NADPH and NADH: Mastering the Redox Code in Health, Disease, and Therapeutics
This article provides a comprehensive exploration of the distinct yet interconnected roles of NADPH and NADH in cellular redox biology.
NADPH and NADH: Mastering the Redox Code in Health, Disease, and Therapeutics
Abstract
This article provides a comprehensive exploration of the distinct yet interconnected roles of NADPH and NADH in cellular redox biology. Tailored for researchers and drug development professionals, it synthesizes foundational knowledge on biosynthesis, compartmentalization, and core functions in energy metabolism, antioxidation, and reductive biosynthesis. The content delves into advanced methodologies for real-time monitoring of these coenzyme pools, addresses the pathological consequences of their dysregulation in aging and cancer, and evaluates emerging therapeutic strategies targeting their metabolism. By integrating foundational principles with cutting-edge applications and comparative analysis, this review serves as a critical resource for navigating the complexities of redox biology in drug discovery and development.
The Redox Essentials: Defining the Distinct Roles of NADH and NADPH
Chemical Structures and Fundamental Redox Properties
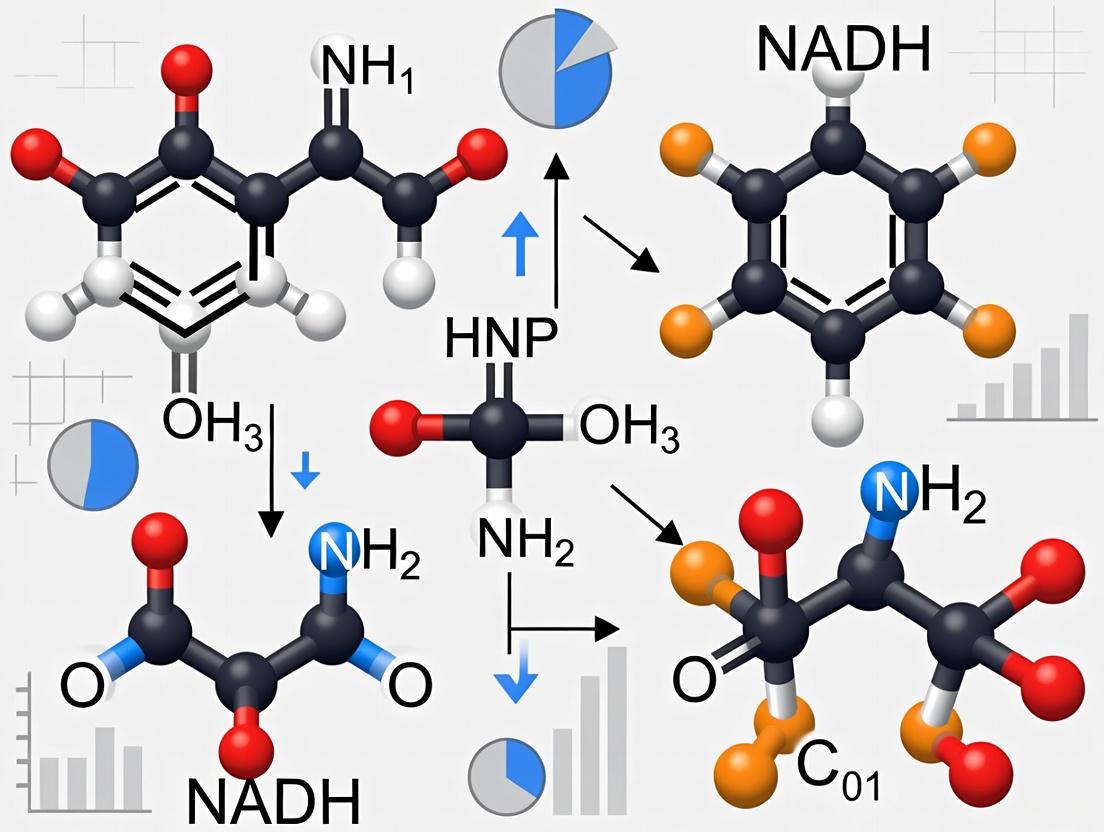
The nicotinamide adenine dinucleotide cofactors, NAD(H) and NADP(H), are fundamental to cellular redox biochemistry, serving as essential electron carriers in all living organisms [1]. The NAD pool is primarily engaged in regulating energy-producing catabolic processes, such as glycolysis and mitochondrial oxidative phosphorylation [1] [2]. In contrast, the NADP pool is crucial for anabolic biosynthesis and maintaining the cellular antioxidant defense system [1] [2]. These cofactors exist in interconvertible oxidized and reduced forms: NAD+ accepts electrons to become NADH, while NADP+ accepts electrons to become NADPH [3]. This redox interchange represents a central biochemical mechanism for transferring reducing equivalents between metabolic pathways. The chemical basis of this electron transfer involves a hydride ion transfer to the nicotinamide ring of NAD+ or NADP+, which serves as an electron sink [3]. Understanding the structural characteristics and redox properties of these molecules is crucial for interpreting their roles in cellular metabolism, energy homeostasis, and redox signaling [1] [4].
Chemical Structures and Redox Reactions
Fundamental Structural Characteristics
NAD+ and NADP+ are derivatives of nicotinic acid or nicotinamide [3]. The core structure of both molecules consists of two nucleotides joined through their phosphate groups: one nucleotide contains an adenine base, and the other contains a nicotinamide base [3]. The critical structural distinction between NAD+ and NADP+ lies in the presence of an additional phosphate group on the 2' carbon of the ribose moiety attached to adenine in NADP+ [3]. This seemingly minor modification creates a significant functional divergence, enabling enzymes to distinguish between the two cofactors and compartmentalize their metabolic roles.
The redox-active component of both molecules is the nicotinamide ring, which undergoes reversible reduction through a two-electron hydride transfer mechanism [3]. When reduced, NAD+ and NADP+ accept a hydride ion (H-, which is equivalent to a proton and two electrons), converting to NADH and NADPH, respectively. This reduction occurs specifically at the 4-position of the pyridine ring in the nicotinamide moiety, converting the quaternary nitrogen to a tertiary nitrogen, which eliminates its positive charge [3].
Table 1: Structural and Functional Comparison of NAD(H) and NADP(H)
| Characteristic | NAD(H) | NADP(H) |
|---|---|---|
| Core Structure | Two nucleotides (adenine and nicotinamide) | Identical to NAD(H) with additional phosphate |
| Phosphate Groups | One phosphate group connecting nucleotides | Additional phosphate at 2' position of adenine ribose |
| Redox Active Site | Nicotinamide ring | Identical nicotinamide ring |
| Primary Cellular Role | Catabolic processes | Anabolic processes and antioxidant defense |
| Typical Reduction State | Maintained predominantly oxidized (low NADH/NAD+ ratio) | Maintained predominantly reduced (high NADPH/NADP+ ratio) |
| Redox Reaction | NAD+ + 2e- + H+ NADH | NADP+ + 2e- + H+ NADPH |
The Hydride Transfer Mechanism
All NAD+/NADH and NADP+/NADPH reactions in biological systems involve two-electron redox steps in which a hydride ion is transferred from an organic molecule to the positively charged nitrogen of the nicotinamide ring, which serves as an electron sink [3]. This hydride transfer mechanism is fundamental to the redox function of these cofactors in dehydrogenase-catalyzed reactions. The reaction is reversible, allowing both oxidized and reduced forms to participate in metabolic pathways according to cellular requirements.
The structural similarity between NADH and NADPH means they share identical spectral properties, with both exhibiting intrinsic fluorescence in their reduced forms while their oxidized forms are non-fluorescent [5] [2]. This photophysical property has been exploited for monitoring cellular redox states since the 1950s [2], though it presents challenges in distinguishing between the two pools in living systems without advanced techniques such as fluorescence lifetime imaging microscopy (FLIM) [5] [6].
Quantitative Redox Properties and Metabolic Roles
Cellular Homeostasis and Compartmentalization
The NAD(H) and NADP(H) pools are maintained in distinct redox states to support their specialized metabolic functions. The NADH/NAD+ ratio is typically kept low (approximately 0.01-0.05) in the cytosol to facilitate catabolic processes, as NAD+ is required as an electron acceptor in glycolysis and other oxidative pathways [2] [4]. Conversely, the NADPH/NADP+ ratio is maintained high to support reductive biosynthesis and antioxidant defense mechanisms [2] [4]. This differential regulation is achieved through compartmentalization, with distinct enzymatic machineries regulating these pools in different subcellular locations [1] [7].
The conversion between NAD(H) and NADP(H) is tightly controlled by specific enzymes. NAD kinases (NADKs) facilitate the synthesis of NADP+ from NAD+ by adding the additional phosphate group, while NADP(H) phosphatases (specifically MESH1 and nocturnin in mammals) convert NADP(H) back to NAD(H) [4]. This interconversion represents a crucial regulatory node in maintaining cellular redox homeostasis [4].
Table 2: Quantitative Properties and Metabolic Roles of NAD(P)H
| Parameter | NADH | NADPH |
|---|---|---|
| Fluorescence Lifetime (free) | ~400 ps [5] | ~400 ps [5] |
| Fluorescence Lifetime (enzyme-bound) | 1340-5300 ps (depending on conformation) [5] | 1590-5300 ps (depending on conformation) [5] |
| Typical Cellular Ratio (Reduced/Oxidized) | Low (0.01-0.05 in cytosol) [2] | High (maintained in reduced state) [2] |
| Primary Metabolic Functions | Glycolysis, TCA cycle, oxidative phosphorylation [1] [2] | Fatty acid synthesis, cholesterol synthesis, antioxidant defense [1] [2] |
| Binding Affinity to NAPstar Biosensors (Kr) | 24.4-248.9 µM [7] | 0.9-11.6 µM (NADPH/NADP+ ratio) [7] |
Fluorescence Properties and Lifetime Characteristics
The intrinsic fluorescence of NADH and NADPH provides a valuable window into cellular metabolism. When probed using fluorescence lifetime imaging microscopy (FLIM), NAD(P)H emission typically resolves into two lifetime components: a short component (τ1 = 300-500 ps) associated with freely diffusing species, and a longer component (τ2 = 1500-4500 ps) attributed to enzyme-bound forms [5]. The relative abundance of these species is quantified as α2, representing the fraction of the emitting population exhibiting the longer lifetime [5].
Recent research has revealed that different enzyme binding configurations influence the fluorescence decay of NAD(P)H in live cells [5]. Specifically, the fluorescence lifetimes of bound NADH and NADPH are sensitive to enzyme conformations, with the ~400 ps lifetime of free NADH increasing to 1340(±40)ps in open enzyme conformations and 3200(±200)ps in substrate-free closed conformations [5]. The increases for NADPH were similarly significant, from ~400 ps to 1590(±50)ps and 4400(±200)ps, respectively [5]. These lifetime changes reflect the environmental sensitivity of the nicotinamide moiety, which becomes constrained in enzyme active sites during catalytic cycles.
Advanced Measurement Techniques and Methodologies
Fluorescence Lifetime Imaging Microscopy (FLIM)
FLIM has emerged as a powerful technique for probing NAD(P)H redox states in living systems with subcellular resolution. The methodology exploits the environmental sensitivity of NAD(P)H fluorescence lifetimes to distinguish between free and protein-bound populations, providing insights into metabolic activity [5] [2] [6]. Modern implementation typically involves time-correlated single photon counting (TCSPC) on multiphoton microscopy systems to achieve optimal spatial and temporal resolution [5].
Detailed FLIM Protocol for NAD(P)H:
- Sample Preparation: Cells or tissues are cultured in appropriate medium (e.g., DMEM with 10% fetal bovine serum for HEK293 cells) and plated on glass-bottom dishes for imaging [5].
- Image Acquisition: A femtosecond pulsed laser (e.g., 80 MHz Ti:Sapphire laser at 720 nm excitation) is used for two-photon excitation. Emission is collected through a 440±40 nm bandpass filter to isolate NAD(P)H fluorescence [5].
- Photon Counting: Fluorescence photons are detected using hybrid photomultiplier tubes and processed with TCSPC electronics, histogramming counts at 14.6-ps time intervals [5].
- Lifetime Analysis: Fluorescence decay curves are fitted to a bi-exponential model: I(t) = α1exp(-t/τ1) + α2exp(-t/τ2), where τ1 and τ2 represent the short and long lifetime components, respectively, and α1 and α2 their relative amplitudes [5] [6].
- Data Interpretation: Changes in the mean lifetime (τmean = α1τ1 + α2τ2) and bound fraction (α2) are interpreted in the context of metabolic perturbations, with increased α2 generally indicating a more oxidized NAD(H) pool [6].
Genetically Encoded Biosensors
The development of genetically encoded biosensors represents a significant advancement in monitoring subcellular NADP redox dynamics. The recently introduced NAPstar family of biosensors enables real-time, specific measurements of NADPH/NADP+ ratios across a broad dynamic range with subcellular resolution [7]. These sensors are based on the bacterial transcriptional repressor Rex, which undergoes conformational changes upon NADPH/NADP+ binding that alter the fluorescence of a fused fluorescent protein [7].
NAPstar Implementation Protocol:
- Sensor Expression: Cells are transfected with NAPstar constructs using appropriate gene delivery methods (e.g., lentiviral transduction for stable expression).
- Ratiometric Imaging: Fluorescence is excited at approximately 400 nm, and emission is collected at 515 nm for the T-Sapphire component and at the appropriate wavelength for the mCherry reference fluorophore (excitation ~587 nm, emission ~610 nm) [7].
- Calibration: The TS/mCherry fluorescence ratio is calibrated against known NADPH/NADP+ ratios to establish a standard curve.
- In Vivo Measurement: Live-cell imaging is performed under experimental conditions, with the TS/mCherry ratio providing quantitative information about compartment-specific NADP redox states [7].
Table 3: Research Reagent Solutions for NAD(P)H Redox Studies
| Reagent / Technology | Function / Application | Key Characteristics |
|---|---|---|
| NADMED Assay Kits | Precise measurement of all NAD(P)H forms [8] | Quantifies NAD+, NADH, NADP+, NADPH, GSSG, GSH; compatible with standard lab workflows |
| NAPstar Biosensors | Genetically encoded NADPH/NADP+ ratio sensing [7] | Real-time monitoring; subcellular resolution; Kr(NADPH/NADP+) range: 0.9-11.6 µM |
| FLIM with trFAIM | Time-resolved fluorescence anisotropy imaging [5] | Identifies enzyme binding configurations; distinguishes NADH vs NADPH contributions |
| FK866 (NAD+ Biosynthesis Inhibitor) | Experimental NAD(H) pool depletion [6] | NAMPT inhibitor; reduces NAD(H) pool size; increases NADH fluorescence lifetime |
| Nicotinamide Riboside (NR) | NAD+ precursor to increase NAD(H) pool [6] | Boosts NAD(H) levels via salvage pathway; decreases NADH fluorescence lifetime |
Experimental Applications and Methodological Considerations
Distinguishing Pool Size from Redox State
A critical advancement in NAD(P)H fluorescence research has been the development of methodologies to differentiate between changes in NAD(H) pool size versus alterations in redox state. Traditional intensity-based measurements cannot distinguish these parameters, as both increased reduction and increased total pool size elevate NAD(P)H fluorescence intensity [6]. FLIM addresses this limitation through careful analysis of lifetime components.
Experimental Approach for Pool Size Assessment:
- Chemical Modulation: Treat cells with NAD+ precursors (e.g., nicotinamide riboside, 300 µM) to increase pool size, or inhibitors (e.g., FK866, 5 nM) to decrease pool size [6].
- FLIM Measurement: Acquire NADH lifetime data across cellular compartments (mitochondria, cytoplasm, nucleus).
- Biochemical Validation: Quantify NAD+, NADH, NADP+, and NADPH levels biochemically from parallel samples to correlate lifetime changes with actual pool sizes [6].
- Metabolic Cross-Validation: Assess respiratory parameters (e.g., Oroboros respirometry) and glycolytic flux (lactate secretion) to confirm that lifetime changes reflect pool size alterations rather than redox state modifications [6].
This approach has revealed that increased NAD(H) pool size decreases the mean NADH lifetime, particularly in mitochondria, while decreased pool size increases lifetime across cellular compartments [6]. These patterns can be distinguished from redox-induced changes through their differential effects on lifetime components and correlation with biochemical measurements.
Technical Considerations and Limitations
While NAD(P)H fluorescence techniques provide powerful insights into cellular metabolism, several important considerations must be addressed for proper experimental design and data interpretation:
- pH Sensitivity: The fluorescence properties of NAD(P)H, particularly lifetime measurements, can be influenced by local pH variations, especially in the mitochondrial matrix where pH fluctuations occur during metabolic transitions [6].
- Protein Binding Specificity: The fluorescence lifetime of enzyme-bound NAD(P)H varies significantly depending on the specific enzyme and its conformational state, with different binding configurations associated with lifetimes both longer and shorter than unbound NAD(P)H [5].
- Spectral Overlap: The identical spectral properties of NADH and NADPH necessitate advanced techniques such as FLIM or genetically encoded biosensors to distinguish their contributions to the total fluorescence signal [2] [7].
- Compartmentalization: The NAD(H) and NADP(H) pools are highly compartmentalized within cells, with distinct subcellular redox states that may not be reflected in whole-cell measurements [1] [7].
Advanced techniques such as time-resolved fluorescence anisotropy imaging (trFAIM) can address some of these limitations by identifying multiple enzyme binding configurations and their influence on fluorescence decay kinetics [5]. Combined with mathematical modeling of redox-dependent binding equilibria, these approaches provide increasingly sophisticated interpretation of NAD(P)H fluorescence in the context of cellular biochemistry.
Nicotinamide adenine dinucleotide (NAD+) is a fundamental coenzyme essential for cellular metabolism, serving as a critical cofactor for oxidoreductases and a substrate for NAD+-consuming enzymes such as sirtuins, PARPs, and CD38. The biosynthesis and balance of NAD+ and its phosphorylated counterpart, NADP+, are pivotal for maintaining redox homeostasis, energy metabolism, and numerous biological processes. This whitepaper delineates the three primary NAD+ biosynthetic pathways—de novo, Preiss-Handler, and salvage—framed within the context of redox biology research. We provide a comprehensive technical guide detailing pathway mechanisms, key enzymes, and regulatory checkpoints, supplemented with structured quantitative data, experimental methodologies, and visualization tools. Aimed at researchers and drug development professionals, this review underscores the interconnectedness of NAD+ metabolism with cellular redox states and highlights emerging therapeutic strategies targeting these pathways for treating metabolic diseases, neurodegenerative disorders, and cancer.
The nicotinamide adenine dinucleotide (NAD+) / reduced NAD+ (NADH) and NADP+ / reduced NADP+ (NADPH) redox couples are indispensable for maintaining cellular redox homeostasis and modulating a plethora of biological events, including cellular metabolism [1]. NAD+ functions not only as a coenzyme for oxidoreductases but also as a substrate for NAD+-consuming enzymes, such as sirtuins (SIRT1-7), poly(ADP-ribose) polymerases (PARPs), and cADP-ribose synthases (CD38/CD157) [1]. The phosphorylated form, NADP+, together with its reduced form, NADPH, is primarily involved in maintaining redox balance and supporting biosynthetic pathways for fatty acids and nucleic acids [1]. Deficiency or imbalance of these redox couples has been associated with numerous pathological disorders, including cardiovascular diseases, neurodegenerative diseases, cancer, and aging [1]. The biosynthesis and distribution of cellular NAD(H) and NADP(H) are highly compartmentalized, making it critical to understand how cells maintain the steady levels of these redox couples to ensure normal functions and avoid redox stress [1]. This review focuses on the three major NAD+ biosynthetic pathways, examining their distinct roles, regulation, and contributions to the cellular redox state.
NAD+ Biosynthetic Pathways
In mammalian cells, NAD+ is synthesized from various precursors, including tryptophan (Trp), nicotinic acid (NA), nicotinamide (NAM), and nicotinamide riboside (NR), through three established pathways: the de novo pathway, the Preiss-Handler pathway, and the salvage pathway [1]. The salvage pathway predominates in most cell types, but all pathways are crucial for maintaining NAD+ pools in different tissues and under varying physiological conditions [1].
The De Novo Pathway from Tryptophan
De novo NAD+ synthesis from the amino acid L-tryptophan is an eight-step process mediated by enzymes in the kynurenine pathway [9] [1]. The first and rate-limiting step is the conversion of L-tryptophan to N-formylkynurenine, catalyzed by either indoleamine 2,3-dioxygenase (IDO) or tryptophan 2,3-dioxygenase (TDO) [1]. TDO is primarily expressed in the liver, while IDO expression has been detected in extrahepatic cells, including human vascular endothelial and smooth muscle cells, dermal fibroblasts, macrophages, neurons, microglia, and astrocytes [1]. Subsequent steps involve the transformation of N-formylkynurenine to kynurenine, then to 3-hydroxykynurenine, and finally to an unstable intermediate, 2-amino-3-carboxy-muconate-semialdehyde (ACMS) [9] [1]. ACMS represents a critical branch point: it can be decarboxylated by ACMS decarboxylase (ACMSD) and removed from the NAD+ synthesis pathway, or it can spontaneously cyclize to form quinolinic acid (QA) [1]. QA is then converted to nicotinic acid mononucleotide (NAMN) by quinolinate phosphoribosyltransferase (QPRT). This QPRT reaction is inefficient and constitutes a second rate-limiting step, rendering tryptophan-dependent synthesis less efficient than the other NAD+ biosynthetic pathways [1]. From NAMN, the pathway converges with the Preiss-Handler route.
Table 1: Key Enzymes in the De Novo Synthesis Pathway
| Enzyme | Gene | Function | Tissue/Organelle Specificity |
|---|---|---|---|
| Tryptophan 2,3-dioxygenase | TDO2 | Converts Trp to N-formylkynurenine (rate-limiting) | Primarily liver [1] |
| Indoleamine 2,3-dioxygenase | IDO1 | Converts Trp to N-formylkynurenine (rate-limiting) | Extrahepatic; endothelial cells, fibroblasts, immune cells [1] |
| Kynurenine 3-hydroxylase | N/A | Hydroxylates kynurenine to 3-hydroxykynurenine | Abundant in liver, placenta [1] |
| ACMS decarboxylase | ACMSD | Decarboxylates ACMS, diverting it from NAD+ synthesis | Regulates NAD+ yield from Trp [1] |
| Quinolinate phosphoribosyltransferase | QPRT | Converts quinolinic acid to NAMN (rate-limiting) | Low efficiency [1] |
Diagram 1: The de novo biosynthesis pathway of NAD+ from tryptophan. Key regulatory enzymes and branch points are highlighted.
The Preiss-Handler Pathway
The Preiss-Handler pathway utilizes dietary nicotinic acid (NA, or niacin) as a precursor [9]. This pathway was first identified in human erythrocytes and rat liver and involves a three-step process to convert NA into NAD+ [1]. The first step is the conversion of NA to NAMN, catalyzed by NA phosphoribosyltransferase (NAPRT) at the expense of phosphoribosyl pyrophosphate (PRPP) [9] [1]. NAPRT expression is widespread, and its mRNA has been detected in almost all human tissues tested [1]. Interestingly, NAPRT activity is subject to complex allosteric regulation by ATP and various metabolites. ATP can stimulate or inhibit NAPRT activity at low or high concentrations, respectively, while metabolites like dihydroxyacetone phosphate (DHAP) and pyruvate stimulate its activity, and others like glyceraldehyde-3-phosphate (G3P) and acetyl-CoA inhibit it [1]. NAMN, the product of this reaction, serves as the converging point with the de novo pathway. It is then adenylated to NAAD by nicotinic acid mononucleotide adenylyltransferases (NMNATs) [9]. The final step is the amidation of NAAD to NAD+ by NAD+ synthetase (NADSYN), which uses glutamine or ammonia as an amide donor [9] [1]. NA is a more efficient NAD+ precursor than tryptophan, as 1 mg of dietary NA is equivalent to approximately 60 mg of dietary Trp [1].
The Salvage Pathway
The NAD+ salvage pathway recycles nicotinamide (NAM) generated as a by-product of the enzymatic activities of NAD+-consuming enzymes, such as sirtuins, PARPs, and CD38 [9]. This pathway is crucial for maintaining NAD+ levels in most cell types and predominates under normal physiological conditions [1]. The rate-limiting enzyme in this pathway is nicotinamide phosphoribosyltransferase (NAMPT), which recycles NAM into nicotinamide mononucleotide (NMN) [9] [1]. Subsequently, NMN is converted into NAD+ via the action of NMN adenylyltransferases (NMNATs) [9]. In mammals, three isoforms of NMNATs exist with distinct tissue and organelle-specific distributions, which explains the cellular compartmentalization of NAD+ synthesis [1]. NMNAT1 is an exclusively nuclear enzyme ubiquitously expressed, with high abundance in the heart and skeletal muscle. NMNAT2 is located in the cytosol and Golgi apparatus and is principally expressed in the brain. NMNAT3 is found in the cytosol and mitochondria and is mostly present in the human lung and spleen [1]. The salvage pathway is a key regulatory point in NAD+ metabolism, and its inhibition can significantly impact cellular NAD+ levels.
Table 2: Core Enzymes of the Preiss-Handler and Salvage Pathways
| Pathway | Enzyme | Gene | Function | Key Features |
|---|---|---|---|---|
| Preiss-Handler | Nicotinic Acid Phosphoribosyltransferase | NAPRT1 | Converts NA to NAMN | Widespread expression; allosterically regulated by ATP & metabolites [1] |
| NMN Adenylyltransferases | NMNAT1/2/3 | Converts NAMN to NAAD | Three isoforms with distinct subcellular localizations [9] [1] | |
| NAD+ Synthetase | NADSYN1 | Converts NAAD to NAD+ | Uses glutamine/ammonia [9] | |
| Salvage | Nicotinamide Phosphoribosyltransferase | NAMPT | Recycles NAM to NMN (rate-limiting) | Key regulator of NAD+ levels via salvage [9] [1] |
| NMN Adenylyltransferases | NMNAT1/2/3 | Converts NMN to NAD+ | Same enzymes as Preiss-Handler, different substrate [9] | |
| NAD+-Consuming Enzymes | SIRTs, PARPs, CD38 | Generate NAM as a by-product | Create demand for the salvage pathway [9] |
Diagram 2: The Preiss-Handler and Salvage pathways. The salvage pathway forms a cycle, recycling NAM generated by NAD+-consuming enzymes.
Quantitative Pathway Comparison
The three biosynthetic pathways contribute differently to the cellular NAD+ pool, exhibit distinct efficiencies, and are active in various tissue types. Understanding these quantitative differences is essential for designing targeted metabolic interventions.
Table 3: Quantitative Comparison of NAD+ Biosynthetic Pathways
| Characteristic | De Novo Pathway | Preiss-Handler Pathway | Salvage Pathway |
|---|---|---|---|
| Primary Precursor | Tryptophan [1] | Nicotinic Acid (NA) [9] | Nicotinamide (NAM) [9] |
| Precursor Efficiency | ~60 mg Trp ≈ 1 mg NA [1] | High efficiency [1] | High efficiency; dominant in most cells [1] |
| Key Rate-Limiting Enzyme(s) | IDO/TDO; QPRT [1] | NAPRT [1] | NAMPT [1] |
| Tissue Prevalence | Liver (TDO); widespread extrahepatic (IDO) [1] | Widespread (NAPRT expressed in most tissues) [1] | Predominant in most cell types [1] |
| Major Metabolic Role | De novo generation from amino acid | Generation from vitamin precursor | Recycling of NAM from signaling enzymes |
Interplay with NADPH and Redox Biology
The cellular redox state is centrally regulated by the balance of NAD+/NADH and NADP+/NADPH. These redox couples engage in distinct but interconnected metabolic pathways. The NAD+/NADH ratio is a primary regulator of cellular energy metabolism, governing glycolysis and mitochondrial oxidative phosphorylation. In contrast, the NADP+/NADPH ratio is crucial for reductive biosynthesis (e.g., of fatty acids and nucleic acids) and antioxidant defense, primarily through the glutathione system [1] [10]. The phosphorylation of NAD+ to NADP+ is catalyzed by NAD+ kinase (NADK), the key determinant of cellular NADPH concentration [10]. Research using fluorescence lifetime imaging (FLIM) has demonstrated that the balance between enzyme-bound NADPH and NADH can be quantitatively measured in live cells, as they exhibit distinct fluorescence decay rates when bound to their respective enzymes [10]. This technology has revealed that perturbations in the NADPH/NADH balance are a hallmark of various diseases, including cancer [10]. Furthermore, the redox state of another key metabolite, coenzyme Q (CoQ), which is intricately linked to NADH oxidation in the mitochondrial electron transport chain, also reflects and influences the cellular metabolic state and can contribute to redox signaling [11]. Therefore, the biosynthesis of NAD+ via the de novo, Preiss-Handler, and salvage pathways directly fuels the pools of both NADH and NADPH, making these pathways upstream masters of the cellular redox environment.
Experimental Protocols and Research Tools
Investigating NAD+ biosynthetic pathways and their roles in redox biology requires a combination of genetic, pharmacological, and advanced imaging techniques.
Genetic and Pharmacological Modulation of Pathways
A common experimental approach involves genetically or pharmacologically manipulating key enzymes in the NAD+ biosynthetic pathways to observe the resulting metabolic and phenotypic consequences.
- NADK Manipulation: To alter NADPH levels, researchers can overexpress or knock down NAD+ kinase (NADK). This manipulation significantly changes the [NADPH] without drastically affecting [NADH], allowing for the study of NADPH-specific roles [10].
- NAMPT Inhibition: The inhibitor FK866 is a potent and specific blocker of NAMPT, the rate-limiting enzyme in the salvage pathway. Treating cells with FK866 rapidly depletes NAD+ levels, making it a valuable tool for studying the dependence of cellular processes on the salvage pathway [12].
- Pathway Bypass Strategy: A sophisticated pharmacological strategy to study axon degeneration involved combining FK866 (to inhibit the NMN-producing salvage pathway) with nicotinic acid riboside (NAR). NAR is converted to NAMN via NRK, forcing NAD+ synthesis through the Preiss-Handler pathway and bypassing NMN accumulation. This combination protected neurons, demonstrating a therapeutic strategy for chemotherapy-induced peripheral neuropathy [12].
Fluorescence Lifetime Imaging (FLIM) of NAD(P)H
FLIM is a powerful non-destructive technique to study the redox state of live cells and tissues by exploiting the autofluorescence of NADH and NADPH.
- Principle: While NADH and NADPH are spectrally identical, their fluorescence decay rates (lifetimes) differ when bound to different enzymes. FLIM measures these nanosecond-scale decay rates, allowing for the quantitative separation of the signals from enzyme-bound NADH and NADPH [10] [13].
- Protocol Outline:
- Cell Preparation: Culture cells (e.g., HEK293) on glass-bottom dishes.
- FLIM Imaging: Acquire images using a two-photon microscope equipped with a time-correlated single-photon counting (TCSPC) system. Excitation wavelength is typically ~740 nm for two-photon excitation of NAD(P)H, with emission collected at 440–470 nm [10] [13].
- Data Fitting: Fit the fluorescence decay curve at each pixel to a multi-exponential model. The short lifetime component (~0.4 ns) corresponds to free NAD(P)H, while the longer, variable lifetime component (τbound, ~1.9–5.7 ns) represents the enzyme-bound pool [10] [13].
- Interpretation: An increase in the average Ï„bound indicates a higher ratio of enzyme-bound NADPH to NADH, as NADPH exhibits a longer fluorescence lifetime when bound [10]. This was validated using NADK+ cells (high NADPH) and the NADPH-binding competitor epigallocatechin gallate (EGCG) [10].
Diagram 3: Experimental workflow for Fluorescence Lifetime Imaging (FLIM) to separate NADH and NADPH signals in live cells.
The Scientist's Toolkit: Key Research Reagents
Table 4: Essential Reagents for NAD+ Pathway and Redox Biology Research
| Reagent / Tool | Function / Target | Brief Description & Research Application |
|---|---|---|
| FK866 | NAMPT inhibitor [12] | Small molecule inhibitor of the salvage pathway's rate-limiting enzyme; used to deplete cellular NAD+ and study pathway dependence. |
| Nicotinic Acid Riboside (NAR) | NAD+ precursor [12] | A deamidated form of NR; channels NAD+ synthesis through the Preiss-Handler pathway (via NAMN), bypassing NMN. Used in combination with FK866. |
| E. coli NMN Deamidase (NMNd) | Enzyme converting NMN to NAMN [12] | A genetic tool expressed in cells to reduce NMN levels. Used to investigate the specific role of NMN in axonal degeneration. |
| EGCG (Epigallocatechin gallate) | Competitive inhibitor of NADPH-binding [10] | Preferentially competes for NADPH-binding sites on enzymes. Used in FLIM experiments to specifically reduce the bound NADPH signal. |
| Genetically Encoded Biosensors | e.g., NAD+/NADH or NADP+/NADPH sensors [14] | Fluorescent protein-based sensors (e.g., SoNar, iNAP) that allow real-time, compartment-specific monitoring of pyridine nucleotide ratios in live cells. |
| FLIM (Fluorescence Lifetime Imaging) | Endogenous NAD(P)H fluorescence [10] [13] | An advanced microscopy technique that quantifies fluorescence decay rates to separate the contributions of NADH and NADPH based on their enzyme-bound lifetimes. |
| CS17919 | CS17919, MF:C22H20F4N6O2, MW:476.4 g/mol | Chemical Reagent |
| Sinapinic acid | Sinapinic acid, CAS:7361-90-2, MF:C11H12O5, MW:224.21 g/mol | Chemical Reagent |
The de novo, Preiss-Handler, and salvage pathways form an integrated network for NAD+ biosynthesis, each with unique characteristics, regulatory mechanisms, and tissue-specific importance. The salvage pathway, centered on NAMPT, is the dominant route for NAD+ production in many cells and represents a critical regulatory node. The de novo and Preiss-Handler pathways provide essential backup and alternative inputs, with the Preiss-Handler pathway being particularly efficient. The interplay between these pathways ensures the maintenance of NAD+ and NADPH pools, which in turn govern cellular redox balance, energy metabolism, and signaling. Disruptions in this balance are implicated in a spectrum of diseases, making enzymes in these pathways attractive therapeutic targets. Contemporary research tools, including specific inhibitors like FK866, precursor molecules like NAR, and advanced imaging techniques like FLIM, are revolutionizing our ability to probe these pathways with high specificity in live cells and tissues. A deep understanding of NAD+ biosynthetic pathways is therefore fundamental to advancing redox biology research and developing novel therapeutics for metabolic, neurodegenerative, and oncological diseases.
In redox biology, the distinct roles of nicotinamide adenine dinucleotide (NAD) and its phosphorylated counterpart, nicotinamide adenine dinucleotide phosphate (NADP), are fundamentally defined by their subcellular localization. Although these molecules share closely related structures, they are recognized by unique compartmentalized enzymes and exert dramatically different functions within the cell [1] [15]. The NAD pool, comprising NAD+ and NADH, is primarily engaged in catabolic reactions and cellular energy metabolism, functioning as a central regulator of glycolysis and mitochondrial oxidative phosphorylation [1] [2]. In contrast, the NADP pool (NADP+/NADPH) is predominantly involved in cellular antioxidative effects and anabolic reductive biosynthesis [1] [15]. This functional specialization necessitates strict compartmentalization, with separate cytosolic, mitochondrial, and nuclear pools providing reducing power in each respective location to maintain redox homeostasis and support compartment-specific metabolic needs [16].
The redox states of these separate pyridine nucleotide pools play critical roles in defining the activity of energy-producing pathways, driving oxidative stress, and maintaining antioxidant defences [2]. Defects in the balance of these pathways are associated with numerous diseases, from diabetes and neurodegenerative diseases to heart disease and cancer, making the understanding of their compartmentalization essential for therapeutic development [2] [15]. This whitepaper provides an in-depth technical examination of the distinct pools of NAD(H) and NADP(H) within cellular compartments, their metabolic roles, and the advanced methodologies used to investigate them.
