Hormesis in Redox Biology: Unraveling Biphasic Mechanisms from NRF2 Signaling to Therapeutic Innovation
This article explores the fundamental principle of hormesis, the biphasic dose-response phenomenon where low doses of stressors induce adaptive beneficial effects, within the context of redox biology.
Hormesis in Redox Biology: Unraveling Biphasic Mechanisms from NRF2 Signaling to Therapeutic Innovation
Abstract
This article explores the fundamental principle of hormesis, the biphasic dose-response phenomenon where low doses of stressors induce adaptive beneficial effects, within the context of redox biology. Tailored for researchers and drug development professionals, it synthesizes current evidence on how mild oxidative stress activates conserved molecular pathways, including NRF2, AMPK, and mTOR, to enhance cellular defense systems. The scope ranges from foundational mechanisms and experimental methodologies to the challenges of translating hormesis into reliable clinical applications, such as preconditioning strategies and combating therapeutic resistance. It also provides a critical comparative analysis against linear dose-response models, underscoring hormesis's profound implications for developing novel interventions in aging, degenerative diseases, and oncology.
The Redox Hormesis Paradigm: From Biphasic Dose-Response to Evolutionary Adaptation
Hormesis describes an evolutionarily conserved adaptive response where exposure to a low dose of a stressor that is damaging at higher doses induces a beneficial effect on the cell or organism [1] [2]. In redox biology, this phenomenon is characterized by a biphasic dose-response curve, typically exhibiting a J- or U-shape, where low levels of oxidative stress activate protective signaling pathways, enhancing cellular resilience [1] [3]. This whitepaper details the molecular mechanisms, quantitative parameters, and experimental methodologies underlying redox hormesis, providing a technical guide for research and therapeutic development. The core mechanistic pathways involve the activation of transcription factors like Nrf2 and NF-κB, leading to the upregulated expression of cytoprotective proteins such as antioxidant enzymes, heat-shock proteins, and growth factors [1] [4] [2]. A precise understanding of the "hormetic zone" is critical, as its boundaries define the transition from adaptive beneficial responses to detrimental oxidative damage [5] [6].
The conceptual foundation of hormesis was established by the adage of Paracelsus, "the dose makes the poison" [4] [6]. In modern toxicology, hormesis is specifically defined as "a process in which exposure to a low dose of a chemical agent or environmental factor that is damaging at higher doses induces an adaptive beneficial effect on the cell or organism" [1] [2]. This biphasic dose-response relationship is a fundamental feature observed across various biological models, from microbial systems to humans, and in response to a diverse array of stressors, including chemicals, radiation, heat, and exercise [1] [7].
Within redox biology, the hormetic response is principally triggered by mild oxidative stress, which involves a transient, non-damaging increase in reactive oxygen species (ROS) [4] [3]. These ROS molecules function as critical signaling intermediates that activate specific cytoprotective pathways, a concept often referred to as "mitohormesis" when the signaling originates from mitochondria [3]. The resulting adaptive response enhances the cell's capacity to maintain redox homeostasis, thereby increasing its resilience to subsequent, more severe oxidative insults [8] [6]. This mechanism is integral to the health-promoting effects of several lifestyle interventions, including exercise, dietary energy restriction, and exposure to certain phytochemicals [1] [3].
Molecular Mechanisms of Redox Hormesis
The adaptive benefits of redox hormesis are mediated through the activation of highly conserved cellular signaling pathways. These pathways coordinate the expression of a network of genes responsible for antioxidant defense, detoxification, protein repair, and survival.
Core Signaling Pathways
- Nrf2/ARE Pathway: The transcription factor Nrf2 (nuclear factor erythroid 2-related factor 2) is a primary regulator of the antioxidant response. Under basal conditions, Nrf2 is sequestered in the cytoplasm by its repressor, Keap1. Low-dose oxidative stress induces conformational changes in Keap1, leading to Nrf2 stabilization and its translocation to the nucleus. There, it binds to the Antioxidant Response Element (ARE), driving the expression of a battery of cytoprotective genes, including those for glutathione S-transferases, heme oxygenase-1, and NAD(P)H quinone dehydrogenase 1 [4] [2] [6].
- NF-κB Pathway: The transcription factor NF-κB (nuclear factor kappa-light-chain-enhancer of activated B cells) is another key player. Moderate ROS levels can activate NF-κB, which promotes the expression of genes encoding anti-apoptotic proteins like Bcl-2 and other pro-survival factors [1] [2]. This pathway often operates in parallel with Nrf2 to ensure coordinated cell protection.
- Kinase Signaling Cascades: Several kinases are activated by hormetic stimuli. AMPK, mTOR, and MAPK pathways are involved in sensing cellular energy status and stress, thereby modulating metabolic adaptation and survival [4]. Additionally, specific isoforms of Protein Kinase C (PKC), particularly PKC-δ, can phosphorylate Nrf2, facilitating its release from Keap1 and contributing to the hormetic response [2].
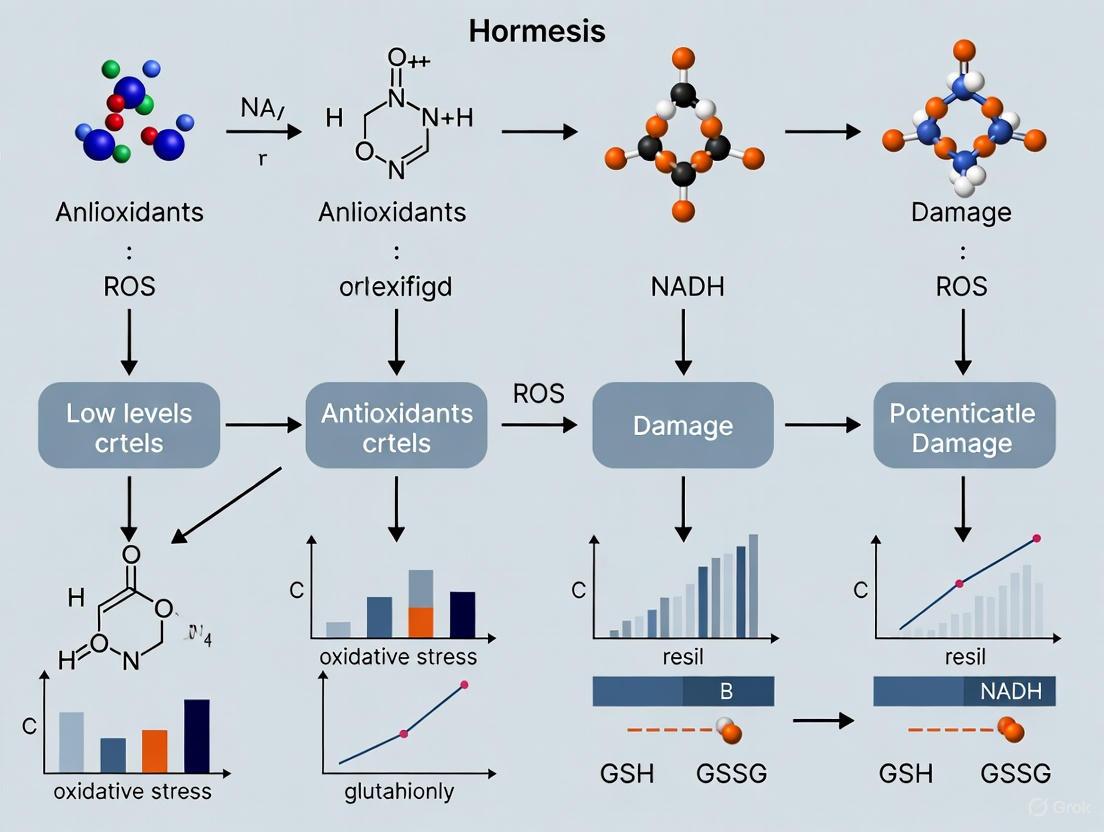
The following diagram illustrates the integrated signaling network activated by mild oxidative stress, leading to cytoprotective outcomes.
Effector Molecules and Cellular Outcomes
The activation of the above signaling cascades culminates in the increased production of effector molecules that execute the protective functions:
- Antioxidant Enzymes: Enzymes such as superoxide dismutase (SOD), catalase (CAT), and glutathione peroxidase are upregulated, directly enhancing the cell's capacity to neutralize ROS [1] [2].
- Phase II Detoxifying Enzymes: Enzymes like NAD(P)H quinone oxidoreductase 1 facilitate the elimination of toxic electrophiles [1] [6].
- Heat Shock Proteins (HSPs): Proteins such as HSP70 and HSP90 function as molecular chaperones, promoting correct protein folding and preventing aggregation under stress conditions [1] [2].
- Growth Factors: Production of factors like brain-derived neurotrophic factor (BDNF) and insulin-like growth factors (IGFs) can be induced, supporting cell growth, survival, and plasticity [1].
Quantitative Characterization of the Biphasic Response
The biphasic dose-response curve of hormesis can be quantitatively modeled to define critical parameters for experimental design and interpretation.
Mathematical Modeling
The hormetic response can be effectively modeled using a Gaussian function that describes an inverted U-shaped curve [5]. The equation is: [ y = \text{baseline} + \text{amplitude} \cdot e^{-\frac{(x - x_0)^2}{2\sigma^2}} ] Where:
- ( y ) is the biological response (e.g., cell viability).
- ( \text{baseline} ) is the response level of the control.
- ( \text{amplitude} ) is the maximum stimulatory response.
- ( x_0 ) is the dose at which the peak stimulatory response occurs.
- ( \sigma ) controls the width of the hormetic zone.
A study on the flavonoid Brosimine B provided a precise quantitative example. The model fitted to retinal cell viability data yielded a peak response (( x_0 )) at 10.2 µM and a hormetic zone width (( \sigma )) of 6.5 µM, with a high coefficient of determination (( R^2 = 0.984 )), confirming a well-defined hormetic relationship [5].
Key Quantitative Parameters from Empirical Data
The table below summarizes quantitative parameters of hormetic responses from various experimental models in the literature.
Table 1: Quantitative Parameters of Hormetic Responses in Experimental Models
| Hormetic Agent / Stressor | Biological System | Endpoint Measured | Stimulatory Dose (Peak or Range) | Maximum Stimulation (% over control) | Inhibitory Dose | Citation |
|---|---|---|---|---|---|---|
| Brosimine B | Avian retinal cell culture | Cell viability (under OGD) | 10 µM (Peak) | ~150% (at 10 µM) | >10 µM | [5] |
| Sulforaphane | Human mesenchymal stem cells | Cell protection / Oxidative damage | 1 µM | Protection from apoptosis & DNA damage | 20 µM (promotes damage) | [6] |
| Hydrogen Peroxide (Preconditioning) | L929 cell line (in vitro) | Adaptive cytoprotection | 50 µM (for 9h) | Increased resistance to severe stress | Higher, prolonged exposure | [2] |
| Olive Oil Polyphenol Extract | HeLa cells (in vitro) | Intracellular Glutathione (GSH) levels | 10-25 µg/mL (depending on extract) | Significant increase in GSH | Higher doses decreased GSH | [6] |
| Ionizing Radiation | Mice (in vivo) | Mean Lifespan | Chronic low-dose | Up to 22% extension | High, acute doses | [3] |
The "hormetic zone" is typically constrained, with the maximum stimulatory response often ranging between 30-60% above the control baseline, and the stimulatory dose range usually falling within a less than 10-fold window below the threshold for toxicity [1] [7].
Experimental Protocols for Investigating Redox Hormesis
Robust experimental design is essential for accurately characterizing hormetic dose-responses. The following provides a generalized protocol and a specific example.
General Workflow for In Vitro Dose-Response Analysis
This workflow outlines the key steps for establishing a hormetic response to a chemical agent in a cell culture model.
Detailed Protocol: Brosimine B in a Retinal Neuroprotection Model
This specific protocol from recent research demonstrates the practical application of the general workflow [5].
- Cell Culture Preparation: Primary mixed retinal cells are isolated from 7-day-old chicken embryos (Gallus gallus domesticus). The retinae are dissected in a calcium and magnesium-free salt solution and cultured for 7 days in Dulbecco’s Modified Eagle Medium (DMEM) supplemented with 10% fetal bovine serum (FBS), 2 mM glutamine, and 2% penicillin-streptomycin.
- Oxygen-Glucose Deprivation (OGD) Model: To simulate ischemic conditions, cells are subjected to OGD by incubation in a sealed chamber for 3, 6, or 24 hours. The culture medium is replaced with glucose-free DMEM without FBS. Control cells are maintained in high-glucose (25 mM) DMEM with 10% FBS in unsealed plates.
- Hormetic Treatment: For dose-response analysis, retinal cells are treated with a range of Brosimine B concentrations (e.g., 1, 5, 10, 25, 50, and 100 µM) for 24 hours. To test preconditioning (hormetic) effects, a protective dose of 10 µM Brosimine B is applied at the beginning of the OGD period.
- Cell Viability Assessment: Cell viability is quantified using the MTT assay. Cells are incubated with 0.5 mg/mL MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) for 3 hours. The resulting formazan crystals are solubilized with DMSO, and absorbance is measured at 570 nm.
- Redox Biomarker Analysis: Reactive oxygen species (ROS) production is measured using fluorescent probes. Antioxidant enzyme activity (e.g., catalase) is assessed via specific kinetic assays.
- Computational Modeling: The biphasic dose-response data for cell viability is fitted to the Gaussian hormetic model to derive biologically interpretable parameters like the peak response dose and the hormetic zone width.
The Scientist's Toolkit: Essential Reagents and Materials
Research in redox hormesis requires a suite of specific reagents and tools to induce stress, measure responses, and probe molecular mechanisms.
Table 2: Key Research Reagent Solutions for Redox Hormesis Studies
| Reagent / Material | Function in Research | Example Use Case |
|---|---|---|
| Hydrogen Peroxide (H₂O₂) | A direct-acting oxidant used to induce mild oxidative stress for preconditioning experiments. | Establishing an oxidative conditioning hormesis (OCH) model (e.g., 50 µM for 9h in L929 cells) [2]. |
| Sulforaphane | A natural compound and potent Nrf2 inducer; a classic hormetic agent. | Studying Nrf2/ARE pathway activation and its role in cytoprotection at low doses (e.g., 1 µM) vs. toxicity at high doses (e.g., 20 µM) [6]. |
| MTT Assay Kit | A colorimetric method for assessing cell viability and metabolic activity, a common endpoint for hormesis. | Quantifying the biphasic effect of a test compound like Brosimine B on cell survival [5]. |
| ROS Detection Probes (e.g., DCFH-DA) | Fluorescent dyes that detect intracellular reactive oxygen species (ROS). | Measuring the initial ROS burst from a hormetic stressor and the subsequent reduction due to adapted antioxidant defenses [5]. |
| Nrf2 & NF-κB Antibodies | For Western Blot and Immunofluorescence to monitor the localization and expression of key transcription factors. | Confirming nuclear translocation of Nrf2 and NF-κB following low-dose oxidative stress [2]. |
| GSH/GSSG Assay Kit | For quantifying the ratio of reduced glutathione (GSH) to oxidized glutathione (GSSG), a key indicator of cellular redox state. | Demonstrating the improvement in antioxidant capacity after hormetic preconditioning (e.g., with olive oil extracts) [6]. |
| Oxygen-Glucose Deprivation (OGD) Setup | A chamber or system to create controlled hypoxic/ischemic conditions in cell culture. | Modeling ischemic stress to test the neuroprotective hormetic effects of compounds like Brosimine B [5]. |
The biphasic dose-response curve of hormesis is a fundamental concept in redox biology, representing a highly conserved adaptive survival mechanism. Its molecular architecture, centered on the Nrf2/ARE pathway and integrated with pro-survival signals from NF-κB and kinase cascades, provides a robust framework for explaining how mild stress can enhance cellular resilience [1] [4] [2]. The quantitative characterization of the hormetic zone is not merely an academic exercise; it is critical for translating this knowledge into clinical applications.
Future research and therapeutic development must rigorously account for hormesis. In drug development, this means carefully mapping dose-response relationships to avoid underdosing, which could inadvertently induce protective responses in target diseases like cancer or infections, leading to resistance [3]. Conversely, harnessing hormesis through preconditioning strategies—such as in ischemic heart disease, neurodegenerative disorders, and metabolic diseases—holds immense promise for preventing or slowing disease progression [1] [3]. Furthermore, the hormetic effects of lifestyle interventions like exercise and dietary energy restriction provide a mechanistic understanding of their well-documented health benefits [1] [9]. As the field advances, integrating hormesis into the core of redox biology research and translational medicine will be essential for developing novel strategies to enhance healthspan and combat age-related diseases.
The concept that the effects of a substance are determined by its dosage is a cornerstone of modern pharmacology and toxicology. This principle, central to the phenomenon of hormesis—a biphasic dose-response characterized by low-dose stimulation and high-dose inhibition—has evolved from ancient empirical observations into a foundational concept in modern molecular biology, particularly in redox biology research [4] [10]. The journey of this idea spans from the self-experimentation of King Mithridates VI to the foundational toxicology of Paracelsus, and now to the molecular dissection of cellular signaling pathways [11]. This whitepaper traces this historical trajectory, documenting how this enduring principle has been refined through centuries of scientific inquiry to inform contemporary research and therapeutic development.
The historical narrative of hormesis provides more than just academic interest; it offers a crucial framework for interpreting modern experimental data in redox biology. Understanding this evolution is essential for today's researchers, as it contextualizes why biological systems frequently exhibit biphasic responses to oxidative stressors, phytochemicals, and therapeutic agents [12]. This report integrates historical context with current molecular understanding, providing technical guidance and methodological resources for investigating hormetic mechanisms in experimental models.
Historical Foundations of the Dose-Response Concept
Ancient and Classical Precedents
Long before the term "hormesis" was coined, the fundamental concept was recognized in various ancient philosophical and practical traditions. Key historical milestones established the foundational idea that the amount of a substance determines its biological effect:
- 8th Century BC Greek Philosophy: Hesiod, in his work Harmonia, introduced the concept of 'moderation and harmony' [11]. This philosophical principle was physically inscribed at the Apollo Temple in Delphi as 'meden agan' (μηδὲν ἄγαν), translating to 'nothing too much' [11]. Cleobulus of Lindos (625-555 BCE) further articulated the principle as 'metron ariston' (μέτρoν ἄριστoν), meaning 'the optimal is the right measure' [11].
- Roman Era Expressions: Latin proverbs such as "ne quid nimis" (nothing in excess) by Terentius and "aurea mediocritas" (the golden mean) by Horace reinforced this dosage-dependent view of substance effects [11].
- Hippocratic Contributions: Hippocrates (460-377 BCE) advanced beyond philosophical principles to practical application, recognizing individual variability in response to drugs. In the Hippocratic Corpus, he noted that "the sweet ones do not benefit everyone, nor do the astringent ones, nor are all the patients able to drink the same things," acknowledging factors such as personal "constitution" that we now understand in terms of genetic susceptibility and epigenetics [11].
Mithridates VI and Practical Toxicology
Mithridates VI Eupator (132-63 BCE), King of Pontus, represents a pivotal figure in the transition from philosophical concept to practical application of hormetic principles [11]. Fearing assassination by poisoning, he systematically experimented with poisons and antidotes, developing what would become known as mithridatism [11] [12].
Table 1: Key Components of Mithridates' Approach to Toxicology
| Aspect | Description | Modern Hormetic Correlation |
|---|---|---|
| Methodology | Regular ingestion of sublethal doses of poisons, particularly arsenic [11]. | Preconditioning: Mild, intermittent exposure to a stressor to build resilience against larger, damaging exposures [11]. |
| Formula Development | Created a complex antidote known as mithridatium or theriac, containing over 50 ingredients to counteract poisons [11]. | Combination Therapies: Use of multiple compounds with synergistic protective effects, activating several defense pathways simultaneously [2]. |
| Experimental Approach | Conducted experiments on prisoners to test poisons and antidotes [11]. | Experimental Models: Use of in vitro and in vivo systems to quantify dose-response relationships and mechanisms. |
| Demonstrated Phenomenon | Acquired resistance to normally lethal doses of poison, demonstrating it at banquets [11]. | Acquired Tolerance: Adaptive responses through enzymatic induction and metabolic functional changes [11]. |
Mithridates' approach demonstrated early understanding of several principles central to modern hormesis research: tolerance development, adaptive immunity to toxins, and the paradoxical benefit of low-dose exposure to otherwise harmful substances [11]. His eventual failure to commit suicide by poison due to his acquired tolerance dramatically illustrates the effectiveness—and potential limitations—of this adaptive strategy [11].
Paracelsus and the Foundation of Modern Toxicology
The 16th-century Swiss-German physician Paracelsus (1493-1541) made the single most influential contribution to the conceptual foundation of dose-response with his seminal declaration: "Sola dosis facit venenum" ("only the dose makes the poison") [4] [13]. This statement established the fundamental principle that any substance can be toxic or beneficial depending on its concentration, moving beyond the notion of inherently "good" or "bad" compounds [13].
Paracelsus' insight provided the philosophical bridge between ancient observations of moderation and the future scientific study of dose-response relationships. His principle implicitly acknowledged what would later be termed the biphasic nature of biological responses to chemical agents, though it would take centuries for this concept to be formally developed and accepted [4].
Modern Conceptualization and Terminology
The formal scientific recognition of hormesis progressed through several key developments in the 19th and 20th centuries:
- 1880s: Arndt-Schulz Law: German pharmacologist Hugo Schulz observed that low concentrations of disinfectants paradoxically stimulated metabolism in yeast, contrary to their inhibitory effects at high concentrations [12] [10]. Initially dismissed as experimental error, this finding eventually led to the formulation of the Arndt-Schulz Law with Rudolf Arndt, proposing that weak stimuli accelerate vital activity, medium stimuli suppress it, and strong stimuli halt it [12].
- 1943: Term Coined: The term "hormesis" (from the Greek hormáein, meaning "to set in motion") was first introduced in published literature by Southam and Ehrlich in their study of red cedar tree extract effects on fungal metabolism [10] [14].
- Late 20th Century: Systematic Validation: After periods of marginalization and controversy (partly due to incorrect associations with homeopathy), the hormesis concept experienced a resurgence led by researchers including Thomas Luckey (radiation hormesis) and Edward J. Calabrese, who conducted systematic, large-scale analyses demonstrating the generality of hormetic dose responses [10].
Table 2: Historical Evolution of Key Hormesis Concepts
| Time Period | Key Figure/Concept | Contribution to Hormesis Understanding |
|---|---|---|
| 8th Century BC | Greek Proverbs ('meden agan') | Philosophical foundation of moderation and avoidance of excess [11]. |
| 1st Century BC | Mithridates VI | Practical application through systematic low-dose poison exposure (mithridatism) [11]. |
| 16th Century | Paracelsus ('Sola dosis facit venenum') | Established dose as primary determinant of toxicity/therapeutic effect [4] [13]. |
| 19th Century | Hugo Schulz & Rudolf Arndt | First experimental evidence of biphasic dose-response (Arndt-Schulz Law) [12] [10]. |
| 20th Century | Southam & Ehrlich | Coined the term "hormesis" [10]. |
| 21st Century | Calabrese et al. | Quantitative analysis, mechanistic studies, and database development [4]. |
Quantitative Characterization of Hormetic Responses
Modern research has established consistent quantitative characteristics of hormetic dose responses that transcend biological models, endpoints, and mechanisms [10]. Understanding these parameters is essential for designing experiments and interpreting results in redox biology and drug development.
Fundamental Quantitative Features
Hormetic responses display remarkably consistent quantitative properties across biological systems:
- Response Magnitude: The maximum stimulatory response in hormesis is typically modest, generally ranging between 30-60% above control/background levels, rarely exceeding two-fold [10]. This constrained amplification reflects the biological limits of plasticity and adaptive capacity.
- Dose-Response Width: The stimulatory range typically extends from approximately 0.1 to 10 times the No-Observed-Adverse-Effect Level (NOAEL) [13]. This defines the "therapeutic window" for hormetic effects.
- Temporal Dynamics: Hormetic responses can occur via either direct stimulation or overcompensation stimulation following an initial disruption in homeostasis [10]. The quantitative features are similar regardless of mechanism, but timing of measurement is critical.
Mathematical Modeling of Biphasic Responses
The biphasic nature of hormetic dose responses can be quantitatively described using mathematical models. Recent research on natural products like Brosimine B demonstrates the application of Gaussian functions to characterize these relationships [15]:
For the flavonoid Brosimine B, the dose-response relationship for retinal cell viability followed an inverted U-shaped curve effectively modeled by the equation:
Y = baseline + amplitude × e^(-(x - x₀)² / (2σ²))
Where:
- Y = measured response (cell viability)
- baseline = control response level
- amplitude = maximum hormetic enhancement
- x₀ = peak hormetic dose (10.2 µM for Brosimine B)
- σ = hormetic zone width (6.5 µM for Brosimine B) [15]
This modeling approach yielded a high coefficient of determination (R² = 0.984), confirming the hormetic response and providing biologically interpretable parameters for optimizing therapeutic applications [15].
Table 3: Quantitative Parameters of Documented Hormetic Responses
| Hormetic Agent | Biological System | Peak Stimulatory Dose | Response Magnitude | Hormetic Zone Width |
|---|---|---|---|---|
| Brosimine B [15] | Retinal cells (OGD model) | 10.2 µM | ~40% increased viability | σ = 6.5 µM |
| Hydrogen Peroxide [2] | L929 cell line (OCH model) | 50 µM | 30-60% increased survival | Not specified |
| General Hormetic Response [10] | Multiple models | Varies by system | Typically 30-60% increase | ~0.1-10 × NOAEL |
Molecular Mechanisms: Linking History to Modern Redox Biology
Contemporary research has revealed the sophisticated molecular machinery underlying the hormetic observations made by ancient and historical figures. The Nrf2-Keap1 antioxidant defense pathway represents a central mechanism through which mild oxidative stress activates adaptive cellular responses [4] [16] [2].
The Nrf2-Keap1 Signaling Pathway
The Nrf2-Keap1 pathway serves as a primary sensor for electrophilic and oxidative stress, coordinating the expression of numerous cytoprotective genes:
Nrf2-Keap1 Pathway Activation
This pathway explains at a molecular level the adaptive responses observed in historical practices. When Mithridates regularly consumed sublethal doses of arsenic, he was likely activating his Nrf2 pathway, enhancing the production of detoxification enzymes and antioxidant proteins that provided protection against higher, lethal doses [11] [13].
Parallel Response Mechanisms in Hormesis
Successful hormetic responses typically involve the coordinated activation of multiple protective pathways beyond just antioxidant defenses [2]. These parallel mechanisms ensure comprehensive cellular protection:
- Antioxidant Response: Activation of Nrf2 and subsequent upregulation of enzymes like superoxide dismutase (SOD), catalase (CAT), and glutathione peroxidase (GPx) to manage redox homeostasis [2].
- Survival Pathway Activation: Simultaneous activation of transcription factors like NF-κB, leading to increased expression of anti-apoptotic proteins such as Bcl-2 [2].
- Protein Quality Control: Enhanced expression of heat shock proteins (HSP70, HSP90) to maintain proper protein folding and degradation [2].
- Metabolic Adaptation: Activation of pathways such as AMPK and sirtuins that modulate energy metabolism and mitochondrial function in response to low-energy stress [4].
The integration of these parallel responses ensures that cells not neutralize oxidative damage but also enhance their repair capacity and resist apoptotic signals, creating a comprehensive adaptive response [2].
Mitohormesis and Metabolic Regulation
Mitohormesis describes the specific adaptive responses of mitochondria to mild stress, particularly relevant to redox biology [12]. Low levels of mitochondrial reactive oxygen species (mtROS) activate signaling pathways that enhance mitochondrial function and cellular resilience:
- Sirtuin Activation: Low-dose oxidative stress activates sirtuins (e.g., SIRT1), which deacetylate and activate transcription factors like PGC-1α, promoting mitochondrial biogenesis [4] [13].
- AMPK Signaling: Energy stress activates AMPK, which inhibits anabolic processes and promotes catabolic pathways to restore energy balance [4].
- mTOR Modulation: Hormetic stressors can transiently inhibit mTOR signaling, promoting autophagy and cellular repair mechanisms [4].
These mitochondrial adaptations illustrate how the hormesis principle operates at the subcellular level, with mild stress optimizing organelle function and contributing to systemic health benefits.
Experimental Methodologies in Hormesis Research
Establishing Oxidative Conditioning Hormesis (OCH) Models
Research into redox hormesis requires carefully controlled experimental models that mimic the mild, intermittent stress that triggers adaptive responses. The Oxidative Conditioning Hormesis (OCH) model provides a standardized approach:
Protocol: Hydrogen Peroxide OCH in L929 Cells [2]
- Cell Culture: Maintain L929 murine fibroblast cells in standard culture conditions (DMEM with 10% FBS, 37°C, 5% CO₂).
- Hormetic Conditioning: Treat cells with a low dose of H₂O₂ (50 µM) for 9 hours.
- Recovery Period: Replace medium with fresh complete medium and incubate for 24 hours.
- Challenge Exposure: Expose preconditioned cells to a normally toxic dose of H₂O₂ (typically 300-500 µM).
- Assessment: Measure cell viability (MTT assay), apoptosis markers (annexin V/PI staining), and activation of defense pathways (Nrf2 nuclear translocation, antioxidant enzyme activity).
This OCH model demonstrates the fundamental hormesis principle: pretreatment with a mild stressor enhances cellular resistance to subsequent, more severe stress [2]. The molecular mechanisms include simultaneous activation of Nrf2-mediated antioxidant responses and NF-κB-mediated survival pathways [2].
Oxygen-Glucose Deprivation (OGD) Model for Neuroprotective Hormesis
The OGD model simulates ischemic conditions to study hormetic neuroprotection, particularly relevant for retinal and neuronal applications:
Protocol: Brosimine B Hormesis in Retinal Cells [15]
- Retinal Cell Culture: Prepare primary cultures of retinal cells from 7-day-old chicken embryos (Gallus gallus domesticus).
- OGD Induction:
- Transfer cells to glucose-free DMEM with low glucose (5.5 mM)
- Place in a sealed hypoxia chamber with 5% CO₂ and balanced N₂ for 3, 6, or 24 hours
- Maintain control cells in high-glucose DMEM (25 mM) in normal oxygen conditions
- Brosimine B Treatment: Apply Brosimine B across a concentration range (1-100 µM) at the beginning of the OGD period.
- Endpoint Assessments:
- Cell viability (MTT assay at 570 nm)
- ROS production (DCFH-DA fluorescence)
- Antioxidant enzyme activity (catalase, SOD assays)
- Computational modeling of dose-response using Gaussian hormetic model
This approach confirmed Brosimine B's hormetic neuroprotection, with peak efficacy at 10 µM enhancing cell viability and reducing ROS production, while higher concentrations (>10 µM) became cytotoxic [15].
OGD Experimental Workflow
In Vivo Models for Systemic Hormetic Responses
Translating cellular hormesis to whole-organism responses requires animal models that capture systemic adaptive mechanisms:
Protocol: Negative Air Ion (NAI) Exposure in Mice [8]
- Animal Subjects: Twenty 19-week-old C57BL/6J male mice divided into four groups:
- Short-term exposure (18 days NAI)
- Long-term exposure (28 days NAI)
- Corresponding control groups without NAI exposure
- NAI Exposure: Continuous exposure to NAI-enriched air generated by an air Cold Atmospheric Plasma-Nanoparticle Removal (aCAP-NR) device.
- Sample Collection: Blood and liver tissue collection after exposure period for metabolomic analysis.
- Metabolomic Profiling: Targeted metabolomics using UHPLC-MS to assess:
- Glutathione metabolism
- Lipid peroxidation products
- Purine metabolism
- Energy metabolism intermediates
This study demonstrated that NAI exposure elicits a hormetic metabolic response, with short-term exposure enhancing mitochondrial efficiency and long-term exposure inducing adaptive reprogramming, including increased inosine levels suggesting enhanced antioxidant and anti-inflammatory responses [8].
The Scientist's Toolkit: Essential Reagents and Models
Table 4: Key Research Reagents and Experimental Models for Hormesis Research
| Reagent/Model | Application in Hormesis Research | Experimental Function | Example Use |
|---|---|---|---|
| Hydrogen Peroxide [2] | Oxidative Conditioning Hormesis (OCH) | Induces mild oxidative stress to trigger adaptive Nrf2 and NF-κB pathways | 50 µM for 9 hours in L929 cells to establish preconditioning [2] |
| Brosimine B [15] | Natural Product Hormesis | Flavonoid with biphasic effects on cell viability; model for therapeutic window determination | 10 µM for neuroprotection in retinal OGD model [15] |
| Sulforaphane [13] | Nrf2 Pathway Activation | Isothiocyanate from cruciferous vegetables; directly modifies Keap1 cysteine residues | Prototype inducer of phase II detoxification enzymes via Nrf2 [13] |
| Oxygen-Glucose Deprivation (OGD) [15] | Ischemic Preconditioning Model | In vitro simulation of ischemia to study neuroprotective hormesis | 3-24 hour exposure in retinal cells to study Brosimine B effects [15] |
| Primary Retinal Cell Culture [15] | Neuronal Hormesis Model | Highly metabolically active tissue sensitive to oxidative stress; model for CNS hormesis | Avian retinal cells for studying oxidative stress neuroprotection [15] |
| L929 Fibroblast Cell Line [2] | Standardized OCH Model | Murine connective tissue cell line for reproducible oxidative conditioning studies | Hydrogen peroxide OCH model establishment [2] |
| C57BL/6J Mice [8] | In Vivo Hormesis Modeling | Well-characterized mouse strain for whole-organism metabolic and physiological adaptations | NAI exposure studies on metabolic reprogramming [8] |
The journey from Mithridatism and Paracelsus' foundational principle to contemporary molecular understanding of hormesis represents one of the most enduring narratives in biological science. What began as ancient observations of moderation and practical attempts to build poison resistance has evolved into a sophisticated framework for understanding how biological systems dynamically respond to stress through redox signaling pathways, transcriptional reprogramming, and metabolic adaptations [11] [4] [16].
For today's researchers and drug development professionals, recognizing the historical context of hormesis provides crucial insights for experimental design and therapeutic development. The consistent quantitative features of hormetic responses—their modest magnitude (typically 30-60% enhancement) and defined dose range (0.1-10 × NOAEL)—offer practical guidelines for identifying genuine hormetic effects versus experimental artifacts [10]. The molecular machinery centered around the Nrf2-Keap1 pathway provides mechanistic validation of Paracelsus' principle that "the dose makes the poison," revealing how cells distinguish between signaling and damaging levels of oxidative stress [16] [2] [13].
As redox biology continues to advance, the hormesis concept provides a unifying framework for investigating diverse phenomena—from mitochondrial adaption and inflammatory preconditioning to dietary phytochemical benefits and exercise-induced resilience [4] [8] [13]. The experimental methodologies and research tools detailed in this whitepaper offer starting points for exploring these applications across different biological systems and therapeutic areas.
The continuing evolution of hormesis from ancient observation to modern molecular mechanism underscores its fundamental importance in biology and medicine. Future research will likely refine our understanding of how these adaptive responses are integrated across organ systems and how they might be harnessed for precision medicine approaches to prevent and treat disease.
Reactive oxygen species (ROS) are oxygen-derived chemical molecules characterized by their reactivity. This group includes both free radicals, such as the superoxide anion (O₂•⁻) and hydroxyl radical (HO•), and non-radical species like hydrogen peroxide (H₂O₂) [17]. For decades, ROS were primarily viewed as toxic byproducts of aerobic metabolism, inflicting damage on cellular components. However, a paradigm shift has occurred with the understanding that at low levels, ROS serve as essential signaling molecules in numerous physiological processes, while at high levels, they cause oxidative distress and damage [18] [19]. This concentration-dependent dualism is a classic example of hormesis, where low-level exposure elicits an adaptive beneficial response, and high-level exposure causes harm [17].
The conceptual framework of redox biology posits that the intracellular redox potential is a tightly regulated homeostatic parameter. The balance between pro-oxidant generation and antioxidant defenses determines the cellular outcome [17]. This review will delve into the molecular mechanisms of ROS as signaling messengers and toxic agents, frame this duality within the hormesis model, and provide researchers with the quantitative data and methodological tools essential for probing this complex field.
Molecular Mechanisms: From Signaling to Damage
ROS as Second Messengers in Redox Signaling
At low, physiological concentrations (typically in the nanomolar range for H₂O₂), ROS function as pivotal second messengers in redox signaling [19]. A primary mechanism involves the reversible oxidation of cysteine residues within proteins. At physiological pH, certain cysteine residues exist as a thiolate anion (Cys-S⁻), making them highly susceptible to oxidation by H₂O₂ to form sulfenic acid (Cys-SOH) [19]. This modification can alter protein function, activity, and interaction.
