DNP-MRI for Redox Imaging: A Revolutionary Tool for In Vivo Metabolic Research and Drug Development
This article provides a comprehensive overview of Dynamic Nuclear Polarization Magnetic Resonance Imaging (DNP-MRI) as a transformative technology for non-invasive, in vivo redox imaging.
DNP-MRI for Redox Imaging: A Revolutionary Tool for In Vivo Metabolic Research and Drug Development
Abstract
This article provides a comprehensive overview of Dynamic Nuclear Polarization Magnetic Resonance Imaging (DNP-MRI) as a transformative technology for non-invasive, in vivo redox imaging. Targeting researchers, scientists, and drug development professionals, we explore the foundational principles of hyperpolarization using nitroxide radicals and other probes to dramatically enhance signal for metabolic imaging. The scope covers core methodologies for real-time mapping of tissue redox status, key applications in oncology, neuroscience, and cardiology, and practical guidance for optimizing experimental protocols and data analysis. We further detail validation strategies against established techniques like EPR and fluorescence imaging and compare DNP-MRI with other metabolic imaging modalities. This guide synthesizes current advancements and outlines future clinical translation pathways, positioning DNP-MRI as a critical tool for understanding disease mechanisms and evaluating novel therapeutics.
Unraveling Redox Biology: The Core Principles and Probes of DNP-MRI Technology
Redox imbalance, a state of disrupted equilibrium between reactive oxygen species (ROS) production and antioxidant defense, is a fundamental pathological mechanism across diverse diseases. In cancer, sustained oxidative stress drives genomic instability, proliferation, and metastasis. In neurodegenerative disorders like Alzheimer's and Parkinson's diseases, redox imbalance promotes protein misfolding, mitochondrial dysfunction, and neuronal death. Quantifying this dynamic, spatially heterogeneous imbalance in vivo is a major challenge. Dynamic Nuclear Polarization Magnetic Resonance Imaging (DNP-MRI), specifically using redox-sensitive probes like [1-¹³C]dehydroascorbic acid (DHA) and [1-¹³C]ascorbic acid (AA), enables non-invasive, real-time mapping of tissue redox states. This Application Note details protocols for utilizing DNP-MRI to interrogate redox biology in disease models, framed within a thesis advancing quantitative redox imaging.
Key Quantitative Data in Redox-Associated Diseases
Table 1: Redox Parameters in Cancer vs. Neurodegenerative Models
| Parameter | Cancer (Glioblastoma Model) | Neurodegeneration (AD Mouse Model) | Measurement Method |
|---|---|---|---|
| ROS Level (Relative) | 2.5 - 4.0 fold increase vs. normal | 1.8 - 2.5 fold increase vs. wild-type | DHE fluorescence, DNP-MRI redox ratio |
| GSH/GSSG Ratio | 5 - 10 (Severely depleted) | 12 - 18 (Depleted) | HPLC assay |
| NADPH/NADP+ Ratio | ~4 (Low) | ~6 (Moderately Low) | Enzymatic cycling assay |
| DNP-MRI Redox Ratio ([AA]/[DHA+AA]) | 0.2 - 0.4 | 0.5 - 0.6 | Hyperpolarized ¹³C MRI |
| Key Altered Enzymes | NRF2 downregulated, NOX4 upregulated | SOD1 activity decreased, GSH peroxidase downregulated | Western blot, activity assays |
Table 2: DNP-MRI Tracers for Redox Imaging
| Tracer | Target Redox Reaction | Reduced Form | Oxidized Form | Key Application |
|---|---|---|---|---|
| [1-¹³C] Pyruvate | Lactate Dehydrogenase (LDH) | [1-¹³C] Lactate | [1-¹³C] Pyruvate | Warburg effect, general metabolism |
| [1-¹³C] Dehydroascorbic Acid (DHA) | Glutathione-dependent reduction | [1-¹³C] Ascorbic Acid (AA) | [1-¹³C] DHA | Primary redox ratio indicator |
| [¹³C] Cystine | Glutathione synthesis | [¹³C] Cysteine | [¹³C] Cystine | Cystine/glutamate antiporter (xCT) activity |
Experimental Protocols
Protocol 1: DNP-MRI Redox Imaging in a Murine Tumor Model
Objective: To map the redox state within a subcutaneous or orthotopic tumor using hyperpolarized [1-¹³C] DHA.
Materials: See "Scientist's Toolkit" below. Procedure:
- Tracer Preparation: Dissolve 35 mg of [1-¹³C] DHA in 1.5 mL of standard glassing matrix (e.g., GE HealthCare's generic polarization matrix). Load into a DNP polarizer (e.g., SPINlab).
- Hyperpolarization: Polarize at ~1.4 K in a 3.35 T magnetic field with microwave irradiation for ~1-2 hours, targeting a polarization level >20%.
- Dissolution & Injection: Rapidly dissolve the hyperpolarized sample in 6 mL of pre-heated, buffered, sterile saline (pH ~7.4). Draw 0.3 mL (final dose ~75 mM/kg) into a sterile syringe. Inject intravenously into the mouse via a tail-vein catheter as a rapid bolus (<3 sec).
- MRI Acquisition: Place animal in MRI scanner (e.g., 7T Agilent/ Bruker). Initiate a dynamic ¹³C spectroscopic imaging sequence (e.g., EPSI or spectral-spatial flyback sequence) 5 seconds post-injection. Key parameters: TR = 50-100 ms, spectral width = 400 Hz, matrix = 16x16, FOV = 30x30 mm.
- Data Analysis: Fit the spectral peaks for [1-¹³C] AA (~185 ppm) and [1-¹³C] DHA (~174 ppm) in each voxel over time. Calculate the Redox Ratio (RR) as: RR = AUC(AA) / [AUC(AA) + AUC(DHA)], where AUC is the area under the time-course curve for each metabolite.
Protocol 2: Ex Vivo Validation of Redox State via Biochemical Assay
Objective: To correlate DNP-MRI redox ratios with tissue biochemical measurements of glutathione.
- Immediately after DNP-MRI, euthanize the animal and rapidly extract the tumor and contralateral control tissue.
- Homogenize tissue in cold 5% metaphosphoric acid.
- Centrifuge at 10,000 x g for 10 min at 4°C.
- Assay the supernatant for total glutathione (GSH+GSSG) and oxidized glutathione (GSSG) using a commercial enzymatic recycling assay (e.g., Cayman Chemical kit #703002).
- Calculate the GSH/GSSG ratio: (Total GSH - 2*GSSG) / GSSG. Plot this ratio against the DNP-MRI-derived Redox Ratio for correlation analysis.