Compartmentalized NAD(H) and NADP(H) Pools: Distribution and Functions
Quantitative Distribution of Pyridine Nucleotides Across Compartments
The biosynthesis and distribution of cellular NAD(H) and NADP(H) are highly compartmentalized, with distinct pools maintained in the cytosol, mitochondria, and nucleus [1]. The following table summarizes the quantitative distribution and characteristics of these pools based on current research findings.
Table 1: Characteristics of NAD(P)H Pools in Cellular Compartments
| Cellular Compartment | Primary Redox Couple | Typical Ratio | Concentration | Key Functions |
|---|---|---|---|---|
| Cytosol | NAD+/NADH | NADH/NAD+: 0.01-0.05 [2] | NADPH: 3.1 ± 0.3 µM (HeLa cells) [15] | Glycolysis, PPP, fatty acid synthesis, antioxidant defense (GSH system) |
| Mitochondria | NAD+/NADH | Low NADH/NAD+ [2] | NADPH: 37 ± 2 µM (HeLa cells) [15] | TCA cycle, oxidative phosphorylation, antioxidant defense (mitochondrial TRX, GSH) |
| Nucleus | NAD+/NADH | Varies by cell state | Information not available in search results | Substrate for Sirtuins, PARPs, DNA repair, epigenetic regulation |
Molecular Machinery Maintaining Compartmentalized Pools
The maintenance of separate NAD(H) and NADP(H) pools requires specialized enzymatic machinery and transport systems in each compartment:
NAD Biosynthesis Enzymes: The three isoforms of NMN adenylyltransferases (NMNATs) exhibit distinct organelle-specific distribution. NMNAT1 is an exclusively nuclear enzyme ubiquitously expressed in human tissues, with high abundance in the heart and skeletal muscle. NMNAT2 is located in the cytosol and Golgi apparatus, principally expressed in the brain. NMNAT3 is found in the cytosol and mitochondria, mostly present in human lung and spleen [1]. This tissue- and organelle-specific expression pattern explains the cellular compartmentalization of NAD+ [1].
NADP Biosynthesis: NADP+ is synthesized from NAD+ via NAD kinases (NADKs), which are found in almost all human organs except skeletal muscle and are localized in both cytosol (cNADK) and mitochondria (mNADK) [15]. The mitochondrial NADK (mNADK) has a distinctive feature—it can directly phosphorylate NADH to generate NADPH to alleviate oxidative stress in mitochondria [15].
Redox Shuttles: The malate-aspartate shuttle facilitates the transfer of reducing equivalents from cytosolic NADH to mitochondrial NAD+, linking glycolytic NADH production to mitochondrial respiration [2]. This shuttle plays a significant role in numerous biological processes, including insulin secretion, cancer cell survival, and heart and neurodegenerative diseases [2].
Methodologies for Investigating Compartmentalized Pools
Fluorescence Lifetime Imaging Microscopy (FLIM)
The intrinsic fluorescence of the reduced forms (NADH and NADPH) has been used as a label-free method for monitoring intracellular redox state for more than 60 years [2]. However, since the fluorescence spectra of NADH and NADPH are indistinguishable, interpreting the signals resulting from their combined fluorescence (labeled NAD(P)H) is complex. Fluorescence Lifetime Imaging Microscopy (FLIM) offers the potential to discriminate between the two separate pools, as the fluorescence lifetime of these molecules is highly sensitive to changes in their local environment [2].
Table 2: Key Methodologies for Studying Compartmentalized NAD(P)H Pools
| Methodology | Key Principle | Compartment Resolution | Primary Applications |
|---|---|---|---|
| NAD(P)H FLIM | Measures fluorescence lifetime (optical half-life) sensitive to molecular environment [2] | Subcellular (mitochondrial vs. cytosolic) | Discrimination between free and protein-bound NAD(P)H; metabolic state assessment |
| Stable Isotope Tracing (²H) | Tracing hydrogen in compartmentalized reactions using NADPH as cofactor [16] | Can resolve cytosolic vs. mitochondrial pathways | Quantifying PPP contribution to cytosolic NADPH; resolving direction of compartmentalized redox reactions |
| Genetically Encoded Biosensors | Protein-based sensors with selective compartment targeting [1] | Specific compartment targeting (e.g., mito-GFP) | Real-time monitoring of compartment-specific NADPH/NADP+ ratios or NADH levels |
| Biochemical Fractionation | Physical separation of cellular compartments followed by HPLC/MS analysis | Isolated mitochondria, cytosol, nuclei | Absolute quantification of pool sizes and redox ratios in purified organelles |
Stable Isotope Tracing for NADPH Metabolism
A sophisticated approach to resolve NADP(H)-dependent pathways in distinct compartments involves using ²H stable isotopes to trace NADPH metabolism. This method enables researchers to:
- Quantify the pentose phosphate pathway contribution to cytosolic NADPH [16]
- Distinguish between cytosolic and mitochondrial NADPH using specialized reporter systems [16]
- Resolve the direction of otherwise identical compartmentalized redox reactions in intact cells [16]
By tracing hydrogen in compartmentalized reactions that use NADPH as a cofactor, including the production of 2-hydroxyglutarate by mutant isocitrate dehydrogenase enzymes, researchers can observe metabolic pathway activity in these distinct cellular compartments [16]. Using this system, scientists have determined the direction of serine/glycine interconversion within the mitochondria and cytosol, highlighting the ability of this approach to resolve compartmentalized reactions in intact cells [16].
Experimental Protocols for Key Methodologies
Protocol: NAD(P)H FLIM for Mitochondrial Redox State Assessment
Principle: This protocol utilizes the natural fluorescence of NADH and NADPH to assess compartmentalized redox states through fluorescence lifetime measurements, which can help distinguish between protein-bound and free states of these cofactors [2].
Procedure:
- Sample Preparation: Culture cells on glass-bottom dishes or prepare tissue slices (100-300 µm thickness) to maintain physiological conditions.
- Two-Photon Excitation: Use a mode-locked titanium-sapphire laser tuned to 740 nm for two-photon excitation of NAD(P)H fluorescence.
- Emission Collection: Collect emitted fluorescence through a 460/80 nm bandpass filter to isolate the NAD(P)H signal.
- Lifetime Data Acquisition: Acquire time-correlated single photon counting (TCSPC) data using a high-sensitivity detector (e.g., photomultiplier tube or hybrid detector).
- Lifetime Analysis: Fit fluorescence decay curves to a bi-exponential model using specialized software:
- Short lifetime component (τ₠≈ 0.4 ns): Represents free NAD(P)H
- Long lifetime component (τ₂ ≈ 2.0 ns): Represents protein-bound NAD(P)H
- Compartment-Specific Analysis: Use mitochondrial markers (e.g., TMRM) to isolate mitochondrial signals, or analyze distinct subcellular regions.
Data Interpretation: Shifts toward longer average lifetimes indicate increased protein binding of NAD(P)H, typically associated with a more oxidized state of the NAD pool in energy-producing pathways [2].
Protocol: Compartment-Specific NADPH Production Using ²H Tracing
Principle: This method uses deuterated water (²H₂O) to trace NADPH metabolism in specific cellular compartments by following the incorporation of deuterium into metabolites dependent on NADPH as a cofactor [16].
Procedure:
- Isotope Labeling: Incubate cells in culture medium supplemented with 4% ²H₂O for 24-48 hours to achieve equilibrium labeling.
- Metabolite Extraction: Harvest cells and use methanol:water extraction to preserve redox metabolites.
- Compartmental Fractionation (Optional): Use digitonin-based permeabilization or mechanical fractionation to isolate mitochondrial and cytosolic fractions.
- LC-MS Analysis: Analyze metabolites using liquid chromatography-mass spectrometry (LC-MS) with multiple reaction monitoring (MRM) for NADPH-dependent metabolites.
- Deuterium Incorporation Quantification: Calculate the percentage of deuterium enrichment in metabolites such as 2-hydroxyglutarate (produced by mutant IDH enzymes) that serve as reporters for NADPH utilization.
- Pathway Contribution Analysis: Use mathematical modeling to attribute NADPH production to specific pathways (PPP, ME, IDH) in each compartment.
Applications: This approach can determine the relative contributions of different pathways to cytosolic versus mitochondrial NADPH pools and resolve the direction of redox reactions within specific compartments [16].
Visualization of Compartmentalized NAD(P)H Metabolism
Diagram Title: NAD(P)H Metabolism Across Cellular Compartments
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for Studying NAD(P)H Compartmentalization
| Tool/Reagent | Vendor/Provider | Function/Application | Key Features |
|---|---|---|---|
| NAD/NADP Assay Kits | NADMED [8] [17] | Precise measurement of all four forms (NAD+, NADH, NADP+, NADPH) | Eliminates limitations of previous methods; fast, reliable, cost-effective; integrates with standard workflows |
| Genetically Encoded Biosensors | Multiple academic sources | Real-time monitoring of compartment-specific NADPH/NADP+ ratios or NADH levels | Targetable to specific compartments (e.g., mito-roGFP); enables live-cell imaging |
| Deuterated Tracers (²H₂O) | Cambridge Isotopes | Tracing NADPH metabolism in specific compartments | Enables quantification of pathway contributions to NADPH pools |
| Fluorescence Lifetime Microscopy Systems | Multiple manufacturers (e.g., Leica, Zeiss) | NAD(P)H FLIM for metabolic state assessment | Discriminates between NADH and NADPH based on lifetime; subcellular resolution |
| Compartment-Specific Enzyme Inhibitors | Multiple suppliers (e.g., Sigma, Tocris) | Selective inhibition of compartment-specific NADPH-producing enzymes | cNADK vs mNADK inhibitors; G6PD inhibitors; IDH-specific inhibitors |
| Sugemalimab | Sugemalimab, CAS:2256084-03-2, MF:C6H11ClN2, MW:146.62 g/mol | Chemical Reagent | Bench Chemicals |
| Nlrp3-IN-13 | Nlrp3-IN-13, MF:C19H15N3O3S, MW:365.4 g/mol | Chemical Reagent | Bench Chemicals |
The compartmentalization of NAD(H) and NADP(H) pools represents a fundamental organizational principle of eukaryotic cells that enables the simultaneous regulation of diverse metabolic processes. Understanding these separate pools—with their distinct biosynthesis pathways, redox states, and functional roles—is crucial for advancing redox biology research and developing targeted therapeutic interventions. The continued refinement of research tools, particularly those enabling precise measurement and spatial resolution of these metabolites, will drive future discoveries in metabolic diseases, cancer, aging, and degenerative disorders. As these methodologies become more sophisticated and accessible, researchers will be better equipped to address a host of pathological conditions characterized by disrupted NAD(P)H homeostasis.
Nicotinamide adenine dinucleotide (NADH) serves as a central redox coenzyme in catabolic energy metabolism, channeling electrons from metabolic pathways to the mitochondrial electron transport chain. This whitepaper provides a technical analysis of NADH's role in glycolysis and oxidative phosphorylation, emphasizing its critical function in energy transduction. We present quantitative data on ATP yields, detailed methodologies for investigating NADH metabolism, and visualization of key pathways. The integration of NADH production and oxidation represents a fundamental coupling mechanism that enables efficient energy harvesting from fuel molecules, with significant implications for therapeutic targeting in metabolic diseases and cancer.
NADH (nicotinamide adenine dinucleotide, reduced form) functions as an essential electron carrier in cellular redox reactions, operating in concert with its oxidized form NAD+ [18]. This redox couple facilitates the transfer of electrons in numerous metabolic processes, particularly those involved in energy extraction from organic fuels. The NAD+/NADH ratio reflects the cellular redox state and regulates metabolic flux between anabolic and catabolic pathways [18]. In the context of energy metabolism, NADH serves as a critical link between carbon-oxidizing pathways and the proton-motive force generation system, ultimately driving ATP synthesis.
The molecular structure of NADH enables its electron-carrying capacity through the nicotinamide ring, which undergoes reversible oxidation and reduction reactions. When NAD+ accepts two electrons and one proton (a hydride ion), it converts to NADH, storing potential energy that can be harnessed for ATP production [19]. This redox coupling is particularly crucial in the two primary ATP-generating processes in aerobic cells: glycolysis in the cytosol and oxidative phosphorylation in mitochondria.
NADH in Glycolysis
Glycolytic Pathway and NADH Production
Glycolysis is a ten-step metabolic pathway occurring in the cytosol that converts one glucose molecule into two pyruvate molecules [20] [21]. This process can be divided into two distinct phases: the preparatory (investment) phase requiring ATP consumption, and the pay-off phase generating ATP and reducing equivalents [20]. A critical NADH-producing step occurs at the sixth reaction of glycolysis, where glyceraldehyde-3-phosphate undergoes oxidation to 1,3-bisphosphoglycerate, catalyzed by glyceraldehyde-3-phosphate dehydrogenase [20]. During this reaction, NAD+ is reduced to NADH, simultaneously with the incorporation of inorganic phosphate to create a high-energy acyl phosphate group.
The glycolytic pathway yields a net production of 2 ATP molecules and 2 NADH molecules per glucose molecule [20] [21]. Under aerobic conditions, these NADH molecules must be reoxidized to regenerate NAD+, which is essential for sustaining glycolytic flux. In eukaryotic cells, this is accomplished by shuttling the reducing equivalents into mitochondria for oxidation by the electron transport chain.
Regulation at the Molecular Level
Glycolytic regulation occurs at several key enzymatic steps, including those catalyzed by hexokinase, phosphofructokinase-1 (PFK-1), and pyruvate kinase [20]. PFK-1 represents the primary regulatory point, controlled by allosteric effectors including ATP, citrate, and fructose-2,6-bisphosphate. The latter is generated by phosphofructokinase-2 (PFK-2), whose activity is hormonally regulated through insulin-mediated dephosphorylation [20]. This intricate regulatory network ensures that glycolytic flux responds to cellular energy status and substrate availability.
Table 1: NADH and ATP Balance in Glycolysis
| Reactant/Product | Quantity per Glucose Molecule | Cellular Location |
|---|---|---|
| Glucose | -1 | Cytosol |
| NAD+ | -2 | Cytosol |
| ADP | -2 | Cytosol |
| Pyruvate | +2 | Cytosol |
| NADH | +2 | Cytosol |
| ATP | +2 (net) | Cytosol |
NADH in Oxidative Phosphorylation
Electron Transport Chain Architecture
The mitochondrial electron transport chain (ETC) consists of four protein complexes embedded in the inner mitochondrial membrane, plus two mobile electron carriers [22] [23] [24]. NADH derived from both glycolysis and the citric acid cycle delivers electrons to Complex I (NADH:ubiquinone oxidoreductase), initiating the electron transfer process [23]. Complex I catalyzes the transfer of electrons from NADH to ubiquinone (coenzyme Q), coupled with the translocation of four protons across the inner mitochondrial membrane [23] [24].
The electron flow continues through Complex III (ubiquinol:cytochrome c oxidoreductase) and Complex IV (cytochrome c oxidase), with additional proton pumping at each complex [22] [23]. The final electron acceptor is molecular oxygen, which is reduced to water at Complex IV [23]. Throughout this process, the stepwise transfer of electrons through complexes with progressively higher reduction potentials enables the controlled release of energy, which is harnessed to create the proton gradient.
Chemiosmotic Coupling and ATP Synthesis
The proton gradient generated by electron transport creates an electrochemical potential across the inner mitochondrial membrane, comprising both a pH gradient (ΔpH) and an electrical potential (ΔΨ) [22]. This proton-motive force drives ATP synthesis through Complex V (ATP synthase), which couples the energetically favorable flow of protons back into the mitochondrial matrix with the phosphorylation of ADP to ATP [22] [23]. The ATP synthase operates through a rotational catalytic mechanism, where proton passage through the F₀ subunit induces conformational changes in the F₠subunit that facilitate ATP synthesis [22].
The oxidation of one NADH molecule typically drives the synthesis of approximately 2.5-3 ATP molecules, though theoretical yields may be higher [22] [23]. This high ATP yield underscores the metabolic advantage of aerobic respiration over anaerobic pathways.
Table 2: ATP Yield from Glucose Oxidation via NADH-Dependent Processes
| Metabolic Process | ATP Produced | NADH Produced | FADHâ‚‚ Produced | Total ATP (approx.) |
|---|---|---|---|---|
| Glycolysis | 2 (net) | 2 | 0 | 2 |
| Pyruvate Oxidation | 0 | 2 | 0 | 0 |
| Citric Acid Cycle | 2 | 6 | 2 | 2 |
| Oxidative Phosphorylation | 0 | -10 (consumed) | -2 (consumed) | ~28 |
| Total | 4 | - | - | ~32 |
Experimental Approaches for NADH Metabolism
Glycolysis Inhibition Studies
Research investigating the interplay between glycolysis and cellular redox state often employs specific glycolytic inhibitors to dissect metabolic contributions [25]. Common inhibitors include:
- 2-deoxyglucose (2-DG): A glucose analog that competitively inhibits hexokinase, the first enzyme in glycolysis [25].
- 3-bromopyruvate (3-BP): A potent alkylating agent that inhibits hexokinase and glyceraldehyde-3-phosphate dehydrogenase [25].
- Dichloroacetate (DCA): Inhibits pyruvate dehydrogenase kinase, thereby activating pyruvate dehydrogenase and promoting oxidative metabolism over glycolysis [25].
Experimental protocols typically involve treating cells (e.g., HepG2 hepatocellular carcinoma cells) with these inhibitors alone or in combination with chemotherapeutic agents like doxorubicin [25]. Treatment duration of 48 hours at physiologically relevant concentrations (e.g., 1μM doxorubicin, 2mM 2-DG, 10μM 3-BP, or 1mM DCA) allows assessment of metabolic and oxidative stress parameters [25].
Assessment of Oxidative Stress Markers
Methodologies for evaluating cellular response to metabolic perturbation include:
- Cytotoxicity analysis: MTT assay measuring mitochondrial reductase activity as an indicator of cell viability [25].
- Apoptosis and necrosis detection: Annexin V staining combined with ethidium homodimer III exclusion assessed via image cytometry [25].
- Oxidative stress markers: Measurement of lipid peroxidation products (malondialdehyde, 4-hydroxyalkenals), reduced glutathione (GSH) levels, and NADPH concentrations [25].
- Gene expression analysis: Quantitative real-time PCR (qRT-PCR) of genes involved in energy metabolism and antioxidant defense [25].
- Metabolite consumption assays: Measurement of glutamine uptake to assess alternative metabolic pathway activation [25].
NADH Fluorescence Lifetime Imaging (FLIM)
Advanced techniques such as Fluorescence Lifetime Imaging Microscopy (FLIM) enable non-invasive monitoring of NADH metabolic states in living cells [26]. This approach capitalizes on the inherent fluorescence of NADH and its sensitivity to enzyme binding, which alters fluorescence decay kinetics. Time-resolved fluorescence anisotropy imaging can distinguish between free and protein-bound NADH, providing insights into the redox state and metabolic flux in different cellular compartments [26].
Research Reagent Solutions
Table 3: Essential Research Reagents for NADH Metabolism Studies
| Reagent | Function/Application | Key Features |
|---|---|---|
| 2-Deoxyglucose (2-DG) | Competitive hexokinase inhibitor | Mimics glucose; traps glycolysis at first step [25] |
| 3-Bromopyruvate (3-BP) | Alkylating agent; inhibits HK and GAPDH | Potent glycolysis inhibitor; induces oxidative stress [25] |
| Dichloroacetate (DCA) | PDK inhibitor; promotes oxidative metabolism | Shifts metabolism from glycolysis to glucose oxidation [25] |
| NAD+ Precursors (NMN, NR) | Boost cellular NAD+ levels | Enhance sirtuin activity; improve mitochondrial function [18] |
| MTT Assay Kit | Cell viability assessment | Measures mitochondrial reductase activity [25] |
| Annexin V Apoptosis Assay | Apoptosis and necrosis detection | Distinguishes early/late apoptosis and necrosis [25] |
| Cytochrome c | Electron transport chain component | Mobile electron carrier between Complex III and IV [23] [24] |
| Coenzyme Q10 | Electron transport chain component | Lipid-soluble electron carrier between Complex I/II and III [23] [24] |
Pathway Visualizations
Therapeutic Implications and Research Perspectives
The central role of NADH in energy metabolism presents attractive targets for therapeutic intervention, particularly in cancer and metabolic disorders. Cancer cells frequently exhibit enhanced glycolytic flux (the Warburg effect) with subsequent lactate production, even under aerobic conditions [25]. This metabolic reprogramming creates dependencies that can be exploited therapeutically. Glycolysis inhibitors such as 2-DG, 3-BP, and DCA can selectively target cancer cells by disrupting their primary ATP and biomass production pathways [25]. Furthermore, these inhibitors can sensitize tumor cells to conventional chemotherapeutic agents like doxorubicin by impairing cellular antioxidant defenses through NADPH depletion [25].
Emerging research focuses on NAD+ precursor supplementation (e.g., nicotinamide mononucleotide [NMN] and nicotinamide riboside [NR]) to boost cellular NAD+ levels, potentially ameliorating age-related metabolic decline and mitochondrial dysfunction [18]. These approaches aim to enhance NAD+-dependent processes including sirtuin-mediated deacetylation and DNA repair by PARP enzymes, with implications for healthy aging and treatment of neurodegenerative diseases [18].
Future research directions include elucidating the complex regulation of NAD+ biosynthesis through de novo, Preiss-Handler, and salvage pathways [18], and developing more specific inhibitors targeting NADH-generating or consuming processes. Advanced imaging techniques like FLIM will continue to provide insights into compartmentalized NADH metabolism in living cells [26], enabling more precise manipulation of these fundamental metabolic pathways for therapeutic benefit.
NADPH in Anabolic Processes and Antioxidant Defense Systems
Nicotinamide adenine dinucleotide phosphate (NADPH) serves as an essential electron donor critical for cellular redox homeostasis, reductive biosynthesis, and antioxidant defense. This whitepaper examines the dual role of NADPH in fueling anabolic processes for cell proliferation and maintaining oxidative stress balance through reduced glutathione and thioredoxin systems. We explore the compartmentalized regulation of NADPH metabolism across cytosolic, mitochondrial, and other cellular environments, highlighting recent advances in measurement technologies and therapeutic targeting. Within the broader context of NADPH/NADH redox biology, understanding NADPH homeostasis provides crucial insights for drug development in cancer, neurodegenerative disorders, and age-related diseases where redox imbalance underpins pathological progression.
NADPH represents a critical redox cofactor that exists in a predominantly reduced state within cells, maintaining a favorable ratio for reductive biochemical reactions [27]. While NADH primarily fuels catabolic processes to generate ATP, NADPH serves as an indispensable electron donor for anabolic reactions and redox defense systems [15]. The structural distinction between these cofactors—an additional phosphate group on the 2' position of the adenosine ribose in NADP(H)—ensures functional separation, as enzymes specifically recognize either NAD(H) or NADP(H) [28] [15].
The regulation of NADPH homeostasis occurs through multiple compartmentalized pathways including the pentose phosphate pathway (PPP), folate metabolism, and NAD kinase activity [15]. Recent research has illuminated how distinct NADPH pools in cytosol and mitochondria independently support different cellular functions, with mitochondrial NADPH generated via NADK2 and several NADP+-reducing enzymes [27]. This compartmentalization allows NADPH to simultaneously support biosynthetic pathways while maintaining redox balance in different cellular locations.
The critical balance between NADPH production and consumption creates a vulnerability that can be therapeutically exploited, particularly in cancer cells that maintain high NADPH levels to support rapid growth and combat oxidative stress [15]. This whitepaper comprehensively examines NADPH's multifaceted roles, with specific quantitative data on its metabolic functions, experimental approaches for its study, and emerging therapeutic strategies targeting NADPH metabolism.
Biological Functions of NADPH
Antioxidant Defense Systems
NADPH serves as the primary reducing power for cellular antioxidant systems, maintaining redox homeostasis by regenerating reduced glutathione and thioredoxin [15].
- Glutathione System: NADPH is an essential cofactor for glutathione reductase, which converts oxidized glutathione (GSSG) back to its reduced form (GSH). Reduced glutathione then serves as a cosubstrate for glutathione peroxidase (GPX) to detoxify hydrogen peroxide (Hâ‚‚Oâ‚‚) and other peroxides into water or alcohol [15].
- Thioredoxin System: Thioredoxin reductase (TRXR) utilizes NADPH as an electron donor to maintain reduced thioredoxin (TRX), which contributes to Hâ‚‚Oâ‚‚ scavenging and provides reducing equivalents for ribonucleotide reductase (RNR) in DNA synthesis [15].
- Enzyme Reactivation: In some cell types, NADPH binds to and reactivates catalase when this Hâ‚‚Oâ‚‚-disposing enzyme becomes inactivated by its own substrate [15].
The critical role of NADPH in redox defense is particularly evident in cancer cells, which maintain high NADPH levels to prevent excessive oxidative stress while permitting ROS-mediated signaling that supports proliferation [15].
Anabolic Processes
NADPH provides essential reducing power for multiple biosynthetic pathways that support cell growth and proliferation:
Table 1: NADPH-Dependent Anabolic Processes
| Anabolic Process | Key NADPH-Dependent Enzymes | Primary Functions |
|---|---|---|
| Fatty Acid Synthesis | Fatty acid synthase (FASN) [28] | Synthesis of fatty acids using acetyl-CoA as primer and malonyl-CoA as two-carbon donor [15] |
| Mitochondrial Fatty Acid Synthesis | Mitochondrial fatty acid synthesis (mtFAS) enzymes [27] [29] | Generation of acyl chains for protein lipoylation; enables efficient mitochondrial translation and oxidative metabolism [27] [29] |
| Cholesterol Synthesis | HMG-CoA reductase (HMGCR) [15] | Rate-limiting enzyme of mevalonate pathway for cholesterol and nonsterol isoprenoid synthesis [15] |
| Nucleotide Synthesis | Dihydrofolate reductase (DHFR) [15] | Reduction of dihydrofolate to tetrahydrofolate (THF) for de novo biosynthesis of thymidylate and purines [15] |
| Amino Acid Synthesis | Pyrroline-5-carboxylate synthetase (P5CS) [27] | Conversion of glutamate to pyrroline-5-carboxylate for proline biosynthesis [27] |
| Drug/Xenobiotic Metabolism | Cytochrome P450 reductase (POR) [15] | Metabolism of drugs, xenobiotics, and steroid hormones [15] |
NADPH in Reactive Oxygen Species Generation
Beyond its antioxidant role, NADPH also serves as a substrate for NADPH oxidases (NOX), which catalyze the generation of superoxide anions or H₂O₂ from NADPH and oxygen [15]. These NOX-mediated ROS function as signaling molecules that regulate various redox-sensitive pathways involved in cancer progression, including those stimulating oncogenes such as Src and Ras [15]. This dual function positions NADPH at the center of redox balance—both preventing oxidative damage through antioxidant systems and facilitating ROS signaling when required for cellular processes.
NADPH Metabolic Pathways and Homeostasis
NADPH homeostasis is regulated by several metabolic pathways that exhibit cell-type and context-dependent contributions. The major NADPH-producing systems maintain compartmentalized NADPH pools to support distinct cellular functions.
Table 2: Major NADPH Producing Pathways and Enzymes
| Pathway/Enzyme | Subcellular Localization | Reaction Catalyzed | Relative Contribution |
|---|---|---|---|
| Pentose Phosphate Pathway (PPP) | Cytosol [15] | G6PD: Glucose-6-phosphate → 6-phosphogluconolactone + NADPH [15] | Primary cytosolic source; major contributor in most cells [15] |
| 6PGD: 6-phosphogluconate → Ribulose-5-phosphate + CO₂ + NADPH [15] | |||
| NAD Kinase (NADK) | Cytosol (NADK1) [15] | NAD⺠+ ATP → NADP⺠+ ADP [15] | De novo NADP⺠synthesis [15] |
| NAD Kinase (NADK2) | Mitochondria [27] [15] | NAD⺠+ ATP → NADP⺠+ ADP [27] [15] | Primary mitochondrial NADP⺠source [27] |
| Malic Enzyme (ME1) | Cytosol [15] | Malate + NADP⺠→ Pyruvate + CO₂ + NADPH [15] | Varies by cell type and metabolic state [15] |
| Malic Enzyme (ME2) | Mitochondria [27] | Malate + NADP⺠→ Pyruvate + CO₂ + NADPH [27] | Mitochondrial NADPH generation [27] |
| Isocitrate Dehydrogenase (IDH1) | Cytosol [15] | Isocitrate + NADP⺠→ α-ketoglutarate + CO₂ + NADPH [15] | Secondary cytosolic source [15] |
| Isocitrate Dehydrogenase (IDH2) | Mitochondria [27] | Isocitrate + NADP⺠→ α-ketoglutarate + CO₂ + NADPH [27] | Mitochondrial NADPH generation [27] |
| Folatemetabolism (MTHFD1) | Cytosol/Mitochondria [30] | Methylenetetrahydrofolate + NADP⺠→ Methenyltetrahydrofolate + NADPH [30] | Secondary source; important in endothelial cells [30] |
The diagram below illustrates the compartmentalization of NADPH metabolism and the key pathways involved in its production and consumption:
Quantitative studies of NADPH concentrations reveal significant compartmental differences. In HeLa cells, NADPH concentration is approximately 3.1 ± 0.3 µM in the cytosol and 37 ± 2 µM in the mitochondrial matrix [15]. The redox potentials of both mitochondrial and cytosolic NADP(H) systems are similar at approximately -400 mV in the liver [15]. These quantitative differences highlight the specialized roles of each compartment, with mitochondria maintaining substantially higher NADPH levels to support its diverse oxidative metabolic functions.
Quantitative NADPH Data in Physiological Contexts
Understanding NADPH concentrations and flux in different physiological and pathological states provides critical insights for therapeutic targeting.
Table 3: Quantitative NADPH Data Across Biological Contexts
| Biological Context | NADPH Level/Parameter | Measurement Method | Functional Significance |
|---|---|---|---|
| HeLa Cells | Cytosol: 3.1 ± 0.3 µM [15] | Genetically encoded sensors [15] | Baseline compartmental distribution |
| Mitochondria: 37 ± 2 µM [15] | Genetically encoded sensors [15] | Higher mitochondrial capacity | |
| Rat Liver | Total NADP(H): 420 nmol/g wet weight [15] | Enzymatic cycling assays [15] | Tissue-level quantification |
| Mitochondrial: 59% of total [15] | Subcellular fractionation [15] | Major mitochondrial pool | |
| Senescent Endothelial Cells | Cytosolic NADPH significantly elevated [30] | iNap1 sensor [30] | Adaptive response to oxidative stress |
| Mitochondrial NADPH unchanged [30] | iNap3 sensor [30] | Compartment-specific regulation | |
| Cancer Cells | High NADPH maintained [15] | Multiple methods [15] | Supports biosynthesis and redox defense |
| L-threonine Production | NADPH limitation impacts yield (0.65 g/g) [31] | Metabolic engineering [31] | Industrial application dependency |
The regulation of NADPH production pathways shows remarkable plasticity across different cellular states. In senescent endothelial cells, cytosolic NADPH increases through G6PD upregulation, while mitochondrial NADPH remains stable [30]. This compartment-specific regulation highlights how cells can fine-tune NADPH distribution to address distinct metabolic needs in different subcellular locations.
Experimental Approaches for NADPH Research
Genetically Encoded NADPH Sensors
Recent advances in genetically encoded biosensors have revolutionized the study of NADPH dynamics in live cells:
iNap Sensors: The iNap1 sensor enables real-time monitoring of NADPH levels in specific cellular compartments. The experimental workflow involves:
- Transfection of cyto-iNap1 or mito-iNap3 constructs into target cells
- Confocal imaging with excitation at 405/420 nm and 488/485 nm
- Ratio metric analysis (405/488 or 420/485) to determine NADPH concentration
- In situ calibration using digitonin (0.001% for plasma membrane, 0.3% for mitochondrial membrane) permeabilization followed by NADPH titration [30]
Validation: Specificity is confirmed using oxidants like diamide (100 µM) that decrease cyto-iNap1 fluorescence but not mito-iNap3 signals, demonstrating stronger antioxidant capacity in mitochondria [30]. The non-responsive variant iNapc serves as a control for environmental effects [30].
Direct Measurement of Mitochondrial Fatty Acid Synthesis
A novel biochemical method developed by Kim et al. enables direct quantification of mitochondrial fatty acid synthesis (mtFAS) activity:
- Acyl Group Analysis: Modification of a method used in Camelina sativa to directly assess acyl modifications on mammalian NDUFAB1 using mass spectrometry [27] [29]
- Sample Preparation: Isolation of mitochondrial fractions and cleavage of acyl chains from target proteins (DLAT, DLST, or NDUFAB1) [27]
- Mass Spectrometry: Relative quantification of various acyl chains attached to NDUFAB1 provides direct readout of mtFAS pathway activity [27]
- Application: Demonstration that NADK2-derived mitochondrial NADPH is required for acyl chain synthesis by mtFAS [27]
Metabolic Engineering Approaches
The Redox Imbalance Forces Drive (RIFD) strategy represents an innovative approach to manipulate NADPH metabolism:
- NADPH Pool Expansion: "Open source" strategies including:
- Expression of cofactor-converting enzymes
- Heterologous cofactor-dependent enzymes
- Enzymes in NADPH synthesis pathways [31]
- Consumption Reduction: Knocking out non-essential NADPH-consuming genes [31]
- Directed Evolution: Using MAGE to evolve redox-imbalanced engineered strains [31]
- Biosensor Integration: NADPH and product dual-sensing biosensors combined with FACS for high-throughput screening [31]
The Scientist's Toolkit: Key Research Reagents
Table 4: Essential Research Reagents for NADPH Studies
| Reagent/Tool | Type | Primary Function | Example Applications |
|---|---|---|---|
| iNap1/iNap3 | Genetically encoded sensor | Real-time NADPH monitoring in cytosol/mitochondria [30] | Live-cell imaging of NADPH dynamics during senescence [30] |
| SoNar | Genetically encoded sensor | Monitoring NADH/NAD+ ratios [30] | Parallel assessment of NAD and NADPH redox states [30] |
| Digitonin | Chemical reagent | Selective membrane permeabilization [30] | Sensor calibration in specific compartments [30] |
| NADK2 knockout models | Genetic model | Study mitochondrial NADPH functions [27] | Elucidating mtFAS and proline synthesis requirements [27] |
| MTHFD1 inhibitors | Small molecule compounds | Block folate-mediated NADPH production [30] | Investigating endothelial cell senescence [30] |
| G6PD modulators | Chemical compounds | Regulate PPP flux and NADPH production [32] [15] | Studying antioxidant capacity in neuronal systems [32] |
| Folic Acid | FDA-approved drug | Enhances NADPH production via MTHFD1 [30] | Testing therapeutic intervention in vascular aging [30] |
| Sos1-IN-16 | Sos1-IN-16, MF:C30H31F3N4O3, MW:552.6 g/mol | Chemical Reagent | Bench Chemicals |
| Elironrasib | Elironrasib, CAS:2641998-63-0, MF:C55H78FN9O8, MW:1012.3 g/mol | Chemical Reagent | Bench Chemicals |
The experimental workflow for studying compartmentalized NADPH metabolism integrates these tools as shown below:
Therapeutic Implications and Research Directions
Targeting NADPH metabolism represents a promising strategy for various diseases:
- Cancer Therapy: Cancer cells maintain high NADPH levels to support rapid growth and combat oxidative stress, creating a therapeutic vulnerability [15]. Strategies include inhibiting NADPH production pathways (PPP, NADK) or increasing NADPH consumption through pro-oxidant therapies [15].
- Neurodegenerative Disorders: In Parkinson's disease, RAS components regulate G6PD expression and NADPH availability in dopaminergic neurons, suggesting angiotensin receptor modulation as a potential therapeutic approach [32].
- Vascular Aging: Folic acid, identified through high-throughput screening of FDA-approved drugs, increases NADPH via MTHFD1 and ameliorates vascular aging in mouse models [30].
- Metabolic Engineering: The RIFD strategy demonstrates that creating redox imbalance forces can drive production of valuable compounds like L-threonine (117.65 g/L yield) [31].
Future research directions should focus on developing more specific compartment-targeted NADPH modulators, understanding tissue-specific NADPH regulation, and exploring combination therapies that simultaneously target multiple NADPH homeostasis mechanisms.