A canonical example is the signaling cascade initiated by growth factors such as Epidermal Growth Factor (EGF) and Platelet-Derived Growth Factor (PDGF). Their binding to Receptor Tyrosine Kinases (RTKs) activates NADPH oxidases (NOX), which generate a localized burst of O₂•⁻, rapidly dismutated to H₂O₂ [19]. This H₂O₂ then reversibly oxidizes and inactivates protein tyrosine phosphatases (PTPs) like PTP1B, as well as the lipid phosphatase PTEN. The transient inhibition of these negative regulators reinforces and prolongs the activation of downstream pro-growth and pro-survival pathways, such as PI3K-AKT and RAS-MEK-ERK [19]. The redox signal is terminated when enzymes like thioredoxin (TRX) reduce the oxidized cysteine back to its thiol state, demonstrating the precise and reversible nature of this regulation [17] [19].
The Transition to Oxidative Stress and Damage
When ROS generation overwhelms the antioxidant capacity of the cell—a state of oxidative distress—the same chemical properties that enable signaling lead to irreversible damage [17]. The sulfenic acid modification on cysteines can be further oxidized to sulfinic (Cys-SO₂H) and sulfonic (Cys-SO₃H) acids, which are often irreversible and lead to permanent protein dysfunction [19].
Furthermore, highly reactive species like the hydroxyl radical (HO•), produced via the Fenton reaction between H₂O₂ and ferrous iron (Fe²⁺), can indiscriminately attack all major classes of macromolecules [19]. This results in:
- Lipid peroxidation: Damaging cell membranes and generating reactive aldehydes that can propagate injury [20].
- Protein carbonylation: Irreversibly modifying proteins, leading to loss of function and aggregation [20].
- DNA damage: Causing strand breaks and base modifications, which can lead to genomic instability [20] [19].
This oxidative damage to biomolecules is a hallmark of numerous chronic diseases and contributes to the aging process [17] [21].
Table 1: Key Reactive Oxygen Species and Their Roles in Signaling and Damage
| ROS | Chemical Nature | Primary Sources | Signaling Role | Damaging Actions |
|---|---|---|---|---|
| Superoxide (O₂•⁻) | Free radical | Mitochondrial ETC, NOX enzymes | Limited; precursor for H₂O₂, can inactivate Fe-S cluster proteins | Inactivates Fe-S cluster enzymes, precursor to more reactive species |
| Hydrogen Peroxide (H₂O₂) | Non-radical | SOD action on O₂•⁻, NOX | Major redox messenger; reversibly oxidizes protein cysteine thiols | Precursor to HO•, can cause irreversible protein overoxidation |
| Hydroxyl Radical (HO•) | Free radical | Fenton reaction (H₂O₂ + Fe²⁺) | None; too reactive and non-specific | Indiscriminate oxidation of lipids, proteins, and DNA |
The following diagram illustrates the central hormesis concept of ROS, showing the transition from physiological signaling to pathological damage as concentrations increase.
The Hormetic Framework in Redox Biology
The biphasic dose-response of ROS is a textbook example of hormesis. Hormesis in redox biology refers to the phenomenon where mild, subtoxic levels of ROS induce an adaptive, protective resilience in cells and tissues [17]. This "pre-conditioning" effect is achieved through the stimulation of redox-sensitive signaling pathways that lead to:
- Upregulation of antioxidant defenses: Increased expression of enzymes like superoxide dismutase (SOD), catalase (CAT), and peroxiredoxins (Prx) via transcription factors such as Nrf2 [17].
- Stimulation of repair mechanisms: Enhanced systems for clearing and repairing damaged proteins and DNA.
- Promotion of cell survival and proliferation: Activation of growth-promoting pathways [17].
Conversely, supraphysiological ROS production exhausts these adaptive systems, leading to the damaging consequences of oxidative distress [17]. The GSH/GSSG ratio is one of the most reliable markers of this intracellular redox equilibrium, shifting towards a more oxidized state under distress [17]. The therapeutic implication is profound: strategies aiming to broadly suppress all ROS with high-dose antioxidants may inadvertently blunt beneficial hormetic signaling, whereas approaches that modulate ROS or boost the endogenous antioxidant response may be more successful [17].
Quantitative Data: Measuring ROS and Oxidative Stress
Quantifying ROS is methodologically challenging due to their high reactivity, short half-lives, and low steady-state concentrations [20]. The choice of technique depends on the specific research question, including the ROS of interest, desired spatial and temporal resolution, and the biological system.
Table 2: Quantitative Methods for ROS Detection and Analysis
| Method | Principle | Key Metrics | Applications | Considerations |
|---|---|---|---|---|
| Electron Paramagnetic Resonance (EPR) | Direct detection of unpaired electrons in radical species using spin traps. | Absolute concentration of radical species (e.g., in capillary blood) [20]. | "Gold standard" for direct ROS measurement; validated in human studies comparing healthy vs. diseased states [20]. | Provides a snapshot of "instantaneous" ROS production; can be technically complex. |
| Fluorescent Probes (e.g., DCFH-DA) | Oxidation of non-fluorescent probe to a fluorescent product by ROS. | Relative fluorescence intensity, proportional to cellular ROS levels. | Cell-based assays, flow cytometry; high-throughput screening. | Susceptible to artifacts (e.g., auto-oxidation); semi-quantitative. |
| Histochemical Staining (DAB, NBT) | ROS-mediated precipitation of colored dyes (brown for DAB/H₂O₂, blue for NBT/O₂•⁻). | Staining area and intensity, quantified by image analysis [22]. | Spatial distribution of ROS in tissues (e.g., plant leaves, histological sections) [22]. | Qualitative to semi-quantitative; requires careful validation and image analysis. |
| Two-Photon Microscopy (TP-FRIM/TP-FLIM) | Ratiometric (FRIM) or fluorescence lifetime (FLIM) imaging of redox-sensitive probes. | Spatial distribution and quantification of specific redox couples (e.g., GSH:GSSG) [23]. | Intravital imaging of deep tissues; high spatiotemporal resolution of redox state [23]. | Requires specialized equipment and genetically encoded or chemical probes. |
Experimental Protocols for ROS Research
Protocol: Direct ROS Measurement in Human Blood Using EPR
This microinvasive method allows for the direct quantification of ROS production rates in capillary blood and has been applied to compare different physiological and pathological states [20].
- Sample Collection: Collect approximately 50 μL of capillary blood from a fingertip into a heparinized capillary tube. Alternatively, 3 mL of venous blood can be drawn from an antecubital vein into heparinized Vacutainer tubes [20].
- Sample Preparation:
- For venous blood, separate plasma by centrifugation at 1,000 × g for 10 minutes at 4°C.
- After plasma removal, carefully collect aliquots of red blood cells (RBCs), discarding the buffy coat.
- Immediately transfer 50 μL of capillary blood, venous whole blood, plasma, or RBCs to EPR analysis.
- EPR Analysis: Mix the blood sample with a spin trap solution (e.g., CMH spin trap). The spin trap reacts with short-lived radicals to form more stable, detectable adducts.
- Data Acquisition and Quantification: Record the EPR spectrum. The amplitude of the EPR signal is proportional to the concentration of the radical adduct, allowing for the calculation of the absolute ROS production rate. Studies show a significant linear relationship between ROS measured in capillary blood and venous blood/plasma/RBCs, validating the capillary method [20].
Protocol: Imaging ROS in Plant Leaves via Histochemistry and Automated Image Analysis
This protocol details the visualization and quantification of H₂O₂ and O₂•⁻ in plant leaves using histochemical staining and automated analysis via the Fiji (ImageJ) platform [22].
- Leaf Staining:
- For H₂O₂ detection: Infiltrate leaves with 3,3'-diaminobenzidine (DAB) solution (1 mg/mL, pH 3.8). Incubate in the dark for 4-8 hours. H₂O₂ polymerizes DAB, producing a brown precipitate [22].
- For O₂•⁻ detection: Infiltrate leaves with nitro blue tetrazolium (NBT) solution (0.1 mg/mL in 10 mM potassium phosphate buffer, pH 7.8). Incubate in the dark for 30-90 minutes. O₂•⁻ reduces NBT to an insoluble blue formazan precipitate [22].
- Destaining and Preservation: After staining, clear the leaves by boiling in 96% ethanol for 10 minutes to remove chlorophyll, which masks the staining. Store the destained leaves in 50% glycerol [22].
- Image Acquisition: Scan the destained leaves using a flatbed scanner at a standard resolution (e.g., 600 DPI).
- Automated Image Analysis with Fiji:
- Open the leaf image in Fiji.
- Use the Trainable Weka Segmentation (TWS) plugin. Manually label representative areas of the stained regions and the unstained leaf background on a subset of images to train a pixel classifier.
- Apply the trained classifier to all images to segment and identify stained (ROS-positive) pixels automatically.
- Quantify the results as the percentage of the total leaf area that is stained. This method has shown high accuracy (Dice Similarity Coefficient ≈ 0.92) compared to manual assessment [22].
The workflow for this automated image analysis is summarized below.
Table 3: Essential Research Reagents and Tools for Redox Biology
| Tool / Reagent | Function/Description | Example Application |
|---|---|---|
| CMH Spin Trap | Cyclic hydroxylamine that reacts with O₂•⁻ and other radicals to form stable nitroxides detectable by EPR. | Direct quantification of superoxide production rates in biological samples like blood [20]. |
| DAB (3,3'-Diaminobenzidine) | Chromogen that polymerizes to a brown precipitate in the presence of H₂O₂ and peroxidase. | Histochemical staining for visualizing spatial distribution of H₂O₂ in tissues (e.g., plant leaves) [22]. |
| NBT (Nitro Blue Tetrazolium) | Yellow-colored tetrazolium salt reduced to insoluble blue formazan by O₂•⁻. | Histochemical staining for detecting superoxide anion localization in tissues and cells [22]. |
| Genetically Encoded Sensors (e.g., roGFP, HyPer) | Fluorescent proteins whose excitation/emission properties change upon oxidation or binding to specific ROS (e.g., H₂O₂). | Real-time, compartment-specific monitoring of redox dynamics in live cells [23]. |
| N-Acetylcysteine (NAC) | Precursor for glutathione (GSH) synthesis; acts as a broad-spectrum antioxidant. | Experimentally modulating cellular redox state to test the role of ROS in signaling pathways [19]. |
| NADPH Oxidase (NOX) Inhibitors (e.g., VAS2870, Apocynin) | Pharmacological agents that inhibit specific sources of ROS generation. | Dissecting the contribution of NOX-derived ROS vs. mitochondrial ROS in cellular processes [17]. |
The understanding of reactive oxygen species has evolved from a monolithic view of them as purely toxic agents to a nuanced appreciation of their dual role governed by the hormesis principle. Low, finely controlled concentrations of ROS are indispensable for physiological signaling, regulating processes from growth to immunity. Conversely, a loss of this control leads to oxidative stress, which is implicated in a myriad of diseases and aging. The future of therapeutic intervention in this field lies not in the non-selective scavenging of all ROS, but in the precise modulation of redox pathways—either by boosting endogenous antioxidant systems in states of deficiency or by selectively inducing ROS in contexts like cancer therapy to push malignant cells beyond their redox tolerance [17]. Mastering this delicate balance is the next frontier in redox biology and medicine.
The Oxygen Paradox and Evolutionary Conservation of Redox Adaptive Responses
The Oxygen Paradox describes the fundamental biological contradiction wherein oxygen, while indispensable for aerobic life, generates reactive oxygen species (ROS) that damage vital cellular structures and contribute to aging and disease [24]. This paradox is resolved through evolutionarily conserved redox adaptive responses known as hormesis, wherein low-dose oxidative stress activates protective signaling pathways that enhance cellular resilience. These adaptive mechanisms, observed from bacteria to humans, involve sophisticated sensing of redox imbalances and activation of genes coordinating antioxidant defense, protein homeostasis, and metabolic reprogramming. This whitepaper examines the molecular underpinnings of these conserved pathways, their quantitative dynamics, and their implications for therapeutic development, providing researchers with methodological frameworks for investigating redox biology in experimental and clinical contexts.
The Oxygen Paradox represents a foundational concept in redox biology, capturing the dual nature of oxygen as both essential for energy metabolism and inherently dangerous due to its conversion to reactive species [24]. This paradox emerged evolutionarily approximately 2.5 billion years ago with the Great Oxidation Event, which forced organisms to develop sophisticated antioxidant networks to mitigate oxygen toxicity while harnessing its metabolic potential [25]. The resolution to this paradox lies in the phenomenon of hormesis—an adaptive response where exposure to low doses of a stressor induces resistance to higher, potentially toxic doses of the same or similar stressors [4].
Hormetic responses follow a characteristic biphasic dose-response curve, typically J-shaped or inverted U-shaped, where low doses stimulate beneficial adaptations while high doses cause damage [4]. In redox biology, this manifests as adaptive homeostasis, wherein transient expansion of the homeostatic range occurs in response to subtoxic oxidative signaling molecules [24]. The mechanistic basis involves activation of conserved redox-sensitive transcription factors, enhancement of antioxidant systems, and remodeling of proteostatic networks [24] [4]. Understanding these evolutionarily conserved mechanisms provides crucial insights for developing interventions targeting age-related diseases, cancer, and degenerative disorders where redox imbalance is a pathological feature.
Evolutionary Conservation of Redox Adaptation
Phylogenetic Evidence and Molecular Mechanisms
The molecular machinery governing redox adaptation demonstrates remarkable evolutionary conservation from simple organisms to humans. The glutathione (GSH) system, a pivotal component of the antioxidant network, appears across phylogeny, with homologous synthesis and utilization pathways in bacteria, plants, invertebrates, and mammals [25]. Even phototrophic bacteria possess GSH synthesis capabilities, indicating the ancient origin of this redox buffering system [25]. The preparation for oxidative stress (POS) hypothesis further demonstrates this conservation, documenting 83 animal species across 8 phyla that upregulate antioxidant defenses during hypoxia to prepare for reoxygenation stress [26].
At the molecular level, key redox-sensing transcription factors show striking conservation:
- The Nrf2-Keap1 pathway (or its orthologs) is conserved from Drosophila (CncC-Keap1) to vertebrates, regulating proteasome expression and oxidative stress resistance [24]
- Hypoxia-inducible factors mediate oxygen sensing across metazoans
- NF-κB and FoxO pathways integrate redox signals in immune and stress responses from insects to mammals
These conserved pathways enable organisms to dynamically adjust their antioxidant capacity based on oxidative challenges, representing a fundamental adaptation to the Oxygen Paradox [25] [26].
Temporal Adaptation Patterns
Redox adaptation mechanisms operate across different timescales, from rapid post-translational modifications to long-term evolutionary adaptations:
Table 1: Timescales of Redox Adaptive Mechanisms
| Timescale | Adaptive Mechanism | Key Components | Biological Outcome |
|---|---|---|---|
| Seconds-Minutes | Enzyme modification | GST oxidation, γGCS activation | Immediate antioxidant enhancement |
| Hours-Days | Transcriptional activation | Nrf2 translocation, ARE activation | Increased antioxidant gene expression |
| Days-Weeks | Epigenetic modification | DNA methylation, histone changes | Sustained adaptive phenotypes |
| Generations | Genomic evolution | Gene selection, pathway refinement | Species-level adaptation |
The short-term adaptations include direct oxidation of glutathione-S-transferases, enhancing their activity, and oxidation-induced conformational changes in γ-glutamylcysteine synthetase relieving feedback inhibition to boost GSH synthesis [25]. On an intermediate timescale, ROS oxidize specific cysteine residues (Cys273, 288, 151) on Keap1, promoting Nrf2 nuclear translocation and antioxidant response element-mediated gene expression [25]. Long-term adaptations occur through epigenetic modifications and selective pressures on genomic sequences, fine-tuning redox regulatory networks over evolutionary timescales [25].
Quantitative Analysis of Redox Adaptive Responses
Redox Potentials and Homeostatic Ranges
Quantitative redox biology provides crucial insights into the dynamics of adaptive responses. The redox state of key thiol couples, particularly the GSSG/2GSH couple, serves as an important indicator of cellular redox environment, best assessed using the Nernst equation:
[ E_{hc} = -252 - \frac{61.5}{2} \log \frac{[GSH]^2}{[GSSG]} \text{ in mV at } 37^\circ C, \text{pH} = 7.2 ]
where (E_{hc}) represents the half-cell reduction potential [27]. Notably, the absolute concentration of GSH significantly influences interpretation—a cell with 10 mM GSH requires a [GSH]/[GSSG] ratio of only 16.6 to achieve the same -228 mV potential as a cell with 1 mM GSH needing a ratio of 166 [27]. This quantitative understanding is essential for comparing redox states across different experimental systems and biological states.
Table 2: Quantitative Parameters of Redox Adaptive Responses
| Parameter | Typical Range | Measurement Significance | Experimental Considerations |
|---|---|---|---|
| [GSH]/[GSSG] ratio | 1-100 mM (GSH), <1% GSSG | Major cellular redox buffer | Total GSH concentration affects ratio interpretation |
| H₂O₂ flux | Nanomolar signaling range | Secondary messenger concentration | Spatial compartmentalization critical |
| Mitochondrial ROS | ~0.2% O₂ conversion | Primary endogenous ROS source | Electron availability limits production |
| Nrf2 activation | Picomolar-nanomolar inducer | Adaptive homeostasis trigger | Different from toxic millimolar concentrations |
| Antioxidant induction | 30-80% increase in POS | Protection magnitude | Transient, returns to baseline post-challenge |
The Superoxide-Peroxide Removal System
The superoxide-peroxide removal (SPR) system forms the core network balancing ROS generation and elimination [27]. This system comprises several interconnected enzymes:
- Superoxide dismutases convert O₂•⁻ to H₂O₂
- Catalase decomposes H₂O₂ to H₂O and O₂
- Glutathione peroxidases reduce H₂O₂ and lipid peroxides using GSH
- Peroxiredoxins eliminate H₂O₂, organic hydroperoxides, and peroxynitrite
- Thioredoxin and glutaredoxin systems regenerate oxidized protein thiols
The SPR system exhibits organelle-specific isoforms that maintain compartmentalized redox environments, with mitochondrial (MnSOD), cytosolic (CuZnSOD), and extracellular SOD isoforms performing specialized functions [27]. Quantitative analysis reveals that mitochondrial MnSOD concentration can be 10-fold higher in the mitochondrial matrix than cytosolic CuZnSOD concentration, despite similar activity units, highlighting the importance of absolute quantification over relative measurements [27].
Methodologies for Investigating Redox Adaptive Responses
Experimental Models and Protocols
Investigation of the Oxygen Paradox and redox adaptation employs diverse model systems and methodological approaches:
Invertebrate Models:
- Drosophila melanogaster: Studies demonstrate age-dependent decline in adaptive homeostasis, with young flies showing H₂O₂ stress adaptation and increased Lon protease expression, while old flies lose this capacity [24]. Transgenic Nrf2 (CncC) activation in young flies upregulates proteasome expression and confers proteotoxic stress resistance.
Mammalian Cell Systems:
- Human Peripheral Blood Mononuclear Cells (PBMCs): The "normobaric oxygen paradox" model exposes cells to varying oxygen concentrations (30%, 100%, 140% O₂) followed by return to normoxia, measuring time-dependent activation of HIF-1α, Nrf2, and mitochondrial biogenesis factors [28].
- Hematopoietic Stem/Progenitor Cells: Redox proteomic analyses compare fetal versus adult cells, identifying 4,438 cysteine residues with differential oxidation susceptibility, highlighting ontogenic changes in redox regulation [29].
POS Induction Protocol:
- Subject organisms to mild hypoxia (2-8 hours, depending on species)
- Maintain at reduced oxygen tension (1-5% O₂)
- Monitor antioxidant enzyme activities (SOD, catalase, GST) during hypoxia and reoxygenation
- Assess oxidative damage markers (protein carbonylation, lipid peroxidation)
- Measure phosphorylation status of redox-sensitive kinases
This protocol typically yields 30-80% increases in antioxidant activities during hypoxia, which return to baseline during reoxygenation [26].
Redox Proteomics and Quantitative Mass Spectrometry
Quantitative redox proteomics enables comprehensive mapping of reversible cysteine oxidation across the proteome:
Workflow:
- Cell lysis under non-reducing conditions with alkylating agents
- Protein digestion with trypsin
- Enrichment of oxidized peptides using thiol-affinity techniques
- LC-MS/MS analysis with isotopic labeling for quantification
- Bioinformatic analysis to identify redox-sensitive cysteine residues
This approach identified ontogenic changes in oxidation state of thiols acting in mitochondrial respiration and protein homeostasis during hematopoietic development and MLL-ENL leukemogenesis [29]. The technology enables detection of specific oxidative post-translational modifications including S-glutathionylation, S-nitrosylation, and sulfenic acid formation that function as redox switches in signaling [30].
Signaling Pathways in Redox Adaptation
The Nrf2-Keap1-ARE Pathway
The Nrf2-Keap1 pathway represents the master regulator of antioxidant gene expression and is highly conserved in redox adaptation:
Pathway Mechanism: Under basal conditions, Keap1 targets Nrf2 for ubiquitination and proteasomal degradation. During oxidative stress, specific cysteine residues (Cys151, 273, 288) on Keap1 become oxidized, causing conformational changes that disrupt Nrf2 ubiquitination. Stabilized Nrf2 translocates to the nucleus, heterodimerizes with small Maf proteins, and binds to Antioxidant Response Elements upstream of genes encoding GST, GSH synthesizing enzymes, NADPH-quinone oxidoreductase, and heme oxygenase-1 [24] [30]. This pathway exemplifies adaptive homeostasis by transducing subtoxic oxidative signals into protective gene expression.
Mitochondrial Biogenesis in Redox Adaptation
Mitochondrial biogenesis integrates with redox adaptation through coordinated regulation by PGC-1α, Nrf2, and TFAM:
Regulatory Network: The normobaric oxygen paradox demonstrates that pulsed hyperoxia (30-140% O₂) activates PGC-1α nuclear translocation, which coactivates Nrf2 expression [28]. Nrf2 then induces NRF1 expression, which together with PGC-1α activates mitochondrial transcription factor A expression, driving mitochondrial biogenesis [28]. This coordinated response enhances mitochondrial quality and function, improving cellular capacity to manage oxidative challenges. The specificity of response varies with oxygen dose—mild hyperoxia (30% O₂) robustly induces TFAM expression, while higher doses (100-140% O₂) show attenuated effects despite PGC-1α activation [28].
The Scientist's Toolkit: Essential Research Reagents and Models
Table 3: Research Reagent Solutions for Redox Biology Investigations
| Reagent/Model | Application | Key Function | Experimental Considerations |
|---|---|---|---|
| Drosophila melanogaster | Aging studies, genetic screens | Conserved Nrf2 ortholog (CncC) | Age-dependent response differences |
| Human PBMCs | Normobaric oxygen paradox | HIF-1α and Nrf2 activation | Dose-dependent response to O₂ levels |
| NADPH oxidase inhibitors | ROS source identification | Selective blockade of enzymatic ROS | Compartment-specific effects |
| Nrf2 activators | Hormesis induction | Subtoxic pathway priming | Concentration-critical window |
| GSH/GSSG probes | Redox potential measurement | Quantitative assessment with Nernst equation | Absolute concentration matters |
| Redox proteomics | Cysteine oxidation mapping | Identification of redox-sensitive proteins | Preservation of oxidation state |
| POS animal models | Hypoxia-tolerant species | Natural hormesis models | Tissue-specific antioxidant responses |
The Oxygen Paradox continues to frame our understanding of redox biology, with evolutionarily conserved adaptive responses providing protection against oxidative challenges. The field is advancing toward quantitative redox biology that integrates absolute measurements of reactive species, redox potentials, and reaction kinetics to model network behavior [27]. Future research will leverage single-cell redox imaging to resolve spatial compartmentalization of signaling, cryo-EM to visualize redox-sensitive protein complexes, and multi-omics integration to map systems-level responses to oxidative challenges.
Therapeutic applications targeting redox adaptation mechanisms show promise in preclinical models, with NRF2 activators in clinical trials for chronic kidney disease and neurodegenerative disorders [30]. However, the hormetic principle necessitates precise dosing, as excessive NRF2 activation promotes tumor growth in some contexts [24] [30]. The emerging paradigm recognizes ROS as specific signaling molecules rather than mere toxic byproducts, suggesting future therapies will target specific redox-sensitive nodes rather than applying blanket antioxidant approaches [17] [30]. This refined understanding of the Oxygen Paradox and its evolutionary solutions continues to inspire novel therapeutic strategies for diseases of aging and metabolism.
This whitepaper provides a comprehensive analysis of the glutathione (GSH) system and redox-sensitive transcription factors, framing their interplay within the mechanistic context of hormesis in redox biology. The tripeptide glutathione serves as the central coordinator of cellular redox homeostasis, while transcription factors including Nrf2, NF-κB, and AP-1 function as molecular sensors that translate oxidative challenges into adaptive genetic responses. We examine how low-level oxidative stress activates these pathways to enhance cellular resilience—a phenomenon fundamental to hormesis. The content includes detailed experimental methodologies, structured quantitative data comparisons, and visual representations of signaling pathways to serve researchers, scientists, and drug development professionals working at the intersection of redox biology and therapeutic development.
The Glutathione (GSH) System: Architecture and Functions
Biochemical Fundamentals and Homeostasis
Glutathione (γ-L-glutamyl-L-cysteinyl-glycine) represents the most abundant low-molecular-weight thiol in biological systems, functioning as the primary redox buffer against oxidative and nitrosative stress [31]. Its reducing power resides in the thiol (-SH) group of its cysteine residue, which serves as an electron donor in redox reactions. The glutathione system maintains a dynamic equilibrium between reduced (GSH) and oxidized (GSSG) forms, with physiological GSH:GSSG ratios typically ranging from 10:1 to 100:1 in various cellular compartments [31]. This redox couple exists in a metastable state rather than a true equilibrium, with its reducing power maintained through enzymatic catalysis rather than spontaneous reactions [32].
Cellular glutathione distribution follows a compartment-specific pattern: approximately 90% resides in the cytosol (the primary site of synthesis), with the remainder distributed to mitochondria, nucleus, and endoplasmic reticulum [31]. The endoplasmic reticulum uniquely maintains a more oxidized environment where GSSG predominates, supporting disulfide bond formation during protein folding [31]. This subcellular partitioning enables compartment-specific redox regulation tailored to organellar functions.
Table 1: Glutathione System Components and Characteristics
| Component | Characteristics | Localization | Primary Function |
|---|---|---|---|
| GSH | Tripeptide (Glu-Cys-Gly); 1-10 mM concentration | Cytosol, mitochondria, nucleus | Redox buffering, detoxification, peroxide scavenging |
| GSSG | Disulfide-linked dimer; <10% of total GSH pool | All compartments, enriched in ER | Oxidized storage form; protein disulfide formation |
| GCL | Heterodimer (GCLC + GCLM); rate-limiting enzyme | Cytosol | Catalyzes γ-glutamylcysteine formation from Glu and Cys |
| GS | Homodimer; ATP-dependent | Cytosol | Adds glycine to γ-glutamylcysteine to form GSH |
| GR | NADPH-dependent flavoenzyme | Cytosol, mitochondria | Reduces GSSG back to GSH, maintaining reduced pool |
| GGT | Membrane-bound heterodimeric glycoprotein | Plasma membrane (kidney, biliary, brain) | Initiates extracellular GSH degradation and recycling |
Synthesis, Regulation, and Recycling
Glutathione biosynthesis occurs through two consecutive ATP-dependent enzymatic reactions [31]. The first and rate-limiting step is catalyzed by glutamate-cysteine ligase (GCL), a heterodimeric enzyme composed of catalytic (GCLC) and modulatory (GCLM) subunits that forms an unusual γ-peptide bond between glutamate and cysteine. The second reaction, catalyzed by glutathione synthetase (GS), adds glycine to form the complete tripeptide. Multiple factors control GSH synthesis, including substrate availability (particularly L-cysteine), GCL subunit expression ratios, feedback inhibition of GCL by GSH, and ATP provision [31].
The glutathione reduction-recycling system maintains the reduced GSH pool through NADPH-dependent enzymes. Glutathione reductase (GR) catalyzes the reduction of GSSG back to GSH, consuming NADPH in the process [33]. In fission yeast (and homologs in higher eukaryotes), GR (Pgr1) demonstrates dual cytosolic and mitochondrial localization, with mitochondrial GR being particularly essential for maintaining redox balance in that compartment [33]. The thioredoxin and glutaredoxin systems provide complementary electron donor pathways that work in concert with glutathione to maintain cellular reducing conditions [33].
Molecular Mechanisms of Redox Regulation
Glutathione participates in redox regulation through multiple mechanistic pathways. It directly scavenges reactive oxygen and nitrogen species (ROS/RNS) through non-enzymatic reactions and serves as an essential cofactor for glutathione peroxidase (GPX) in the reduction of hydroperoxides [31]. Perhaps most significantly, glutathione mediates reversible post-translational protein modifications through S-glutathionylation—the formation of mixed disulfides between protein cysteinyl residues and glutathione [31].
Unlike spontaneous thermodynamic equilibration, protein S-glutathionylation is enzymatically controlled, primarily by glutaredoxins (Grxs) and certain glutathione S-transferases, which catalyze both the addition and removal of glutathione moieties [32]. This enzymatic control ensures specificity and appropriate reaction kinetics for signaling purposes. Through this mechanism, glutathione regulates numerous cellular processes including DNA synthesis via ribonucleotide reductase, apoptosis via caspase-3 modulation, and vessel formation via sirtuin 1 regulation [32].
Redox-Sensitive Transcription Factors: Molecular Sensors and Effectors
Redox-sensitive transcription factors function as molecular sensors that convert changes in cellular redox state into altered gene expression patterns. These factors contain critical cysteine residues that undergo reversible oxidative modifications, leading to conformational changes, altered DNA binding affinity, or modified interactions with regulatory proteins [34]. The primary transcription factors involved in redox sensing include Nuclear Factor-E2-related factor-2 (Nrf2), Nuclear Factor-kappa B (NF-κB), and Activator Protein-1 (AP-1), each responding to distinct but overlapping redox signals.
Table 2: Redox-Sensitive Transcription Factors and Functions
| Transcription Factor | Redox Sensor | Target Genes | Biological Functions | Role in Hormesis |
|---|---|---|---|---|
| Nrf2 | Cysteine residues in Keap1 | ARE-driven genes: antioxidant enzymes, phase II detoxification enzymes | Antioxidant defense, detoxification, metabolic adaptation | Primary mediator of adaptive responses to low-dose stressors |
| NF-κB | Cysteine residues in IKK complex and DNA-binding domains | Pro-inflammatory cytokines, chemokines, adhesion molecules | Inflammation, immune response, cell survival | Biphasic response: low doses enhance defense, high doses promote damage |
| AP-1 | Redox-sensitive cysteine residues in Fos/Jun subunits | Matrix metalloproteinases, cyclin D1, pro-inflammatory genes | Cell proliferation, differentiation, apoptosis | Context-dependent modulation of stress responses |
| HIF-1α | Oxygen-dependent degradation domain; redox-sensitive | Glycolytic enzymes, VEGF, erythropoietin | Angiogenesis, metabolic adaptation to hypoxia | Links oxygen sensing to redox adaptation |
Nrf2-Keap1-ARE Pathway: Master Regulator of Antioxidant Defense
The Nrf2-Keap1 system represents the primary cellular defense mechanism against oxidative and electrophilic stress [34] [30]. Under basal conditions, Nrf2 is sequestered in the cytoplasm by its inhibitor Keap1, which targets Nrf2 for constitutive ubiquitination and proteasomal degradation. Oxidative stress or exposure to electrophilic compounds triggers conformational changes in Keap1 through modification of specific cysteine residues, leading to Nrf2 stabilization and nuclear translocation [13]. In the nucleus, Nrf2 binds to Antioxidant Response Elements (AREs) in the promoter regions of over 500 cytoprotective genes [30].
Nrf2 target genes include those encoding antioxidant enzymes (superoxide dismutase, catalase, glutathione peroxidase), glutathione synthesis enzymes (GCL, GS), phase II detoxification enzymes (glutathione S-transferases, NADPH:quinone oxidoreductase), and proteins involved in glutathione regeneration [30] [35]. This coordinated gene expression program enhances cellular capacity to neutralize reactive species, eliminate electrophilic toxins, and maintain redox homeostasis. The Nrf2 pathway is particularly significant in hormesis, as many hormetic compounds (e.g., sulforaphane, curcumin, quercetin) act through this mechanism to induce adaptive protection [13].
NF-κB Pathway: Inflammatory Signaling and Redox Control
NF-κB comprises a family of Rel-related transcription factors that serve as critical regulators of inflammatory and immune responses [36]. In unstimulated cells, NF-κB is sequestered in the cytoplasm by inhibitory IκB proteins. Various stimuli, including ROS, RNS, and inflammatory cytokines, activate the IκB kinase (IKK) complex, which phosphorylates IκB, leading to its ubiquitination and degradation [36]. This process liberates NF-κB, allowing its translocation to the nucleus and binding to κB enhancer elements in target genes.
NF-κB regulates the expression of numerous pro-inflammatory mediators, including tumor necrosis factor-α (TNF-α), interleukin-1 (IL-1), interleukin-6 (IL-6), inducible nitric oxide synthase (iNOS), and cyclooxygenase-2 (COX-2) [36] [35]. The pathway demonstrates complex redox sensitivity, with low levels of ROS potentially activating NF-κB while higher levels may inhibit its DNA-binding activity through oxidation of critical cysteine residues [36]. This biphasic response pattern positions NF-κB as a key mediator in hormetic processes, particularly those involving inflammatory preconditioning.
Experimental Approaches and Methodologies
Assessing Glutathione System Status
Comprehensive evaluation of the glutathione system requires multiple complementary approaches to capture its dynamic nature:
GSH/GSSG Quantification: Accurate measurement of reduced and oxidized glutathione remains fundamental to assessing cellular redox status. The standard protocol involves rapid acid extraction (typically with perchloric or metaphosphoric acid) to prevent artifactual oxidation during sample processing, followed by derivatization with fluorescent tags such as monobromobimane and separation with high-performance liquid chromatography (HPLC) with fluorescence detection [31]. This method allows simultaneous quantification of GSH, GSSG, and mixed disulfides with sensitivity in the picomole range. Care must be taken to minimize auto-oxidation during sample preparation through rapid processing and acid stabilization.
Enzymatic Activity Assays: Glutathione-related enzyme activities provide functional readouts of system capacity. Glutathione reductase activity is measured by monitoring NADPH oxidation at 340 nm during the reduction of GSSG to GSH [33]. Glutathione peroxidase activity is typically assayed using hydrogen peroxide or cumene hydroperoxide as substrates, coupled with NADPH consumption through the glutathione reductase reaction [31]. Glutamate-cysteine ligase activity, representing the rate-limiting step in GSH synthesis, is measured by following the formation of γ-glutamylcysteine using HPLC or colorimetric methods [31].
Compartment-Specific Redox Probes: Genetically encoded fluorescent probes such as roGFP (redox-sensitive green fluorescent protein) fused to glutaredoxin provide compartment-specific measurements of glutathione redox potential (EGSH) in real-time within living cells [32]. These probes utilize the equilibrium between roGFP and glutaredoxin to report on the GSH:GSSG ratio, allowing dynamic monitoring of redox changes in specific organelles such as mitochondria or endoplasmic reticulum.
Monitoring Transcription Factor Activation
Nuclear Translocation Assays: Transcription factor activation is commonly assessed through subcellular localization studies. Immunofluorescence staining followed by confocal microscopy allows visual determination of Nrf2 or NF-κB translocation from cytoplasm to nucleus [34] [35]. Quantitative image analysis provides statistical data on activation kinetics. Alternatively, cellular fractionation followed by Western blotting of nuclear and cytoplasmic extracts offers a biochemical approach to quantify distribution changes.
DNA-Binding Activity Measurements: Electrophoretic mobility shift assays (EMSA) using radiolabeled oligonucleotides containing ARE or κB sequences assess the DNA-binding capacity of transcription factors in nuclear extracts [35]. Supershift assays with specific antibodies confirm protein identity. For higher throughput, ELISA-based DNA-binding assays commercialize this approach with colorimetric or fluorescent readouts.
Transcriptional Activity Reporter Systems: Luciferase reporter constructs under the control of ARE or κB promoter elements provide sensitive, dynamic measurements of transcription factor activity [35]. Stable cell lines with integrated reporters enable long-term studies and compound screening. Simultaneous use of multiple reporters with different promoters allows specificity assessment.