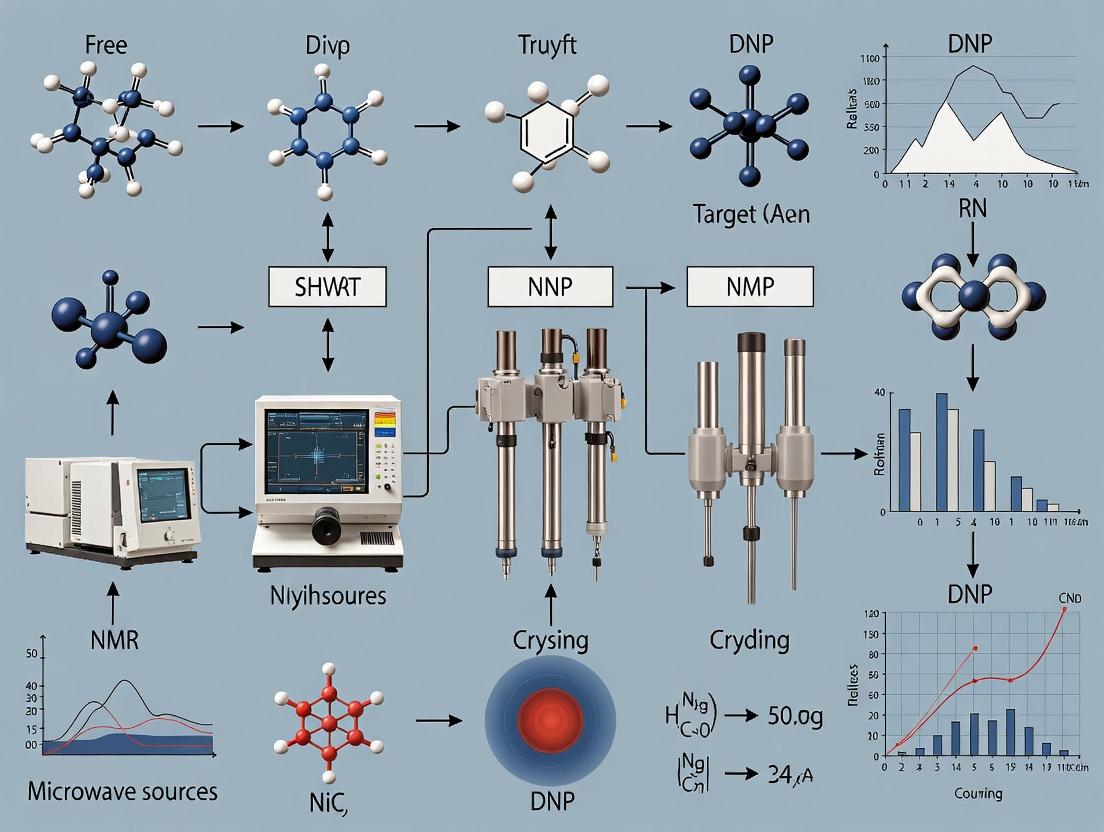
Diagrams
Title: Redox Imbalance in Cancer Signaling
Title: DNP-MRI Redox Imaging Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for DNP-MRI Redox Research
| Item | Function & Relevance | Example Vendor/Cat. # (Illustrative) |
|---|---|---|
| Hyperpolarizer System | Polarizes ¹³C nuclei to boost MRI signal >10,000-fold. | GE HealthCare SPINlab; Bruker Hypersense. |
| [1-¹³C] Dehydroascorbic Acid (DHA) | Primary redox-sensitive molecular probe for DNP. | Cambridge Isotope Laboratories (CLM-4202). |
| Polarization Matrix | Glassing agent required for efficient DNP. | GE HealthCare (Part of SPINlab consumables). |
| High-Field MRI Scanner | For in vivo acquisition of hyperpolarized ¹³C signals. | Agilent/Bruker 7T-9.4T preclinical systems. |
| GSH/GSSG Assay Kit | Gold-standard biochemical validation of redox state. | Cayman Chemical #703002. |
| Dihydroethidium (DHE) | Cell-permeable fluorescent probe for superoxide detection. | Thermo Fisher Scientific D11347. |
| Anti-NRF2 Antibody | Validate NRF2 pathway involvement via Western blot. | Cell Signaling Technology #12721. |
| NOX4 Inhibitor (e.g., GKT137831) | Tool compound to manipulate redox state in models. | MedChemExpress HY-12205. |
This Application Note details the implementation of Dynamic Nuclear Polarization (DNP)-MRI for probing cellular redox metabolism. This content supports a broader thesis investigating the DNP-MRI system as a non-invasive, quantitative tool for imaging redox state dynamics in vivo, with direct applications in cancer metabolism research, neurodegenerative disease profiling, and therapeutic response monitoring in drug development.
Key Sensitivity Comparison: Conventional vs. Hyperpolarized MRI
The fundamental limitation of conventional MRI is its low sensitivity, stemming from the tiny population difference between nuclear spin states at thermal equilibrium. Hyperpolarization techniques, like DNP, transiently boost this signal by >10,000-fold.
Table 1: Quantitative Comparison of Sensitivity Parameters
| Parameter | Conventional ¹³C MRI | DNP-Hyperpolarized ¹³C MRI | Gain Factor |
|---|---|---|---|
| Signal-to-Noise Ratio (SNR) for [1-¹³C]pyruvate | ~1 (baseline) | >10,000 | >10,000x |
| Polarization Level | ~0.001% (at 3T, 37°C) | >20% (typical) | >20,000x |
| Required Sample Concentration | >100 mM (often impractical) | <10 mM (biologically relevant) | >10x reduction |
| Temporal Resolution for Metabolic Imaging | Minutes to hours | Seconds to 2-3 minutes | ~100x improvement |
| Typical Acquisition Window | Unlimited (steady state) | ~5 * T₁ (e.g., ~2-5 min for ¹³C-pyruvate) | Transient observation |
Core Principle: The DNP Workflow for Redox Imaging
DNP transfers the high polarization of unpaired electrons to target nuclei (e.g., ¹³C, ¹⁵N), followed by rapid dissolution and injection for real-time metabolic MRI.
Diagram Title: DNP-MRI Workflow for Metabolic Redox Imaging
Featured Protocol: Hyperpolarized [1-¹³C]Pyruvate MRI for Redox State Assessment
This protocol measures the lactate dehydrogenase (LDH)-catalyzed conversion of pyruvate to lactate, reflecting the NADH/NAD⁺ redox state.
Title: In Vivo Redox Imaging in a Murine Tumor Model using HP [1-¹³C]Pyruvate.
Objective: To quantify the conversion rate (kPL) of hyperpolarized [1-¹³C]pyruvate to [1-¹³C]lactate as a biomarker of altered cellular redox state in response to a therapeutic intervention.
Materials & Reagents:
- [1-¹³C]Pyruvic acid with trityl radical (e.g., OX063 or GE9190).
- DNP polarizer (e.g., HyperSense/SPINlab, Bruker, GE).
- 3T or higher preclinical MRI scanner with dual-tuned ¹H/¹³C coils.
- Murine tumor model (e.g., subcutaneously implanted cancer cells).