Advanced Tools and Techniques for Monitoring NAD(H) and NADP(H) Dynamics
Genetically Encoded Biosensors (e.g., iNap, SoNar) for Compartment-Specific Real-Time Imaging
Cellular metabolism relies on the intricate balance of nicotinamide adenine dinucleotide cofactors, with NADH serving as a central carrier of reducing equivalents in catabolic processes and NADPH providing reducing power for anabolic reactions and antioxidant defense [1]. The NAD+/NADH and NADP+/NADPH redox couples constitute essential metabolic redox buffers that regulate cellular energy metabolism, redox homeostasis, and signaling pathways [1]. Disruption of these redox systems has been implicated in numerous pathological conditions, including cancer, neurodegenerative diseases, and aging [1]. Historically, methods for measuring these metabolites relied on destructive techniques such as chromatography, mass spectrometry, and enzymatic cycling assays, which provided only static snapshots and failed to preserve spatial and temporal information [33] [34].
The development of genetically encoded fluorescent biosensors has revolutionized our ability to monitor metabolic dynamics in live cells with subcellular resolution [35]. These molecular tools combine ligand-binding domains with fluorescent proteins, enabling real-time tracking of metabolite fluctuations, enzymatic activities, and signaling events in their native cellular context [35]. This technical guide focuses on the emerging class of biosensors designed specifically for monitoring NADPH and NADH redox states, with particular emphasis on compartment-specific imaging applications that are illuminating the spatial organization of redox metabolism in health and disease.
Biosensor Engineering and Design Principles
Molecular Architecture of Redox Biosensors
Genetically encoded biosensors for NADPH and NADH typically employ a modular design consisting of a sensing domain and a reporting domain [35] [7]. The sensing domain is derived from natural bacterial transcriptional regulators or metabolic enzymes that specifically bind NADPH or NADH, while the reporting domain consists of fluorescent proteins whose spectral properties change upon ligand binding.
The Rex protein from Thermus aquaticus (T-Rex) has served as a particularly versatile sensing domain for both NADH and NADPH biosensors [33] [7]. In its native form, T-Rex preferentially binds NADH, but strategic mutagenesis of key residues in the binding pocket can switch its specificity toward NADPH [33]. Structural analyses reveal that NADP(H)-binding proteins typically contain positively charged residues that interact electrostatically with the 2'-phosphate group of NADP(H), while NAD(H)-binding proteins feature negatively charged residues in equivalent positions [33].
For the reporting domain, circularly permuted fluorescent proteins (cpFPs) have proven particularly valuable because their fluorescence properties are highly sensitive to conformational changes in the sensing domain [33] [7]. Commonly used cpFPs include cpYFP (circularly permuted yellow fluorescent protein) in sensors like iNap and SoNar, and cpT-Sapphire in the newer NAPstar sensors [33] [7]. The circular permutation rearranges the FP structure such that the original N- and C-termini are connected by a short linker while new termini are created at another location in the barrel structure, making the chromophore more accessible to environmental changes.
Key Design Strategies and Optimization
Several strategic approaches have been employed to optimize the performance of redox biosensors:
Affinity tuning: By introducing specific mutations in the ligand-binding pocket, researchers have created biosensor variants with a range of dissociation constants (Kd), enabling measurements across different concentration ranges [33]. For example, the iNap family includes variants with apparent Kd values for NADPH ranging from ~1.3 µM to ~29 µM [33].
Ratiometric design: Most modern redox biosensors incorporate ratiometric measurement capabilities, either through dual-excitation or through fusion with a reference fluorescent protein of different color [33] [7]. This design minimizes artifacts caused by variations in sensor expression level, photobleaching, or cell thickness.
pH resistance: Since intracellular pH fluctuations can affect fluorescence, leading biosensors have been engineered for reduced pH sensitivity [33]. The iNap sensors, for instance, exhibit minimal fluorescence changes in response to pH variations within the physiological range [33].
Subcellular targeting: Addition of localization sequences (e.g., mitochondrial targeting sequence, nuclear localization signal) enables compartment-specific measurements [33] [36]. This has revealed striking differences in NADPH concentrations between cellular compartments, with mitochondrial matrix levels (~37 μM) significantly exceeding cytosolic levels (~3 μM) [33].
Leading NAD(P)H Biosensors and Their Characteristics
The iNap Sensor Family for NADPH Detection
The iNap (indicator for NADPH) sensors represent a breakthrough in specific NADPH monitoring [33]. Developed through structure-guided engineering of the SoNar sensor, iNap sensors feature a chimeric design combining cpYFP with the NAD(H)-binding domain of T-Rex that has been mutated to favor NADPH binding [33].
Key characteristics of iNap sensors:
- High selectivity: iNap sensors show strong responsiveness to NADPH but minimal reaction to NADH, NAD+, or NADP+ [33]
- Wide dynamic range: iNap1 exhibits an ~900% ratiometric fluorescence change upon NADPH binding [33]
- pH resistance: Fluorescence excited at 420 nm is largely pH-insensitive, and pH effects on 485 nm excitation can be corrected using control sensors [33]
- Rapid response kinetics: The sensors respond quickly to NADPH changes, enabling real-time monitoring of metabolic fluctuations [33]
The iNap platform includes multiple variants with different affinities, allowing researchers to select the optimal sensor for their specific experimental context and expected NADPH concentrations [33].
SoNar for NADH/NAD+ Redox State
SoNar is a highly responsive sensor for the NADH/NAD+ ratio, developed before the iNap series [33]. Also derived from cpYFP and T-Rex, SoNar exhibits dramatic conformational changes and fluorescence enhancement upon NADH binding, with a 30-fold increase in fluorescence ratio between fully oxidized and reduced states [33]. Its exceptional sensitivity has enabled detection of subtle metabolic changes in living cells and in vivo, but its responsiveness to both NADH and NADPH initially complicated interpretation until the development of more specific sensors.
NAPstars: Next-Generation NADP Redox State Sensors
The recently developed NAPstar family represents a significant advancement in NADP redox state monitoring [7]. These sensors are based on Peredox-mCherry but incorporate mutations that alter binding specificity from NADH to NADPH [7].
Innovative features of NAPstar sensors:
- Genuine redox state reporting: NAPstars respond to both NADPH and NADP+, enabling measurement of the actual NADPH/NADP+ ratio rather than just NADPH concentration [7]
- Broad dynamic range: NAPstars can monitor NADPH/NADP+ ratios across a 5000-fold range (approximately 0.001 to 5) [7]
- Dual readout compatibility: The sensors can be used with both ratiometric fluorescence and fluorescence lifetime imaging (FLIM) [7]
- Enhanced brightness: The T-Sapphire-based design offers higher apparent brightness in biological systems compared to cpYFP-based sensors [7]
Table 1: Comparison of Genetically Encoded Biosensors for NAD(P)H Monitoring
| Sensor Name | Primary Target | Dynamic Range | Affinity (Kd) | Key Features | Applications |
|---|---|---|---|---|---|
| iNap1 | NADPH | ~900% ratio change | ~2.0 μM | pH-resistant, highly specific to NADPH | Cytosolic and mitochondrial NADPH pools [33] |
| iNap3 | NADPH | Similar to iNap1 | ~25 μM | Lower affinity variant | Mitochondrial NADPH measurement [33] |
| SoNar | NADH/NAD+ ratio | 30-fold fluorescence increase | ~1.2 μM (NADH) | Extreme sensitivity | Live cell and in vivo NADH dynamics [33] |
| NAPstar1 | NADPH/NADP+ ratio | 5000-fold ratio range | Kr: ~0.006 | Reports genuine redox state | Real-time subcellular NADP redox dynamics [7] |
| NAPstar3 | NADPH/NADP+ ratio | 5000-fold ratio range | Kr: ~0.03 | Intermediate affinity | Cell cycle-linked oscillations [7] |
| Peredox | NADH/NAD+ ratio | ~2.5-fold ratio change | ~1.2 μM (NADH) | Ratiometric with mCherry | NADH monitoring in cytosol and mitochondria [7] |
Experimental Workflows and Methodologies
Sensor Expression and Subcellular Targeting
Implementing genetically encoded biosensors requires careful consideration of expression strategies and verification of subcellular localization:
Expression Systems:
- Plasmid Transfection: Standard approach for many cell lines; suitable for transient expression [34]
- Lentiviral Transduction: Essential for difficult-to-transfect cells (e.g., HL60 leukemic cells) and stable cell line generation [36]
- Adeno-Associated Virus (AAV): Useful for in vivo applications and primary cells [34]
Subcellular Targeting:
- Cytosol: Usually default localization; can be enhanced with nuclear export signals [33]
- Mitochondria: Achieved by N-terminal fusion with mitochondrial targeting sequence (e.g., cytochrome c oxidase subunit VIII) [33] [36]
- Nucleus: Incorporated nuclear localization signals (NLS) [36]
- Endoplasmic Reticulum: Added ER localization sequences [36]
Table 2: Essential Research Reagent Solutions for Biosensor Applications
| Reagent/Category | Specific Examples | Function/Application | Experimental Notes |
|---|---|---|---|
| Expression Vectors | pLVX, lentiviral packaging systems (pLPI, pLPII, pLPVSVG) | Sensor delivery and stable cell line generation | Critical for hard-to-transfect cells like AML lines [36] |
| Selection Agents | Puromycin, G418 | Selection of stably expressing cells | Typical concentration: 3 μg/mL puromycin [36] |
| Transfection Reagents | Lipofectamine 2000/3000 | Plasmid delivery | Optimize for specific cell type [36] |
| Localization Sequences | MLS, NLS, ELS | Subcellular targeting | Verify localization with microscopy [33] [36] |
| Metabolic Modulators | 2-deoxy-glucose, oxamate, LPS/IFN-γ | Perturbation of NAD(P)H metabolism | Establish dose-response relationships [33] |
| Microscopy Systems | Confocal (e.g., Zeiss LSM 980), plate readers | Fluorescence measurement | Airyscan improves resolution; environmental control crucial [36] |
Imaging and Data Acquisition Protocols
Live-Cell Imaging Conditions:
- Maintain temperature at 37°C using environmental chambers [36]
- Control COâ‚‚ at 5% for bicarbonate-buffered systems [34]
- Minimize light exposure to prevent phototoxicity and photobleaching
- Acquire images at appropriate intervals (e.g., every 5 minutes for metabolic studies) [36]
Ratiometric Measurements:
- For dual-excitation sensors (e.g., iNap, NAPstars): Alternate between 420/485 nm (iNap) or 400/490 nm (NAPstars) excitation while collecting emission at 515-530 nm [33] [7]
- For FRET-based sensors: Excite donor and collect donor and acceptor emission
- Include control sensors (e.g., iNapc) to account for pH variations or expression differences [33]
Data Analysis:
- Calculate ratio values (R) for each time point: R = Fâ‚/Fâ‚‚ where Fâ‚ and Fâ‚‚ are fluorescence intensities at the two excitation/emission wavelengths
- Normalize ratios to initial baseline (R/Râ‚€) for time-course experiments
- Convert ratio values to metabolite concentrations using in vitro calibration curves when possible [33]
Experimental Workflow for Biosensor Applications
Calibration and Validation Approaches
In Vitro Calibration:
- Purify recombinant sensor protein [7]
- Measure fluorescence spectra in defined buffers with known NADPH/NADP+ ratios [33] [7]
- Determine apparent Kd values and dynamic range [33]
In Situ Validation:
- Use pharmacological agents to perturb specific pathways (e.g., G6PD inhibition for pentose phosphate pathway) [33]
- Compare with alternative methods (enzymatic cycling assays, HPLC) when feasible [33]
- Express control sensors (e.g., iNapc) to identify artifacts [33]
Applications in Redox Biology Research
Compartment-Specific NADPH Dynamics
The implementation of targeted biosensors has revealed striking compartmentalization of NADPH metabolism:
Cytosolic vs. Mitochondrial NADPH Pools:
- Free NADPH concentration is approximately 10-fold higher in mitochondria (~37 μM) compared to cytosol (~3 μM) in HeLa cells [33]
- Both pools are regulated by cytosolic NAD+ kinase (NADK), highlighting intercompartmental coordination [33]
- Mitochondrial NADPH shows greater stability under oxidative stress compared to cytosolic NADPH [33]
Nuclear NADPH:
- NADPH readily exchanges between cytosol and nucleus, suggesting a shared pool [33]
- Nuclear NADPH may support epigenetic regulation and DNA repair processes
Metabolic Pathway Analysis
Biosensors have enabled real-time dissection of NADPH production and consumption pathways:
Pentose Phosphate Pathway (PPP):
- Knockdown of glucose-6-phosphate dehydrogenase (G6PD), the rate-limiting enzyme of PPP, slightly decreases cytosolic NADPH levels [33]
- 6-phosphogluconate dehydrogenase (PGD) knockdown shows minimal effect, suggesting G6PD as the primary regulatory point [33]
NADPH Oxidase Signaling:
- NADPH oxidases (Nox family) consume NADPH to generate reactive oxygen species for signaling [37]
- iNap sensors have detected NADPH decreases during macrophage activation by LPS/IFN-γ [33]
Oxidative Stress Response:
- NAPstar sensors revealed the glutathione system as the primary mediator of antioxidative electron flux during acute oxidative challenge across eukaryotes [7]
- Cells maintain remarkable NADPH homeostasis under stress, indicating robust redox buffering capacity [33] [7]
Disease Modeling and Drug Discovery
Cancer Metabolism:
- iNap sensors have been deployed in ovarian cancer models to study metabolic adaptations to chemotherapy [34]
- Carboplatin-resistant patient-derived organoids show distinct NADPH dynamics compared to sensitive counterparts [34]
Liver Fibrosis:
- NADPH oxidases (particularly Nox2 and Nox4) contribute to hepatic stellate cell activation and liver fibrogenesis [38]
- Redox biosensors could enable screening of antifibrotic therapies targeting NADPH metabolism
Leukemia Research:
- Compartment-specific GSH/GSSG measurements in AML cells reveal heterogeneous redox responses to chemotherapeutics [36]
- Drugs like cytarabine and doxorubicin differentially affect subcellular redox states [36]
NADPH Metabolic Pathways in Redox Biology
Technical Considerations and Limitations
Potential Artifacts and Control Experiments
pH Sensitivity:
- Although modern sensors are pH-resistant, significant intracellular pH changes can still affect readings [33]
- Solution: Use pH-insensitive excitation wavelengths (e.g., 420 nm for iNap) and include control sensors [33]
Sensor Overexpression Effects:
- High expression levels may buffer metabolite concentrations or cause cellular stress
- Solution: Titrate expression levels, use minimal promoter systems, and compare with alternative measurement methods
Cross-Reactivity:
- Early NADPH sensors showed some responsiveness to NADH [33]
- Solution: Use newly developed sensors with improved specificity (e.g., NAPstars) and validate with pharmacological perturbations [7]
Methodological Limitations
Absolute Quantification:
- In vivo calibration remains challenging due to uncertain sensor occupancy and compartment-specific environments
- Approaches: Use multiple sensors with different affinities, perform in situ calibration with permeabilized cells
Spatiotemporal Resolution:
- Diffusion kinetics may limit detection of very rapid or localized changes
- Advances: Newer sensors with faster kinetics and targeted to microdomains are addressing this limitation
Phototoxicity and Photobleaching:
- Extended time-lapse imaging can affect cell viability and sensor performance
- Mitigation: Optimize imaging intervals, use minimal illumination, and employ sensitive detectors
Future Directions and Emerging Applications
The field of genetically encoded biosensors continues to evolve rapidly, with several promising developments on the horizon:
Multiplexed Imaging:
- Combination of multiple sensors with distinct spectral properties will enable simultaneous monitoring of NADPH, NADH, ATP, and other metabolites
- Red-shifted sensors will facilitate deeper tissue imaging and reduced autofluorescence
Advanced Imaging Modalities:
- Fluorescence lifetime imaging (FLIM) compatibility, as demonstrated with NAPstars, provides an additional readout parameter independent of sensor concentration [7]
- Super-resolution techniques will enable mapping of metabolic microdomains below the diffraction limit
In Vivo and Clinical Applications:
- Biosensor-expressing organoids serve as sophisticated disease models for drug screening [34]
- AAV-delivered sensors may enable metabolic imaging in intact tissues and animal models
- Potential for human application in endoscopic detection or intraoperative guidance
Integration with Other Technologies:
- Combination with CRISPR/Cas9 for simultaneous metabolic monitoring and genetic manipulation
- Correlation with transcriptomics and proteomics for multi-omics approaches to cellular metabolism
As these tools become more sophisticated and accessible, they will continue to transform our understanding of redox biology and provide new insights into the metabolic basis of health and disease.
Leveraging Biosensors for High-Throughput Drug Screening (e.g., FDA-Approved Library Screening)
The integration of advanced biosensing technologies with high-throughput screening (HTS) platforms has revolutionized the landscape of modern drug discovery, particularly in the critical evaluation of FDA-approved drug libraries for repurposing opportunities. This paradigm shift enables researchers to rapidly identify novel therapeutic applications for existing compounds, significantly reducing the time and cost associated with traditional drug development. Central to this technological advancement is the growing appreciation of redox biology, specifically the pivotal roles of NADPH and NADH as essential metabolic coenzymes that maintain cellular redox homeostasis [39]. These pyridine nucleotides serve not only as fundamental mediators of electron transfer in countless biochemical reactions but also as critical indicators of cellular metabolic state and stress, making them highly valuable targets for biosensing in drug screening campaigns.
The coexistence of NADH and NADPH systems in mammalian cells, though functionally distinct, provides a comprehensive window into cellular metabolic health. NADH primarily fuels catabolic pathways, driving energy production through processes like oxidative phosphorylation, while NADPH predominantly powers anabolic reactions and antioxidative defense systems, protecting cells from oxidative damage [39]. This functional division offers researchers dual parameters for assessing drug effects on cancer cell viability, metabolic reprogramming, and treatment-induced oxidative stress. Modern biosensors capable of monitoring these redox couples with subcellular resolution are now uncovering the complex metabolic alterations that occur in response to pharmacological intervention, providing unprecedented insights into drug mechanisms of action within physiologically relevant model systems.
Core Concepts: Biosensor Technologies for HTS
Fundamental Principles and Typologies of Biosensors in Drug Screening
Biosensors for high-throughput drug screening incorporate diverse transduction mechanisms, each with distinct advantages for specific screening applications. Electrochemical biosensors measure electrical signals (current, potential, or impedance) resulting from biochemical interactions, offering high sensitivity, miniaturization capability, and compatibility with complex biological fluids [40]. Optical biosensors, including those based on surface-enhanced Raman scattering (SERS), fluorescence, and surface plasmon resonance (SPR), detect changes in light properties upon analyte binding, enabling highly multiplexed and non-invasive monitoring of cellular responses [40] [41]. Microwave resonator biosensors represent an emerging category that detects dielectric permittivity variations induced by changes in live cell concentrations, enabling label-free, non-optical quantification of cellular responses to therapeutic compounds [42].
The recent integration of artificial intelligence (AI), particularly machine learning and deep learning algorithms, with optical biosensors has created a transformative paradigm for HTS data analysis. AI-enhanced biosensors demonstrate superior capabilities in intelligent signal processing, pattern recognition, and automated decision-making, significantly improving analytical sensitivity and specificity while reducing false-positive rates in drug screening [41]. Furthermore, the coupling of biosensors with complementary metal-oxide-semiconductor (CMOS) technology has enabled massive scalability and miniaturization, facilitating the development of high-density sensor arrays necessary for large-scale compound library screening [42].
NAD(P)H Biosensing: Technical Specificities and Physiological Significance
Genetically encoded biosensors for NADPH and NADH have revolutionized our ability to monitor redox metabolism with subcellular precision in living cells. The iNap sensor, specifically engineered for NADPH detection, exhibits high specificity and responsiveness to physiological NADPH concentrations, enabling real-time monitoring of oxidative pentose phosphate pathway activity and antioxidative capacity [30]. Concurrently, the SoNar indicator provides accurate measurements of NADH/NAD+ ratios, reflecting the metabolic flux through glycolytic and mitochondrial pathways [30]. The compartmentalized expression of these sensors—targeted to either cytosol or mitochondria—has revealed critical insights into the independent regulation of NADPH and NADH metabolism in different subcellular locations during drug treatments [30].
The physiological significance of monitoring these redox couples in drug screening extends beyond mere metabolic mapping. NADPH levels directly influence cellular sensitivity to oxidative stress-inducing chemotherapeutics, while NADH availability dictates energy production capacity and can signal metabolic vulnerabilities in cancer cells [39]. The ratio of NAD+/NADH reflects the overall redox state of the cell, whereas NADPH predominantly maintains redox defense systems. Understanding these nuanced relationships through advanced biosensing provides critical insights into drug mechanisms, potential resistance pathways, and synergistic therapeutic opportunities, particularly when screening FDA-approved libraries for repurposing in oncology and age-related diseases.
Experimental Workflows and Protocols
Integrated HTS Workflow Using Biosensors
The following diagram illustrates a comprehensive high-throughput screening workflow that integrates multiple biosensing technologies for drug repurposing, from initial compound screening to in vivo validation:
This workflow demonstrates the sequential integration of biosensor technologies, beginning with large compound libraries and progressively applying more physiologically relevant models to validate identified hits. The process leverages multiple biosensing modalities to triage compounds efficiently before committing resources to advanced validation stages.
Detailed Experimental Protocol: Fluorescence Lifetime-Based FRET Screening
The following protocol outlines the specific methodology for conducting fluorescence lifetime-based FRET screening of FDA-approved compound libraries, as applied to TDP-43 proteinopathy research [43]:
1. Biosensor Cell Line Preparation
- Culture HEK293T or other relevant cell lines in appropriate medium supplemented with 10% FBS and 1% penicillin-streptomycin at 37°C in a 5% CO₂ atmosphere.
- Transfect cells with FRET biosensor constructs (e.g., full-length TDP-43 FLT-FRET biosensor) using lipofectamine 3000 according to manufacturer's protocol.
- Select stable transformants using appropriate antibiotics (e.g., 2 μg/mL puromycin) for 2-3 weeks, with medium changes every 3-4 days.
- Validate biosensor expression and functionality via fluorescence microscopy and Western blotting before screening.
2. Library Compound Handling and Dispensing
- Obtain FDA-approved drug library (e.g., 2,682-compound Selleck library) as 10 mM stock solutions in DMSO.
- Using an acoustic droplet ejector (e.g., Echo 550), transfer compounds to 384-well assay plates at desired final concentrations (typically 1-10 μM).
- Include controls on each plate: negative control (DMSO vehicle only), positive control for biosensor response.
3. Fluorescence Lifetime Imaging and Analysis
- Plate biosensor-expressing cells in black-walled, clear-bottom 384-well plates at density of 5,000-10,000 cells/well.
- Incubate plates for 24 hours at 37°C, 5% CO₂ to allow cell attachment.
- Add pre-dispensed compounds using liquid handler, incubate for desired treatment period (typically 24-48 hours).
- Acquire fluorescence lifetime images using time-correlated single photon counting (TCSPC) confocal microscope with 405 nm excitation laser.
- Collect emission signals at 475 nm (cyan fluorescent protein) and 527 nm (yellow fluorescent protein) channels.
- Calculate fluorescence lifetime (Ï„) and FRET efficiency using equation: E = 1 - (Ï„DA/Ï„D), where Ï„DA is donor lifetime in presence of acceptor, Ï„D is donor lifetime alone.
4. Hit Identification and Validation
- Identify primary hits as compounds producing statistically significant changes in FRET efficiency compared to DMSO controls (typically >3 standard deviations from mean).
- Confirm hits in dose-response experiments (8-point 1:3 serial dilutions) to determine ECâ‚…â‚€/ICâ‚…â‚€ values.
- Employ counter-screens (e.g., NTD-deletion constructs) to confirm target specificity [43].
Detailed Experimental Protocol: NADPH Biosensor-Based Screening in Vascular Aging
This protocol details the methodology for screening FDA-approved compounds using NADPH biosensors to identify compounds that ameliorate vascular aging [30]:
1. NADPH Biosensor Expression in Primary Cells
- Culture primary human aortic endothelial cells (HAECs) in endothelial growth medium-2 at 37°C, 5% CO₂.
- Transduce HAECs with lentiviral vectors encoding compartment-specific NADPH biosensors (cyto-iNap1 or mito-iNap3) at MOI of 10-20.
- Select transduced cells with appropriate antibiotics (e.g., 2 μg/mL puromycin) for 1 week.
- Validate sensor localization and function via confocal microscopy and in situ calibration with digitonin-permeabilized cells exposed to NADPH standards.
2. Induction of Cellular Senescence and Compound Screening
- Induce senescence in HAECs by treatment with angiotensin II (2 μM for 72 hours), high glucose (25 mM for 48 hours), or through replicative exhaustion (passage >12).
- Confirm senescence phenotype by β-galactosidase staining and p16/p21 immunoblotting.
- Plate senescent HAECs in 384-well plates at 8,000 cells/well, incubate for 24 hours.
- Using liquid handler, transfer 1,419 FDA-approved compounds from library stocks to assay plates (final concentration 10 μM).
- Incubate compounds with cells for 48 hours at 37°C, 5% CO₂.
3. NADPH Imaging and Quantification
- Acquire fluorescence ratio images (420/485 nm excitation) using high-content imaging system or confocal microscope.
- Calculate NADPH levels from calibration curves generated with known NADPH concentrations.
- Identify hit compounds that significantly modulate cytosolic NADPH levels toward more youthful phenotype.
- Validate hits through secondary assays measuring ROS production, G6PD activity, and HDAC3 inhibition.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 1: Essential Research Reagents and Materials for Biosensor-Based HTS
| Reagent/Material | Specifications | Primary Function | Example Application |
|---|---|---|---|
| FDA-Approved Drug Libraries | Prestwick Chemical Library (1,267 compounds); Selleck FDA-approved Library (2,682 compounds) | Source of clinically evaluated compounds for repurposing screening | Initial HTS campaigns to identify bioactive compounds [43] [44] [45] |
| Genetically Encoded Biosensors | iNap1 (NADPH sensor); SoNar (NADH/NAD+ sensor); FLT-FRET biosensors | Real-time monitoring of metabolic and molecular events in living cells | Tracking NADPH dynamics in senescent cells; monitoring protein-protein interactions [43] [30] |
| 3D Cell Culture Systems | Ultra-low attachment (ULA) plates; hydrogels; extracellular matrix components | Physiologically relevant models for drug evaluation | 3D spheroid models of NRAS-mutated melanoma; vascular aging models [30] [45] |
| High-Throughput Screening Platforms | Automated liquid handlers; acoustic droplet ejectors; high-content imaging systems | Automated compound dispensing and assay readout | Screening 1,300+ compounds in 3D melanoma spheroids [45] |
| Specialized Cell Lines | Primary human cells; genetically engineered biosensor cell lines; patient-derived cell lines | Biologically relevant screening models | HAECs for vascular aging studies; NRAS-mutated melanoma cell lines [30] [45] |
| CCG-203971 | CCG-203971, CAS:1443437-74-8, MF:C23H21ClN2O3, MW:408.9 g/mol | Chemical Reagent | Bench Chemicals |
| WB436B | WB436B, MF:C21H20N6O3S, MW:436.5 g/mol | Chemical Reagent | Bench Chemicals |
Signaling Pathways and Molecular Mechanisms
NADPH-Mediated Signaling in Vascular Aging and Drug Response
The following diagram illustrates the key molecular pathways involving NADPH metabolism in vascular aging and the points of intervention for screening-identified compounds:
This pathway illustrates how screening-identified compounds like folic acid can modulate NADPH metabolism through multiple enzymatic pathways to ameliorate age-related vascular dysfunction. The G6PD-mediated oxidative pentose phosphate pathway represents the primary NADPH generation route, while folic acid activates an alternative pathway through MTHFD1 to boost NADPH production and counteract senescence [30].
Programmed Cell Death Pathways Activated by Screening Hits
The diagram below outlines the multiple programmed cell death pathways induced by hit compounds identified through HTS, using menadione as an example:
This multi-modal cell death induction represents a powerful therapeutic strategy identified through HTS with biosensor readouts. Menadione, discovered through screening an FDA-approved library, activates MAPK8 signaling which subsequently triggers three distinct programmed cell death pathways simultaneously, overcoming the limitations of single-pathway targeting and potentially reducing the likelihood of resistance development [44].
Quantitative Data Analysis and Interpretation
Performance Metrics of Biosensor Technologies in HTS
Table 2: Performance Metrics of Biosensor Technologies in High-Throughput Screening
| Biosensor Technology | Sensitivity/LOD | Throughput Capacity | Key Advantages | Demonstrated Application in HTS |
|---|---|---|---|---|
| SERS-Based Immunoassay | LOD: 16.73 ng/mL for α-fetoprotein | High (384-well format) | Label-free detection; multiplexing capability; resistance to photobleaching | Cancer biomarker detection using Au-Ag nanostars [40] |
| Fluorescence Lifetime (FLT)-FRET | Low micromolar potency for target engagement | Medium to High (depends on imaging speed) | Quantitative measurement of molecular interactions in living cells; insensitivity to concentration variations | Monitoring TDP-43 multimerization for ALS/FTD drug discovery [43] |
| NADPH Biosensors (iNap) | Compartment-specific NADPH detection in live cells | High (384-well format) | Subcellular resolution; real-time kinetic measurements; compatible with high-content screening | Identification of folic acid as vascular aging therapeutic [30] |
| Microwave Resonator Biosensors | Low limit of detection for live cell quantification | High (rapid, non-optical readout) | Label-free operation; non-invasive measurement; minimal sample volume requirements | Cancer cell cytotoxicity screening in response to chemotherapeutics [42] |
Quantitative Outcomes from Representative HTS Campaigns
Table 3: Quantitative Outcomes from Representative HTS Campaigns Using Biosensors
| Screening Focus | Library Size | Hit Rate | Key Identified Compounds | Validated Efficacy | Reference |
|---|---|---|---|---|---|
| TDP-43 Multimerization Stabilizers | 2,682 FDA-approved compounds | Not specified | Ketoconazole | Stabilized functional nuclear TDP-43 multimers with low micromolar potency; rescued pathology in C. elegans model [43] | [43] |
| NRAS-mutated Melanoma Therapeutics | ~1,300 compounds | 17 initial hits (≈1.3%) | Daunorubicin HCl, Pyrvinium Pamoate | Potent anti-melanoma activity in 3D models; superior to Trametinib in MEKi-resistant cells [45] | [45] |
| Programmed Cell Death Inducers in CRC | 1,068 FDA-approved compounds | 12 primary hits (>50% viability reduction); 2 validated hits | Menadione, Crystal Violet | Induced multiple PCD pathways via MAPK8 activation; effective in colorectal cancer models [44] | [44] |
| Vascular Aging Amelioration | 1,419 FDA-approved compounds | Not specified | Folic Acid | Elevated cytosolic NADPH via MTHFD1; alleviated vascular aging in naturally aged mice [30] | [30] |
The integration of advanced biosensing technologies with high-throughput screening of FDA-approved drug libraries has established a powerful paradigm for accelerating drug discovery and repurposing. The ability to monitor NADPH and NADH dynamics with subcellular resolution in physiologically relevant 3D model systems provides unprecedented insights into the metabolic effects of pharmacological intervention, enabling more informed candidate selection and mechanism elucidation. As these technologies continue to evolve, several emerging trends promise to further transform the landscape of biosensor-enabled HTS.
The convergence of CMOS-integrated biosensors with AI-driven data analytics will likely enable even higher throughput and more sophisticated pattern recognition in screening outcomes [41] [42]. Furthermore, the development of multiplexed biosensing platforms capable of simultaneously monitoring multiple parameters (e.g., NADPH/NADH ratios, specific molecular interactions, and metabolic fluxes) in the same cellular context will provide more comprehensive systems-level understanding of drug effects. Finally, the increasing implementation of single-cell biosensing approaches in HTS workflows will uncover cell-to-cell heterogeneity in drug responses, potentially revealing minority subpopulations with distinct sensitivity profiles that could inform resistance mechanisms. These technological advances, firmly grounded in the fundamental principles of redox biology, will continue to drive innovation in drug repurposing and development, ultimately accelerating the delivery of novel therapeutics to patients.
Metabolic Flux Analysis to Map NADPH Production Pathways
Nicotinamide adenine dinucleotide phosphate (NADPH) serves as a fundamental cofactor in cellular redox biochemistry, functioning as a primary electron donor in anabolic reactions and oxidative defense. In the broader context of redox biology, the balance between NADPH and its oxidized form (NADPâº), alongside the analogous NADH/NAD⺠pair, constitutes a critical regulatory system for cellular metabolism. Over 1,500 microbial reactions depend on NADH/NAD⺠and NADPH/NADP⺠cofactors, with 887 specifically utilizing NADP(H) [31]. This cofactor system maintains cellular redox homeostasis, influences stress response pathways, and provides reducing equivalents for biosynthesis, making its accurate quantification essential for understanding metabolic health and disease pathogenesis.
The regulation of NADPH intersects with reactive oxygen species (ROS) metabolism, where NADPH oxidases (NOXs) constitute a major ROS source. The NOX enzyme family, comprising seven isoforms (NOX1-5 and DUOX1/2), functions as electron-transporting membrane enzymes that generate ROS following specific physiological stimuli [46] [47]. While ROS at physiological levels function as crucial signaling molecules, dysregulated ROS production contributes to oxidative damage in pathological conditions, including fibrosis, cancer, cardiovascular diseases, and neurodegenerative disorders [46] [48]. Metabolic flux analysis (MFA) provides the computational and experimental framework to quantify NADPH production and utilization rates, offering unprecedented insights into the dynamic regulation of these critical redox pathways.
Fundamentals of Metabolic Flux Analysis
Theoretical Principles
Metabolic flux analysis represents a computational approach for quantifying the intracellular flow of metabolites through biochemical networks. At its core, MFA applies mass balance constraints to stoichiometric models of metabolism, enabling the prediction of pathway reaction rates (fluxes) from experimental data. The fundamental principle relies on the quasi-steady-state assumption, where metabolic intermediate concentrations remain constant while fluxes through pathways vary. This approach systematically accounts for all extracellular carbon inputs and outputs alongside major intracellular pathways to reconstruct comprehensive flux maps depicting cell metabolism [49].
Flux Balance Analysis (FBA) serves as the primary mathematical framework for MFA, employing linear programming to optimize an objective function (e.g., biomass production or ATP synthesis) under cellular constraints [50]. Unlike static metabolomic snapshots, flux analysis captures the dynamic nature of metabolism, revealing how carbon precursors partition between competing pathways and how regulation occurs at the network level. This is particularly valuable for understanding NADPH metabolism because multiple parallel pathways—including the oxidative pentose phosphate pathway (oxPPP), folate metabolism, and malic enzyme reactions—contribute to its production, creating a complex, compartmentalized network [30].
Technical Platforms and Methodologies
Modern MFA implementations typically employ stable isotope tracing combined with mass spectrometric detection to experimentally determine intracellular fluxes. The general workflow involves feeding cells or tissues with ¹³C- or ¹âµN-labeled nutrients (e.g., [¹³C]-glucose), followed by tracking the incorporation of heavy isotopes into metabolic products over time. LC-MS platforms then measure the mass isotopomer distributions (MIDs) of intracellular metabolites, which serve as inputs for computational flux estimation [51].
Several specialized software platforms facilitate MFA implementation:
Table 1: Key Software Tools for Metabolic Flux Analysis
| Software Tool | Primary Function | Key Features | Availability |
|---|---|---|---|
| INCA | Isotopomer Network Compartmental Analysis | Comprehensive flux estimation from isotopic labeling data | MATLAB-based, free for academics [49] |
| METAFlux | Flux Balance Analysis from gene expression | Infers metabolic fluxes from bulk and single-cell RNA-seq data | Computational pipeline [50] |
| PIRAMID | Quantification of metabolite mass isotopomer distributions | Automated MID quantification from mass spectrometry data | MATLAB-based, free for academics [49] |
| ETA | Elementary metabolite unit analysis | Flux analysis using metabolic tracing data | MATLAB-based, free for academics [49] |
Technical advancements in mass spectrometry, particularly the implementation of SWATH DIA (Data-Independent Acquisition), have significantly enhanced MFA capabilities by eliminating missing data in flux studies and enabling comprehensive metabolite coverage [51]. High-performance systems like the X500R QTOF and QTRAP 6500+ provide the sensitivity and quantitative precision required for reliable flux determination, while the SelexION device adds differential mobility spectrometry for improved isomer separation [51].
