Chemical Inducer | Thiol-reducing agent; Artificially creates reductive environment | In vitro induction of ER stress via disruption of disulfide bonds [90] |
| N-Acetylcysteine (NAC) | Chemical Inducer | Cysteine pro-drug; Boosts glutathione synthesis | Investigating paradoxical pro-oxidant effects at high doses [90] |
| MitoSOX Red | Fluorescent Probe | Detects mitochondrial superoxide (O₂•⁻) | Measurement of paradoxical ROS burst in RS [90] [92] |
| (^{13})C-Glucose | Tracer | Tracks carbon fate through metabolic pathways | Mapping flux through glycolysis vs. PPP in RS models [91] [90] |
Therapeutic Targeting and Future Directions
The bidirectional nature of redox imbalance necessitates a departure from broad-spectrum antioxidant therapies, which can inadvertently exacerbate RS [90] [3]. Future strategies must be precise and context-dependent.
- Redox-Modulating Therapies: Approaches that selectively target the source of excess reducing equivalents are under development. This includes inhibitors of specific metabolic enzymes that drive NADPH production and activators of NADH-shuttling systems to improve mitochondrial oxidation [89] [15].
- NRF2 Pathway Modulation: While NRF2 activation is a canonical antioxidant response, its persistent activation in chronic diseases can promote RS. Fine-tuning NRF2 activity—activating it transiently or inhibiting it in specific contexts—represents a sophisticated therapeutic avenue [57] [15].
- Drug Repurposing and Nanomedicine: Existing metabolic drugs, such as metformin, may exert part of their benefit by modulating redox homeostasis. Nanocarriers can be designed to deliver redox-active agents specifically to diseased tissues, minimizing off-target effects and preventing systemic RS [89].
A critical challenge is the development of non-invasive, selective biomarkers for RS to facilitate patient stratification and monitor therapeutic efficacy. Furthermore, future research must define the thresholds at which physiological redox adaptations transition into pathological RS, enabling truly personalized redox medicine.
Reductive stress is an underappreciated yet critical component of redox homeodynamics, intricately involved in the pathogenesis of major human diseases. Its paradoxical ability to drive oxidative damage and disrupt cellular signaling underscores the complexity of redox biology. Moving beyond the obsolete model of simply scavenging oxidants, a new era of redox medicine is emerging. This era demands a precise understanding of context-specific redox imbalances and the development of targeted therapies that can restore the delicate, dynamic equilibrium of redox homeodynamics, offering hope for treating a wide spectrum of chronic diseases.
The conceptual framework for modulating redox states in disease has evolved from a static view of homeostasis—the maintenance of a stable internal environment—to the more dynamic concept of homeodynamics, which recognizes the complex, adaptive interplay between oxidative and reductive processes. This paradigm shift is critical for developing effective spatiotemporally controlled delivery systems, as it acknowledges that successful therapeutic intervention requires dynamic modulation of redox states rather than simply restoring a single equilibrium point. Redox homeodynamics encompasses the intricate network of signaling pathways and feedback loops that organisms use to maintain functional stability in response to continuous internal and external challenges. Within this framework, reductive stress (RS)—an overabundance of reducing equivalents such as NADPH, NADH, and glutathione—has emerged as equally significant as oxidative stress (OS) in driving pathological processes, particularly in chronic inflammatory diseases [57].
The tumor microenvironment (TME) represents a prime example of dysregulated redox homeodynamics, characterized by significant redox imbalances compared to normal tissues. Cancer cells typically exhibit elevated intracellular glutathione (GSH) levels (2-10 mM), approximately three orders of magnitude higher than extracellular concentrations, creating a steep redox gradient that can be exploited for targeted drug delivery [93]. This redox disparity, coupled with other TME features such as hypoxia and metabolic reprogramming, provides a biochemical foundation for designing spatiotemporally controlled delivery systems that specifically target diseased tissues while minimizing off-target effects on healthy cells. The development of such systems requires sophisticated strategies that can respond to these dynamic redox cues with precise spatial and temporal resolution.
Redox Signaling Fundamentals and Molecular Targets
Key Molecular Players in Redox Homeodynamics
Cellular redox homeodynamics is governed by a complex interplay between reactive species generation and antioxidant defense systems. Reactive oxygen species (ROS), including superoxide (O₂•−), hydrogen peroxide (H₂O₂), and hydroxyl radicals (•OH), are continuously produced primarily through mitochondrial oxidative phosphorylation, with additional contributions from NADPH oxidase (NOX) family enzymes and the endoplasmic reticulum [15]. These species function as crucial signaling molecules at physiological levels but cause damage at pathological concentrations. The counterbalancing antioxidant system operates through multiple layers of defense: the first line includes enzymes like superoxide dismutase (SOD), catalase, and glutathione peroxidase (GPx), while the second line involves redox buffers such as the glutathione (GSH/GSSG) and thioredoxin systems, supported by NADPH as a key reducing equivalent [15].
The transcription factor NRF2 serves as a master regulator of the adaptive antioxidant response. Under basal conditions, NRF2 is bound to its repressor KEAP1 and targeted for degradation. However, oxidative modifications of critical cysteine residues in KEAP1 lead to NRF2 stabilization and nuclear translocation, where it activates the transcription of numerous cytoprotective genes [15]. This system represents a fundamental homeodynamic circuit that dynamically adjusts cellular antioxidant capacity in response to redox challenges. Simultaneously, redox-sensitive signaling pathways including NF-κB, MAPK, and inflammasome activation translate redox fluctuations into altered gene expression and inflammatory responses, creating intricate cross-talk between redox status and immune function [57].
Redox Dysregulation in Disease
Deviation from redox homeodynamics manifests as either oxidative or reductive stress, both implicated in disease pathogenesis. Chronic inflammation provides a compelling example of redox dysregulation, where oxidative stress activates redox-sensitive transcription factors like NF-κB, driving pro-inflammatory cytokine production and perpetuating inflammatory cycles [57]. Conversely, reductive stress—characterized by excessive reducing equivalents—can paradoxically sustain inflammatory responses by altering disulfide bond formation in signaling proteins and impairing mitochondrial function [57].
In cancer, redox dysregulation is a hallmark, with tumor cells maintaining high antioxidant capacity (particularly elevated GSH) to counteract increased ROS generation from accelerated metabolism. This adaptation creates a vulnerable dependency that can be therapeutically exploited [93]. Similar redox imbalances feature in neurodegenerative disorders, cardiovascular diseases, and metabolic syndromes, making spatiotemporal control of redox-modulating agents a broadly relevant therapeutic approach.
Spatiotemporal Control Strategies for Redox Modulation
Internally Triggered Redox-Responsive Systems
Table 1: Internally Triggered Redox-Responsive Nanocarriers
| Stimulus | Responsive Element | Release Mechanism | Key Features | Applications |
|---|---|---|---|---|
| High GSH/GSSG Ratio | Disulfide bonds (S-S) | Thiol-disulfide exchange, nanoparticle disintegration | High sensitivity to intracellular TME (2-10 mM GSH); promotes GSH depletion | Tumor-specific drug delivery; combinatorial therapy with ROS-inducing agents [93] |
| ROS Overproduction | Selenide bonds, thioketal, phenylboronic acid | Oxidative cleavage of linkers | Responds to elevated H₂O₂/•OH in inflamed/infected tissues | Targeted anti-inflammatory delivery; atherosclerosis, neurodegeneration [94] |
| Abnormal Enzyme Activity | Enzyme-cleavable substrates (e.g., esterases, phosphatases) | Enzymatic hydrolysis of covalent drug-carrier bonds | High substrate specificity; often combined with other stimuli | Esterase-rich tumor targeting; phosphatase-activated prodrugs [94] |
Internally triggered systems exploit pathological biochemical gradients inherent to disease microenvironments for controlled drug release. Disulfide bond-based nanocarriers represent one of the most extensively studied redox-responsive systems, leveraging the significant differential in glutathione (GSH) concentrations between the extracellular space (∼2-20 μM) and intracellular compartments (2-10 mM) [93]. These systems utilize disulfide bonds incorporated into polymer backbones, cross-linkers, or side chains that undergo cleavage via thiol-disulfide exchange reactions with GSH, leading to structural disassembly and cargo release. The thermodynamic favorability (ΔG < 0) of these exchange reactions drives the responsiveness, though kinetics can be modulated through molecular design [93]. A significant advantage of this approach is its self-amplifying nature: GSH consumption during disulfide cleavage further disrupts redox homeostasis, potentially enhancing oxidative stress-based therapies and triggering regulated cell death pathways like ferroptosis and cuproptosis through GPX4 inhibition and DLAT oligomerization, respectively [93].
Externally Triggered Spatiotemporal Control Systems
Table 2: Externally Triggered Redox-Modulating Delivery Systems
| Stimulus | Nanoparticle Composition | Control Mechanism | Spatiotemporal Precision | Therapeutic Applications |
|---|---|---|---|---|
| NIR Light | Gold nanoparticles, PNIPAM hybrid nanogels | Photothermal heating-induced conformational change | High (mm scale); tunable via wavelength, intensity, duration | Plasmonic hybrid nanogels for cytosolic delivery via endosomal rupture [95] |
| Magnetic Fields | Iron oxide nanoparticles | Hyperthermia, mechanical force | Moderate to high (cm scale) | Magnetic field-guided targeting and thermal ablation [94] |
| Ultrasound | Microbubbles, liposomes | Cavitation, thermal effects, membrane permeabilization | Moderate (cm scale); good tissue penetration | Enhanced drug penetration in solid tumors [94] |
Externally triggered systems provide superior spatiotemporal control by responding to physical stimuli applied directly to target tissues. Near-infrared (NIR) light-responsive systems are particularly promising due to superior tissue penetration and minimal phototoxicity compared to UV/visible light. These systems often incorporate photothermal agents like gold nanoparticles (GNPs) that convert light energy to heat, inducing conformational changes in temperature-responsive polymers such as poly(N-isopropyl acrylamide) (PNIPAM) [95]. Advanced designs include self-integrated plasmonic hybrid nanogels (PHNs) that combine GNPs with thermo-responsive polymers in a single nanostructure, enabling light-driven drug release through photothermally induced conformational changes and facilitating endosomal escape through localized membrane disruption [95]. This approach achieves precise spatiotemporal control by enabling drug release only in illuminated areas, with parameters such as wavelength, power, illumination time, and area providing additional control dimensions [95].
Other external triggers include magnetic fields using iron oxide nanoparticles for both targeting via magnetic gradients and triggering via hyperthermia, and ultrasound employing microbubbles or nanodroplets that undergo cavitation or thermal effects for localized drug release [94]. These modalities can be combined with redox-responsive elements to create multi-stimuli systems that leverage both biological and physical triggers for enhanced specificity.
Experimental Protocols and Methodologies
Synthesis of Redox-Responsive Disulfide-Based Nanocarriers
Protocol: Synthesis of Disulfide-Cross-Linked Polymeric Nanoparticles
- Materials: Cystamine dihydrochloride (disulfide-containing cross-linker), N-isopropylacrylamide (NIPAM, thermoresponsive monomer), acrylic acid (AA, for carboxyl functionality), ammonium persulfate (APS, initiator), tetramethylethylenediamine (TEMED, accelerator), dialysis membrane (MWCO 3.5-14 kDa).
- Procedure:
- Dissolve cystamine (150 mg, 0.67 mmol), NIPAM (200 mg, 1.77 mmol), and AA (25 mg, 0.35 mmol) in 10 mL deoxygenated deionized water under nitrogen purge.
- Add APS solution (20 mg in 0.5 mL water) and TEMED (20 μL) to initiate radical polymerization.
- React for 6-12 hours at room temperature with continuous stirring under nitrogen atmosphere.