- Physiological buffer for dissolution (40 mM Tris, 100 mg/L EDTA, pH ~7.4-7.8).
- Catheter for tail-vein injection.
Procedure:
- Sample Preparation: Mix 35 mg of [1-¹³C]pyruvic acid with 15 mM trityl radical. Load into a DNP sample cup.
- Hyperpolarization: Insert cup into polarizer. Irradiate with microwave (94 GHz for 3.35T polarizer) at ~1.2 K for 60-90 minutes to achieve polarization >20%.
- Dissolution: Upon completion, rapidly dissolve with 6 mL of pre-heated, pressurized dissolution buffer (resulting in ~80 mM, pH ~7.4-7.8 pyruvate solution).
- Animal Preparation: Anesthetize tumor-bearing mouse. Secure tail-vein catheter. Position animal in MRI scanner bed with temperature monitoring.
- Injection & Acquisition:
- Rapidly inject 200 µL of HP solution over ~10 seconds.
- Simultaneously initiate a dynamic ¹³C spectroscopic-imaging sequence (e.g., IDEAL spiral, EPSI) covering the tumor.
- Acquisition parameters: TR = 3 s, spectral width = 500 Hz, matrix = 8x8 or 16x16, FOV = 30x30 mm, temporal resolution ~3-6 s, total acquisition = 60-120 s.
- Data Analysis:
- Fit time-resolved spectral peaks for pyruvate (171 ppm) and lactate (185 ppm).
- Calculate area-under-curve (AUC) ratios: Lactate/Pyruvate.
- Model conversion kinetics using a two-site exchange model to derive the apparent rate constant kPL.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for HP ¹³C Redox Imaging Experiments
| Item | Function & Critical Notes |
|---|---|
| [1-¹³C]Pyruvic Acid (with radical) | The primary metabolic substrate. Radical (e.g., trityl OX063) enables DNP. Must be stored and handled under inert atmosphere. |
| Polarizing Agent (e.g., Trityl OX063) | Stable radical that mediates electron-to-nucleus polarization transfer under microwave irradiation. |
| Dissolution Buffer (Tris/EDTA) | Provides biocompatible, pH-stabilized medium for rapid dissolution. High purity is critical to preserve polarization. |
| Quality Control NMR System | Low-field NMR spectrometer integrated into polarizer to measure polarization level pre-dissolution (target >20%). |
| Dual-Tuned ¹H/¹³C RF Coil | MRI coil enabling anatomical ¹H imaging and sensitive ¹³C detection of metabolic signals. |
| Pyruvate-to-Lactate Kinetic Modeling Software | Custom or commercial software (e.g., MATLAB toolkit, MINT) to fit dynamic data and extract kPL. |
Metabolic Pathway Visualization: HP Pyruvate in Redox Metabolism
The lactate/pyruvate ratio is in equilibrium with the cytosolic NADH/NAD⁺ ratio via LDH, providing a direct readout of cellular redox state.
Diagram Title: HP Pyruvate Metabolism Linked to NADH/NAD⁺ Redox State
Advanced Application Protocol: Assessing Therapeutic Response
Title: Quantifying Early Redox Modulation in Tumors Post-Oxidative Stress Therapy.
Objective: To detect an increase in the lactate/pyruvate ratio (kPL) as an early indicator of reductive stress following administration of a pro-oxidant therapeutic.
Protocol Modifications from Section 4:
- Study Arms: Include control and treated animal cohorts (n≥5).
- Timing: Perform baseline HP MRI, administer drug, then follow-up HP MRI at 24h and 48h.
- Enhanced Analysis:
- Generate voxel-wise maps of kPL and lactate/pyruvate AUC ratio.
- Co-register with ¹H anatomical images for region-of-interest analysis in tumor core vs. periphery.
- Perform statistical comparison (e.g., Student's t-test) of mean kPL between cohorts at each time point.
Expected Outcome: A significant increase in the lactate/pyruvate ratio in treated tumors, indicating a compensatory shift to a more reduced state, detectable prior to changes in tumor volume.
Within the broader thesis on developing a Dynamic Nuclear Polarization Magnetic Resonance Imaging (DNP-MRI) system for redox imaging research, this document details the critical application notes and protocols. This workflow is central to non-invasively mapping tissue redox status, a key biomarker in cancer, neurodegenerative diseases, and drug efficacy studies. The protocol encompasses the preparation and injection of the polarizing radical, the in vivo polarization process, and the acquisition of redox-sensitive images.
Core Workflow and Signaling Pathways
2.1 Diagram: DNP-MRI Redox Imaging Workflow
2.2 Diagram: Key Redox Reaction of Nitroxide Radicals
Detailed Experimental Protocols
3.1 Protocol A: Preparation and Quality Control of Nitroxide Radical Probe Objective: To prepare a sterile, biocompatible solution of a nitroxide radical (e.g., 3-Carbamoyl-PROXYL, ³¹P-labeled trityl radical) for in vivo injection.
- Weighing: Under inert atmosphere if needed, weigh 5-10 mg of radical powder into a sterile vial.
- Dissolution: Reconstitute in 1-2 mL of sterile, isotonic saline (0.9% NaCl) or phosphate-buffered saline (PBS). Vortex for 2 minutes.
- Filtration: Pass the solution through a 0.22 μm sterile syringe filter into a new, pyrogen-free vial.
- QC - Concentration Verification: Measure UV-Vis absorbance at the characteristic peak (e.g., ~245 nm for PROXYL). Compare to a standard curve for precise concentration determination. Target injection concentration: 50-200 mM.
- QC - Electron Paramagnetic Resonance (EPR): Confirm radical integrity and measure initial concentration. A single, sharp EPR signal indicates purity.
3.2 Protocol B: In Vivo DNP and Rapid Transfer for MRI Objective: To polarize nuclear spins (¹H or ³¹P) in vivo and rapidly transfer the animal to the MRI scanner for image acquisition.
- Animal Placement: Anesthetize the animal (e.g., using isoflurane) and position it within the low-field DNP polarizer.
- Radical Injection: Administer the prepared radical solution via tail vein (IV) or intraperitoneal (IP) route at a dose of 0.1-0.3 mmol/kg body weight.
- DNP Polarization: Apply a low-frequency microwave irradiation (e.g., ~94 GHz for 0.35 T) for a predetermined time (typically 30-90 seconds) to transfer electron polarization to nuclei.
- Fast Transfer: Immediately cease irradiation and rapidly transfer the animal to the isocenter of the high-field (e.g., 7T or higher) MRI scanner. The transfer system must be automated and swift (<3 seconds is ideal).
- Trigger Acquisition: Initiate the MRI acquisition sequence immediately upon confirming animal positioning.
3.3 Protocol C: Redox-Sensitive MRI Acquisition Sequence Objective: To acquire T1-weighted images where signal intensity is modulated by the redox-dependent conversion of the nitroxide radical.