Target Gene Expression Analysis: Downstream verification of transcription factor activity comes from measuring mRNA levels of characteristic target genes (e.g., NQO1, HO-1 for Nrf2; TNF-α, IL-8 for NF-κB) using quantitative RT-PCR [35]. Protein levels of these targets provide functional confirmation through Western blotting or ELISA.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Studying GSH and Redox Signaling
| Reagent Category | Specific Examples | Research Application | Mechanistic Insight |
|---|---|---|---|
| Nrf2 Activators | Sulforaphane, CDDO-Me, Tert-butylhydroquinone | Induce ARE-driven gene expression | Keap1 cysteine modification; Nrf2 stabilization |
| NF-κB Modulators | Pyrrolidine dithiocarbamate (inhibitor), LPS (activator), BAY-11-7082 (IKK inhibitor) | Probe inflammatory signaling pathways | IκB phosphorylation/degradation; nuclear translocation |
| GSH Depletors | Buthionine sulfoximine (BSO), Diethylmalate | Create GSH-deficient conditions | GCL inhibition; substrate limitation |
| ROS Generators | Menadione, Hydrogen peroxide, Tert-butyl hydroperoxide | Induce controlled oxidative stress | Mitochondrial vs. NADPH oxidase source differentiation |
| Redox Sensors | roGFP, HyPer, MitoSOX | Real-time monitoring of redox states | Compartment-specific redox potential measurements |
| Enzyme Inhibitors | Auranofin (thioredoxin reductase inhibitor), Mercaptosuccinate (GR inhibitor) | Dissect contributions of specific pathways | System redundancy and compensation mechanisms |
Hormesis in Redox Biology: Integrating GSH and Transcription Factors
Conceptual Framework of Hormesis
Hormesis describes the biphasic dose-response phenomenon characterized by low-dose stimulation and high-dose inhibition, resulting in adaptive beneficial effects [4]. This concept finds its philosophical roots in the 16th century observations of Paracelsus, who recognized that "the dose makes the poison" [13]. In redox biology, hormesis manifests as the ability of low-level oxidative stress to activate adaptive responses that enhance cellular resilience, while severe oxidative stress causes damage and dysfunction [4]. The quantitative features of hormesis include a characteristic stimulation zone typically ranging from 0.1-10 times the No-Observed-Adverse-Effect Level (NOAEL), with stimulatory responses generally 30-60% above baseline [4].
The hierarchical activation of cellular defense mechanisms forms the basis of redox hormesis. Low-level ROS production initially triggers the Nrf2 pathway, enhancing antioxidant capacity through increased expression of enzymes like superoxide dismutase, catalase, and glutathione peroxidase [13]. As stress intensity increases, additional pathways including NF-κB and MAPK become engaged, coordinating more comprehensive protective responses. At high stress levels, these protective systems become overwhelmed, leading to oxidative damage to macromolecules and cell death [34].
Molecular Mechanisms of Redox Hormesis
The glutathione system and redox-sensitive transcription factors interact to mediate hormetic responses through several integrated mechanisms:
Mitohormesis: Low-level mitochondrial ROS generation activates signaling pathways that enhance mitochondrial function and cellular stress resistance [4]. This process involves the activation of sirtuins and peroxisome proliferator-activated receptor gamma coactivator 1-alpha (PGC-1α), promoting mitochondrial biogenesis and metabolic adaptation [13]. The glutathione system regulates mitohormesis by modulating mitochondrial ROS levels and participating in the redox regulation of key signaling molecules.
Electrophilic Signaling: Numerous phytochemicals with hormetic properties (e.g., sulforaphane from broccoli, curcumin from turmeric) function as electrophilic compounds that modify specific cysteine residues in Keap1, activating the Nrf2 pathway and enhancing antioxidant gene expression [13]. These electrophiles typically derive from plant foods and create a mild stress that pre-adapts cells to subsequent challenges.
Epigenetic Reprogramming: Redox-mediated changes in epigenetic marks contribute to long-lasting adaptive responses. Sulforaphane inhibits histone deacetylases (HDACs), while epigallocatechin-3-gallate (EGCG) from green tea inhibits DNA methyltransferases (DNMTs) [13]. These epigenetic modifications alter chromatin structure and gene expression patterns, creating a "redox memory" that enhances future stress responses.
Inflammatory Preconditioning: Low-grade NF-κB activation by minimal inflammatory stimuli can induce protective mechanisms that mitigate subsequent inflammatory challenges [36]. This phenomenon has particular relevance in lung injury models, where preconditioning reduces damage from conditions like mechanical ventilation or ischemia-reperfusion [36] [37].
Experimental Evidence and Research Applications
The hormetic paradigm has transformed understanding of redox biology and therapeutic development. Research demonstrates that mild oxidative preconditioning protects against subsequent severe oxidative challenges across multiple model systems [4]. In neuronal cells, moderate GSH depletion activates adaptive signaling through the NO/cGMP pathway, enhancing resistance to subsequent oxidative insults [31]. In pulmonary systems, preconditioning with low-dose oxidants reduces injury from mechanical ventilation or ischemia-reperfusion through NF-κB-mediated mechanisms [36] [37].
Therapeutic applications of redox hormesis include approaches to enhance resilience in neurodegenerative diseases, mitigate inflammatory conditions, and improve cancer therapeutic responses [4] [34]. The recognition that many dietary phytochemicals exert their beneficial effects through hormetic mechanisms has stimulated research into "functional foods" and nutraceuticals designed to optimize redox adaptive responses [13]. Future research directions include quantifying hormetic response parameters across different biological systems, identifying critical nodes in redox signaling networks, and developing targeted interventions that specifically enhance adaptive pathways without triggering damage responses.
Visualizing Redox Signaling Pathways
Nrf2 and NF-κB Pathways in Redox Signaling
Hormetic Biphasic Response to Oxidative Stress
The glutathione system and redox-sensitive transcription factors form an integrated network that maintains cellular redox homeostasis and mediates adaptive responses to oxidative challenges. Within the framework of hormesis, these components translate low-level stress into enhanced defensive capacity through mechanisms including Nrf2-mediated antioxidant gene expression, NF-κB-regulated inflammatory preconditioning, and glutathione-dependent redox buffering. Understanding these interactions provides fundamental insights into cellular resilience mechanisms and offers promising avenues for therapeutic interventions designed to optimize redox adaptive responses in various disease contexts. Future research will continue to elucidate the precise molecular switches that determine the transition from adaptive to detrimental responses, enabling more targeted approaches to manipulating redox biology for therapeutic benefit.
Mechanistic Pathways and Biomedical Applications of Redox Hormesis
Hormesis, the beneficial adaptive response to mild stress, is a fundamental concept in redox biology and aging research. This biphasic dose-response phenomenon, characterized by low-dose stimulation and high-dose inhibition, is governed by an intricate network of highly conserved signaling pathways [4]. The nuclear factor erythroid 2-related factor 2 (NRF2)-Kelch-like ECH-associated protein 1 (KEAP1), AMP-activated protein kinase (AMPK), mechanistic target of rapamycin (mTOR), and Sirtuin (SIRT)-Forkhead box O (FOXO) pathways function as critical stress sensors and integrators of cellular homeostasis. They orchestrate compensatory adaptations that enhance cellular defense systems, ultimately promoting survival and longevity [4]. Under conditions of mild oxidative or metabolic stress, these pathways activate cytoprotective gene expression, enhance autophagy, and improve metabolic efficiency—core mechanisms underlying the hormetic response. This whitepaper provides an in-depth technical analysis of these four core signaling pathways, detailing their molecular mechanisms, experimental methodologies, and cross-talk within the context of hormesis in redox biology.
Pathway Mechanisms and Regulatory Networks
NRF2-KEAP1 Signaling Pathway
The NRF2-KEAP1 system is the primary regulator of cytoprotective responses to oxidative and electrophilic stress. Under basal conditions, the cytoplasmic repressor KEAP1 forms a homodimer that binds NRF2 via its DLG and ETGE motifs, sequestering it in the cytoplasm and facilitating its Cul3-mediated ubiquitination and proteasomal degradation [38]. Oxidative stress modifies critical cysteine residues in KEAP1, disrupting this interaction and allowing NRF2 to accumulate and translocate to the nucleus. There, it heterodimerizes with small Maf proteins and binds to the Antioxidant Response Element (ARE), driving the transcription of a battery of over 200 cytoprotective genes [38] [39]. These genes encode proteins such as superoxide dismutase (SOD), catalase (CAT), glutathione S-transferase (GST), glutamate-cysteine ligase catalytic subunit (GCLC), and haem oxygenase 1 (HMOX1) [38] [39].
NRF2 activation occurs through both KEAP1-dependent and KEAP1-independent mechanisms. The latter involves several kinases, including glycogen synthase kinase-3β (GSK-3β), protein kinase C (PKC), and phosphatidylinositol 3-kinase (PI3K) [38]. GSK-3β can phosphorylate Fyn, leading to NRF2 phosphorylation and nuclear export, or directly phosphorylate NRF2 at serine residues within the Neh6 domain, targeting it for β-TrCP-mediated ubiquitination and degradation. Conversely, PKC can phosphorylate NRF2 at Ser40, facilitating its dissociation from KEAP1, and inhibit GSK-3β, thereby promoting NRF2 nuclear accumulation and antioxidant activity [38].
AMPK Signaling Pathway
AMPK serves as a central energy sensor that maintains energy balance during metabolic stress. A recent landmark study revealed a novel redox-sensitive activation pathway where reactive oxygen species (ROS) promote the S-glutathionylation of PKCζ at cysteine 48 [40]. This post-translational modification facilitates PKCζ interaction with the nuclear transport protein KPNA2 and its translocation into the nucleus, where it phosphorylates LKB1 at serine 428. This phosphorylation triggers LKB1 export to the cytoplasm, where it activates AMPK via phosphorylation at Thr172 [40]. This pathway is essential under energy-deficient conditions such as glucose deprivation or metformin treatment. Disruption of ROS homeostasis with antioxidants like N-acetylcysteine (NAC) or vitamin E blocks this cascade, indicating the essential role of ROS as signaling intermediates in AMPK activation [40].
mTOR Signaling Pathway
mTOR is a highly conserved serine/threonine kinase that exists in two distinct multi-protein complexes: mTOR complex 1 (mTORC1) and mTOR complex 2 (mTORC2) [41]. mTORC1 acts as a master regulator of cell growth and metabolism by promoting anabolic processes like protein synthesis and lipid biogenesis while inhibiting catabolic processes such as autophagy. mTORC2 regulates cell survival and cytoskeleton organization. The mTOR pathway integrates inputs from growth factors, energy status, oxygen, and amino acids [41] [42]. Under conditions of nutrient abundance and growth factor signaling, mTORC1 is active and promotes cell growth. During nutrient deprivation or energy stress, AMPK activation inhibits mTORC1, shifting cells toward a catabolic state and inducing autophagy [41]. This reciprocal relationship is crucial for the hormetic response, where mild inhibition of mTOR extends healthspan and lifespan across model organisms, while constitutive activation accelerates aging and age-related diseases [42].
SIRT-FOXO Signaling Pathway
The SIRT-FOXO pathway represents a critical interface between energy metabolism, stress resistance, and longevity. SIRT1, an NAD+-dependent deacetylase, functions as a metabolic sensor that links cellular energy status to stress adaptation and survival outcomes [43] [44] [45]. SIRT1 deacetylates and activates FOXO transcription factors (FOXO1, FOXO3, FOXO4, and FOXO6), enhancing the expression of genes involved in oxidative stress resistance, cell cycle arrest, apoptosis, and metabolism [44] [46]. This SIRT1-FOXO axis is regulated by multiple post-translational modifications, including phosphorylation, acetylation, and ubiquitination, which determine FOXO subcellular localization, DNA-binding affinity, and stability [46]. Under conditions of energy stress or oxidative challenge, increased NAD+ levels activate SIRT1, which then deacetylates FOXO factors, modulating their transcriptional activity toward specific target genes that promote stress resistance and longevity without inducing apoptosis [44].
Pathway Cross-Talk in Hormesis
These core pathways do not function in isolation but engage in extensive cross-talk to fine-tune the hormetic response. AMPK activation directly phosphorylates FOXO3, enhancing its transcriptional activity and promoting expression of genes involved in stress resistance and metabolic adaptation [46]. Similarly, SIRT1 and AMPK engage in reciprocal activation, with AMPK increasing NAD+ levels to enhance SIRT1 activity, while SIRT1 deacetylates and activates AMPK kinase LKB1 [40] [44]. The NRF2 and mTOR pathways also interact significantly, with NRF2 shown to directly regulate mTOR, linking cytoprotective gene expression to a major metabolic regulator that generates redox activity [41]. Furthermore, SIRT1 deacetylates NRF2, enhancing its transcriptional activity and creating a positive feedback loop that amplifies the antioxidant response [43]. This intricate network ensures a coordinated adaptation to stress, where energy-sensing pathways (AMPK, mTOR) modulate antioxidant defense systems (NRF2) and stress resilience pathways (SIRT-FOXO) to maintain homeostasis under challenging conditions.
Experimental Methodologies and Protocols
Assessing NRF2-KEAP1 Pathway Activation
Quantitative RT-PCR for ARE-Regulated Genes: To evaluate NRF2 pathway activation, measure mRNA expression of canonical NRF2 target genes. Isolate total RNA using commercial kits (e.g., Solarbio Total RNA Extraction Kit). Reverse transcribe 1μg of total RNA using the Universal RT-PCR Kit (M-MLV). Perform qRT-PCR with specific primers for GCLC, GCLM, HMOX1, NQO1, SRXN1, and TXNRD1 using SYBR Green chemistry on a real-time PCR system [39]. Normalize expression to housekeeping genes (e.g., β-actin, GAPDH) using the 2^(-ΔΔCt) method.
siRNA-Mediated Gene Knockdown: To dissect KEAP1-dependent and independent mechanisms, transfer cells with specific siRNAs targeting KEAP1, GSK-3β, or PKC using appropriate transfection reagents. Include non-targeting siRNA as a negative control. After 48-72 hours, treat cells with stressors (e.g., 10μM benzo[a]pyrene) or vehicle control (DMSO) for specified durations (e.g., 3, 6, 12, 24h) [38]. Analyze pathway components by Western blot and qRT-PCR to confirm knockdown efficiency and assess pathway activation.
Nuclear-Cytoplasmic Fractionation and Western Blotting: Prepare nuclear and cytoplasmic fractions using commercial extraction kits. Separate 30-50μg of protein by SDS-PAGE, transfer to PVDF membranes, and probe with antibodies against NRF2, KEAP1, Lamin B1 (nuclear marker), and β-tubulin (cytoplasmic marker). Quantify band intensity to determine NRF2 nuclear translocation [38].
Monitoring AMPK Activation via Novel Redox-Sensitive Pathway
Detecting PKCζ S-Glutathionylation: To investigate the redox-sensitive AMPK activation pathway, treat cells under energy stress conditions (glucose deprivation or 2mM metformin) with or without antioxidant pretreatment (5mM NAC or 100μM vitamin E) [40]. Harvest cells and lyse in non-reducing buffer. Immunoprecipitate PKCζ using specific antibodies and detect S-glutathionylation using anti-glutathione antibody. Confirm the essential cysteine residue (Cys48) through site-directed mutagenesis.
LKB1 Phosphorylation and Localization: Monitor LKB1 phosphorylation at Ser428 and cellular localization by immunofluorescence and Western blotting following energy stress. Use specific phospho-Ser428 LKB1 antibodies for detection. For nuclear-cytoplasmic fractionation, confirm LKB1 translocation from nucleus to cytoplasm under energy stress conditions [40].
AMPK Activity Assay: Measure AMPK phosphorylation at Thr172 by Western blot using phospho-specific antibodies. Perform kinase activity assays using the SAMS peptide (HMRSAMSGLHLVKRR) as substrate according to manufacturer protocols. Correlate AMPK activity with metabolic outcomes such as glucose uptake and lipid oxidation [40].
Evaluating mTOR Pathway Activity
mTORC1/mTORC2 Specific Assays: Assess mTOR complex-specific activity by monitoring phosphorylation of downstream substrates. For mTORC1, measure phospho-S6K (Thr389) and phospho-4E-BP1 (Thr37/46). For mTORC2, evaluate phospho-AKT (Ser473) [41] [42]. Use rapamycin (20nM) and Torin1 (250nM) as specific mTOR inhibitors to distinguish between complexes.
Autophagy Flux Analysis: Monitor mTOR-mediated regulation of autophagy by transfecting cells with mRFP-GFP-LC3 reporter construct. Under mTOR inhibition, increased autophagic flux appears as red puncta (mRFP+/GFP-), representing autolysosomes. Alternatively, treat cells with lysosomal inhibitors (e.g., chloroquine 50μM or bafilomycin A1 100nM) and measure LC3-II accumulation by Western blot [42].
SIRT-FOXO Pathway Analysis
SIRT1 Activity Assay: Measure SIRT1 deacetylase activity using fluorogenic substrates (e.g., Fluor de Lys-SIRT1 substrate). Treat cells with SIRT1 activators (resveratrol 10-50μM) or inhibitors (EX527 1μM) as controls. Monitor changes in NAD+ levels using commercial kits as SIRT1 activity is NAD+-dependent [44] [45].
FOXO Localization and Transcriptional Activity: Transfect cells with FOXO-responsive luciferase reporter constructs (e.g., pGL4-FHRE-luc) to measure FOXO transcriptional activity. Determine FOXO subcellular localization by immunofluorescence using antibodies against specific FOXO proteins. Monitor phosphorylation status at regulatory sites (e.g., FoxO1 Ser256, FoxO3a Ser253) by Western blot [44] [46].
Chromatin Immunoprecipitation (ChIP): Crosslink proteins to DNA with formaldehyde, sonicate chromatin, and immunoprecipitate with anti-FOXO antibodies. Analyze bound DNA sequences by qPCR for known FOXO target genes (e.g., Bim, FasL, p27^Kip1, MnSOD) [44].
Quantitative Data Presentation
Table 1: NRF2 Target Gene Expression Under Oxidative Stress
| Gene Symbol | Protein Name | Fold Change (48h) | Function | Detection Method |
|---|---|---|---|---|
| HMOX1 | Haem Oxygenase 1 | 4.5 ± 0.3 | Haem catabolism, antioxidant | qRT-PCR, ELISA |
| NQO1 | NAD(P)H Quinone Dehydrogenase 1 | 3.8 ± 0.4 | Quinone reduction, detoxification | qRT-PCR, Activity Assay |
| GCLC | Glutamate-Cysteine Ligase Catalytic Subunit | 2.9 ± 0.2 | Rate-limiting GSH synthesis | qRT-PCR, Western Blot |
| TXNRD1 | Thioredoxin Reductase 1 | 2.7 ± 0.3 | Thioredoxin regeneration, redox homeostasis | qRT-PCR, Activity Assay |
| SRXN1 | Sulfiredoxin 1 | 3.2 ± 0.3 | Redox regulation of peroxiredoxins | qRT-PCR |
Table 2: mTOR Inhibition Effects on Aging Markers in Model Organisms
| Organism | mTOR Inhibitor | Lifespan Extension | Healthspan Improvements | Key Molecular Changes |
|---|---|---|---|---|
| S. cerevisiae | Rapamycin (10nM) | 25% | Increased stress resistance | ↓ Sch9 activity, ↑ autophagy |
| C. elegans | let-363 RNAi | 30% | Delayed age-related decline | ↓ mTORC1, ↑ DAF-16 nuclear localization |
| D. melanogaster | Rapamycin (100μM) | 15% | Improved mobility | ↓ S6K phosphorylation, ↑ autophagy |
| M. musculus | Rapamycin (14ppm) | 10-15% (female) | Improved cardiac function, cognitive preservation | ↓ p-S6K, ↑ LC3-II, ↓ p-AKT |
Table 3: SIRT1-FOXO Pathway Modulation in Disease Models
| Disease Model | Intervention | SIRT1 Activity Change | FOXO Regulation | Functional Outcome |
|---|---|---|---|---|
| Diabetic Cardiomyopathy | Resveratrol (50μM) | ↑ 2.5-fold | FoxO1 deacetylation, ↑ nuclear translocation | ↓ Apoptosis, improved contractility |
| Ischemic Heart | Icariin (20mg/kg) | ↑ 1.8-fold | FoxO3a deacetylation | ↓ Mitochondrial oxidative damage |
| Doxorubicin-Induced Cardiotoxicity | Cilostazol (30mg/kg) | ↑ 2.1-fold | FoxO1 phosphorylation | ↓ Apoptosis, improved ejection fraction |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents for Pathway Analysis
| Reagent/Category | Specific Examples | Application/Function | Key Experimental Considerations |
|---|---|---|---|
| NRF2 Activators | Sulforaphane (1-10μM), Tert-butylhydroquinone | Induce NRF2 nuclear translocation | Dose-dependent effects; high concentrations may cause off-target effects |
| KEAP1 Inhibitors | CDDO-Me, siRNA against KEAP1 | Disrupt KEAP1-NRF2 interaction | Monitor NRF2 ubiquitination status |
| AMPK Activators | Metformin (1-2mM), AICAR (0.5-2mM) | Activate AMPK directly or indirectly | Consider cell-specific effects on energy metabolism |
| mTOR Inhibitors | Rapamycin (20-100nM), Torin1 (250nM) | Selective mTORC1 or pan-mTOR inhibition | Distinguish acute vs chronic treatment effects |
| SIRT1 Modulators | Resveratrol (10-50μM), EX527 (1μM) | Activate or inhibit SIRT1 deacetylase activity | NAD+ dependency; cell type-specific responses |
| FOXO Reporters | FHRE-luciferase, FoxO-GFP fusion proteins | Monitor FOXO transcriptional activity and localization | Consider FOXO isoform-specific effects |
| Antioxidants | N-acetylcysteine (1-5mM), Vitamin E (50-100μM) | Scavenge ROS, test redox-sensitive pathways | Can interfere with physiological ROS signaling |
| siRNA/shRNA | KEAP1, GSK-3β, PKC, SIRT1, FOXO isoforms | Gene-specific knockdown | Confirm efficiency with multiple targets |
| Phospho-Specific Antibodies | p-AMPK (Thr172), p-mTOR (Ser2448), p-FoxO (Ser253/256) | Detect pathway activation status | Validate specificity with appropriate controls |
The NRF2-KEAP1, AMPK, mTOR, and SIRT-FOXO pathways represent an integrated network that orchestrates the hormetic response to mild stress, ultimately promoting cellular resilience and organismal health. The experimental methodologies outlined provide a framework for investigating these pathways in both basic research and drug discovery contexts. Quantitative assessment of pathway activity, particularly through the biomarker panels and reagent tools described, enables precise evaluation of therapeutic interventions targeting these pathways. As research advances, continued exploration of the nuanced cross-talk between these systems will further elucidate the molecular basis of hormesis and its potential applications in mitigating age-related diseases and enhancing healthspan.
Cellular adaptation to environmental stressors is a fundamental biological process that occurs across vastly different timescales. In the context of redox biology, this adaptive continuum can be understood through the framework of hormesis—a biphasic dose-response phenomenon where low doses of a stressor induce stimulatory/adaptive effects, while higher doses cause inhibition or damage [4]. This review delineates the molecular progression from immediate, short-term adaptive responses, characterized by direct post-translational modifications and rapid signaling events, to sustained long-term adaptations involving comprehensive transcriptional reprogramming and epigenetic restructuring. The hormetic principle provides a unifying conceptual framework, revealing how transient, low-level stress exposure primes and activates pathways that, if sustained, can lead to fixed, heritable adaptive states [4]. Understanding this continuum is critical for researchers and drug development professionals aiming to manipulate adaptive pathways for therapeutic benefit, particularly in diseases involving redox imbalance, such as cancer, neurodegenerative disorders, and metabolic conditions.
Core Concepts: Hormesis in Redox Biology
The concept of hormesis, encapsulated by the maxim "the dose makes the poison," describes an evolutionarily conserved adaptive strategy [4]. In redox terms, low-level oxidative stress (eustress) activates cytoprotective signaling, while excessive stress (distress) causes damage. This biphasic response is orchestrated through specific molecular mechanisms:
- Dose-Dependent Signaling: Low doses of reactive oxygen species (ROS) activate key survival pathways including NF-κB, MAPK, AMPK, and NRF2, upregulating cytoprotective proteins like antioxidant enzymes, heat-shock proteins, and growth factors [4] [47]. These pathways enhance cellular defense capabilities and improve resilience.
- Adaptive Plasticity: Hormesis enhances phenotypic plasticity, allowing cells to maintain homeostasis under stress. This plasticity can promote long-term adaptive evolution when the short-term response aligns with environmental demands [48] [4].
- Therapeutic Implications: The hormetic principle reveals that antioxidant therapies must be precisely calibrated; broad-spectrum interventions may disrupt essential redox signaling and produce adverse effects, highlighting the need for targeted approaches [47].
Short-Term Adaptation: Rapid Response Mechanisms
Short-term adaptation encompasses rapid, often reversible, molecular changes that enable immediate cellular survival without requiring new gene expression.
Direct Enzyme Modification and Metabolic Reprogramming
Cells instantly recalibrate metabolic fluxes through allosteric regulation and post-translational modifications of pre-existing enzymes. In response to hypoxia, for instance, metabolic pathways are rapidly adjusted to optimize ATP production and manage redox balance [48] [49].
Table 1: Key Redox-Sensitive Post-Translational Modifications in Short-Term Adaptation
| Modification Type | Functional Consequence | Example Enzymes/Proteins | Regulatory Impact |
|---|---|---|---|
| Disulfide Bond Formation | Reversible oxidation of cysteine thiols | Protein disulfide isomerases | Alters protein structure/activity [47] |
| S-Glutathionylation | Addition of glutathione moiety | Metabolic enzymes, kinases | Protection from over-oxidation [47] |
| S-Nitrosylation | Addition of nitric oxide derivative | Caspases, NF-κB pathway | Modulates apoptosis, inflammation [47] |
| Phosphorylation | Phosphate group addition by kinases | MAPK, AMPK pathway components | Amplifies stress signals [4] |
Rapid Stress Signaling Pathways
Immediate stress detection triggers transient signaling cascades that coordinate the initial adaptive response:
- Heat Shock Response (HSR): Proteotoxic stress rapidly activates heat shock factors (HSFs), particularly HSF1, which drives chaperone gene transcription while globally repressing non-chaperone genes through dramatic remodeling of the 3D chromatin architecture [50].
- Oxidative Stress Sensing: The NRF2-KEAP1 system acts as a primary redox sensor. Under oxidative stress, NRF2 is stabilized and transactivates genes encoding antioxidant enzymes like SOD, catalase, and GPX4, constituting the first line of cellular defense [47].
- Energy Stress Management: AMPK activation during energy depletion switches on catabolic pathways while inhibiting anabolic processes, rapidly conserving energy and maintaining viability [4].
Long-Term Adaptation: Sustained Reprogramming Mechanisms
When stress persists, cells transition from transient responses to stable adaptive states through profound reprogramming of gene expression networks.
Transcriptional Reprogramming
Sustained stress induces a fundamental rewiring of the transcriptional landscape:
- Metabolic Pathway Conservation: Comparative transcriptomic studies in high-altitude adaptation reveal that metabolic pathways activated during short-term stress (e.g., hypoxia) are similarly enriched in long-term evolutionary adaptations, suggesting common paths to molecular adaptation [48].
- Enhanced Transcriptional Activation: Transcriptional activation from previously silenced genes requires overcoming chromatin-based repression. Nuclear actin and actin-binding proteins facilitate this process by promoting chromatin remodeling and enhancing the activity of RNA polymerases [51].
- HSF-Mediated Sustained Response: Acute heat stress triggers a canonical HSR, but prolonged proteotoxic challenges lead to HSF-mediated stress signaling that intersects with broader proteostasis networks, creating a stable adaptive state [50].
Epigenetic Reprogramming
Epigenetic mechanisms provide the molecular memory that stabilizes long-term adaptive phenotypes:
- Histone Modification Redistribution: Chronic hypoxia induces H3K4me3 expansion and redistribution at promoters, driven by oxygen-sensitive inhibition of KDM5 demethylases. This remodeling facilitates widespread changes in transcription start site (TSS) selection, altering 5'UTR isoforms and subsequent translational output [49].
- DNA Methylation Reprogramming: During development and cellular differentiation, global erasure and re-establishment of DNA methylation patterns enable fundamental cell state transitions, a process recapitulated in stress-induced cellular reprogramming [52].
- Transgenerational Epigenetic Inheritance: Environmentally induced epigenetic changes can be transferred to subsequent generations via the germline, potentially mediating transgenerational adaptation to persistent stressors [53].
Table 2: Epigenetic Mechanisms in Long-Term Adaptation
| Epigenetic Mechanism | Inducing Stressors | Molecular Actors | Functional Outcome |
|---|---|---|---|
| H3K4me3 Remodeling | Hypoxia, metabolic stress | COMPASS complexes, KDM5 demethylases | Altered TSS selection, 5'UTR remodeling [49] |
| DNA Methylation Erasure/Establishment | Developmental signals, severe stress | TET enzymes, DNMTs | Cell fate resetting, stable gene silencing [52] |
| Chromatin Remodeling | Proteotoxic stress, heat shock | Nuclear actin, BAF complexes | Increased accessibility of occluded genes [50] [51] |
| Transgenerational Inheritance | Environmental toxins, diet | Germline epigenetic marks | Phenotypic transmission to offspring [53] |
The Hormetic Continuum: From Short-Term to Long-Term Adaptation
The transition from transient to stable adaptation represents a fundamental principle in biology where phenotypic plasticity can facilitate adaptive evolution [48] [4].
Molecular Links and Transition Mechanisms
- Metabolic Pathway Conservation: Transcriptomic analyses of cells subjected to short-term high-altitude stressors (hypoxia, UVR, cold) and genomic comparisons of long-term highland species reveal convergent adaptation through shared metabolic pathways [48]. This indicates that the initial plastic response to stress can be genetically assimilated over evolutionary time.
- From Signaling to Transcription: Short-term redox signaling through NRF2 not only provides immediate antioxidant protection but also induces expression of genes that can influence the epigenetic landscape, such as those involved in NAD+ biosynthesis, thereby creating a permissive environment for stable epigenetic reprogramming [47].
- Nuclear Actin as a Mediator: Nuclear actin and actin-binding proteins physically integrate rapid signaling with sustained transcriptional outputs by regulating chromatin remodeling complexes and RNA polymerase activity, thus bridging the gap between initial stress perception and long-term gene expression changes [51].
Reversibility and Reset Mechanisms
A defining feature of the adaptation continuum is the differential reversibility of the responses:
- Short-Term Reactivity: Post-translational modifications are inherently reversible through dedicated enzyme systems (e.g., thioredoxin/glutathione systems reduce oxidized cysteine residues) [47].
- Epigenetic Plasticity: While more stable than PTMs, epigenetic marks can be globally reset, most dramatically during fertilization, where reprogramming factors in the oocyte cytoplasm restore youthful epigenetic states, effectively reversing the aging clock [54].
- Developmental Windows: The efficiency of reprogramming varies with cellular differentiation state; highly specialized cells exhibit more occluded gene states that resist reactivation, requiring more intensive intervention to overcome chromatin-based repression [51].
Experimental Approaches and Methodologies
Key Experimental Models and Protocols
- In Vitro Stress Paradigms: Experimental simulation of high-altitude conditions in great tit and mouse embryonic fibroblasts (GEF/MEF) involves exposure to hypoxia (3% O₂), cold (4°C), and UVR (100 J/m²) for durations ranging from 1-24 hours to assess short-term transcriptional responses [48].
- Transcriptomic and Epigenomic Profiling: RNA-seq, nanoCAGE sequencing, polysome profiling, and ChIP-seq are employed to comprehensively map transcriptomes, translatomes, and epigenetic landscapes under stress conditions [48] [49].
- Nuclear Reprogramming Assays: Somatic cell nuclear transfer (SCNT) and induced pluripotent stem (iPS) cell generation demonstrate the profound reprogramming capacity of oocyte cytoplasm and transcription factor combinations, effectively resetting epigenetic age [54].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Investigating Adaptive Responses
| Reagent/Category | Specific Examples | Research Function |
|---|---|---|
| Pharmacological Epigenetic Modulators | KDM5 inhibitors, MLL-COMPASS inhibitors | Probe causal relationships between specific histone modifications and TSS switching [49] |
| Redox Probes and Sensors | Genetically encoded biosensors (e.g., roGFP), H₂O₂-specific fluorescent dyes | Quantify spatial-temporal dynamics of redox changes in live cells [47] |
| Stress Pathway Activators/Inhibitors | mTOR inhibitors, ISR inducers, HSP90 inhibitors | Dissect contributions of specific signaling nodes to integrated stress response [50] [49] |
| Chromatin Remodeling Assay Components | Antibodies for H3K4me3 ChIP, ATAC-seq reagents, nuclear actin probes | Map chromatin accessibility and histone modification dynamics [51] [49] |
Visualizing the Adaptive Continuum
The following diagrams illustrate key signaling pathways and regulatory relationships in the transition from short-term to long-term adaptation.
Hormetic Signaling in Redox Adaptation
Diagram Title: Biphasic Stress Response Determining Adaptive vs. Pathological Outcomes
Transcriptional and Epigenetic Reprogramming in Hypoxia
Diagram Title: Hypoxia-Induced Gene Expression Reprogramming Through HIF1 and Epigenetic Mechanisms
The continuum from short-term adaptation to long-term reprogramming represents a fundamental paradigm in cellular stress biology. Understanding the molecular hinges that connect immediate redox-sensitive signaling with stable epigenetic restructuring provides unprecedented opportunities for therapeutic intervention. Future research should focus on:
- Quantitative Dynamical Models: Developing mathematical models that predict the transition points from plastic to fixed adaptive states.
- Single-Cell Multi-Omics: Applying single-cell transcriptomic, epigenomic, and proteomic technologies to dissect heterogeneity in adaptive responses.
- Targeted Reprogramming Therapies: Designing small molecules that specifically modulate the key transition nodes, such as nuclear actin dynamics or specific histone demethylases, to direct adaptive outcomes in diseases of aging, cancer, and metabolic disorders.
The hormesis framework provides a powerful lens through which to view the entire adaptation spectrum, emphasizing that the strategic induction of mild stress could precondition cells, tissues, and organisms for enhanced resilience—a concept with profound implications for both fundamental biology and translational medicine.
Hormesis is an evolutionarily conserved adaptive response characterized by a biphasic dose-response relationship, where exposure to low doses of a stressor induces beneficial effects, while higher doses are inhibitory or toxic [4]. This phenomenon, often summarized as "what doesn't kill you makes you stronger," provides a fundamental framework for understanding how mild stress exposure can enhance physiological resilience and potentially extend healthspan. The concept of hormesis has gained substantial traction in biogerontology and redox biology, with researchers establishing databases containing over 9,000 hormetic models [4]. In recent years, the number of publications on hormesis has steadily increased, reflecting growing scientific interest in its mechanisms and applications [4].
The essence of hormesis lies in its ability to reconstruct homeostasis through targeted stress exposure. When applied at low intensities, stressors trigger adaptive signaling pathways that upregulate cytoprotective proteins, enhance cellular defense mechanisms, and improve overall system performance [4]. In the context of redox biology, this translates to a hormetic shift in the cellular redox environment toward a more reductive state, thereby improving resilience to subsequent oxidative challenges [55]. The universal applicability of hormesis is evident across various stressors, including physical stimuli like temperature extremes, chemical agents such as reactive oxygen species (ROS) and phytochemicals, and biological challenges [4]. Understanding these mechanisms provides crucial insights for developing interventions to enhance healthspan and combat age-related diseases.
Core Mechanistic Principles
The Biphasic Dose-Response Relationship
The biphasic dose-response curve is the signature characteristic of hormetic phenomena. This non-linear relationship demonstrates that biological responses to stressors are not monotonic but rather exhibit stimulation at low doses and inhibition at high doses [4]. The quantitative features of this curve include a stimulation zone typically 30-60% above the control baseline, with the stimulatory response occurring within a dose range approximately 10- to 20-fold in width [4]. The peak stimulatory response generally occurs at a level approximately 30-60% above the baseline, providing a quantitative framework for evaluating potential hormetic agents.
The mechanistic foundation of this biphasic pattern lies in the overcompensation response to initial disruption of homeostasis. Low-level stress triggers adaptive signaling pathways that not only restore but enhance baseline function, resulting in improved cellular defense capabilities. However, as the stress intensity increases beyond the system's compensatory capacity, damage accumulates, leading to the inhibitory phase of the response curve [4]. This fundamental pattern is consistently observed across various model systems, from cellular assays to whole-organism studies, and for diverse stressors including the phytochemicals, exercise, and dietary regimens that form the focus of this review.
Redox Signaling and Oxidative Eustress
Reactive oxygen species (ROS) serve as paradigmatic hormetic agents through their dual role in cellular signaling and damage. At moderate, transient concentrations, ROS function as essential signaling molecules in a state termed "oxidative eustress" that activates pathways enhancing antioxidant gene expression, promotes mitochondrial biogenesis, and improves physiological function [56] [34]. This stands in contrast to oxidative distress, which occurs when ROS levels exceed the scavenging capacity of cellular antioxidant systems, leading to macromolecular damage and dysfunction [56].
The compartmentalization of redox signaling is crucial for its hormetic properties. Eukaryotic cells maintain distinct redox environments across different organelles, with the secretory pathway being strongly oxidizing to support disulfide bond formation, while the cytoplasm maintains a more reducing environment [56]. In skeletal muscle, redox states exhibit marked subcellular heterogeneity, with specific regions such as the subsarcolemmal, perinuclear, and neuromuscular junction areas engaging uniquely in redox signaling during stress exposure [56]. This spatial regulation ensures that ROS can exert specific signaling functions while minimizing widespread oxidative damage, enabling their role as mediators of hormetic adaptation.