- Purify the resulting nanoparticles by dialysis against distilled water for 24 hours with frequent water changes.
- Lyophilize the purified nanoparticles for long-term storage at -20°C.
- Characterization: Determine particle size and polydispersity by dynamic light scattering (DLS). Confirm disulfide incorporation via Raman spectroscopy (S-S stretch at ~500-550 cm⁻¹) or Ellman's assay for free thiol quantification. Verify redox-responsive disassembly by treating with 10 mM dithiothreitol (DTT) or GSH and monitoring size reduction via DLS [93] [96].
Fabrication of NIR-Responsive Plasmonic Hybrid Nanogels
Protocol: One-Pot Synthesis of Gold-PNIPAM Hybrid Nanogels
- Materials: Chloroauric acid (HAuCl₄, gold precursor), N-isopropylacrylamide (NIPAM), N,N'-methylenebisacrylamide (MBA, cross-linker), Darocur 1173 (photoinitiator), alginate-based linker (optional, for enhanced stability).
- Procedure:
- Prepare reaction mixture containing HAuCl₄ (0.5-1 mM), NIPAM (100 mM), MBA (5 mM), and Darocur 1173 (2 mM) in deionized water.
- Expose the mixture to 365 nm UV light (1.2 W/cm² intensity) for 10 minutes with continuous stirring to simultaneously reduce gold ions and polymerize monomers.
- Monitor nanoparticle growth by measuring hydrodynamic diameter and UV-Vis absorbance at regular intervals until stable (~10 minutes).
- Purify resulting plasmonic hybrid nanogels (PHNs) by centrifugation (15,000 rpm, 20 minutes) and resuspend in PBS or water.
- For drug loading, incubate purified PHNs with drug solution (e.g., doxorubicin) for 24 hours followed by removal of unencapsulated drug via filtration or centrifugation.
- Characterization: Analyze morphology and gold nanoparticle integration via transmission electron microscopy (TEM). Confirm composition by X-ray photoelectron spectroscopy (XPS) for elemental analysis. Evaluate photothermal conversion efficiency by measuring temperature increase under NIR laser irradiation (e.g., 808 nm, 1-2 W/cm²). Assess drug release kinetics with and without laser irradiation using dialysis-based methods with UV-Vis detection [95].
In Vitro Assessment of Redox-Responsive Drug Release
Protocol: Evaluating GSH-Triggered Drug Release Kinetics
- Materials: Redox-responsive nanoparticles, glutathione (reduced form, GSH), phosphate-buffered saline (PBS, pH 7.4), dialysis membrane (appropriate MWCO), fluorescence spectrometer or HPLC.
- Procedure:
- Prepare nanoparticle suspensions in release media (PBS, pH 7.4) with varying GSH concentrations (0 μM, 10 μM, 1 mM, 10 mM) to simulate extracellular and intracellular environments.
- Place samples in dialysis tubes and immerse in corresponding release media maintained at 37°C with gentle shaking.
- At predetermined time points, withdraw release medium samples and replace with fresh pre-warmed medium to maintain sink conditions.
- Analyze drug concentration in collected samples using HPLC for precise quantification or fluorescence spectroscopy for fluorescent drugs (e.g., doxorubicin).
- Calculate cumulative drug release percentage and plot release kinetics for each GSH condition.
- Data Analysis: Compare release profiles at different GSH concentrations to confirm redox responsiveness. Fit data to mathematical models (e.g., Korsmeyer-Peppas, Higuchi) to elucidate release mechanisms. Significant acceleration of drug release at high GSH concentrations (mM range) confirms successful redox-triggered deployment [93].
Pathway Visualization and Experimental Workflows
Redox-Responsive Drug Release Mechanism
Diagram 1: Mechanism of GSH-Triggered Drug Release from Redox-Responsive Nanocarriers. This pathway illustrates how high intracellular glutathione (GSH) concentrations in target cells trigger disulfide bond cleavage in nanocarriers, leading to controlled drug release and subsequent therapeutic effects including GSH depletion-induced cell death pathways.
Plasmonic Hybrid Nanogel Synthesis and Application
Diagram 2: Workflow for Plasmonic Hybrid Nanogel Synthesis and NIR-Triggered Drug Delivery. This experimental workflow outlines the one-pot synthesis of light-responsive nanocarriers and their application in spatially controlled drug delivery through near-infrared (NIR) light activation, which triggers both drug release and endosomal escape mechanisms.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Developing Redox-Responsive Delivery Systems
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Redox-Sensitive Linkers | Cystamine, Disulfide-diacrylate, DSP (Dithiobis(succinimidyl propionate)) | Incorporates cleavable disulfide bonds; enables GSH-responsive degradation | Critical for intracellular targeting; kinetics vary with linker structure [93] |
| Stimuli-Responsive Polymers | PNIPAM (Poly(N-isopropylacrylamide)), PLGA (Poly(lactic-co-glycolic acid)), Chitosan-derivatives | Provides structural framework; enables temperature, pH, or enzyme responsiveness | PNIPAM offers sharp thermal transition at ~32°C; ideal for photothermal systems [95] |
| Photothermal Agents | Gold nanoparticles (spheres, rods, shells), Polydopamine, Carbon-based materials | Converts light to heat; triggers conformational changes or endosomal escape | Gold offers tunable plasmonics; size and shape determine absorption maxima [95] |
| Cross-linking Agents | MBA (N,N'-methylenebisacrylamide), EGDA (ethylene glycol diacrylate) | Provides structural integrity to nanocarriers | Cross-link density affects drug loading and release kinetics [95] |
| Antioxidant/Anti-inflammatory Agents | Molecular hydrogen (H₂), N-acetylcysteine (NAC), Curcumin, Resveratrol | Directly modulates redox balance; scavenges ROS | H₂ selectively neutralizes •OH and ONOO⁻; requires specialized delivery [97] |
| Characterization Tools | Ellman's reagent (DTNB), DCFH-DA, Amplex Red | Quantifies thiol groups, ROS production | Essential for validating redox responsiveness and mechanism [93] |
The strategic integration of spatiotemporal control technologies with redox-modulating agents represents a paradigm shift in precision medicine, moving beyond the simplistic antioxidant approaches that have dominated redox therapeutics. By embracing the concept of redox homeodynamics, next-generation delivery systems can dynamically interface with pathological redox states to restore physiological signaling rather than merely suppressing oxidative processes. The most promising approaches combine multiple responsive elements—such as disulfide bonds for GSH sensitivity with photothermal nanoparticles for external control—creating multi-stimuli systems that achieve unprecedented specificity.
Future advancements will likely focus on developing more sophisticated feedback-controlled systems that can autonomously adjust therapeutic output based on real-time redox status, potentially through integration with biosensing elements. Additionally, addressing the challenge of reductive stress as a complementary therapeutic target will expand the application of these technologies beyond classic oxidative stress conditions. As our understanding of redox biology deepens and nanofabrication techniques advance, spatiotemporally controlled redox modulation will continue to evolve toward increasingly precise, dynamic, and personalized therapeutic interventions capable of addressing the complex redox dynamics in cancer, chronic inflammation, neurodegeneration, and other redox-related disorders.
Validating the Framework: Comparative Analysis of Homeodynamics in Disease and Therapy
The conceptual framework for understanding redox balance in biological systems has evolved from a static homeostasis model to a dynamic homeodynamics paradigm. Redox homeostasis traditionally describes a stable, steady-state balance between reactive oxygen species (ROS) production and neutralization by antioxidant defenses [3]. In contrast, redox homeodynamics recognizes redox states as a continuous, adaptive flow process that maintains system stability through dynamic interactions and feedback loops [3]. This distinction is particularly crucial in cardiac physiology, where redox processes function not merely as potential damaging agents but as essential hormetic signals that facilitate cellular communication through adaptive proteins in cardiovascular tissue [98] [99].
During cardiopulmonary bypass (CPB), this dynamic balance is profoundly disrupted, creating a state of redox dyshomeostasis characterized by excessive ROS production that overwhelms compensatory mechanisms [98] [100]. The heart failure state prior to surgery establishes a precondition of altered redox homeodynamics, making myocardial tissue particularly vulnerable to the oxidative insult of CPB. Understanding these dynamics provides critical insights for developing targeted therapeutic strategies to mitigate postoperative complications in cardiac surgery patients [100] [99].
Redox Biomarker Alterations in CPB: Quantitative Analysis
Systemic Redox Biomarker Changes
Comprehensive analysis of redox biomarkers in patients undergoing open-heart surgery with CPB reveals significant alterations in both oxidative damage markers and antioxidant capacity. The following table summarizes key quantitative changes observed in controlled studies:
Table 1: Systemic Redox Biomarker Changes Following Cardiopulmonary Bypass
| Biomarker Category | Specific Biomarker | Pre-CPB Value | Post-CPB Value | Statistical Significance (p-value) | Biological Interpretation |
|---|---|---|---|---|---|
| Protein Oxidation | Protein Carbonyl | Elevated baseline | Significantly increased | Pre-op: p=0.009Post-op: p=0.013 [98] | Marker of irreversible oxidative protein damage |
| Antioxidant Enzymes | Glutathione Peroxidase (GPx) | Variable baseline | Significantly decreased | p=0.000 [98] | Reduced capacity to eliminate lipid hydroperoxides |
| Antioxidant Enzymes | Catalase (CAT) | Predictive baseline activity | Altered activity | p=0.017 [98] | Importance in eliminating increased hydroperoxide load before CPB |
| Transcription Coactivators | PGC-1α | Baseline levels | Significant variations | p=0.000 [98] | Key regulator of mitochondrial biogenesis and antioxidant defense |
Heart Failure-Specific Redox Perturbations
Patients with preoperative heart failure, particularly those with reduced ejection fraction (HFrEF), demonstrate exaggerated redox imbalances following CPB compared to those with preserved ejection fraction (HFpEF):
Table 2: Redox Biomarker Profiles in Heart Failure Patients Undergoing CPB
| Biomarker | HFpEF Group | HFrEF Group | Biological Significance | Clinical Correlation |
|---|---|---|---|---|
| 3-Nitrotyrosine (3-NT) | Moderate levels | Significantly elevated in plasma and atrial tissue [100] | Marker of peroxynitrite-mediated protein damage | Associated with increased myocardial oxidative damage |
| Malondialdehyde (MDA) | Moderate levels | Significantly elevated in plasma and atrial tissue [100] | Lipid peroxidation product | Indicates membrane damage and oxidative stress severity |
| NLRP3 Inflammasome | Moderate expression | Markedly elevated in atrial tissue and pericardial fluid [100] | Inflammatory pathway activation | Linked to postoperative atrial fibrillation (pAF) |
| IL-1β and IL-18 | Moderate levels | Significantly increased [100] | Pro-inflammatory cytokines | Drivers of sterile inflammation and cardiac remodeling |
Experimental Methodologies for Assessing Redox Homeodynamics
Patient Selection and Study Design
Investigation of redox homeodynamics in CPB requires carefully controlled clinical studies with specific inclusion criteria:
- Population: Adults aged 18-75 years undergoing elective coronary artery bypass graft (CABG) surgery or isolated valve replacement surgery [98] [99]
- Exclusion Criteria: Combined CABG and valve procedures, emergency surgery, obesity (BMI >30 kg/m²) [98]
- Control Groups: Patients with valvular disease without documented atherosclerotic cardiovascular disease provide comparative groups for assessing systemic redox effects [98]
- Sample Size Calculation: Determined using statistical power analysis (95% confidence interval, power ratio of 0.95) with minimum sample size of 24 patients per group [98]
Sample Collection and Processing Protocols
Standardized sample collection procedures are critical for reliable redox biomarker assessment:
- Timing: Venous blood samples collected half an hour before CPB and within the first half hour after CPB termination [98]
- Processing: Centrifugation at 3000 rpm for 15 minutes at 4°C to obtain serum [98]
- Storage: Aliquoting and immediate storage at -80°C until analysis to preserve redox status [98]
- Tissue Sampling: Intraoperative collection of atrial tissue biopsies and pericardial fluid for localized assessment of redox changes [100]
Analytical Techniques for Redox Biomarker Quantification
Comprehensive assessment of redox homeodynamics requires multiple analytical approaches:
- Spectrophotometric Methods: For measuring antioxidant enzyme activities (catalase, glutathione peroxidase) and lipid peroxidation products (MDA, TBARS) [98] [100]
- Immunochemical Methods: For quantifying transcription factors (Nrf2, PGC-1α) and protein oxidation markers (protein carbonyls, 3-nitrotyrosine) [98] [99]
- Immunohistochemistry: For spatial localization of ROS, 3-NT, and NLRP3 in atrial tissue sections [100]
- ROC Analysis: Statistical method for evaluating biomarker predictive value for clinical outcomes [98]
Molecular Mechanisms and Signaling Pathways
Redox Signaling Pathways in Cardiac Tissue
The complex interplay of redox-sensitive signaling pathways during CPB involves both adaptive and maladaptive responses:
Redox Signaling Pathways Activated During CPB
Transcription Factor Regulation in Redox Homeodynamics
Key transcription factors orchestrate the adaptive response to redox challenges during CPB:
Nrf2-Keap1 Pathway: Nrf2 is a critical redox-sensitive transcription factor that dissociates from its inhibitor Keap1 under oxidative stress, translocating to the nucleus to activate antioxidant response element (ARE)-mediated gene expression [98] [99]. This includes genes encoding NAD(P)H dehydrogenase (quinone 1) (NQO1), superoxide dismutase (MnSOD), catalase (CAT), and glutathione peroxidases (GPx) [99].