- Sequence Selection: Use a rapid, T1-weighted gradient echo sequence (e.g., Fast Low Angle Shot - FLASH).
- Pre-Injection Baseline: Acquire a set of baseline images before radical injection.
- Post-Injection Time Series: Initiate repeated acquisition immediately after transfer. Typical parameters: TR/TE = 50/2.5 ms, flip angle = 30°, matrix = 128x128, slice thickness = 1-2 mm.
- Dynamic Acquisition: Continue acquisition for 5-10 minutes to capture the signal decay kinetics, which reflect the in vivo reduction rate of the radical.
- Data Export: Export raw k-space or reconstructed image data in DICOM or MATLAB format for analysis.
Table 1: Common Nitroxide Radicals for In Vivo DNP-MRI
| Radical Probe | Target Nucleus | Typical Dose (mmol/kg) | Polarization Time (s) | Key Redox Partner | Notes |
|---|---|---|---|---|---|
| 3-Carbamoyl-PROXYL | ¹H | 0.15 - 0.30 | 60 - 90 | Ascorbate, Mitochondrial Complex I | Widely used, well-characterized kinetics. |
| ³¹P-labeled Trityl | ³¹P | 0.05 - 0.15 | 30 - 60 | Oxygen, Cytochrome P450 | Direct ³¹P detection, very long T₁, oxygen sensitive. |
| Tetraethylisoindoline | ¹H | 0.10 - 0.25 | 45 - 75 | Glutathione (GSH) | Higher stability in biological systems. |
Table 2: Typical DNP-MRI Acquisition Parameters (Rodent, 7T Scanner)
| Parameter | Value Range | Purpose/Impact |
|---|---|---|
| Microwave Frequency | 93.8 - 94.2 GHz | Matches EPR frequency of radical at polarizer field. |
| Polarizer Field Strength | 0.35 T (approx.) | Optimal for nitroxide radicals. |
| MRI Field Strength | 7.0 T | Provides high SNR and spectral resolution. |
| TR/TE (FLASH) | 40-100 ms / 1.5-3 ms | Optimizes T1-weighting and speed. |
| Temporal Resolution | 5 - 15 seconds/frame | Captures rapid redox dynamics. |
| Signal Enhancement (ϵ) | 50 - 200-fold | Compared to thermal polarization at 7T. |
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Materials and Reagents for DNP-MRI Redox Imaging
| Item | Function/Benefit | Example Product/Catalog # |
|---|---|---|
| Nitroxide Radical (e.g., 3-CP) | Polarizing agent; redox sensor whose metabolism alters MRI contrast. | Toronto Research Chemicals (TRC), C-570000. |
| Sterile Saline (0.9% NaCl) | Isotonic vehicle for radical dissolution and injection. | Baxter, 2F7124. |
| 0.22 μm Syringe Filter | Ensures sterility and removes particulate matter from radical solution. | Millipore Sigma, SLGP033RS. |
| Isoflurane | Volatile anesthetic for animal immobilization during DNP/MRI. | Piramal Critical Care, NDC 66794-017-25. |
| MRI-Compatible Monitoring System | Monitors physiology (temp, respiration) during scanning. | SA Instruments, Model 1025. |
| Phantoms for Calibration | Contains known radical concentrations for signal normalization. | Custom agarose phantoms with NiCl₂ for T1 shortening. |
| Image Analysis Software | Processes dynamic MRI data to generate parametric redox maps. | MATLAB with custom scripts, PMOD, Horos. |
Dynamic Nuclear Polarization Magnetic Resonance Imaging (DNP-MRI) is a transformative hyperpolarization technique that dramatically increases the sensitivity of MRI, enabling real-time metabolic and redox imaging in vivo. The core principle involves polarizing exogenous paramagnetic probes (radicals) at cryogenic temperatures and transferring this enhanced polarization to nuclei (e.g., ^13C, ^15N) upon dissolution. For redox imaging, the metabolic fate of these radicals themselves becomes the contrast mechanism. Nitroxides and trityl radicals are two pivotal classes of redox-sensitive probes, each with distinct chemical and metabolic properties that define their utility in imaging oxidative stress, tissue oxygenation, and aberrant redox metabolism associated with diseases like cancer, ischemia, and neurodegeneration. This article details their application notes and experimental protocols within a DNP-MRI research framework.
Table 1: Key Characteristics of Nitroxide and Trityl Radical Probes
| Property | Nitroxides (e.g., TEMPOL, 3CP) | Trityl Radicals (e.g., OX063, Finland Trityl) |
|---|---|---|
| Core Structure | Cyclic nitroxide (>N–O•) | Triarylmethyl radical (CAr3•) |
| Primary Redox Reaction | Reduction to diamagnetic hydroxylamine (>N–OH) | Reversible reduction to diamagnetic hydroderivative |
| Key Redox Partner | Primarily ascorbate, glutathione, mitochondrial complexes | Primarily molecular oxygen (O₂), acting as an oxygen sensor |
| Half-life in Blood (in vivo) | Short (~minutes) | Long (~hours) |
| EPR Linewidth | Broader (~1-2 G) | Extremely narrow (<200 mG) |
| DNP Performance | Good polarization, but broad EPR line requires wideband irradiation | Excellent, very narrow EPR line allows efficient, uniform microwave irradiation |
| Primary Imaging Readout | Rate of signal decay reports on reducing capacity | T1 or linewidth changes report on pO₂ |
| Key Metabolic Pathways | Enzymatic (e.g., cytochrome P450, oxidoreductases) and non-enzymatic one-electron reduction | Reversible, non-enzymatic one-electron reduction by oxygen |
Table 2: Representative In Vivo Redox Parameters Measured
| Probe | Model System | Measured Parameter | Typical Value | Biological Implication |
|---|---|---|---|---|
| 3-CP | Murine tumor | Reduction Rate Constant (k) | 0.1 - 0.5 min⁻¹ | Higher k indicates more reducing environment |
| TEMPOL | Ischemic heart | Reduction Half-life (t₁/₂) | ~30-60 sec | Shorter t₁/₂ in ischemic tissue |
| OX063 Trityl | Tumor xenograft | pO₂ (via T1 oximetry) | 1-20 mmHg | Identifies hypoxic tumor regions |
| Finland Trityl | Brain ischemia | Oxygen Consumption Rate (OCR) | 2-10 µM O₂/s | Quantifies metabolic disruption |
Experimental Protocols
Protocol 1: In Vivo Redox Mapping Using Nitroxide DNP-MRI
Objective: To image the spatial distribution of reducing capacity in a tumor model using a nitroxide probe.
Materials: See "Scientist's Toolkit" (Section 5).
Procedure:
- Probe Preparation & Polarization:
- Dissolve 15 mM of deuterated nitroxide (e.g., 3CP-d₁₇) in a 50/50 v/v glycerol/water mixture with 5 mM of an oxidation agent (e.g., K₃[Fe(CN)₆]).