NADPH Production Pathways in Mammalian Systems
Major NADPH-Generating Enzymes and Pathways
In mammalian cells, particularly endothelial cells, NADPH generation occurs through three primary metabolic pathways that are independently regulated in different cellular compartments [30]:
Oxidative Pentose Phosphate Pathway (oxPPP): This represents the major NADPH source in most cell types. Glucose-6-phosphate dehydrogenase (G6PD), the rate-limiting enzyme, catalyzes the first committed step, generating NADPH and 6-phosphogluconolactone. 6-Phosphogluconate dehydrogenase (PGD) produces a second NADPH molecule later in the pathway. oxPPP critically regulates endothelial cell function, promoting vascular maturation by controlling vascular matrix composition and supporting highly proliferative cells [30].
Folate Metabolism: Methylenetetrahydrofolate dehydrogenase (MTHFD) generates NADPH through the oxidation of methylenetetrahydrofolate. This pathway has gained therapeutic interest, with folic acid supplementation demonstrating efficacy in elevating NADPH levels and ameliorating vascular aging in mouse models [30].
Malic Enzyme (ME) Reactions: NADPâº-dependent malic enzymes decarboxylate malate to pyruvate, generating NADPH in the cytosol or mitochondria. This pathway connects NADPH production to glutaminolysis and TCA cycle activity.
Recent research using genetically encoded NADPH sensors (iNap1) has revealed compartment-specific NADPH regulation, with cytosolic NADPH increasing during endothelial cell senescence while mitochondrial NADPH remains relatively stable [30]. This compartmentalization creates distinct NADPH pools with potentially different functional impacts.
Quantitative Flux Distribution
The relative contribution of each NADPH-producing pathway varies by cell type, metabolic state, and environmental conditions. The following table summarizes experimental flux measurements in mammalian systems:
Table 2: Quantitative Contributions of NADPH Production Pathways
| Pathway | Key Enzymes | Reported Contribution Range | Primary Cellular Role | Tissue/Cell Type Specificity |
|---|---|---|---|---|
| oxPPP | G6PD, PGD | 40-70% of total NADPH production | Redox defense, lipid synthesis | Highest in liver, endothelial cells, proliferating cells [30] |
| Folate Cycle | MTHFD1, MTHFD2 | 10-25% of total NADPH production | Nucleotide synthesis, methylation reactions | Significant in endothelial cells, cancer cells [30] |
| Malic Enzyme | ME1 (cytosolic), ME3 (mitochondrial) | 15-30% of total NADPH production | Lipogenesis, glutamine metabolism | Elevated in adipocytes, hepatic cells, certain cancers |
| IDH1/2 | IDH1 (cytosolic), IDH2 (mitochondrial) | 5-15% of total NADPH production | Redox balance, reductive carboxylation | Tissue-dependent expression patterns |
The diagram below illustrates the compartmentalization and relative fluxes through these major NADPH-producing pathways in a mammalian cell:
Diagram 1: Major NADPH production pathways show compartmentalization in mammalian cells. The oxidative pentose phosphate pathway (G6PD/PGD) in the cytosol generates 2 NADPH molecules per glucose-6-phosphate. The folate cycle (MTHFD1) and malic enzyme (ME1 in cytosol, ME3 in mitochondria) provide additional NADPH sources. Relative flux widths indicate approximate contribution under standard metabolic conditions.
Experimental Protocols for NADPH Flux Quantification
Stable Isotope Tracer Experiments
Protocol: [1,2-¹³C₂]-Glucose Tracing for oxPPP Flux Determination
Principle: This method quantifies flux through the oxidative pentose phosphate pathway by tracking the rearrangement of carbon atoms in metabolic intermediates. The non-oxidative phase of PPP scrambles the carbon positions, producing unique isotopomer patterns that can be distinguished from glycolysis.
Reagents and Materials:
- [1,2-¹³C₂]-Glucose (≥99% isotopic purity)
- Cell culture medium without glucose
- Dialyzed fetal bovine serum (to remove unlabeled glucose)
- Methanol:acetonitrile:water (40:40:20 v/v) extraction solvent
- LC-MS system with electrospray ionization (e.g., SCIEX X500R QTOF)
- Appropriate analytical column (e.g., HILIC or reversed-phase)
Procedure:
- Pre-equilibration: Culture cells in glucose-free medium for 1 hour to deplete intracellular glucose stores.
- Tracer Incubation: Replace medium with fresh medium containing 10 mM [1,2-¹³C₂]-glucose. Incubate for timepoints ranging from minutes to 24 hours depending on metabolic rate.
- Metabolite Extraction: At designated timepoints, quickly wash cells with ice-cold saline and add extraction solvent (1 mL per 10ⶠcells). Scrape cells and transfer to microcentrifuge tubes.
- Sample Processing: Vortex for 10 minutes at 4°C, then centrifuge at 16,000 × g for 15 minutes. Transfer supernatant to MS vials.
- LC-MS Analysis: Separate metabolites using HILIC chromatography with a gradient from 10 mM ammonium acetate (pH 9.0) to acetonitrile. Operate MS in negative ion mode for most metabolites.
- Data Processing: Extract mass isotopomer distributions (MIDs) for pentose phosphate pathway intermediates (ribose-5-phosphate, sedoheptulose-7-phosphate), glycolytic intermediates, and nucleotides.
Flux Calculation: Use software such as INCA to fit the experimental MIDs to a metabolic network model containing both oxPPP and non-oxidative PPP reactions. The ratio of [3-¹³C]-lactate to [2-¹³C]-lactate provides a direct measure of oxPPP flux relative to glycolysis [49] [51].
Compartment-Specific NADPH Measurement
Protocol: Genetically Encoded NADPH Sensor Imaging
Principle: The iNap1 sensor is a fluorescent protein-based biosensor that undergoes conformation changes upon NADPH binding, altering its fluorescence excitation spectrum. Targeted to different cellular compartments, it enables real-time monitoring of NADPH dynamics.
Reagents and Materials:
- cyto-iNap1 and mito-iNap3 plasmid constructs
- Primary human aortic endothelial cells (HAECs)
- Lipofectamine 3000 transfection reagent
- Confocal microscope with 405 nm and 488 nm laser lines
- Angiotensin II (2 μM) for senescence induction
- Digitonin (0.001% for plasma membrane permeabilization, 0.3% for mitochondrial membrane)
Procedure:
- Cell Transfection: Plate HAECs at 50-60% confluence in glass-bottom dishes. Transfect with 1-2 μg plasmid DNA using Lipofectamine according to manufacturer's protocol.
- Sensor Validation: 24-48 hours post-transfection, validate sensor localization via confocal microscopy. Perform in situ calibration by permeabilizing cells with digitonin and exposing to NADPH standards (0-200 μM).
- Time-Lapse Imaging: Acquire ratiometric images with sequential 405 nm and 488 nm excitation, collecting emission at 500-550 nm. Maintain cells at 37°C with 5% CO₂ during imaging.
- Senescence Induction: Add angiotensin II (2 μM) to culture medium and monitor NADPH changes over 72 hours.
- Data Analysis: Calculate 405/488 nm fluorescence ratio for each time point. Normalize to baseline readings. Compare cytosolic versus mitochondrial NADPH responses.
Key Findings: This approach revealed that cytosolic NADPH increases during endothelial cell senescence induced by angiotensin II, high glucose, endothelin-1, or homocysteine, while mitochondrial NADPH remains relatively unchanged [30].
Advanced MFA Applications in NADPH Research
Integrating Gene Expression and Flux Analysis
The METAFlux framework enables researchers to infer metabolic fluxes directly from bulk and single-cell RNA sequencing data, bridging transcriptomics with metabolic physiology. This approach applies flux balance analysis to genome-scale metabolic models constrained by gene expression patterns, allowing flux prediction in contexts where traditional isotope tracing is impractical [50].
Workflow:
- Model Reconstruction: Start with a tissue- or cell-specific genome-scale metabolic model (e.g., Recon3D).
- Expression Integration: Map RNA-seq data to enzyme-coding genes in the model, using expression levels as proxies for enzymatic capacity constraints.
- Flux Calculation: Solve the flux optimization problem to identify NADPH production rates that satisfy metabolic demands while consistent with expression patterns.
- Validation: Compare predictions with targeted isotope tracing experiments for key NADPH-producing reactions.
This methodology has proven particularly valuable for characterizing metabolic heterogeneity in tumor microenvironments and understanding how NADPH metabolism supports differential cell fate decisions [50].
Redox Imbalance as a Metabolic Engineering Strategy
Recent advances in microbial metabolic engineering demonstrate how deliberate manipulation of NADPH flux can enhance bioproduction. The Redox Imbalance Forces Drive (RIFD) strategy intentionally creates NADPH excess through "open source and reduce expenditure" approaches, then harnesses this driving force to direct carbon flux toward desired products [31].
Implementation Strategies:
- Open Source Approaches:
- Express cofactor-converting enzymes (e.g., NADH-dependent transhydrogenases)
- Introduce heterologous NADPH-dependent enzymes
- Overexpress NADPH synthesis pathway enzymes (G6PD, PGD)
- Expenditure Reduction:
- Knock out non-essential NADPH-consuming reactions
- Replace NADPH-dependent enzymes with NADH-dependent alternatives
- Downregulate competing anabolic pathways
In L-threonine production, where biosynthesis requires substantial NADPH, RIFD implementation achieved yields of 117.65 g/L with 0.65 g/g yield—among the highest reported [31]. This demonstrates how quantitative understanding of NADPH flux can be leveraged for biotechnological applications.
The Scientist's Toolkit: Essential Reagents and Platforms
Table 3: Key Research Tools for NADPH Flux Analysis
| Category | Specific Tool/Reagent | Function/Application | Key Features |
|---|---|---|---|
| Isotope Tracers | [1,2-¹³C₂]-Glucose | oxPPP flux determination | Enables discrimination between oxidative and non-oxidative PPP |
| [U-¹³C]-Glutamine | TCA cycle and anaplerosis flux | Traces NADPH production via malic enzyme | |
| Biosensors | iNap1 (cytosolic) | Real-time NADPH monitoring | Ratiometric, ( K_d ) = 3.8 μM for NADPH [30] |
| iNap3 (mitochondrial) | Compartment-specific NADPH | Targeted to mitochondrial matrix | |
| Software Platforms | INCA | Comprehensive flux analysis | Isotopomer modeling, MATLAB-based [49] |
| METAFlux | Flux from expression data | Works with RNA-seq data [50] | |
| PIRAMID | MID quantification | Automated processing of MS data [49] | |
| Analytical Systems | SCIEX X500R QTOF | High-resolution metabolomics | Small footprint, advanced metabolomics [51] |
| QTRAP 6500+ system | Sensitive metabolite detection | Hybrid triple quadrupole-linear ion trap [51] | |
| Chemical Inhibitors | GKT137831 | NOX1/4 inhibitor | Dual inhibitor, Ki ~0.1-0.2 μM [46] [47] |
| Setanaxib | NOX1/4 inhibitor | In Phase II trials for fibrosis [52] | |
| APX-115 | Pan-NOX inhibitor | Broad-spectrum, Ki 0.57-1.08 μM [52] | |
| SKLB646 | SKLB646, MF:C28H26F3N7O, MW:533.5 g/mol | Chemical Reagent | Bench Chemicals |
| Syk-IN-6 | Syk-IN-6, MF:C21H22N6O2, MW:390.4 g/mol | Chemical Reagent | Bench Chemicals |
The following diagram illustrates a recommended workflow integrating these tools for comprehensive NADPH flux analysis:
Diagram 2: Integrated workflow for NADPH flux analysis combines experimental, analytical, and computational phases. Stable isotope tracing and biosensor imaging provide complementary data streams, while computational tools like INCA and METAFlux integrate these datasets to generate comprehensive NADPH flux maps.
Metabolic flux analysis provides an indispensable framework for quantifying NADPH production pathways within their physiological context. By integrating stable isotope tracing, compartment-specific biosensors, and computational modeling, researchers can move beyond static metabolite measurements to dynamic flux assessment. This approach has revealed the remarkable compartmentalization of NADPH metabolism, with cytosolic pools responding dynamically to stressors like angiotensin II while mitochondrial pools remain stable [30].
The therapeutic implications of understanding NADPH flux are substantial, particularly in diseases characterized by oxidative stress. NOX enzymes—major NADPH consumers—contribute to numerous pathologies, and selective inhibitors like setanaxib and GKT137831 are advancing through clinical development [46] [52]. Simultaneously, strategies to enhance NADPH production, such as folic acid supplementation acting through MTHFD1, show promise for ameliorating age-related vascular decline [30].
As MFA methodologies continue evolving, particularly with single-cell flux inference and more sophisticated biosensors, our understanding of NADPH's role in redox biology will deepen. This knowledge will inform novel therapeutic strategies for conditions ranging from fibrosis and cancer to neurodegenerative diseases, ultimately enabling precise manipulation of redox metabolism for therapeutic benefit.
Nicotinamide adenine dinucleotide (NAD+) and its phosphorylated counterpart, nicotinamide adenine dinucleotide phosphate (NADP+), along with their reduced forms (NADH and NADPH), are essential cofactors that govern cellular redox homeostasis and energy metabolism. The NAD+/NADH redox couple primarily regulates cellular energy metabolism, including glycolysis and mitochondrial oxidative phosphorylation. In contrast, the NADP+/NADPH redox couple maintains redox balance and supports biosynthetic processes and antioxidant defense systems [1]. These redox couples function in distinct cellular compartments and participate in independently regulated metabolic pathways, allowing for precise control over both energy production and redox protection [30] [1].
Recent advances in genetically encoded biosensors have enabled real-time monitoring of compartmentalized NADPH pools, revealing that cytosolic and mitochondrial NADPH levels are differentially regulated during cellular processes such as senescence. Research has demonstrated that cytosolic NADPH increases during endothelial cell senescence, while mitochondrial NADPH remains relatively stable, highlighting the compartment-specific nature of NADPH metabolism in aging processes [30]. This nuanced understanding of NADPH dynamics provides a foundation for developing targeted intervention strategies using genetic manipulation and pharmacological approaches to modulate redox balance for therapeutic benefit in age-related diseases and other pathological conditions characterized by redox imbalance.
Genetic Manipulation Strategies for Redox Regulation
Overexpression Approaches
Gene overexpression techniques enable researchers to enhance the expression of specific genes involved in NADPH generation or utilization, thereby modulating cellular redox states. The G6PD/NADPH pathway represents a promising target, as studies have demonstrated that G6PD (glucose-6-phosphate dehydrogenase) overexpression significantly elevates cytosolic NADPH levels, inhibits glutathione oxidation and HDAC3 activity, and suppresses endothelial cell senescence and vascular aging [30].
Effective overexpression requires careful selection of delivery vectors and expression systems. Lentiviral vectors are particularly valuable for stable, long-term expression, as they integrate into the host genome and provide persistent transgene expression. For primary cells and organoid systems, optimized protocols using lentiviral transduction with stem cell-promoting factors enhance the efficiency of genetic modification [53]. These systems often utilize constitutive promoters (EF1α, PGK) that are less susceptible to epigenetic silencing compared to traditional CMV promoters, ensuring consistent transgene expression [53].
For more precise temporal control, tetracycline-regulated systems enable inducible gene expression, allowing researchers to initiate overexpression at specific time points. This is particularly valuable for studying genes that might impair cellular proliferation or viability if constitutively expressed [53]. Additionally, cell-type-specific promoters can restrict transgene expression to particular cellular populations, enabling more targeted manipulation of redox pathways in complex biological systems.
Knockdown Approaches
Gene knockdown strategies allow for the reduction of specific gene expression to elucidate function or modulate pathological processes. Multiple technologies are available for gene knockdown, each with distinct mechanisms and applications as outlined in Table 1 below.
Table 1: Comparison of Gene Knockdown Methods
| Method | Key Feature | Mechanism of Action | Duration | Primary Applications |
|---|---|---|---|---|
| RNA Interference (RNAi) | Sequence-specific mRNA targeting | RISC-mediated mRNA degradation | Transient (siRNA) or stable (shRNA) | Functional genomics, target validation |
| Morpholino Oligonucleotides | Translation blockade | Steric hindrance of ribosomal assembly | Transient | Developmental studies, early embryonic manipulation |
| CRISPR Interference (CRISPRi) | Transcriptional repression | dCas9-repressor binding to promoter regions | Stable | Gene silencing without DNA cleavage, functional screening |
| Antisense Oligonucleotides (ASOs) | mRNA binding and inhibition | Prevention of translation or promotion of degradation | Transient | Therapeutic applications, functional studies |
RNA interference technologies include both small interfering RNA (siRNA) for transient knockdown and short hairpin RNA (shRNA) for stable, long-term gene suppression. siRNA involves the design of sequences complementary to the target mRNA, which are introduced into cells via transfection methods such as lipofection or electroporation. Once incorporated into the RNA-induced silencing complex (RISC), siRNA guides the degradation of the target mRNA [54]. For persistent knockdown, shRNA sequences can be cloned into plasmid or viral vectors and introduced via transduction, enabling integration into the genome and long-term suppression [54].
CRISPR interference represents a more recent advancement in gene knockdown technology. This approach utilizes a catalytically dead Cas9 (dCas9) protein fused to a transcriptional repressor domain (e.g., KRAB). The dCas9-repressor complex is guided to promoter regions of target genes by specific gRNAs, where it inhibits transcription without cleaving the DNA [54]. This method offers high specificity and avoids potential off-target effects associated with nuclease-active CRISPR systems.
Experimental Protocols for Genetic Manipulation
Protocol for Stable Overexpression in Primary Cells
Vector Construction: Clone the gene of interest (e.g., G6PD) into a lentiviral expression vector containing a constitutive promoter (EF1α or PGK) and a selection marker (e.g., puromycin resistance or fluorescent reporter) [53].
Virus Production: Generate lentiviral particles by transfecting HEK293T cells with the transfer vector and packaging plasmids using lipid-based transfection reagents. Collect supernatant containing viral particles at 48-72 hours post-transfection [53].
Cell Preparation and Transduction: Dissociate target cells (e.g., primary endothelial cells) into single-cell suspensions using gentle enzymatic digestion (Accutase). Plate cells at optimal density (300,000 cells per 35-mm dish for primary cells) and transduce with viral supernatant in the presence of polybrene (4-8 μg/mL) to enhance infection efficiency [53].
Selection and Expansion: Begin antibiotic selection (e.g., puromycin at predetermined optimal concentration) 48 hours post-transduction. Maintain selection for 5-7 days, then expand resistant cells for experimental analysis [30].
Validation: Confirm overexpression using qPCR for mRNA levels and Western blotting for protein expression. Assess functional consequences by measuring NADPH levels using enzymatic assays or genetically encoded sensors, and evaluate phenotypic effects through senescence-associated β-galactosidase staining and analysis of senescence markers (p16, p21) [30].
Protocol for CRISPRi-Mediated Knockdown
Guide RNA Design: Design gRNAs targeting the promoter region of the gene of interest. Bioinformatics tools should be used to minimize off-target effects [54].
Vector Preparation: Clone gRNA sequences into appropriate expression vectors. Prepare dCas9-KRAB repressor construct if not already available in the target cells [54].
Delivery: Introduce both dCas9-KRAB and gRNA constructs into target cells via lentiviral transduction or lipid-based transfection, optimizing conditions for specific cell type [54].
Validation: Assess knockdown efficiency using qPCR and Western blotting. Evaluate functional consequences on NADPH metabolism using appropriate assays [30].
Figure 1: Genetic Manipulation Strategies Targeting G6PD/NADPH Pathway in Vascular Aging. Overexpression of G6PD elevates NADPH, promoting reduced glutathione and HDAC3 inhibition to protect against senescence. Conversely, G6PD knockdown decreases NADPH, increasing oxidative stress and accelerating senescence.
Pharmacological Agonists and Antagonists in Redox Regulation
Fundamental Concepts in Pharmacology
Pharmacological interventions targeting redox pathways utilize compounds that modulate the activity of enzymes and receptors involved in NADPH and NADH metabolism. Understanding modern pharmacological concepts is essential for designing effective intervention strategies:
Constitutive receptor activity refers to the ability of receptors to adopt active conformations and signal in the absence of activating ligands. This discovery led to the identification of inverse agonists - ligands that reduce constitutive receptor activity, producing effects opposite to those of agonists [55].
Functional selectivity describes how a drug acting at a single receptor subtype can have multiple intrinsic efficacies that differ depending on which response pathway is measured. This means a compound can simultaneously act as an agonist for one signaling pathway while functioning as an antagonist or inverse agonist for another pathway coupled to the same receptor [55]. This concept is particularly relevant for targeting complex redox signaling networks where multiple downstream effects may be desirable.
Pharmacological Targeting of NADPH Metabolism
Pharmacological screening approaches have identified several compounds that modulate NADPH levels and redox homeostasis. High-throughput screening of 1,419 FDA-approved drugs using genetically encoded NADPH sensors revealed folic acid as a potent NADPH elevator. Folic acid is catalyzed by methylenetetrahydrofolate dehydrogenase (MTHFD) to generate NADPH, and it has demonstrated efficacy in ameliorating vascular aging in angiotensin II-infused mice and naturally aged mice [30].
The oxidative pentose phosphate pathway represents another key target for pharmacological intervention. Compounds that activate G6PD, the rate-limiting enzyme in this pathway, can boost NADPH production. Research has shown that decreased nitric oxide concentration promotes G6PD de-S-nitrosylation at C385, increasing its activity and elevating NADPH levels [30]. This post-translational modification mechanism provides a potential target for small molecule drugs designed to enhance G6PD activity specifically.
Table 2: Pharmacological Agents Targeting NADPH Metabolism and Redox Balance
| Pharmacological Agent | Molecular Target | Biological Effect | Therapeutic Application |
|---|---|---|---|
| Folic Acid | MTHFD (Methylenetetrahydrofolate dehydrogenase) | Increases NADPH generation via folate metabolism | Ameliorates vascular aging in mouse models [30] |
| Compounds affecting G6PD S-nitrosylation | G6PD at C385 residue | Potentiates G6PD activity by preventing S-nitrosylation | Potential application in age-related vascular dysfunction [30] |
| NAD+ Precursors | NAD+ biosynthetic pathways | Enhance NAD+ levels, indirectly supporting NADPH generation | Investigated for metabolic diseases, age-related disorders [1] |
| NRF2 Activators | NRF2 transcription factor | Enhance expression of antioxidant genes including NADPH-generating enzymes | Oxidative stress-related conditions [48] |
Experimental Protocols for Pharmacological Studies
Protocol for High-Throughput NADPH Drug Screening
Cell Preparation: Seed primary human aortic endothelial cells (HAECs) expressing the genetically encoded NADPH sensor iNap1 in 96-well or 384-well plates at optimized density [30].
Drug Treatment: Apply compound libraries (e.g., FDA-approved drug collections) at appropriate concentrations (typically 1-10 μM), including positive and negative controls. Incubate for predetermined time periods (e.g., 24-72 hours) [30].
Fluorescence Measurement: Monitor iNap1 fluorescence using plate readers capable of ratiometric measurements (excitation at 405/488 nm, emission detection appropriate for the sensor). Calculate 405/488 nm ratios to determine NADPH levels [30].
Validation and Dose-Response: Confirm hits from primary screening in dose-response experiments. Determine EC50 values for active compounds using non-linear regression analysis of concentration-response curves [30].
Functional Validation: Assess the effects of confirmed hits on cellular senescence markers (SA-β-galactosidase activity, p16 and p21 expression), oxidative stress parameters, and functional endpoints relevant to the disease model [30].
Protocol for Evaluating Drug Effects in Aging Models
In Vitro Senescence Models: Induce senescence in primary cells using angiotensin II (2 μM for 72 hours), high glucose (25 mM for 48 hours), or replicative exhaustion. Treat with test compounds at various time points during or after senescence induction [30].
In Vivo Aging Models: Administer test compounds to aged mice (e.g., 18-24 months old) or accelerated aging models (e.g., angiotensin II-infused mice). Include young controls (4 months old) for comparison. Delivery methods may include oral gavage, intraperitoneal injection, or dietary administration depending on compound properties [30].
Endpoint Analysis: Assess vascular function, tissue NADPH levels, senescence markers in tissues, and functional parameters relevant to the aging phenotype. Compare results to young and aged untreated controls [30].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for NADPH/NADH Redox Studies
| Research Tool | Specific Examples | Application | Key Features |
|---|---|---|---|
| Genetically Encoded Biosensors | iNap1 (NADPH sensor), SoNar (NADH/NAD+ ratio sensor) | Real-time monitoring of compartmentalized NADPH and NADH levels | Subcellular targeting capabilities (cytosolic, mitochondrial); rationetric measurements [30] |
| Gene Delivery Vectors | Lentiviral vectors (EF1α, PGK promoters), PiggyBac transposon system | Stable genetic manipulation (overexpression/knockdown) | High transduction efficiency; stable integration; inducible systems available [53] |
| Gene Editing Systems | CRISPR/Cas9 (knockout), CRISPRi (knockdown), TALENs, ZFNs | Targeted genetic manipulation | High specificity; CRISPRi enables repression without DNA cleavage [56] [54] |
| Senescence Assays | SA-β-galactosidase staining, p16/p21 immunoblotting, SASP factor analysis | Assessment of cellular aging | Well-established markers for senescent cells [30] |
| NADPH Measurement Tools | Enzymatic cycling assays, HPLC, mass spectrometry | Quantitative NADPH determination | Absolute quantification; requires cell homogenization [30] |
| STING agonist-1 | STING agonist-1, CAS:702662-50-8, MF:C21H16ClFN2O3S, MW:430.9 g/mol | Chemical Reagent | Bench Chemicals |
| LXG6403 | LXG6403, MF:C15H15N5OS2, MW:345.4 g/mol | Chemical Reagent | Bench Chemicals |
Figure 2: Experimental Workflow for NADPH/NADH Redox Biology Research. The diagram outlines parallel approaches for genetic and pharmacological strategies, converging on NADPH assessment and functional phenotyping.
Genetic manipulation and pharmacological intervention strategies targeting NADPH and NADH metabolism represent powerful approaches for investigating and therapeutically modulating redox biology in aging and disease. The integration of precise genetic tools—including overexpression systems and targeted knockdown technologies—with specific pharmacological agents that modulate NADPH generation and utilization enables comprehensive investigation of redox pathways. The continuing development of more specific genetic tools and targeted pharmacological compounds promises to enhance our ability to precisely manipulate redox balance for research and therapeutic purposes. As these technologies advance, they will undoubtedly yield new insights into the complex roles of NADPH and NADH in health and disease, potentially leading to novel interventions for age-related conditions and other pathologies characterized by redox imbalance.
Dysregulation and Redox Stress: From Molecular Pathology to Therapeutic Correction
Defining Oxidative and Reductive Stress in Disease Contexts
Redox biology, the study of reduction-oxidation reactions within living organisms, is fundamental to cellular homeostasis. At its core are two pivotal states of imbalance: oxidative stress and reductive stress. Oxidative stress occurs when there is an excess of reactive oxygen species (ROS) relative to antioxidant defenses, leading to cellular damage [57]. Conversely, reductive stress (RS) is characterized by an abnormal accumulation of reducing equivalents—such as NADH and NADPH—creating a disproportionately reduced intracellular environment despite intact oxidation-reduction systems [58] [59]. The NAD+/NADH and NADP+/NADPH redox couples are central regulators of this delicate balance, acting as critical electron carriers that influence numerous biological processes, from energy metabolism to cellular signaling [1]. Disruption of these redox couples contributes significantly to disease pathogenesis, making them a focal point in therapeutic development.
Molecular Definitions and Key Players
Oxidative Stress: An Imbalance of Free Radicals
Oxidative stress is defined as an imbalance between free radicals and antioxidants in the body, which leads to cell damage [57]. Free radicals, such as superoxide radicals (O₂•â») and hydroxyl radicals (•OH), are unstable molecules missing an electron, making them highly reactive as they seek to stabilize by stealing electrons from cellular components like proteins, lipids, and DNA [57] [60]. Under physiological conditions, free radicals play beneficial roles in immune function and cell signaling [60]. However, when their production overwhelms the body's antioxidant defenses—which include enzymes like superoxide dismutase (SOD), catalase (CAT), and glutathione peroxidase (GPx)—oxidative damage ensues [60].
Reductive Stress: An Excess of Reducing Equivalents
Reductive stress is the counterpart to oxidative stress, characterized by a surplus of reducing equivalents like NADH, NADPH, and glutathione (GSH) relative to their oxidized forms [58] [59]. This state creates a highly reduced intracellular environment that disrupts normal redox signaling and biochemical processes. While it can result from an overactive antioxidant response, chronic reductive stress can paradoxically induce oxidative stress through a feedback loop, as some redox proteins may donate electrons to molecular oxygen, inadvertently generating ROS [58] [59]. This cyclical relationship complicates the role of redox imbalance in disease.
Central Redox Couples: NADPH and NADH
The NAD+/NADH and NADP+/NADPH couples are essential for maintaining redox homeostasis. Their distinct roles and characteristics are summarized in the table below.
Table 1: Key Characteristics of NAD(H) and NADP(H) Redox Couples
| Feature | NAD+/NADH | NADP+/NADPH |
|---|---|---|
| Primary Cellular Role | Regulator of cellular energy metabolism (glycolysis, oxidative phosphorylation) [1] | Maintaining redox balance, supporting biosynthesis of fatty acids and nucleic acids [1] |
| Redox Function | Oxidizing agent (NAD+); accepts electrons to become NADH [61] | Reducing agent (NADPH); donates electrons in anabolic and antioxidant reactions [1] [61] |
| Standard Midpoint Potential | -0.32 volts [61] | Similar to NAD+/NADH, but specialized for different biochemical pathways |
| Maintenance of Reduced Pool | Primarily through catabolic reactions [1] | Pentose phosphate pathway, NAD+ kinase (NADK) activity [1] |
| Subcellular Distribution | Highest concentration in mitochondria (40-70% of cellular NAD+) [1] [61] | Varies by compartment; cytosolic and mitochondrial pools regulated separately [1] |
Signaling Pathways and Disease Mechanisms
Redox Signaling in Oxidative Stress
Oxidative stress activates several key signaling pathways that contribute to disease. A primary mechanism involves the activation of pro-inflammatory and pro-fibrotic pathways. For instance, in liver fibrosis, ROS derived from NADPH oxidases (NOXs) are crucial for activating hepatic stellate cells (HSCs) into collagen-producing myofibroblasts [62]. Furthermore, ROS can activate the transcription factor NF-κB, which regulates the expression of numerous genes involved in inflammation, cell survival, and proliferation [59]. This pathway is implicated in atherosclerosis, where oxidative modification of LDL cholesterol by ROS leads to endothelial inflammation and plaque formation [57] [60].
Figure 1: Key Signaling Pathways in Oxidative Stress. Oxidative stress and ROS create a feed-forward loop that drives inflammation, cell death, and tissue fibrosis via pathways like NF-κB.
Reductive Stress Signaling and Pathological Consequences
Reductive stress exerts its pathological effects through distinct mechanisms. A central player is the transcription factor Nrf2, which normally induces the expression of antioxidant response genes. Uncontrolled amplification of Nrf2 signaling can lead to an overproduction of antioxidant enzymes, depleting ROS excessively and pushing the cell into a reductive state [58] [59]. The resulting excess of NADH creates "electron pressure" on the mitochondrial electron transport chain (ETC). This pressure can increase electron leakage, paradoxically generating superoxide radicals and leading to mitochondrial dysfunction [59]. Moreover, a highly reducing environment in the endoplasmic reticulum (ER) impairs the formation of essential disulfide bonds in proteins, causing protein misfolding, the unfolded protein response (UPRER), and potentially cytotoxic protein aggregation [58] [59].
Figure 2: Mechanisms of Reductive Stress. Excess reducing equivalents drive pathology via Nrf2 over-activation and mitochondrial electron pressure, leading to protein misfolding.
Disease Contexts and Implications
Oxidative Stress in Chronic Degenerative Diseases
Oxidative stress is a well-established contributor to a wide spectrum of chronic conditions by directly damaging critical cellular components.
- Cancer: Oxidative damage to DNA causes mutations and chromosomal abnormalities that can initiate and promote cancer development. Lesions like 8-oxo-2'-deoxyguanosine (8-OHdG) are mutagenic and linked to various cancers [57] [60].
- Cardiovascular Diseases: ROS trigger atherosclerosis by oxidizing LDL cholesterol, which is then taken up by macrophages to form foam cells, the hallmark of atherosclerotic plaques [57] [60].
- Neurological Diseases: Diseases such as Alzheimer's, Parkinson's, and multiple sclerosis have been linked to oxidative stress, which contributes to neuron loss and progressive dementia [57] [60].
- Liver Fibrosis: Chronic oxidative stress is a key driver in the activation of hepatic stellate cells into collagen-producing myofibroblasts, leading to excessive scar tissue deposition in the liver [62].
The Emerging Role of Reductive Stress in Pathology
While less recognized than its oxidative counterpart, reductive stress is increasingly implicated in several disease processes.
- Cardiomyopathy: Reductive stress, potentially induced by high levels of heat shock protein 27 (Hsp27), has been linked to an increased probability of developing cardiomyopathy [58] [63].
- Metabolic Disorders: Overnutrition can induce reductive stress, which is now considered a key pathway in disorders like obesity and type 2 diabetes. An excess of reducing equivalents disrupts normal metabolic signaling and mitochondrial function [63].
- Cancer and Therapy Resistance: Cancer cells can exploit a reductive environment to promote growth and resist treatments like chemotherapy and radiotherapy [58] [1].
- Aging: A reductive environment in the endoplasmic reticulum has been associated with cellular senescence. Interestingly, elevating the ER's oxidation status can slow the aging process in cells [58].
Table 2: Comparative Roles of Oxidative and Reductive Stress in Select Diseases
| Disease | Role of Oxidative Stress | Role of Reductive Stress |
|---|---|---|
| Cardiomyopathy | Triggers plaque formation in arteries, leading to heart attack [57] | Linked to protein aggregation and cardiomyopathy, e.g., via Hsp27 [58] [63] |
| Cancer | Damages DNA in healthy cells, raising cancer risk [57] | Promotes cancer metastasis and resistance to therapy [58] [1] |
| Metabolic Syndrome/Diabetes | Contributes to insulin resistance and complications [60] | A key pathway induced by overnutrition, disrupting metabolism [63] |
| Aging | Speeds up the body's aging process [60] | Present in senescent cells; slowing ER reductive stress delays aging [58] |
| Neurological Disease | Linked to Alzheimer's, Parkinson's, and multiple sclerosis [57] | Associated with Alzheimer's disease pathology [59] |
Experimental Assessment and Methodologies
Accurately measuring the cellular redox state is complex due to the compartmentalized nature of NAD(H) and NADP(H) pools. The following methodologies are central to redox biology research.
Measuring the Redox State of NAD(H) and NADP(H) Couples
- Genetically Encoded Biosensors: Modern research utilizes genetically encoded fluorescent biosensors targeted to specific subcellular compartments (e.g., cytosol, mitochondria). These sensors, such as those for NADH/NAD+ ratio, undergo conformational changes upon binding the metabolite, altering their fluorescence properties and allowing real-time monitoring in live cells [1].
- Ultraviolet (UV) Spectrophotometry: The oxidized and reduced forms of NAD have distinct UV absorption spectra. NADH absorbs strongly at 339 nm, whereas NAD+ does not. Measuring the absorbance at 340 nm is a classic, well-established method to track the conversion between NAD+ and NADH in enzyme assays [61].
- Fluorescence Microscopy of NADH: Native NADH is fluorescent when excited with near-UV light (~335 nm), emitting blue light (~445-460 nm). NAD+ is not fluorescent. This intrinsic fluorescence allows for the measurement of the NAD+/NADH ratio in living cells. Importantly, the fluorescence properties change when NADH binds to proteins, providing information on the bound vs. free state, which is crucial for understanding enzyme kinetics and metabolic state [61] [1].