Model Stressors and Inducers
Phytochemicals
Sulforaphane
Sulforaphane (SF) is an isothiocyanate derived from glucoraphanin, primarily found in cruciferous vegetables such as broccoli, cauliflower, and Brussels sprouts [57]. It functions as the most potent naturally occurring inducer of the Keap1/Nrf2 pathway, which serves as the master regulator of cellular antioxidant and detoxification responses [57]. Upon exposure to SF or oxidative stress, Nrf2 dissociates from its cytosolic inhibitor Keap1 and translocates to the nucleus, where it binds to the Antioxidant Response Element (ARE), initiating transcription of a battery of cytoprotective genes [34] [57].
The hormetic properties of sulforaphane emerge from its ability to modulate redox-sensitive signaling pathways at low concentrations, including the MAPK and NF-κB pathways [34]. Through these mechanisms, SF demonstrates beneficial effects in both sex-specific conditions and hormone-mediated health issues by influencing the hypothalamic-pituitary-gonadal (HPG), hypothalamic-pituitary-adrenal (HPA), and hypothalamic-pituitary-thyroid (HPT) axes [57]. The complex interplay between SF-induced Nrf2 activation and hormonal regulation exemplifies the systemic nature of hormetic responses, extending beyond cellular defense to encompass endocrine function.
Resveratrol
Resveratrol (3,5,4′-trihydroxy-trans-stilbene) is a natural polyphenolic phytoalexin found in grapes, peanuts, berries, and red wine [58] [59]. Contrary to initial perceptions as a direct antioxidant, resveratrol exerts many of its effects through pro-oxidative triggering that activates adaptive cellular responses [55]. Under physiologically relevant conditions (generally <50 µM), resveratrol generates oxidation products, including reactive oxygen species, which initiate a cascade of events leading to enhanced stress resistance [55].
The cellular response to resveratrol depends significantly on activation of the redox-sensitive transcription factor Nrf2, leading to coordinated gene expression reprogramming [55]. In primary human epidermal keratinocytes, this process results in a 1.3-fold increase in endogenously generated glutathione and a quantitative reduction of the cellular redox environment by 2.61 mV mmol GSH per g protein [55]. This hormetic shift protects cells against additional oxidative stress, demonstrating the preparatory function of mild resveratrol-induced oxidation. Additionally, resveratrol activates sirtuins, particularly SIRT1, which modulates mitochondrial biogenesis, reduces inflammation, and promotes autophagy through pathways including AMPK/PGC-1α and SIRT1/mTOR [58]. Resveratrol exhibits a biphasic, dose-dependent response consistent with hormesis, where low to moderate doses (≤500 mg/day) produce beneficial effects, while higher doses (≥1000 mg/day) are associated with adverse gastrointestinal effects [59].
Exercise
Physical activity represents a fundamental physiological hormetic stressor that induces systemic adaptations through redox-mediated mechanisms. The relationship between exercise intensity and beneficial effects follows a typical hormetic curve, where physical inactivity and overtraining represent the detrimental extremes, and moderate activity optimizes health outcomes [60]. Exercise-induced ROS production originates from multiple sources, including NADPH oxidases (NOX2) and electron leakage from the mitochondrial respiratory chain [56]. These ROS sources function as signaling molecules that activate pathways enhancing antioxidant gene expression, promote mitochondrial biogenesis, and improve muscle contractility [56].
The concept of "oxidative eustress" is particularly relevant to exercise physiology, where moderate levels of free radicals induced during physical activity trigger the body's antioxidant defenses and improve muscle adaptation [34]. This adaptive response includes upregulation of antioxidant enzymes such as superoxide dismutase (SOD-1) and catalase through the p62-Keap1/Nrf2 and AKT/MAPK/Nrf2 signaling pathways [58]. The hormetic benefits of exercise extend beyond skeletal muscle to systemic effects mediated by circulating factors termed "exerkines," which include metabolites, cytokines, peptides, and nucleic acids secreted by various tissues in response to physical activity [56]. These exerkines facilitate inter-organ communication and coordinate systemic responses to exercise, many of which are influenced by and influence redox states in distant organs [56].
Caloric Restriction
Caloric restriction (CR), defined as reduced caloric intake without malnutrition, is a well-established intervention that extends healthspan and lifespan across diverse species, from yeast to rodents [61] [62]. The hormetic nature of CR involves mild metabolic stress that activates compensatory adaptive responses, enhancing physiological resilience. Dietary restriction triggers evolutionarily conserved nutrient-sensing pathways, including AMP-activated protein kinase (AMPK) and Target of Rapamycin Complex 1 (TORC1) signaling, which subsequently modulate cellular processes such as autophagy, mitochondrial function, oxidative stress responses, and protein synthesis [61].
The redox aspects of CR have been subject to debate, with some studies suggesting increased ROS production activates stress response pathways, while the largest body of work indicates that CR improves overall redox state [62]. In rodent models, CR consistently decreases tissue levels of oxidatively modified lipids, proteins, and DNA, with a particularly pronounced effect on reducing oxidative damage to mitochondrial components that accumulates with aging [62]. The reduction in ROS release from mitochondria or tissues of CR animals represents a key mechanism underlying these protective effects [62]. Recent research has explored the synergistic interaction between CR and rapamycin (a TORC1 inhibitor), revealing that their combination produces unique transcriptomic signatures that extend cellular lifespan in both yeast and human cells [61].
Table 1: Quantitative Parameters of Hormetic Stressors
| Stressor | Hormetic Dose Range | Key Signaling Pathways | Redox Effects | Adaptive Outcomes |
|---|---|---|---|---|
| Sulforaphane | Low micromolar concentrations | Keap1/Nrf2, MAPK, NF-κB | Increased antioxidant gene expression, GSH synthesis | Enhanced detoxification, anti-inflammatory effects, hormone axis modulation [57] |
| Resveratrol | <50 µM (in vitro), ≤500 mg/day (human) | Nrf2, SIRT1, AMPK/PGC-1α | Transient ROS generation, increased GSH (1.3-fold) [55] | Improved stress resistance, mitochondrial biogenesis, anti-inflammatory [55] [58] |
| Exercise | Moderate intensity/volume | Nrf2, NF-κB, PGC-1α | Transient ROS signaling (oxidative eustress) | Enhanced antioxidant defenses, mitochondrial biogenesis, systemic resilience [60] [56] |
| Caloric Restriction | 10-40% reduction from ad libitum | AMPK, TORC1, Nrf2 | Reduced mitochondrial ROS release, decreased oxidative damage | Lifespan extension, improved metabolic health, enhanced stress resistance [62] [61] |
Experimental Methodologies
In Vitro Assessment of Phytochemical Hormesis
Resveratrol Hormesis Protocol:
- Cell Culture: Use primary neonatal normal human epidermal keratinocytes (NHEK) cultured in keratinocyte growth medium (KGM) or appropriate cell models [55].
- Treatment Preparation: Prepare resveratrol stock solution in DMSO and dilute to working concentrations (typically 1-50 µM) in serum-free medium. Maintain DMSO concentration below 0.1% in all treatments [55].
- Experimental Groups: Include (1) vehicle control (DMSO only), (2) low-dose resveratrol (1-10 µM), (3) intermediate-dose resveratrol (10-30 µM), and (4) high-dose resveratrol (30-50 µM) groups [55].
- Exposure Time: Treat cells for 24-72 hours, depending on endpoint measurements.
- Viability Assessment: Measure cell viability using MTT or WST-1 assays. Expect a ~30-60% increase in viability at optimal low doses compared to control [55].
- ROS Detection: Quantify intracellular ROS using fluorescent probes like DCFH-DA. Note: Initial increase in ROS is expected within first few hours of treatment [55].
- Gene Expression Analysis: Extract RNA and analyze Nrf2-target gene expression (e.g., glutathione peroxidase, heme oxygenase-1) via qRT-PCR [55].
- Glutathione Measurement: Quantify cellular glutathione levels using HPLC or commercial kits. Expect approximately 1.3-fold increase with optimal resveratrol pretreatment [55].
- Stress Challenge: Apply secondary oxidative stress (e.g., 0.78% ethanol) to assess protective effects of pretreatment [55].
Sulforaphane Nrf2 Activation Assay:
- Cell Culture: Maintain appropriate cell lines (e.g., HepG2, HEK293) in complete medium.
- Treatment: Apply sulforaphane (0.5-5 µM) for 6-24 hours [57].
- Nuclear Translocation: Fix cells and immunostain for Nrf2 with nuclear counterstaining. Quantify nuclear-to-cytosolic ratio.
- ARE-Luciferase Reporter: Transfect cells with ARE-luciferase construct and measure luciferase activity after 24-hour treatment.
- Target Gene Analysis: Measure expression of NQO1, HO-1, and GSTs via western blot or qRT-PCR [57].
Exercise Intervention Protocols
Redox Signaling Assessment in Human Exercise:
- Participant Preparation: Recruit healthy volunteers (age-matched as needed) and obtain informed consent. Conduct preliminary testing for VO₂max and establish individual exercise intensities.
- Exercise Protocol: Implement moderate-intensity continuous training (MICT) at 60-70% VO₂max for 30-60 minutes, 3-5 times per week for 8-12 weeks [56].
- Tissue Sampling: Collect muscle biopsies from vastus lateralis pre-training, immediately post-exercise (acute), and after training period (chronic).
- ROS Measurement: Use electron spin resonance (EPR) spectroscopy or fluorescent probes (DHE, MitoSOX) in fresh tissue sections to detect superoxide production [56].
- Antioxidant Enzyme Activity: Assess SOD, catalase, and glutathione peroxidase activities in muscle homogenates spectrophotometrically.
- Protein Carbonylation and Lipid Peroxidation: Measure protein carbonyls via DNPH assay and lipid peroxidation through TBARS or HNE-modified proteins [56].
- Gene Expression Analysis: Isolve RNA and analyze Nrf2-target genes, PGC-1α, and mitochondrial biogenesis markers via qRT-PCR.
- Exerkine Profiling: Collect blood samples pre- and post-exercise and analyze plasma exerkines (e.g., IL-6, IL-10, FGF21) via ELISA or multiplex assays [56].
Caloric Restriction Methodologies
Yeast Chronological Lifespan Analysis with Transcriptomics:
- Strain and Culture: Use prototrophic S. cerevisiae strain CEN.PK113-7D to avoid amino acid-related artifacts. Culture in synthetic defined (SD) medium with 2% glucose [61].
- CR Conditions: Implement calorie restriction using 0.5% glucose compared to control (2% glucose). For combination studies, add 2 nM rapamycin (RM) [61].
- Sampling Time Points: Collect samples at 5 hours (mitotic/exponential phase) and 72 hours (postmitotic/stationary phase) after inoculation at OD600nm=0.2 [61].
- Viability Assessment: Measure chronological lifespan by monitoring survival in stationary phase using colony-forming unit counts.
- RNA Sequencing: Extract high-quality RNA, prepare libraries, and perform RNA-sequencing. Include biological replicates (n≥3) for each condition [61].
- Bioinformatic Analysis: Conduct differential expression analysis (DESeq2), gene ontology enrichment, and pathway analysis (KEGG, Reactome).
- Validation: Confirm key findings using qRT-PCR for selected genes of interest.
- ROS Measurements: Assess intracellular ROS using fluorescent probes with appropriate controls for potential artifacts [62].
Table 2: Research Reagent Solutions for Hormesis Studies
| Reagent/Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Cell Culture Models | Primary human epidermal keratinocytes (NHEK) [55], Prototrophic yeast CEN.PK113-7D [61] | In vitro hormesis screening, Lifespan studies | Primary cells maintain physiological relevance; prototrophic yeast avoids amino acid confounding effects |
| Chemical Inducers | Trans-resveratrol [55], Sulforaphane [57], Rapamycin [61] | Phytochemical hormesis studies, CR mimetics | Resveratrol isomerization affects activity; sulforaphane stability in solution; rapamycin solvent controls |
| ROS Detection Probes | DCFH-DA, Dihydroethidium (DHE), MitoSOX Red [62] [56] | Redox signaling measurement, Oxidative stress assessment | Probe selectivity limitations (DCF detects multiple ROS); pH sensitivity; appropriate controls essential |
| Gene Expression Tools | ARE-luciferase reporter constructs [57], Nrf2 antibodies, qRT-PCR primers for Nrf2 targets | Pathway activation assessment, Mechanistic studies | Transfection efficiency controls; antibody specificity validation; reference gene stability |
| Exercise Assessment | VO₂max equipment, Muscle biopsy needles, ELISA exerkine kits [56] | Human exercise studies, Systemic effect analysis | Standardized exercise protocols; proper sample processing; assay validation requirements |
| Lifespan Assessment | Colony forming unit assays, Automated cell counters [61] | Chronological lifespan studies, Cell viability | Consistent plating techniques; appropriate dilution series; multiple time point measurements |
Signaling Pathways and Visualization
Integrated Hormetic Signaling Network
The major signaling pathways activated by hormetic stressors converge on a core network that regulates cellular defense, metabolism, and resilience. The diagram below illustrates the integrated signaling network through which sulforaphane, resveratrol, exercise, and caloric restriction mediate their hormetic effects.
Nrf2-Keap1 Signaling Pathway
The Nrf2-Keap1 pathway represents a central mechanism through which multiple hormetic stressors enhance cellular defense capabilities. The following diagram details the molecular events in Nrf2 activation and downstream responses.
Exercise-Induced Redox Signaling
Physical activity triggers complex redox signaling events that mediate its hormetic benefits. This diagram illustrates the key sources of ROS during exercise and their signaling targets.
The study of model stressors and inducers within the framework of hormesis provides powerful insights into fundamental biological principles that govern adaptive responses and resilience. Sulforaphane, resveratrol, exercise, and caloric restriction represent diverse yet complementary approaches to enhancing physiological function through targeted stress activation. The converging mechanisms among these inducers, particularly through the Nrf2 pathway, sirtuin activation, and AMPK/TORC1 signaling, reveal an evolutionarily conserved network for maintaining redox homeostasis and cellular defense.
Future research directions should focus on elucidating the quantitative parameters of hormetic responses, including precise dose-response relationships, temporal dynamics, and individual variability factors. The development of targeted delivery systems, such as nanoencapsulation technologies for resveratrol and other phytochemicals, represents a promising approach to overcoming bioavailability limitations while maximizing therapeutic benefits [59]. Additionally, exploring synergistic combinations of hormetic interventions, as demonstrated by the enhanced effects of caloric restriction combined with rapamycin [61], may reveal novel strategies for optimizing healthspan and combating age-related diseases.
As the field advances, translating these mechanistic insights into evidence-based interventions will require rigorous randomized controlled trials with standardized protocols, validated biomarkers of hormetic responses, and consideration of individual factors such as genetics, age, and physiological status. The continued exploration of hormesis mechanisms in redox biology promises to yield innovative approaches for enhancing human health and resilience through the judicious application of mild stress.
Preconditioning represents one of the most robust manifestations of hormesis in biomedical science, wherein exposure to a low-dose, non-lethal stressor significantly enhances tissue resilience against subsequent, more severe insults. The foundational observation in 1986 by Murry et al. demonstrated that brief, sublethal ischemia reduced myocardial infarct size by approximately 75% following prolonged coronary occlusion in dogs, establishing the ischemic preconditioning phenomenon [63]. This adaptive response has since been generalized across numerous species, extended to various organs including brain, liver, and kidneys, and broadened to include diverse conditioning stimuli—physical, mechanical, physiological, dietary, and pharmacological [63]. The conceptual framework of preconditioning aligns precisely with the core principles of hormesis, characterized by a biphasic dose-response where low doses stimulate protective adaptations while high doses cause damage [4]. Within redox biology, preconditioning represents a form of "positive oxidative stress" that activates endogenous defense mechanisms through precisely regulated redox signaling [64]. This technical guide comprehensively examines the quantitative features, molecular mechanisms, experimental methodologies, and therapeutic applications of preconditioning-induced hormesis for neuro- and cardio-protection.
Quantitative Foundations of Preconditioning Hormesis
The hormetic dose-response relationship in preconditioning follows consistent quantitative patterns that transcend biological models, conditioning agents, and mechanistic pathways. Analysis of 154 preconditioning agents reveals that the maximum protective response typically ranges between 30% and 60% enhancement above baseline, with the protective dose range usually spanning less than 100-fold [63]. This characteristic modest stimulation occurs within a specific therapeutic window, outside which protective effects diminish.
Temporal Dynamics of Protection: Preconditioning hormesis manifests through distinct temporal phases of protection [63]:
- Early Window (1-3 hours): Rapid but transient protection mediated by post-translational modifications of existing proteins
- Late/Delayed Window (12-72 hours): More sustained protection requiring de novo protein synthesis and genomic reprogramming
Table 1: Quantitative Characteristics of Preconditioning Hormesis
| Parameter | Quantitative Range | Biological Specificity |
|---|---|---|
| Maximum Protective Effect | 30-60% above baseline | Independent of biological model, endpoint, or mechanism |
| Dose/Concentration Range | Typically <100-fold | Consistent across pharmacological, chemical, and physical stressors |
| Onset of Early Protection | 1-3 hours post-conditioning | Mediated by rapid post-translational modifications |
| Onset of Late Protection | 12-24 hours post-conditioning | Requires new protein synthesis and genomic activation |
| Duration of Protection | Early: 2-3 hours; Late: 48-72 hours | Dependent on conditioning stimulus and tissue type |
Table 2: Protection Windows in Preconditioning Hormesis
| Protection Phase | Key Mediators | Signaling Pathways | Molecular Effectors |
|---|---|---|---|
| Early (1-3 hours) | Post-translational modifications, ion channel regulation | PKC, MAPK, PI3K/Akt, ROS signaling | KATP channels, antioxidant enzymes, mitochondrial complexes |
| Late/Delayed (12-72 hours) | De novo protein synthesis, transcriptional activation | NF-κB, Nrf2, HIF-1α | Antioxidant enzymes, heat shock proteins, growth factors, anti-apoptotic proteins |
Molecular Mechanisms: Redox Signaling in Preconditioning
The molecular architecture of preconditioning-induced hormesis centers on sophisticated redox signaling networks that convert initially stressful stimuli into protective adaptations. Rather than causing indiscriminate oxidative damage, preconditioning generates precisely controlled reactive oxygen and nitrogen species (ROS/RNS) that function as signaling messengers [64].
Key Signaling Pathways
Multiple evolutionarily conserved signaling cascades mediate the hormetic response to preconditioning:
- NF-κB Pathway: Activated by various preconditioning stimuli, regulating inflammatory responses and cell survival programs [4]
- MAPK Pathways: Transduce stress signals into transcriptional and post-translational responses [4]
- PI3K/Akt Pathway: Critical pro-survival signaling cascade inhibiting apoptosis and enhancing metabolic resilience [4]
- Nrf2-Keap1 System: Master regulator of antioxidant response element (ARE)-driven gene expression [63]
- HIF-1α Signaling: Activated by hypoxic preconditioning, coordinating adaptive responses to low oxygen [63]
Protein Redox Modifications as a Central Defense Mechanism
Reversible redox modifications of cysteine residues serve as a fundamental cellular defense mechanism in preconditioning hormesis, creating an "on-and-off" switch that regulates protein function during stress challenges [64]. These modifications include:
- S-Sulfenation (–SOH): Formation of sulfenic acid, a sensor of oxidative stress
- S-Nitrosylation (–SNO): NO-mediated regulation of protein activity
- S-Glutathionylation (–SSG): Mixed disulfide formation with glutathione
- Disulfide Bond Formation: Intramolecular or intermolecular bridges that modulate protein function
The detection of these reversible modifications employs the biotin switch assay, involving blocking of unmodified cysteines with alkylating reagents like N-ethylmaleimide (NEM), specific reduction of modified residues (ascorbic acid for S-nitrosylation, arsenite for S-sulfenation, glutaredoxin for S-glutathionylation), followed by relabeling with biotin-conjugated NEM for detection and affinity purification [64].
Molecular Architecture of Preconditioning Hormesis: This diagram illustrates the sequential activation of redox signaling pathways and protein modifications that convert mild stress into cytoprotective adaptations.
Experimental Models and Methodologies
Cerebral Ischemic Preconditioning Model
A recent innovative application demonstrates unilateral common carotid artery occlusion (UCCAo) as a preconditioning stimulus to induce ischemic tolerance against transient global cerebral ischemia (tGCI) [65]. This model simulates chronic cerebral hypoperfusion as a preconditioning stimulus.
Experimental Protocol:
- Animals: Adult CD1 mice (22-25 weeks), both sexes
- Preconditioning Stimulus: Permanent right unilateral common carotid artery occlusion (rUCCAo)
- Conditioning Period: 10-12 weeks to establish chronic cerebral hypoperfusion
- Lethal Ischemia: Bilateral common carotid artery occlusion (BCCAo) for 5 minutes
- Assessment Timepoints: Days 1 and 7 post-surgery
Functional and Molecular Assessments:
- Behavioral: Neurological-deficit scoring, rotarod test, grip strength test, open field test, novel object recognition test
- Histopathological: Glial activation (GFAP, IBA1), synaptic markers (PSD-95, synaptophysin)
- Molecular: Hypoxia markers (Hif1a), autophagy (Becn1), neurogenesis (Sox2), BDNF, VEGF
Key Findings: Preconditioning reduced mortality, improved neurological scores, enhanced motor and cognitive recovery, controlled glial activation, and upregulated synaptic plasticity markers, demonstrating robust ischemic tolerance [65].
Remote Ischemic Preconditioning (RIPC)
Remote preconditioning represents a clinically translatable approach where brief ischemia in one tissue or organ protects remote tissues from subsequent ischemic injury [63] [66]. The molecular basis involves humoral factors, neuronal signaling, and immune modulation.
Systemic Protection Through Remote Preconditioning: This diagram illustrates how ischemic stimuli applied to peripheral tissues initiate protective signaling that confers resilience to critical organs like the brain and heart.
The Scientist's Toolkit: Essential Research Reagents and Models
Table 3: Research Reagent Solutions for Preconditioning Studies
| Reagent/Category | Specific Examples | Research Application | Mechanistic Role |
|---|---|---|---|
| Chemical Preconditioning Agents | Cyanide, 3-nitropropionic acid, CO, cannabinoids | Induction of chemical hormesis | Mitochondrial ROS signaling, HIF-1α stabilization |
| Pharmacological Activators | δ-opioid agonists (BW373U86), adenosine analogs | Receptor-mediated preconditioning | G-protein coupled receptor signaling, KATP channel activation |
| Oxidative Stress Modulators | Ambroxol, raloxifene, curcumin, thioredoxin inducers | Redox preconditioning models | Nrf2 activation, glutathione metabolism enhancement |
| Cysteine Modification Detection | N-ethylmaleimide (NEM), biotin-conjugated alkylators, dimedone probes | Biotin switch assay for redox modifications | Specific detection of S-sulfenation, S-nitrosylation, S-glutathionylation |
| Molecular Pathway Inhibitors | PI3K inhibitors (LY294002), MAPK inhibitors, antioxidant compounds | Pathway validation studies | Mechanistic dissection of signaling cascades |
| Cell Death Assays TUNEL staining, caspase activity assays, LDH release | Quantification of protective efficacy | Apoptosis and necrosis measurement | |
| Metabolic Probes | Seahorse extracellular flux analyzers, mitochondrial membrane potential dyes | Bioenergetic assessment | Mitochondrial function and metabolic adaptation analysis |
Therapeutic Applications and Future Directions
The translational potential of preconditioning hormesis spans multiple clinical domains, particularly in neurology and cardiology. Current research focuses on several promising areas:
Clinical Translation Challenges
Despite robust preclinical evidence, clinical implementation faces several challenges:
- Timing Considerations: The therapeutic window for preconditioning must be precisely calibrated relative to anticipated ischemic events
- Patient-Specific Factors: Age, comorbidities, and concomitant medications significantly influence preconditioning efficacy [66]
- Dose Optimization: Determining the optimal hormetic dose for human applications requires careful titration
Emerging Applications
- Stroke Prophylaxis: Identifying safe preconditioning stimuli for high-risk patients
- Cardiac Surgery: Implementing preconditioning protocols to reduce perioperative ischemic injury
- Neurodegenerative Diseases: Harnessing hormetic principles to enhance neuronal resilience in chronic conditions
- Cancer Therapy Paradox: Understanding how preconditioning mechanisms may inadvertently promote tumor resistance [66]
Technological Innovations
Recent advances in preconditioning research include:
- Exosome-Mediated Protection: Harnessing extracellular vesicles as carriers of protective signals [66]
- Metabolic Reprogramming: Targeting mitochondrial function and cellular energy metabolism
- Epigenetic Modulation: Utilizing histone modifications and DNA methylation to sustain protective phenotypes [66]
- Nanoparticle-Based Delivery: Developing targeted delivery systems for preconditioning mimetics
The continued elucidation of preconditioning mechanisms within the hormesis framework provides exciting opportunities for developing novel therapeutic strategies that enhance innate cellular defense systems against ischemic injury in both neurological and cardiovascular contexts.
Hormesis is an adaptive response characterized by a biphasic dose-response relationship, where exposure to low doses of a stressor induces a stimulatory or beneficial effect, while higher doses cause inhibition or toxicity [4]. This phenomenon, rooted in the ancient Paracelsian principle that "the dose makes the poison," has profound implications in cancer biology, particularly within the context of redox imbalance and cellular stress responses [4] [34]. In carcinogenesis and cancer treatment, hormetic mechanisms manifest through multiple pathways, influencing everything from tumor initiation to therapy resistance.
The essence of hormesis lies in its ability to activate preconditioning mechanisms that enhance cellular defense systems. When applied to cancer biology, this reveals a paradoxical dimension: the same low-dose stressors that may potentially inhibit tumor growth in some contexts can also be co-opted by cancer cells to promote survival advantages and therapy resistance [67] [34] [68]. This dual nature positions hormesis at the critical interface of tumor suppression and promotion, making its understanding essential for developing more effective therapeutic strategies.
Quantitative Characteristics of Hormetic Responses
The quantitative features of hormetic dose responses follow predictable patterns that have been systematically characterized across biological systems. Analysis of 2,189 candidate anticancer agents tested across 13 strains of yeast revealed that 52.5% of chemicals displayed hormetic concentration-responses in at least one strain, with many showing this effect across multiple strains [69].
Table 1: Quantitative Features of Hormetic Responses in Anticancer Agent Screening
| Parameter | Mean Value | Biological Range | Experimental Context |
|---|---|---|---|
| Maximum Stimulatory Response | 27% above control | Typically 30-60% above control | Yeast Anticancer Drug Screen [69] |
| Width of Stimulatory Zone | 5-fold concentration range | ~10-fold average | Various biological models [69] |
| Interval from Maximum Stimulation to ZEP | 3.7-fold | Typically 4-5-fold | NCI Yeast Panel [69] |
| Hormesis Prevalence | 52.5% of chemicals | Varies by biological system | 2,189 candidate anticancer agents [69] |
ZEP: Zero Equivalent Point (the highest dose showing a response equal to the control response)
These quantitative characteristics demonstrate the consistent yet context-dependent nature of hormetic responses. The maximum stimulatory response typically ranges between 30-60% above control levels, while the width of the hormetic zone generally spans approximately 10-fold concentrations [69]. These parameters establish the boundaries within which low-dose stimulation occurs, providing critical reference points for designing therapeutic strategies that either exploit or avoid hormetic effects.
Hormetic Mechanisms in Redox Biology and Cancer
The molecular mechanisms underlying hormesis involve complex signaling network interactions that regulate cellular responses to oxidative stress. Cancer cells, particularly cancer stem cells (CSCs), exploit these mechanisms to maintain redox homeostasis and promote survival under therapeutic stress [34].
Redox-Sensitive Signaling Pathways
Diagram 1: Dual Role of ROS in Hormetic and Toxic Signaling Pathways
The Nrf2-Keap1 pathway serves as a central regulator of cellular defense against oxidative and electrophilic insults. Under basal conditions, Keap1 targets Nrf2 for degradation, but oxidative stress disrupts this interaction, allowing Nrf2 translocation to the nucleus where it binds to the Antioxidant Response Element (ARE) and induces expression of antioxidant and detoxifying enzymes [34]. In CSCs, highly active Nrf2 signaling maintains redox homeostasis and confers therapy resistance through upregulation of glutathione (GSH), superoxide dismutase (SOD), and catalase, along with metabolic adaptation via the pentose phosphate pathway for NADPH production [34].
The NF-κB pathway demonstrates the contextual duality of hormetic responses in cancer. At low ROS levels, NF-κB activation promotes CSC survival, immune evasion, and therapy resistance through upregulation of anti-apoptotic genes and cross-talk with Notch and Wnt pathways [34]. However, chronic or high-level NF-κB activation contributes to neuroinflammation and neuronal damage in neurodegenerative contexts, demonstrating its pathway-specific functionality [34].
Similarly, the MAPK pathway exhibits concentration-dependent effects: moderate ROS activates ERK, JNK, and p38 MAPK to promote self-renewal and survival in CSCs, while excessive ROS induces differentiation or apoptosis through the same pathways [34].
Experimental Evidence of Chemotherapeutic Hormesis
In Vitro Demonstration in Ovarian Cancer Models
Recent investigations in ovarian cancer models provide compelling evidence for chemotherapeutic hormesis. Studies using NOS3 ovarian cancer cells, particularly drug-resistant variants (NOS3TR), demonstrated enhanced proliferation when exposed to low concentrations of cisplatin (CDDP) and paclitaxel (PTX) [67]. This hormetic effect was further amplified under hypoxic conditions, mimicking the tumor microenvironment (TME) [67].
Table 2: Experimental Evidence of Chemotherapeutic Hormesis in Ovarian Cancer Models
| Experimental Component | Findings | Methodology | Citation |
|---|---|---|---|
| Cell Proliferation | Low-dose CDDP and PTX stimulated proliferation of drug-resistant NOS3TR cells | Live-cell imaging with IncuCyte ZOOM; MTS assay | [67] |
| Hypoxic Amplification | Hormetic effects enhanced under 1% O2 conditions | Hypoxic chamber experiments | [67] |
| Cell Cycle Alterations | Low-dose CDDP upregulated G2/M checkpoint and mitotic spindle pathways | Flow cytometry with PI staining; RNA sequencing | [67] |
| ROS Pathway Activation | Increased glutathione levels and oxidative stress response | Metabolome analysis; capillary electrophoresis time-of-flight MS | [67] |
| Molecular Pathways | Upregulation of cell cycle progression pathways | RNA sequencing; gene set enrichment analysis | [67] |
Protocol: Assessing Chemotherapeutic Hormesis In Vitro
Objective: To evaluate the potential hormetic effects of chemotherapeutic agents on cancer cell proliferation.
Materials and Reagents:
- Ovarian cancer cell lines (e.g., NOS3, A2780) and their drug-resistant variants (e.g., NOS3TR)
- Chemotherapeutic agents: cisplatin (CDDP), paclitaxel (PTX)
- RPMI 1640 medium supplemented with 10% fetal bovine serum
- 96-well plates for cell culture
- IncuCyte ZOOM system for live-cell imaging or MTS assay reagents
- Hypoxic chamber (1% O2) for TME-mimicking conditions
- Annexin V RED reagent for apoptosis assays
- Propidium iodide staining solution for cell cycle analysis
Methodology:
- Cell Seeding: Seed cells onto 96-well plates at density of 2,000 cells/well and allow to adhere for 24 hours [67].
- Drug Treatment: Prepare step-diluted concentrations of chemotherapeutic agents (e.g., 1.2, 3.7, 11, 33, and 100 μM) and apply to cells [67].
- Proliferation Monitoring: Transfer plates to IncuCyte ZOOM system for live-cell imaging, recording images every hour for 72 hours. Use software to determine confluence by masking cell regions [67].
- Validation Assay: Parallel assessment using MTS assay - add CellTiter 96 Aqueous One Solution after 72-hour incubation, measure optical density at 490nm [67].
- Hypoxic Conditions: Repeat experiments in 1% O2 atmosphere to simulate TME [67].
- Cell Cycle Analysis: Harvest cells after 48h treatment, fix with 70% ethanol, stain with propidium iodide/RNase A solution, and analyze using flow cytometry [67].
- Apoptosis Assessment: Seed cells in 6-well plates, treat with step-diluted CDDP, and use Annexin V RED reagent according to manufacturer's protocol [67].
Mathematical Modeling of Hormesis in Combination Therapies
Mathematical modeling provides powerful tools for understanding the complex dynamics of hormesis in cancer treatment. Recent models have explored combinations of radio/chemotherapy with immunotherapy, revealing paradoxical effects and synergistic opportunities [68].
Model Framework for Combination Therapy
The interactions between effector cells (E), tumor cells (T), and cytokines (IL-2) with pulsed radio/chemo-immunotherapy can be described by the following system [68]:
Diagram 2: Mathematical Model Structure for Combination Therapy with Hormetic Effects
The model reveals that combination therapy can produce mixed response curves (MRCs) with complex dynamics, including multiple humps and a "mixed fuzzy region" between the hormetic zone and toxic threshold [68]. These complexities pose significant challenges for clinical trial design and interpretation but also offer opportunities for optimized therapeutic sequencing.
Key Findings from Mathematical Modeling
- Low-dose radio/chemotherapy combined with high-dose immunotherapy effectively inhibits tumor growth while counteracting side-effects of radio/chemotherapy on effector cells and cytokines [68]
- The net benefit and synergistic effect of combined therapy is conducive to tumor treatment and inhibition [68]
- Threshold conditions exist for tumor-free periodic solutions, providing mathematical basis for treatment strategy design [68]
- Pulsatile treatment schedules can maximize therapeutic efficacy while minimizing hormetic stimulation of tumor growth [68]
Research Reagent Solutions for Hormesis Studies
Table 3: Essential Research Reagents for Investigating Hormesis in Cancer Biology
| Reagent/Cell Line | Specifications | Research Application | Citation |
|---|---|---|---|
| Ovarian Cancer Cell Lines | NOS2, NOS3, NOS4; PTX-resistant strains: NOS2TR, NOS3TR, NOS4TR | In vitro modeling of chemotherapeutic hormesis in drug-sensitive and resistant contexts | [67] |
| Chemotherapeutic Agents | Cisplatin (CDDP), Paclitaxel (PTX) at step-diluted concentrations (1.2, 3.7, 11, 33, 100 μM) | Induction and quantification of hormetic dose-responses | [67] |
| Hypoxic Chamber System | 1% O2 atmosphere capability | Simulation of tumor microenvironment conditions that amplify hormetic effects | [67] |
| Live-Cell Imaging System | IncuCyte ZOOM with confluence masking software | Real-time monitoring of cell proliferation and death in response to treatment | [67] |
| Apoptosis Detection | Annexin V RED reagent | Quantification of programmed cell death versus proliferative responses | [67] |
| Cell Cycle Analysis | Propidium iodide staining with RNase A, flow cytometry | Assessment of cell cycle alterations under low-dose chemotherapeutic exposure | [67] |
| Molecular Analysis | RNA sequencing, metabolome analysis (capillary electrophoresis time-of-flight MS) | Mechanistic investigation of pathway alterations in hormetic responses | [67] |
Clinical Implications and Therapeutic Strategies
The phenomenon of chemotherapeutic hormesis necessitates a paradigm shift in oncology treatment design. Traditional maximum tolerated dose approaches may inadvertently stimulate tumor growth in specific microenvironments, particularly in resistant subclones and under hypoxic conditions [67]. Instead, more nuanced strategies that account for the biphasic nature of dose responses are needed.
Strategic Approaches to Mitigate Hormetic Risks
Combination Therapy Optimization: Mathematical modeling demonstrates that low-dose radio/chemotherapy combined with high-dose immunotherapy can effectively inhibit tumor growth while counteracting side-effects on immune effector cells [68]. This approach leverages the synergistic potential of combined modalities while minimizing the risk of hormetic stimulation.
Microenvironment-Targeted Interventions: Since hypoxic conditions amplify chemotherapeutic hormesis [67], strategies that normalize the tumor vasculature or directly target hypoxic regions may reduce this risk. This includes the use of hypoxia-activated prodrugs and anti-angiogenic agents in combination with conventional chemotherapy.
Metabolic Pathway Modulation: The observed upregulation of glutathione and ROS pathway activation in hormetic responses [67] suggests that targeting antioxidant systems may mitigate low-dose stimulation. Interventions that modulate Nrf2 signaling or deplete glutathione reserves could potentially reverse hormetic advantages in cancer cells.
Adaptive Therapy Approaches: Leveraging evolutionary dynamics through adaptive therapy strategies, which maintain sensitive cells to suppress resistant growth, may circumvent hormetic stimulation by avoiding continuous selective pressure that favors resistant clones with hormetic capabilities.
Future Directions and Research Opportunities
The investigation of hormesis in cancer biology presents numerous opportunities for advancing therapeutic strategies. Key research priorities include:
Single-Cell Analysis of Hormetic Responses: Heterogeneity in hormetic responses within tumor populations likely contributes to therapeutic resistance. Single-cell RNA sequencing and proteomic approaches could identify subpopulations with heightened hormetic potential.