- Load the sample into a commercial DNP polarizer (e.g., HyperSense, SPINlab).
- Irradiate with microwaves (~94 GHz) at ~1.2 K for >1 hour to build polarization.
Dissolution & Injection:
- Dissolve the polarized sample in ~4 mL of superheated, pressurized buffer (pH ~7.4).
- Rapidly transfer the solution (~10 mL/s) to a sterile vial.
- Within 5-10 seconds, administer a bolus injection (typically 0.2 mL/kg) into the tail vein of an anesthetized, tumor-bearing mouse positioned in the MRI scanner.
MRI Acquisition:
- Use a fast gradient-echo or balanced SSFP pulse sequence.
- Initiate a dynamic series of ^13C images immediately upon injection.
- Acquisition Parameters (example): TR/TE = 3.5/1.5 ms, flip angle = 10°, matrix = 32x32, slice thickness = 5 mm, temporal resolution = 3-5 s.
Data Analysis:
- Fit the signal intensity decay (S(t)) for each voxel to a mono-exponential model: S(t) = S₀ * exp(-k * t), where k is the first-order reduction rate constant.
- Generate parametric maps of k and S₀.
Protocol 2: Tissue Oxygenation Mapping via Trityl Radical T1 Oximetry
Objective: To quantify spatial pO₂ in tissues using the oxygen-dependent T1 of a trityl radical.
Materials: See "Scientist's Toolkit" (Section 5).
Procedure:
- Polarization: Polarize a 15 mM solution of OX063 trityl radical in a DNP polarizer as described in Protocol 1, Step 1.
Injection & Distribution: Inject the dissolved, polarized probe intravenously. Allow 1-2 minutes for systemic distribution.
T1 Mapping Acquisition:
- Acquire a series of ^13C images using an inversion-recovery or variable flip angle (VFA) sequence.
- For inversion recovery: Use a non-selective adiabatic inversion pulse followed by imaging readouts at progressively increasing inversion times (TIs).
- Typical Parameters: 8-10 TIs ranging from 1 s to 60 s.
Calibration & Analysis:
- Fit signal recovery curves for each voxel to the T1 recovery model to extract T1.
- Convert T1 to pO₂ using a pre-determined calibration curve specific to the probe and temperature: pO₂ = (1/T1 - 1/T1₀) / ξ, where T1₀ is the T1 under anoxic conditions and ξ is the oxygen relaxivity of the probe (measured ex vivo).
Visualization of Pathways & Workflows
Diagram Title: DNP-MRI Redox Imaging Workflow with Probe Pathways
Diagram Title: Nitroxide-Ascorbate Redox Reaction
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for DNP-MRI Redox Imaging Experiments
| Item / Reagent | Function & Rationale |
|---|---|
| Deuterated Nitroxide (e.g., 3CP-d₁₇) | Extends in vivo half-life by slowing non-redox degradation; essential for obtaining sufficient imaging time window. |
| Trityl Radical (e.g., OX063) | Stable, narrow-line radical for high DNP efficiency and precise pO₂ mapping via T1 oximetry. |
| DNP Polarizer (SPINlab/HyperSense) | Instrument to achieve hyperpolarization via microwave irradiation at cryogenic temperatures. |
| Polarization Matrix (Glycerol/D₂O) | Glass-forming solvent for polarization; deuteration reduces ^1H background and improves polarization. |
| Oxidation Agent (K₃[Fe(CN)₆]) | Added to nitroxide samples to scavenge reducing impurities, preserving radical integrity during polarization. |
| Buffered Saline (pH 7.4) | Isotonic, physiologically compatible dissolution medium for rapid injection. |
| 13C RF Coil (Dual-tune ^1H/^13C) | MRI hardware optimized for sensitive detection of the hyperpolarized ^13C signal. |
| Inversion-Recovery Pulse Sequence | MRI pulse sequence programmed to accurately measure the T1 relaxation time of the trityl probe. |
| Animal Monitoring System | Maintains physiological stability (temp, respiration) during imaging, which is critical for reproducible redox data. |
Within the broader thesis on developing a Dynamic Nuclear Polarization Magnetic Resonance Imaging (DNP-MRI) system for redox imaging, this work focuses on a critical mechanistic link: the quantifiable relationship between the longitudinal relaxation time (T1) of a paramagnetic contrast agent and the local reducing capacity of tissue. The core principle is that the T1 of redox-sensitive radicals (e.g., nitroxides, trityl radicals) is directly modulated by their chemical reduction to diamagnetic, MRI-silent species. By imaging T1 decay, one can spatially map redox status, a key biomarker in cancer, neurodegenerative diseases, and drug development.
Core Chemical Principles & Signaling Pathways
The signal decay (shortening of T1) of a paramagnetic probe is governed by its electron spin relaxation. In a reducing environment, the probe undergoes biochemical reduction (e.g., nitroxide to hydroxylamine), losing its paramagnetism. This chemical decay pathway directly competes with and enhances the physical T1 relaxation pathway.
Diagram Title: Pathways of Paramagnetic Probe Signal Modulation
Application Notes: Quantitative Relationships
The observed longitudinal relaxation rate (R1obs = 1/T1obs) in the presence of reduction is a sum of the physical and chemically driven rates:
R1obs = R1phys + k_red
where k_red is the first-order reduction rate constant, proportional to the local concentration of reducing equivalents. In a DNP-MRI experiment, the hyperpolarized signal intensity S(t) following a radiofrequency pulse is given by:
S(t) = S0 * exp(-t / T1obs)
Tracking S(t) voxel-wise allows for the calculation of parametric T1obs maps, which are subsequently converted to maps of k_red or "Reducing Capacity."
Table 1: Key Redox-Sensitive Probes and Their Reduction Properties
| Probe Name | Class | Redox Potential (mV) | Primary Reductant | T1 @ 1.5T, 37°C (ms) | Key Application |
|---|---|---|---|---|---|
| 3CP | Trityl Radical | -450 vs NHE | Ascorbate, Mitochondrial Q pool | ~20-30 (oxidized) | Hypoxic tumor metabolism |
| TEMPO | Nitroxide | ~+800 vs NHE | Ascorbate, CYP450 enzymes, Thioredoxin | ~100-200 (oxidized) | Generalized tissue redox |
| 4-Hydroxy-TEMPO | Nitroxide | ~+800 vs NHE | Ascorbate | ~150-250 (oxidized) | Oxidative stress models |
| ¹⁵N-PDT | ¹⁵N-labeled Nitroxide | +760 vs NHE | Glutathione/Thioredoxin systems | Varies | High-resolution redox mapping |
Table 2: Representative Reduction Rate Constants (k_red) in Biological Systems
| Biological Context | Probe Used | Estimated k_red (s⁻¹) | Method | Implication for T1 |
|---|---|---|---|---|
| Normal Liver Tissue | 3CP | 0.15 - 0.25 | DNP-MRI | T1obs ~ 4-5 ms |
| Hepatocellular Carcinoma | 3CP | 0.05 - 0.10 | DNP-MRI | T1obs ~ 8-12 ms |
| Ischemic Myocardium | TEMPO | 0.8 - 1.2 | Overhauser MRI | T1obs ~ 0.8-1.2 s |
| Normoxic Tumor (9L glioma) | 4-Hydroxy-TEMPO | 0.3 - 0.5 | Time-resolved EPR | - |
| Cell Lysate (High GSH) | ¹⁵N-PDT | 1.5 - 2.5 | NMR Spectroscopy | - |
Detailed Experimental Protocols
Protocol 1: In Vitro Calibration of T1 vs. Reductant Concentration
Objective: Establish a calibration curve relating observed T1 to the concentration of a specific reductant (e.g., ascorbate).