- High-Performance Liquid Chromatography (HPLC): To obtain absolute concentrations of NAD+, NADH, NADP+, and NADPH, researchers use HPLC to separate and quantify these metabolites from cell or tissue extracts. This method requires careful sample preparation, often involving rapid extraction with acid or base to preserve the in vivo redox state of the labile cofactors [1].
Inducing and Quantifying Reductive Stress
- Induction with Chemical Agents:
- 1,4-Dithiothreitol (DTT): A strong reducing agent used experimentally to create a reductive environment, particularly in the ER, to study its effects on disulfide bond formation and protein folding [63].
- Glutathione Ethyl Ester (GEE): A cell-permeable precursor that elevates intracellular levels of reduced glutathione (GSH), directly shifting the GSH/GSSG ratio towards a more reduced state and inducing reductive stress [63].
- N-acetylcysteine (NAC): While often used as an antioxidant, chronic or high-dose treatment with NAC can paradoxically induce reductive stress by significantly elevating cellular reducing capacity [59] [63].
- Genetic Models:
- Overexpression of Antioxidant Enzymes: Transgenic models that overexpress enzymes like catalase or superoxide dismutase can deplete physiological ROS levels, leading to a reductive state [58] [59].
- Expression of Mutant Proteins: Models expressing mutant proteins associated with protein aggregation, such as the human αB-crystallin R120G mutant (hR120G cryAB), spontaneously develop reductive stress and cardiomyopathy [63].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Studying Redox Stress
| Research Reagent | Function in Redox Studies |
|---|---|
| N-acetylcysteine (NAC) | A precursor to glutathione; used as an antioxidant but can induce reductive stress at high doses [59] [63]. |
| 1,4-Dithiothreitol (DTT) | A strong reducing agent used to experimentally induce reductive stress, particularly in the ER [63]. |
| Glutathione Ethyl Ester (GEE) | A cell-permeable form of glutathione used to increase the intracellular GSH pool and shift the redox state towards reduction [63]. |
| Sulforaphane | An activator of the Nrf2 pathway; used to study the consequences of upregulated antioxidant gene expression [63]. |
| NADH Oxidase (LbNOX) | A bacterial enzyme expressed in mitochondria or cytosol of model systems to selectively oxidize NADH and alleviate reductive stress [63]. |
| Genetically Encoded Biosensors | Fluorescent proteins (e.g., roGFP, RexYFP) targeted to organelles to measure dynamic changes in redox couples like NADH/NAD+ and GSH/GSSG [1]. |
| CSC-6 | CSC-6, MF:C18H12F3NO2S2, MW:395.4 g/mol |
| KRAS inhibitor-40 | KRAS inhibitor-40, MF:C53H68ClF4N9O8S, MW:1102.7 g/mol |
Figure 3: Experimental Workflow for Redox Stress Research. A generalized pipeline for investigating oxidative and reductive stress, from model system selection to phenotypic analysis.
Concluding Perspectives and Future Directions
The intricate interplay between oxidative and reductive stress underscores a fundamental principle in redox biology: cellular health depends on a precise redox balance, not merely the absence of oxidation. The NADPH and NADH redox couples sit at the nexus of this balance, governing metabolic flux, antioxidant defense, and signaling pathways. Future research must continue to unravel the complex, compartmentalized regulation of these redox couples and their interactions with other signaling networks, such as those involving hypoxia-inducible factor (HIF) [1]. Furthermore, the paradoxical ability of chronic reductive stress to induce oxidative damage, and of antioxidant oversupplementation to potentially cause harm, highlights the need for nuanced therapeutic strategies [59]. Emerging approaches, including pharmacological interventions or nutrient-based NAD+ precursors, hold promise for treating metabolic and age-related diseases [1]. A deeper understanding of how to measure and manipulate these redox states will be crucial for addressing a host of pathological conditions effectively, paving the way for a new class of redox-based therapeutics.
Nicotinamide adenine dinucleotide phosphate (NADPH) plays a critical role in vascular aging through compartment-specific regulation of redox homeostasis. Recent advances reveal that cytosolic NADPH elevation during endothelial cell senescence represents an adaptive response mediated through glucose-6-phosphate dehydrogenase (G6PD) upregulation and histone deacetylase 3 (HDAC3) signaling pathways. Folate metabolism, particularly through methylenetetrahydrofolate dehydrogenase (MTHFD), generates NADPH and demonstrates therapeutic potential for ameliorating vascular aging. This whitepaper integrates current understanding of NADPH metabolism in vascular aging, detailing molecular mechanisms, experimental methodologies, and emerging therapeutic strategies targeting the NADPH redox system for age-related cardiovascular diseases.
Nicotinamide adenine dinucleotide phosphate (NADPH) serves as an essential redox cofactor distinct from NADH in both compartmentalization and biological function. While NADH primarily drives oxidative phosphorylation and ATP production, NADPH provides reducing power for antioxidant defense and reductive biosynthesis [30] [64]. The NADPH/NADP+ ratio maintains cellular redox homeostasis, protecting against oxidative stress—a key driver of vascular aging [65]. Intracellular NADPH consumption and production are independently regulated in different cellular compartments, with the oxidative pentose phosphate pathway (oxPPP), folate metabolism, and malic enzymes serving as principal NADPH sources in endothelial cells [30].
Vascular aging manifests through endothelial dysfunction, arterial stiffness, and cellular senescence, with NADPH metabolism emerging as a central regulatory node [65]. The vascular endothelium, a single cell layer lining blood vessels, maintains vascular homeostasis, and its senescence initiates and progresses cardiovascular diseases [30]. This technical review examines the intricate relationships between NADPH metabolism, G6PD regulation, folate-dependent pathways, and HDAC3 signaling in vascular aging contexts.
Compartmentalized NADPH Dynamics in Aging Vasculature
Subcellular NADPH Pools and Measurement Techniques
Traditional enzymatic assays, mass spectrometry, and chromatography require cell homogenization and cannot differentiate compartment-specific NADPH pools, where it regulates distinct functions [30]. Genetically encoded sensors like iNap1 enable real-time monitoring of subcellular NADPH dynamics:
- Cytosolic NADPH monitoring: iNap1 targeted to cytosol (cyto-iNap1)
- Mitochondrial NADPH monitoring: iNap3 targeted to mitochondria (mito-iNap3)
- Calibration: Permeabilization with 0.001% (plasma membrane) or 0.3% digitonin (mitochondrial inner membrane) followed by NADPH titration
- Specificity validation: iNap1 responds linearly to NADPH concentrations, while control iNapc remains nonresponsive [30]
Table 1: Compartmental NADPH Dynamics in Endothelial Cell Senescence Models
| Senescence Model | Cytosolic NADPH | Mitochondrial NADPH | Experimental System |
|---|---|---|---|
| Angiotensin II (2 μM, 72h) | ↑ Significant increase | No significant change | Primary human aortic ECs |
| High Glucose (25 mM, 48h) | ↑ Significant increase | No significant change | Primary human aortic ECs |
| Endothelin-1 (10 nM, 48h) | ↑ Significant increase | No significant change | Primary human aortic ECs |
| Homocysteine (50 μM, 72h) | ↑ Significant increase | No significant change | Primary human aortic ECs |
| Replicative senescence | ↑ Significant increase | No significant change | Primary human aortic ECs |
| Naturally aged mice (18mo vs 4mo) | ↑ Significant increase | Not measured | Isolated aortic ECs |
Divergent Responses in Vascular Aging
Research demonstrates consistently elevated cytosolic NADPH during endothelial cell (EC) senescence across multiple models, while mitochondrial NADPH remains stable [30]. This compartment-specific regulation highlights the importance of subcellular analysis in understanding redox biology in aging. Notably, cytosolic NADPH elevation was confirmed in ECs isolated from thoracic aorta of old (18 months) compared to young (4 months) mice, and NADPH content was higher in thoracic aorta of naturally aged mice (24 months old) versus young mice (4 months old) [30]. Plasma NADPH levels also trend upward in aging humans [30].
G6PD Regulation of NADPH in Vascular Aging
G6PD Activity and S-Nitrosylation
Glucose-6-phosphate dehydrogenase (G6PD), the rate-limiting enzyme in oxPPP, critically regulates NADPH production during vascular aging:
- Mechanism: Decreased nitric oxide concentration promotes G6PD de-S-nitrosylation at C385, increasing its activity
- Consequence: Enhanced G6PD activity elevates cytosolic NADPH during EC senescence
- Functional impact: G6PD overexpression alleviates, while its knockdown aggravates, vascular aging [30]
The indispensable role of NADPH in G6PD-mediated protection occurs through increased reduced glutathione and inhibited HDAC3 activity [30]. This positions G6PD as a central regulator in the compensatory response to vascular aging.
Experimental Evidence for G6PD in Senescence
- Genetic manipulation: G6PD overexpression significantly elevates NADPH level, inhibits glutathione oxidation and HDAC3 activity, and suppresses EC senescence and vascular aging
- Therapeutic validation: G6PD/NADPH pathway is upregulated by stimulators of vascular aging and plays a causal role in limiting endothelial cell aging [30]
Table 2: G6PD Manipulation Effects on Vascular Aging Parameters
| Intervention | NADPH Level | GSH/GSSG Ratio | HDAC3 Activity | Senescence Markers | Vascular Aging |
|---|---|---|---|---|---|
| G6PD Overexpression | ↑ Significant increase | ↑ Increased reduction | ↓ Inhibition | ↓ Reduced β-gal, p16, p21 | Ameliorated |
| G6PD Knockdown | ↓ Significant decrease | ↓ Increased oxidation | ↑ Activation | ↑ Elevated β-gal, p16, p21 | Aggravated |
Folate Metabolism and NADPH Generation
Folate Pathways in NADPH Production
Folate metabolism represents a significant NADPH source through methylenetetrahydrofolate dehydrogenase (MTHFD). The folate pathway involves:
- Dietary forms: Natural folates (polyglutamated) and synthetic folic acid (oxidized)
- Absorption: Dietary folates deconjugated to monoglutamate forms in small intestine
- Cellular uptake: Through reduced folate carriers (RFCs) and folate receptors
- Activation: Reduction to dihydrofolate (DHF) and tetrahydrofolate (THF) by dihydrofolate reductase (DHFR)
- NADPH generation: MTHFD catalyzes NADPH production in folate metabolism [66]
The biologically active form L-5-methyltetrahydrofolate (L-methylfolate) is critical for one-carbon metabolism and homocysteine conversion to methionine, reducing vascular toxicity [66].
Folate in Vascular Aging: U-shaped Relationship
Epidemiological evidence reveals a complex relationship between folate status and aging:
- NHANES analysis: U-shaped relationship between red blood cell (RBC) folate and phenotypic age acceleration (PhenoAgeAccel)
- Inflection point: 732.9 ng/mL RBC folate
- Below threshold: PhenoAgeAccel decreased by 0.0027 years per 1 ng/mL increase in RBC folate
- Above threshold: PhenoAgeAccel increased by 0.0058 years per 1 ng/mL increase in RBC folate [67]
This U-shaped relationship indicates that both deficiency and excess of folate may adversely affect vascular health, requiring precise optimization for therapeutic intervention.
HDAC3 as NADPH-Mediated Signaling Hub
HDAC3 in Metabolic Reprogramming
Histone deacetylase 3 (HDAC3) has emerged as a critical mediator of vascular metabolic reprogramming:
- Expression: HDAC3 upregulated in retinal vessels of oxygen-induced retinopathy (OIR) mice and human diabetic retinopathy samples
- Function: HDAC3 drives pathological neovascularization by promoting endothelial cell metabolic reprogramming toward glycolysis
- Mechanism: HDAC3 induces mitochondrial fission and hexokinase 2 (HK2) signaling, increasing glycolytic flux [68]
HDAC3 inhibition with RGFP966 (2, 8 μM) attenuates oxygen-glucose deprivation/reoxygenation (OGD/R)-induced angiogenesis and mitochondrial fission [68].
NADPH-HDAC3 Interrelationship
Research confirms NADPH is indispensable for G6PD to protect against vascular aging through inhibiting HDAC3 activity [30]. This positions HDAC3 as a downstream effector of NADPH-mediated protection in vascular aging, connecting redox metabolism to epigenetic regulation in senescent cells.
Experimental Models and Methodologies
Endothelial Cell Senescence Models
- Angiotensin II-induced: 2 μM for 72 hours in primary human aortic endothelial cells (HAECs)
- Validation markers: Increased β-galactosidase staining, elevated p16, p21, VCAM-1 protein levels, increased SASP factors (IL-1β, IL-6, IL-8, CXCL1) mRNA [30]
- Other inducters: High glucose (25 mM, 48h), endothelin-1 (10 nM, 48h), homocysteine (50 μM, 72h), replicative senescence [30]
NADPH Measurement Techniques
- Genetically encoded sensors: iNap1 for NADPH (excitation 405/420 nm and 488/485 nm, ratio reflects NADPH level)
- Control sensor: iNapc as nonresponsive variant for normalization
- SoNar indicator: For NADH/NAD+ ratio measurement, with cpYFP control [30]
- Validation treatments: Diamide (oxidant, 100 μM) lowers cyto-iNap1 but not mito-iNap3 [30]
In Vivo Vascular Aging Models
- Natural aging: Comparison of young (4 months) versus old (18-24 months) mice
- Angiotensin II-infused mice: Model for accelerated vascular aging
- Assessment: NADPH measurement in isolated aortic ECs, vascular reactivity studies [30]
Therapeutic Screening and Clinical Translation
Drug Screening Approaches
High-throughput metabolic screening of 1,419 FDA-approved drugs identified folic acid as effectively elevating NADPH and alleviating vascular aging [30]. This screening utilized the iNap1 sensor system in endothelial cells, enabling detection of NADPH-modulating compounds.
Folate Intervention Studies
- Mechanism: Folic acid, catalyzed by MTHFD to generate NADPH, alleviates vascular aging in angiotensin II-infused mice and naturally aged mice
- Human evidence: Folate supplementation improves endothelial function, especially in cardiovascular risk populations, by increasing nitric oxide bioavailability and reducing oxidative stress [66]
- Clinical consideration: Mandatory folic acid fortification reduces neural tube defects but raises concerns about unmetabolized folic acid with high supplementation [66]
Table 3: Research Reagent Solutions for NADPH-Vascular Aging Studies
| Reagent/Tool | Application | Key Features | Experimental Use |
|---|---|---|---|
| iNap1 sensor | NADPH monitoring | Genetically encoded, compartment-specific | Live-cell NADPH imaging in cytosol or mitochondria |
| SoNar indicator | NADH/NAD+ ratio | Responsive to redox changes | Monitoring NAD+ metabolism in aging models |
| Angiotensin II | Senescence induction | 2 μM for 72 hours | Establishing EC senescence in HAECs |
| RGFP966 | HDAC3 inhibition | Selective HDAC3 inhibitor | Probing HDAC3 role in metabolic reprogramming |
| G6PD assays | Enzyme activity | Measures S-nitrosylation status | Evaluating G6PD regulation in redox balance |
| L-methylfolate | Active folate form | Bypasses metabolic conversion issues | Therapeutic studies in vascular aging models |
Integrated Signaling Pathways
NADPH Signaling in Vascular Aging
The compartment-specific regulation of NADPH metabolism, particularly cytosolic NADPH elevation through G6PD and folate pathways, represents a critical adaptive mechanism in vascular aging. The connection between NADPH metabolism and endothelial cell senescence provides a unique angle for understanding vascular aging and an efficient target for therapy [30]. Future research should focus on:
- Tissue-specific NADPH dynamics: How different vascular beds regulate NADPH during aging
- Therapeutic optimization: Precise folate dosing to avoid U-shaped effects
- HDAC3 targeting: Developing specific inhibitors for vascular aging applications
- Clinical translation: Moving from mechanistic understanding to interventional studies
The NADPH-redox system integrates metabolic, epigenetic, and functional components in vascular aging, offering multiple nodes for therapeutic intervention in age-related cardiovascular diseases.
NADPH Oxidases (NOX) as Critical ROS Generators in Signaling and Disease
Within the field of redox biology, the reduced form of nicotinamide adenine dinucleotide phosphate (NADPH) is a crucial electron donor for anabolic processes and antioxidant defense. A primary consumer of NADPH is the NADPH oxidase (NOX) family of enzymes, whose dedicated function is the regulated generation of reactive oxygen species (ROS) [69] [70]. For decades, ROS were viewed predominantly as toxic byproducts of metabolism; however, the discovery and characterization of the NOX family have cemented the understanding that ROS also function as essential second messengers in cellular signaling [69] [71]. This whitepaper provides an in-depth technical guide to the NOX family, detailing their molecular mechanisms, physiological and pathological roles, associated experimental methodologies, and their emerging promise as therapeutic targets. The critical dependence of NOX enzymes on NADPH, as opposed to the metabolically distinct NADH, firmly positions them as key components in the cellular redox circuitry, integrating metabolic state with redox-dependent signaling outcomes [70] [71].
The NOX Family: Isoforms, Distribution, and Functions
The NOX family comprises seven members in humans: NOX1, NOX2, NOX3, NOX4, NOX5, DUOX1, and DUOX2. These isoforms share a core function of ROS production but differ significantly in their tissue distribution, regulatory mechanisms, and primary biological roles [70] [72] [73]. NOX2 was the first discovered and is best known for its role in the "respiratory burst" in phagocytic cells, where it generates superoxide to destroy pathogens [70] [71]. The other isoforms have since been identified to play diverse parts in processes ranging from hormone synthesis and cellular differentiation to otoconia formation in the inner ear [72].
Table 1: The NOX Family of Enzymes
| Isoform | Main Tissue Distribution | Primary ROS Product | Key Physiological Roles | Regulatory Partners/Mechanisms |
|---|---|---|---|---|
| NOX1 | Colon, Vascular Smooth Muscle | Superoxide (O₂•â») | Host Defense, Cell Proliferation | NOXO1, NOXA1, Rac1 [46] |
| NOX2 | Phagocytes, Endothelium | Superoxide (O₂•â») | Microbial Killing, Innate Immunity | p47phox, p67phox, p40phox, Rac2 [46] [70] |
| NOX3 | Inner Ear | Superoxide (O₂•â») | Biogenesis of Otoconia | p47phox, NOXO1 [70] |
| NOX4 | Kidney, Vasculature, Heart | Hydrogen Peroxide (Hâ‚‚Oâ‚‚) | Oxygen Sensing, Cell Differentiation | p22phox, Poldip2; Constitutively Active [72] |
| NOX5 | Spleen, Testis, Lymphocytes | Superoxide (O₂•â») | Unknown (Not expressed in rodents) | Ca²⺠Binding via EF Hands [72] |
| DUOX1/2 | Thyroid, Respiratory Epithelium | Hydrogen Peroxide (H₂O₂) | Thyroid Hormone Synthesis, Innate Host Defense | DUOXA1/2; Ca²⺠Binding via EF Hands [70] [73] |
A critical concept in NOX biology is that a baseline, normal level of ROS formation supports a wide range of physiological processes, while a disruption in redox balance—caused by either under- or over-production of ROS—is associated with myriad diseases [69]. The NOX enzymes are as distinct in their distribution and activation as they are in their cellular functions, ranging from host defense and post-translational modifications to transcriptional, epigenetic, and cell differentiation effects [69].
Molecular Architecture and Electron Transfer Mechanism
All NOX isoforms are transmembrane proteins that share a common catalytic core. This core consists of a C-terminal cytosolic dehydrogenase (DH) domain that binds FAD and NADPH, and an N-terminal transmembrane (TM) domain containing six alpha-helices [46] [70]. The TM domain chelates two heme groups, positioned orthogonally to the membrane plane, which form an electron transfer chain [46].
The mechanism of electron flow follows a conserved path:
- Two electrons are transferred from NADPH in the DH domain to the FAD cofactor, reducing it to FADHâ‚‚.
- One electron is then shuttled from FADHâ‚‚ to the inner heme group.
- The electron moves sequentially through the inner heme to the outer heme group.
- Finally, the electron is transferred from the outer heme to molecular oxygen (Oâ‚‚) on the extracellular side or within the lumen of an organelle, reducing it to superoxide anion (O₂•â») [46].
Certain isoforms, such as NOX4, DUOX1, and DUOX2, primarily produce hydrogen peroxide (Hâ‚‚Oâ‚‚). This is thought to occur due to an intramolecular dismutation reaction or a two-electron transfer mechanism within the enzyme structure [72]. The recent resolution of cryo-EM structures for DUOX1/2 and other NOX isoforms has provided unprecedented insights into the Oâ‚‚-binding site and the residues critical for this enzymatic activity [46].
Figure 1: NOX Electron Transfer Mechanism. Electrons are transferred from cytosolic NADPH via FAD and two heme groups to reduce oxygen to superoxide.
Physiological and Pathological Roles of NOX-Derived ROS
Physiological Signaling
NOX-derived ROS are now recognized as crucial signaling molecules that mediate their effects through the oxidative post-translational modification of target proteins, including kinases, phosphatases, and transcription factors [69]. Key physiological functions include:
- Innate Immunity: NOX2 in phagocytes is critical for microbial defense. Its activation leads to a massive production of superoxide and secondary ROS like hypochlorous acid within the phagosome, directly destroying engulfed pathogens [70] [73].
- Mechanotransduction: Cells exposed to mechanical forces, such as vascular endothelial cells under shear stress or stretched cardiomyocytes, utilize NOX-derived ROS as signaling messengers. Different patterns of mechanical stress specifically induce and activate different NOX isoforms, linking physical stimuli to biochemical responses [72].
- Hormone Synthesis: DUOX2 in the thyroid gland produces Hâ‚‚Oâ‚‚, which is essential as a substrate for thyroid peroxidase in the synthesis of thyroid hormones [70] [71].
NOX Enzymes in Human Disease
Dysregulation of NOX activity is a common feature in many chronic and acute diseases, making these enzymes attractive therapeutic targets.
- Neurodegenerative Diseases: Overactivation of NOX1, NOX2, and NOX4 in microglia and neurons contributes to oxidative damage, neuroinflammation, and neuronal loss in conditions like Alzheimer's and Parkinson's disease. NOX inhibition has shown promise in pre-clinical models to preserve neuronal integrity [74].
- Cardiovascular and Fibrotic Diseases: NOX1, NOX2, and NOX4 are implicated in vascular dysfunction, hypertension, cardiac remodeling, and fibrotic disorders of the lung, liver, and kidney. The constitutive producer NOX4, in particular, has a complex role, being protective in some contexts (e.g., hypoxic endothelium) and detrimental in others (e.g., rhabdomyolysis-induced kidney injury) [75].
- Cancer: NOX-derived ROS can promote tumor cell proliferation, survival, and invasion. Furthermore, NOX4 in cancer-associated fibroblasts (CAFs) contributes to an immunosuppressive tumor microenvironment [52].
- Chronic Granulomatous Disease (CGD): This rare immunodeficiency is caused by loss-of-function mutations in genes encoding components of the NOX2 complex (e.g., NOX2, p47phox, p22phox). It results in a defective respiratory burst and recurrent, severe infections [70] [71].
Experimental Analysis of NOX Activity and Inhibition
The study of NOX enzymes requires specific methodological approaches to distinguish their activity from other cellular sources of ROS.
Key Methodologies
- Cell-Free Assay Systems: This classical method involves using membrane fractions containing the NOX-p22phox heterodimer and cytosolic fractions containing activator proteins (e.g., p47phox, p67phox). Upon mixing with NADPH, ROS production is measured, allowing for the dissection of individual component requirements [70] [71].
- Comprehensive Inhibitor Screening: A rigorous evaluation of putative NOX inhibitors is essential. This involves a platform of biochemical and biophysical assays to distinguish true enzyme inhibitors from compounds that merely act as ROS scavengers or interfere with the detection assay. For example, Diphenylene iodonium (DPI) inhibits NOXs by forming stable adducts with their FAD and heme prosthetic groups, while VAS2870 and VAS3947 act as covalent inhibitors by alkylating a conserved cysteine residue in the dehydrogenase domain [76].
Table 2: Selected NOX Inhibitors in Research and Development
| Inhibitor Name | Reported Specificity | Proposed Mechanism of Action | Development Stage |
|---|---|---|---|
| Diphenylene Iodonium (DPI) | Broad-spectrum | Reacts with FAD & heme cofactors | Research compound [76] |
| VAS2870 / VAS3947 | Pan-NOX | Covalent alkylation of a cysteine residue | Research compound [76] |
| Setanaxib | NOX1/4 | Selective inhibition | Phase II/III (PBC, IPF, Cancer) [52] |
| APX-115 | Broad-spectrum | Pan-NOX inhibition | Phase II (Diabetic Nephropathy) [52] |
| GKT137831 | NOX1/4 | Dual inhibitor | Pre-clinical/Clinical [75] |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for NOX Research
| Reagent / Tool | Function in NOX Research |
|---|---|
| Cell-Free System (Membrane + Cytosolic fractions) | Reconstitutes NOX activity in vitro to study assembly, kinetics, and regulation [70]. |
| DPI (Diphenylene Iodonium) | A classic, non-specific flavoprotein inhibitor used to implicate NOX/ROS in a process [76]. |
| VAS3947 | A covalent, bona-fide pan-NOX inhibitor with reduced flavoprotein-independent effects vs. DPI [76]. |
| siRNA/shRNA (isoform-specific) | To knock down the expression of specific NOX isoforms or regulatory subunits in cell culture models. |
| Nox-deficient Mouse Models | Genetically modified mice (e.g., Nox2-/-, Nox4-/-) to study isoform-specific functions in vivo [75]. |
| Luminol/Lucigenin Chemiluminescence | Common probes for detecting extracellular superoxide production by activated NOX complexes. |
| Hâ‚‚DCFDA / Amplex Red | Fluorescent probes used to detect intracellular and extracellular Hâ‚‚Oâ‚‚, respectively. |
| FRF-06-057 | FRF-06-057, MF:C19H13N3O3S, MW:363.4 g/mol |
Therapeutic Targeting of NOX Enzymes
The therapeutic landscape for NOX enzymes is bifurcated into two main strategies: inhibition for conditions of overactivity and replacement for deficiency states.
NOX Replacement Therapies: This approach primarily targets Chronic Granulomatous Disease (CGD). Strategies include:
- Gene Therapy: Using lentiviral vectors or CRISPR-based editing to introduce a functional copy of the defective gene (e.g., NOX2) into a patient's hematopoietic stem cells [52].
- mRNA Therapies: Designed to temporarily produce functional NOX subunits to restore immune function [52].
NOX Inhibitor Therapies: The development of isoform-selective or dual-specificity NOX inhibitors is a rapidly advancing field for a wide range of diseases driven by oxidative stress.
- Setanaxib, an oral NOX1/4 inhibitor, is in advanced clinical trials for primary biliary cholangitis (PBC), idiopathic pulmonary fibrosis (IPF), and cancers. It is proposed to reduce inflammation and fibrosis and, in the tumor microenvironment, to target NOX4-expressing CAFs to enhance immune cell infiltration [52].
- APX-115, a first-in-class broad-spectrum NOX inhibitor, is being evaluated for diabetic nephropathy and acute kidney injury, aiming to block oxidative damage in renal tissues [52].
The NOX-targeted therapy market is expected to expand significantly in the coming years, driven by increasing demand for targeted therapies, expanding indications, and ongoing scientific validation [52].
NADPH oxidases stand at the crossroads of metabolism and redox signaling, consuming NADPH to generate precisely localized and regulated ROS signals. Their dual role as essential physiological mediators and drivers of pathology underscores their biological complexity. Continued efforts to unravel their detailed molecular structures and activation mechanisms, coupled with the development of highly selective pharmacological tools, are critical. As research progresses, therapeutic strategies that either augment or suppress NOX activity hold substantial promise for treating a vast spectrum of human diseases, from rare immunodeficiencies to common neurodegenerative, fibrotic, and cardiovascular disorders.
Nicotinamide adenine dinucleotide phosphate (NADPH) serves as a critical electron donor and reducing equivalent in cellular processes, playing a paradoxical role in cancer biology by supporting both redox defense and anabolic biosynthesis. This whitepaper examines NADPH homeostasis within the framework of redox biology, exploring how cancer cells reprogram NADPH metabolism to maintain redox balance while fueling rapid proliferation. We analyze the molecular mechanisms governing NADPH production and consumption, detail experimental methodologies for investigating NADPH dynamics, and discuss emerging therapeutic strategies that target NADPH metabolism. By integrating current research findings with practical experimental approaches, this review provides researchers and drug development professionals with a comprehensive technical guide to NADPH's central role in cancer progression and treatment resistance.
The redox balance within cancer cells represents a critical vulnerability that malignant cells exploit for survival and growth. NADPH stands at the crossroads of redox regulation and metabolic reprogramming, serving as the principal reducing equivalent that powers cellular antioxidant systems while simultaneously providing necessary electrons for biosynthetic pathways. Unlike its catabolic counterpart NADH, which primarily facilitates energy production, NADPH is specifically channeled toward reductive biosynthesis and redox maintenance [15]. This fundamental distinction positions NADPH as a master regulator of the cellular redox state and a key determinant in cancer cell fate.
Cancer cells experience elevated levels of reactive oxygen species (ROS) due to heightened metabolic activity, oncogenic signaling, and mitochondrial dysfunction [77]. While excessive ROS can cause lethal damage to cellular components, moderately elevated ROS functions as critical signaling molecules that promote proliferation, angiogenesis, and metastasis [77]. To survive this self-inflicted oxidative stress, cancer cells become dependent on a hyperactive antioxidant shield primarily orchestrated by NADPH-driven systems, including the glutathione (GSH) and thioredoxin (Trx) systems [77]. This reliance on precisely maintained redox homeostasis creates a therapeutic opportunity to target NADPH metabolism and selectively eliminate malignant cells.
The intricate relationship between NADPH and cancer extends beyond redox defense to encompass the biosynthetic demands of rapidly proliferating cells. NADPH provides essential reducing power for multiple anabolic pathways, including fatty acid synthesis, nucleotide production, and cholesterol biosynthesis [15]. The reprogramming of NADPH metabolism in cancer represents a fascinating adaptation that illustrates the metabolic flexibility of tumor cells and their ability to coordinate redox balance with biosynthetic requirements. Understanding these dynamics within the broader context of NADH/NADPH redox biology provides critical insights for developing novel cancer therapeutics.
Biological Functions of NADPH in Cancer Cells
Antioxidative Defense Systems
NADPH serves as the primary reducing agent for maintaining cellular antioxidant capacity, directly impacting cancer cell survival under conditions of oxidative stress. The glutathione and thioredoxin systems represent the two major NADPH-dependent antioxidant mechanisms in cancer cells:
Glutathione System: Glutathione reductase (GR) utilizes NADPH as an electron donor to regenerate reduced glutathione (GSH) from its oxidized form (GSSG) [15]. GSH then acts as a co-substrate for glutathione peroxidase (GPX), which reduces hydrogen peroxide (H2O2) and lipid hydroperoxides to water and alcohols, respectively [78] [15]. The GPX family consists of eight members (GPX1-GPX8) that collectively mitigate oxidative stress and maintain redox homeostasis [78].
Thioredoxin System: Thioredoxin reductase (TRXR) consumes NADPH to maintain thioredoxin (TRX) in its reduced form, which contributes to scavenging H2O2 and reducing ribonucleotide reductase (RNR) for DNA synthesis [15]. Additionally, NADPH can bind to and reactivate catalase when it has been inactivated by H2O2, further enhancing the antioxidant defense mechanism in some cell types [15].
The critical importance of these systems is evidenced by the dependence of cancer cells on NADPH for survival. To sustain their hyperactive antioxidant defenses, tumor cells typically maintain high levels of NADPH, creating a potential vulnerability that can be exploited therapeutically [15].
Reductive Biosynthesis
Beyond its role in antioxidant defense, NADPH serves as an essential electron donor for anabolic pathways that support rapid tumor growth:
Fatty Acid Synthesis: NADPH provides reducing equivalents for fatty acid synthase (FASN), the main rate-limiting enzyme in fatty acid synthesis, which uses acetyl-CoA as a primer and malonyl-CoA as a two-carbon donor [15].
Nucleotide Synthesis: NADPH is required for dihydrofolate reductase (DHFR) to catalyze the reduction of dihydrofolate to tetrahydrofolate (THF) in folate metabolism, which is essential for de novo biosynthesis of thymidylate, purines, and some amino acids [15].
Cholesterol and Steroid Synthesis: NADPH acts as the reducing reagent for 3-hydroxy-3-methylglutaryl-coenzyme A reductase (HMGCR), the rate-limiting enzyme of the mevalonate pathway that leads to cholesterol and nonsterol isoprenoid synthesis [15].
Amino Acid Metabolism: NADPH provides needed electrons for iron-sulfur (Fe/S) protein assembly that participates in non-essential amino acid biosynthesis and lipoic acid synthesis [15].
The dual utilization of NADPH for both redox defense and biosynthetic processes creates metabolic competition within cancer cells, necessitating sophisticated regulatory mechanisms to allocate NADPH according to cellular priorities.
Free Radical Generation
Paradoxically, while NADPH is crucial for antioxidant defense, it also serves as a substrate for NADPH oxidases (NOX) that generate free radicals. NOX enzymes (NOX1-5 and dual oxidases DUOX1-2) catalyze the production of superoxide anions or H2O2 from NADPH and oxygen [15]. These NOX-derived ROS function as signaling molecules that regulate various redox-sensitive pathways involved in cancer progression by stimulating oncogenes such as Src and Ras, while inactivating tumor suppressor proteins including TP53 and PTEN [15].
Table 1: NADPH-Dependent Biological Functions in Cancer Cells
| Function Category | Specific Processes | Key Enzymes/Systems | NADPH Role |
|---|---|---|---|
| Antioxidant Defense | ROS detoxification | Glutathione system (GR, GPX) | Regenerate GSH from GSSG |
| ROS scavenging | Thioredoxin system (TRXR, TRX) | Maintain reduced thioredoxin | |
| H2O2 decomposition | Catalase | Reactivate catalase after H2O2 inactivation | |
| Reductive Biosynthesis | Fatty acid synthesis | Fatty acid synthase (FASN) | Provide reducing equivalents |
| Nucleotide synthesis | Dihydrofolate reductase (DHFR) | Reduce dihydrofolate to THF | |
| Cholesterol synthesis | HMGCR | Rate-limiting step in mevalonate pathway | |
| Amino acid metabolism | Iron-sulfur protein assembly | Electron donation for biosynthesis | |
| Free Radical Generation | Redox signaling | NADPH oxidases (NOX1-5, DUOX1-2) | Substrate for superoxide/H2O2 production |
Molecular Mechanisms Regulating NADPH Homeostasis
NADPH Production Pathways
Cancer cells employ multiple metabolic routes to maintain NADPH homeostasis, with different pathways contributing variably depending on cancer type and context:
Pentose Phosphate Pathway (PPP): The PPP serves as the largest contributor of cytosolic NADPH, with NADPH generation occurring through three irreversible reactions in the oxidative branch [15]. Glucose-6-phosphate dehydrogenase (G6PD) catalyzes the first and rate-limiting step, dehydrogenating glucose-6-phosphate to yield 6-phosphogluconolactone and NADPH [15]. Subsequently, 6-phosphogluconate dehydrogenase (PGD) catalyzes the oxidative decarboxylation of 6-phosphogluconate to synthesize ribulose-5-phosphate and a second molecule of NADPH [15]. G6PD activity is frequently increased in various cancers, including bladder, breast, prostate, and gastric cancers, compared with normal tissues [15].
Foliate-Mediated One-Carbon Metabolism: This pathway represents a major source of NADPH, particularly in rapidly proliferating cells [15]. The mitochondrial folate cycle generates NADPH through the activity of methylenetetrahydrofolate dehydrogenase (MTHFD) enzymes [79]. Serine metabolism couples de novo nucleotide synthesis with glutathione production, highlighting its connection to redox homeostasis [79].
Malic Enzymes (ME): The NADP+-dependent malic enzymes (ME1 in cytosol and ME3 in mitochondria) catalyze the oxidative decarboxylation of malate to pyruvate, generating NADPH in the process [15]. These enzymes provide an important link between the TCA cycle and NADPH production.