PGC-1α Activation: This transcriptional coactivator integrates mitochondrial biogenesis with antioxidant defense by coordinating the expression of antioxidant genes through interaction with Nrf2 [98] [99]. PGC-1α promotes mitochondrial oxidative metabolism, neovascularization, and fatty acid oxidation in heart muscle [98].
NLRP3 Inflammasome Activation: In HFrEF patients, heightened oxidative stress triggers NLRP3 inflammasome assembly, leading to caspase-1 activation and subsequent maturation of pro-inflammatory cytokines IL-1β and IL-18, creating a vicious cycle of inflammation and oxidative damage [100].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Redox Homeodynamics Studies
| Reagent/Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| Oxidative Damage Assay Kits | Protein Carbonyl ELISA, 3-Nitrotyrosine ELISA, Lipid Hydroperoxide Assay | Quantification of oxidative modification of proteins and lipids | Sample collection and storage at -80°C is critical for accurate measurements |
| Antioxidant Enzyme Activity Assays | Catalase Activity Assay, Glutathione Peroxidase Assay, Superoxide Dismutase Activity Assay | Assessment of endogenous antioxidant defense capacity | Enzyme activities are sensitive to freeze-thaw cycles; analyze promptly |
| Transcription Factor Analysis Kits | Nrf2 Transcription Factor Assay, PGC-1α ELISA, NLRP3 Inflammasome Assay | Evaluation of redox-sensitive signaling pathway activation | Nuclear extraction required for transcription factor studies |
| Molecular Biology Reagents | qPCR primers for NQO1, GPx, CAT, IL-1β, IL-18 | Gene expression analysis of antioxidant and inflammatory markers | Use reference genes appropriate for cardiac tissue |
| Immunohistochemistry Reagents | ROS detection probes, antibodies against 3-NT, NLRP3 | Spatial localization of oxidative stress and inflammation in tissue sections | Optimal fixation conditions vary by antibody |
Methodological Workflow for Comprehensive Redox Assessment
Comprehensive Redox Assessment Workflow
The shift from viewing redox imbalance merely as "increased oxidative stress and decreased biofunction" to understanding the physiological role of redox signaling regulation represents a paradigm change in cardiovascular medicine [98] [99]. The identification of specific biomarkers such as protein carbonyls, glutathione peroxidase, catalase, and PGC-1α provides actionable targets for therapeutic intervention [98]. Future research on the effects of CPB on systemic redox regulation processes through redox signaling mechanisms will significantly contribute to developing targeted strategies to minimize oxidative damage associated with cardiac surgery [98] [100] [99]. The homeodynamics perspective offers a more comprehensive framework for understanding the temporal evolution of redox changes in heart failure patients undergoing CPB, potentially leading to personalized approaches based on preoperative redox profiles.
The conceptual framework for understanding cellular redox regulation has evolved from a static homeostasis to a dynamic homeodynamic model. Redox homeodynamics recognizes that the redox state is not a fixed equilibrium but a continuous, adaptive interplay between oxidant production and antioxidant capacity, essential for maintaining normal physiological function [3]. In cancer biology, this paradigm is critically exploited; malignant cells exhibit a "redox paradox" where they operate under a state of chronic, elevated oxidative stress that simultaneously drives pro-tumorigenic signaling and creates a context-specific vulnerability [81] [101]. Cancer cells successfully navigate this paradoxical state through metabolic reprogramming that increases reactive oxygen species (ROS) generation while concomitantly upregulating powerful antioxidant systems to maintain a new, precarious redox homeodynamic set point [81] [101] [3]. This reprogramming creates a malignant redox state characterized by dependence on a hyperactive antioxidant shield, fundamentally distinguishing it from the redox state of normal cells and thereby presenting a therapeutic window for selective targeting [81] [102]. The strategic disruption of this finely tuned, yet vulnerable, homeodynamic balance represents a novel frontier in targeted cancer therapy, moving beyond traditional cytotoxic approaches to mechanistically target the core redox infrastructure of cancer cells [81] [101] [102].
Molecular Architecture of the Malignant Redox State
Cancer cells exhibit a multi-faceted reprogramming of ROS generation, leveraging endogenous sources to create a pro-tumorigenic signaling environment. Key sources of elevated ROS include:
- Mitochondrial Dysfunction: The mitochondrial electron transport chain (ETC) is a primary ROS source. Electron leakage from Complex I and Complex III generates superoxide anion (O₂•⁻), which is rapidly converted to hydrogen peroxide (H₂O₂) by superoxide dismutase (SOD) [81]. Cancer cells, despite possessing functional mitochondria, often exhibit heightened ETC activity and metabolic stress that increase electron leakage, thereby elevating ROS production [81] [15].
- NADPH Oxidases (NOXs): The NOX enzyme family, particularly NOX1, NOX2, and NOX4, catalyzes the deliberate generation of O₂•⁻ by transferring electrons from NADPH to molecular oxygen [81] [15]. NOX-derived ROS and mitochondrial ROS engage in a positive feedback loop, mutually amplifying their production. Furthermore, NOX activation is linked to oncogenic signaling pathways, such as those driven by RAS [81].
- Endoplasmic Reticulum (ER) Stress: The ER contributes to ROS generation through oxidative protein folding, where O₂ acts as a source of oxidizing equivalents for disulfide bond formation, producing H₂O₂ as a byproduct [81]. Under conditions of ER stress, protein misfolding further exacerbates ROS production, initiating the unfolded protein response [81].
Table 1: Primary Sources of ROS in Cancer Cells
| ROS Source | Key Enzymes/Components | Primary ROS Generated | Role in Oncogenesis |
|---|---|---|---|
| Mitochondria | ETC Complex I & III | O₂•⁻, H₂O₂ | Heightened metabolic activity, Warburg effect [81] |
| NADPH Oxidases | NOX1, NOX2, NOX4, NOX5 | O₂•⁻ | Oncogenic signaling (e.g., RAS), feedback with mitochondria [81] [15] |
| Endoplasmic Reticulum | Protein Disulfide Isomerase (PDI), ERO1 | H₂O₂ | Oxidative protein folding, ER stress response [81] |
Adaptive Antioxidant Defense Systems
To survive this self-inflicted oxidative onslaught, cancer cells co-opt and hyperactivate core cellular antioxidant systems, creating a powerful, interconnected defense shield. The major systems include:
- The Nrf2-Keap1 Axis: Nrf2 is the master regulator of the antioxidant response. Under basal conditions, Nrf2 is bound by Keap1 and targeted for proteasomal degradation. Oxidative stress or oncogenic signaling leads to Keap1 cysteine modification, Nrf2 stabilization, and its translocation to the nucleus, where it activates the transcription of a battery of antioxidant and cytoprotective genes [81] [15]. These genes include NAD(P)H quinone dehydrogenase 1 (NQO1), heme oxygenase-1 (HO-1), and the enzymes for glutathione synthesis [81] [103] [15].
- The Glutathione (GSH) System: Glutathione is the most prevalent cellular thiol and a critical redox buffer. The GSH:GSSG ratio is a key indicator of cellular redox state [62]. GSH serves as a cofactor for enzymes like glutathione peroxidases (GPx), which reduce H₂O₂ and lipid peroxides, and glutathione S-transferases (GSTs), involved in detoxification [81] [62]. Many tumors exhibit elevated GSH levels, which contribute to drug resistance [62] [104].
- The Thioredoxin (Trx) System: This system, comprising thioredoxin (Trx), thioredoxin reductase (TrxR), and NADPH, works in parallel with the GSH system to reduce protein disulfides and peroxides, maintaining a reducing intracellular environment [81] [102]. It is crucial for DNA synthesis and apoptosis regulation [102].
Figure 1: The Malignant Redox Homeodynamic Network. Cancer cells exhibit increased ROS from mitochondria, NOX enzymes, and the ER. This drives oncogenic signaling (e.g., PI3K/AKT) and simultaneously activates master antioxidant systems (Nrf2, GSH, Trx) to maintain a new, pro-tumorigenic redox set point [81] [101].
Therapeutic Strategies to Disrupt Redox Homeodynamics
The reliance of cancer cells on a rewired redox state represents a compelling therapeutic vulnerability. Strategies aim to pharmacologically "tip the scales," pushing the already-stressed cancer cell beyond its homeodynamic capacity into lethal oxidative distress.
Pro-oxidant Therapies
This approach aims to directly overwhelm the antioxidant defenses of cancer cells. Agents include:
- High-Dose Vitamin C (Ascorbic Acid): Pharmacological doses can generate H₂O₂ in the extracellular space, exploiting the cancer cell's often altered redox-active metal metabolism and reduced capacity to detoxify peroxides, leading to selective tumor cell death [81] [101].
- Arsenic Trioxide (ATO): An established therapeutic for acute promyelocytic leukemia, ATO increases cellular ROS levels and disrupts mitochondrial function, effectively inducing apoptosis in susceptible cancer cells [81] [101].
Targeting Master Regulatory Systems
- Inhibiting the Nrf2-Keap1 Axis: While Nrf2 is cytoprotective, its persistent activation in some cancers promotes growth and drug resistance. Inhibitors like Brusatol and ML385 block Nrf2 function, thereby disabling the transcriptional core of the antioxidant response and sensitizing tumors to therapy [81] [101].
- Disrupting the Glutathione System: Depleting GSH is a potent strategy. Compounds like sulfasalazine and erastin inhibit the cystine/glutamate antiporter system (xCT), blocking cysteine uptake—a critical precursor for GSH synthesis. This not only depletes GSH but also induces a unique, iron-dependent form of cell death called ferroptosis, characterized by overwhelming lipid peroxidation [81] [101].
- Targeting the Thioredoxin System: Auranofin, a repurposed anti-rheumatic drug, potently and irreversibly inhibits thioredoxin reductase (TrxR), crippling this key redox system and leading to oxidative stress-induced cell death [81] [101] [102].