Materials: See Scientist's Toolkit. Procedure:
- Prepare a series of 10 phosphate-buffered saline (PBS, pH 7.4) solutions containing a fixed concentration of your paramagnetic probe (e.g., 100 µM 3CP).
- Spike each solution with a known, varying concentration of sodium ascorbate (0, 10, 50, 100, 250, 500, 1000 µM). Keep solutions on ice to prevent premature decay.
- For each solution, rapidly transfer to a pre-warmed (37°C) NMR tube and insert into the MRI scanner or NMR spectrometer.
- Acquire T1 using an inversion-recovery or variable flip angle fast low-angle shot (VFA-FLASH) sequence.
- Inversion-Recovery: Use inversion times (TI) from 1 ms to 5 * T1phys (e.g., 1, 10, 50, 100, 250, 500, 1000, 2000 ms).
- VFA-FLASH: Use at least 5 flip angles (e.g., 2°, 5°, 10°, 15°, 20°) with a long TR > 5*T1.
- Fit the signal recovery (IR) or signal vs. flip angle (VFA) data to extract T1obs for each ascorbate concentration.
- Plot 1/T1obs vs. [Ascorbate]. The slope yields the second-order rate constant, enabling the conversion of in vivo T1 maps to quantitative ascorbate-equivalent reducing capacity.
Protocol 2: In Vivo DNP-MRI Redox Imaging Workflow
This protocol outlines the core steps for acquiring T1-based redox maps in an animal model using a hyperpolarized probe.
Diagram Title: DNP-MRI Redox Imaging Experimental Workflow
Detailed Steps:
- Polarization: Load ~20 µL of 15 mM trityl radical (e.g., 3CP) solution mixed with a polarization agent (e.g., OX063) into a DNP polarizer. Irradiate with microwaves at ~1.4 K and 6.7 T for >1 hour to achieve polarization levels >20%.
- Dissolution & Injection: Rapidly dissolve the polarized sample in ~4 mL of superheated, buffered solution. Immediately inject the bolus intravenously into the anesthetized animal (e.g., mouse tumor model) over ~2-3 seconds.
- Dynamic Imaging: Initiate a dynamic, multi-slice T1-weighted imaging sequence on the MRI scanner (e.g., 3T preclinical system) at the time of injection. Sequence Example (FLASH): TR/TE = 3.0/1.5 ms, flip angle = 10°, matrix = 64x64, FOV = 30x30 mm, slice thickness = 2 mm, temporal resolution = 2-3 seconds. Acquire data for 2-3 minutes.
- Data Processing:
- For each voxel, plot signal intensity S(t) over time.
- Fit the decay curve to the equation: S(t) = S0 * exp(-t / T1obs) + C, where C accounts for background signal.
- Generate a parametric map of T1obs (in milliseconds).
- Redox Map Calculation:
- Using the calibration constant from Protocol 1, convert the T1obs map to a map of the apparent reduction rate constant: kred map = (1 / T1obs map) - R1phys. Assume R1phys is constant (measured in vitro without reductants).
- The kred map is directly interpreted as a Reducing Capacity Map.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for T1-Based Redox Imaging
| Item | Function & Rationale | Example Product/Source |
|---|---|---|
| Redox-Sensitive Radical | Serves as the paramagnetic T1 sensor. Trityls offer low redox potential for hypoxia; nitroxides are broader spectrum. | 3-Carboxy-PROXYL (3CP), Oxo63 Trityl (GE HealthCare), 4-Hydroxy-TEMPO (Sigma-Aldrich) |
| Polarizing Agent (for DNP) | Doped into radical solution to enhance polarization via the cross-effect mechanism. | Trityl OX063 (for trityls), TEMPO (for nitroxides) |
| DNP Polarizer | Instrument to hyperpolarize nuclei, providing the massive signal enhancement required for in vivo tracer imaging. | HyperSense (Oxford Instruments), SpinLab (GE HealthCare) |
| Reductant Standards | For in vitro calibration of T1 response. Ascorbate and NADH are biologically relevant. | L-Ascorbic acid, Sodium salt (Sigma-Aldrich), β-Nicotinamide adenine dinucleotide (NADH) |
| Physiological Buffer | Maintains pH and ionic strength for in vitro experiments and dissolution. | Dulbecco's Phosphate Buffered Saline (DPBS), pH 7.4 |
| Biological Reductant Quencher | To "freeze" redox state ex vivo for validation. | N-Ethylmaleimide (NEM, thiol blocker), Metaphosphoric acid (stabilizes ascorbate) |
| MRI Contrast Phantom | Contains tubes with known T1 values for scanner calibration. | Eurospin T1/T2 phantom (Diagnostic Sonar) |
| Image Analysis Software | For voxel-wise fitting of dynamic data to exponential decay models. | MATLAB with custom scripts, PMOD, Horos (open-source DICOM viewer) |
Mapping Metabolic Dysfunction: DNP-MRI Protocols and Translational Applications
Step-by-Step Experimental Protocol for Preclinical Redox Imaging
Redox imbalance is a hallmark of numerous pathologies, including cancer, neurodegenerative diseases, and ischemic injury. The integration of Dynamic Nuclear Polarization-Magnetic Resonance Imaging (DNP-MRI) enables the non-invasive, real-time imaging of redox status in vivo by monitoring the metabolic fate of hyperpolarized (HP) probes, such as [1-¹³C]dehydroascorbic acid ([1-¹³C]DHA) or [1-¹³C]pyruvate. This protocol details the stepwise procedure for conducting preclinical redox imaging studies within the framework of a DNP-MRI research thesis, providing application notes for quantitative assessment of tissue redox capacity.