Isocitrate Dehydrogenases (IDH1/2): Cytosolic IDH1 and mitochondrial IDH2 catalyze the oxidative decarboxylation of isocitrate to α-ketoglutarate, producing NADPH [15]. Mutations in IDH1/2 occur in several cancer types and result in the production of the oncometabolite 2-hydroxyglutarate while altering NADPH production.
Nicotinamide Nucleotide Transhydrogenase (NNT): Located in the mitochondrial inner membrane, NNT catalyzes the reversible reduction of NADP+ by NADH, coupled to proton translocation across the membrane [15]. This enzyme represents an important mechanism for maintaining mitochondrial NADPH pools.
NAD Kinases (NADK): NADKs catalyze the phosphorylation of NAD+ to form NADP+, the precursor to NADPH [15]. Both cytosolic (cNADK) and mitochondrial (mNADK) isoforms exist, with cNADK frequently overexpressed in multiple tumor types [15]. A novel cNADK mutant (NADK-I90F) found in pancreatic ductal adenocarcinoma exhibits increased enzyme activity, leading to elevated NADPH levels and reduced ROS [15].
Table 2: Major NADPH Production Pathways in Cancer Cells
| Pathway | Subcellular Location | Key Enzymes | Contribution to NADPH Pool | Cancer Types with Frequent Alterations |
|---|---|---|---|---|
| Pentose Phosphate Pathway | Cytosol | G6PD, PGD | High (largest contributor in cytosol) | Bladder, breast, prostate, gastric cancers |
| Foliate-Mediated One-Carbon Metabolism | Mitochondria, Cytosol | MTHFD1L, MTHFD2 | Moderate to High | Colon cancer, acute myeloid leukemia |
| Malic Enzymes | Cytosol (ME1), Mitochondria (ME3) | ME1, ME3 | Moderate | Breast cancer, pancreatic ductal adenocarcinoma |
| Isocitrate Dehydrogenases | Cytosol (IDH1), Mitochondria (IDH2) | IDH1, IDH2 | Moderate | Gliomas, acute myeloid leukemia (mutant forms) |
| Nicotinamide Nucleotide Transhydrogenase | Mitochondria | NNT | Context-dependent | Various cancers |
| NAD Kinases | Cytosol, Mitochondria | cNADK, mNADK | Foundational (produces NADP+ precursor) | Pancreatic ductal adenocarcinoma, diffuse large B-cell lymphoma |
NADPH Consumption Pathways
The regulation of NADPH homeostasis involves not only production but also controlled consumption through various enzymatic systems:
Antioxidant Systems: The glutathione and thioredoxin systems represent the primary consumers of NADPH for redox maintenance. Glutathione reductase and thioredoxin reductase continuously utilize NADPH to maintain their respective redox buffers in reduced states [15].
Biosynthetic Enzymes: Multiple anabolic enzymes compete for NADPH pools, including fatty acid synthase, dihydrofolate reductase, and HMG-CoA reductase [15]. The relative activity of these pathways depends on the specific biosynthetic requirements of the cancer cell.
NADPH Oxidases: NOX family enzymes consume NADPH to generate superoxide and hydrogen peroxide, which function as signaling molecules [15]. NOX4, in particular, has been identified as a key source of ROS in various cancers and is frequently upregulated in tumors [80] [81].
Cytochrome P450 Reductase: This enzyme utilizes NADPH for drug metabolism, xenobiotic detoxification, and steroid hormone synthesis [15].
The balance between NADPH production and consumption must be precisely regulated to maintain redox homeostasis while supporting anabolic processes. Cancer cells develop unique dependencies on specific NADPH production pathways based on their tissue of origin, oncogenic drivers, and microenvironmental context.
Diagram 1: NADPH Homeostasis Regulation in Cancer Cells. This diagram illustrates the major production and consumption pathways that maintain NADPH balance in cancer cells, highlighting the metabolic nodes that can be targeted therapeutically. (Title: NADPH Homeostasis Regulation)
Therapeutic Targeting of NADPH Metabolism
Pro-oxidant Therapies
The reliance of cancer cells on NADPH-dependent antioxidant systems creates a vulnerability that can be exploited through pro-oxidant therapies designed to overwhelm cellular defenses:
High-Dose Vitamin C: Pharmacological concentrations of ascorbate generate hydrogen peroxide through autoxidation, selectively targeting cancer cells with compromised antioxidant capacity [77]. The resulting oxidative stress induces lethal damage when it exceeds the buffering capacity of NADPH-dependent systems.
Arsenic Trioxide (ATO): This agent promotes ROS accumulation and has shown significant tumor-selective toxicity, particularly in hematological malignancies [77]. ATO efficacy is enhanced in cells with limited NADPH regeneration capacity.
Redox-Active Metal Complexes: Manganese porphyrins and other redox-active metal complexes strategically leverage the differential redox state of normal versus cancer cells through both pro-oxidant and indirect Nrf2-mediated antioxidative mechanisms [77]. Several such agents are currently in advanced clinical trials.
Targeting NADPH-Regenerating Enzymes
Inhibiting NADPH production pathways represents a promising therapeutic strategy:
G6PD Inhibitors: Targeting the rate-limiting enzyme of the PPP disrupts the primary source of cytosolic NADPH, impairing both redox defense and nucleotide synthesis [15]. However, developing specific G6PD inhibitors with acceptable therapeutic indices has proven challenging.
NADK Inhibition: Silencing cNADK with shRNA impairs the NADPH pool and suppresses cancer cell growth in diffuse large B-cell lymphoma and colon cancer models [15]. The identification of NADK-I90F mutant in pancreatic cancer suggests a potential biomarker for patient selection.
MTHFD2 Inhibition: Targeting the mitochondrial folate pathway enzyme MTHFD2 disrupts NADPH production in cancer cells while sparing normal cells, showing promise in preclinical models [79].
Targeting Antioxidant Systems
Direct inhibition of NADPH-dependent antioxidant systems can disrupt redox homeostasis:
Nrf2 Inhibitors: The master regulator of antioxidant response Nrf2 can be targeted with compounds such as Brusatol or ML385, which disrupt the core antioxidant response and sensitize cancer cells to oxidative stress [77].
Glutathione System Disruption: Inhibiting cysteine uptake with sulfasalazine or erastin potently induces ferroptosis, a non-apoptotic cell death driven by lipid peroxidation [77]. This approach exploits the dependence of GPX4 on glutathione for its antioxidant function.
Thioredoxin System Inhibition: The repurposed drug auranofin irreversibly inhibits thioredoxin reductase (TrxR), disrupting this key NADPH-dependent antioxidant system [77].
Targeting NOX4
NOX4 has emerged as a promising therapeutic target across multiple cancer types:
NOX4 Inhibitors: Setanaxib, a NOX4/1 inhibitor, can effectively reverse cancer-associated fibroblast (CAF) differentiation, significantly promote infiltration of CD8+ T cells into tumors, and enhance immunotherapy efficacy [80] [81]. In breast cancer models, NOX4 downregulation inhibits proliferation and metastasis [80].
Combination Strategies: Setanaxib synergistically inhibits tumor cell proliferation and promotes apoptosis when combined with gefitinib, and potentiates immunotherapy by overcoming CAF-mediated CD8+ T-cell exclusion [81].
Table 3: Therapeutic Strategies Targeting NADPH Metabolism
| Therapeutic Approach | Specific Agents/Targets | Mechanism of Action | Development Stage |
|---|---|---|---|
| Pro-oxidant Therapies | High-dose vitamin C, Arsenic trioxide | Overwhelm antioxidant defenses by increasing ROS | Clinical trials |
| Redox-Active Metal Complexes | Manganese porphyrins | Leverage differential redox states via pro-oxidant/Nrf2 mechanisms | Advanced clinical trials |
| NADPH Production Inhibition | G6PD inhibitors, NADK inhibitors, MTHFD2 inhibitors | Reduce NADPH regeneration capacity | Preclinical to early clinical |
| Antioxidant System Disruption | Nrf2 inhibitors (Brusatol, ML385) | Disrupt master regulator of antioxidant response | Preclinical |
| Ferroptosis Induction | Cysteine uptake inhibitors (sulfasalazine, erastin) | Induce glutathione depletion and lipid peroxidation | Preclinical to clinical |
| Thioredoxin Inhibition | Auranofin | Irreversibly inhibit thioredoxin reductase | Repurposed drug, clinical trials |
| NOX4 Inhibition | Setanaxib | Inhibit ROS-producing enzyme, modulate TME | Clinical trials |
Experimental Methods for NADPH Research
Optical Redox Imaging (ORI)
Optical redox imaging provides a non-invasive method for monitoring NADH redox status in live cells and tissues:
Principle: ORI detects intrinsic fluorescence from NADH and oxidized flavoproteins (Fp) containing flavin adenine dinucleotide (FAD) [82]. The optical redox ratio (ORR), calculated as Fp/(NADH + Fp) or FAD/(NADH + FAD), correlates with NAD+/(NADH + NAD+) and reflects bioenergetic activities [82].
Methodology: Cells are seeded in glass-bottom dishes and imaged using a wide-field fluorescence microscope with appropriate filter sets: NADH excitation 370-400 nm, emission 414-450 nm; Fp excitation 450-488 nm, emission 500-530 nm [82]. Images are acquired from multiple random fields per dish, with experiments repeated on separate days for biological replication.
Applications: ORI has been used to detect associations between more oxidized NADH redox status and cancer aggressiveness [82]. In triple-negative breast cancer cell lines, more invasive MDA-MB-231 cells exhibit more oxidized NADH redox status and higher cytoplasmic ROS levels than less invasive HCC1806 cells, regardless of passage number [82].
Genetic Manipulation of NADPH-Related Genes
RNA interference and CRISPR-Cas9 systems enable targeted manipulation of NADPH metabolism:
Protocol for NOX4 Knockdown: Pan-cancer analyses have validated NOX4 as a therapeutic target through in vitro loss-of-function experiments [80] [81]. Following NOX4 downregulation using siRNA or shRNA, functional assays including Wound healing, Transwell, and CCK-8 assays are conducted to assess proliferation, migration, and invasion capabilities [80].
Validation Methods: Successful genetic manipulation is confirmed through RT-PCR for mRNA expression and immunohistochemistry for protein expression [83]. Primers for NOX4 detection include: Forward: 5'-GTG TCT AAG CAG AGC CTC AGC ATC-3', Reverse: 5'-CGG AGG TAA GCC AAG AGT GTT CG-3' [83].
Metabolic Flux Analysis
Stable isotope tracing coupled with mass spectrometry enables quantitative analysis of NADPH production pathways:
Isotope Labeling: Cells are cultured with [1,2-13C]glucose or [U-13C]glutamine to track carbon flow through NADPH-producing pathways such as the PPP, TCA cycle, and folate metabolism [79].
Mass Spectrometry Analysis: LC-MS/MS is used to measure isotope enrichment in metabolites, allowing calculation of relative contributions of different pathways to NADPH production [79].
Data Interpretation: The contribution of the oxidative PPP to NADPH production is assessed by comparing M+2 labeling patterns in glycolytic and pentose phosphate pathway intermediates [79].
Diagram 2: Experimental Workflow for NADPH Research. This diagram outlines a comprehensive experimental approach for investigating NADPH metabolism in cancer models, integrating redox assessment, genetic manipulation, and functional analysis. (Title: NADPH Research Workflow)
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for NADPH Studies
| Reagent Category | Specific Examples | Application/Function | Key Considerations |
|---|---|---|---|
| NADPH Detection | NADP/NADPH-Glo Assay | Quantify NADPH levels in cell extracts | Distinguishes NADPH from NADH |
| SoNar sensor | Live-cell imaging of NADPH/NADP+ ratio | Genetically encoded biosensor | |
| ROS Detection | DCFDA/H2DCFDA | General cellular ROS detection | Measures primarily H2O2 |
| MitoSOX Red | Mitochondrial superoxide detection | Targeted to mitochondria | |
| Antioxidant Inhibitors | Auranofin | Thioredoxin reductase inhibitor | Also affects other selenoproteins |
| BSO (buthionine sulfoximine) | Glutathione synthesis inhibitor | Depletes cellular GSH pools | |
| NADPH Production Inhibitors | 6-AN (6-aminonicotinamide) | G6PD inhibitor | Non-specific at higher concentrations |
| ME1 inhibitors | Malic enzyme 1 inhibitors | Emerging chemical tools | |
| Genetic Manipulation | siRNA/shRNA against NOX4 | Knockdown NOX4 expression | Validate with multiple constructs |
| CRISPR-Cas9 for IDH1/2 | Gene knockout or mutation | Model specific cancer mutations | |
| Metabolic Tracers | [1,2-13C]glucose | PPP flux measurement | Enables M+2 labeling pattern analysis |
| [U-13C]glutamine | TCA cycle and reductive carboxylation | Assess alternative NADPH pathways |
The dual role of NADPH in supporting both redox defense and biosynthetic processes represents a fundamental aspect of cancer metabolism that offers promising therapeutic opportunities. As research in this field advances, several key areas warrant further investigation:
First, the contextual dependencies of different NADPH production pathways need better characterization across cancer types and states. While the PPP is generally considered the major contributor to cytosolic NADPH, the relative importance of alternative routes varies significantly based on genetic background, tissue of origin, and microenvironmental factors [15] [79]. Understanding these nuances will be essential for developing targeted therapies that exploit specific metabolic vulnerabilities.
Second, the dynamic regulation of NADPH allocation between competing cellular processes remains poorly understood. How cancer cells prioritize NADPH utilization under conditions of nutrient limitation, oxidative stress, or during the metastatic cascade represents a critical area for future research [77] [79]. Advanced imaging techniques and real-time metabolic sensors will help elucidate these regulatory mechanisms.
Finally, the integration of NADPH-targeting approaches with conventional therapies and immunotherapies holds significant promise. Preclinical evidence suggests that modulating NADPH metabolism can enhance the efficacy of both chemotherapy and immunotherapy [80] [81]. As selective inhibitors of NADPH-metabolizing enzymes continue to develop, their rational combination with established treatment modalities may yield improved outcomes for cancer patients.
In conclusion, NADPH sits at the nexus of cancer redox biology and metabolic reprogramming, serving competing yet essential functions that maintain redox homeostasis while supporting anabolic growth. Targeting this delicate balance offers a promising avenue for selective cancer therapy that merits continued investigation within the broader context of NADH/NADPH redox biology research.
Nicotinamide adenine dinucleotide phosphate (NADPH) and its oxidized form, NADP+, represent essential redox couples that play a critical role in maintaining cellular homeostasis. Within the context of redox biology research, NADPH serves as the principal electron donor in reductive biosynthesis and antioxidant defense systems, while NADH primarily functions as a key electron carrier in mitochondrial energy production [84]. This fundamental metabolic division establishes NADPH as a crucial regulator of cellular redox state, with its depletion leading to impaired antioxidant capacity and increased susceptibility to oxidative stress-related pathologies. The NADPH pool is compartmentalized within subcellular organelles, with independent regulation in the cytosol and mitochondria creating distinct metabolic microenvironments that influence specialized cellular functions [85]. The balance between NADPH and NADH systems has emerged as a critical factor in health and disease, with dysregulation contributing to numerous pathological conditions including cancer, neurodegenerative diseases, cardiovascular disorders, and aging-related pathologies.
The enzymatic source of NADP+, the direct precursor for NADPH synthesis, is NAD kinase (NADK), which catalyzes the phosphorylation of NAD+ to NADP+ [86]. This reaction positions NADK as a master metabolic regulator controlling substrate availability for all NADPH-producing enzymes. Recent research has unveiled the therapeutic potential of targeting NADPH-generating enzymes, particularly NADK, for modulating redox balance in various disease contexts. This whitepaper provides a comprehensive technical guide to the current understanding of NADPH metabolism, with emphasis on NADK and associated enzymes as promising targets for therapeutic optimization in redox-related diseases.
The NADPH Metabolic Network
Cellular NADPH is generated through multiple complementary metabolic pathways that function in a compartment-specific manner. The major NADPH-producing systems include:
- Pentose Phosphate Pathway (PPP): The oxidative branch of PPP, catalyzed by glucose-6-phosphate dehydrogenase (G6PD) and 6-phosphogluconate dehydrogenase (6PGD), represents the primary cytosolic source of NADPH [85]. This pathway directly links glucose metabolism to NADPH production and is particularly important in rapidly dividing cells and those facing significant oxidative stress.
- Malic Enzyme (ME1): Cytosolic malic enzyme generates NADPH through the oxidative decarboxylation of malate to pyruvate, connecting the tricarboxylic acid (TCA) cycle with NADPH production [86].
- Folate Metabolism: Methylenetetrahydrofolate dehydrogenase (MTHFD) in folate metabolism represents another significant source of cytosolic NADPH, particularly in endothelial cells [85].
- Mitochondrial NADPH Generation: Mitochondrial NADPH is primarily produced by NAD+ kinase 2 (NADK2), which phosphorylates NAD+ to NADP+ within mitochondria [87]. Additional mitochondrial sources include nicotinamide nucleotide transhydrogenase (NNT), isocitrate dehydrogenase 2 (IDH2), and mitochondrial malic enzyme (ME3) [86].
The compartmentalization of these NADPH pools creates distinct redox environments that regulate specialized cellular processes, from antioxidant defense in the cytosol to lipoic acid synthesis and oxidative metabolism in mitochondria [87] [85].
NAD Kinase (NADK): The Master Regulator
NADK exists in two primary isoforms with distinct subcellular localizations and functions:
- Cytosolic NADK (NADK1): This isoform represents the primary enzyme responsible for generating the cytosolic NADP+ pool [86]. It catalyzes the ATP-dependent phosphorylation of NAD+ to NADP+, controlling substrate availability for all cytosolic NADPH-producing enzymes. Structural studies using cryo-electron microscopy have revealed that human NADK adopts a tetrameric architecture with N- and C-terminal extensions acting as opposing regulatory elements [88].
- Mitochondrial NADK (NADK2): Located within mitochondria, NADK2 phosphorylates NAD+ to NADP+ using ATP, establishing the mitochondrial NADP+ pool essential for mitochondrial NADPH-dependent processes [87]. Recent research demonstrates that NADK2 is critical for maintaining protein lipoylation through supporting mitochondrial fatty acid synthesis (mtFAS), which is necessary for optimal activity of key mitochondrial enzyme complexes including the pyruvate dehydrogenase complex [87].
Table 1: NADK Isoforms and Characteristics
| Parameter | NADK1 (Cytosolic) | NADK2 (Mitochondrial) |
|---|---|---|
| Subcellular Location | Cytosol | Mitochondrial matrix |
| Primary Function | Maintain cytosolic NADP+ pool | Maintain mitochondrial NADP+ pool |
| Key Metabolic Roles | Redox defense, Ferroptosis regulation, Biosynthesis | Protein lipoylation, Oxidative metabolism, mtFAS |
| Structural Features | Tetrameric architecture with regulatory N- and C-terminal extensions [88] | Dimeric organization, regulated by lysine acetylation [88] |
| Associated Diseases | Cancer, Ferroptosis-related pathologies | Dienoyl-CoA reductase deficiency, Metabolic disorders |
Quantitative Analysis of NADP(H) Metabolism
Physiological NADP(H) Levels Across Tissues
A comprehensive meta-analysis of NAD(P)(H) quantification across mammalian tissues has revealed significant variability in measurements, reflecting differences in methodologies, pre-analytical conditions, and interspecies variation [89]. This variability highlights the critical importance of standardized protocols for NADP(H) quantification in both preclinical and clinical studies.
Table 2: NADP(H) Concentrations in Selected Mammalian Tissues
| Tissue | Species | NADP+ (nmol/g) | NADPH (nmol/g) | NADPH/NADP+ Ratio | Measurement Method |
|---|---|---|---|---|---|
| Liver | Mouse | 50-120 | 150-300 | 1.5-3.0 | LC-MS/Enzyme cycling |
| Brain | Rat | 20-50 | 60-120 | 2.0-3.5 | LC-MS/Enzyme cycling |
| Kidney | Human | 30-80 | 100-200 | 2.5-4.0 | LC-MS/HPLC |
| Muscle | Mouse | 10-30 | 40-80 | 3.0-4.5 | Enzyme cycling |
| Blood | Human | 5-15 | 20-50 | 3.0-5.0 | LC-MS/Enzyme cycling |
Note: Ranges represent compiled data from multiple studies; actual values depend on specific experimental conditions and methodologies [89].
Methodological Considerations for NADP(H) Quantification
Accurate measurement of NADP(H) metabolites requires careful attention to pre-analytical conditions and methodological selection:
- Sample Processing: Rapid enzyme inactivation is essential, typically achieved through freeze-clamping or immediate immersion in cold organic solvents (acetonitrile, methanol) [89]. Acidic extraction with perchloric acid is suitable for oxidized forms but can degrade reduced NADPH.
- Quantification Methods:
- Enzyme Cycling Assays: Employ spectrophotometric or fluorometric detection; widely used but susceptible to interference (46.7% of recent studies) [89].
- Liquid Chromatography-Mass Spectrometry (LC-MS): Provides superior specificity and sensitivity; allows multiplexed metabolite quantification (13.2% of studies) [89].
- Genetically Encoded Sensors: Enable real-time monitoring of compartmentalized NADPH dynamics in live cells (e.g., iNap sensors) [85].
Experimental Models and Methodologies
Establishing NADK-Ferroptosis Relationships
The role of NADK in regulating ferroptosis susceptibility has been systematically investigated using complementary experimental approaches:
Pharmacological Inhibition
- Compound: Thionicotinamide (thioNAM) serves as a specific NADK inhibitor [86].
- Protocol: HT1080 cells are treated with thioNAM (concentration range: 10-100 μM) for 24-48 hours prior to induction of ferroptosis with RSL-3 (1-10 μM) [86].
- Validation: NADP(H) depletion confirmed via LC-MS or enzymatic cycling assays; ferroptosis specificity controlled with Ferrostatin-1 (1-10 μM) co-treatment [86].
Genetic Manipulation
- Knockdown Approaches: siRNA-mediated silencing of NADK using sequence 5′-GGA GAA CAT GAT CGT GTA T-3′ with Lipofectamine 3000 transfection reagent [86].
- Overexpression Studies: Plasmid-driven NADK expression to rescue NADPH levels and ferroptosis phenotype [86].
- Efficiency Validation: Western blot analysis and qRT-PCR performed 24-48 hours post-transfection to confirm modulation of NADK expression [86].
Metabolic Rescue Experiments
- NAD+ Precursor Supplementation: Nicotinamide mononucleotide (NMN) administered at 0.5-2 mM to test NAD+ salvage pathway engagement [86].
- Pathway-Specific Interventions: Concurrent modulation of G6PD or ME1 expression to map metabolic interactions with NADK [86].
Monitoring Compartmentalized NADPH Dynamics
Real-time assessment of subcellular NADPH dynamics employs genetically encoded sensors:
Sensor Expression and Calibration
- Sensor Variants: Cytosolic iNap1 (cyto-iNap1) and mitochondrial iNap3 (mito-iNap3) targeted to respective compartments [85].
- Calibration Protocol:
- Permeabilize plasma membrane (0.001% digitonin) or mitochondrial inner membrane (0.3% digitonin)
- Expose to NADPH concentration gradient (0-500 μM)
- Measure fluorescence ratio (405/488 nm or 420/485 nm excitation) [85]
- Specificity Controls: Employ non-responsive iNapc variant to control for non-specific effects [85].
Experimental Applications
- Senescence Models: Angiotensin II (2 μM, 72 hours), high glucose (25 mM, 48 hours), replicative senescence [85].
- Pharmacological Screening: iNap-enabled high-throughput screening of 1419 FDA-approved drugs identified folic acid as NADPH modulator [85].
Research Reagent Solutions Toolkit
Table 3: Essential Research Reagents for NADPH/NADK Investigations
| Reagent/Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| NADK Inhibitors | Thionicotinamide (thioNAM) | Pharmacological NADK inhibition | Dose-dependent NADP(H) depletion; 10-100 μM range [86] |
| Genetic Tools | NADK siRNA (5′-GGA GAA CAT GAT CGT GTA T-3′) | Gene silencing | Lipofectamine 3000 transfection; validate with WB/qRT-PCR [86] |
| NADK overexpression plasmids | Functional rescue studies | Test multiple constructs for efficacy [86] | |
| NAD+ Precursors | Nicotinamide Mononucleotide (NMN) | Boost NAD+ salvage pathway | 0.5-2 mM concentration; enhances NADK substrate availability [86] |
| Ferroptosis Modulators | RSL-3 | GPX4 inhibition; ferroptosis induction | 1-10 μM range; use with Ferrostatin-1 controls [86] |
| Ferrostatin-1 | Ferroptosis inhibitor | 1-10 μM; confirms ferroptosis specificity [86] | |
| NADPH Sensors | iNap1, iNap3 | Compartmentalized NADPH monitoring | Requires proper subcellular targeting and calibration [85] |
| Activity Assays | G6PD activity kits | PPP flux assessment | Coupled enzymatic assays; monitor 340 nm absorbance [85] |
| GSH/GSSG detection kits | Redox status assessment | Fluorometric or colorimetric detection [90] [86] |
Pathway Visualization and Experimental Workflows
NADPH Metabolism and Ferroptosis Regulation Pathway
NADPH-Ferroptosis Regulatory Axis
Experimental Workflow for NADK Functional Analysis
NADK Functional Analysis Workflow
Therapeutic Targeting Strategies and Clinical Outlook
NADK as a Therapeutic Target
Emerging evidence positions NADK as a promising therapeutic target for multiple disease contexts:
- Cancer Therapy: NADK inhibition depletes NADPH pools essential for cancer cell proliferation, redox balance, and anabolic processes [86] [88]. The recent resolution of NADK's high-resolution structure via cryo-EM provides a structural framework for rational inhibitor design [88].
- Neurodegenerative Diseases: In Alzheimer's disease models, NADK activation promotes NADPH production and neuronal protection against ferroptosis [90]. Schisandra total lignans (STL) demonstrate neuroprotection via NADK activation, with Gomisin D identified as the key component binding NADK [90].
- Vascular Aging: Compartment-specific NADK modulation offers potential for addressing endothelial senescence, with cytosolic NADPH elevation showing protective effects in aged vasculature [85].
Compartment-Specific Therapeutic Approaches
The independent regulation of NADPH pools in cellular compartments enables targeted therapeutic strategies:
- Cytosolic Targeting: Interventions focusing on NADK1 or cytosolic NADPH-producing enzymes (G6PD, ME1) particularly benefit conditions involving oxidative stress and ferroptosis [86] [85].
- Mitochondrial Targeting: NADK2 modulation affects fundamental mitochondrial processes including fatty acid synthesis, protein lipoylation, and oxidative metabolism [87]. This approach holds promise for mitochondrial disorders and energy metabolism-related conditions.
Clinical Translation and Drug Development
Several compounds targeting NADPH metabolism have advanced in preclinical development:
- Natural Products: Schisandra lignans, particularly Gomisin D, show NADK-activating properties with potential application in neurodegenerative diseases [90].
- Repurposed Drugs: High-throughput screening identified folic acid as an NADPH-elevating compound via MTHFD1, showing efficacy in vascular aging models [85].
- Novel Inhibitors: Structure-based drug design leveraging NADK structural information promises more specific and potent inhibitors for oncology applications [88].
The continued elucidation of NADPH metabolism and NADK regulation will undoubtedly yield novel therapeutic opportunities for addressing the growing burden of redox-related diseases in aging populations.
Comparative Biology and Therapeutic Validation of Redox-Targeting Agents
Nicotinamide adenine dinucleotide phosphate (NADPH) is an essential electron donor responsible for maintaining cellular redox homeostasis and supporting reductive biosynthesis. Its homeostasis is regulated by varied signaling pathways and several metabolic enzymes that undergo adaptive alteration in cancer cells [15]. The metabolic reprogramming of NADPH renders cancer cells both highly dependent on this metabolic network for antioxidant capacity and more susceptible to oxidative stress, presenting a unique therapeutic vulnerability [15]. This review provides a comparative analysis of NADPH metabolism between cancer and non-cancer cells, examining the distinct biological functions, regulatory mechanisms, and therapeutic implications within the broader context of redox biology.
Biological Functions of NADPH: A Comparative Perspective
Antioxidant Defense Systems
In both cancer and non-cancer cells, NADPH is crucial for combating oxidative stress; however, the demand and regulation of this function differ substantially. Cancer cells typically exhibit elevated levels of reactive oxygen species (ROS) due to their high metabolic rates and proliferative state. To prevent excessive oxidative stress that can induce cytotoxicity and lead to DNA damage and cell apoptosis, tumor cells strategically adjust multiple antioxidant enzymes and molecules dependent on NADPH generation [15].
Table 1: Comparative Analysis of NADPH-Dependent Antioxidant Pathways
| Pathway/Component | Role in Non-Cancer Cells | Adaptation in Cancer Cells |
|---|---|---|
| Glutathione System | Maintains basal redox homeostasis | Enhanced utilization to counteract elevated ROS from rapid proliferation |
| Thioredoxin System | Supports regular protein redox regulation | Upregulated to maintain redox balance despite metabolic stress |
| Catalase Reactivation | Standard Hâ‚‚Oâ‚‚ clearance | Increased demand due to higher ROS production in tumor microenvironment |
Non-cancer cells maintain appropriate NADPH levels for routine cellular functions and stress response. For instance, in vascular endothelial cells, NADPH metabolism plays a critical role in combating age-related oxidative stress [30]. Conversely, cancer cells maintain persistently high NADPH levels not only for robust redox defense but also to fuel biosynthetic reactions that sustain rapid growth [15]. This heightened dependency creates a metabolic vulnerability that can be therapeutically exploited.
Reductive Biosynthesis
NADPH provides reducing equivalents for essential anabolic processes, but the scale and pathway preferences differ markedly between normal and cancerous cells:
- Lipid Synthesis: Non-cancer cells regulate lipogenesis according to physiological needs, while cancer cells exhibit enhanced de novo lipogenesis to support membrane biogenesis for rapid proliferation [91] [92]. Enzymes such as fatty acid synthase (FASN) are overexpressed in cancers like non-small cell lung cancer (NSCLC) [92].
- Nucleotide Production: Normal cells utilize NADPH-dependent pathways for regulated nucleotide synthesis, whereas cancer cells dramatically upregulate these pathways to meet the demands of continuous proliferation [91].
- Amino Acid Metabolism: Both cell types require NADPH for amino acid synthesis, but cancer cells increase transport and metabolism of amino acids like glutamine to support biomass accumulation [91].
NADPH Oxidases and Redox Signaling
NADPH oxidases (NOXs) represent a specialized family of enzymes that consume NADPH to generate controlled levels of reactive oxygen species for signaling purposes [69]. In non-cancer cells, NOX-derived ROS function as second messengers in physiological signaling pathways. In cancer cells, NOX-mediated ROS specifically regulate various redox-sensitive signaling pathways involved in cancer progression by stimulating oncogenes, such as Src and Ras, and inactivating tumor suppressor proteins, such as TP53 and PTEN [15].
Molecular Regulation of NADPH Homeostasis
NADPH Production Pathways
Cancer cells reprogram multiple metabolic pathways to maintain high NADPH levels. The relative contribution of different NADPH-producing pathways varies between normal and malignant cells, with cancer cells often enhancing flux through several parallel routes.
Table 2: NADPH Generation Pathways in Normal vs. Cancer Cells
| Pathway | Key Enzymes | Normal Cell Regulation | Cancer Cell Adaptation |
|---|---|---|---|
| Pentose Phosphate Pathway (PPP) | G6PD, PGD | Balanced with glycolytic flux | Significantly upregulated; G6PD overexpression common in cancers |
| Folate Metabolism | MTHFD | One-carbon unit metabolism | Enhanced to support nucleotide synthesis and NADPH production |
| Malic Enzyme | ME1 | Context-dependent activity | Increased expression; alternative NADPH source when PPP inhibited |
| Isocitrate Dehydrogenase | IDH1, IDH2 | TCA cycle function | Wild-type upregulated; mutant forms produce 2-HG instead of NADPH |
| NAD Kinase | NADK | NADP⺠synthesis regulation | Overexpressed in multiple tumors; mutants with enhanced activity |
The pentose phosphate pathway serves as the largest contributor of cytosolic NADPH in most cell types [15]. Studies have proved that NADPH production is dramatically increased by enhancing the flux of glucose into the PPP oxidative branch in various cancers [15]. Glucose-6-phosphate dehydrogenase (G6PD), the rate-limiting enzyme of PPP, shows increased activity in several cancer types, including bladder, breast, prostate, and gastric cancers compared with normal tissues [15].
Beyond the PPP, cancer cells utilize multiple alternative pathways for NADPH generation. The folate-mediated one-carbon metabolism and malic enzymes contribute significantly to NADPH production in proliferating cancer cells [15]. NAD kinase (NADK), which catalyzes the phosphorylation of NAD⺠to form NADPâº, is overexpressed in multiple tumor types, with specific mutants exhibiting enhanced enzyme activity in cancers like pancreatic ductal adenocarcinoma [15].
Compartmentalization of NADPH Pools
Recent research highlights the importance of subcellular NADPH compartmentalization, with independent regulation in different cellular compartments [30]. Using genetically encoded NADPH sensors, studies in endothelial cells have demonstrated that cytosolic and mitochondrial NADPH pools can be differentially regulated during cellular senescence [30]. In cancer cells, this compartmentalization likely supports distinct functions, with mitochondrial NADPH crucial for managing oxidative stress in that organelle, and cytosolic NADPH supporting biosynthetic pathways.
Quantitative Differences in NADPH Metabolism
Table 3: Quantitative Metrics of NADPH Metabolism
| Parameter | Normal Cells | Cancer Cells | Measurement Context |
|---|---|---|---|
| NADPH Concentration | ~3.1 ± 0.3 µM (cytosol), ~37 ± 2 µM (mitochondria) in HeLa cells [15] | Elevated levels maintained | Compartmentalized measurements in HeLa cells |
| PPP Flux | Basal level meeting cellular needs | Dramatically increased | Various cancer types |
| G6PD Activity | Tissue-specific baseline | Significantly upregulated | Bladder, breast, prostate, gastric cancers |
| NADK Expression | Normal tissue levels | Overexpressed | Multiple tumor types |
| Oxidative Stress Response | Balanced ROS-NADPH relationship | High ROS with compensatory NADPH elevation | Cancer vs. non-cancer comparisons |
Cancer cells exhibit metabolic reprogramming that creates distinct NADPH homeostasis compared to non-cancer cells. The appropriate levels of intracellular reactive oxygen species in cancer cells are essential for signal transduction and cellular processes, necessitating robust NADPH-dependent antioxidant systems [15]. Compared with non-tumor cells, tumor cells usually maintain high levels of NADPH, not only to power redox defense but also to use for biosynthetic reactions to sustain their rapid growth [15].
Experimental Approaches for NADPH Research
Methodologies for NADPH Quantification
Genetically Encoded NADPH Sensors
The development of genetically encoded indicators like iNap1 has revolutionized the study of compartmentalized NADPH dynamics [30]. The experimental protocol involves:
- Sensor Expression: Transfect cells with iNap1 targeted to specific compartments (cytosol or mitochondria)
- Calibration: Permeabilize cells with digitonin (0.001% for plasma membrane, 0.3% for mitochondrial membrane) and expose to increasing NADPH concentrations for in situ calibration
- * Imaging*: Collect fluorescence upon 405/420 nm and 488/485 nm excitation
- Quantification: Calculate ratio (405/488 or 420/485) to reflect NADPH levels
- Validation: Use non-responsive variant (iNapc) as control and test specificity with oxidants like diamide
This approach has revealed that cytosolic NADPH increases during endothelial cell senescence, while mitochondrial NADPH remains stable [30], demonstrating the power of compartment-specific NADPH monitoring.
Traditional Biochemical Assays
- Enzymatic Cycling Assays: Measure NADPH concentrations in cell homogenates using recycling reactions with intermediate electron acceptors
- Mass Spectrometry: Provides absolute quantification of NADPH and related metabolites
- Chromatography: Separates NADPH from similar molecules for accurate measurement
Assessment of Pathway Flux
Isotopic Tracer Analysis
- Glucose Labeling: Incubate cells with [1-¹³C]glucose or [2-¹³C]glucose
- Metabolite Extraction: Harvest cells and extract polar metabolites
- Mass Spectrometry Analysis: Determine labeling patterns in PPP metabolites
- Flux Calculation: Use computational modeling to estimate PPP flux relative to glycolysis
This approach has demonstrated that cancer cells significantly increase flux through the oxidative PPP to generate NADPH [15].