Table 2: Redox-Directed Therapeutic Agents and Their Mechanisms
| Therapeutic Class | Example Agents | Molecular Target | Key Mechanistic Outcome |
|---|---|---|---|
| Pro-oxidant | High-Dose Vitamin C, Arsenic Trioxide (ATO) | Intracellular redox buffer | H₂O₂ generation, mitochondrial disruption [81] [101] |
| Nrf2 Inhibitor | Brusatol, ML385 | Nrf2 signaling pathway | Disables core antioxidant transcription program [81] [101] |
| GSH System Disruptor | Sulfasalazine, Erastin | Cystine/glutamate antiporter (xCT) | GSH depletion, induction of ferroptosis [81] [101] |
| Trx System Inhibitor | Auranofin | Thioredoxin Reductase (TrxR) | Irreversible inhibition of TrxR, oxidative stress [81] [101] |
| GST Inhibitor | Telcyta (Canfosfamide) | Glutathione S-Transferase P1-1 (GSTP1-1) | GST-activated prodrug releases cytotoxic alkylating agent [62] |
| Myelostimulant | Telintra (Ezatiostat) | Glutathione S-Transferase P1-1 (GSTP1-1) | Inhibits GSTP1-JNK interaction, stimulates hematopoiesis [62] |
Experimental Protocols for Validating Redox Therapies
In Vitro Assessment of Redox Status and Cell Viability
Objective: To evaluate the effect of a redox-directed compound (e.g., Erastin) on cellular ROS, glutathione levels, and viability in a cancer cell line.
Materials:
- Cell line of interest (e.g., HT-1080 fibrosarcoma for ferroptosis studies).
- Redox therapeutic agent (e.g., Erastin, Auranofin, dissolved in DMSO).
- Fluorescent probes: CellROX Deep Red Reagent (for general ROS), H2DCFDA (for H₂O₂), MitoSOX Red (for mitochondrial superoxide).
- GSH-Glo Glutathione Assay kit.
- Cell Titer-Glo Luminescent Cell Viability Assay.
Methodology:
- Cell Seeding and Treatment: Seed cells in 96-well plates at a density optimized for 24-48 hours growth. After adherence, treat with a concentration gradient of the redox therapeutic for 4-24 hours. Include vehicle (DMSO) and positive controls (e.g., Auranofin for ROS induction).
- ROS Measurement:
- After treatment, replace medium with fresh medium containing the appropriate fluorescent probe (e.g., 5 µM CellROX).
- Incubate for 30-60 minutes at 37°C protected from light.
- Wash cells with PBS and measure fluorescence using a plate reader (Ex/Em ~640/665 nm for CellROX). Normalize fluorescence to cell number or protein content.
- Glutathione Measurement:
- Use the GSH-Glo Assay per manufacturer's instructions.
- Briefly, lyse treated cells and incubate with the GSH-Glo Reagent. The generated luminescence is proportional to GSH concentration.
- Viability Assessment:
- Use the Cell Titer-Glo Assay to measure ATP levels as a surrogate for viability, following the kit protocol. Record luminescence.
Data Analysis: Plot dose-response curves for ROS, GSH, and viability. Calculate IC₅₀ values for viability and EC₅₀ for ROS induction/GSH depletion. A successful pro-ferroptotic agent like Erastin should show a dose-dependent decrease in GSH, a subsequent increase in ROS (specifically lipid ROS, measured with BODIPY 581/591 C11), and a corresponding decrease in viability.
In Vivo Efficacy Model for Redox Therapeutics
Objective: To determine the antitumor efficacy of a redox-targeting drug in a mouse xenograft model.
Materials:
- Immunocompromised mice (e.g., NOD/SCID or nude mice).
- Luciferase-tagged cancer cells.
- Redox therapeutic and vehicle for in vivo dosing.
- In vivo imaging system (IVIS) or calipers for tumor measurement.
Methodology:
- Tumor Implantation: Subcutaneously inject luciferase-expressing cancer cells into the flanks of mice. Allow tumors to establish to a palpable size (~50-100 mm³).
- Randomization and Dosing: Randomize mice into vehicle control and treatment groups (n=8-10). Administer the redox therapeutic (e.g., via intraperitoneal injection or oral gavage) at the maximum tolerated dose (MTD) determined in prior toxicity studies.
- Tumor Monitoring: Measure tumor volumes 2-3 times weekly using calipers (Volume = (length × width²)/2). Alternatively, perform bioluminescence imaging weekly after IP injection of D-luciferin to quantify tumor burden.
- Endpoint and Biomarker Analysis: At the study endpoint, euthanize mice and collect tumors. Snap-freeze a portion for biochemical analysis (e.g., immunoblotting for Nrf2, TrxR, or protein carbonyl content as a marker of oxidative damage) and preserve another portion in formalin for immunohistochemistry (IHC) analysis of biomarkers like 4-HNE (for lipid peroxidation) and Ki-67 (for proliferation).
Data Analysis: Plot tumor growth curves for each group and calculate the percent tumor growth inhibition (TGI%). Statistical significance is typically determined using a repeated-measures ANOVA. Survival analysis can be performed using Kaplan-Meier curves if the endpoint is survival.
Figure 2: Experimental Workflow for Redox Therapy Validation. The diagram outlines the key steps for in vitro characterization of redox and cytotoxic effects, and in vivo evaluation of antitumor efficacy and biomarker modulation [81] [98] [102].
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Redox Cancer Drug Discovery Research
| Reagent / Assay Name | Core Function | Application in Redox Research |
|---|---|---|
| CellROX Oxidative Stress Reagents | Fluorescent detection of general ROS | Quantifying overall cellular oxidative stress upon treatment [81] |
| MitoSOX Red Mitochondrial Superoxide Indicator | Selective detection of mitochondrial O₂•⁻ | Assessing mitochondrial-specific ROS generation [81] |
| GSH-Glo Glutathione Assay | Luminescent quantification of glutathione levels | Measuring GSH depletion (e.g., by erastin or sulfasalazine) [81] [62] |
| Liperfluo / BODIPY 581/591 C11 | Fluorescent detection of lipid peroxidation | Essential for confirming induction of ferroptosis [81] [101] |
| C11-BODIPY⁵⁸¹/⁵⁹¹ | Lipid peroxidation sensor | Ferroptosis validation; fluorescence shift upon oxidation [81] |
| Cell Titer-Glo Luminescent Cell Viability Assay | ATP quantification as viability proxy | Measuring cytotoxic outcomes of redox disruption [81] [102] |
| Erastin | xCT system inhibitor | Inducing ferroptosis by depleting cysteine/GSH [81] [101] |
| Auranofin | Thioredoxin Reductase (TrxR) inhibitor | Positive control for Trx system inhibition and ROS induction [81] [101] [102] |
Targeting the rewired redox homeodynamics of cancer cells offers a powerful and rational strategy for selective cancer therapy. The molecular understanding of how cancer cells balance pro-tumorigenic ROS signaling with adaptive antioxidant defenses has unveiled specific vulnerabilities, such as the Nrf2 axis, GSH, and Trx systems. Exploiting these vulnerabilities with agents like Nrf2 inhibitors, ferroptosis inducers, and TrxR inhibitors is showing significant promise in preclinical models and early clinical trials. Future success in this field will depend on the continued elucidation of redox signaling networks, the development of more specific redox modulators, and the application of predictive biomarkers for personalized patient stratification, ultimately translating the concept of redox homeodynamics into effective clinical outcomes [81] [103] [15].
This whitepaper provides a comparative analysis of the homeostasis and homeodynamics frameworks for interpreting clinical trial data within redox biology research. While homeostasis emphasizes stability through negative feedback systems, homeodynamics incorporates dynamic adaptation, nonlinear responses, and allostatic load as essential principles for understanding complex biological responses. Through examination of clinical evidence, experimental protocols, and conceptual models, we demonstrate how the homeodynamic perspective offers superior explanatory power for interpreting paradoxical clinical outcomes and advancing therapeutic development, particularly in conditions involving oxidative stress. The integration of homeodynamic principles promises to enhance the precision of clinical trial design and data interpretation in complex diseases.
The interpretation of clinical trial data requires robust theoretical frameworks to explain therapeutic outcomes and biological responses. Traditionally, homeostasis—defined as a self-regulating process by which biological systems maintain stability while adjusting to changing external conditions—has served as the central organizing principle of physiology [105]. This concept, refined by Walter Cannon from Claude Bernard's "milieu intérieur," envisions physiological systems operating through feedback mechanisms to maintain constancy [106] [1]. However, emerging evidence from complex biological systems, particularly in redox biology, reveals limitations in this equilibrium-centered model.
The homeodynamics framework addresses these limitations by incorporating dynamic adaptation, nonlinear responses, and hierarchical control as fundamental properties of living systems [105]. Where homeostasis seeks to reduce variability, homeodynamics embraces variability as essential for biological adaptation [1]. This distinction proves particularly relevant in interpreting clinical trials where therapeutic interventions targeting oxidative stress often produce paradoxical outcomes that challenge homeostatic expectations [66] [15].
This analysis examines how these competing frameworks influence the interpretation of clinical trial data, with specific emphasis on redox biology and therapeutic development. By comparing conceptual foundations, clinical evidence, and methodological approaches, we provide researchers with enhanced tools for designing trials and interpreting complex biological responses.
Conceptual Framework Comparison
Core Principles of Homeostasis
The homeostatic model centers on maintaining internal constancy through specific physiological mechanisms:
Feedback Control Systems: Homeostatic regulation employs sensors, setpoints, error detectors, controllers, and effectors in reflex loops that primarily operate through negative feedback to resist perturbation [1]. For example, chemosensors in carotid bodies measure arterial PCO₂ and PO₂, sending information to brainstem control centers that effect changes in breathing rate to maintain balance [1].
Setpoint Maintenance: The concept of a predetermined setpoint or desired physiological range is fundamental to homeostasis, with physiological responses aimed at returning systems to this predefined state following disturbance [1].
Stability as Goal: Homeostasis prioritizes stability, viewing deviation from setpoints as potentially pathological [105]. This perspective underlies traditional drug development approaches that often target single pathways to restore "normal" function.
Core Principles of Homeodynamics
Homeodynamics reconceptualizes physiological regulation through several key principles:
Dynamic Adaptation: Rather than maintaining fixed setpoints, homeodynamic systems exhibit adaptive setpoints that change based on environmental challenges and physiological history [1] [105]. This explains phenomena like fever and metabolic adaptation during fasting, where the "new normal" represents an adaptive response rather than dysfunction [1].
Allostatic Load: The cumulative burden of chronic adaptation to stressors represents allostatic load, which homeodynamics recognizes as a crucial factor in disease susceptibility and therapeutic response [1].
Hierarchical Control and Feedback Redundancy: Homeodynamic regulation involves multiple interacting feedback systems with hierarchical control, resulting in finer regulatory control and greater flexibility [105].
Nonlinear Responses: Homeodynamic systems frequently exhibit biphasic, threshold, and paradoxical responses that cannot be explained by simple linear models [64].
Table 1: Comparative Analysis of Conceptual Frameworks
| Feature | Homeostasis | Homeodynamics |
|---|---|---|
| Primary Focus | Stability, constancy, equilibrium | Adaptation, dynamic interaction, response capacity |
| Setpoint Concept | Fixed, predetermined | Adaptive, context-dependent |
| Response to Perturbation | Resistance through negative feedback | Adaptive response through integrated networks |
| View of Variability | Noise to be minimized | Functional capacity and flexibility |
| Temporal Perspective | Immediate maintenance of constancy | Cumulative adaptation history (allostatic load) |
| Therapeutic Implication | Restore "normal" function | Enhance adaptive capacity |
Clinical Trial Interpretation Through Competing Frameworks
The Case of Antioxidant Trials
The interpretation of antioxidant clinical trials provides a compelling case for the homeodynamic perspective. The homeostatic framework would predict that increasing antioxidant capacity should linearly reduce oxidative damage and improve outcomes. However, multiple large-scale clinical trials have demonstrated limited efficacy or even harm with broad-spectrum antioxidant supplementation [66] [15] [64].