Temporal Dynamics of Hormetic Signaling: The transition from adaptive to toxic responses occurs within specific temporal windows that remain poorly characterized. Detailed kinetic studies of pathway activation could identify critical timing for therapeutic interventions.
Microenvironmental Influences on Hormetic Thresholds: Systematic mapping of how various TME components (hypoxia, acidity, stromal interactions) modulate hormetic thresholds would enhance our ability to predict and control these responses.
Computational Model Refinement: Expanding mathematical models to incorporate spatial heterogeneity, immune cell diversity, and multi-scale interactions would improve their predictive power for designing combination therapies.
The integration of hormesis principles into cancer biology represents both a challenge and an opportunity. By understanding and accounting for these biphasic dose responses, researchers and clinicians can develop more effective therapeutic strategies that leverage adaptive responses while avoiding unintended stimulation of tumor growth.
Navigating Challenges and Optimizing Hormetic Interventions in Research and Therapy
Hormesis is a fundamental dose-response phenomenon characterized by biphasic kinetics, where exposure to low doses of a stressor induces a stimulatory or beneficial effect, while higher doses produce inhibitory or toxic effects [4] [70]. This adaptive response represents a central evolutionary strategy across biological systems, from microbial organisms to mammals [70]. The term "hormetic zone" specifically refers to the quantifiable dose range within which these stimulatory effects occur, bounded below by the no-effect level and above by the toxic threshold [71]. The conceptual foundation of hormesis dates back to the 16th century with Paracelsus's assertion that "the dose makes the poison," but it was not until recent decades that its mechanistic foundations and quantitative features have been systematically characterized through large-scale database analysis and molecular studies [13] [72].
The hormetic zone defines the bounds of biological plasticity – the capacity of organisms to adapt to environmental challenges without succumbing to toxicity [70]. Understanding the precise parameters of this zone is particularly crucial in biomedical contexts, where harnessing hormetic mechanisms offers promising avenues for therapeutic interventions, especially in drug development for conditions involving oxidative stress, neurodegenerative diseases, and aging [4] [73]. This technical guide provides a comprehensive framework for quantifying the hormetic zone, with specific emphasis on experimental methodologies, quantitative parameters, and molecular mechanisms relevant to redox biology research and pharmaceutical development.
Quantitative Characteristics of the Hormetic Zone
The hormetic dose response exhibits consistent quantitative features that are generalizable across biological models, endpoints, and chemical classes [72] [70]. These characteristics can be systematically measured and provide the foundation for experimental design and data interpretation.
Core Quantitative Parameters
Large-scale analyses of hormetic dose responses, encompassing approximately 9,000 dose responses in the hormesis database, reveal three fundamental parameters that define the hormetic zone [69] [72]:
Table 1: Core Quantitative Features of the Hormetic Zone
| Parameter | Typical Range | Mean Value | Biological Significance |
|---|---|---|---|
| Maximum Stimulatory Response | 130-160% of control | ~130-140% of control | Defines limits of biological plasticity; constrained by evolutionary resource allocation |
| Width of Stimulatory Range | <50-fold | ~5-fold (from ZEP to toxic threshold) | Determines therapeutic window for potential applications |
| Interval from Maximum Stimulation to ZEP | 4-5 fold | ~3.7-fold | Indicates steepness of response gradient below peak effect |
The maximum stimulatory response is typically modest, generally ranging between 30-60% above control levels, with a mean of approximately 27% above controls (127% of control) observed in anticancer agent screening [69]. This consistent observation across biological models suggests an evolutionary compromise between enhanced performance and the metabolic costs of adaptation [70]. The quantitative features remain remarkably consistent independent of the biological model, endpoint measured, or chemical class, highlighting the fundamental nature of the hormetic response [72].
Recent evidence suggests that these parameters can be influenced by study design. The maximum hormetic response increases by approximately 5-7% for each additional dose evaluated below the threshold dose, potentially approaching the 180-200% range with optimal study design [73]. Furthermore, the hormetic dose zone typically extends less than 50-fold when starting immediately below the threshold dose, with the width from the maximum stimulation to the toxicological threshold averaging approximately 3.7-fold [69].
Hormetic Zone in Specific Biomedical Contexts
In anticancer research, analysis of 2,189 candidate anticancer agents across 13 yeast strains revealed that 52.5% of chemicals displayed hormetic concentration-responses in at least one strain, with 24 agents showing hormesis in all 13 strains [69]. The quantitative features in this context demonstrated a mean maximum stimulation of 27% above controls, with a 5-fold width for the concentration range showing stimulation above 10% of control, and a 3.7-fold width from the maximum stimulation to the toxicological threshold [69].
Table 2: Hormetic Parameters for Selected Anticancer Agents (in vitro)
| Anticancer Agent | Maximal Response of Hormetic Reaction (Mh) | hED50 | cED50 | h/c ED50 Ratio |
|---|---|---|---|---|
| Gemcitabine | Data not reported | Lowest among agents tested | Data not reported | Lowest among agents tested |
| 5-Fluorouracil | Data not reported | Lowest among agents tested | Data not reported | Lowest among agents tested |
| Cisplatin | Data not reported | Intermediate | Data not reported | Intermediate |
| Vinorelbine | Data not reported | Intermediate | Data not reported | Intermediate |
| Paclitaxel | Data not reported | Highest among agents tested | Data not reported | Highest among agents tested |
Agents with lower h/c ED50 ratios, such as gemcitabine and 5-fluorouracil, demonstrated more pronounced promotive effects, highlighting the importance of quantifying the relationship between hormetic and cytotoxic concentrations for therapeutic applications [74]. The hormetic reaction for these agents progressed exponentially with culturing time, indicating temporal dynamics must be considered in quantitative assessments [74].
Molecular Mechanisms: The Nrf2 Signaling Pathway
The consistency of hormetic responses across biological systems suggests common underlying mechanisms, with the Nrf2-mediated antioxidant response emerging as a central pathway [73]. The Nrf2 pathway serves as a master regulator of cellular redox homeostasis and represents a primary molecular mechanism through which subtoxic stressors activate cytoprotective responses.
Nrf2 Activation Pathway
The Nrf2 signaling pathway can be visualized through the following molecular mechanism:
The mechanism begins when low-dose stressors (chemical or radiation) induce mild reactive oxygen species (ROS) production [73]. These ROS function as signaling molecules rather than damaging agents at hormetic doses, triggering a conformational change in the Keap1 protein through modification of critical cysteine residues [13] [73]. This modification releases the transcription factor Nrf2, which is then stabilized and translocates to the nucleus [73]. In the nucleus, Nrf2 binds to Antioxidant Response Elements (ARE) in the promoter regions of target genes, initiating the transcription of a network of over 500 cytoprotective genes [13] [73]. This coordinated gene expression enhances cellular resilience through multiple mechanisms, including antioxidant defense, detoxification, anti-inflammation, and facilitation of mitochondrial biogenesis [73].
Network Effects and Cross-Talk
The Nrf2 pathway does not function in isolation but engages in productive cross-talk with other signaling networks, including NF-κB, MAPK, AMPK, and mTOR pathways [4] [73]. This network interaction enables the integrated cellular response that characterizes hormesis, coordinating multiple adaptive mechanisms that collectively enhance biological performance within the constraints of the hormetic zone [70] [73]. The activation of these interconnected pathways results in the expression of phase 2 enzymes, antioxidant enzymes, heat-shock proteins, growth factors, and proteins involved in regulating cellular energy metabolism [4].
The hierarchical organization of these signaling networks ensures that the magnitude of response remains within the bounds of biological plasticity, with the quantitative features of the hormetic dose response emerging from the integrated output of these multiple interacting pathways [70]. This mechanistic understanding provides a foundation for targeted therapeutic interventions that aim to harness hormetic mechanisms for disease prevention and treatment.
Experimental Protocols for Quantifying Hormetic Zones
Rigorous experimental design is essential for accurate quantification of the hormetic zone. The following protocols provide methodological frameworks for detecting and characterizing hormetic responses in research settings.
Comprehensive Dose-Response Study Design
The experimental workflow for quantifying hormetic zones requires careful planning at each stage:
Dose Selection Protocol:
- Utilize a minimum of five concentrations below the estimated toxic threshold [69]
- Include concentrations at 1.2, 3.7, 11, 33, and 100 μM as a starting template, adapting as needed for specific agents [69]
- Ensure adequate dose spacing with 3-5 fold increments to resolve the hormetic zone [69]
- Include sufficient replicate samples (e.g., octuplicate samples for in vitro assays) to provide statistical power [74]
Temporal Kinetics Assessment:
- Conduct measurements at multiple time points as hormetic responses may have different temporal patterns than toxic responses [70]
- For anticancer agent screening, monitor responses over 24-hour period with multiple assessment points to capture exponential progression of hormetic reactions [74]
- Consider preconditioning and postconditioning protocols where a low dose is administered before or after a toxic challenge to assess adaptive resilience [73]
Endpoint Selection and Measurement:
- Define stimulatory and inhibitory responses using a priori criteria, typically setting hmax ≤ 80% of control response for inhibition and Smin ≥ 110% of control response for stimulation [69]
- Measure multiple endpoints where possible, including cell proliferation, DNA repair, antioxidant defenses, autophagy, and mitochondrial function [70]
- Utilize validated assays such as MTT assay for cell viability with proper controls including solvent controls and untreated controls [74]
Statistical Modeling and Data Analysis
Hormetic Dose-Response Modeling:
- Apply biphasic sigmoidal models for curve fitting, such as the equation: y = (a - b/(1 + exp(clog(x) - d)))/(1 + exp(elog(x) - f)) [74]
- Use non-linear least square regression with algorithms such as Davidon-Fletcher-Powell for parameter estimation [74]
- Compare model adequacy using information criteria such as the Akaike Information Criterion [74]
Parameter Quantification:
- Calculate the maximum stimulatory response (Mh) as the peak response above controls [74]
- Determine the hED50 (half-maximal effective dose for hormetic reaction) and cED50 (half-maximal effective dose for cytotoxicity) [74]
- Compute the h/c ED50 ratio to assess the therapeutic window [74]
- Identify the Zero Equivalent Point (ZEP) where the response crosses the control value [69] [72]
Validation and Quality Control:
- Implement replication protocols with experiments conducted on separate days to account for variability [69]
- Include appropriate controls in each experiment: unexposed controls, solvent controls, and agent-specific controls (e.g., cycloheximide in yeast assays) [69]
- Establish criteria for assay validity a priori (e.g., assay invalid if growth occurs in cycloheximide controls for cycloheximide-sensitive strains) [69]
The Scientist's Toolkit: Research Reagent Solutions
This section provides essential reagents and methodological solutions for researchers quantifying hormetic zones in redox biology and drug development contexts.
Table 3: Essential Research Reagents for Hormesis Studies
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Nrf2 Activators | Sulforaphane, Curcumin, Quercetin, Ginsenoside, Anthraquinone-BME | Induction of hormetic responses via antioxidant pathway activation | Dose-dependent effects; typically effective in nM to low μM range [73] |
| Anticancer Agents | Gemcitabine, Cisplatin, 5-Fluorouracil, Vinorelbine, Paclitaxel | Study of hormetic zones in chemotherapeutic contexts | h/c ED50 ratio predicts prominence of hormetic effects [74] |
| Cell-Based Assay Systems | A549 lung cancer cells, RAW 264.7 mouse macrophages, primary neuronal cultures | In vitro quantification of hormetic parameters | Cell line selection influences response characteristics [74] [73] |
| Viability Assays | MTT assay, Histoculture Drug Response Assay (HDRA) | Assessment of cell proliferation and viability in hormetic zones | HDRA maintains cell-to-cell contact for better clinical predictability [74] |
| Oxidative Stress Probes | DCFDA, DHE, MitoSOX | Quantification of ROS signaling in hormetic responses | Distinguish between signaling and damaging ROS levels [73] |
| Pathway Inhibitors | KEAP1 siRNA, Nrf2 inhibitors | Mechanistic studies of hormetic pathways | Confirm Nrf2 dependency of observed responses [73] |
Experimental Model Selection:
- Yeast strains (Saccharomyces cerevisiae) with mutations in DNA damage repair or cell cycle control genes provide high-throughput screening platforms [69]
- Mammalian cell lines with specific genetic backgrounds relevant to disease models enable translation to therapeutic contexts [74]
- Primary cell cultures and 3D tissue models may provide more physiologically relevant hormetic response data [74]
Analytical Tools:
- Statistical software with non-linear regression capabilities (e.g., R, GraphPad Prism, MacCurveFit) for biphasic dose-response modeling [71] [74]
- High-content screening systems for multiparameter assessment of hormetic responses [69]
- Oxidative stress monitoring systems for real-time assessment of redox changes during hormetic responses [73]
The precise quantification of the hormetic zone provides a critical framework for understanding biological plasticity and developing therapeutic strategies that harness adaptive responses. The consistent quantitative features of hormesis – particularly the modest stimulation range (typically 130-160% of control) and constrained dose range (generally <50-fold) – define fundamental boundaries of biological performance [69] [72] [70]. The Nrf2-mediated antioxidant response represents a central mechanistic pathway through diverse stressors activate cytoprotective adaptations within these constrained parameters [73].
For researchers and drug development professionals, rigorous experimental design incorporating appropriate dose selection, temporal kinetics, and statistical modeling of biphasic responses is essential for accurate quantification of hormetic zones [69] [71] [74]. The growing recognition of hormesis as a fundamental biological principle continues to transform approaches to toxicology, pharmacology, and therapeutic intervention, particularly in aging, neurodegenerative diseases, and cancer treatment [4] [70] [73]. As research in this field advances, the precise delineation of hormetic zones will increasingly inform the development of targeted therapies that optimize adaptive responses while minimizing toxic effects.
Hormesis, the biphasic dose-response phenomenon where low-dose stressors stimulate beneficial adaptations, is a central theme in redox biology. The manifestation of this adaptive response is not uniform but is profoundly shaped by the specific experimental and biological context. This technical review delineates how three critical factors—cell type, exposure duration, and biomarker heterogeneity—orchestrate the fate of hormetic outcomes. Through an analysis of current literature, we provide a framework for researchers to design robust experiments, account for contextual variability, and accurately interpret the complex mechanisms underpinning redox hormesis, thereby facilitating its potential application in therapeutic development.
The concept of hormesis describes an evolutionary conserved adaptive response where exposure to a low dose of a stressor that is detrimental at high doses, elicits a beneficial, stimulatory effect on the cell or organism [4]. In the realm of redox biology, this is frequently observed as the adaptive and protective upregulation of antioxidant and cytoprotective pathways in response to mild oxidative or electrophilic stress [6] [75]. This process is fundamental to maintaining redox homeostasis, the delicate balance between oxidant production and antioxidant defense that is crucial for healthy physiological function [75].
However, the induction of hormesis is not a simple, linear process. The resulting phenotype—whether protective or detrimental—is a complex toxicological event based on a network of beneficial and detrimental effects that are poorly understood [6]. A significant challenge in the field is the heterogeneity of reported responses, often leading to seemingly contradictory results. This review posits that such variability is not noise but rather a direct consequence of the interplay between core experimental and biological variables. We will critically examine how cell type-specific factors, temporal dynamics of exposure, and the selection of biomarker endpoints collectively dictate the qualitative and quantitative nature of the hormetic response. Understanding these factors is paramount for leveraging hormesis as a mechanistic basis for improving therapeutic strategies in conditions ranging from neurodegenerative diseases to metabolic disorders [30].
Critical Factor 1: Cell Type
The biological system under investigation is a primary determinant of the hormetic response. Different cell types possess unique genetic, metabolic, and signaling backgrounds that shape their perception of and reaction to a redox challenge.
Mechanistic Basis for Cell-Type Specificity
The inherent differentiation state, metabolic profile, and baseline redox status of a cell create a distinct context for stress response. Key signaling pathways such as NRF2, NF-κB, and AMPK/mTOR are universally involved in hormesis, but their activation dynamics and downstream targets can vary significantly between cell types [4] [30]. For instance, the NRF2-mediated antioxidant response is a master regulator of redox homeostasis, but the specific battery of genes it activates (e.g., GCLC, GCLM, HMOX1, NQO1) can be tissue- and cell-type-dependent [39]. Furthermore, the expression levels of receptors, drug transporters, and metabolizing enzymes like cytochrome P450 (CYPs) and glutathione S-transferases differ across cell types, leading to variations in the intracellular concentration of the bioactive compound and thus, the observed effect [6].
Experimental Evidence
A compelling illustration of this factor comes from studies on olive oil polyphenols. Research shows that a specific phenolic extract increased intracellular glutathione (GSH) in human cervical adenocarcinoma HeLa cells at doses of 15.0 and 20.0 μg, while in human hepatocarcinoma HepG2 cells, a similar extract elevated GSH at 1 μg/mL but exhibited a pro-oxidant effect at 1.5 μg/mL [6]. This demonstrates a narrow, cell-type-specific "hormetic gain zone." Similarly, the same olive oil sample decreased a lipid peroxidation biomarker (TBARS) in low doses but increased it at high doses in human endothelial EA.hy926 cells, a response not observed in the other cell lines [6]. These findings underscore that the dose which constitutes a "low-dose" stimulation is not an absolute value but is relative to the cellular context.
Table 1: Cell-Type Dependent Hormetic Responses to Bioactive Compounds
| Bioactive Compound | Cell Type 1 | Observed Response (Cell 1) | Cell Type 2 | Observed Response (Cell 2) | Key Implication |
|---|---|---|---|---|---|
| Olive Oil Polyphenol Extract | HeLa (Cervical Adenocarcinoma) | GSH increased at 15-20 μg | HepG2 (Hepatocarcinoma) | GSH increased at 1 μg; decreased at 1.5 μg | Metabolic capacity alters effective hormetic dose. |
| Sulforaphane | Human Mesenchymal Stem Cells | 1 μΜ: protection from oxidative damage and apoptosis. | In vivo tissue models (implied) | Tissue-specific gene expression profiles via NRF2. | Differentiation state influences stress resilience. |
| Negative Air Ions (NAIs) [in vivo] | Liver & Blood Cells (Mouse Model) | Short-term: Enhanced mitochondrial efficiency. Long-term: Metabolic reprogramming. | Brain Cells (Mouse Model) | Activated autophagic clearance, reduced neurodegeneration markers [8]. | Target organ function dictates adaptive outcome. |
Critical Factor 2: Exposure Duration
The temporal component of the stressor application is a critical, yet often overlooked, variable that defines the hormetic phenotype. The distinction between acute, short-term, and long-term exposure can lead to fundamentally different adaptive outcomes.
Temporal Dynamics of Adaptation
Hormesis is a dynamic process. An acute exposure may trigger an immediate but transient protective signaling cascade, such as the rapid phosphorylation of redox-sensitive kinases. Short-term exposure allows for the initiation of transcriptional programs and the synthesis of protective proteins like heat-shock proteins and antioxidant enzymes. In contrast, long-term or chronic exposure can lead to metabolic reprogramming and the establishment of a new physiological "set point" [75]. This temporal progression is evident in exercise physiology, where a single bout of exercise generates reactive oxygen species (ROS) that act as signaling molecules (oxidative eustress), while repeated bouts (training) lead to sustained upregulation of antioxidant defenses, a classic hormetic adaptation [76].
Experimental Evidence
A recent 2025 study on negative air ions (NAIs) provides a clear example of time-dependent hormesis. In a mouse model, metabolomic profiling revealed that short-term exposure (18 days) to an NAI-enriched environment led to increased mitochondrial efficiency and energy homeostasis. In contrast, long-term exposure (28 days) induced a more profound adaptive metabolic reprogramming, characterized by elevated inosine levels, suggesting a shift towards enhanced antioxidant and anti-inflammatory responses [8]. This demonstrates that the hormetic phenotype evolves, and that the optimal duration of exposure for a desired outcome must be empirically determined. Similarly, in physical training, the beneficial redox modulation is a result of repeated, acute bouts of exercise that collectively build resilience, aligning with the hormesis principle [76].
Diagram 1: Temporal dynamics of hormetic exposure leading to distinct adaptive outcomes.
Critical Factor 3: Biomarker Heterogeneity
The selection of biomarkers to assess hormetic responses is a critical decision that can dramatically influence the interpretation of an experiment. Relying on a single biomarker often provides an incomplete or misleading picture, as different biomarkers capture distinct aspects of the complex redox network.
The Multi-Faceted Nature of Redox Biomarkers
Redox biomarkers can be broadly categorized, each with its own strengths and limitations. A comprehensive assessment should include:
- Antioxidant Enzymes: Superoxide dismutase (SOD), catalase (CAT), glutathione peroxidase (GPx). Their activity can be stimulated or inhibited in a biphasic manner [77] [6].
- Low-Molecular-Weight Antioxidants: Reduced glutathione (GSH). Levels can increase with mild stress but deplete under severe oxidation.
- Markers of Oxidative Damage: Malondialdehyde (MDA) for lipid peroxidation; 8-hydroxy-2'-deoxyguanosine (8-OHdG) for DNA oxidation; protein carbonyls for protein oxidation [78].
- Redox-Sensitive Signaling Nodes: Activation of pathways like NRF2, measured via target genes like NQO1 and HMOX1 [39].
The "hormetic gain zone" is not uniform across these biomarkers. A dose that beneficially upregulates GSH might simultaneously have no effect on SOD activity or might even increase a damage marker like MDA, reflecting the complexity of the underlying biological network [6].
Experimental Evidence
The phenomenon of biomarker heterogeneity is starkly illustrated by studies on olive oil extracts. A tyrosol-rich extract was shown to increase intracellular GSH levels in a wide dose range (10.0–25.0 μg), a clear adaptive response. However, this same extract could simultaneously decrease the activity of the antioxidant enzyme GPx at specific doses within this range [6]. This demonstrates that hormesis is not a global "on/off" switch for all antioxidant systems but a nuanced recalibration of the redox network. Similarly, in exercise research, different intensities of training have disparate effects on various biomarkers: vigorous exercise consistently increases overall antioxidant capacity and decreases oxidants, while non-vigorous exercise may not significantly alter all redox biomarkers [77]. This underscores the need for a multi-parametric biomarker panel to accurately capture the hormetic response.
Table 2: Key Redox Biomarkers and Their Interpretation in Hormesis Studies
| Biomarker Category | Specific Example | Common Measurement Method | Hormetic Interpretation | Considerations |
|---|---|---|---|---|
| Antioxidant Enzyme | Superoxide Dismutase (SOD) | Spectrophotometry | Upregulation indicates enhanced capacity to dismantle superoxide radical. | Activity vs. protein level must be distinguished. |
| Antioxidant Enzyme | Glutathione Peroxidase (GPx) | Spectrophotometry, ELISA | Increased activity suggests improved H₂O₂ detoxification. | Can be transiently inhibited by high ROS. |
| Redox Status | Reduced Glutathione (GSH) | HPLC, spectrophotometric assays | Elevated levels indicate a reductive shift and enhanced antioxidant reserve. | The GSH/GSSG ratio is more informative than GSH alone. |
| Lipid Peroxidation | Malondialdehyde (MDA) | TBARS Assay, HPLC | Decrease indicates reduced oxidative damage to lipids. | TBARS assay can lack specificity; HPLC/MS is preferred. |
| DNA Oxidation | 8-OHdG | ELISA, HPLC-ECD/MS | Decrease indicates reduced oxidative damage to DNA. | Gold standard for genotoxic stress. |
| NRF2 Pathway Activity | NQO1, HMOX1 mRNA/Protein | RT-qPCR, Western Blot | Upregulation confirms activation of the key adaptive pathway. | A panel of 6 genes (GCLC, GCLM, HMOX1, NQO1, SRXN1, TXNRD1) is recommended [39]. |
Integrated Experimental Design and Protocols
To navigate the complexity introduced by the three critical factors, a rigorous and integrated experimental design is non-negotiable. Below is a framework and a detailed protocol exemplifying this approach.
A Framework for Robust Hormesis Research
- Multi-Cellular Model Screening: Initial screening should utilize at least two relevant, physiologically distinct cell types (e.g., hepatic HepG2 and neuronal SH-SY5Y for neurotoxicology studies).
- Comprehensive Time-Course and Dose-Response Matrix: Experiments must include multiple time points (e.g., 6h, 24h, 48h, 7-day chronic) and a wide range of doses (from sub-physiological to clearly toxic) to map the biphasic response landscape.
- Multi-Parametric Biomarker Panels: Assessment should include a combination of functional assays (cell viability), enzymatic activities (SOD, CAT, GPx), redox status (GSH/GSSG), damage markers (MDA, 8-OHdG), and signaling pathway activation (NRF2 target gene expression).
Detailed Experimental Protocol: Assessing Hormesis of a Phytochemical
Objective: To characterize the hormetic profile of Sulforaphane (SFN) in two cell lines. Background: SFN is a well-known NRF2 inducer with demonstrated biphasic effects [6].
Materials and Reagents:
- Cell Lines: Human hepatoma HepG2 and human neuroblastoma SH-SY5Y.
- Test Compound: Sulforaphane (SFN), dissolved in DMSO.
- Key Assay Kits: MTT assay kit (cell viability), GSH-Glo Glutathione Assay, Lipid Hydroperoxide (LPO) Assay kit, SOD Activity Assay Kit, RNA extraction kit and RT-qPCR reagents for NQO1, HMOX1, and GAPDH.
Procedure:
- Cell Culture and Seeding: Maintain cells in standard conditions. Seed cells in 96-well or 24-well plates at an optimized density for 24 hours prior to treatment.
- Dose-Response and Time-Course Treatment: Treat cells with a SFN concentration range (e.g., 0.1 µM, 0.5 µM, 1 µM, 5 µM, 10 µM, 20 µM, 50 µM) and a vehicle control (DMSO). Include replicates for each condition.
- Harvesting: Harvest cells at multiple time points (e.g., 24h and 48h) post-treatment.
- Multi-Parametric Analysis:
- Cell Viability: Perform MTT assay at 24h and 48h.
- Redox Status: Measure intracellular GSH levels using the luminescence-based GSH-Glo Assay.
- Oxidative Damage: Quantify lipid peroxidation via the LPO assay.
- Antioxidant Enzyme Activity: Assess total SOD activity using a spectrophotometric kit.
- NRF2 Pathway Activation: Extract total RNA and perform RT-qPCR to measure mRNA expression of NQO1 and HMOX1. Normalize to GAPDH.
- Data Analysis: Plot dose-response curves for all endpoints. The hormetic zone is identified where viability is ≥110% of control, accompanied by a concurrent upregulation of GSH, SOD, and NRF2 targets, with low LPO.
Diagram 2: A integrated workflow for robust experimental design in redox hormesis studies.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Redox Hormesis Research
| Reagent / Solution | Function in Experiment | Example Use Case |
|---|---|---|
| Sulforaphane (SFN) | A well-characterized NRF2 pathway inducer used as a model hormetic agent. | Positive control for activating antioxidant response elements; studying biphasic dose-response [6]. |
| GSH-Glo Glutathione Assay | A luminescence-based kit for specific and sensitive quantification of cellular reduced glutathione (GSH) levels. | Measuring the reductive shift in the redox state as an adaptive response to low-dose stress. |
| MitoSOX Red | A fluorogenic dye targeting mitochondrial superoxide, allowing live-cell imaging and flow cytometry. | Assessing compartment-specific ROS production during low-dose stress exposure. |
| Antibody Panel for NRF2 Targets | Antibodies against proteins like NQO1, HMOX1 for Western Blot analysis. | Confirming activation of the NRF2 signaling pathway at the protein level. |
| RT-qPCR Primer Panels | Primer sets for genes like GCLC, GCLM, NQO1, HMOX1, SRXN1 to assess NRF2 signaling. | Quantifying transcriptional activation of the adaptive antioxidant response [39]. |
| LC-MS/MS Platform | Gold-standard method for specific quantification of oxidative damage biomarkers (e.g., F2-isoprostanes, 8-OHdG). | Accurately measuring low levels of oxidative damage to lipids and DNA with high specificity [78]. |
The journey to harnessing the therapeutic potential of redox hormesis hinges on a sophisticated understanding of its contextual nature. This review establishes that the hormetic response is not a generic phenomenon but is meticulously sculpted by the triad of cell type, exposure duration, and biomarker heterogeneity. The experimental evidence conclusively shows that a dose beneficial in one cell type may be inert or toxic in another; that short-term adaptations can evolve into long-term reprogramming; and that reliance on a single biomarker can paint a misleading picture of the underlying redox status. Therefore, the future of hormesis research and its translation into drug development and precision medicine lies in the adoption of integrated, multi-parametric experimental designs. By systematically accounting for these critical factors, researchers can move beyond phenomenological observations towards a mechanistic and predictive understanding of how mild stress primes cellular defense systems, ultimately informing strategies to enhance resilience against age-related and metabolic diseases.
Abstract Within the framework of redox hormesis, cells respond to mild oxidative stress by activating coordinated parallel pathways that enhance survival and antioxidant capacity. This whitepaper delineates the molecular mechanisms of two critical pro-survival pathways—the Nuclear Factor Erythroid 2–Related Factor 2 (Nrf2)/Antioxidant Response Element (ARE) axis and the Protein Kinase D1 (PKD1)-dependent signaling cascade. We provide a detailed experimental methodology for investigating these pathways, complete with quantitative data analysis and standardized visualization of the signaling networks. The objective is to offer a technical guide for researchers and drug development professionals aiming to exploit these adaptive mechanisms for therapeutic intervention.
Cellular redox homeostasis is not a state of static equilibrium but a dynamic balance, more accurately described as redox homeodynamics [16]. This dynamic system is continuously shaped by metabolic flux and environmental cues, with reactive oxygen species (ROS) like hydrogen peroxide (H₂O₂) acting as pivotal signaling molecules [16] [79]. The concept of hormesis is central to understanding the biological effects of these redox signals. Hormesis describes the adaptive, beneficial response of cells and organisms to low-level stressors [16] [17].
In redox biology, a mild, non-damaging increase in ROS (a state of oxidative eustress) triggers protective and pro-survival mechanisms. Conversely, excessive ROS production leads to oxidative distress, causing macromolecular damage and cell death [16] [17]. This hormetic response is mediated by the activation of specific, parallel signaling pathways that sense oxidants and transduce these signals into coordinated transcriptional and metabolic reprogramming. The "Redox Code" outlines the organizational principles of these biological redox reactions, emphasizing how redox networks form an adaptive system to respond to the environment [16] [79]. This guide focuses on the experimental dissection of two key parallel pathways that ensure a coordinated antioxidant and pro-survival outcome: the Nrf2/ARE pathway and the PKD1 pathway.
Molecular Mechanisms of Parallel Response Pathways
Cells deploy a sophisticated network of sensors and transducers to convert redox signals into pro-survival outcomes. The following pathways operate in parallel to ensure a robust and coordinated defense.
The Nrf2-Keap1-ARE Pathway
The Nrf2 pathway is the primary regulator of cytoprotective gene expression.
- Mechanism: Under basal conditions, Nrf2 is sequestered in the cytoplasm by its inhibitor, Keap1 (Kelch-like ECH-associated protein 1), and targeted for constitutive ubiquitination and proteasomal degradation. Keap1 functions as a sensitive redox sensor via its highly reactive cysteine residues [79]. Under oxidative eustress, these cysteines are modified, leading to a conformational change in Keap1 that disrupts its ability to target Nrf2 for degradation.
- Stabilization and Translocation: Newly synthesized Nrf2 stabilizes and translocates into the nucleus.
- Gene Transactivation: In the nucleus, Nrf2 forms a heterodimer with small Maf proteins and binds to the Antioxidant Response Element (ARE) in the promoter regions of target genes [79] [80]. This transactivates a battery of genes involved in antioxidant defense and detoxification.
The PKD1-SIRT1-FOXO Pathway
The PKD1 pathway represents a crucial pro-survival signaling axis that is rapidly activated by oxidative stress.
- Mechanism: H₂O₂ and other oxidants can activate Protein Kinase D1 (PKD1) at the plasma membrane or in the cytoplasm.
- Nuclear Translocation and SIRT1 Activation: Upon activation, a fraction of PKD1 translocates to the nucleus. There, it phosphorylates and activates Sirtuin 1 (SIRT1), a NAD⁺-dependent deacetylase critical for cellular stress resistance and metabolism [80].
- FOXO Regulation: Activated SIRT1 deacetylates transcription factors of the FOXO family (e.g., FOXO3a), modulating their activity towards pro-survival and antioxidant gene expression, such as MnSOD, while suppressing pro-apoptotic targets [80]. This pathway integrates oxidative stress signaling with energy status (via NAD⁺) to promote cellular resilience.
The diagram below illustrates the coordinated interplay between these two parallel pathways in response to a mild oxidative stimulus.
Experimental Protocols for Pathway Analysis
A multi-faceted approach is required to empirically validate the activation and function of these parallel pathways. The following workflow provides a robust methodology.
Experimental Workflow for Hormesis Studies
The diagram below outlines a sequential protocol for treating cells, confirming ROS generation, and analyzing downstream pathway events.
Detailed Methodologies
3.2.1 Cell Culture and Hormetic Stimulation
- Cell Lines: Utilize relevant cell models such as primary fibroblasts, HepG2 (liver carcinoma), or neuronal cell lines.
- Stimuli Preparation: Prepare a stock solution of H₂O₂ in sterile buffer. Dilute to working concentrations (e.g., 50-200 µM) in pre-warmed culture media immediately before use. Alternatively, use pharmacological Nrf2 inducers like CDDO-Me (10-100 nM).
- Treatment Protocol: Culture cells to 70-80% confluence. Replace media with treatment media containing the hormetic stimulus or vehicle control. Incubate for a predetermined period (e.g., 1-2 hours) at 37°C, 5% CO₂. Terminate stimulation by removing the treatment media and washing cells with phosphate-buffered saline (PBS).
3.2.2 Quantitative ROS Measurement
- Protocol: Load cells with 10 µM H₂DCFDA in serum-free media for 30 minutes at 37°C. Wash cells with PBS to remove excess dye. Treat cells as described. Measure fluorescence intensity using a flow cytometer (excitation/emission: ~492-495/517-527 nm) or a fluorescence microplate reader at various time points post-stimulation. Express data as fold-change in fluorescence intensity relative to untreated controls.
3.2.3 Protein Analysis by Western Blot
- Cell Lysis: Lyse cells in RIPA buffer supplemented with protease and phosphatase inhibitors.
- Subcellular Fractionation: Use a commercial nuclear/cytosolic fractionation kit to separate cellular compartments. Confirm fraction purity by probing for markers like Lamin B1 (nuclear) and GAPDH (cytosolic).
- Immunoblotting: Resolve 20-40 µg of protein by SDS-PAGE and transfer to a PVDF membrane. Block membranes and probe with primary antibodies against Nrf2, PKD1, phospho-PKD1 (Ser744/748), SIRT1, Acetyl-FOXO, and FOXO. Use appropriate HRP-conjugated secondary antibodies and chemiluminescent detection. Normalize protein levels to loading controls (e.g., β-Actin, GAPDH).
3.2.4 Gene Expression Analysis by qRT-PCR
- RNA Isolation: Extract total RNA using a commercial kit, including a DNase I digestion step.
- cDNA Synthesis: Synthesize cDNA from 1 µg of RNA using a reverse transcription kit with oligo(dT) and/or random primers.
- Quantitative PCR: Perform qPCR using SYBR Green master mix and gene-specific primers for targets such as NQO1, HMOX1 (HO-1), GCLC, and SOD2. Calculate relative gene expression using the 2^(-ΔΔCt) method, normalizing to housekeeping genes like GAPDH or HPRT1.
Quantitative Data Analysis and Interpretation
The successful induction of a hormetic response is characterized by specific, quantifiable changes in molecular readouts and functional outcomes.
Pathway-Specific Molecular Signatures
Table 1: Expected quantitative changes in key molecular markers following a successful hormetic stimulus.
| Analyte | Assay | Basal Level | Post-Hormetic Stimulus (Expected Change) | Biological Significance |
|---|---|---|---|---|
| Cellular ROS | H₂DCFDA Fluorescence | 1.0 (relative units) | 1.5 - 3.0 fold increase (Transient, peaks at 15-30 min) | Confirms mild oxidative eustress trigger [16]. |
| Nuclear Nrf2 | Western Blot (Nuclear Fraction) | Low | 3 - 8 fold increase (Peaks at 2-4 h) | Indicates Nrf2 pathway activation and translocation [79]. |
| p-PKD1/PKD1 | Western Blot | Low | 2 - 5 fold increase (Peaks at 15-30 min) | Indicates rapid PKD1 pathway activation. |
| NQO1 mRNA | qRT-PCR | 1.0 (relative expression) | 5 - 20 fold increase (Peaks at 12-24 h) | Direct measure of Nrf2/ARE-dependent transcription [79]. |
| SOD2 mRNA | qRT-PCR | 1.0 (relative expression) | 3 - 10 fold increase (Peaks at 12-24 h) | Measure of FOXO-dependent pro-survival gene expression [80]. |
Functional Outcomes of Hormesis
Table 2: Measurable functional consequences of activating parallel response pathways.
| Functional Assay | Control Cells | Hormetically-Primed Cells | Interpretation |
|---|---|---|---|
| Cell Viability (MTT)After 24h culture | 100% | 100-110% | Hormesis does not compromise short-term viability. |
| Clonogenic SurvivalAfter 10-14 days | Baseline colonies | 120-150% of baseline | Indicates enhanced long-term proliferative capacity and fitness [17]. |
| Resistance to Lethal Oxidant Challengee.g., 500 µM - 1 mM H₂O₂ for 4h | Low survival (e.g., 20-40%) | High survival (e.g., 60-80%) | Demonstrates acquired resilience, the hallmark of hormetic preconditioning [16] [17]. |
| GSH/GSSG Ratio | Baseline (e.g., ~10:1) | Significantly elevated (e.g., >20:1) | Confirms enhanced antioxidant capacity via Nrf2-driven GSH synthesis [17]. |
The Scientist's Toolkit: Essential Research Reagents
A successful investigation into these pathways requires a carefully selected set of high-quality reagents and tools.