Key Research Reagent Solutions
| Reagent / Material | Function in Redox Imaging | Key Notes |
|---|---|---|
| Hyperpolarized [1-¹³C]Dehydroascorbic Acid ([1-¹³C]DHA) | Primary redox probe. Reduced to [1-¹³C]vitamin C (ascorbate) intracellularly, rate informs redox capacity. | Requires rapid dissolution post-polarization. Sensitive to pH and temperature. |
| Hyperpolarized [1-¹³C]Pyruvate | Metabolic probe. Conversion to [1-¹³C]lactate via LDH informs NADH/NAD⁺ ratio, a redox couple. | Well-established polarization protocol. Provides complementary metabolic/redox data. |
| Trityl OX063 Radical (e.g., AH111501) | Polarizing agent for dissolution DNP. Enables >10,000-fold signal enhancement of ¹³C nuclei. | Must be filtered post-dissolution for in vivo use. |
| Phosphate-Buffered Saline (PBS), pH 7.4 | Dissolution medium for HP agent. Physiological pH and ionic strength are critical. | Must be degassed and pre-heated to ~180°C for dissolution. |
| Anaesthesia System (e.g., Isoflurane/O₂) | Maintains animal physiological stability during long imaging sessions. | Consistent depth is vital for reproducible metabolism. |
| Physiological Monitoring Suite (Temp., ECG, Resp.) | Monitors core temperature and animal viability. Essential for metabolic study validity. | Temperature maintained at 37±0.5°C using warm air. |
| DNP Polarizer (e.g., SPINlab, Hypra) | Hardware for generating the hyperpolarized state via microwave irradiation at ~1K. | Calibration and quality control of polarization levels are mandatory. |
Table 1: Key Quantitative Metrics from HP [1-¹³C]DHA Redox Imaging
| Metric | Formula / Description | Typical Value (Normal Tissue) | Pathological Alteration (e.g., Tumor) |
|---|---|---|---|
| Redox Rate Constant (k_DHA→Asc) | Pseudo-first-order rate from kinetic modeling. | 0.05 - 0.07 min⁻¹ | Often increased (↑ redox demand). |
| Reduced Ascorbate AUC | Area Under Curve of [1-¹³C]Asc signal. | Tissue-dependent | Can be increased or decreased. |
| DHA/Asc Signal Ratio | Peak area ratio at a defined time point (e.g., t=30s). | ~0.5 - 1.5 | Highly variable; context-dependent. |
| T₁ of [1-¹³C]DHA | Longitudinal relaxation time at 3T. | ~20 - 30 s | Can affect apparent kinetics. |
Table 2: Comparative Probe Kinetics in Common Models
| Disease Model | Preferred HP Probe | Expected Kinetic Change (vs Control) | Primary Redox Information |
|---|---|---|---|
| Glioblastoma | [1-¹³C]DHA | ↑ k_DHA→Asc | Increased glutathione-mediated recycling. |
| Prostate Cancer | [1-¹³C]Pyruvate | ↑ k_Pyr→Lac | Increased lactate production, correlated with NADH. |
| Hepatic Ischemia-Reperfusion | [1-¹³C]DHA | ↓ k_DHA→Asc, ↓ Asc AUC | Loss of redox capacity, depletion of antioxidants. |
| Diabetic Kidney Disease | [1-¹³C]Pyruvate | Altered Pyr/Lac ratio | Shift in cytosolic redox state (NADH/NAD⁺). |
Detailed Experimental Protocol
Part A: Pre-Imaging Preparation (Day -1 to Day 0)
- Animal Model Preparation: Induce relevant pathology (e.g., tumor xenograft, ischemia). Include healthy controls. Fast animals for 4-6 hours prior to imaging to standardize basal metabolism.
- Probe Preparation: Prepare 40 mM [1-¹³C]DHA or [1-¹³C]pyruvate mixed with trityl radical in glycerol-water glassing matrix. Load into sample cup for the polarizer.
- MRI System Preparation: Calibrate the ¹³C transmit gain and center frequency on a ¹³C-enriched acetate phantom. Configure multinuclear (¹H/¹³C) acquisition sequences.
Part B: Hyperpolarization and Dissolution (Day of Experiment)
- Polarization: Insert sample into SPINlab polarizer. Polarize at ~1.4 K and 5 T for [1-¹³C]pyruvate (~2-3 hours) or [1-¹³C]DHA (~6-8 hours) to achieve >20% polarization.
- Dissolution: At time T=0, initiate rapid dissolution with 6 mL of superheated, degassed PBS (180°C, 10 bar). Resulting solution is ~80 mM, physiological temperature and pH.
- Quality Control: Immediately measure polarization level via solid-state NMR in the quality control station. Filter solution through a 0.2 μm sterile filter into a sterile syringe.
Part C: Animal Administration and Data Acquisition (Day of Experiment)
- Animal Setup: Anesthetize animal (e.g., 1-2% isoflurane in O₂). Place in MRI cradle with warming system. Secure tail vein catheter for HP injection.
- Baseline Anatomical ¹H MRI: Acquire high-resolution T2-weighted ¹H images for anatomical co-registration.
- HP ¹³C Data Acquisition:
- At T = 10s post-dissolution, start dynamic spectroscopic or imaging sequence.
- At T = 15s, manually or automatically inject HP agent via tail vein as a rapid bolus (~0.2 mL/sec, total dose 0.3 mmol/kg).
- Acquire dynamic data for 2-3 minutes. A typical pulse sequence is a low-flip-angle spectral-spatial excitation with 2D-3D EPSI or spiral readout for imaging, or single-voxel spectroscopy for kinetics.
- Sequence Parameters Example: TR=1-3s, temporal resolution 3-6s/frame, spectral width 250-300 Hz, matrix size 16x16 (spectroscopic imaging).
Part D: Data Processing and Analysis
- Spectral Processing: Apply apodization (5-10 Hz line broadening), zero-filling, and Fourier transformation to time-domain data. Perform phasing and baseline correction.
- Quantification: Integrate peak areas for substrate (DHA or pyruvate) and product (ascorbate or lactate) for each time point.
- Kinetic Modeling: Fit the time-resolved data to an appropriate kinetic model (e.g., inputless 2-site exchange model) to extract rate constants (kDHA→Asc, kPyr→Lac) and metabolic maps.
- Co-registration & Statistics: Overlay metabolic parameter maps on ¹H anatomical images. Perform region-of-interest analysis and group-wise statistical testing (t-test, ANOVA).
Visualizations
Preclinical Redox Imaging with DNP-MRI Workflow
HP DHA Reduction Pathway and MRI Detection
This document provides detailed application notes and protocols for quantitative redox imaging analysis, a core methodology within a broader thesis on developing a Dynamic Nuclear Polarization Magnetic Resonance Imaging (DNP-MRI) system for in vivo redox imaging research. DNP-MRI enables the sensitive, real-time detection of redox-sensitive probes, such as nitroxides, whose signal decay (reduction) rates report on the localized reducing capacity of tissue. Calculating spatial redox maps and quantitative reduction rate constants from this data is critical for studying oxidative stress in disease models and evaluating the efficacy of redox-modulating therapeutics.
The primary quantitative outputs from DNP-MRI redox imaging experiments are summarized below.