Through a homeodynamic lens, reactive oxygen species (ROS) function as crucial signaling molecules at physiological concentrations, participating in synaptic plasticity, neuronal differentiation, immune function, and adaptation to neuronal activity [66]. The biphasic nature of ROS signaling—where low levels mediate physiological signaling (eustress) while high levels cause damage (distress)—explains why non-targeted antioxidant interventions disrupt redox signaling rather than restoring optimal function [64].
Heart Failure Hemodynamics Trial
Analysis of the Flolan International Randomized Survival Trial (FIRST) demonstrates how homeodynamic interpretation provides superior explanatory power for clinical outcomes [107]. This trial enrolled 471 patients with class IIIb/IV heart failure and ejection fraction ≤25%, all undergoing pulmonary artery catheterization. Patients received either epoprostenol or placebo, with epoprostenol therapy guided by pulmonary artery catheter measures.
Multivariable modeling revealed that decreased pulmonary capillary wedge pressure (PCWP) significantly predicted 1-year survival (hazard ratio, 0.96 for every 1-mm Hg decrease). However, contrary to homeostatic expectations, patients with ≥9 mm Hg decrease in PCWP showed no better survival than control patients with limited hemodynamic changes [107].
A homeodynamic interpretation recognizes that the achieved hemodynamic "improvement" represented excessive perturbation of an adapted state rather than meaningful functional enhancement. The complex, integrated nature of advanced heart failure requires consideration of allostatic load and adaptive capacity beyond simple hemodynamic parameters.
Table 2: Clinical Trial Examples and Framework Interpretation
| Trial/Intervention | Homeostatic Interpretation | Homeodynamic Interpretation |
|---|---|---|
| Broad-Spectrum Antioxidants | Failed to adequately reduce oxidative stress | Disrupted physiological redox signaling networks |
| FIRST Trial (Epoprostenol) | Hemodynamic improvement should predict survival | Excessive perturbation of adapted state ignores allostatic load |
| Statins (Beyond Lipid Lowering) | Primary mechanism: cholesterol reduction | Recognizes pleiotropic effects on Nrf2/HO-1 signaling and redox modulation [66] |
| Resveratrol Supplementation | Direct antioxidant activity | Modulation of redox-sensitive signaling pathways and adaptive responses [66] |
Experimental Methodologies for Redox Assessment
Comprehensive Redox Biomarker Profiling
Precision medicine approaches to redox assessment require multidimensional biomarker analysis that reflects the complexity of redox regulation:
ROS Generation Assessment: Measure ROS from specific sources including mitochondrial electron transport chain (using MitoSOX Red), endoplasmic reticulum (using ER-Tracker Red), and NADPH oxidases (using DPI inhibition) [66] [15].
Antioxidant Capacity Quantification: Evaluate NRF2-mediated antioxidant responses by measuring superoxide dismutase (SOD), catalase, glutathione peroxidase (GPx) activities, and key molecules including nicotinamide adenine dinucleotide phosphate (NADPH) and glutathione (GSH) [15].
Oxidative Damage Markers: Assess lipid peroxidation (malondialdehyde, 4-hydroxynonenal), protein carbonylation, and DNA oxidation (8-hydroxy-2'-deoxyguanosine) [64].
Redox-Sensitive Protein Modifications: Detect reversible oxidative modifications including disulfide bonds (S-S), S-glutathionylation (SSG), S-nitrosylation (SNO), and S-sulfenylation (SOH) using modified biotin switch assays and mass spectrometry [15].
Integration with Omics Technologies
Advanced redox assessment integrates multi-omics approaches to capture system-wide dynamics:
Redox Proteomics: Identify and quantify redox-sensitive cysteine modifications using ICAT (isotope-coded affinity tags) and OxICAT methods [66].
Metabolomic Profiling: Characterize redox metabolites including NAD⁺/NADH, NADP⁺/NADPH, GSH/GSSG, and Trx/TrxSS ratios using LC-MS/MS [66].
Transcriptomic Analysis: Evaluate NRF2-dependent gene expression networks and redox-sensitive transcription factors using RNA sequencing [15].
Signaling Pathway Visualization
Redox Homeostasis Regulation Pathway
This diagram illustrates the integrated network of reactive oxygen species (ROS) generation, antioxidant defense mechanisms, and redox signaling that maintains redox homeostasis. The system demonstrates key homeodynamic properties through adaptive NRF2-mediated responses to oxidative challenges and bidirectional signaling between redox modifications and cellular responses [15] [64].
Precision Redox Medicine Trial Design
This workflow outlines a homeodynamics-informed clinical trial design incorporating comprehensive patient stratification, targeted interventions based on redox phenotypes, and multidimensional response monitoring that assesses both molecular and functional adaptation.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Redox Homeodynamics Research
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| ROS Detection Probes | MitoSOX Red (mitochondrial O₂•⁻), DCFH-DA (general ROS), Amplex Red (H₂O₂) | Specific detection of ROS from different cellular sources and compartments |
| Antioxidant Activity Assays | SOD Activity Assays, Catalase Activity Kits, GPx Activity Measurement | Quantification of specific antioxidant enzyme activities in tissues and cells |
| Thiol Redox Status Probes | Monobromobimane (GSH), Rox-Far Red (mitochondrial GSH), Redox-Sensitive GFPs | Measurement of glutathione redox potential and compartment-specific redox status |
| NRF2 Pathway Modulators | Sulforaphane (activator), ML385 (inhibitor), NRF2 siRNA | Investigation of NRF2-mediated antioxidant response element signaling |
| Protein Oxidation Detection | Biotin Switch Assay kits, OxyBlot kits, Anti-nitrotyrosine antibodies | Detection and quantification of specific protein oxidative modifications |
| Lipid Peroxidation Assays | MDA/TBARS Assays, Lipid Hydroperoxide Assay, BODIPY-C11 probe | Measurement of lipid peroxidation products and membrane oxidative damage |
| Redox Metabolomics | NAD⁺/NADH, NADP⁺/NADPH, GSH/GSSG Assay Kits | Quantitative analysis of central redox metabolites and their ratios |
Discussion and Future Directions
The integration of homeodynamic principles into clinical trial design and interpretation represents a paradigm shift with profound implications for therapeutic development. This approach moves beyond simplistic "rebalance" models to embrace the complexity, adaptability, and historical context of physiological systems.
Implications for Trial Design
Future clinical trials informed by homeodynamics should incorporate several key design elements:
Stratification by Redox Phenotype: Patient selection should include comprehensive redox biomarker profiling to identify specific dysregulation patterns (e.g., impaired antioxidant defense vs. excessive ROS production) rather than grouping all "oxidative stress" conditions together [66] [64].
Adaptive Intervention Strategies: Trial designs should allow for protocol adaptation based on individual dynamic responses, potentially using biomarker trends rather than fixed doses to guide therapy [15].
Multidimensional Endpoints: Beyond traditional clinical endpoints, trials should assess adaptive capacity, allostatic load, and system resilience using integrated biomarker networks [105].
Therapeutic Development Opportunities
The homeodynamics framework reveals several promising therapeutic approaches:
Targeted Redox Modulators: Small molecule inhibitors targeting specific cysteine residues in redox-sensitive proteins have demonstrated promising preclinical outcomes, setting the stage for clinical trials [15].
NRF2 Pathway Therapeutics: Context-specific NRF2 activators that enhance antioxidant capacity without disrupting redox signaling networks offer potential for conditions with impaired antioxidant defense [15].
Combination Therapies: Strategic combinations that simultaneously address multiple nodes in redox regulatory networks may produce synergistic benefits unattainable with single-target approaches [66].
The comparative analysis of homeostasis versus homeodynamics frameworks demonstrates the superior explanatory power of homeodynamics for interpreting complex clinical trial data, particularly in redox biology. The recognition of dynamic adaptation, nonlinear responses, and allostatic load provides more accurate models of physiological behavior and therapeutic response. As precision medicine advances, embracing homeodynamic principles will be essential for developing effective therapies that work with rather than against the inherent adaptive capacity of biological systems. Researchers and drug development professionals should incorporate these concepts into trial design, endpoint selection, and data interpretation to advance therapeutic innovation for complex diseases.
The compelling narrative that oxidative stress contributes to chronic diseases logically positioned antioxidant supplementation as a promising therapeutic strategy. Yet, despite pathophysiological, epidemiological, and mechanistic data suggesting efficacy, large-scale clinical trials with broad-spectrum antioxidants have largely yielded disappointing results [108] [109]. This contradiction represents a critical paradox in modern therapeutics that challenges fundamental assumptions about redox biology. The repeated failure of these trials, involving tens of thousands of patients, cannot be dismissed merely as methodological flaws but rather signals a essential deficiency in our conceptual understanding of redox regulation [109] [15].
This review posits that the failure of broad-spectrum antioxidant therapies stems primarily from an outdated homeostatic model of redox regulation—one that views oxidants simplistically as toxic byproducts to be eliminated. We argue for a paradigm shift toward a homeodynamic framework, wherein reactive oxygen species (ROS) function as crucial signaling molecules within complex, spatially organized networks that dynamically maintain system integrity [45] [110]. Within this homeodynamic perspective, oxidative stress represents not merely an imbalance between oxidants and antioxidants, but a disruption in the spatiotemporal organization of redox signaling networks that maintain physiological function [15].
Redox Homeodynamics: From Static Balance to Dynamic Regulation
Fundamental Principles of the Redox Code
The conceptual foundation for understanding redox homeodynamics is encapsulated in the "Redox Code"—a set of organizational principles governing biological redox reactions [45] [15]. This framework comprises four core principles:
- First Principle: Bioenergetics, catabolism, and anabolism are organized through high-flux NADH and NADPH systems operating near equilibrium with central metabolic fuels. These systems create the fundamental reducing environment that powers cellular metabolism while simultaneously generating controlled oxidant production [45].
- Second Principle: Macromolecular structure and activities are linked to NADH and NADPH systems through kinetically controlled sulfur switches in the redox proteome. These switches, primarily on cysteine residues, allow reversible oxidation-reduction modifications that regulate protein function and signaling pathways [15].
- Third Principle: Activation and deactivation cycles of H₂O₂ production linked to NADH and NADPH systems support redox signaling and spatiotemporal sequential responses for differentiation and multicellular development. This principle establishes ROS as deliberate signaling molecules rather than accidental byproducts [45].
- Fourth Principle: Redox networks, from microcompartments to subcellular and cellular organization, form an adaptive system to respond to the environment. These networks enable compartmentalized redox regulation that defies simplistic systemic antioxidant approaches [15].
The Physiological Goldilocks Zone: Eustress Versus Distress
A cornerstone of the homeodynamic model is the recognition that ROS operate within a physiological range dubbed the "Goldilocks Zone," "Homeodynamic Space," or "Golden Mean" [110]. Within this zone, ROS function as essential signaling molecules in processes termed oxidative eustress (beneficial stress), including:
- Embryonal development and tissue differentiation
- Cellular growth and proliferation pathways
- Neural activity and synaptic plasticity
- Skeletal muscle adaptation to exercise
- Circadian rhythm regulation
- Immune function and host defense
Beyond this zone, whether through deficiency or excess, lies oxidative distress—the pathological state associated with molecular damage and disease pathogenesis [45] [15]. This dual nature of redox signaling explains why non-discriminant antioxidant supplementation often disrupts essential physiological processes while attempting to mitigate pathological ones.