Table 3: Key research reagents and resources for studying parallel redox response pathways.
| Reagent / Resource | Specification / Example | Primary Function in Research |
|---|---|---|
| Anti-Nrf2 Antibody | Rabbit monoclonal, validated for WB/IF/ChIP | Detection of total Nrf2 protein levels and subcellular localization. |
| Anti-Phospho-PKD1 Antibody | Rabbit polyclonal, specific for Ser744/748 | Specific detection of the activated (phosphorylated) form of PKD1. |
| Anti-SIRT1 Antibody | Mouse monoclonal, validated for WB/IP | Detection of SIRT1 protein levels and analysis of interacting partners. |
| H₂DCFDA | Cell-permeant dye, >95% purity | Quantitative and qualitative measurement of intracellular ROS levels. |
| CDDO-Me (RTA 402) | Synthetic Triterpenoid, ≥98% | Potent pharmacological activator of the Nrf2 pathway; positive control. |
| SIRT1 Inhibitor (EX-527) | Selective, cell-permeant, ≥98% | Tool for probing the functional role of SIRT1 in the PKD1-SIRT1 axis. |
| Nuclear Extraction Kit | Commercial kit with protease inhibitors | Isolation of nuclear and cytosolic fractions for protein localization studies. |
| Human HEK293 or HepG2 Cells | ATCC CRL-1573 / HB-8065 | Well-characterized, transfertable cell lines suitable for redox signaling studies. |
The parallel and dual activation of the Nrf2/ARE and PKD1/SIRT1/FOXO pathways constitutes a fundamental mechanistic basis for the hormetic response in redox biology. This coordinated network ensures that a low-level oxidative stress signal is efficiently translated into a comprehensive protective program, enhancing antioxidant capacity and promoting pro-survival signaling. The experimental framework and quantitative benchmarks provided herein serve as a foundational guide for validating these mechanisms in various disease models. For drug development, targeting the upstream regulators of these pathways—rather than employing blunt antioxidant therapies—holds significant promise for inducing therapeutic hormesis in conditions ranging from neurodegenerative diseases to cancer.
The biphasic nature of the cellular response to reactive oxygen species (ROS), characterized by low-dose adaptive stimulation and high-dose inhibitory damage, represents a fundamental concept in redox biology known as hormesis. This in-depth technical guide examines the precise molecular mechanisms governing the transition from adaptive hormesis to oxidative distress, a critical threshold with profound implications for drug development and therapeutic interventions. We provide a detailed analysis of the quantitative parameters defining this transition, elaborate the key signaling pathways involved, and present standardized experimental methodologies for its investigation. Furthermore, we visualize critical pathway interactions and compile essential research reagents, offering scientists a comprehensive toolkit for navigating this crucial redox landscape in preclinical research and clinical application design.
The concept of hormesis describes an evolutionarily conserved dose-response phenomenon characterized by low-dose stimulation and high-dose inhibition [4] [81]. In redox biology, this translates to low levels of reactive oxygen species (ROS) activating adaptive, protective pathways that enhance cellular resilience, while supraphysiological ROS production overwhelms antioxidant defences and leads to oxidative distress—a damaging state implicated in aging, neurodegeneration, cardiovascular diseases, and cancer [17] [82]. The transition between these two states is not merely a quantitative increase in ROS, but a qualitative shift in cellular signaling resulting from the disruption of redox homeodynamics, the dynamic maintenance of redox balance [16]. Understanding this transition is paramount for developing therapeutic strategies that exploit hormesis for protection while avoiding the pitfalls of oxidative damage, particularly in the context of anticancer therapies where pro-oxidant approaches are being investigated [17].
Quantitative Boundaries: Defining the Transition Zone
The shift from adaptive hormesis to oxidative distress is governed by definable quantitative parameters. A comprehensive analysis of nearly 8,000 hormetic dose responses reveals that the stimulatory hormetic response is typically modest, with a maximum stimulation of 30-60% above control levels [83]. The width of this stimulatory zone is variable but generally spans less than a 100-fold dose range [83]. Beyond this zone, the system reaches a zero equivalent point or threshold, beyond which oxidative distress ensues [17] [83].
Table 1: Quantitative Parameters of the Hormetic Zone and Oxidative Distress
| Parameter | Hormetic Zone | Oxidative Distress Zone | Measurement Context |
|---|---|---|---|
| Response Magnitude | 130-160% of control response [83] | Significant inhibition (>20% below control) [17] | Varies by endpoint (e.g., growth, survival) |
| Dose Range Width | Typically <100-fold [83] | N/A | Dependent on biological model and stressor |
| Key Threshold | Zero Equivalent Point (dose where response crosses from stimulation to inhibition) [83] | Toxicological Threshold | Defined by experimental dose-response |
| GSH/GSSG Ratio | Maintained or transiently altered with rapid recovery [17] | Significantly decreased, sustained shift [17] | Major indicator of intracellular redox potential |
| ROS Level | Low, nanomolar H₂O₂ (stimulatory) [84] | High, micromolar to millimolar H₂O₂ (toxic) [84] | Varies by cell type and compartment |
The transition is also marked by a critical shift in the global intracellular redox potential, most reliably monitored by the ratio of oxidized to reduced glutathione (GSSG/GSH) [17]. In the hormetic zone, this ratio experiences transient, manageable fluctuations. In oxidative distress, the antioxidant systems are overwhelmed, leading to a sustained, detrimental shift in this ratio and causing damage to lipids, proteins, and DNA [17] [16].
Molecular Mechanisms of the Transition
Key Signaling Pathways and Their Role in Hormesis and Distress
The cellular decision between adaptation and distress is mediated by sophisticated molecular machinery that senses ROS levels and transduces the signal into a specific biological response.
The Nrf2/ARE Pathway
The transcription factor Nuclear factor erythroid 2-related factor 2 (Nrf2) serves as a master regulator of the antioxidant response. Under basal conditions, Nrf2 is sequestered in the cytoplasm by its inhibitor, Keap1, and targeted for degradation. Low levels of ROS or electrophiles modify specific cysteine residues on Keap1, inhibiting its function and allowing Nrf2 to translocate to the nucleus [85] [16]. There, it binds to the Antioxidant Response Element (ARE), initiating the transcription of a battery of cytoprotective genes, including those for glutathione synthesis, NADPH production, and ROS-detoxifying enzymes like heme oxygenase-1 (HO-1) [85] [82]. This constitutes a primary hormetic mechanism. However, during oxidative distress, this system can be overwhelmed or impaired, failing to mount an adequate protective response.
The NF-κB Pathway
The transcription factor NF-κB plays a dual role in the stress response. Low-level ROS can lead to its transient activation, contributing to cellular resilience and immune regulation [4]. In contrast, sustained and high levels of ROS lead to chronic NF-κB activation, driving the expression of pro-inflammatory cytokines (e.g., TNF-α, IL-6), which perpetuate a state of inflammation and tissue damage, characteristics of oxidative distress [17] [86].
Mitochondrial and Proteostatic Networks
Mitochondria are both a primary source and a target of ROS. Hormetic stimuli, such as mild metabolic stress or calorie restriction, induce a compensatory increase in mitochondrial efficiency and biogenesis, a process termed mitohormesis [85] [82]. This is accompanied by the upregulation of the protein quality control (PQC) system, including heat shock proteins (HSPs) and proteolytic systems like the 20S proteasome and Lon protease, which selectively remove oxidatively damaged proteins [84] [85]. When the oxidative challenge exceeds the capacity of these systems, damaged proteins accumulate, and mitochondrial dysfunction amplifies ROS production, creating a vicious cycle that propels the cell into oxidative distress [17] [84].
The following diagram illustrates the interplay between these critical pathways in determining the cellular fate in response to escalating ROS levels.
The Role of the Exposome and Redox Homeodynamics
The individual cellular response to oxidative challenges is not isolated but is significantly modulated by the exposome—the totality of environmental exposures throughout the lifespan [8] [16]. Factors such as diet, physical activity, and exposure to pollutants and other chemicals precondition the redox systems, altering the threshold for the transition to oxidative distress. This dynamic interplay necessitates a shift in perspective from static redox homeostasis to redox homeodynamics, which acknowledges the continuous, active maintenance of a fluctuating redox balance in response to a changing internal and external environment [16]. The failure of this adaptive, homeodynamic capacity is a hallmark of the transition to distress.
Experimental Protocols for Investigating the Transition
Robust experimental models are essential for delineating the boundaries of hormesis and oxidative distress. The following provides a detailed methodology for a classic preconditioning and challenge assay in mammalian cells, a cornerstone protocol in the field.
Preconditioning and Challenge Assay in Murine Embryonic Fibroblasts (MEFs)
This protocol assesses the ability of a mild oxidative pretreatment to induce adaptive hormesis, conferring protection against a subsequent, otherwise toxic, oxidative challenge [84].
Key Research Reagents:
- Cell Line: Murine Embryonic Fibroblasts (MEFs), CRL-2214 from ATCC.
- Culture Medium: Dulbecco’s Modified Eagle’s Medium (DMEM) supplemented with 10% fetal bovine serum (Complete Medium).
- Stressor Agent: Hydrogen Peroxide (H₂O₂), diluted to working concentrations in sterile buffer or medium.
- Viability/Growth Assay: Metrics such as cell counting, MTT assay, or crystal violet staining.
- Oxidative Damage Marker: Antibodies for specific protein carbonylation or lipid peroxidation (e.g., 4-HNE).
- Proteasome Activity Assay: Fluorogenic peptides (e.g., Suc-LLVY-AMC) for 20S proteasome chymotrypsin-like activity.
Detailed Procedure:
- Cell Culture and Seeding: Maintain MEFs in complete medium at 37°C under 5% CO₂. Seed cells at an appropriate density (e.g., 5x10^4 cells per well in a 24-well plate) and allow them to adhere for 24 hours.
- Preconditioning (Hormetic Stimulus): Treat cells with a mild, non-toxic dose of H₂O₂. The optimal concentration must be determined empirically; for MEFs, a final concentration of 1 µM H₂O₂ has been used effectively [84]. Incubate cells with the preconditioning dose for a defined period (e.g., 1 hour).
- Adaptation Period: Remove the H₂O₂-containing medium, wash cells with PBS, and add fresh complete medium. Allow cells to adapt for a critical period of 18-24 hours. This window is essential for the transcriptional and translational activation of defense mechanisms, including the synthesis of the 20S proteasome [84].
- Oxidative Challenge: After the adaptation period, expose both preconditioned and naive control cells to a high, toxic challenge dose of H₂O₂. For MEFs, a challenge of 1 mM H₂O₂ for 1 hour can be used to induce significant oxidative stress while minimizing immediate apoptosis [84].
- Post-Challenge Recovery and Analysis: Replace the challenge medium with fresh complete medium. Analyze endpoints at various time points post-challenge (e.g., immediately, 24h, 48h).
- Cell Viability/Growth: Quantify the protective effect of preconditioning by comparing viability/growth of preconditioned vs. non-preconditioned cells.
- Biomolecular Damage: Measure levels of protein oxidation (e.g., carbonylation) or lipid peroxidation.
- Protective Mechanism Analysis: Assess the activity and/or expression of antioxidant enzymes (e.g., via Western blot for HO-1, SOD2) and proteolytic capacity (e.g., proteasome activity assays).
Interpretation: Successful hormetic adaptation is demonstrated by a statistically significant increase in viability and a decrease in oxidative damage markers in preconditioned cells compared to non-preconditioned controls following the challenge dose.
The experimental workflow and the critical timing of the adaptation period are visualized below.
Investigating Repeated and Chronic Stress
It is critical to note that the adaptive hormetic response is transient. Research shows that repeated H₂O₂ exposures only allow for effective re-adaptation if sufficient recovery periods (increased beyond 24 hours) are provided between stresses. If the frequency of stress is too high, or the stress becomes chronic at even low doses, the adaptive capacity fails, and the response can shift toward toxicity and reduced longevity, as demonstrated in both mammalian cells and Drosophila melanogaster [84]. This underscores the importance of dose, timing, and recovery in the practical application of hormetic principles.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Studying Redox Hormesis and Oxidative Distress
| Reagent / Assay | Function & Application | Specific Examples |
|---|---|---|
| Hydrogen Peroxide (H₂O₂) | A stable, membrane-diffusible ROS used as a direct chemical stressor in preconditioning and challenge experiments [84]. | Diluted in buffer/culture medium; used at µM (hormesis) to mM (distress) ranges. |
| Menadione / Paraquat | Redox-cycling compounds that generate intracellular superoxide anions, used to model endogenous ROS stress. | Useful for investigating mitochondrial and enzymatic ROS sources. |
| N-Acetylcysteine (NAC) | A precursor to glutathione and a direct antioxidant. Used to modulate the cellular redox buffer capacity and test the specificity of ROS-mediated effects. | Thiol donor; can attenuate hormesis if scavenges essential signaling ROS. |
| siRNA/shRNA for Nrf2/Keap1 | Molecular tools for genetic knockdown to validate the functional role of the Nrf2-ARE pathway in the observed adaptive response. | Critical for mechanistic studies to establish causal relationships. |
| Antibody: Anti-HO-1 | Marker for Nrf2 pathway activation via Western blot or immunofluorescence. A classic inducible stress protein. | Quantifies the magnitude of the antioxidant gene response. |
| Antibody: Anti-Nitrotyrosine | Marker for protein nitration, a specific footprint of peroxynitrite formation and oxidative distress. | Distinguishes distress from eustress; indicates severe RNS/ROS damage. |
| GSH/GSSG Assay Kit | Quantifies the ratio of reduced to oxidized glutathione, the primary indicator of global intracellular redox state. | Essential for confirming a hormetic stimulus vs. a distressful insult. |
| Proteasome Activity Assay | Measures chymotrypsin-like, trypsin-like, and caspase-like activities of the 20S proteasome. | Evaluates the upregulation of proteolytic capacity as a hormetic mechanism [84]. |
| H2DCFDA / MitoSOX Red | Cell-permeable fluorogenic probes for detecting general cellular ROS and mitochondrial superoxide, respectively. | Provides real-time, albeit semi-quantitative, assessment of ROS levels. |
The precise boundary between adaptive hormesis and oxidative distress is a dynamic interface determined by the interplay of dose, time, genetic background, and the exposome. A deep understanding of the molecular mechanisms—centered on the Nrf2/ARE pathway, inflammatory regulation, and proteostatic networks—is crucial for exploiting hormesis therapeutically. Future research must focus on refining quantitative biomarkers to accurately map this transition in humans and developing technologies, such as controlled cold atmospheric plasma [8], to deliver precise hormetic stimuli. The challenge and opportunity for drug development lie in designing interventions that safely harness protective hormesis without inadvertently tipping the balance into the realm of oxidative distress, thereby unlocking novel strategies for preventing and treating a wide spectrum of age-related and degenerative diseases.
Experimental Design Considerations for Reliable Detection of Biphasic Dose-Responses
In redox biology, the biphasic dose-response, or hormesis, is a fundamental phenomenon where low doses of a stressor induce adaptive beneficial effects, while high doses cause inhibition or damage [87] [70]. This paradoxical response pattern is particularly relevant in the context of reactive oxygen species (ROS), where low levels function as signaling molecules activating protective pathways, and excessive levels cause oxidative distress [16]. The reliable detection of these responses is therefore not merely a methodological concern but essential for accurately interpreting biological mechanisms and developing therapeutic applications.
The concept of hormesis represents an evolutionarily conserved adaptive strategy where the response outcome exhibits a non-linear relationship with different doses of stimulation [87]. Under mild stress from low-dose stimuli, organisms can positively regulate physiological functions by inducing reconstruction of homeostasis, whereas high doses disrupt balance and compromise compensatory mechanisms [87]. In redox biology specifically, this manifests through precise spatiotemporal control of oxidant generation, predominantly H₂O₂, which serves as a second messenger triggering cell signals through reversible oxidation of protein cysteine residues [16]. Understanding the experimental parameters necessary to reliably capture this biphasic reality is crucial for advancing both basic science and therapeutic development.
Core Principles of Biphasic Response Experimental Design
Quantitative Characteristics of Hormetic Responses
The hormetic dose-response curve exhibits distinct quantitative features that must guide experimental design. The maximal stimulatory response typically ranges between 30% and 60% greater than the control baseline, with the stimulatory dose range usually spanning a 5- to 100-fold range below the threshold for toxicity [15] [70]. These consistent characteristics across biological models and stressors suggest evolutionary constraints on biological plasticity [70].
Table 1: Quantitative Features of the Biphasic Dose-Response
| Parameter | Typical Range | Biological Significance |
|---|---|---|
| Amplitude of Stimulation | 30-60% above control | Defines limits of biological plasticity [70] |
| Width of Stimulatory Zone | 5-100 fold (typically 5-10 fold) | Range of adaptive benefit [15] |
| Zero Equivalent Point | Point of no net effect | Transition between beneficial and harmful effects [87] |
| ED₅₀ | Dose for half-maximal inhibition | Standard measure of potency [88] |
Critical Design Elements for Reliable Detection
Several methodological considerations are paramount for accurately capturing biphasic responses. The historical neglect of hormesis can often be attributed to inadequate study designs that failed to accommodate these specific requirements [70].
Dose Selection and Spacing: Studies must include sufficient doses in the low-dose zone to characterize the hormetic region adequately. The capacity to detect hormesis is significantly affected by dose spacing in the low dose zone, with optimal designs incorporating 8-10 concentrations at minimum to ensure the hormetic peak isn't missed [70]. The dose range should extend from clearly sub-threshold to unequivocally toxic levels to capture the complete response spectrum.
Temporal Considerations: The hormetic response is kinetic, meaning the optimal window for observing stimulation may occur at different timepoints than inhibitory effects. Multiple sampling times are essential, as toxic doses may elicit responses on different time scales than hormetic doses [70]. Preconditioning responses, where a mild initial stress protects against subsequent challenges, have particularly distinct temporal parameters [12].
Replication and Statistical Power: The modest effect size of hormesis (typically 30-60% stimulation) necessitates sufficient replication to achieve statistical power for detecting these biologically significant but quantitatively modest responses [70]. Underpowered studies risk false negatives regarding hormetic effects.
Mathematical Modeling of Biphasic Responses
Appropriate Curve-Fitting Approaches
Proper statistical analysis of biphasic data requires specialized models beyond standard sigmoidal curves. The Brain-Cousens and Cedergreen models are established mathematical frameworks specifically designed for hormetic dose-response relationships [88]. These models modify standard log-logistic functions to accommodate the biphasic nature of the data.
The Brain-Cousens model incorporates a hormesis parameter (f) that should equal zero in the absence of hormesis, reverting the equation back to a standard sigmoidal function [88]. Similarly, the Cedergreen model includes an additional parameter (a) that controls the rate of hormetic increase prior to the peak [88]. For both models, a hormetic effect is statistically confirmed when the 95% confidence interval of the hormesis parameter does not overlap with zero [88].
Table 2: Key Parameters in Hormetic Modeling
| Parameter | Description | Interpretation |
|---|---|---|
| ED₅₀ | Effective dose that reduces response halfway between upper and lower asymptotes | Standard measure of potency [88] |
| b | Steepness of descending part of curve | Analogous to Hill coefficient [88] |
| f | Hormesis parameter | Confirms hormesis when CI doesn't include 0 [88] |
| M | Dose providing maximum stimulatory response | Optimal beneficial dose [88] |
| LDS | Limiting dose for stimulation | Highest dose where hormetic increase vanishes [88] |
| ymax% | Percent change between control and maximum response | Quantifies amplitude of hormesis [88] |
Area Under the Curve (AUC) Analysis for Biphasic Data
Standard AUC calculations require modification for biphasic responses. When the response of interest has a non-zero baseline with inherent variability, the AUC must be calculated relative to this variable baseline rather than assuming an absolute zero point [89]. Furthermore, biphasic responses often contain both positive (above baseline) and negative (below baseline) components that should be calculated separately to properly characterize multiphasic profiles [89]. This approach prevents cancellation of opposing effects and enables accurate quantification of net response magnitude.
Experimental Protocols for Redox Biology Applications
In Vitro Assessment of Oxidative Stress Modulation
The Brosimine B study provides an exemplary protocol for evaluating biphasic effects in a redox biology context [15]. This research investigated a flavonoid's effects on retinal cells under oxygen-glucose deprivation (OGD), simulating ischemic conditions.
Cell Culture and Treatment:
- Primary retinal cell cultures from 7-day-old chicken embryos maintained in DMEM with 10% FBS, 2 mM glutamine, and 2% penicillin-streptomycin [15]
- OGD induced by incubation in sealed chambers with low-glucose DMEM (5.5 mM) without FBS [15]
- Brosimine B tested across concentrations (1, 5, 10, 25, 50, 100 μM) to capture full dose-response range [15]
Endpoint Measurements:
- Cell viability assessed via MTT assay measuring formazan crystal formation at 570 nm [15]
- ROS production quantified using fluorescent probes (DCFH-DA)
- Antioxidant enzyme activities (catalase, SOD) measured spectrophotometrically
Computational Modeling:
- Data fitted to inverted U-shaped Gaussian function: Y = baseline + amplitude × e^[-(x-x₀)²/2σ²] [15]
- Parameters included peak response concentration (x₀) and hormetic zone width (σ)
This approach successfully identified significant neuroprotection at 10 μM Brosimine B with cytotoxic effects at higher concentrations, demonstrating a classic biphasic response mediated through modulation of oxidative stress pathways [15].
Signaling Pathway Analysis in Hormetic Mechanisms
Hormetic responses frequently involve activation of specific molecular pathways that can be experimentally measured:
NF-κB Pathway Activation:
- Assess nuclear translocation via immunofluorescence or subcellular fractionation
- Measure IκB phosphorylation and degradation via Western blot
- Monitor target gene expression (e.g., antioxidant enzymes) by qPCR
Nrf2-Keap1 Signaling:
- Evaluate Nrf2 nuclear accumulation under mild oxidative stress
- Measure ARE-driven gene expression (e.g., NADPH quinone oxidoreductase, heme oxygenase-1)
- Assess Keap1 cysteine modification under redox challenge
Sirtuin-FOXO Pathway:
- Monitor SIRT1 activity through deacetylation assays
- Measure FOXO transcription factor localization and DNA binding
- Quantify expression of FOXO target genes involved in stress resistance
Hormetic Signaling in Redox Biology
The Scientist's Toolkit: Essential Reagents and Methods
Table 3: Research Reagent Solutions for Biphasic Response Studies
| Reagent/Method | Function | Application Example |
|---|---|---|
| Oxygen-Glucose Deprivation (OGD) | Induces controlled oxidative stress | In vitro ischemia models [15] |
| MTT/Tetrazolium Assays | Measures cell viability/proliferation | Quantifying biphasic growth responses [15] |
| DCFH-DA Probe | Detects intracellular ROS | Monitoring redox changes in hormesis [16] |
| tert-Butyl Hydroperoxide (tBHP) | Chemical inducer of oxidative stress | Standardized oxidative challenge [90] |
| N-Acetylcysteine (NAC) | Thiol antioxidant, ROS scavenger | Mechanistic studies of redox signaling [16] |
| SIRT1 Activators/Inhibitors | Modulates sirtuin pathway | Testing hormesis mechanisms [12] |
| Phytochemical Hormetins | Natural product stressors | Resveratrol, sulforaphane, brosimine B [15] [91] |
Analytical Framework and Validation Approaches
Statistical Confirmation of Biphasic Patterns
Establishing a true hormetic response requires rigorous statistical validation beyond visual inspection of curve shapes. The hormesis parameter (f) in the Brain-Cousens model must demonstrate statistical significance with confidence intervals not overlapping zero [88]. Additionally, model selection criteria such as Akaike Information Criterion (AIC) should favor biphasic models over monotonic ones when appropriate.
Receiver Operating Characteristic (ROC) analysis combined with clinical trial simulation (CTS) offers a robust framework for optimizing dose titration of narrow therapeutic index compounds exhibiting biphasic responses [92]. This approach defines dosing algorithms that minimize toxicity while maximizing efficacy by leveraging exposure-response relationships [92].
Addressing Common Detection Challenges
Several factors complicate reliable detection of biphasic responses and require specific countermeasures:
Temporal Mismatch: The optimal timepoint for observing stimulation may differ from inhibition timing. Solution: Conduct comprehensive time-course experiments rather than single endpoint measurements [70].
Baseline Variability: Natural fluctuations in baseline measurements can obscure biphasic patterns. Solution: Implement variable baseline AUC calculations that account for this inherent variability [89].
Signal Cancellation: Multiphasic responses with opposing effects may cancel net measurements. Solution: Decompose responses into positive and negative AUC components for separate analysis [89].
Insufficient Resolution: Standard dose ranges may skip the hormetic zone entirely. Solution: Implement preliminary range-finding studies with dense sampling in low-dose regions before definitive experiments.
The reliable detection of biphasic dose-responses demands specialized experimental designs that account for their unique quantitative characteristics, temporal parameters, and statistical properties. In redox biology, where the fundamental role of hormesis in adaptive responses to oxidative stress is increasingly recognized, these methodological considerations become particularly critical. By implementing the appropriate mathematical models, analytical frameworks, and experimental protocols outlined in this guide, researchers can more accurately characterize these biologically fundamental response patterns and advance their applications in therapeutic development and toxicological risk assessment.
Validating Redox Hormesis: Comparative Analysis, Clinical Evidence, and Risk Assessment
For decades, risk assessment for ionizing radiation and chemical carcinogens has been dominated by the Linear No-Threshold (LNT) model, which assumes that even the smallest dose of a stressor increases cancer risk in a directly proportional manner [93] [94]. This model has formed the bedrock of regulatory policies worldwide, leading to the ALARA principle (As Low As Reasonably Achievable) in radiation protection [94] [95]. However, the LNT model is increasingly challenged by the concept of hormesis, a dose-response phenomenon characterized by low-dose stimulation and high-dose inhibition [4]. The core of this scientific debate centers on whether low doses of stressors activate beneficial biological responses that enhance an organism's defense mechanisms, a phenomenon with profound implications for redox biology research and its application to drug development and disease prevention [17] [4].
The LNT model's simplicity has made it attractive for regulatory purposes, but critics argue it oversimplifies biological complexity [93]. In contrast, hormesis represents a more nuanced, biphasic response that aligns with the ancient toxicological principle articulated by Paracelsus: "Sola dosis facit venenum" ("Only the dose makes the poison") [4]. This review examines the scientific evidence supporting hormesis, its molecular mechanisms within the framework of redox biology, and its potential to transform risk assessment paradigms.
Molecular Mechanisms of Hormesis in Redox Biology
Redox Homeostasis and Oxidative Stress
At the heart of hormetic mechanisms lies the concept of redox homeostasis, a critical balance between reactive oxygen species (ROS) generation and antioxidant defenses [17]. ROS, including superoxide anion (O₂•⁻), hydrogen peroxide (H₂O₂), and hydroxyl radical (HO•), are not merely toxic byproducts of metabolism but crucial signaling molecules at physiological levels [17]. The mitochondrial electron transport chain constitutes a primary source of ROS, with deliberate generation occurring through enzymes like NADPH oxidase (NOX) [17]. Supraphysiological ROS production leads to oxidative distress, causing damage to biomolecules and contributing to chronic diseases [17].
Cellular protection against ROS involves a sophisticated network of enzymatic antioxidants including superoxide dismutase (SOD), catalase (CAT), and peroxiredoxins (Prx) [17]. The tripeptide glutathione (GSH) plays a particularly pivotal role in ROS detoxification, with the GSH/GSSG ratio serving as a key indicator of intracellular redox potential [17]. The pentose phosphate pathway maintains adequate NADPH levels necessary for regenerating reduced glutathione, highlighting the integration of redox balance with core metabolic processes [17].
Signaling Pathways Mediating Hormetic Responses
Hormetic stimuli activate an intricate network of signaling pathways that orchestrate adaptive responses. These pathways stimulate the expression of cytoprotective proteins that enhance cellular resilience to subsequent stressors.
Diagram 1: Molecular Signaling Pathways in Hormesis. This diagram illustrates the key molecular events through which low-dose stressors activate cytoprotective signaling pathways, leading to enhanced cellular resilience. Central pathways include NRF2, NF-κB, and MAPK/AMPK/mTOR cascades that coordinate the expression of antioxidant and repair proteins.
The NRF2 pathway serves as a master regulator of the antioxidant response, inducing phase II detoxifying enzymes and proteins responsible for glutathione synthesis [4] [96]. Simultaneously, NF-κB activation regulates inflammatory responses, while MAPK pathways integrate stress signals to determine cell fate decisions [4]. The energy-sensing AMPK pathway and nutrient-responsive mTOR pathway further fine-tune the hormetic response based on cellular metabolic status [4]. These interconnected pathways collectively enhance cellular defense systems, improving resistance to subsequent, potentially damaging exposures.
Temporal Dynamics and Dose-Response Characteristics
Hormetic responses follow characteristic temporal patterns, with initial activation of stress responses followed by a protective phase that may last from hours to months [97]. This adaptive window allows organisms to maintain functional integrity despite ongoing environmental challenges. The quantitative features of hormesis include a stimulatory zone typically 30-60% above baseline response, with the stimulating dose range usually within 10- to 20-fold of the zero-equivalent point [4].
Comparative Analysis of LNT and Hormesis Models
Fundamental Principles and Historical Development
The LNT model originated from early genetic studies by Muller in 1927, who observed radiation-induced mutations and suggested there was "no threshold dose" [94] [98]. This concept gained regulatory traction in the 1950s through recommendations by the National Council on Radiation Protection and Measurements (NCRP) and the Federal Radiation Council [94]. The model's mathematical simplicity and perceived conservative approach led to its adoption for radiation protection standards, despite ongoing scientific debate about its applicability to low doses [94] [99].
In contrast, hormesis represents a more biologically grounded model recognizing the evolutionary conservation of adaptive stress responses across species [4]. The hormesis concept has gained substantial experimental support over recent decades, with databases now documenting over 9,000 hormetic dose responses across various biological models, stressors, and endpoints [4].
Table 1: Fundamental Characteristics of LNT vs. Hormesis Models
| Characteristic | Linear No-Threshold (LNT) Model | Hormesis Model |
|---|---|---|
| Dose-Response Shape | Linear at all doses | Biphasic: Low-dose stimulation, high-dose inhibition |
| Biological Principle | Damage proportional to energy absorbed | Adaptive overcompensation to mild stress |
| Threshold Concept | No threshold; risk exists at any dose | Distinct threshold between beneficial and harmful effects |
| Cellular Mechanism | Direct DNA damage with imperfect repair | Activation of defense signaling pathways & repair systems |
| Evolutionary Basis | Not considered | Evolutionarily conserved adaptive response |
| Regulatory Status | Widely adopted for radiation & chemical risk assessment | Emerging concept with limited regulatory acceptance |
Quantitative Risk Assessment Comparisons
Recent epidemiological studies and re-evaluations of historical data provide compelling quantitative comparisons between LNT and hormesis predictions. A 2025 study from Columbia University and Japan's Radiation Effects Research Foundation applied causal machine learning to the dataset of Japanese atomic bomb survivors, finding no statistically significant increase in mortality risk below 0.05 Gray (approximately 50 mSv) [93]. This threshold aligns with current U.S. occupational limits of 50 mSv per year and challenges the fundamental premise of LNT [93].
Table 2: Epidemiological Evidence Comparing LNT and Hormesis Predictions
| Study Population | LNT Model Prediction | Hormesis Model Observation | Significance |
|---|---|---|---|
| Japanese Atomic Bomb Survivors (2025 analysis) | Linear increase in cancer risk from lowest doses | No significant risk increase below 0.05 Gy [93] | Challenges LNT foundation using advanced statistical methods |
| Taiwanese Cobalt-60 Contaminated Buildings (1982-2002) | Increased cancer incidence from ~0.048 Gy average dose | Significantly reduced solid cancers (SIR: 0.7, 95% CI: 0.6-0.9) [100] | Demonstrates protective effect in large human population |
| Nuclear Workers Study (300,000 workers) | Predictable cancer risk based on cumulative dose | Lower than expected risk, suggesting adaptive protection [95] | Supports dose-rate effectiveness factor (DREF >1) |
| Radon Exposure Studies | Linear increase in lung cancer risk | Reduced lung cancer incidence at low doses in multiple studies [100] | Illustrates potential for non-linear risk assessment |
The Taiwan cobalt-60 contamination episode provides particularly compelling evidence for hormesis, where residents exposed to an average radiation dose of ~0.048 Gy showed a significantly reduced cancer incidence (Standardized Incidence Ratio of 0.7) compared to the general population [100]. This 30% reduction in expected cancers directly contradicts LNT predictions and demonstrates the potential public health implications of hormetic responses in real-world exposure scenarios.
Experimental Methodologies in Hormesis Research
Standardized Protocols for Hormesis Investigation
Research into hormetic mechanisms requires carefully designed experimental approaches that account for the biphasic nature of dose responses and the temporal dynamics of adaptive processes. The following workflow outlines a comprehensive approach for investigating hormesis in laboratory settings:
Diagram 2: Experimental Workflow for Hormesis Research. This diagram outlines a systematic approach for investigating hormetic responses, emphasizing the importance of dose selection, temporal design, and comprehensive molecular and functional assessments to validate biphasic dose-response relationships.
Critical to hormesis research is the inclusion of an adequate number of dose concentrations (typically 8-10) spanning the anticipated threshold region, with particular attention to doses below the traditional no-observed-adverse-effect level (NOAEL) [4]. The temporal component must include sufficient recovery periods between preconditioning and challenge doses to allow adaptive mechanisms to fully manifest.
Essential Research Tools and Reagents
Investigating hormetic mechanisms requires specialized reagents and methodologies for detecting subtle changes in stress response pathways. The following table summarizes key research solutions essential for rigorous hormesis research:
Table 3: Essential Research Reagents and Methodologies for Hormesis Investigation
| Research Tool Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| ROS Detection Probes | DCFH-DA, DHE, MitoSOX | Quantifying intracellular and mitochondrial ROS generation | Require careful calibration and control for auto-oxidation |
| Antioxidant Activity Assays | SOD activity kits, CAT assays, GSH/GSSG ratios | Measuring enzymatic and non-enzymatic antioxidant capacity | GSH/GSSG ratio is a key indicator of cellular redox state [17] |
| DNA Damage Markers | γH2AX foci, comet assay | Assessing DNA strand breaks and repair capacity | γH2AX is sensitive but not specific to double-strand breaks [97] |
| Pathway Activation Reporters | NRF2 translocation assays, NF-κB luciferase reporters | Tracking activation of key signaling pathways | Requires validation with multiple approaches |
| Cell Viability Assays | MTT, clonogenic assays, apoptosis markers | Determining functional consequences of exposures | Clonogenic assays are gold standard for radiation studies |
| Polyphenol Compounds | Resveratrol, curcumin, quercetin | Investigating hormetic phytochemical mechanisms | Exhibit biphasic effects on oxidative stress [96] |
| Omics Technologies | Transcriptomics, proteomics of stress pathways | Global assessment of adaptive responses | Essential for uncovering novel mechanisms |
Particular attention must be paid to polyphenol compounds like resveratrol, which have demonstrated hormetic properties through activation of NRF2 pathway and modulation of sirtuin activities [96]. These natural compounds provide valuable tools for exploring the therapeutic potential of hormetic mechanisms.
Implications for Drug Development and Therapeutic Strategies
The hormesis paradigm offers transformative approaches for pharmaceutical development, particularly in preventive medicine and age-related diseases. The concept of pharmaceutical hormesis suggests that low doses of otherwise toxic compounds can potentially induce beneficial adaptive responses [4]. This approach is particularly relevant for neurodegenerative disorders like Alzheimer's and Parkinson's diseases, where preconditioning with mild stressors may enhance neuronal resilience to subsequent pathological insults [4].
In oncology, hormesis principles are informing novel strategies for combining conventional therapies with hormetic conditioning. Low-dose radiation or chemotherapeutic agents may potentially prime normal tissues—though not tumor cells—to better withstand full-dose therapeutic regimens, thereby reducing side effects and improving treatment tolerance [17] [97]. However, this approach requires careful validation to ensure cancer cells do not similarly benefit from protective responses.