Functional Assessment of NADPH-Dependent Processes
Redox Homeostasis Evaluation
- GSH/GSSG Ratio: Measure using enzymatic recycling assays or LC-MS
- ROS Detection: Use fluorescent probes (DCFH-DA, DHE) to monitor reactive oxygen species
- Enzyme Activities: Assess glutathione reductase, thioredoxin reductase, and catalase activities
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for NADPH Metabolism Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| NADPH Sensors | iNap1, iNapc (control) | Real-time, compartment-specific NADPH monitoring in live cells |
| PPP Modulators | G6PD inhibitors (e.g., DHEA), G6PD activators | Investigate PPP contribution to NADPH pool |
| NOX Inhibitors | DPI (diphenyleneiodonium), apocynin | Assess NOX-derived ROS contribution to redox signaling |
| Metabolic Inhibitors | Glutaminase inhibitors, FASN inhibitors, OXPHOS inhibitors | Target specific NADPH-related pathways to study metabolic flexibility |
| Isotopic Tracers | [1-¹³C]glucose, [2-¹³C]glucose, ¹³C-glutamine | Measure pathway flux through metabolic tracing |
| Oxidative Stress Inducers | Diamide, Hâ‚‚Oâ‚‚, menadione | Challenge NADPH-dependent antioxidant systems |
| Antioxidant Reagents | N-acetylcysteine, vitamin E | Modulate cellular redox state for mechanistic studies |
Therapeutic Implications and Research Perspectives
The distinct NADPH metabolism of cancer cells presents attractive therapeutic opportunities. Modulating the unique NADPH homeostasis might be an effective strategy to eliminate cancer cells [15]. Several approaches are under investigation:
- Direct NADPH Metabolism Targeting: Inhibiting key NADPH-producing enzymes like G6PD or NADK
- Indirect Pathway Disruption: Targeting processes that increase ROS production while simultaneously inhibiting NADPH-generation pathways
- Synthetic Lethal Approaches: Exploiting metabolic vulnerabilities created by specific mutations, such as those in TCA cycle enzymes [93]
The metabolic plasticity of cancer cells poses a significant challenge, as inhibition of one NADPH source often leads to compensatory upregulation of alternative pathways [93]. Future research directions should include:
- Developing more specific inhibitors of NADPH-producing enzymes
- Exploring combination therapies that simultaneously target multiple NADPH sources
- Investigating compartment-specific NADPH modulation strategies
- Utilizing advanced technologies like single-cell metabolomics to understand metabolic heterogeneity
Visualizing NADPH Metabolism Pathways
NADPH Metabolism Network in Cancer vs. Non-Cancer Cells
Experimental Workflow for NADPH Metabolism Analysis
This comparative analysis reveals fundamental differences in NADPH metabolism between cancer and non-cancer cells. Cancer cells reprogram multiple metabolic pathways to maintain high NADPH levels, supporting both their enhanced antioxidant defenses and elevated biosynthetic requirements. The distinct NADPH homeostasis of cancer cells represents a promising therapeutic target, though the metabolic plasticity of tumors presents significant challenges. Future research should focus on understanding compartment-specific NADPH regulation, metabolic heterogeneity within tumors, and developing combination therapies that simultaneously target multiple NADPH-related vulnerabilities. The continuing elucidation of NADPH metabolism in the context of redox biology will undoubtedly yield new insights for both basic science and therapeutic development.
Cross-Species and Cross-Tissue Comparisons of NAD(H)/NADP(H) Homeostasis
The nicotinamide adenine dinucleotide (NAD+) and nicotinamide adenine dinucleotide phosphate (NADP+) pools, along with their reduced forms (NADH and NADPH), constitute fundamental redox couples essential for cellular metabolism, energy production, and antioxidant defense [94] [1]. The NAD+/NADH redox couple primarily regulates catabolic processes and cellular energy metabolism, whereas the NADP+/NADPH couple is crucial for anabolic biosynthesis and maintaining redox homeostasis against oxidative stress [94] [4] [95]. The homeostasis of these cofactors is tightly regulated through biosynthesis, consumption, recycling, and conversion between their different forms [94] [4].
Understanding the compartmentalized distribution and steady-state levels of these metabolites across different tissues and species is critical for elucidating their roles in both physiological and pathophysiological contexts. Disruptions in NAD(H) and NADP(H) homeostasis have been implicated in a spectrum of diseases, including metabolic disorders, cancer, neurodegenerative conditions, and the aging process itself [1] [96]. This whitepaper synthesizes current quantitative data on NAD(P)(H) levels across species and tissues, details advanced methodologies for their quantification, and frames these findings within the broader context of redox biology research, providing a technical guide for scientists and drug development professionals.
Physiological Roles and Metabolic Pathways of NAD(P)(H)
Distinct Cellular Functions of NAD(H) and NADP(H)
The NAD and NADP pools, while structurally similar, serve distinct and specialized functions within the cell. The NAD+/NADH couple is a central regulator of energy metabolism, acting as a primary electron carrier in catabolic reactions such as glycolysis, the tricarboxylic acid (TCA) cycle, and mitochondrial oxidative phosphorylation [94] [1]. The transfer of electrons from metabolic fuels to NAD+ forms NADH, which subsequently donates these electrons to the electron transport chain to drive ATP synthesis [94]. Beyond its redox function, NAD+ serves as an essential co-substrate for several classes of enzymes, including sirtuins (SIRTs), poly(ADP-ribose) polymerases (PARPs), and CD38/CD157 [94] [96]. These NAD+-consuming enzymes cleave NAD+ to produce nicotinamide and ADP-ribose (or cyclic ADP-ribose), facilitating critical post-translational modifications and signaling events that regulate DNA repair, gene expression, and calcium signaling [94].
In contrast, the NADP+/NADPH couple is predominantly involved in anabolic biosynthesis and cellular defense mechanisms. NADPH provides the reducing equivalents necessary for the synthesis of fatty acids, cholesterol, nucleotides, and neurotransmitters [94]. Furthermore, it is the primary electron donor for regenerative antioxidant systems, such as the glutathione and thioredoxin systems, which neutralize reactive oxygen species (ROS) and maintain cellular redox balance [94] [30]. NADPH oxidases (NOX) also utilize NADPH to generate superoxide anions, which play roles in antimicrobial defense and cell signaling [94]. The distinct functional roles of these redox couples necessitate their independent regulation and compartmentalization within the cell.
Metabolic Pathways Regulating NAD(P)(H) Homeostasis
Cellular NAD+ pools are maintained through three major biosynthetic pathways: the de novo pathway from tryptophan, the Preiss-Handler pathway from nicotinic acid (NA), and the salvage pathway, which recycles nicotinamide (NAM) back to NAD+ [1] [96]. The salvage pathway, catalyzed by the rate-limiting enzyme nicotinamide phosphoribosyltransferase (NAMPT), is responsible for the majority of NAD+ biosynthesis in most cell types [1]. NAD+ can be phosphorylated to NADP+ by NAD+ kinases (NADKs), and NADP(H) can be dephosphorylated back to NAD(H) by phosphatases such as MESH1 and nocturnin, enabling conversions between the pools [94].
NADPH is generated through several metabolic routes, with the oxidative pentose phosphate pathway (oxPPP)—catalyzed by glucose-6-phosphate dehydrogenase (G6PD) and 6-phosphogluconate dehydrogenase—being the major contributor in the cytosol [94] [30]. Other enzymes, including NADP+-dependent isocitrate dehydrogenases (IDH1/2), malic enzymes (ME1/3), and methylenetetrahydrofolate dehydrogenase (MTHFD), also generate NADPH in various cellular compartments [94] [30]. The diagram below illustrates the core metabolic pathways and interconversions that maintain NAD(H) and NADP(H) homeostasis.
Figure 1: Core Metabolic Pathways of NAD(H) and NADP(H) Homeostasis. The diagram illustrates the biosynthetic pathways (De Novo, Preiss-Handler, Salvage), key interconversions between redox states (NAD+/NADH, NADP+/NADPH), and major NAD+-consuming enzymes. NADPH is generated by enzymes such as G6PD, IDH, Malic Enzyme, and MTHFD [94] [1] [30].
Quantitative Cross-Species and Cross-Tissue Comparisons
A comprehensive meta-analysis of NAD(P)(H) concentrations across mammalian tissues reveals significant variability, influenced by species, tissue type, and methodological approaches [89]. The following tables summarize the physiological levels of these metabolites in various tissues from mice, rats, and humans, providing a reference for comparative studies.
Table 1: Physiological NAD+ and NADH Concentrations in Mammalian Tissues. Data are presented as mean ± standard deviation or range (where available) in nmol/g tissue. Adapted from a meta-analysis of 205 studies [89].
| Tissue | Species | NAD+ (nmol/g) | NADH (nmol/g) | NAD+/NADH Ratio | Primary Method |
|---|---|---|---|---|---|
| Liver | Mouse | 300 - 450 | 150 - 200 | ~2.5 | Enzyme Cycling |
| Rat | 650 - 900 | 120 - 180 | ~5.0 | Enzyme Cycling | |
| Human | 250 - 400 | 80 - 120 | ~3.5 | LC-MS | |
| Brain | Mouse | 70 - 120 | 30 - 50 | ~2.5 | Enzyme Cycling |
| Rat | 80 - 150 | 25 - 45 | ~3.5 | HPLC | |
| Human | 50 - 100 | 20 - 40 | ~2.8 | LC-MS | |
| Muscle | Mouse | 90 - 140 | 40 - 60 | ~2.3 | Enzyme Cycling |
| Rat | 100 - 180 | 35 - 55 | ~3.2 | Enzyme Cycling | |
| Human | 80 - 130 | 30 - 50 | ~2.7 | LC-MS | |
| Kidney | Mouse | 200 - 300 | 70 - 100 | ~2.9 | Enzyme Cycling |
| Rat | 250 - 400 | 80 - 120 | ~3.3 | Enzyme Cycling | |
| Human | 180 - 280 | 60 - 90 | ~3.1 | LC-MS | |
| Heart | Mouse | 250 - 350 | 90 - 130 | ~2.7 | Enzyme Cycling |
| Rat | 280 - 400 | 100 - 150 | ~2.8 | Enzyme Cycling | |
| Human | 220 - 320 | 80 - 120 | ~2.8 | LC-MS |
Table 2: Physiological NADP+ and NADPH Concentrations in Mammalian Tissues. Data are presented as mean ± standard deviation or range (where available) in nmol/g tissue. Adapted from a meta-analysis of 205 studies [89].
| Tissue | Species | NADP+ (nmol/g) | NADPH (nmol/g) | NADPH/NADP+ Ratio | Primary Method |
|---|---|---|---|---|---|
| Liver | Mouse | 20 - 40 | 150 - 250 | ~7.5 | Enzyme Cycling |
| Rat | 25 - 45 | 180 - 300 | ~8.0 | Enzyme Cycling | |
| Human | 15 - 35 | 120 - 200 | ~8.0 | LC-MS | |
| Brain | Mouse | 10 - 20 | 60 - 100 | ~8.0 | Enzyme Cycling |
| Rat | 12 - 25 | 70 - 110 | ~7.0 | HPLC | |
| Human | 8 - 18 | 50 - 90 | ~8.8 | LC-MS | |
| Muscle | Mouse | 5 - 15 | 30 - 50 | ~6.7 | Enzyme Cycling |
| Rat | 8 - 18 | 35 - 55 | ~6.0 | Enzyme Cycling | |
| Human | 6 - 14 | 25 - 45 | ~6.4 | LC-MS | |
| Kidney | Mouse | 15 - 30 | 80 - 120 | ~6.7 | Enzyme Cycling |
| Rat | 20 - 35 | 90 - 140 | ~6.5 | Enzyme Cycling | |
| Human | 12 - 28 | 70 - 110 | ~7.5 | LC-MS | |
| Heart | Mouse | 18 - 35 | 100 - 150 | ~7.1 | Enzyme Cycling |
| Rat | 20 - 40 | 110 - 160 | ~6.8 | Enzyme Cycling | |
| Human | 15 - 30 | 90 - 140 | ~7.5 | LC-MS |
The data reveals several key patterns. First, the NADPH/NADP+ ratio is consistently much higher than the NAD+/NADH ratio across all tissues and species, reflecting the distinct functional priorities of these redox couples: NADPH is maintained in a highly reduced state to support reductive biosynthesis and antioxidant defense, while the NAD+/NADH couple operates in a more oxidized state to favor catabolic oxidation reactions [94] [89]. Second, tissues with high metabolic and biosynthetic activity, such as the liver, generally exhibit higher absolute levels of both NAD(H) and NADP(H) pools. Third, significant inter-species and inter-method variability exists, underscoring the challenges of direct cross-study comparisons and the critical need for standardized quantification protocols [89].
Methodologies for Quantifying NAD(P)(H) Homeostasis
Analytical Techniques for Metabolite Quantification
Accurate quantification of NAD(P)(H) is methodologically challenging due to their labile nature, rapid interconversion, and compartmentalization. The most common techniques include enzyme cycling assays, high-performance liquid chromatography (HPLC), and liquid chromatography-mass spectrometry (LC-MS) [89].
- Enzyme Cycling Assays: These are widely used, colorimetric or fluorometric methods that exploit the redox properties of the cofactors. They are relatively accessible and sensitive but can suffer from interference and lack specificity when distinguishing between closely related isoforms (e.g., NADH vs. NADPH) without careful optimization [89].
- Liquid Chromatography-Mass Spectrometry (LC-MS): This is considered the gold standard for specificity and sensitivity. It allows for the simultaneous quantification of multiple NAD+ metabolites and the use of isotopically labeled internal standards to control for matrix effects and recovery. However, it is expensive, technically demanding, and requires rigorous validation [89].
- Pre-analytical Considerations: A critical factor for accurate quantification is sample preparation. Metabolite extraction must rapidly inactivate enzymes to prevent artifactual interconversion. The use of acid extraction (e.g., perchloric acid) can degrade the reduced forms (NADH, NADPH), making neutralized conditions or alternative solvents (e.g., acetonitrile/methanol) preferable for a comprehensive profile. The timing of tissue harvest (pre- vs. post-mortem) also significantly impacts the results [89].
Genetically Encoded Biosensors for Compartmentalized Analysis
Traditional bulk methods require cell homogenization, losing critical spatial information. Genetically encoded biosensors have revolutionized the field by enabling real-time, subcellular monitoring of these metabolites in live cells [30] [6].
- iNap Sensors: These are highly specific genetically encoded indicators for NADPH. By targeting iNap to specific compartments (e.g., cyto-iNap1, mito-iNap3), researchers have demonstrated that cytosolic and mitochondrial NADPH pools are independently regulated. For instance, during endothelial cell senescence, the cytosolic NADPH level increases while the mitochondrial pool remains unchanged [30].
- SoNar Sensor: This is a genetically encoded biosensor that is responsive to the NADH/NAD+ ratio. It has been used to demonstrate compartment-specific metabolic shifts in response to pharmacological treatments [30].
- Fluorescence Lifetime Imaging Microscopy (FLIM): FLIM of NADH autofluorescence is a powerful label-free technique that distinguishes between free and protein-bound NADH based on their distinct fluorescence lifetimes (~400 ps for free, ~2500 ps for bound) [5] [6]. The mean fluorescence lifetime (τmean) and the fraction of protein-bound NADH (α2) serve as sensitive indicators of cellular metabolic state. Recent studies show that NADH FLIM is sensitive not only to the redox state but also to the total NAD(H) pool size, which is crucial for interpreting data in contexts like aging where the pool size may decline [6]. The following workflow illustrates a typical FLIM experiment for metabolic analysis.
Figure 2: Experimental Workflow for NADH FLIM. The process involves two-photon excitation (TPE) and time-correlated single photon counting (TCSPC) to acquire fluorescence decay curves at each pixel. The data is fitted to a bi-exponential model to extract the lifetimes (τ1, τ2) and relative amplitudes (α1, α2) of free and protein-bound NADH, which are used to calculate the mean lifetime (τmean) and infer metabolic state [5] [6].
The Scientist's Toolkit: Key Research Reagents and Materials
Table 3: Essential Research Reagents for Studying NAD(P)(H) Homeostasis
| Reagent / Tool | Function / Target | Key Application in Research |
|---|---|---|
| FK866 (APO866) | NAMPT Inhibitor | Depletes cellular NAD+ by blocking the salvage pathway, used to study NAD+ deficiency [6]. |
| Nicotinamide Riboside (NR) | NAD+ Precursor | Boosts NAD+ levels via the salvage pathway, used to investigate NAD+ repletion strategies [6]. |
| iNap Biosensor | Genetically encoded NADPH sensor | Enables real-time, compartment-specific monitoring of NADPH dynamics in live cells [30]. |
| SoNar Biosensor | Genetically encoded NADH/NAD+ ratio sensor | Reports on changes in the NADH/NAD+ redox state in different cellular compartments [30]. |
| NADH FLIM | Fluorescence Lifetime Imaging Microscopy | A label-free method to assess cellular metabolic state via NADH lifetime and binding status [5] [6]. |
| Polyclonal Anti-G6PD | G6PD Antibody | Used for Western Blot and Immunostaining to quantify expression of this key NADPH-producing enzyme [30]. |
Advanced Concepts and Regulatory Mechanisms
Redox-Dependent Conformational Equilibria and FLIM Signatures
The interpretation of NAD(P)H FLIM data is becoming increasingly sophisticated. It is now understood that the fluorescence lifetime is not simply a binary measure of "free" vs. "bound" cofactor, but is exquisitely sensitive to the specific protein environment and conformational state of the enzyme to which NAD(P)H is bound [5]. For example, binding to lactate dehydrogenase (LDH) in an "open" conformation yields a different lifetime signature than binding in a "closed," substrate-bound conformation [5]. Furthermore, the redox state of the cell influences the equilibrium between these different enzyme-cofactor complexes. A more reduced state (favoring NADH and NADPH) promotes the formation of abortive ternary complexes (e.g., enzyme-NADH-reduced substrate), which are associated with particularly long fluorescence lifetimes [5]. This means that the observed FLIM parameters (τmean, α2) report not just on the fraction of bound cofactor, but on the integrated redox state of the NAD and NADP pools and the conformational equilibria of the metabolic enzymes they are engaged with.
NADPH as a Direct Modulator of Mitochondrial Carriers
Beyond its role as a cofactor, emerging evidence suggests NADPH can act as a direct regulator of mitochondrial function. A recent study demonstrated that NADPH, but not NADP+, significantly enhances the transport activity of the mitochondrial 2-oxoglutarate carrier (OGC) by ~60% [97]. Kinetic analysis indicated increased Vmax and reduced Km for 2-oxoglutarate, and molecular docking suggested a specific interaction with cytosolic loops of the OGC involving residues K206 and K122 [97]. This modulation positions the OGC as a sensor of the mitochondrial redox state, potentially coordinating with the malate/aspartate and isocitrate/oxoglutarate shuttles to maintain redox balance. This novel mechanism expands the functional repertoire of NADPH from a mere redox currency to a direct allosteric regulator of mitochondrial transport, with implications for understanding oxidative stress responses in pathologies like neurodegeneration and cancer.
The homeostasis of NAD(H) and NADP(H) is a complex, multi-layered process fundamental to cellular redox biology. Cross-species and cross-tissue analyses reveal consistent patterns—such as the highly reduced state of the NADPH pool—but also significant quantitative variability that must be accounted for in experimental design and interpretation. The advancement from bulk biochemical assays to spatially resolved techniques like genetically encoded biosensors and FLIM has provided unprecedented insight into the compartmentalized nature of this homeostasis. Furthermore, the evolving understanding that these cofactors influence cellular processes not only through their redox properties but also via conformational equilibria and direct protein modulation, as seen with the OGC, opens new avenues for research. A precise and nuanced understanding of NAD(P)(H) homeostasis across tissues and species is paramount for developing targeted therapeutic interventions for a wide range of diseases, from metabolic syndromes to aging and cancer.
Within the realm of redox biology, the nicotinamide adenine dinucleotide (NAD) system is fundamental to cellular energy metabolism and homeostasis. This system comprises two key pairs: NADâº/NADH, which primarily regulates cellular energy production, and NADPâº/NADPH, which maintains redox defense and supports biosynthetic processes [1]. The integrity of these redox couples is crucial for health; their deficiency or imbalance has been associated with a host of pathological disorders, including cardiovascular diseases, cancer, and aging [1]. Consequently, proteins that interact with or regulate these cofactors have emerged as prominent targets for therapeutic intervention. Validating these targets through robust preclinical evidence is a critical step in the drug discovery pipeline, serving to de-risk subsequent clinical development by providing confidence that modulating a target will produce a therapeutic effect [98]. This guide delves into the core methodologies of genetic and pharmacological validation, framing them within the specific context of NADPH and NADH redox biology to equip researchers and drug development professionals with the strategic and technical knowledge for successful target assessment.
Genetic Validation of Redox Targets
Genetic validation leverages human and model system genetics to establish a causal link between a gene or pathway and a disease phenotype. For targets involved in NADPH and NADH biology, this provides foundational evidence that modulation can impact redox homeostasis and disease pathophysiology.
Human Genetic Evidence as a Predictor of Success
Human genetic evidence has emerged as a powerful tool for prioritizing drug targets, with genetically supported targets being more than twice as likely to succeed in clinical development. A comprehensive 2024 analysis demonstrated that the probability of success (POS) for drug mechanisms with genetic support is 2.6 times greater than for those without [99]. This relative success varies across therapy areas, being most pronounced in metabolic, respiratory, and endocrine diseases—areas where redox biology is often implicated [99].
Table 1: Impact of Genetic Evidence on Clinical Success by Therapy Area (Selected)
| Therapy Area | Relative Success (vs. Non-Genetically Supported) | Relevance to Redox Biology |
|---|---|---|
| Metabolic | >3x | Central role of NADPH/NADH in energy metabolism and lipid synthesis [1]. |
| Haematology | >3x | Redox balance critical in blood cell function and differentiation. |
| Cardiovascular | >2x | NADPH oxidases (NOX) are key sources of ROS in vascular disease [100]. |
| Oncology | ~2.3x (Somatic evidence) | Altered redox metabolism is a hallmark of cancer progression [101]. |
The source and quality of genetic evidence significantly impact its predictive value. Support from Mendelian diseases (e.g., via OMIM) is highly robust, associated with a 3.7-fold higher success rate [99]. Furthermore, the confidence in variant-to-gene mapping in genome-wide association studies (GWAS) is critical; higher confidence scores are correlated with an increased probability of success [99].
Key Genetic Methodologies and Workflows
Several high-throughput genetic technologies are instrumental in identifying and validating novel targets.
- Genome-Wide Association Studies (GWAS): GWAS identify common genetic variants associated with complex diseases or traits. While invaluable, a challenge is that many variants lie in non-coding regions, complicating functional interpretation [102].
- Whole-Exome/Genome Sequencing (WES/WGS): WES and WGS are more adept at identifying rare, coding variants, including loss-of-function (LOF) mutations. Beneficial LOF mutations that confer disease resistance are particularly valuable for target discovery, as mimicking their effect pharmacologically is a key drug development strategy [102]. Examples include LOF mutations in PCSK9 for hypercholesterolemia and ANGPTL3 for cardiovascular disease [102].
The following workflow outlines the process of genetic target identification and validation in the context of redox biology.
Experimental Protocols for Genetic Validation
Following the identification of a genetic association, functional validation in cellular and animal models is essential.
Protocol: In Vitro Target Validation using siRNA/shRNA
- Cell Model Selection: Choose a disease-relevant cell line (e.g., primary human aortic endothelial cells for vascular aging studies [30]).
- Gene Knockdown: Transferd cells with target-specific small interfering RNA (siRNA) or transduce with short hairpin RNA (shRNA) lentiviral particles for stable knockdown. Include a non-targeting scrambled sequence as a negative control.
- Validation of Knockdown: Confirm reduction in target mRNA expression via qPCR and protein level via Western blotting 48-72 hours post-transfection.
- Phenotypic and Redox Assessment:
- Proliferation/Senescence: Assess using assays like β-galactosidase staining (for senescence) or MTT (for viability) [30].
- Redox Metabolite Measurement: Use genetically encoded biosensors (e.g., iNap for NADPH, SoNar for NADH/NAD⺠ratio) to monitor compartmentalized changes in redox couples [30]. Alternatively, employ enzymatic cycling assays or mass spectrometry.
- Functional Assays: Measure downstream pathway outputs, such as ROS production or glutathione levels [48].
Pharmacological Validation of Redox Targets
Pharmacological validation uses chemical tools to probe target biology and establish a therapeutic hypothesis. It confirms that the effects observed genetically can be replicated by a drug-like molecule.
Fluorescence-Based Imaging of NAD(P)H
A key technique for studying the effects of pharmacological interventions on NAD(P)H-related redox biology is Fluorescence Lifetime Imaging Microscopy (FLIM). The fluorescence lifetime of free NAD(P)H is ~400 ps, but when enzyme-bound, it increases significantly—to over 3000 ps in some configurations [5]. The relative abundance of the bound fraction (α2) serves as a sensitive, intrinsic reporter of cellular metabolic state.
Protocol: NAD(P)H FLIM to Assess Metabolic Intervention
- Sample Preparation: Plate live cells (e.g., HEK293, primary mesenchymal stem cells) on glass-bottom dishes. Apply the pharmacological inhibitor or activator of interest.
- Image Acquisition: Use a multi-photon microscope equipped with time-correlated single photon counting (TCSPC) electronics. Excite NAD(P)H at ~720 nm and collect emission at 440(±40) nm [5]. Acquire data until sufficient photon counts are obtained for robust fitting (~2 minutes per field of view).
- Data Analysis: Fit the fluorescence decay curve at each pixel to a multi-exponential model. Standard parameters include:
- Ï„1 (short lifetime): Representing free NAD(P)H.
- Ï„2 (long lifetime): Representing enzyme-bound NAD(P)H.
- α2: The fraction of the emitting population contributing to τ2, indicative of the bound ratio [5].
- Interpretation: A shift in α2 or τ2 upon treatment indicates a change in the metabolic equilibrium, such as altered enzyme-binding configurations driven by the redox state of the NAD and NADP pools [5].
Targeting NADPH Oxidases (NOXs): A Case Study
The NOX family of enzymes, which are major generators of superoxide using NADPH as a substrate, are attractive pharmacological targets in conditions like thrombosis and depression comorbidity [100]. Validating NOX inhibitors requires careful dissection of direct target engagement versus antioxidant effects.
Protocol: Differentiating Direct NOX Inhibition from Redox Scavenging A comprehensive study highlighted the importance of using multiple assays to identify bona fide inhibitors [76].
- Cell-Free Enzymatic Assay: Purify NOX enzyme components. Monitor superoxide production (e.g., via cytochrome c reduction) in the presence of NADPH and the test compound. This identifies direct enzyme inhibitors.
- Counter-Screening for Redox Scavenging: In a cell-free system, generate superoxide or Hâ‚‚Oâ‚‚ independently of NOX (e.g., using xanthine/xanthine oxidase). Test the compound's ability to quench these ROS, identifying molecules with mere antioxidant properties [76].
- Cellular Activity Assay: Measure compound-induced reduction in ROS production in intact cells overexpressing a specific NOX isoform.
- Biophysical Target Engagement: Use techniques like surface plasmon resonance or crystallography to confirm direct binding. For example, diphenylene iodonium (DPI) engages the flavin and heme prosthetic groups of NOXs, while VAS3947 covalently alkylates a conserved cysteine in the dehydrogenase domain [76].
The following diagram illustrates the decision-making pathway for characterizing a putative NOX inhibitor.
The Scientist's Toolkit: Key Research Reagents
Successful validation relies on a suite of specialized reagents and tools.
Table 2: Essential Reagents for Validating Redox Targets
| Reagent / Tool | Function in Validation | Specific Example / Application |
|---|---|---|
| Genetically Encoded Biosensors | Real-time, compartment-specific monitoring of redox metabolites. | iNap1 (NADPH sensor) [30]; SoNar (NADH/NAD⺠sensor) [30]. |
| Pharmacological Inhibitors | Chemical probes to modulate target activity. | VAS3947 (covalent NOX inhibitor) [76]; DPI (flavin/heme binder) [76]. |
| siRNA/shRNA Libraries | For targeted gene knockdown in cellular models. | Validating the role of G6PD in endothelial senescence [30]. |
| FLIM-FRET Microscopy | Quantifying protein-protein interactions and metabolic states via fluorescence lifetime. | Measuring NAD(P)H enzyme-binding states to report on cellular metabolism [5]. |
| Crispr-Cas9 System | For generating knockout cell lines or transgenic animal models. | Creating humanized mouse models to study primate-specific pathways [98]. |
Integrating Genetic and Pharmacological Evidence
The most compelling preclinical validation packages synergistically integrate genetic and pharmacological data. This convergence provides a multi-faceted argument for a target's role in disease and its "druggability." For instance, human genetics may identify G6PD as associated with vascular aging, where its upregulation is protective [30]. Subsequently, pharmacological strategies—either by direct enzyme activation or via upstream pathways—can be deployed to mimic this beneficial genetic effect. A high-throughput screen using an NADPH sensor identified folic acid, which acts through methylenetetrahydrofolate dehydrogenase (MTHFD) to generate NADPH, as an effective intervention that alleviated vascular aging in mice [30]. This integrated approach, from human genetics to pharmacological intervention, de-risks the drug development process and provides a clear path toward therapeutic translation.
The validation of drug targets within the NADPH/NADH redox ecosystem demands a rigorous, multi-pronged strategy. Genetic evidence, particularly from human studies, provides a powerful foundation for target selection, significantly enhancing the probability of clinical success. This must be followed by meticulous pharmacological validation using advanced techniques such as FLIM and specific chemical probes to confirm target engagement and elucidate the underlying redox biology. By systematically integrating these preclinical approaches—from population-level genetics to compartmentalized metabolic imaging—researchers can build a robust evidence base for therapeutic targets, ultimately accelerating the development of novel treatments for a wide spectrum of redox-related diseases.
Emerging Clinical Evidence for NAD+ Precursors and Redox-Modulating Drugs
Nicotinamide adenine dinucleotide (NAD+) and its reduced form (NADH), along with its phosphorylated counterpart NADP+/NADPH, represent fundamental redox couples essential for cellular metabolism and homeostasis. The NAD+/NADH ratio is a primary regulator of cellular energy metabolism, critical for catabolic redox reactions in processes such as glycolysis and mitochondrial oxidative phosphorylation [103] [1]. In contrast, the NADP+/NADPH couple functions as a crucial reducing power for anabolic processes and maintaining antioxidant defense systems [1] [4]. These redox couples operate in distinct yet interconnected cellular compartments, with their balance meticulously regulated through biosynthesis, consumption, recycling, and enzymatic conversion via NAD kinases (NADKs) and NADP(H) phosphatases [4]. The central thesis of modern redox biology posits that the progressive dysregulation of these systems—particularly the observed decline in NAD+ levels during aging—represents a fundamental contributor to age-related functional decline and disease pathogenesis [104] [105]. This whitepaper comprehensively evaluates the emerging clinical evidence for therapeutic strategies targeting NAD+ metabolism, framing them within the broader context of NAD(H) and NADP(H) redox biology.
NAD+ Biosynthesis Pathways and Homeostatic Regulation
Major Biosynthetic Pathways
Cellular NAD+ homeostasis is maintained through multiple biosynthetic pathways that utilize different precursors, with tissue-specific expression patterns determining the predominant route in different physiological contexts [103] [1].
- De Novo Pathway: This pathway starts from tryptophan (Trp) and is primarily active in the liver and kidneys. The initial rate-limiting step is catalyzed by indoleamine 2,3-dioxygenase (IDO) or tryptophan 2,3-dioxygenase (TDO), converting Trp to N-formylkynurenine. A second rate-limiting step is catalyzed by quinolinate phosphoribosyltransferase (QPRT) [1].
- Preiss-Handler Pathway: This pathway utilizes nicotinic acid (NA) as a precursor, which is converted to nicotinic acid mononucleotide (NAMN) by nicotinic acid phosphoribosyltransferase (NAPRT). NAMN is then adenylated to NAAD before final conversion to NAD+ [103] [1].
- Salvage Pathway: This predominant pathway in most tissues recycles nicotinamide (NAM) generated as a byproduct of NAD+-consuming reactions. The rate-limiting enzyme nicotinamide phosphoribosyltransferase (NAMPT) converts NAM to nicotinamide mononucleotide (NMN), which is subsequently converted to NAD+ by NMN adenylyltransferases (NMNAT1-3) [103] [1].
The diagram below illustrates the compartmentalization and interconnectivity of these major NAD+ biosynthetic pathways.
Compartmentalization and Systemic Regulation
NAD+ metabolism exhibits significant compartmentalization within cells, with distinct pools in the cytoplasm, nucleus, and mitochondria regulated by different enzyme isoforms [1] [4]. NMNAT1 is nuclear, NMNAT2 is cytosolic and Golgi-associated, while NMNAT3 is found in mitochondria and cytoplasm [1]. Systemic NAD+ homeostasis involves inter-organ communication, with extracellular NAMPT (eNAMPT) secreted by adipocytes and other cells potentially facilitating NAD+ precursor conversion between tissues [103]. The circadian clock also regulates NAD+ biosynthesis, creating oscillations in NAD+ levels that coordinate metabolic processes with daily cycles [4].
Age-Associated NAD+ Decline and Pathophysiological Consequences
Evidence for NAD+ Decline in Aging
Multiple preclinical studies have consistently demonstrated an age-related decline in NAD+ levels across various tissues, though clinical evidence remains more limited [104]. Proposed mechanisms for this decline include increased consumption by NAD+-utilizing enzymes (PARPs, CD38, sirtuins), reduced biosynthesis through decreased NAMPT expression, and impaired precursor uptake [104] [106]. The decline is not uniform across all tissues, with metabolically active organs such as the brain, liver, and skeletal muscle showing particular vulnerability [103].
Impact on Mitochondrial Function and Redox Homeostasis
The age-related decline in NAD+ has profound implications for mitochondrial function and cellular redox balance through several interconnected mechanisms:
- Impaired Oxidative Phosphorylation: NAD+ is essential for the tricarboxylic acid (TCA) cycle and electron transport chain, with declining levels leading to reduced ATP production and energetic deficits [103].
- Mitochondrial Quality Control Disruption: NAD+ is required for mitophagy and mitochondrial unfolded protein response (UPRmt), essential pathways for maintaining mitochondrial health [103].
- Reductive Stress: NAD+ deficiency can paradoxically lead to reductive stress through accumulation of reducing equivalents like NADH, disrupting ROS-dependent signaling and causing mitochondrial dysfunction [107].
- Sirtuin Inhibition: Declining NAD+ impairs sirtuin activity, affecting epigenetic regulation, DNA repair, and metabolic adaptation [103].
The following diagram illustrates how NAD+ decline disrupts mitochondrial and redox homeostasis, creating a pathological feedback loop.
NAD+ Precursors: Clinical Evidence and Clinical Applications
Established NAD+ Precursors
The table below summarizes the key NAD+ precursors that have advanced to clinical investigation, their mechanisms of action, and clinical evidence.
Table 1: Clinically Investigated NAD+ Precursors and Their Properties
| Precursor | Biosynthetic Pathway | Typical Clinical Dose | Key Clinical Findings | Safety Profile |
|---|---|---|---|---|
| Nicotinic Acid (NA) | Preiss-Handler | 250-1000 mg/day | Efficient NAD+ booster, improves lipid profiles, but flushing limits tolerability [108] | Generally safe, flushing common [108] |
| Nicotinamide (NAM) | Salvage | 250-1000 mg/day | Effective NAD+ booster, may inhibit sirtuins at high doses [108] | Well-tolerated, no flushing [108] |
| Nicotinamide Riboside (NR) | NRK-mediated Salvage | 250-1000 mg/day | Increases NAD+ metabolome, reduces inflammatory markers, improves neuromuscular function [108] | Generally well-tolerated, mild GI effects reported [109] [108] |
| Nicotinamide Mononucleotide (NMN) | Salvage | 250-500 mg/day | Increases NAD+ levels, potential improvements in physical performance [108] | Safe in published trials [108] |
Clinical Trial Evidence by Disease Area
Recent clinical trials have investigated NAD+ precursors across multiple age-related conditions, with the most comprehensive evidence emerging from studies conducted between 2020-2025.