Table 1: Distinctive Features of Redox Homeostasis versus Redox Homeodynamics
| Feature | Redox Homeostasis | Redox Homeodynamics |
|---|---|---|
| Conceptual Model | Static balance | Dynamic, adaptive regulation |
| ROS Perspective | Toxic byproducts | Essential signaling molecules |
| Spatial Organization | Uniform distribution | Compartmentalized gradients |
| Temporal Dimension | Steady-state maintenance | Rhythmic, pulsatile fluctuations |
| Therapeutic Goal | Global oxidant reduction | Targeted pathway modulation |
| Adaptive Capacity | Limited | High, with hormetic responses |
Analysis of Failed Antioxidant Trials: Beyond Mere Scavenging
Clinical Evidence of Limited Efficacy
The empirical case against broad-spectrum antioxidants is substantial. Major clinical trials investigating antioxidants such as vitamin E, vitamin C, and β-carotene for chronic diseases have consistently failed to demonstrate significant benefits, despite strong epidemiological correlations [109]. These negative outcomes span diverse conditions including cardiovascular diseases, neurodegenerative disorders, and diabetes complications. Even in ophthalmology, where oxidative stress is unequivocally implicated in cataract pathogenesis, the Age-Related Eye Disease Study 2 (AREDS2) found that supplementation with endogenous antioxidants like lutein/zeaxanthin, ascorbic acid, and vitamin E had no overall effect on the need for cataract surgery [111].
Mechanistic Limitations of Broad-Spectrum Approaches
The failure of these trials exposes critical limitations in the broad-spectrum antioxidant approach:
- Disruption of Physiological Signaling: Non-specific antioxidant scavenging inadvertently quenches ROS-mediated signaling cascades essential for normal cellular function. For instance, low levels of ROS have been shown to initiate redox signaling and cell proliferation in human lens epithelial cells, demonstrating a physiological role for ROS in growth and development unrelated to pathology [111].
- Pro-oxidant Conversion: Some antioxidants, including vitamin E and vitamin C, can exhibit pro-oxidant activity under certain conditions, particularly at higher concentrations [109] [112]. For example, high concentrations of vitamin C can promote the Fenton reaction, generating hydroxyl radicals and toxic degradation products like dehydroascorbic acid that may accelerate cataract formation [112].
- Insufficient Target Engagement: Many antioxidants have limited bioavailability or fail to reach the specific subcellular compartments where pathological oxidative damage occurs. The lens presents a particular challenge, with anatomical and intracellular barriers that limit delivery of glutathione (GSH) and other antioxidants to different lens regions [111].
- Inadequate Trial Duration: The chronic, progressive nature of oxidative stress-related diseases suggests that antioxidant interventions may need to be administered for decades to show effect, whereas most clinical trials typically last only several years [109].
Diagram 1: Contrasting interventional approaches to redox modulation. The broad-spectrum antioxidant approach (red pathway) typically fails due to non-specific action and disruption of physiological signaling, while targeted approaches (green pathway) aim to restore redox homeodynamics through precise mechanistic interventions.
Emerging Alternatives: Strategic Approaches to Redox Modulation
NRF2 Pathway Activation
Rather than direct oxidant scavenging, activation of the transcription factor NRF2 (nuclear factor erythroid 2-related factor 2) represents a sophisticated approach to enhancing endogenous antioxidant capacity. NRF2 serves as a master regulator of the antioxidant response, controlling the expression of hundreds of genes involved in glutathione homeostasis, NADPH regeneration, and detoxification pathways [113] [15]. Under physiological conditions, NRF2 is sequestered in the cytoplasm by its inhibitor KEAP1 (Kelch-like ECH-associated protein 1) and targeted for degradation. Oxidative stress triggers conformational changes in KEAP1, releasing NRF2 to translocate to the nucleus and activate antioxidant response element (ARE)-mediated gene expression [113].
This endogenous system offers several advantages over direct antioxidant supplementation:
- Amplification: A single transcriptional activator can upregulate multiple protective enzymes
- Compartmentalization: The induced enzymes are naturally targeted to appropriate cellular locations
- Feedback regulation: The system is subject to natural feedback control, reducing risk of reductive stress
- Durability: Induced enzymes provide sustained protection rather than transient scavenging
Experimental evidence supports NRF2 activation as a promising strategy for ocular diseases. In lens epithelial cells, NRF2 activation enhances expression of glutathione, superoxide dismutase, catalase, and molecular chaperones that collectively protect against cataract formation [113]. Similar protective effects have been demonstrated in retinal models, suggesting broad applicability for ophthalmological conditions [15].
Glutathione System Enhancement
Given glutathione's pivotal role as the principal lenticular antioxidant, strategies to enhance its bioavailability represent another targeted approach. However, direct glutathione supplementation is fraught with challenges including rapid degradation, poor cellular uptake, and anatomical barriers in the eye [111]. Alternative strategies include:
- Cysteine Prodrugs: Lipid-permeable cysteine analogues like N-acetylcysteine (NAC) increase intracellular cysteine availability, bypassing the rate-limiting step in glutathione synthesis. NAC has shown promise in experimental models by decreasing ROS expression and reducing UVB-induced apoptosis in lens cells [113].
- Precursor Supplementation: Providing precursors such as glycine and glutamate can enhance glutathione synthesis under conditions of substrate limitation.
- Enzymatic Cofactor Support: Ensuring adequate supplies of NADPH, the essential cofactor for glutathione reductase, supports glutathione regeneration from its oxidized form.
Table 2: Experimental Strategies for Glutathione Enhancement in Redox-Related Diseases
| Strategy | Mechanism | Example Compounds | Experimental Evidence |
|---|---|---|---|
| NRF2 Activation | Transcriptional upregulation of synthesis enzymes | Sulforaphane, Bardoxolone methyl | Increased GSH levels and protection against oxidative stress in lens epithelial cells [113] |
| Cysteine Prodrugs | Increased substrate availability for synthesis | N-acetylcysteine (NAC) | Decreased ROS and reduced UVB-induced apoptosis in lens cells [113] |
| GSH Regeneration | Enhanced reduction of GSSG to GSH | NADPH precursors | Maintained GSH/GSSG ratio under oxidative challenge [114] |
| Transport Enhancement | Improved cellular uptake | Liposomal GSH, GSH esters | Increased intracellular GSH in various cell types [111] |
Redox-Sensitive Protein Targeting
Emerging approaches focus on specific redox-sensitive proteins whose functions are altered in disease states. These targets include:
- Protein Disulfide Isomerases: Enzymes that catalyze disulfide bond formation and isomerization in the endoplasmic reticulum
- Thioredoxin System Components: Including thioredoxin, thioredoxin reductase, and peroxiredoxins that regulate redox-dependent signaling
- Glutaredoxins: Thiol-disulfide oxidoreductases that catalyze reversible glutathionylation reactions
- Sulfhydryl Oxidases: Enzymes that generate disulfide bonds while reducing oxygen to hydrogen peroxide
Small molecule inhibitors that target specific cysteine residues in these redox-sensitive proteins have demonstrated promising preclinical outcomes, setting the stage for forthcoming clinical trials [15]. For instance, glutaredoxin deficiency has been associated with increased susceptibility to oxidative stress in the lens, and its restoration represents a potential therapeutic strategy [114].
Experimental Approaches and Methodologies
Assessing Redox Homeodynamics: Technical Considerations
Evaluating the efficacy of redox-targeted therapies requires moving beyond static measurements of oxidative damage to dynamic assessments of redox regulation. Key methodological approaches include:
- Redox Proteomics: Comprehensive analysis of reversible oxidative protein modifications, particularly cysteine oxidations, provides insights into functional changes in signaling pathways [15].
- Compartment-Specific ROS Sensors: Genetically encoded fluorescent probes targeted to specific subcellular locations (mitochondria, endoplasmic reticulum, nucleus) enable spatiotemporal resolution of ROS fluctuations [45].
- Thiol Redox Status Assessment: Measurement of glutathione/glutathione disulfide (GSH/GSSG) ratios, glutaredoxin activity, and thioredoxin reduction potential offers functional readouts of redox buffering capacity [114].
- Oxidant Production Mapping: Detection of specific ROS sources (NOX enzymes, mitochondrial complexes, endoplasmic reticulum) helps identify pathological versus physiological ROS generation [15].
In Vitro Models for Cataract Research
Lens epithelial cell cultures subjected to oxidative stressors (H₂O₂, UV radiation, hyperglycemic conditions) provide valuable screening platforms for potential therapeutics [113] [114]. Key methodological considerations include:
- Stressors: Physiological versus pathological ROS generation (e.g., low-dose H₂O₂ for signaling studies versus high-dose for toxicity)
- Endpoint Assessments: Cell viability, protein aggregation, antioxidant enzyme activities, and marker expression (NRF2 translocation, KEAP1 modification)
- Temporality: Acute versus chronic exposure paradigms to distinguish compensatory adaptations from therapeutic effects
Diagram 2: Comprehensive assessment of redox homeodynamics in experimental models. A multi-assay approach across different biological complexity levels provides complementary insights into redox regulation.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Redox Homeodynamics Research
| Reagent Category | Specific Examples | Research Applications | Technical Considerations |
|---|---|---|---|
| NRF2 Activators | Sulforaphane, CDDO-methyl ester, Dimethyl fumarate | Induction of endogenous antioxidant systems | Dose-response critical; high concentrations may cause reductive stress |
| KEAP1-NRF2 Interaction Inhibitors | ML385, NRF2-activating peptides | Disruption of NRF2 degradation complex | Specificity validation required against other protein-protein interactions |
| Cysteine Prodrugs | N-acetylcysteine (NAC), N-acetylcysteine amide | Enhanced glutathione synthesis | Monitor both reduced and oxidized forms; consider cellular uptake efficiency |
| GSH System Modulators | Buthionine sulfoximine (BSO), GSH monoethyl ester | GSH depletion or enhancement | BSO is irreversible inhibitor; compensation mechanisms may develop |
| Redox-Sensitive Fluorophores | H2DCFDA, MitoSOX, roGFP | ROS detection in specific compartments | Validation with specific inhibitors required; consider photobleaching and auto-oxidation |
| Thiol Status Probes | Monobromobimane, DTNB | Quantification of reduced thiol pools | Sample processing must prevent artificial oxidation; rapid measurement needed |
| Oxidant-Generating Enzymes Inhibitors | Apocynin, VAS2870, MitoTEMPO | Specific inhibition of ROS sources | Specificity varies; confirm target engagement with functional assays |
The repeated failures of broad-spectrum antioxidant trials have paradoxically advanced our understanding of redox biology by exposing the limitations of a simplistic homeostatic model. The emerging paradigm of redox homeodynamics recognizes that oxidative signaling is not a pathological aberration but an essential feature of biological regulation. This perspective fundamentally reshapes therapeutic strategy—from global oxidant suppression to targeted modulation of specific redox nodes and pathways.
Future progress in redox medicine will depend on developing therapies that respect the spatial, temporal, and functional complexity of redox networks. Promising directions include NRF2 pathway modulation, glutathione system enhancement, and targeted manipulation of specific redox-sensitive proteins. As we deepen our understanding of the "Redox Code" that governs these networks, we move closer to therapies that can dynamically maintain the "Goldilocks Zone" of redox signaling—the precise balance required for optimal health and function.
The lens of homeodynamics thus provides not just a theoretical framework but a practical roadmap for developing effective redox-based therapies. By learning from past failures and embracing biological complexity, we can transform the antioxidant paradox into a new therapeutic paradigm.