The field of biogerontology has particularly embraced hormetic concepts, with interventions like caloric restriction and phytonutrient supplementation demonstrating lifespan-extending effects through activation of stress response pathways [4]. These approaches work through mitohormesis—the concept that mild mitochondrial stress activates compensatory mechanisms that improve cellular function and longevity.
Regulatory Considerations and Future Research Directions
The transition from LNT to hormesis-based risk assessment faces significant challenges, including regulatory inertia, methodological complexities, and the need for consensus standards for identifying and quantifying hormetic responses [99] [97]. However, the accumulating evidence against LNT is becoming increasingly difficult to disregard. As noted in recent analyses, the LNT model "may have created an irrational fear of radiation" [94], leading to substantial societal costs from excessive regulation and public anxiety.
Future research should prioritize:
- Prospective human studies specifically designed to detect hormetic responses [100]
- Dose-rate effectiveness factor quantification across multiple stressor types [95]
- Personalized hormesis approaches accounting for genetic and environmental factors influencing individual susceptibility
- Integrated LNT-Hormesis models that more accurately reflect biological reality across dose ranges [97]
The recent executive order proposing "determinate radiation limits" to replace LNT and ALARA principles signals a potential regulatory shift acknowledging the limitations of current risk assessment models [94]. For drug development professionals, understanding hormesis mechanisms creates opportunities for developing novel preconditioning therapies and combination treatments that harness innate protective mechanisms rather than merely inhibiting pathological processes.
The accumulating evidence from radiation biology, toxicology, and redox research strongly supports hormesis as a biologically valid alternative to the LNT model. The biphasic dose-response relationship observed across numerous stressors and biological endpoints reflects evolutionarily conserved mechanisms for maintaining homeostasis in fluctuating environments. For researchers and drug development professionals, incorporating hormesis principles offers exciting possibilities for developing more effective therapeutic strategies that work with, rather than against, the body's innate adaptive capacities. While regulatory paradigms evolve slowly, the scientific case for a hormesis-informed approach to risk assessment and therapeutic development continues to strengthen, promising to transform both environmental regulation and clinical practice in the coming decades.
This whitepaper examines two significant paradoxical phenomena in biomedical research: radiation hormesis and the obesity paradox. The radiation hormesis concept demonstrates that low-dose radiation exposure can induce stimulatory or protective effects, contrary to the detrimental impacts observed at high doses. Simultaneously, the obesity paradox presents the counterintuitive finding that elevated body mass index may correlate with improved survival outcomes in specific chronic disease populations. This analysis frames both phenomena within the context of redox biology and hormetic mechanisms, exploring the potential shared pathways through which mild stressors activate adaptive responses that confer subsequent protection. The synthesis of epidemiological evidence with molecular mechanisms provides insights for therapeutic development and clinical practice, particularly for researchers and drug development professionals working in metabolic disorders, cardiology, and oncology.
Historical Context and Definitions
The conceptual foundation of hormesis was established in the 16th century by Paracelsus, who recognized that "all things are poison, and nothing is without poison, only the dose permits something not to be poisonous" [4]. This fundamental insight anticipates the modern understanding of biphasic dose-response relationships observed across various biological systems. The term "hormesis" describes an adaptive response where exposure to low doses of a stressor induces stimulatory effects, while higher doses produce inhibitory or toxic outcomes [4]. This phenomenon exhibits universal applicability across physical stressors (temperature, ionizing radiation), chemical stressors (reactive oxygen species, herbicides), and biological stressors, affecting responses at cellular, organ, individual, and population levels [4].
The obesity paradox represents another counterintuitive phenomenon in clinical epidemiology. Contrary to established knowledge that obesity functions as a risk factor for numerous diseases, the paradox reveals that obese patients may demonstrate better mortality rates, improved morbidity profiles, and enhanced survival outcomes compared to non-obese populations with similar medical conditions [101]. This phenomenon has been observed most prominently in cardiovascular diseases but is increasingly documented in critically ill patients, those with chronic kidney disease, and certain cancer populations [101].
Purpose and Scope
This technical analysis synthesizes epidemiological evidence for both radiation hormesis and the obesity paradox within a unified conceptual framework centered on redox biology mechanisms. We examine the shared characteristics between these phenomena, including their non-linear response patterns, activation of adaptive pathways, and potential implications for therapeutic interventions. By integrating evidence across these seemingly disparate fields, we aim to identify common biological principles that may inform future research directions and clinical applications for drug development professionals and translational researchers.
Theoretical Foundations: Hormesis Mechanism in Redox Biology
Redox Homeostasis and Signaling
The maintenance of redox homeostasis represents a critical physiological process for healthy cellular function. This state preserves nucleophilic tone through continuous signaling for the production and elimination of electrophiles and nucleophiles [75]. Within this framework, both oxidant and antioxidant signaling constitute essential features of redox homeostasis, maintained through feedback reactions that rapidly reverse redox shifts [75].
Reactive oxygen species (ROS), including superoxide anion (O₂•⁻), hydrogen peroxide (H₂O₂), and hydroxyl radical (HO•), function as crucial signaling molecules at physiological levels [17]. Mitochondrial respiration contributes significantly to ROS generation, with a proportion of oxygen in the respiratory chain partially reduced to O₂•⁻ [17]. Additionally, specialized enzymes including NADPH oxidase (NOX) isoforms deliberately produce ROS to regulate diverse cellular functions, including cell survival, migration, differentiation, and synaptic plasticity [17].
Table 1: Major Reactive Oxygen Species and Their Sources
| ROS Type | Chemical Formula | Primary Sources | Biological Significance |
|---|---|---|---|
| Superoxide anion | O₂•⁻ | Mitochondrial electron transport chain, NOX enzymes | Signaling molecule, precursor to other ROS |
| Hydrogen peroxide | H₂O₂ | SOD enzyme activity, NOX enzymes | Key signaling molecule, diffusible |
| Hydroxyl radical | HO• | Fenton reaction, water radiolysis | Highly reactive, damages biomolecules |
| Nitric oxide | NO• | Nitric oxide synthases | Vasodilation, neurotransmission |
Molecular Mechanisms of Hormetic Adaptation
Hormesis functions through the activation of complex signaling networks that cannot be reduced to a single biological theory. The preliminary patterns that have emerged reveal that hormetic responses are mediated through several conserved pathways:
- Transcription Factor Activation: Nuclear factor kappa-B (NF-κB), Nuclear factor erythroid 2-related factor 2 (NRF2), and p53 pathways [17] [4]
- Kinase Signaling: Mitogen-activated protein kinase (MAPK), AMP-activated protein kinase (AMPK), and phosphatidylinositide 3-kinases/protein kinase B (PI3K/Akt) cascades [4]
- Cytoprotective Protein Upregulation: Phase 2 enzymes, antioxidant enzymes, heat-shock proteins, and growth factors [4]
These pathways collectively diminish oxidative stress and inflammation levels, mitigate cellular senescence, and influence aging phenotypes [4]. This process enables tissue repair, restoration of cellular homeostasis, and enhancement of the organism's defense capabilities and adaptability.
Diagram 1: Hormetic Biphasic Response Pathway
Radiation Hormesis: Evidence and Mechanisms
Epidemiological Evidence
Radiation hormesis has been documented across various epidemiological studies, demonstrating consistent patterns of reduced disease incidence or improved survival following low-dose radiation exposure. Key evidence includes:
- Nuclear Worker Studies: Research on radiation workers consistently shows lower cancer mortality rates compared to control populations, with some studies reporting 10-30% reduction in solid cancer mortality [4].
- High Background Radiation Areas: Populations in regions with naturally elevated radiation levels (Yangjiang, China; Kerala, India) exhibit reduced cancer incidence and longer lifespans compared to control regions [4].
- Radon Exposure Studies: Residential radon studies have demonstrated an unexpected inverse relationship between low-level radon exposure and lung cancer risk in certain populations [4].
The quantitative characteristics of radiation hormesis include a typical stimulatory magnitude of 30-60% response enhancement, with a stimulatory width generally ranging 10-20-fold in dose range below the zero-equivalent point [4].
Table 2: Epidemiological Evidence for Radiation Hormesis
| Study Type | Population | Observed Effects | Magnitude | References |
|---|---|---|---|---|
| Nuclear workers | Occupational cohorts | Reduced cancer mortality | 10-30% reduction | [4] |
| High background areas | General populations in high-radiation regions | Decreased cancer incidence, increased longevity | 15-40% risk reduction | [4] |
| Medical imaging | Patients with low-dose diagnostic exposure | Reduced subsequent cancer risk | Non-significant risk reduction | [4] |
| Radon exposure | Residential populations | Inverse association with lung cancer at low doses | 10-15% risk reduction | [4] |
Redox Mechanisms in Radiation Hormesis
The protective effects of low-dose radiation are mediated through redox-sensitive pathways that enhance cellular defense systems:
- Antioxidant System Activation: Low-dose radiation upregulates superoxide dismutase (SOD), catalase (CAT), and glutathione peroxidase (GPX) activities, enhancing cellular capacity to manage oxidative stress [17].
- DNA Repair Enhancement: Activation of base excision repair and nucleotide excision repair pathways improves genomic stability and reduces mutation accumulation [4].
- Immune System Stimulation: Low-dose radiation modulates immune function through NF-κB activation, leading to enhanced surveillance and elimination of transformed cells [4].
- Detoxification Enzyme Induction: Phase 2 enzymes such as NAD(P)H quinone dehydrogenase 1 (NQO1) and glutathione S-transferases (GSTs) are induced, enhancing cellular capacity to neutralize electrophilic toxins [17].
These mechanisms collectively contribute to the observed protective effects against subsequent higher-dose exposures through a phenomenon known as radioadaptation.
The Obesity Paradox: Clinical Evidence and Potential Explanations
Epidemiological Patterns Across Disease States
The obesity paradox challenges conventional medical understanding by demonstrating associations between increased body mass index (BMI) and improved survival across various pathological conditions:
- Cardiovascular Disease: In heart failure populations, overweight and obese patients (BMI 25-35 kg/m²) show 16-30% lower mortality compared to normal-weight patients [101].
- Chronic Kidney Disease: Among end-stage renal disease patients undergoing dialysis, obesity correlates with 20-25% improved survival [101].
- Critical Illness: In intensive care units, obese patients frequently demonstrate lower mortality rates despite longer ventilator dependence and hospital stays [101].
- Cancer: Select malignancies demonstrate paradoxical associations where overweight status correlates with improved treatment response and extended survival [101].
The reliance on BMI as the primary obesity metric complicates interpretation, as it fails to distinguish between lean mass and adipose tissue distribution, potentially confounding the observed relationships [101].
Table 3: Obesity Paradox Evidence Across Medical Conditions
| Medical Condition | Population Characteristics | Observed Survival Benefit | Potential Explanations |
|---|---|---|---|
| Chronic Heart Failure | Overweight (BMI 25-29.9) vs. normal weight | 16-30% lower mortality | Metabolic reserves, neurohormonal modulation |
| End-stage Renal Disease | Obese (BMI >30) on dialysis | 20-25% improved survival | Nutritional status, inflammatory modulation |
| Acute Coronary Syndromes | Overweight and obese patients | 15-20% lower in-hospital mortality | Earlier presentation, cardioprotective adipokines |
| Critical Illness | Obese ICU patients | 10-15% lower mortality | Metabolic reserve, inflammatory adaptation |
Potential Mechanistic Explanations
Several hypotheses have been proposed to explain the obesity paradox, many intersecting with redox biology principles:
- Metabolic Reserve Hypothesis: Adipose tissue provides energy reserves during catabolic states, preventing cachexia and supporting recovery [101].
- Endotoxin Buffering: Adipose tissue may sequester lipophilic toxins and inflammatory mediators, reducing their systemic impact [101] [75].
- Hormetic Adipokine Signaling: Adipose tissue secretes cardioprotective cytokines that may induce adaptive responses through mild inflammatory signaling [101].
- Renin-Angiotensin System Modulation: Expanded plasma volume in obesity may maintain perfusion pressure while reducing maladaptive neurohormonal activation [101].
The timing hypothesis suggests that obesity may offer protective metabolic reserves in established disease while remaining detrimental in primary disease prevention [101].
Convergent Mechanisms: Integrating Both Phenomena
Shared Redox Signaling Pathways
Radiation hormesis and the obesity paradox share common mechanistic features within redox biology frameworks:
- Mitochondrial Signaling: Both phenomena involve mitochondrial ROS production that activates cytoprotective pathways at low levels but causes damage at higher levels [17] [4].
- NRF2-KEAP1 Pathway Activation: Low-dose radiation and metabolic stressors both activate the NRF2 antioxidant response pathway, enhancing expression of antioxidant genes and detoxification enzymes [17] [75].
- Inflammatory Priming: Mild oxidative stress from either radiation or adipose-derived cytokines can induce a preconditioning effect that enhances resistance to subsequent insults [4] [75].
- Autophagy Regulation: Both low-dose radiation and metabolic stress modulate autophagic flux, clearing damaged cellular components and maintaining functional homeostasis [4].
Non-Linear Response Patterns
Both phenomena exhibit characteristic biphasic dose-response relationships consistent with hormetic principles:
- Dose-Response Curve: The typical hormetic curve shows low-dose stimulation and high-dose inhibition, with a maximum stimulatory response typically 30-60% above baseline [4].
- Temporal Dynamics: The adaptive responses in both phenomena require time for gene expression and protein synthesis, typically exhibiting a delayed onset of several hours [4].
- Threshold Variability: Individual thresholds for protective versus detrimental effects vary based on genetic background, age, comorbidities, and environmental factors [101] [4].
Diagram 2: Convergent Redox Signaling Pathways
Experimental Approaches and Methodologies
Research Design Considerations
Studying hormetic phenomena requires specific methodological approaches to account for their non-linear nature:
- Dose-Response Characterization: Studies must include multiple dose levels across a broad range to adequately capture biphasic responses, with particular attention to low-dose regions often neglected in traditional toxicology [4].
- Temporal Dynamics: Experimental designs should incorporate multiple time points to account for the delayed onset of adaptive responses and potential transient effects [4].
- Stressor Interactions: Investigations should consider real-world exposure scenarios involving multiple simultaneous stressors that may interact to modulate hormetic thresholds [4].
Specific Methodological Protocols
Radiation Hormesis Experimental Protocol
Objective: To evaluate the hormetic response to low-dose radiation exposure and its underlying redox mechanisms.
Materials and Methods:
- Cell Culture: Primary human fibroblasts or appropriate cell lines cultured under standard conditions
- Radiation Source: calibrated X-ray or gamma-ray source capable of delivering precise low doses (0.01-0.5 Gy)
- Assessment Endpoints:
- ROS production measured by fluorescent probes (DCFH-DA, MitoSOX)
- Antioxidant enzyme activities (SOD, CAT, GPX) via spectrophotometric assays
- Glutathione status (GSH/GSSG ratio) using HPLC or enzymatic recycling assay
- DNA damage markers (γ-H2AX foci, comet assay)
- Gene expression (NRF2 targets, DNA repair genes) via qRT-PCR
- Protein analysis (NRF2, NF-κB, MAPK pathways) via western blotting
Procedure:
- Expose cells to radiation doses ranging from 0.01 Gy to 2.0 Gy
- Collect samples at multiple time points (1h, 6h, 24h, 48h) post-exposure
- Assess immediate oxidative stress markers and delayed adaptive responses
- Challenge cells with high-dose radiation (2-4 Gy) 24h after priming dose to assess adaptive protection
- Include appropriate controls (sham irradiation, antioxidant pretreatment, pathway inhibitors)
Obesity Paradox Clinical Study Protocol
Objective: To examine the relationship between adiposity, oxidative stress parameters, and clinical outcomes in chronic disease populations.
Study Design: Prospective cohort study with matched analysis
Participant Selection:
- Inclusion: Patients with established chronic disease (heart failure, CKD, or selected cancers)
- Stratification: By BMI categories (underweight <18.5, normal 18.5-24.9, overweight 25-29.9, obese ≥30 kg/m²)
- Covariate assessment: Body composition (DEXA or BIA), comorbidities, medications, socioeconomic factors
Laboratory Assessments:
- Redox status markers: plasma GSH/GSSG ratio, lipid peroxidation products (MDA, 4-HNE), protein carbonyls
- Inflammatory markers: hs-CRP, IL-6, TNF-α, adiponectin, leptin
- Metabolic parameters: lipid profile, insulin, glucose, HOMA-IR
- Oxidative stress resistance: ex vivo lymphocyte challenge with H₂O₂
Statistical Analysis:
- Multivariable Cox proportional hazards models for survival analysis
- Mediation analysis to examine pathways linking adiposity to outcomes
- Threshold determination using restricted cubic splines
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Hormesis and Redox Biology Studies
| Reagent/Category | Specific Examples | Research Application | Key Functions |
|---|---|---|---|
| ROS Detection Probes | DCFH-DA, MitoSOX Red, DHE | Quantifying intracellular and mitochondrial ROS levels | Oxidation yields fluorescent signals proportional to ROS production |
| Antioxidant Enzyme Assays | SOD activity kits, Catalase activity assays, GPX kits | Measuring antioxidant capacity in cell/tissue extracts | Spectrophotometric measurement of enzyme-specific activities |
| Thiol Status Assessment | DTNB (Ellman's reagent), Monochlorobimane | Quantifying glutathione and protein thiol status | Colorimetric or fluorescent detection of reduced thiol groups |
| Pathway Inhibitors/Activators | NRF2 inducers (sulforaphane), NOX inhibitors (apocynin) | Manipulating specific redox signaling pathways | Experimental modulation to establish mechanistic relationships |
| Oxidized Biomarker Assays | MDA/TBARS assays, protein carbonyl kits, 8-OHdG ELISA | Assessing oxidative damage to lipids, proteins, DNA | Quantification of specific oxidation products as damage markers |
| Molecular Biology Tools | NRF2 siRNA, antioxidant response element (ARE) reporters | Genetic manipulation of redox pathways | Establishing causal relationships in signaling mechanisms |
Research Gaps and Future Directions
Despite substantial progress in understanding both radiation hormesis and the obesity paradox, significant knowledge gaps remain:
- Molecular Connecting Pathways: Limited understanding exists regarding the precise molecular mechanisms connecting adipose tissue signaling to radioprotective effects [101] [4].
- Individual Variability Factors: The genetic, epigenetic, and environmental factors determining individual susceptibility to hormetic responses require further characterization [101].
- Optimal Dosing Parameters: The precise dose ranges, timing, and fractionation schemes for maximizing adaptive protection remain inadequately defined [4].
- Translational Applications: Strategies for safely harnessing hormetic principles in clinical practice and public health need careful development and validation [4].
Future research should prioritize integrated approaches that combine epidemiological observations with mechanistic laboratory studies, utilizing advanced technologies in redox proteomics, metabolomics, and systems biology to comprehensively map the networks underlying these adaptive phenomena.
Hormesis, the biphasic dose-response phenomenon characterized by low-dose stimulation and high-dose inhibition, provides a fundamental framework for understanding how mild stressors enhance systemic resilience. This whitepaper synthesizes current evidence on the efficacy of three principal hormetin categories—phytochemicals, physical stressors, and nutritional interventions—within redox biology research. We examine comparative molecular mechanisms, quantitative dose-response parameters, and experimental methodologies, highlighting the central role of the Nrf2/ARE pathway, sirtuin activation, and mitochondrial adaptive signaling (mitohormesis). The analysis reveals that while all hormetins share common signaling architectures, their temporal dynamics, efficacy magnitudes, and applications in preconditioning strategies differ significantly. Integrated understanding of these profiles provides a rational basis for designing targeted interventions in drug development and therapeutic applications.
Hormesis represents an evolutionarily conserved adaptive response where exposure to low doses of stressors induces beneficial effects, while higher doses become inhibitory or toxic [4] [81]. This phenomenon follows a characteristic biphasic dose-response curve, typically exhibiting a stimulatory response at low doses (approximately 30-60% above baseline) with a stimulatory zone width of approximately 5-10 fold [69]. The biological foundation of hormesis lies in its ability to activate preconditioning mechanisms that enhance cellular resilience to subsequent, more severe stressors [81].
In redox biology, hormetic responses are primarily mediated through the modulation of reactive oxygen species (ROS) and the subsequent activation of cytoprotective pathways [16]. Low-level oxidative stress triggers adaptive responses through the "redox code," a set of organizational principles governing biological redox reactions [16]. This code coordinates bioenergetics through NADH/NADPH systems, utilizes sulfur-based redox switches in proteins, and establishes spatiotemporal response networks that enable adaptive communication across cellular compartments [16]. The concept of redox homeodynamics more accurately describes this dynamic steady state than classical homeostasis, emphasizing the continuous flux and adaptive recalibration of redox systems in response to hormetic stimuli [16].
Molecular Mechanisms of Hormetic Signaling
Central Signaling Pathways
Hormetins converge on a limited set of highly conserved signaling pathways that regulate cellular stress resistance, antioxidant defense, and metabolic adaptation:
Nrf2/ARE Pathway: The primary regulator of antioxidant gene expression. Under basal conditions, Nrf2 is sequestered in the cytoplasm by its inhibitor Keap1. Electrophilic compounds or ROS promote Nrf2 dissociation, nuclear translocation, and binding to Antioxidant Response Elements (ARE), driving expression of over 500 cytoprotective genes including glutathione peroxidase, superoxide dismutase, and NADPH quinone oxidoreductase 1 [13] [102] [16].
Sirtuin-FOXO Pathway: Sirtuins (particularly SIRT1), NAD+-dependent deacetylases, are activated by energy stressors and phytochemicals like resveratrol. They deacetylate transcription factors including FOXOs, PGC-1α, and p53, enhancing stress resistance, mitochondrial biogenesis, and metabolic efficiency [103] [13].
Mitohormesis: Low-level mitochondrial stress activates compensatory mechanisms that enhance mitochondrial function and cellular resilience. This involves AMPK activation, PGC-1α-mediated mitochondrial biogenesis, and increased expression of mitochondrial chaperones and antioxidant enzymes [13].
The following diagram illustrates the integrated cellular response to hormetic stimuli through these key pathways:
Vitagene Regulation
A critical mechanism in hormesis involves the upregulation of vitagenes, a group of genes involved in cellular stress resistance [103]. Key vitagenes include:
- Heme oxygenase-1 (HO-1): Activated by hidrox and curcumin, provides potent antioxidant and anti-inflammatory effects [103]
- Heat shock protein 70 (Hsp70): Molecular chaperone that prevents protein misfolding and aggregation [103]
- Thioredoxin/Thioredoxin reductase system: Maintains redox balance through dithiol-disulfide exchange mechanisms [103]
- Sirtuin-1: Activated by resveratrol, links energy status to stress resistance and mitochondrial function [103]
These vitagenes operate within an integrated network, with low-dose stressors activating the Nrf2 pathway resulting in their coordinated upregulation, ultimately inhibiting reactive oxygen species (ROS) overproduction and enhancing cellular resilience [103].
Comparative Efficacy of Hormetin Categories
Quantitative Dose-Response Characteristics
The efficacy of hormetins varies significantly across categories, with distinct dose-response parameters, magnitude of effects, and temporal dynamics. The table below summarizes these quantitative characteristics based on current experimental evidence:
| Hormetin Category | Specific Examples | Optimal Dose Range | Maximal Stimulation | Hormetic Zone Width | Key Molecular Targets |
|---|---|---|---|---|---|
| Dietary Phytochemicals | Resveratrol [103] [13] | 1-10 μM | 25-40% above baseline | 5-15 fold | Sirtuin-1, Nrf2, AMPK |
| Sulforaphane [13] [102] | 2-15 μM | 30-50% above baseline | 3-10 fold | Nrf2/ARE, HDAC inhibition | |
| Curcumin [103] [81] | 5-20 μM | 20-35% above baseline | 5-8 fold | Nrf2, NF-κB inhibition | |
| Brosimine B [15] | ~10 μM | ~30% above baseline | σ=6.5 μM | Nrf2/ARE, antioxidant enzymes | |
| EGCG [102] | 10-25 μM | 25-45% above baseline | 5-12 fold | Nrf2, DNA methyltransferase inhibition | |
| Physical Stressors | Moderate Exercise [60] | 60-75% VO₂max | 15-30% above baseline | 3-6 fold | AMPK, PGC-1α, BDNF |
| Hyperthermia [81] | 38-40°C | 20-40% above baseline | 2-4°C range | HSP70, HSF1, Nrf2 | |
| Intermittent Hypoxia [81] | 10-15% O₂ | 10-25% above baseline | 2-5 fold | HIF-1α, EPO, antioxidant enzymes | |
| Nutritional Interventions | Caloric Restriction [13] [102] | 20-40% reduction | 25-60% above baseline | 15-30% range | Sirtuins, AMPK, mTOR inhibition |
| Intermittent Fasting [81] | 16-20 hour fasts | 20-40% above baseline | 12-24 hour window | Ketosis, Nrf2, autophagy | |
| Probiotics [103] | 10⁹-10¹¹ CFU | 15-35% above baseline | 10-100 fold | Nrf2, BDNF, tight junctions |
Efficacy in Disease Models
The therapeutic potential of hormetins is demonstrated across various disease models:
Neurodegenerative Disorders: Polyphenols and probiotics in synergy improve gut bioavailability and blood-brain barrier permeability, inhibiting oxidative stress and neuroinflammation linked to Alzheimer's and Parkinson's diseases [103]. Hormetic nutrients suppress oxidative stress, inflammation, and microbiota deregulation, consequently improving cognitive performance [103].
Metabolic Diseases: Capsaicin activates transient receptor potential (TRP) channels, leading to increased thermogenesis, improved mitochondrial function, and enhanced insulin sensitivity, reducing risks of obesity and type 2 diabetes [13].
Retinal Disorders: Brosimine B at 10 μM significantly enhances cell viability and reduces ROS production in retinal ischemia models, while higher concentrations (>10 μM) induce cytotoxic effects [15].
Experimental Protocols and Methodologies
Standardized Hormesis Assay Protocol
Based on analysis of published methodologies, the following protocol provides a robust framework for evaluating hormetic responses:
Cell Culture Preparation
- Utilize appropriate cell lines (e.g., primary retinal cells [15], neuronal cultures, or established lines like SH-SY5Y or HEK293)
- Culture in standard conditions (DMEM with 10% FBS, 2 mM glutamine, penicillin/streptomycin)
- Seed cells at optimal density (e.g., 10⁴ cells/well for 96-well plates [69])
Hormetin Treatment
- Prepare serial dilutions covering 3-5 logarithmic units (e.g., 1 μM to 100 μM for phytochemicals)
- Include vehicle controls (typically DMSO ≤0.1%)
- Implement exposure times from 2-48 hours based on compound kinetics
Stress Challenge Models
- Oxygen-Glucose Deprivation (OGD): Incubate cells in sealed chambers with glucose-free medium for 3-24 hours [15]
- Chemical Oxidants: Apply H₂O₂ (50-500 μM) or tert-butyl hydroperoxide
- Inflammatory Stress: Use lipopolysaccharide (LPS, 100 ng/mL) or TNF-α (10-50 ng/mL)
Viability and Function Assessment
- MTT Assay: Incubate with 0.5 mg/mL MTT for 3 hours, solubilize with DMSO, read at 570 nm [15]
- ROS Measurement: Utilize DCFDA or dihydroethidium staining with flow cytometry or fluorimetry
- Antioxidant Enzymes: Assess catalase, SOD, and GPx activity via commercial kits
- Molecular Analyses: Western blotting for Nrf2, sirtuins, HO-1; qPCR for vitagenes
Data Analysis
- Fit data to biphasic models (e.g., inverted U-shaped Gaussian function: Y = baseline + amplitude · e^[-(x-x₀)²/2σ²]) [15]
- Calculate ZEP (Zero Equivalent Point), maximum stimulation, and hormetic zone width
- Determine statistical significance using ANOVA with post-hoc tests (n≥3)
The experimental workflow for assessing hormetic responses typically follows this structure:
Advanced Methodological Considerations
High-Content Screening for Hormesis
- Automated microscopy platforms enable multi-parameter analysis of sublethal endpoints including mitochondrial membrane potential, nuclear translocation of transcription factors (Nrf2), and reactive oxygen species flux [69]
- Yeast-based screening platforms (e.g., NCI Yeast Anticancer Drug Screen) allow rapid assessment of 2,189+ compounds across 13 genetically distinct strains, identifying ~52.5% with hormetic properties [69]
Computational Modeling of Biphasic Responses
- Hormetic dose-responses can be modeled using Gaussian functions: Y = baseline + amplitude · e^[-(x-x₀)²/2σ²], where x₀ represents peak concentration and σ defines hormetic zone width [15]
- For Brosimine B, this approach yielded biologically interpretable parameters with high goodness-of-fit (R² = 0.984) [15]
Organoid and Microphysiological Systems
- Emerging technologies like gut-brain axis organoids enable investigation of hormetic responses in tissue context, capturing complex interactions between polyphenols, probiotics, and host cells [103]
- These systems better replicate the food matrix effects, where the complex assembly of nutrients, fiber, and constituents modulates bioavailability and bioactivity [13]
The Scientist's Toolkit: Essential Research Reagents
| Research Tool Category | Specific Examples | Key Applications | Technical Considerations |
|---|---|---|---|
| Nrf2 Pathway Modulators | Sulforaphane [13] [102], L-Sulforaphane (Cayman #14783) | Nrf2/ARE activation, phase II enzyme induction | Use 2-15 μM range; monitor KEAP1 cysteine modifications |
| Tert-butylhydroquinone (Sigma-Aldrich #112941) | Positive control for Nrf2 activation | Optimal at 10-50 μM; may induce cytotoxicity above 100 μM | |
| ML385 (MedChemExpress #HY-100523) | Selective Nrf2 inhibitor | Use 5-20 μM for pathway inhibition studies | |
| Sirtuin Activators | Resveratrol (Sigma-Aldrich #R5010) [103] [13] | SIRT1 activation, mitochondrial biogenesis | Biphasic response: 1-10 μM optimal; cytotoxic above 50 μM |
| SRT1720 (Tocris #2781) | Potent SIRT1 activator | 1-5 μM range for cellular studies; higher potency than resveratrol | |
| ROS Detection Probes | CM-H2DCFDA (Thermo Fisher #C6827) | General oxidative stress detection | Requires esterase activity; multiple oxidant sensitivity |
| MitoSOX Red (Thermo Fisher #M36008) | Mitochondrial superoxide detection | Specific to O₂•⁻; use 5 μM loading concentration | |
| Amplex Red (Thermo Fisher #A12222) | H₂O₂ quantification | Coupled with horseradish peroxidase; highly sensitive | |
| Vitagene Detection | HO-1 Antibodies (Cell Signaling #5853S) | Heme oxygenase-1 quantification | Key Nrf2 target; indicator of hormetic response |
| Hsp70 Antibodies (Enzo #ADI-SPA-812) | Heat shock protein 70 detection | Cellular stress response biomarker | |
| Cell Viability Assays | MTT (Sigma-Aldrich #M5655) [15] | Metabolic activity assessment | Formazan crystal formation; mitochondrial dependent |
| PrestoBlue (Thermo Fisher #A13261) | Real-time viability monitoring | Resazurin reduction; non-terminal endpoint | |
| Gut-Brain Axis Models | Probiotic Strains (Lactobacillus, Bifidobacterium) [103] | Microbiota-hormesis interactions | Use 10⁹-10¹¹ CFU; assess SCFA production |
| Caco-2/HT29-MTX co-culture | Intestinal barrier function | Permeability assays (TEER); tight junction staining |
The comparative analysis of hormetins reveals a conserved mechanistic architecture centered on Nrf2-mediated antioxidant responses, sirtuin-activated longevity pathways, and mitochondrial adaptive mechanisms. However, significant differences in temporal dynamics, magnitude of effects, and therapeutic windows exist across phytochemical, physical, and nutritional interventions. Future research should prioritize several key areas:
First, the synergistic potential between hormetin categories warrants systematic investigation, particularly the emerging evidence that polyphenols combined with probiotics enhance gut bioavailability and blood-brain barrier permeability [103]. Second, personalized hormesis approaches based on genetic polymorphisms in Nrf2, sirtuins, and vitagenes could optimize therapeutic efficacy. Third, advanced delivery systems including nanoformulations may improve the bioavailability and target specificity of hormetic phytochemicals.
The integration of hormesis principles into drug development offers promising avenues for preventive therapeutics and conditioning strategies. However, rigorous attention to biphasic dose-response characteristics is essential, as efficacy rapidly transitions to toxicity within relatively narrow concentration windows. The continued elucidation of redox-based hormetic mechanisms will undoubtedly yield novel approaches for enhancing resilience across numerous pathological contexts.
This technical guide provides a comprehensive framework for validating key redox biomarkers within the context of hormesis mechanisms in redox biology research. The document details standardized methodologies for assessing the glutathione redox ratio (GSH/GSSG), monitoring NRF2 translocation dynamics, and quantifying expression of antioxidant enzymes. These biomarkers provide critical insights into the biphasic adaptive responses characteristic of hormesis, where low-level oxidative stress activates protective mechanisms that enhance cellular resilience. Designed for researchers, scientists, and drug development professionals, this guide integrates current scientific understanding with practical experimental protocols to advance the development of targeted therapeutic interventions that modulate redox signaling pathways.
Hormesis describes a phenomenon where exposure to a low-dose stressor induces an adaptive, beneficial response, in contrast to the damage caused by high-dose exposure [104] [17]. In redox biology, this is exemplified by the observation that subtoxic oxidant doses can induce adaptations that ultimately enhance the cellular antioxidant capacity. This adaptive process is fundamentally regulated by the dynamic interplay between reactive oxygen species (ROS) and the antioxidant response system [104]. The GSH/GSSG ratio serves as a primary indicator of cellular redox status, while the transcription factor NRF2 acts as a master regulator of the antioxidant response, coordinating the expression of a vast array of cytoprotective genes [105] [106] [107]. The validation of these biomarkers, along with the downstream antioxidant enzymes they regulate, is therefore essential for quantifying the hormetic response and developing therapies that can strategically induce this adaptive pathway.
The GSH/GSSG Ratio as a Quantitative Redox Biomarker
Biological Significance and Validation Rationale
The tripeptide glutathione (GSH) is the most abundant non-protein thiol in biological systems and a pivotal component of the antioxidant network. The ratio of its reduced (GSH) to oxidized (GSSG) form provides a sensitive measure of cellular redox status [108] [17]. Under physiological conditions, the intracellular GSH/GSSG ratio is maintained at >100:1, reflecting a reduced state conducive to normal cellular function [109]. During oxidative stress, GSH is consumed to counteract oxidants, leading to an increase in GSSG and a consequent decrease in this ratio, sometimes to levels as low as 10:1 or even 1:1 [108]. This shift toward a more oxidized state is not merely a marker of damage; within the hormesis framework, a moderate, transient oxidation serves as a crucial signaling event that activates adaptive responses, including the upregulation of GSH synthesis itself [104].
The diagnostic power of this biomarker is underscored by clinical studies across various pathologies. For instance, in colorectal cancer patients, the GSSG/GSH ratio in serum demonstrated higher sensitivity and specificity than classical tumor markers like CEA and CA19.9 [110]. Similarly, significant variations in the GSH:GSSG ratio have been observed across different pediatric cancers, suggesting its potential as a diagnostic and prognostic indicator [108].
Experimental Protocol: HPLC-EC Analysis of GSH/GSSG
High-Performance Liquid Chromatography with Electrochemical Detection (HPLC-EC) is a highly sensitive and specific method for the simultaneous quantification of GSH and GSSG in biological samples.
- Sample Preparation: Blood samples should be collected into pre-chilled tubes containing a thiol-stabilizing agent (e.g., acid citrate dextrose) to prevent auto-oxidation. Plasma or serum is separated by centrifugation (e.g., 4,000 × g for 10 min at 4°C) and immediately deproteinized with a strong acid like perchloric acid (PCA) or metaphosphoric acid. The resulting supernatant, stabilized with a chelating agent like EDTA, must be analyzed promptly or stored at -80°C [108] [109].
- Chromatographic Conditions:
- Column: Reverse-phase C18 (e.g., Zorbax Eclipse AAA C18, 150 x 4.6 mm, 3.5-μm particles).
- Mobile Phase: A gradient elution with a mixture of an aqueous solvent (e.g., 80 mM trifluoroacetic acid) and an organic solvent (e.g., HPLC-grade methanol) is typically used.
- Flow Rate: 1.0 mL/min.
- Temperature: Column temperature maintained at 35°C [108].
- Electrochemical Detection: A multi-channel coulometric detector is used. The optimal potentials for detecting GSH and GSSG must be determined empirically, but typically range from +400 to +900 mV. Using multiple electrodes in series enhances specificity [108].
- Validation Parameters:
- Linearity: Prepare standard curves for GSH and GSSG in the relevant biological matrix.
- Recovery: Spiked samples should demonstrate recoveries >80% for both analytes [108].
- Sensitivity: Determine the limit of detection (LOD) and limit of quantitation (LOQ) based on a signal-to-noise ratio of 3:1 and 10:1, respectively.