Table 2: Clinical Trial Outcomes of NAD+ Precursors in Age-Related Conditions (2020-2025)
| Disease Area | Population | Precursor | Intervention | Key Outcomes | Reference |
|---|---|---|---|---|---|
| Healthy Aging | Healthy older adults (N=24) | NR | 500 mg single dose | Increased NAD(P)H, decreased oxidative stress, improved physical performance in older individuals only [108] | [108] |
| Healthy Aging | Healthy middle-aged men (N=42) | NMN | 250 mg/day, 6-12 weeks | Trend toward improved gait speed and left grip strength [108] | [108] |
| Metabolic Disease | Overweight adults | NR | 1000 mg/day, 12 weeks | Increased NAD+ levels in peripheral blood mononuclear cells [108] | NCT02921659 [108] |
| Neurodegeneration | Older adults (N=22-24) | NR | 500 mg twice daily, 6 weeks | Increased serum NAD+ metabolome, decreased neurodegenerative markers in neuron-derived extracellular vesicles [108] | [108] |
| Acute Kidney Injury | Aged patients | NR + Pterostilbene | Combination therapy | Minor gastrointestinal symptoms, nausea, and diarrhea reported [108] | [108] |
Experimental Approaches and Research Methodologies
Standardized Protocols for NAD+ Research
NAD+ Quantification in Clinical Samples
Accurate measurement of NAD+ and related metabolites represents a fundamental methodology in this field. The following protocol has been validated in multiple clinical studies:
- Sample Collection: Collect blood, tissue biopsies, or other biological samples under standardized conditions, immediately flash-freeze in liquid nitrogen, and store at -80°C to prevent metabolite degradation [108].
- Metabolite Extraction: Homogenize samples in extraction buffer (typically 80% methanol or acetonitrile) containing internal standards (e.g., 13C-NAD+ or D4-NAD+) for quantification [1].
- Liquid Chromatography Separation: Use reverse-phase HPLC with a C18 column and gradient elution with mobile phases containing ion-pairing agents (e.g., tributylamine) to separate NAD+ metabolites [1].
- Mass Spectrometric Detection: Employ triple-quadrupole or Q-TOF mass spectrometry in multiple reaction monitoring (MRM) mode for sensitive and specific detection of NAD+ metabolites [1].
- Data Analysis: Normalize NAD+ levels to protein content or cell count, and express as fold-change relative to control groups with appropriate statistical analysis [108].
Assessment of Mitochondrial Function
Evaluation of NAD+ supplementation effects on mitochondrial function typically includes:
- High-Resolution Respirometry: Use Oroboros O2k or Seahorse Analyzer to measure oxygen consumption rates in isolated mitochondria or intact cells with substrate-uncoupler-inhibitor titration (SUIT) protocols [103].
- ATP Production Assays: Quantify cellular ATP levels using luciferase-based assays under basal and stressed conditions [103].
- Mitochondrial Membrane Potential: Assess using fluorescent dyes (JC-1, TMRM) with flow cytometry or fluorescence microscopy [103].
- Reactive Oxygen Species Measurement: Detect mitochondrial superoxide and hydrogen peroxide production using MitoSOX Red and Amplex Red assays, respectively [107].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for NAD+ and Redox Biology Studies
| Reagent/Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| NAD+ Precursors | Nicotinamide Riboside (NR), Nicotinamide Mononucleotide (NMN) | In vitro and in vivo NAD+ boosting studies | Purity critical (>98%); stability in solution varies; consider esterified forms for enhanced bioavailability [109] [108] |
| NAD+ Quantification Kits | Colorimetric (CycLex), Luminescent (Promega), LC-MS Standards (Sigma) | Quantifying NAD+/NADH ratios in cells/tissues | LC-MS provides highest specificity; kit-based methods offer convenience; consider compartmentalization (nuclear vs. cytosolic vs. mitochondrial pools) [1] |
| Sirtuin Inhibitors/Activators | EX527 (SIRT1 inhibitor), Resveratrol (SIRT1 activator) | Determining sirtuin-specific effects in NAD+ studies | Specificity varies; use multiple compounds with different mechanisms to confirm findings [103] |
| CD38 Inhibitors | 78c, Apigenin | Reducing NAD+ consumption in aging models | Confirm target engagement via cADPR production; consider genetic knockdown validation [103] |
| Mitochondrial Function Assays | Seahorse XF Kits, MitoSOX Red, TMRM | Assessing bioenergetic capacity and mitochondrial health | Multiple assays recommended for comprehensive assessment; consider cell type-specific optimization [103] [107] |
| Genetic Models | NAMPT KO, CD38 KO, SIRT1 KO mice/cells | Establishing causal relationships in NAD+ pathways | Tissue-specific conditional KO often necessary due to developmental effects of global KO [103] |
The following diagram outlines a comprehensive experimental workflow for evaluating NAD+ precursors in preclinical and clinical research.
Emerging Therapeutic Strategies and Clinical Challenges
Novel NAD+-Targeting Approaches
Beyond traditional precursors, several innovative strategies are emerging in clinical development:
- Reduced NAD+ Precursors: Dihydronicotinamide riboside (NRH) and dihydronicotinamide mononucleotide (NMNH) represent reduced forms that can be converted to NADH, potentially offering more efficient NAD+ boosting through distinct metabolic routes [103].
- Combination Therapies: NAD+ precursors combined with sirtuin activators (e.g., pterostilbene) or CD38 inhibitors may provide synergistic benefits, though clinical evidence remains limited [108].
- Microbiome-Targeted Approaches: Emerging evidence suggests gut microbiota significantly influence NAD+ precursor metabolism, opening avenues for microbiome-modulating interventions [106].
- Nanotechnology Applications: Nanoparticle-based delivery systems show promise for targeted NAD+ precursor delivery to specific tissues and for modulating reductive stress in cancer therapy [107].
Current Challenges and Future Directions
Despite promising preclinical evidence, several challenges have limited the clinical translation of NAD+-based interventions:
- Limited Clinical Efficacy: While NAD+ precursors consistently increase NAD+ levels in humans, functional benefits have been more modest than predicted from animal studies [104] [109].
- Tissue-Specific Delivery: Achieving therapeutic NAD+ concentrations in target tissues, particularly the brain, remains challenging due to bioavailability and blood-brain barrier limitations [104].
- Biomarker Development: Validated biomarkers for assessing target engagement and biological effects in humans are still needed [109].
- Long-Term Safety: The long-term consequences of chronic NAD+ boosting remain unknown, requiring larger and longer-duration clinical trials [109].
- Interindividual Variability: Genetic polymorphisms, microbiome composition, and lifestyle factors contribute to variable responses to NAD+ precursors [106].
Future research directions should prioritize large-scale, well-controlled clinical trials with standardized outcome measures, development of tissue-specific delivery systems, and personalized approaches based on individual metabolic and genetic profiles.
The clinical evidence for NAD+ precursors continues to evolve, demonstrating consistent effects on increasing NAD+ bioavailability with generally favorable safety profiles. However, translating these biochemical effects into meaningful clinical benefits has proven more challenging than initially anticipated. The interplay between NAD+ metabolism and the broader redox biology framework—particularly the balance between NAD+/NADH and NADP+/NADPH couples—represents a critical area for further investigation. Future success in this field will likely require more sophisticated approaches to tissue-targeted delivery, combination therapies addressing multiple aspects of NAD+ metabolism, and personalized strategies based on individual metabolic phenotypes. As our understanding of NAD+ biology deepens and clinical evidence matures, NAD+-targeted interventions hold substantial promise for addressing age-related functional decline and multiple chronic diseases rooted in metabolic and redox dysregulation.
Redox biology, centered on the intricate balance of reduction-oxidation reactions, is undergoing a transformative shift from generalized antioxidant approaches to targeted, personalized therapeutic strategies. The nicotinamide adenine dinucleotide (NAD+) and NAD phosphate (NADP+) systems and their reduced forms (NADH and NADPH) constitute a fundamental metabolic hub that governs cellular redox homeostasis and signaling networks [1] [96]. These redox couples function not merely as metabolic cofactors but as dynamic regulators of multiple cellular processes, including energy metabolism, genomic stability, epigenetic modification, and cell survival decisions [48] [96]. The emerging understanding of how compartmentalized NAD(P)H pools influence redox-sensitive pathways has revealed profound heterogeneity in redox stress responses across individuals and disease states, rendering one-size-fits-all antioxidant therapies largely ineffective [48] [110]. This whitepaper delineates the experimental and conceptual framework for advancing personalized redox medicine, with particular emphasis on the pivotal roles of NADPH and NADH in shaping patient-specific therapeutic outcomes.
NAD(P)H in Redox Homeostasis: Biochemical Foundations and Compartmentalization
The NAD+/NADH and NADP+/NADPH redox couples, while structurally similar, serve distinct biochemical functions with precise subcellular compartmentalization. The NAD+/NADH pair primarily regulates cellular energy metabolism, functioning as a key hydride carrier in mitochondrial oxidative phosphorylation, glycolysis, and the tricarboxylic acid (TCA) cycle [1] [96]. In contrast, the NADP+/NADPH system predominantly maintains redox defense and supports reductive biosynthesis, providing reducing equivalents for glutathione regeneration, thioredoxin system function, and detoxification of reactive oxygen species (ROS) via NADPH-dependent antioxidant enzymes [1].
Subcellular Distribution of NAD(P)H Pools
Recent advances in genetically encoded biosensors have revealed compartment-specific concentrations of these redox couples, with significant implications for targeted therapeutic interventions:
- Cytoplasmic NAD+: ~70 μM
- Nuclear NAD+: ~110 μM
- Mitochondrial NAD+: ~90 μM [96]
The mitochondrial NAD(H) pool appears relatively segregated from cytosolic and nuclear pools, attributed to the membrane impermeability of NAD(H) [96]. This compartmentalization necessitates precise targeting of therapeutic interventions to address redox dysregulation in specific cellular locations.
NADPH-Generating Systems and Their Regulatory Roles
NADPH production occurs through multiple enzymatic pathways that display tissue-specific expression and regulation:
- Glucose-6-phosphate dehydrogenase (G6PD): The rate-limiting enzyme of the pentose phosphate pathway
- Malic enzyme (ME1): Cytosolic NADPH generation
- Isocitrate dehydrogenases (IDH1/2): Mitochondrial and cytosolic isoforms
- Nicotinamide nucleotide transhydrogenase (NNT): Mitochondrial proton-translocating enzyme that generates NADPH at the expense of the mitochondrial proton gradient [1]
Table 1: Primary NADPH-Generating Enzymes and Their Cellular Roles
| Enzyme | Subcellular Location | Primary Function | Therapeutic Relevance |
|---|---|---|---|
| G6PD | Cytosol | Pentose phosphate pathway, rate-limiting NADPH production | Protection against oxidative hemolysis; potential target in cancer metabolism |
| IDH1 | Cytosol | Conversion of isocitrate to α-ketoglutarate with NADPH generation | IDH1 mutations in cancer produce 2-hydroxyglutarate; targeted inhibitors available |
| IDH2 | Mitochondria | Mitochondrial NADPH production | Mutations in gliomas and AML; small molecule inhibitors in clinical use |
| ME1 | Cytosol | Pyruvate to malate conversion with NADPH generation | Supports antioxidant defense and lipogenesis; overexpressed in some cancers |
| NNT | Mitochondria | Transhydrogenation between NADH and NADP+ using proton gradient | Key for mitochondrial redox balance; genetic variations affect stress susceptibility |
Diagnostic Approaches for Personalized Redox Assessment
Fluorescence Lifetime Imaging Microscopy (FLIM) for NAD(P)H Monitoring
Time-resolved fluorescence anisotropy imaging of NAD(P)H represents a cutting-edge methodology for non-invasively monitoring metabolic states in living cells and tissues [26]. This technique capitalizes on the inherent fluorescence of reduced NADH and NADPH (collectively referred to as NAD(P)H) when excited with ultraviolet light.
Experimental Protocol: NAD(P)H FLIM for Metabolic Phenotyping
- Sample Preparation: Cells or tissue sections are maintained under physiologically relevant conditions (37°C, 5% CO₂) in phenol red-free medium to minimize background fluorescence.
- Image Acquisition: Two-photon excitation at ~740 nm with time-correlated single-photon counting (TCSPC) detection. A 60x water-immersion objective (NA ≥1.2) provides optimal resolution. Data collection typically requires 60-180 seconds per field of view.
- Lifetime Analysis: Fluorescence decay curves are fitted to a multi-exponential model: I(t) = αâ‚exp(-t/Ï„â‚) + α₂exp(-t/Ï„â‚‚) + α₃exp(-t/τ₃) where Ï„ represents lifetime components and α their relative amplitudes.
- Interpretation: The short lifetime component (τ₠≈ 0.4-0.5 ns) corresponds to free NAD(P)H, while longer lifetimes (τ₂ ≈ 1-2 ns, τ₃ ≈ 3-5 ns) represent protein-bound NAD(P)H. The ratio of bound-to-free NAD(P)H correlates with the oxidative phosphorylation-to-glycolysis balance [26].
- Anisotropy Measurements: Polarized detection enables rotational diffusion analysis, providing information on enzyme binding and conformational changes.
This approach has revealed that redox states of NAD and NADP pools control the steady-state equilibrium of binding configurations, which determines the observed fluorescence decay – a critical insight for interpreting metabolic imaging data [26].
Multi-Omics Integration for Redox Profiling
Comprehensive redox assessment requires integration of multiple analytical platforms:
- Redox Proteomics: Mass spectrometry-based identification of cysteine oxidation, S-nitrosylation, S-glutathionylation, and carbonylation modifications
- Metabolomics: LC-MS quantification of NAD+/NADH, NADP+/NADPH ratios, glutathione (GSH/GSSG), TCA cycle intermediates, and oxidative damage markers
- Transcriptomics: RNA-seq analysis of NRF2-target genes, NADPH-producing enzymes, and antioxidant defense systems
- Epigenomics: Assessment of redox-sensitive epigenetic modifications, including DNA and histone methylation patterns influenced by NAD+-dependent sirtuins and α-ketoglutarate-dependent dioxygenases [48] [96] [110]
Table 2: Key Biomarkers for Redox Status Assessment
| Biomarker Category | Specific Markers | Analytical Method | Biological Significance |
|---|---|---|---|
| NAD(P)H Dynamics | NAD+/NADH, NADP+/NADPH ratios, NAD(P)H FLIM lifetimes | LC-MS, enzymatic assays, FLIM | Energy metabolism status, reductive capacity |
| Thiol Redox Status | GSH/GSSG ratio, cysteine oxidation states, glutathionylated proteins | HPLC, redox proteomics | Antioxidant capacity, redox signaling status |
| Oxidative Damage | 8-oxo-dG (DNA), protein carbonylation, 4-HNE adducts, F2-isoprostanes | Immunoassays, LC-MS, HPLC | Cumulative oxidative stress burden |
| Enzyme Activities | SOD, catalase, GPx, GST, NRF2 activation | Enzymatic assays, reporter assays | Functional antioxidant capacity |
| Genetic Markers | SNPs in SOD, GPX, GST, NOX isoforms, NRF2 pathway | Whole-genome sequencing, PCR | Inherited susceptibility to redox imbalance |
Targeted Therapeutic Strategies in Personalized Redox Medicine
NAD+ Precursor Therapies
NAD+ precursor supplementation represents a foundational approach for restoring redox homeostasis in conditions of NAD+ depletion:
- Nicotinamide Riboside (NR) and Nicotinamide Mononucleotide (NMN): These precursors enter the NAD+ salvage pathway via nicotinamide phosphoribosyltransferase (NAMPT) and NR kinases, effectively boosting intracellular NAD+ levels [96].
- Nicotinic Acid (NA): Utilizes the Preiss-Handler pathway through NAPRT1 conversion to NA mononucleotide [1] [96].
- Tryptophan: Serves as a de novo NAD+ precursor through the kynurenine pathway, though this route is less efficient than salvage pathways [1].
Individual genetic variations in NAD+ biosynthetic enzymes (NAMPT, NMNATs, NADSYN) significantly influence response to these precursors, necessitating pharmacogenetic profiling for optimal outcomes [96].
NRF2 Activators and Context-Dependent Application
The transcription factor NRF2 serves as a master regulator of antioxidant response elements, controlling the expression of numerous detoxification and antioxidant enzymes. Several NRF2 activators have entered clinical development:
- Dimethyl Fumarate: Approved for multiple sclerosis and psoriasis, induces NRF2-mediated antioxidant responses
- Sulforaphane: Derived from broccoli sprouts, promotes NRF2 nuclear translocation
- Bardoxolone Methyl: Synthetic triterpenoid with potent NRF2-activating properties [48] [110]
The therapeutic application of NRF2 activators requires careful patient stratification, as prolonged, unregulated NRF2 activation may promote cancer progression in certain contexts by enhancing stress resistance in transformed cells [48].
Mitochondria-Targeted Antioxidants
Compartment-specific redox interventions represent a significant advance over broad-spectrum antioxidants:
- MitoQ: Ubiquinone conjugated to triphenylphosphonium cation, accumulating in the mitochondrial matrix
- SS-31 (Elamipretide): Cell-permeable tetrapeptide that targets cardiolipin in the inner mitochondrial membrane
- SkQ1: Plastoquinone conjugated to decyltriphenylphosphonium, demonstrating efficacy in preclinical neurodegeneration models [110]
These compounds specifically address mitochondrial oxidative stress, which is implicated in neurodegenerative diseases, metabolic disorders, and aging-related pathologies.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Redox Biology Investigations
| Reagent/Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Genetically Encoded Redox Biosensors | HyPer (Hâ‚‚Oâ‚‚), roGFP (glutathione redox potential), Frex (NADH) | Real-time monitoring of specific redox couples in living cells | Require calibration; specificity varies between probes |
| NAD(P)H FLIM Reagents | Two-photon FLIM systems, low-autofluorescence media | Metabolic imaging, protein-binding status of NAD(P)H | Specialized equipment required; complex data analysis |
| NRF2 Pathway Modulators | Sulforaphane, bardoxolone methyl, ML385 (NRF2 inhibitor) | Manipulation of antioxidant response pathway | Context-dependent effects; cytotoxicity at high doses |
| NAD+ Precursors | Nicotinamide riboside, NMN, nicotinic acid | NAD+ repletion studies | Differential bioavailability; pathway-specific preferences |
| Mitochondria-Targeted Probes | MitoSOX Red, MitoTracker, JC-1 | Mitochondrial ROS and membrane potential assessment | Potential artifacts; require appropriate controls |
| Thiol-Reactive Probes | Maleimide derivatives, iodoacetamide-alkyne probes | Redox proteomics, cysteine oxidation mapping | Sample processing under non-oxidizing conditions critical |
| OXPHOS Inhibitors | Rotenone (Complex I), antimycin A (Complex III), oligomycin (ATP synthase) | Mitochondrial stress tests, ROS source identification | Dose optimization required to avoid non-specific effects |
Visualization of Redox Signaling Networks and Therapeutic Targeting
The following diagram illustrates the core NAD(P)H-dependent redox signaling network and potential intervention points:
NAD(P)H Redox Network and Targeting
This network visualization illustrates the compartmentalization of NAD(H) (primarily mitochondrial energy metabolism) and NADP(H) (primarily cytosolic redox defense) systems, highlighting key intervention points for personalized redox therapies.
Experimental Framework for Combination Therapy Development
Protocol for Evaluating Redox-Modulating Combination Therapies
Objective: Systematically assess synergistic interactions between NAD+ precursors and targeted therapies in patient-derived cellular models.
Methodology:
Patient-Derived Model Establishment:
- Generate primary cell cultures from patient biopsies or induced pluripotent stem cells (iPSCs)
- Characterize baseline redox parameters (NAD+/NADH ratios, GSH/GSSG, mitochondrial ROS)
High-Content Redox Screening:
- Treat cells with NAD+ precursors (NR, NMN; 0.1-1.0 mM) in combination with targeted agents (NRF2 activators, mitochondria-targeted antioxidants)
- Quantify multiple redox endpoints simultaneously using fluorescent probes (CellROX for ROS, MitoTracker for mitochondrial mass, TMRM for membrane potential)
Metabolic Flux Analysis:
- Employ Seahorse XF Analyzer to measure oxygen consumption rate (OCR) and extracellular acidification rate (ECAR)
- Calculate ATP production rates, maximal respiration, and spare respiratory capacity
Transcriptomic and Proteomic Profiling:
- Perform RNA-seq to identify pathway enrichment following combination treatments
- Conduct redox proteomics to map cysteine oxidation changes
Synergy Analysis:
The future of redox medicine lies in abandoning one-size-fits-all antioxidant approaches in favor of mechanism-based, patient-stratified interventions that account for individual variations in NAD(P)H metabolism and redox signaling networks. Successful implementation will require: (1) Advanced diagnostic platforms for comprehensive redox phenotyping (2) Genetic profiling to identify polymorphisms in NADPH-generating enzymes and antioxidant systems (3) Development of compartment-specific redox modulators (4) Sophisticated clinical trial designs that incorporate biomarker-driven patient selection
The integration of AI-driven analysis of multi-omics datasets with dynamic redox imaging will enable unprecedented precision in matching patients with optimal redox-modulating regimens, ultimately revolutionizing therapeutic approaches for cancer, neurodegenerative diseases, metabolic disorders, and aging-related conditions.
Conclusion
The intricate interplay between NADPH and NADH forms the cornerstone of cellular redox regulation, governing processes from energy production to antioxidant defense and biosynthetic capacity. Dysregulation of these systems is a hallmark of numerous pathologies, including cancer, vascular aging, and neurodegenerative disorders. The development of sophisticated tools, such as genetically encoded biosensors, has revolutionized our ability to probe compartment-specific dynamics, enabling high-throughput discovery of therapeutic agents like folic acid, which shows promise in ameliorating vascular aging. Future research must focus on understanding the nuanced crosstalk between different NADPH pools and pathways, validating novel targets like G6PD and NADK in clinical settings, and developing personalized redox therapies that consider individual metabolic contexts. Successfully targeting the NADPH/NADH axis holds immense potential for creating a new class of therapeutics that can restore redox balance across a spectrum of human diseases.
References
- 1. NAD(H) and NADP(H) Redox Couples and Cellular Energy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5737637/]
- 2. Investigating mitochondrial redox state using NADH ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5145803/]
- 3. 7.8: The Chemistry of NAD+ and FAD [https://chem.libretexts.org/Courses/Brevard_College/CHE_301_Biochemistry/07%3A_Nutrition/7.08%3A_The_Chemistry_of_NAD_and_FAD]
- 4. Homeostatic regulation of NAD(H) and NADP(H) in cells [https://www.sciencedirect.com/science/article/pii/S2352304223004294]
- 5. Redoxâ€dependent binding and conformational equilibria ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12519055/]
- 6. Visualizing subcellular changes in the NAD(H) pool size ... [https://www.nature.com/articles/s42003-024-06123-7]
- 7. A family of NADPH/NADP+ biosensors reveals in vivo ... [https://www.nature.com/articles/s41467-024-55302-x]
- 8. Announcing NADMED as Tier 4 Sponsor of ARDD 2025 [https://www.eurekalert.org/news-releases/1093949]
- 9. NAD+ biosynthetic pathways (WP3645) - Homo sapiens [https://www.wikipathways.org/pathways/WP3645.html]
- 10. Separating NADH and NADPH fluorescence in live cells ... [https://www.nature.com/articles/ncomms4936]
- 11. Coenzyme Q biochemistry and biosynthesis - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC10106368/]
- 12. Pharmacological bypass of NAD+ salvage pathway protects ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6196523/]
- 13. Evaluating Cell Metabolism Through Autofluorescence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6352511/]
- 14. Illuminating redox biology using NADH- and NADPH ... [https://www.nature.com/articles/nmeth.4336]
- 15. NADPH homeostasis in cancer: functions, mechanisms ... [https://www.nature.com/articles/s41392-020-00326-0]
- 16. Tracing Compartmentalized NADPH Metabolism in the ... [https://www.sciencedirect.com/science/article/pii/S109727651400402X]
- 17. NADMED Named Tier 4 Sponsor for ARDD 2025 [https://bioengineer.org/nadmed-named-tier-4-sponsor-for-ardd-2025/]
- 18. Pharmacology and Potential Implications of Nicotinamide ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8612620/]
- 19. Understanding the Role of NADH in Cellular Respiration [https://driphydration.com/blog/nadh-cellular-respiration/?srsltid=AfmBOooSqVscVrtN-4-9ZR49xhTwPkguxk-u8m9iCQZuHsKA96cTAcrk]
- 20. Biochemistry, Glycolysis - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK482303/]
- 21. Glycolysis [https://en.wikipedia.org/wiki/Glycolysis]
- 22. The Mechanism of Oxidative Phosphorylation - The Cell - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK9885/]
- 23. Biochemistry, Oxidative Phosphorylation - StatPearls - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK553192/]
- 24. Oxidative phosphorylation [https://en.wikipedia.org/wiki/Oxidative_phosphorylation]
- 25. Inhibition of glycolysis disrupts cellular antioxidant defense ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6487699/]
- 26. Redox-dependent binding and conformational equilibria ... [https://pubmed.ncbi.nlm.nih.gov/40878865/]
- 27. Mitochondrial NADPH propels oxidative metabolism - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12507123/]
- 28. The multi-faceted role of NADPH in regulating inflammation ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1328484/full]
- 29. Hoxhaj Lab discovers how mitochondria use NADPH to ... [https://cri.utsw.edu/hoxhaj-lab-discovers-how-mitochondria-use-nadph-to-fuel-fatty-acid-synthesis-lipoylation/]
- 30. Elevating cytosolic NADPH metabolism in endothelial cells ... [https://www.nature.com/articles/s41467-025-64652-z]
- 31. Developing a Redox Imbalance Forces Drive (RIFD) ... [https://www.sciencedirect.com/science/article/abs/pii/S1096717625001181]
- 32. The NADPH Link between the Renin Angiotensin System and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10604245/]
- 33. Genetically encoded fluorescent sensors reveal dynamic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5555402/]
- 34. Using genetically encoded fluorescent biosensors to ... [https://ovarianresearch.biomedcentral.com/articles/10.1186/s13048-022-01046-5]
- 35. Genetically Encoded Fluorescent Biosensors Illuminate the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7462118/]
- 36. Construction of Genetically Encoded Biosensors to Monitor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9909732/]
- 37. The Importance of NADPH Oxidases and Redox Signaling in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5488012/]
- 38. Role of NADPH oxidases in the redox biology of liver fibrosis [https://www.sciencedirect.com/science/article/pii/S2213231715000774]
- 39. NAD(H) and NADP(H) in plants and mammals - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12178909/]
- 40. Biosensors, Volume 15, Issue 9 (September 2025) [https://www.mdpi.com/2079-6374/15/9]
- 41. Emerging trends in AI-integrated optical biosensors for point ... [https://pubs.rsc.org/en/content/articlehtml/2025/cc/d5cc04899k]
- 42. Insights in biosensors and biomolecular electronics 2024 ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1668411/full]
- 43. A Novel Approach for ALS and FTD Drug Discovery [https://pubmed.ncbi.nlm.nih.gov/40493571/]
- 44. Screening of an FDA-Approved Drug Library: Menadione ... [https://www.mdpi.com/1424-8247/18/8/1145]
- 45. High-throughput drug screening in advanced pre-clinical 3D ... [https://jeccr.biomedcentral.com/articles/10.1186/s13046-025-03539-9]
- 46. NADPH Oxidases: From Molecular Mechanisms to Current ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10510401/]
- 47. Structure and mechanisms of ROS generation by NADPH ... [https://www.sciencedirect.com/science/article/abs/pii/S0959440X18301805]
- 48. Redox regulation: mechanisms, biology and therapeutic ... [https://www.nature.com/articles/s41392-024-02095-6]
- 49. MFA Suiteâ„¢ | MFA Suite [https://mfa.vueinnovations.com/mfa]
- 50. Inferring Metabolic Flux from Gene Expression Data Using ... [https://pubmed.ncbi.nlm.nih.gov/40779111/]
- 51. Metabolic Flux Analysis [https://sciex.com/applications/biomedical-and-omics-research/metabolomics/metabolic-flux-analysis]
- 52. NADPH Oxidase (NOX)-Replacement Therapies Market to ... [https://www.prnewswire.com/news-releases/nadph-oxidase-nox-replacement-therapies-market-to-observe-stunning-growth-during-the-forecast-period-20252034-across-7mm--delveinsight-302495483.html]
- 53. Strategies for genetic manipulation of adult stem cell- ... [https://www.nature.com/articles/s12276-021-00609-8]
- 54. Gene Knockdown methods To Determine Gene Function! [https://www.biosyn.com/tew/Gene-Knockdowns-Methods-To-Determine-Gene-Function!.aspx]
- 55. Making Sense of Pharmacology: Inverse Agonism and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6165953/]
- 56. Current strategies employed in the manipulation of gene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9673226/]
- 57. Oxidative Stress: Causes, Symptoms & Treatment [https://my.clevelandclinic.org/health/articles/oxidative-stress]
- 58. Reductive stress [https://en.wikipedia.org/wiki/Reductive_stress]
- 59. Reductive Stress in Inflammation-Associated Diseases and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5666780/]
- 60. Oxidative Stress: Harms and Benefits for Human Health [https://pmc.ncbi.nlm.nih.gov/articles/PMC5551541/]
- 61. Nicotinamide adenine dinucleotide [https://en.wikipedia.org/wiki/Nicotinamide_adenine_dinucleotide]
- 62. Role of NADPH oxidases in the redox biology of liver fibrosis [https://pubmed.ncbi.nlm.nih.gov/26204504/]
- 63. Reductive stress: The key pathway in metabolic disorders ... [https://www.sciencedirect.com/science/article/pii/S2090123225000311]
- 64. NADP in the Cell Cytosol Influences Vascular Aging [https://www.fightaging.org/archives/2025/11/nadp-in-the-cell-cytosol-influences-vascular-aging/]
- 65. Arterial stiffness and vascular aging: mechanisms, ... [https://www.nature.com/articles/s41392-025-02346-0]
- 66. Vitamins, Vascular Health and Disease - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12472326/]
- 67. Association between red blood cell folate and accelerated ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1504441/full]
- 68. HDAC3 mediates retinal endothelial cell metabolic ... [https://pubmed.ncbi.nlm.nih.gov/41023273/]
- 69. NADPH oxidases: redox regulation of cell homeostasis and ... [https://pubmed.ncbi.nlm.nih.gov/39814410]
- 70. NADPH Oxidases (NOX): An Overview from Discovery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8228183/]
- 71. NADPH Oxidases (NOX): An Overview from Discovery, ... [https://www.mdpi.com/2076-3921/10/6/890]
- 72. Nox Family NADPH Oxidases in Mechano-Transduction [https://pmc.ncbi.nlm.nih.gov/articles/PMC3924808/]
- 73. The role of NADPH oxidases in infectious and ... [https://www.sciencedirect.com/science/article/pii/S2213231721003190]
- 74. Targeting NOX inhibitors in neurodegeneration [https://pubmed.ncbi.nlm.nih.gov/40481920/]
- 75. Special Issue : NADPH Oxidases (NOXs) - Antioxidants [https://www.mdpi.com/journal/antioxidants/special_issues/NOX]
- 76. A closer look into NADPH oxidase inhibitors [https://www.sciencedirect.com/science/article/pii/S2213231720301269]
- 77. The Redox Paradox: Cancer's Double-Edged Sword for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12561025/]
- 78. Targeting the redox-programmed cell death axis in breast ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12500867/]
- 79. Metabolic Reprogramming at the Edge of Redox [https://www.mdpi.com/1422-0067/26/2/498]
- 80. NOX4 serves as a pan-cancer prognostic biomarker and ... [https://www.nature.com/articles/s41598-025-09690-9]
- 81. Pan-cancer analysis of NADPH oxidase 4 identifying its ... [https://www.sciencedirect.com/science/article/abs/pii/S1567576924023373]
- 82. Passage dependence of NADH redox status and reactive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11557164/]
- 83. NOX4 as an emerging prognostic and immunological ... [https://www.nature.com/articles/s41598-025-03499-2]
- 84. Review article NAD(H) and NADP(H) in plants and mammals [https://www.sciencedirect.com/science/article/pii/S1674205225001637]
- 85. Elevating cytosolic NADPH metabolism in endothelial cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12583496/]
- 86. NADK Governs Ferroptosis Susceptibility by Orchestrating ... [https://www.mdpi.com/2076-3921/14/12/1396]
- 87. Mitochondrial NADPH fuels mitochondrial fatty... | Nature Cell Biology [https://www.nature.com/articles/s41556-025-01655-4?error=cookies_not_supported&code=a90215e4-3b14-4eaf-bdba-164194dcf5c3]
- 88. Scientists unveil high-resolution human NAD kinase ... [https://cri.utsw.edu/high-resolution-human-nad-kinase-structure-key-cancer-metabolism-regulator/]
- 89. Meta-analysis of NAD(P)(H) quantification results exhibits ... [https://www.nature.com/articles/s41598-023-29607-8]
- 90. Schisandra total lignans ameliorate neuronal ferroptosis in ... [https://pubmed.ncbi.nlm.nih.gov/40088743/]
- 91. Metabolic Reprogramming of Cancer Cells and Therapeutics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12439291/]
- 92. Metabolic reprogramming and therapeutic targeting in non- ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1564226/full]
- 93. Altered metabolism in cancer: insights into energy pathways ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-02119-3]
- 94. Homeostatic regulation of NAD(H) and NADP(H) in cells - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11233901/]
- 95. NAD(H) and NADP(H) Redox Couples and Cellular Energy ... [https://pubmed.ncbi.nlm.nih.gov/28648096/]
- 96. NAD+ metabolism: pathophysiologic mechanisms and ... [https://www.nature.com/articles/s41392-020-00311-7]
- 97. Modulatory Effect of Nicotinamide Adenine Dinucleotide ... [https://www.mdpi.com/1420-3049/29/21/5154]
- 98. Molecular Target Validation in preclinical drug discovery [https://www.drugtargetreview.com/article/821/molecular-target-validation-in-preclinical-drug-discovery/]
- 99. Refining the impact of genetic evidence on clinical success [https://www.nature.com/articles/s41586-024-07316-0]
- 100. NADPH-oxidases as potential pharmacological targets for ... [https://pubmed.ncbi.nlm.nih.gov/38310682/]
- 101. Cellular redox imbalance on the crossroad between ... [https://www.sciencedirect.com/science/article/pii/S2213231722001094]
- 102. Drug development advances in human geneticsâ€based targets [https://pmc.ncbi.nlm.nih.gov/articles/PMC10857782/]
- 103. The role of NAD+ metabolism and its modulation ... - Nature [https://www.nature.com/articles/s44324-025-00067-0]
- 104. NAD + precursor supplementation in human ageing [https://pubmed.ncbi.nlm.nih.gov/41083806/]
- 105. Roles of Nicotinamide Adenine Dinucleotide (NAD+) in ... [https://www.frontiersin.org/research-topics/51855/roles-of-nicotinamide-adenine-dinucleotide-nad-in-aging-and-age-related-diseaseundefined]
- 106. The therapeutic perspective of NAD + precursors in age ... [https://www.sciencedirect.com/science/article/pii/S0006291X24001256?srsltid=AfmBOopTv5JEgJEiNKhvZm8bvn-lagZkViCk-U4ZjL0cX2Wz5FfhQ9t&53061b3a_page=6&e4d7314d_page=4]
- 107. Nanomedicineâ€Driven Modulation of Reductive Stress for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12407351/]
- 108. Clinical evidence for the use of NAD+ precursors to slow ... [https://sciexplor.com/articles/Geromedicine.2025.0008]
- 109. Emerging strategies, applications and challenges of ... [https://pubmed.ncbi.nlm.nih.gov/40926126/]
- 110. The Redox Revolution in Brain Medicine [https://www.mdpi.com/1422-0067/26/15/7498]