The conceptual framework for understanding biological redox regulation has evolved significantly, shifting from the static notion of homeostasis to the dynamic, adaptive concept of homeodynamics. Redox homeostasis traditionally described the maintenance of a stable internal environment through balanced oxidant and antioxidant systems [14]. In contrast, redox homeodynamics recognizes that living systems undergo continuous and dynamic interactions to maintain functional stability, where redox reactions act as crucial regulators of adaptation, stress responses, and signaling pathways [14]. This paradigm shift provides the foundational context for evaluating precision redox interventions, which strategically target specific nodes within these dynamic networks rather than applying broad antioxidant approaches. This article examines two successful exemplars of this precision approach: Telintra (Ezatiostat) as a specific glutathione S-transferase P (GSTP) inhibitor, and NRF2 activators that precisely modulate the KEAP1-NRF2-ARE pathway.
Telintra (Ezatiostat): A Precision GSTP Inhibitor
Mechanism of Action: Targeting GSTP in Signaling Networks
Telintra (TLK199, Ezatiostat) is a nanomolar inhibitor of glutathione S-transferase P (GSTP) that exemplifies precision redox intervention through its specific targeting of a key regulatory protein in redox-sensitive signaling pathways [115]. Unlike earlier approaches that sought to broadly modulate glutathione pathways, Telintra specifically disrupts the protein-protein interactions between GSTP and stress kinases, particularly c-Jun N-terminal kinase (JNK) [115] [62].
Graphical Abstract: Telintra Mechanism of Action
GSTP functions as an endogenous negative regulatory switch for JNK, sequestering it in an inactive complex under basal conditions [115]. Telintra administration causes dissociation of this complex, leading to GSTP oligomerization and subsequent JNK activation, which drives downstream transcriptional programs affecting proliferation, differentiation, and apoptosis [115]. This mechanism is particularly relevant in myelodysplastic syndrome (MDS), where Telintra promotes hematopoiesis through precise modulation of this redox-sensitive pathway rather than through general antioxidant effects.
Experimental Evidence and Clinical Translation
Preclinical studies demonstrated that Telintra treatment of primary human bone marrow stromal cells resulted in production of G-CSF, GM-CSF, and interleukin-6 at levels 200% to 400% greater than control [116]. In models of chemotherapy-induced neutropenia, a single oral or injected dose of Telintra produced up to a 500% increase in serum G-CSF levels, accelerating neutrophil recovery in a therapeutically meaningful timeframe [116].
Table 1: Quantitative Effects of Telintra in Preclinical Studies
| Experimental Model | Treatment Protocol | Key Outcomes | Magnitude of Effect |
|---|---|---|---|
| Primary human bone marrow stromal cells | In vitro treatment with Telintra | Increased cytokine production | 200-400% increase in G-CSF, GM-CSF, IL-6 |
| Chemotherapy-induced neutropenia model | Single oral or injected dose | Increased serum G-CSF levels | Up to 500% increase |
| Chemotherapy-induced neutropenia model | Standard dosing protocol | Accelerated neutrophil recovery | Statistically significant earlier recovery |
Clinical trials have validated this precision approach, with Telintra demonstrating improvements in all three major blood cell lineages (white blood cells, red blood cells, and platelets) in MDS patients, including those in intermediate and high-risk groups [115] [62]. The successful progression of Telintra through Phase I/II clinical trials underscores the therapeutic potential of precisely-targeted redox interventions.
NRF2 Activators: Precision Modulation of the Antioxidant Response
KEAP1-NRF2-ARE Pathway Mechanics
The KEAP1-NRF2-ARE pathway represents a master regulatory system for cellular redox homeostasis, serving as a prime target for precision redox interventions [117]. Under basal conditions, NRF2 is continuously ubiquitinated by the KEAP1-CUL3-RBX1 E3 ligase complex and degraded by the proteasome, maintaining low basal expression of antioxidant genes [117]. Cellular stress, particularly electrophilic stress or oxidative challenge, modifies specific cysteine residues in KEAP1 (notably Cys-151, Cys-273, and Cys-288), disrupting this complex and allowing NRF2 accumulation and translocation to the nucleus [117].
Graphical Abstract: NRF2 Activation Mechanisms
In the nucleus, NRF2 forms heterodimers with small MAF proteins and binds to Antioxidant Response Elements (AREs), driving expression of a battery of cytoprotective genes including those involved in glutathione synthesis (GCLC, GCLM), antioxidant protection (HMOX1, NQO1), and detoxification (GSTs) [117] [118]. This coordinated transcriptional program enables adaptive responses to oxidative and electrophilic stress.
Precision Approaches to NRF2 Activation
Contemporary NRF2-targeted therapies demonstrate increasing molecular precision through distinct mechanisms:
Electrophilic Activators
Compounds like bardoxolone methyl (CDDO-Me) and omaveloxolone (RTA-408) covalently modify specific cysteine residues in KEAP1 (primarily Cys-151), preventing NRF2 ubiquitination and degradation [117]. These agents have shown clinical efficacy in multiple conditions, including chronic kidney disease, Friedreich's ataxia, and multiple sclerosis [117].
Non-Electrophilic Activators
Recent advances include non-covalent KEAP1-NRF2 protein-protein interaction inhibitors such as PRL-295 and ADJ-310, which directly block the KEAP1-NRF2 interaction without covalent modification [118]. These compounds demonstrate improved target specificity with reduced off-target effects compared to electrophilic activators [118].
Table 2: Clinically Advanced NRF2 Activators and Their Applications
| Compound | Mechanism Class | Molecular Target | Clinical Status | Primary Disease Targets |
|---|---|---|---|---|
| Bardoxolone-methyl (CDDO-Me) | Electrophilic | KEAP1-Cys-151 | Phase III | Diabetic nephropathy, CKD, Alport syndrome |
| Omaveloxolone (RTA-408) | Electrophilic | KEAP1-Cys-151 | FDA Approved (2023) | Friedreich's ataxia |
| Dimethyl fumarate | Electrophilic | KEAP1-Cys-151 | FDA Approved | Multiple sclerosis, psoriasis |
| PRL-295 | Non-electrophilic | KEAP1-NRF2 PPI | Preclinical | Diabetic wound healing |
| ADJ-310 | Non-electrophilic | KEAP1-NRF2 PPI | Preclinical | Diabetic wound healing |
Experimental Validation of Non-Electrophilic NRF2 Activators
Recent investigations demonstrate the therapeutic potential of precision non-electrophilic NRF2 activators. In diabetic wound healing models, both ADJ-310 and PRL-295 maintained human keratinocyte (HaCaT) viability at 98-99% even at 10 µM concentrations, while significantly enhancing cell proliferation and migration in scratch assays [118]. RNA-sequencing analysis revealed that PRL-295 activated NRF2 with a narrower transcriptomic profile than the electrophilic activator CDDO-Me, demonstrating enhanced precision with fewer off-target effects [118].
In vivo studies in Leprdb/db diabetic mice demonstrated that both ADJ-310 and PRL-295 significantly improved wound healing outcomes and upregulated known NRF2 target genes in treated tissue [118]. These findings highlight the potential of precision NRF2 activators for therapeutic applications where reduced off-target effects are clinically advantageous.
Experimental Methodologies for Precision Redox Research
Core Assessment Techniques
Research into precision redox interventions employs specialized methodologies to evaluate compound effects on specific molecular targets and downstream physiological responses:
In Vitro Target Engagement Assays:
- Isothermal titration calorimetry to measure binding affinity between KEAP1 and NRF2 [117]
- Fluorescence polarization assays for protein-protein interaction disruption [118]
- Ubiquitination assays to quantify NRF2 stabilization [117]
Cellular Functional Assays:
- Scratch/wound closure assays with human keratinocytes (HaCaT cells) to assess migration [118]
- Quantitative PCR and RNA-sequencing to evaluate NRF2 target gene expression [118]
- Cytokine production measurements in bone marrow stromal cells [116]
In Vivo Validation Models:
- Chemotherapy-induced neutropenia models for hematopoiesis assessment [116]
- Diabetic wound healing models (Leprdb/db mice) for tissue repair evaluation [118]
- Myelodysplastic syndrome models for hematologic improvement [115]
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Precision Redox Investigations
| Reagent/Cell Line | Application | Key Function in Research |
|---|---|---|
| HaCaT keratinocytes | In vitro wound healing models | Representative epithelial cells for migration and proliferation assays |
| Primary human bone marrow stromal cells | Hematopoiesis studies | Assessment of cytokine production and hematopoietic support |
| Leprdb/db diabetic mice | In vivo wound healing studies | Diabetic wound model for therapeutic efficacy evaluation |
| Recombinant KEAP1 Kelch domain | Binding assays | Target protein for measuring compound affinity and mechanism |
| NRF2 knockout cells/mice | Specificity validation | Control systems to confirm NRF2-dependent effects |
| ARE-luciferase reporter cells | Pathway activation screening | Rapid assessment of NRF2 transcriptional activity |
The success stories of Telintra and NRF2 activators demonstrate the transformative potential of precision redox interventions that target specific nodes within dynamic redox regulatory networks. Unlike broad-spectrum antioxidant approaches, these targeted strategies modulate specific redox-sensitive signaling pathways with greater therapeutic precision and reduced off-target effects. The transition from electrophilic to non-electrophilic NRF2 activators represents a further refinement in precision, enabling more specific therapeutic effects while minimizing non-specific reactivity [118].
Future developments in precision redox medicine will require continued advancement in several key areas: development of more precise assessment methods for redox homeodynamics, rational selection of oxidative modulators based on specific disease characteristics, optimization of delivery systems for targeted tissue distribution, and creation of precise interventions that consider individual genetic and environmental factors to achieve optimal therapeutic outcomes across diverse diseases [14]. As these technologies mature, precision redox interventions are poised to deliver increasingly sophisticated therapeutic options for conditions ranging from hematologic disorders to diabetic complications and beyond.
Conclusion
The shift from redox homeostasis to homeodynamics represents a fundamental advancement in our understanding of cellular physiology and pathology. This dynamic framework more accurately reflects the continuous, adaptive nature of redox regulation and provides a superior model for explaining the complex, context-dependent roles of oxidants and antioxidants. The key takeaway is that future therapeutic success hinges on moving beyond non-specific antioxidant supplementation towards precise modulation of specific redox-sensitive pathways and nodes. This requires a deep understanding of the individual's redox landscape, the development of reliable quantitative biomarkers, and the design of targeted interventions that can restore a healthy redox dynamic without disrupting essential signaling. Embracing the homeodynamics paradigm will be crucial for unlocking the next generation of precision medicines for a wide spectrum of chronic diseases.