Table 1: Representative GSH/GSSG Ratios in Physiological and Pathological States
| Condition / Tissue | GSH/GSSG Ratio | Context and Notes |
|---|---|---|
| Resting Mammalian Cell | >100:1 [109] | Cytosolic ratio; indicates a reduced redox state. |
| Endoplasmic Reticulum | ~3:1 [109] | More oxidizing environment for proper protein folding. |
| Golgi Apparatus | Highly Oxidizing [111] | EGSH = -157 mV; low GSH concentration (1-5 mM). |
| Oxidative Stress (Models) | 10:1 to 1:1 [108] | Varies with severity and model of oxidative insult. |
| Pediatric Anaplastic Ependymoma | Lowest among cancers [108] | Blood serum analysis of pediatric patients (n=116). |
| Pediatric Retinoblastoma | Highest among cancers [108] | Blood serum analysis of pediatric patients (n=116). |
| Colorectal Cancer | Significantly decreased [110] | Serum ratio; proposed as a sensitive tumor marker. |
NRF2 Translocation as a Mechanistic Hormesis Marker
NRF2-KEAP1 Signaling Pathway in Hormetic Adaptation
NRF2 (Nuclear factor erythroid 2-related factor 2) is the master transcriptional regulator of over 200 cytoprotective genes. Under homeostatic conditions, NRF2 is continuously ubiquitinated and targeted for proteasomal degradation by its cytosolic repressor, KEAP1 (Kelch-like ECH-associated protein 1) [106] [107]. This interaction represents the molecular sensor for redox hormesis. Low-dose oxidative or electrophilic stress modifies critical cysteine residues on KEAP1, leading to a conformational change that disrupts its ability to target NRF2 for degradation [105] [106]. This stabilization allows newly synthesized NRF2 to accumulate and translocate to the nucleus, where it heterodimerizes with small MAF proteins and binds to the Antioxidant Response Element (ARE) in the promoter regions of its target genes [106] [107]. This process, which can be initiated within hours of a hormetic stimulus such as acute exercise, orchestrates a coordinated antioxidant and detoxification response [104] [105].
Diagram Title: NRF2-KEAP1 Pathway in Hormetic Activation
Experimental Protocol: Immunofluorescence for NRF2 Translocation
Immunofluorescence microscopy is the primary method for visualizing and quantifying the subcellular localization of NRF2.
- Cell Culture and Treatment: Plate cells on glass coverslips and allow to adhere. Treat with a hormetic stimulus (e.g., low-dose sulforaphane, 1-10 µM H₂O₂, or apply electrical pulse stimulation to mimic exercise [105]). Include both vehicle controls and a positive control (e.g., a known NRF2 activator).
- Fixation and Permeabilization: After treatment, rinse cells with PBS and fix with 4% paraformaldehyde for 15 minutes at room temperature. Permeabilize cells with 0.1-0.5% Triton X-100 in PBS for 10-15 minutes.
- Immunostaining:
- Blocking: Incubate with a blocking solution (e.g., 5% BSA or normal serum) for 1 hour.
- Primary Antibody: Incubate with a validated, high-specificity anti-NRF2 antibody (critical to avoid cross-reactivity [106]) diluted in blocking buffer overnight at 4°C.
- Secondary Antibody: After washing, incubate with a fluorophore-conjugated secondary antibody (e.g., Alexa Fluor 488 or 594) for 1 hour at room temperature, protected from light.
- Nuclear Counterstain and Mounting: Stain nuclei with DAPI or Hoechst. Mount coverslips onto slides using an anti-fade mounting medium.
- Imaging and Quantification:
- Acquire high-resolution images using a confocal or epifluorescence microscope with consistent settings across all samples.
- Quantitative Analysis: Use image analysis software (e.g., ImageJ) to quantify the fluorescence intensity of NRF2 in the nucleus versus the cytoplasm for a statistically significant number of cells (e.g., n>100 per condition). The nuclear-to-cytoplasmic (N/C) ratio of NRF2 signal is the key metric for translocation.
Expression of Antioxidant Enzymes as Functional Hormetic Output
Key Enzymes and Their Regulatory Logic
The functional output of the NRF2-mediated hormetic response is the transcriptional upregulation of a battery of antioxidant and phase II detoxification enzymes. Key targets include:
- γ-Glutamylcysteine Synthetase (γ-GCS): The rate-limiting enzyme in de novo GSH synthesis. Its upregulation is a hallmark of the sustained adaptive response, increasing the cellular capacity to regenerate GSH [104].
- Heme Oxygenase-1 (HO-1): Degrades heme to produce biliverdin (a potent antioxidant), carbon monoxide, and free iron, conferring protection against oxidative insult [105] [107].
- NAD(P)H:quinone oxidoreductase 1 (NQO1): Catalyzes the two-electron reduction of quinones, preventing their participation in redox cycling and ROS generation [106].
- Glutathione S-transferase (GST): Conjugates GSH to a wide range of electrophilic toxins, facilitating their excretion [104].
- Glutathione Peroxidase (GPx): Utilizes GSH to reduce hydrogen peroxide and lipid hydroperoxides to water and corresponding alcohols, respectively [17] [107].
The induction profiles of these enzymes represent a functional validation of a successful hormetic adaptation.
Experimental Protocol: Western Blot Analysis
Western blotting allows for the semi-quantitative assessment of protein levels for these key antioxidant enzymes.
- Protein Extraction: Lyse cells or homogenize tissue samples in RIPA buffer supplemented with protease and phosphatase inhibitors. Centrifuge at high speed (e.g., 15,000 × g) to clear the lysate.
- Electrophoresis and Transfer: Separate equal amounts of protein (20-40 µg) by SDS-PAGE and transfer to a nitrocellulose or PVDF membrane.
- Immunoblotting:
- Blocking: Block the membrane with 5% non-fat milk or BSA in TBST for 1 hour.
- Primary Antibody Incubation: Probe with specific primary antibodies against the target proteins (e.g., anti-γ-GCS, anti-HO-1, anti-NQO1) and a loading control (e.g., GAPDH, β-Actin) overnight at 4°C.
- Secondary Antibody Incubation: Incubate with an HRP-conjugated secondary antibody for 1 hour at room temperature.
- Detection and Analysis: Develop the blots using enhanced chemiluminescence (ECL) reagent and image with a digital imager. Quantify band intensities using densitometry software and normalize to the loading control.
Table 2: Key Antioxidant Enzymes Regulated by the NRF2-ARE Pathway
| Enzyme | Abbreviation | Function in Redox Homeostasis | Response to Hormesis |
|---|---|---|---|
| γ-Glutamylcysteine Synthetase | γ-GCS | Rate-limiting enzyme in GSH synthesis [104]. | Upregulated; increases cellular GSH synthesis capacity [104]. |
| Heme Oxygenase-1 | HO-1 | Degrades heme to antioxidant products like biliverdin [107]. | Strongly induced; provides cytoprotection [105]. |
| NAD(P)H Quinone Dehydrogenase 1 | NQO1 | Prevents quinone redox cycling [106]. | Induced; reduces oxidative stress from quinones [105]. |
| Glutathione S-Transferase | GST | Conjugates GSH to electrophiles for detoxification [104]. | Activated via oxidation in short-term; transcriptionally upregulated long-term [104]. |
| Glutathione Peroxidase | GPx | Reduces H₂O₂ and organic hydroperoxides using GSH [107]. | Upregulated; enhances peroxide scavenging capacity [105]. |
| Superoxide Dismutase | SOD | Dismutates superoxide (O₂•⁻) to H₂O₂ [107]. | Upregulated (e.g., SOD2 in myocardium [105]). |
| Catalase | CAT | Converts H₂O₂ to H₂O and O₂ [107]. | Upregulated in some models (e.g., myocardium [105]). |
Integrated View: Temporal Hierarchy of Redox Biomarkers in Hormesis
The adaptive hormetic response unfolds over distinct temporal scales, and a robust validation strategy must account for this hierarchy. The following diagram integrates the biomarkers into a cohesive temporal framework:
Diagram Title: Temporal Hierarchy of Redox Biomarkers in Hormesis
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table compiles key reagents essential for conducting experiments in redox hormesis biomarker validation.
Table 3: Essential Research Reagents for Redox Biomarker Analysis
| Reagent / Material | Primary Function | Application Examples |
|---|---|---|
| High-Specificity Anti-NRF2 Antibody | Detection of NRF2 for Western Blot (WB) and Immunofluorescence (IF). | Critical for accurate localization; must target the correct molecular weight band (~90-110 kDa) and avoid cross-reactivity [106]. |
| Anti-KEAP1 Antibody | Detection of the NRF2 repressor protein (WB, IF). | Useful for monitoring the KEAP1-NRF2 complex. |
| Antibodies against Antioxidant Enzymes | Protein level quantification (WB). | Targets: HO-1, NQO1, γ-GCS catalytic/subunit, GST, SOD, Catalase. |
| Coulometric Electrochemical Detector | Detection of GSH and GSSG in HPLC. | Provides high sensitivity and specificity for redox state analysis [108]. |
| Reverse Phase C18 Column | Chromatographic separation of GSH and GSSG. | Essential for HPLC-based glutathione quantification [108]. |
| Thiol-Stabilizing Agents | Prevention of GSH auto-oxidation during sample prep. | e.g., Acid citrate dextrose, N-ethylmaleimide (NEM), metaphosphoric acid [109]. |
| NRF2 Activators (Inducers) | Positive control for pathway activation. | e.g., Sulforaphane, tertiary-butyl hydroquinone (tBHQ) [105]. |
| Proteasome Inhibitor | Stabilizes NRF2 by inhibiting its degradation. | e.g., MG132; used to experimentally demonstrate NRF2 turnover [106]. |
The translation of antioxidant therapies from promising preclinical data to clinical practice represents one of the most significant challenges in modern redox biology. Despite robust mechanistic evidence linking oxidative stress to numerous pathological conditions, randomized controlled trials (RCTs) of antioxidant supplements have yielded largely disappointing results [112]. This contradiction underscores a fundamental complexity in biological redox systems, where the traditional oxidative stress hypothesis has proven insufficient to explain the nuanced role of reactive oxygen species (ROS) in cellular signaling and physiological function [113]. The clinical translation of antioxidant supplementation is fraught with controversies that stem from a failure to appreciate the biphasic nature of redox signaling and the critical concept of hormesis – where low levels of oxidants activate adaptive stress response pathways that enhance cellular resilience [17] [4].
The initial enthusiasm for antioxidant supplementation was grounded in a straightforward premise: if oxidative damage contributes to disease pathology, then augmenting endogenous antioxidant defenses should confer therapeutic benefit. This rationale propelled numerous large-scale clinical trials, many of which failed to demonstrate efficacy and some of which revealed unexpected adverse effects [112] [113]. For instance, the Alpha-Tocopherol and Beta-Carotene (ATBC) trial found an 18% increased risk of lung cancer among smokers supplemented with β-carotene, while the Beta-Carotene and Retinol Efficacy Trial (CARET) reported a 25% increase in lung cancer incidence in high-risk populations receiving combined β-carotene and retinyl palmitate supplementation [113]. These findings forced a paradigm shift from the simplistic "oxidants are bad, antioxidants are good" model toward a more sophisticated understanding of redox biology that incorporates hormesis and precise redox regulation [17] [4].
Redox Homeostasis and Hormesis: Conceptual Framework for Antioxidant Action
The Dual Nature of Reactive Oxygen Species
Reactive oxygen species (ROS) encompass a variety of oxygen-derived molecules including free radicals like superoxide anion (O₂•⁻) and hydroxyl radical (HO•), as well as non-radical species such as hydrogen peroxide (H₂O₂) [17]. While excessive ROS production can damage biomolecules through oxidation, physiological ROS levels serve as crucial signaling molecules that regulate cellular processes including proliferation, differentiation, and immune function [17] [112]. The concentration-dependent effects of ROS exemplify the hormetic principle: low levels stimulate adaptive responses, while high levels cause damage [4].
The major enzymatic sources of ROS include NADPH oxidases (NOX), which primarily produce O₂•⁻, and the mitochondrial electron transport chain, where electron leakage generates O₂•⁻ as a byproduct of oxidative phosphorylation [17]. Under pathological conditions, xanthine oxidase and cytochrome P450 systems also contribute significantly to ROS production [17]. The cellular antioxidant network includes enzymatic components such as superoxide dismutase (SOD), catalase (CAT), glutathione peroxidase (GPx), and peroxiredoxins (PRDX), as well as non-enzymatic antioxidants like glutathione (GSH), vitamins C and E, bilirubin, and uric acid [17] [113].
Hormesis in Redox Biology
Hormesis describes the biphasic dose-response phenomenon wherein low doses of a stressor trigger beneficial adaptive responses, while high doses cause inhibition or damage [4]. In redox biology, this manifests as mitohormesis (mitochondrial adaptation to low-level ROS) and activation of cytoprotective pathways that enhance cellular resilience [114] [4]. The molecular mechanisms underlying redox hormesis involve the activation of transcription factors such as Nrf2, which coordinates the expression of antioxidant and detoxification enzymes, and NF-κB, which regulates inflammatory responses [4]. These pathways are increasingly recognized as critical mediators of the health benefits associated with certain phytochemicals and mild stressors [115].
The following diagram illustrates the key signaling pathways activated under conditions of mild oxidative stress that lead to hormetic adaptations:
Clinical Evidence: Systematic Analyses of Antioxidant Interventions
Failed Trials and Adverse Outcomes
The discrepancy between epidemiological evidence suggesting protective effects of antioxidant-rich diets and interventional trials of isolated antioxidant supplements highlights the complexity of translating redox biology into clinical practice [112] [113]. The table below summarizes key clinical trials that demonstrated neutral or negative outcomes for antioxidant supplementation:
Table 1: Major Clinical Trials Demonstrating Neutral or Adverse Effects of Antioxidant Supplementation
| Trial (Year) | Population | Intervention | Duration | Primary Outcomes | Adverse Effects |
|---|---|---|---|---|---|
| ATBC (1990s) | 29,133 male smokers | β-carotene, vitamin E | 5-8 years | No reduction in lung cancer incidence | 18% increase in lung cancer with β-carotene |
| CARET (1990s) | Smokers and asbestos-exposed workers | β-carotene + retinyl palmitate | 4 years | Trial terminated early | 25% increased lung cancer risk |
| HOPE-TOO (2005) | High-risk CVD patients | Vitamin E (400 IU/day) | 7 years | No CV benefit | Increased risk of heart failure |
| SELECT (2009) | 35,533 men | Vitamin E + selenium | 5.5 years | No prostate cancer prevention | Increased diabetes risk with selenium |
The failure of these large-scale interventions stems from several factors, including the disruption of physiological redox signaling, interference with endogenous antioxidant systems, and the possibility of reductive stress – a condition wherein excessive antioxidant capacity disrupts essential ROS-mediated processes [113]. Furthermore, the timing of intervention may be critical, as antioxidants may be more effective in prevention than in reversing established disease pathology [112].
Conditional Successes and Context-Dependent Efficacy
Despite numerous disappointments, some clinical trials have demonstrated benefits under specific conditions, highlighting the context-dependent nature of antioxidant efficacy. A 2025 meta-analysis of 39 RCTs involving 1,714 participants found that antioxidants alone could enhance muscle strength in older adults, with the combination of antioxidants and exercise proving more effective than either intervention alone for improving physical function [116]. Similarly, a subgroup analysis of patients with type 2 diabetes and a specific haptoglobin genotype (Hp 2-2) revealed that vitamin E supplementation reduced cardiovascular risk by 43%, highlighting the importance of patient stratification in antioxidant therapy [113].
Another 2025 meta-analysis of 27 RCTs examining propolis supplementation demonstrated significant reductions in inflammatory markers (CRP, IL-6, TNF-α) and increases in antioxidant capacity (GSH, GPx) [117]. The following table summarizes conditions associated with more favorable responses to antioxidant interventions:
Table 2: Contexts Associated with Positive Outcomes from Antioxidant Interventions
| Context | Intervention | Outcome | Proposed Mechanism |
|---|---|---|---|
| Sarcopenia in older adults [116] | Antioxidants + exercise | Improved muscle strength & physical function | Reduced oxidative stress, enhanced protein synthesis |
| Type 2 diabetes with Hp 2-2 genotype [113] | Vitamin E | 43% reduced cardiovascular risk | Compensation for genetic antioxidant deficiency |
| General inflammation [117] | Propolis | Reduced CRP, IL-6, TNF-α | Enhanced antioxidant capacity (GSH, GPx) |
| Cognitive decline [113] | Long-term β-carotene | Slowed cognitive degeneration | Protection against neuronal oxidative damage |
Molecular Mechanisms: Hormetic Pathways and Their Pharmacological Modulation
Nrf2-Keap1-ARE Signaling Pathway
The Kelch-like ECH-associated protein 1 (Keap1)-Nuclear factor erythroid 2-related factor 2 (Nrf2)-Antioxidant Response Element (ARE) pathway represents the primary cellular defense mechanism against oxidative stress and is a key target for hormetic interventions [4] [115]. Under basal conditions, Nrf2 is bound to Keap1 in the cytoplasm and targeted for proteasomal degradation. Oxidative modification of critical cysteine residues on Keap1 by electrophilic molecules or ROS leads to Nrf2 stabilization and translocation to the nucleus, where it heterodimerizes with small Maf proteins and binds to ARE sequences, activating the transcription of over 500 cytoprotective genes [115].
These genes encode phase II detoxifying enzymes (e.g., GST, NQO1), antioxidant proteins (e.g., SOD, CAT, GPx, HO-1), and drug transporters that collectively enhance cellular resilience. Numerous dietary hormetins, including sulforaphane from cruciferous vegetables, curcumin from turmeric, and quercetin from apples, activate the Nrf2 pathway through electrophilic modification of Keap1 [115]. The following experimental protocol outlines a standard approach for evaluating Nrf2 pathway activation:
Experimental Protocol 1: Assessment of Nrf2 Pathway Activation
- Cell Culture: Maintain relevant cell lines (e.g., HepG2, HEK293) in appropriate medium.
- Treatment: Expose cells to test compounds (0.1-10 μM) or vehicle control for 2-24 hours.
- Nuclear Extraction: Use commercial kits to isolate nuclear and cytosolic fractions.
- Western Blotting: Analyze Nrf2 protein levels in nuclear fractions using anti-Nrf2 antibodies.
- qRT-PCR: Measure mRNA expression of Nrf2 target genes (NQO1, HO-1, GCLC).
- ARE-Luciferase Reporter Assay: Transfert cells with ARE-driven luciferase construct and measure activity after treatment.
- Functional Assays: Assess cellular antioxidant capacity (ORAC, FRAP) and resistance to oxidative challenge.
Mitochondrial Adaptive Responses (Mitohormesis)
Mitohormesis describes the adaptive response of mitochondria to mild stress, resulting in enhanced mitochondrial function and increased stress resistance [4]. Low levels of mitochondrial ROS activate multiple signaling pathways, including those mediated by AMPK, SIRT1, and PGC-1α, leading to mitochondrial biogenesis, improved oxidative phosphorylation efficiency, and metabolic adaptations [114] [115]. Dietary components such as resveratrol, quercetin, and EGCG can induce mitohormesis through mild uncoupling or inhibition of mitochondrial complex I, resulting in increased NAD+/NADH ratio and activation of sirtuins [115].
The diagram below illustrates the experimental workflow for studying mitohormetic responses in cell culture models:
Methodological Considerations and Research Tools
The Scientist's Toolkit: Essential Reagents and Assays
Research in redox biology and hormesis requires specialized reagents and methodologies to accurately assess oxidative stress parameters and adaptive responses. The following table details key research tools essential for investigating antioxidant mechanisms and hormetic responses:
Table 3: Essential Research Reagents and Assays for Redox Biology and Hormesis Studies
| Reagent/Assay | Application | Key Features | Technical Considerations |
|---|---|---|---|
| DCFH-DA | Intracellular ROS detection | Cell-permeable, converts to fluorescent DCF upon oxidation | Subject to autoxidation; multiple ROS types |
| MitoSOX Red | Mitochondrial superoxide detection | Cationic triphenylphosphonium derivative targets mitochondria | Specific for O₂•⁻; validate with inhibitors |
| GSH/GSSG Assay | Redox status assessment | Measures reduced/oxidized glutathione ratio | Rapid processing required; avoid oxidation |
| Nrf2 Antibodies | Western blot, immunofluorescence | Detect nuclear translocation | Validate specificity with knockdown controls |
| ARE-Luciferase Reporter | Nrf2 pathway activation | Transcriptional activity measurement | Transfection efficiency normalization |
| Seahorse XF Analyzer | Mitochondrial function | Real-time OCR and ECAR measurements | Optimize cell density and inhibitor concentrations |
| Antibody Arrays | Inflammatory cytokine profiling | Multiplex analysis of multiple targets | Cross-reactivity validation required |
Experimental Design Considerations
Robust investigation of hormetic responses requires careful experimental design with particular attention to dose-ranging studies. The typical hormetic dose-response features a low-dose stimulatory zone (approximately 0.1-10 times the No-Observed-Adverse-Effect Level) and a high-dose inhibitory zone [4]. Researchers should include multiple low concentrations below the traditional threshold for toxicity to adequately characterize biphasic responses. Time-course experiments are equally important, as hormetic adaptations often require time for gene expression and protein synthesis, whereas high-dose toxicity may manifest more rapidly [4].
For clinical translation, consideration of patient populations with elevated oxidative stress (e.g., specific genetic backgrounds, disease states) may enhance the likelihood of detecting beneficial effects [112] [113]. The combination of antioxidants with physiological stressors such as exercise may also yield synergistic benefits by augmenting naturally occurring adaptive responses [116] [114].
Future Perspectives and Translational Strategies
The failures of past antioxidant trials necessitate a paradigm shift toward precision redox medicine that acknowledges the complexity of redox signaling and the therapeutic potential of hormesis [112] [4]. Future strategies should include:
- Patient Stratification: Identification of biomarkers (genetic, metabolic, or oxidative stress markers) to select populations most likely to benefit from antioxidant interventions [113].
- Hormetic Conditioning: Development of interventions that elicit mild oxidative stress to activate endogenous defense mechanisms rather than direct antioxidant supplementation [114] [4].
- Chronotherapeutic Approaches: Timing of interventions to align with circadian rhythms of redox regulation and specific disease phases [112].
- Dietary Matrix-Based Approaches: Investigation of whole foods and complex mixtures that provide low doses of multiple hormetins rather than isolated high-dose antioxidants [115].
The emerging understanding of reductive stress as a pathological condition underscores the risks of indiscriminate antioxidant use and highlights the need for maintaining optimal redox balance rather than maximizing antioxidant capacity [113]. Future research should focus on defining this optimal redox set point across different tissues and physiological states to guide targeted therapeutic interventions.
The clinical translation of antioxidant supplementation has been hampered by an oversimplified understanding of redox biology that failed to account for the essential signaling functions of ROS and the adaptive benefits of mild oxidative stress through hormesis. The disappointing results of major antioxidant trials stand in contrast to the beneficial effects observed in specific contexts where redox balance is compromised or hormetic pathways are engaged. Moving forward, successful clinical translation will require a more nuanced approach that respects the complexity of redox regulation, employs patient stratification, and considers hormetic interventions that enhance endogenous defense mechanisms rather than merely scavenging ROS. The future of redox-based therapeutics lies not in blanket antioxidant supplementation, but in precision approaches that modulate redox signaling to maintain optimal physiological function and enhance resilience to oxidative challenge.
Conclusion
The hormesis mechanism in redox biology represents a fundamental, evolutionarily conserved adaptive strategy where mild oxidative stress potently stimulates robust defense and repair systems. The key takeaways underscore the centrality of biphasic dose-responses, the critical role of pathways like NRF2 and AMPK, and the necessity of precisely defining the hormetic zone for any intervention. Future research must prioritize overcoming the challenges of dose optimization, temporal dynamics, and biological variability to successfully harness hormesis. The implications for biomedical research are vast, pointing toward novel therapeutic paradigms that exploit endogenous protective pathways to combat aging, neurodegenerative diseases, and cancer, ultimately moving beyond the outdated linear model toward a more nuanced and effective hormesis-based framework in medicine.
References
- 1. Defined - PMC Hormesis [https://pmc.ncbi.nlm.nih.gov/articles/PMC2248601/]
- 2. New considerations on hormetic response against ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4390794/]
- 3. When less is more: hormesis against stress and disease [https://microbialcell.com/researcharticles/when-less-is-more-hormesis-against-stress-and-disease/]
- 4. Current advances and future trends of hormesis in disease [https://www.nature.com/articles/s41514-024-00155-3]
- 5. Frontiers | Brosimine B and the Biphasic - Dose : Insights... Response [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1558726/abstract]
- 6. Reconceptualization of Hormetic Responses in the Frame ... [https://www.mdpi.com/1422-0067/23/1/49]
- 7. : Hormesis - Biphasic to Fungicides in... | IntechOpen Dose Responses [https://www.intechopen.com/chapters/44734]
- 8. The Hormetic Adaptative Capacity and Resilience to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12025095/]
- 9. in Metabolism Hormesis [https://www.numberanalytics.com/blog/hormesis-metabolism-guide]
- 10. Hormesis: a fundamental concept in biology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5354598/]
- 11. The dose response principle from philosophy to modern ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6226566/]
- 12. Hormesis: Decoding Two Sides of the Same Coin [https://www.mdpi.com/1424-8247/8/4/865]
- 13. Dietary hormesis: beyond nutrition and energy supply - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12280001/]
- 14. Oxytocin, Vasopressin and Stress: A Hormetic Perspective [https://www.mdpi.com/1467-3045/47/8/632]
- 15. Brosimine B and the biphasic dose-response: insights into ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1558726/full]
- 16. Fundamentals of redox regulation in biology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11921270/]
- 17. Hormesis and Oxidative Distress: Pathophysiology of Reactive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9405171/]
- 18. ROS Function in Redox Signaling and Oxidative Stress [https://www.sciencedirect.com/science/article/pii/S0960982214003261]
- 19. ROS Function in Redox Signaling and Oxidative Stress - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4055301/]
- 20. A Quantitative Method to Monitor Reactive Oxygen Species ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4211297/]
- 21. Oxygen Toxicity and Reactive Oxygen Species: The Devil ... [https://www.nature.com/articles/pr2009174]
- 22. Automated image analysis for quantification of reactive ... [https://www.sciencedirect.com/science/article/abs/pii/S1046202316301505]
- 23. Imaging Reactive Oxygen Species-Induced Modifications in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4900226/]
- 24. The Oxygen Paradox, the French Paradox, and age-related ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5745211/]
- 25. Time in Redox Adaptation Processes: From Evolution to ... [https://www.mdpi.com/1422-0067/17/10/1649]
- 26. Is “Preparation for Oxidative Stress” a Case of ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2018.00945/full]
- 27. Quantitative Redox Biology: An approach to understanding ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3661692/]
- 28. Pulsed Hyperoxia Acts on Plasmatic Advanced Glycation ... [https://www.mdpi.com/1422-0067/25/4/2394]
- 29. Quantitative analysis of redox proteome reveals oxidation- ... [https://www.sciencedirect.com/science/article/pii/S221323172200115X]
- 30. Redox regulation: mechanisms, biology and therapeutic ... [https://www.nature.com/articles/s41392-024-02095-6]
- 31. Glutathione: new roles in redox signaling for an old ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4144092/]
- 32. Redox regulation by glutathione needs enzymes [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2014.00168/full]
- 33. The glutathione system maintains the thiol redox balance ... [https://www.sciencedirect.com/science/article/pii/S0891584925002229]
- 34. Oxidative Stress and Redox Imbalance - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC11988017/]
- 35. Redox-Sensitive Transcription Factors as Prime Targets for ... [https://www.sciencedirect.com/science/article/pii/S0022316622105456]
- 36. Science review: Redox and oxygen-sensitive transcription ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC153445/]
- 37. Redox and oxygen-sensitive transcription factors in the ... [https://ccforum.biomedcentral.com/articles/10.1186/cc1840]
- 38. Nrf2 Signaling Pathway Activation through Keap1 ... [https://www.sciencedirect.com/science/article/abs/pii/S0166445X25002772]
- 39. Altered NRF2 signalling in systemic redox imbalance [https://pmc.ncbi.nlm.nih.gov/articles/PMC12554130/]
- 40. New redox-sensitive pathway reveals how cells activate ... [https://www.news-medical.net/news/20250724/New-redox-sensitive-pathway-reveals-how-cells-activate-AMPK-in-response-to-metabolic-stress.aspx]
- 41. The complex interplay between redox dysregulation and ... [https://www.sciencedirect.com/science/article/abs/pii/S0006295224007305]
- 42. Exploring the role of mTOR pathway in aging and age-related ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12419451/]
- 43. SIRT1 as a masterful reciprocal regulator of molecular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12213863/]
- 44. SIRT1-FOXOs signaling pathway: A potential target for ... [https://www.sciencedirect.com/science/article/abs/pii/S0898656824003772]
- 45. From Sirtuin Biology to Human Diseases: An Update - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3522245/]
- 46. The multifaceted impact of physical exercise on FoxO ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1614732/full]
- 47. Redox regulation: mechanisms, biology and therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11885647/]
- 48. Comparison between short-term stress and long-term ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8873613/]
- 49. Epigenetic alterations facilitate transcriptional and ... [https://www.nature.com/articles/s41556-025-01786-8]
- 50. at the intersection of the heat shock... Transcriptional reprogramming [https://pubmed.ncbi.nlm.nih.gov/38103561/]
- 51. regulation and nuclear Transcriptional : roles of... reprogramming [https://link.springer.com/article/10.1007/s00018-012-1235-7]
- 52. Epigenetic programming and reprogramming during ... [https://www.nature.com/articles/nsmb.2489]
- 53. Present and future challenges for the investigation of ... [https://www.sciencedirect.com/science/article/pii/S0160412023000491]
- 54. Aging, Rejuvenation, and Epigenetic Reprogramming [https://pmc.ncbi.nlm.nih.gov/articles/PMC3336960/]
- 55. Hormetic shifting of redox environment by pro-oxidative ... [https://www.sciencedirect.com/science/article/pii/S0891584916303793]
- 56. Intracellular and Extracellular Redox Signals During ... [https://www.sciencedirect.com/science/article/abs/pii/S0891584925013085]
- 57. The Impact of Sulforaphane on Sex-Specific Conditions ... [https://www.mdpi.com/2076-3417/15/2/522]
- 58. Resveratrol: Molecular Mechanisms, Health Benefits, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12152427/]
- 59. New Perspectives on the Use of Resveratrol in ... [https://www.mdpi.com/1467-3045/47/9/692]
- 60. Exercise, hormesis and ageing - Biogerontology [https://link.springer.com/article/10.1007/s10522-024-10170-2]
- 61. Systematic transcriptomics analysis of calorie restriction ... [https://www.nature.com/articles/s42003-025-08178-6]
- 62. Does this diet increase or decrease oxidant production? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6837320/]
- 63. Preconditioning is hormesis part I: Documentation, dose- ... [https://www.sciencedirect.com/science/article/abs/pii/S1043661815301912]
- 64. Protein Redox Modification as a Cellular Defense ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4026984/]
- 65. Investigating Molecular Mechanisms in Ischemic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11947376/]
- 66. The role of preconditioning in the development of resilience [https://www.sciencedirect.com/science/article/pii/S2468202022000158]
- 67. Chemotherapeutic hormesis induced by the tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11696277/]
- 68. Hormetic and synergistic effects of cancer treatments revealed ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-023-11542-6]
- 69. Quantification of Hormesis in Anticancer-Agent Dose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2695573/]
- 70. How does hormesis impact biology, toxicology, and ... [https://www.nature.com/articles/s41514-017-0013-z]
- 71. Statistical modeling of the hormetic dose zone and the toxic ... [https://academic.oup.com/etc/article/34/5/1169/7761584]
- 72. The hormesis database: The occurrence of hormetic dose ... [https://www.sciencedirect.com/science/article/abs/pii/S0273230011001309]
- 73. The hormetic dose-response mechanism: Nrf2 activation [https://www.sciencedirect.com/science/article/abs/pii/S1043661821001109]
- 74. A Theoretical Model for the Hormetic Dose-response Curve ... [https://ar.iiarjournals.org/content/35/11/5851]
- 75. Redox homeostasis: The Golden Mean of healthy living [https://www.sciencedirect.com/science/article/pii/S2213231716300106]
- 76. Intracellular and Extracellular Redox Signals During ... [https://www.sciencedirect.com/science/article/pii/S0891584925013085]
- 77. Effect of exercise intensity on redox biomarkers in healthy adults [https://pmc.ncbi.nlm.nih.gov/articles/PMC12367122/]
- 78. Linking oxidative stress biomarkers to disease progression ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1611842/full]
- 79. Beyond Antioxidants: How Redox Pathways Shape Cellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12466437/]
- 80. Oxidative Stress: Signaling Pathways, Biological Functions, and Disease - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12209598/]
- 81. The Hormesis Concept: Strengths and Shortcomings [https://www.mdpi.com/2218-273X/13/10/1512]
- 82. Less Can Be More: The Hormesis Theory of Stress Adaptation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8000639/]
- 83. Hormesis provides a generalized quantitative estimate of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3058190/]
- 84. Oxidative stress adaptation with acute, chronic, and ... [https://www.sciencedirect.com/science/article/abs/pii/S0891584912018011]
- 85. Hormesis, cellular stress response and vitagenes as critical ... [https://www.sciencedirect.com/science/article/abs/pii/S0098299711000513]
- 86. Comparison of Hormonal, Inflammatory, Muscle Damage ... [https://www.mdpi.com/2075-4663/13/6/184]
- 87. Current advances and future trends of hormesis in disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC11096327/]
- 88. Modeling Biphasic, Non-Sigmoidal Dose-Response ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10462167/]
- 89. Assessment of Pharmacologic Area Under the Curve When ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3152796/]
- 90. Biphasic dose-response and effects of near-infrared ... [https://www.sciencedirect.com/science/article/pii/S1011134424001180]
- 91. Biphasic Dose-Response Induced by Phytochemicals [https://www.mdpi.com/2077-0383/9/3/718]
- 92. Receiver Operating Characteristic Analysis and Clinical Trial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6263661/]
- 93. New Study: Low-Dose Radiation Not As Harmful As Previously Believed [https://www.forbes.com/sites/annabroughel/2025/09/07/new-study-low-dose-radiation-not-as-harmful-as-previously-believed/]
- 94. Linear no-threshold model [https://en.wikipedia.org/wiki/Linear_no-threshold_model]
- 95. A better model? Low levels of radiation and... -- ANS / Nuclear Newswire [https://www.ans.org/news/2025-08-05/article-7155/a-better-model-low-levels-of-radiation-and-health-effects/]
- 96. Hormesis and health: molecular mechanisms and the key ... [https://www.sciencedirect.com/science/article/pii/S2772753X25001467]
- 97. Replacing LNT: The Integrated LNT-Hormesis Model - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7160778/]
- 98. Origin of the linearity no threshold (LNT) dose-response ... [https://pubmed.ncbi.nlm.nih.gov/23887208/]
- 99. The Controversial Linear No-Threshold Model [https://jnm.snmjournals.org/content/58/1/7]
- 100. Linear No-Threshold Model VS . Radiation Hormesis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3834742/]
- 101. Exploring the obesity parADOX: A multisystem review [https://pubmed.ncbi.nlm.nih.gov/40680931/]
- 102. Hormetic Dietary Phytochemicals - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2635914/]
- 103. Hormetic Nutrition and Redox Regulation in Gut–Brain Axis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11047582/]
- 104. Time in Redox Adaptation Processes - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC5085682/]
- 105. Nrf2 mediates redox adaptations to exercise - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5078682/]
- 106. The Nrf2-Antioxidant Response Element Signaling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2679427/]
- 107. Nrf2 and Oxidative Stress: A General Overview of ... [https://www.mdpi.com/2076-3921/11/12/2345]
- 108. Redox status expressed as GSH:GSSG ratio as a marker for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3506742/]
- 109. Assessment of glutathione/glutathione disulphide ratio and ... [https://www.sciencedirect.com/science/article/abs/pii/S0891584917307244]
- 110. The Effectiveness of Glutathione Redox Status as a ... [https://pubmed.ncbi.nlm.nih.gov/34201191/]
- 111. Characterization of the glutathione redox state in the Golgi ... [https://www.sciencedirect.com/science/article/pii/S2213231725000734]
- 112. Targeting oxidative stress in disease: promise and ... [https://www.nature.com/articles/s41573-021-00233-1]
- 113. More than Just Antioxidants: Redox-Active Components ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9774234/]
- 114. The Hormetic Adaptative Capacity and Resilience to ... [https://www.mdpi.com/2227-9059/13/4/949]
- 115. Dietary hormesis: beyond nutrition and energy supply [https://www.nature.com/articles/s41538-025-00518-4]
- 116. Systematic review and meta-analysis of antioxidants with ... [https://www.nature.com/articles/s41598-025-16917-2]
- 117. Propolis supplementation on inflammatory and oxidative ... [https://pubmed.ncbi.nlm.nih.gov/40421039/]