References
- 1. Physiology, Homeostasis - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK559138/]
- 2. Adaptive Homeostasis - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC4868097/]
- 3. Redox homeostasis: The Golden Mean of healthy living [https://www.sciencedirect.com/science/article/pii/S2213231716300106]
- 4. Redox Homeostasis and Natural Dietary Compounds [https://pmc.ncbi.nlm.nih.gov/articles/PMC6265930/]
- 5. Cellular Redox Homeostasis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8469889/]
- 6. Editorial: The pharmacological effects and mechanisms of ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1665486/full]
- 7. The Role of Redox Homeostasis in Tumor Progression [https://pubmed.ncbi.nlm.nih.gov/40759207/]
- 8. Redox signaling at the crossroads of human health and disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC8971743/]
- 9. Unravelling the Biological Roles of Reactive Oxygen Species [https://pmc.ncbi.nlm.nih.gov/articles/PMC4445605/]
- 10. Redox Signalling - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/redox-signalling]
- 11. Glutathione in Cellular Redox Homeostasis - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC6272787/]
- 12. Redox Regulation of Cell Survival by the Thioredoxin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2821134/]
- 13. The Role of NADPH Oxidases and Oxidative Stress in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6321244/]
- 14. Redox signaling and homeostasis [https://www.sciopen.com/article/10.26599/OSHM.2025.9610003]
- 15. Redox regulation: mechanisms, biology and therapeutic ... [https://www.nature.com/articles/s41392-024-02095-6]
- 16. Oxidative Cysteine Post Translational Modifications Drive ... [https://www.mdpi.com/2076-3921/13/8/883]
- 17. Cysteines as Redox Molecular Switches and Targets of ... [https://www.frontiersin.org/journals/molecular-neuroscience/articles/10.3389/fnmol.2017.00167/full]
- 18. REDOX-BASED REGULATION OF SIGNAL TRANSDUCTION [https://pmc.ncbi.nlm.nih.gov/articles/PMC2453533/]
- 19. The role of cysteine residues as redox-sensitive regulatory ... [https://www.sciencedirect.com/science/article/abs/pii/S0959440X04001769]
- 20. Redox Signaling from Mitochondria - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC7023504/]
- 21. Redox signalling regulates breast cancer metastasis via ... [https://www.nature.com/articles/s41416-023-02522-5]
- 22. Redox signaling and homeostasis in the control of metabolism ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11650601/]
- 23. Antioxidant and Adaptative Response Mediated by Nrf2 ... [https://www.mdpi.com/2076-3921/8/6/196]
- 24. Redox Homeostasis and Nrf2-Regulated Mechanisms Are ... [https://www.mdpi.com/2076-3921/13/2/193]
- 25. P692: THE KEAP1-NRF2 REDOX PATHWAY IS OF CENTRAL ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10429369/]
- 26. PGC-1α Is a Master Regulator of Mitochondrial Lifecycle ... [https://www.mdpi.com/2076-3921/12/5/1075]
- 27. PGC-1α, Inflammation, and Oxidative Stress - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC7085407/]
- 28. Interaction Between the Nrf2 and PGC-1α Signaling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6527603/]
- 29. Oxidative Stress and Redox Imbalance - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC11988017/]
- 30. Redox signaling in cardiovascular health and disease - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3883979/]
- 31. The Relationship of Redox With Hallmarks of Cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC9072740/]
- 32. Redox Homeostasis in Cardiovascular Disease - PMC - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC8971707/]
- 33. Redox Mechanisms in Neurodegeneration: From Disease ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6393771/]
- 34. Redox changes and cellular senescence in Alzheimer's ... [https://www.sciencedirect.com/science/article/pii/S2213231724000247]
- 35. Editorial: Redox-signaling in neurodegenerative diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC10158492/]
- 36. Oxidative stress and inflammation in the pathogenesis of ... [https://www.sciencedirect.com/science/article/pii/S2211383524004040]
- 37. Modulation of redox homeostasis: A strategy to overcome ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2023.1156538/full]
- 38. The Redox Revolution in Brain Medicine [https://www.mdpi.com/1422-0067/26/15/7498]
- 39. Redox Homeostasis and Antioxidant Signaling: A Metabolic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1167537/]
- 40. Investigation of Antioxidant Enzymes (GST, GSH, R-GSSG) in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12449866/]
- 41. Redox Biomarkers – An Effective Tool for Diagnosing COVID ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11063110/]
- 42. Mapping the oxidative stress metabolome in neurology by ... [https://www.sciencedirect.com/science/article/pii/S2213231725004380]
- 43. Redox Homeostasis and Molecular Biomarkers in ... [https://www.mdpi.com/2076-3921/13/10/1163]
- 44. Antioxidant and oxidative enzymes, genetic variants ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1700263/full]
- 45. Fundamentals of redox regulation in biology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11921270/]
- 46. Regulatory Dynamics of Nrf2 With Sirtuins in the Brain [https://pmc.ncbi.nlm.nih.gov/articles/PMC12395324/]
- 47. Modulation of Nrf2 and Mitochondrial Function [https://www.mdpi.com/1424-8247/18/11/1698]
- 48. Transcription factor NRF2: New therapeutic approach to ... [https://www.sciencedirect.com/science/article/abs/pii/B9780443219924000257]
- 49. Nrf1 is an indispensable redox-determining factor for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9520269/]
- 50. Peripheral monocyte transcriptional signatures of ... [https://pubmed.ncbi.nlm.nih.gov/40771809/]
- 51. Fundamentals of redox regulation in biology - PubMed - NIH [https://pubmed.ncbi.nlm.nih.gov/38689066/]
- 52. Unraveling the redox code to improve physiological research ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11527825/]
- 53. A quantitative tissue-specific landscape of protein redox ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8164166/]
- 54. Advanced analytical strategies to study oxidized lipids and ... [https://www.sciencedirect.com/science/article/abs/pii/S0891584919312316]
- 55. Quantitative spatial visualization of X-ray irradiation via ... [https://www.sciencedirect.com/science/article/pii/S0891584924009808]
- 56. Quantitative Redox Imaging Software [https://pubmed.ncbi.nlm.nih.gov/26154420/]
- 57. Redox Imbalance in Inflammation: The Interplay of Oxidative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12189482/]
- 58. Connecting the exposome with redox regulation in health and ... [https://redoxmedicine2025.febsevents.org/]
- 59. Quantitative analysis of redox proteome reveals oxidation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9157258/]
- 60. Targeted Redox Regulation α-Ketoglutarate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12071522/]
- 61. New Insight into Redox Homeostasis and Oxidative Stress ... [https://www.mdpi.com/journal/antioxidants/special_issues/0632N5Y2QG]
- 62. Redox platforms in cancer drug discovery and development [https://www.sciencedirect.com/science/article/abs/pii/S1367593110001559]
- 63. Oxidative stress: from molecular studies to clinical intervention ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12443558/]
- 64. Understanding Cellular Redox Homeostasis: A Challenge for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8745322/]
- 65. Importance of systemic redox homeostasis biomarkers and ... [https://pubmed.ncbi.nlm.nih.gov/40100412/]
- 66. Redox Homeostasis and Molecular Biomarkers in Precision ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11504313/]
- 67. Redox medicine: translation of basic science to the clinic [https://www.sciencedirect.com/journal/free-radical-biology-and-medicine/special-issue/10VQ4BP5J90]
- 68. Exploring the Interplay of Antioxidants, Inflammation, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12469104/]
- 69. The antioxidant paradox: less paradoxical now? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3575931/]
- 70. Potential harms of supplementation with high doses ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9241084/]
- 71. Redox homeostasis: the linchpin in stem cell self-renewal ... [https://www.nature.com/articles/cddis201350]
- 72. Paradoxical Roles of Antioxidant Enzymes: Basic Mechanisms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4839492/]
- 73. Scientists find a molecule that mimics exercise and slows ... [https://www.sciencedaily.com/releases/2025/11/251113071620.htm]
- 74. Scientists find molecule that mimics exercise, slows ageing [https://desitalkchicago.com/scientists-find-molecule-that-mimics-exercise-slows-ageing-study/]
- 75. Free radicals and their impact on health and antioxidant ... [https://www.nature.com/articles/s41420-024-02278-8]
- 76. Oxidative stress in cancer: from tumor and ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02375-x]
- 77. Oxidative Stress Fundamentals [https://www.mdpi.com/2076-3417/15/18/10191]
- 78. Interplay of oxidative stress and antioxidant mechanisms in ... [https://link.springer.com/article/10.1007/s00204-025-04146-5]
- 79. Oxidative cell death in cancer: mechanisms and ... [https://www.nature.com/articles/s41419-024-06939-5]
- 80. Living on the Edge: ROS Homeostasis in Cancer Cells and ... [https://www.mdpi.com/2076-3921/14/8/1002]
- 81. The Redox Paradox: Cancer's Double-Edged Sword for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12561025/]
- 82. The impact of oxidative balance on all-cause and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11756090/]
- 83. The association between oxidative balance scores and all ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1522048/full]
- 84. ROS Function in Redox Signaling and Oxidative Stress - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4055301/]
- 85. Thiol-Based Redox Switches - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4059413/]
- 86. Thiol-based redox switches: From chemistry to physiology and ... [http://meetings.embo.org/event/25-thiol-switches]
- 87. Beyond Antioxidants: How Redox Pathways Shape Cellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12466437/]
- 88. Reactive Oxygen Species: Beyond Their Reactive Behavior [https://pmc.ncbi.nlm.nih.gov/articles/PMC7829243/]
- 89. The Role of Reductive Stress in the Pathogenesis ... [https://pubmed.ncbi.nlm.nih.gov/40076537/]
- 90. The Role of Reductive Stress in the Pathogenesis ... [https://www.mdpi.com/1422-0067/26/5/1910]
- 91. Reductive stress: The key pathway in metabolic disorders ... [https://www.sciencedirect.com/science/article/pii/S2090123225000311]
- 92. Redox Homeostasis in Red Blood Cells: From Molecular ... [https://www.mdpi.com/1467-3045/47/8/655]
- 93. Redox-manipulating nanocarriers for anticancer drug delivery [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-024-02859-w]
- 94. Spatio-temporal control strategy of drug delivery systems ... [https://www.sciencedirect.com/science/article/pii/S016836591730514X]
- 95. Spatiotemporally controlled drug delivery via photothermally ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-023-01935-x]
- 96. Redox-manipulating nanocarriers for anticancer drug ... [https://pubmed.ncbi.nlm.nih.gov/39342211/]
- 97. Advances in hydrogen delivery strategies for therapeutic ... [https://www.sciencedirect.com/science/article/pii/S0169409X25002194?dgcid=rss_sd_all]
- 98. Importance of systemic redox homeostasis biomarkers and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12380947/]
- 99. Importance of systemic redox homeostasis biomarkers and ... [https://link.springer.com/article/10.1007/s00595-025-03026-w]
- 100. Oxidative Stress and NLRP3 Inflammasome as Markers of ... [https://www.mdpi.com/2076-3921/14/11/1311]
- 101. The Redox Paradox: Cancer's Double-Edged Sword for ... [https://www.mdpi.com/2076-3921/14/10/1187]
- 102. Redox-Directed Cancer Therapeutics: Molecular Mechanisms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2824519/]
- 103. Modulation of redox homeostasis: A strategy to overcome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10073466/]
- 104. Redox pathways in cancer drug discovery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2759182/]
- 105. Homeostasis: The Underappreciated and Far Too Often ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2020.00200/full]
- 106. Homeostatic medicine: a strategy for exploring health and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9510546/]
- 107. Hemodynamics as Surrogate End Points for Survival in ... [https://pubmed.ncbi.nlm.nih.gov/11376303/]
- 108. [Unexpected Failure of Antioxidant Clinical Trials] [https://pubmed.ncbi.nlm.nih.gov/20527403/]
- 109. Why have antioxidants failed in clinical trials? [https://pubmed.ncbi.nlm.nih.gov/18474268/]
- 110. Oxidative eustress: On constant alert for redox homeostasis [https://www.sciencedirect.com/science/article/pii/S221323172100015X]
- 111. Minimizing Oxidative Stress in the Lens: Alternative ... [https://www.mdpi.com/2076-3921/13/10/1193]
- 112. Molecular Medicine Reports [https://www.spandidos-publications.com/10.3892/mmr.2024.13387]
- 113. Antioxidant System and Endoplasmic Reticulum Stress in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10842247/]
- 114. Oxidative Stress in Cataract Formation: Is There a Treatment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11505147/]
- 115. Development of Telintra as an Inhibitor of Glutathione S- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8963531/]
- 116. Telik, Inc. Announces Positive Data Demonstrating That ... [https://www.biospace.com/telik-inc-announces-positive-data-demonstrating-that-telintra-tm-enhances-production-of-g-csf-and-gm-csf]
- 117. Activators and Inhibitors of NRF2: A Review of Their Potential ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6664516/]
- 118. Non-electrophilic NRF2 activators promote wound healing ... [https://www.nature.com/articles/s41598-024-75786-3]