Table 1: Core Quantitative Redox Metrics
| Metric | Symbol | Unit | Description | Biological Significance |
|---|---|---|---|---|
| Signal Intensity | S(t) | a.u. | Time-dependent voxel intensity from the redox probe. | Direct readout of probe concentration. |
| Initial Intensity | S₀ | a.u. | Signal intensity at time t=0 post-injection. | Related to perfusion and probe delivery. |
| Reduction Rate Constant | k | min⁻¹ | Pseudo-first-order rate constant for signal decay. | Primary measure of local reducing capacity. |
| Half-Life | t₁/₂ | min | Time for signal to reduce to half: ln(2)/k. | Intuitive metric for redox status. |
| Redox Map | - | min⁻¹ or min | Spatial array (image) of k or t₁/₂ values. | Visualizes heterogeneity in redox metabolism. |
Table 2: Typical Reduction Rate Constants in Tissues (Example Data)
| Tissue / Condition | Approx. k (min⁻¹) | Approx. t₁/₂ (min) | Notes (from literature) |
|---|---|---|---|
| Normal Liver | 0.5 - 1.2 | 0.6 - 1.4 | High metabolic/reducing activity. |
| Tumor (Subcutaneous) | 0.1 - 0.3 | 2.3 - 6.9 | Often more hypoxic and reducing. |
| Brain Tissue | 0.05 - 0.2 | 3.5 - 13.9 | Variable by region; blood-brain barrier affects probe delivery. |
| With Antioxidant Treatment | ↓ 20-50% | ↑ 20-50% | Reduction rate decreases as oxidative stress is mitigated. |
| With Pro-oxidant Treatment | ↑ 30-80% | ↓ 30-80% | Reduction rate increases due to elevated reducing equivalents. |
Experimental Protocols
Protocol 3.1:In VivoDNP-MRI Redox Imaging Experiment
Objective: To acquire temporal image data for calculating redox maps and rate constants. Materials: See Scientist's Toolkit (Section 5). Procedure:
- Probe Preparation: Dissolve a nitroxide radical probe (e.g., 3-Carboxy-PROXYL) in PBS to a concentration of 100 mM. Filter sterilize (0.22 µm).
- Animal Preparation: Anesthetize the rodent (e.g., mouse with tumor xenograft) and place it in the MRI scanner with temperature and respiratory monitoring.
- Baseline Scan: Acquire a pre-contrast baseline T1-weighted anatomical image.
- DNP Polarization & Injection: Polarize the probe solution in the DNP polarizer for a predetermined time (~1-2 hours) to achieve sufficient signal enhancement. Rapidly transfer the hyperpolarized solution and inject via tail vein catheter as a bolus (typically 200 µL for a mouse).
- Dynamic Imaging: Initiate a fast, repetitive imaging sequence (e.g., low-flip-angle gradient echo) immediately upon injection. Acquire images every 5-10 seconds for a total duration of 3-5 minutes, capturing the entire signal dynamics.
- Data Export: Export temporal image series in DICOM or similar format for analysis.
Protocol 3.2: Calculation of Reduction Rate Constants and Redox Maps
Objective: To quantitatively analyze temporal signal decay to generate parametric redox maps. Software: MATLAB, Python (NumPy, SciPy), or ImageJ with appropriate plugins. Input Data: 4D Image stack (x, y, z, time) from Protocol 3.1. Procedure:
- Preprocessing:
- Apply spatial registration to correct for animal motion during the time series.
- Perform signal normalization, if required, using a reference region.
- Define a Region of Interest (ROI) in a background area for noise estimation.
- Model Fitting per Voxel:
- For each voxel (i, j), extract the signal intensity time course, S(t).
- Fit the data to a mono-exponential decay model with offset: S(t) = S₀ · exp(-k · t) + C where S₀ is initial intensity, k is the reduction rate constant, and C is a constant offset accounting for background or non-decaying signal.
- Use a non-linear least squares algorithm (e.g., Levenberg-Marquardt) for fitting. Constrain parameters to physiologically plausible ranges (k > 0).
- Calculate the half-life: t₁/₂ = ln(2) / k.
- Generation of Parametric Maps:
- Create a 2D map where the value at each voxel is the fitted k or t₁/₂.
- Apply a mask to exclude voxels with poor fit quality (e.g., low R² value or high uncertainty in k).
- Use a consistent, perceptually uniform color scale (e.g., viridis, plasma) to display the redox map.
- Statistical Analysis:
- Calculate mean and standard deviation of k and t₁/₂ within defined anatomical or pathological ROIs (e.g., tumor vs. contralateral muscle).
- Perform appropriate statistical tests (e.g., student's t-test) to compare groups.
Visualization Diagrams
Title: DNP-MRI Redox Imaging and Analysis Workflow
Title: Signal Decay Model and Redox Map Generation
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents and Materials for DNP-MRI Redox Imaging
| Item | Function in Experiment | Example/Notes |
|---|---|---|
| Nitroxide Radical Probe | The redox-sensitive contrast agent. Its signal is enhanced via DNP and decays in vivo at a rate proportional to reducing capacity. | 3-Carboxy-PROXYL, TEMPOL, or isotopically labeled variants (e.g., 15N). |
| DNP Polarizer | Instrument used to hyperpolarize the probe solution via microwave irradiation at low temperature (~1 K) and high magnetic field, boosting MRI signal by >10,000x. | Commercial systems (e.g., HyperSense, SpinLab). |
| Preclinical MRI Scanner | High-field MRI system for small animals used to acquire anatomical and dynamic images of the hyperpolarized probe distribution. | Typically 7T or higher field strength with rapid imaging capabilities. |
| Sterile Phosphate Buffered Saline (PBS) | Vehicle for dissolving the nitroxide probe. Must be sterile and pyrogen-free for in vivo injection. | -- |
| Filter (0.22 µm) | For sterilizing the probe solution prior to injection. | -- |
| Animal Model | Disease model for studying redox biology (e.g., tumor xenograft, models of inflammation, or ischemia-reperfusion). | Immunocompromised mice for xenografts; transgenic models. |
| Data Analysis Software | For processing 4D image data, performing voxel-wise fitting, and generating parametric maps. | Custom scripts in MATLAB/Python, or software like Mnova (Mestrelab). |
This document provides detailed application notes and protocols for Dynamic Nuclear Polarization Magnetic Resonance Imaging (DNP-MRI) in oncological research, a core component of the broader thesis "Development and Validation of a DNP-MRI System for In Vivo Redox Imaging." The ability to non-invasively and quantitatively image tumor hypoxia and oxidative stress dynamics is critical for evaluating treatment response, particularly for emerging radiotherapy, chemotherapy, and redox-modulating therapies.
Key Quantitative Data on Tumor Microenvironment
Table 1: Key Biomarkers and Imaging Targets in Tumor Hypoxia & Oxidative Stress
| Biomarker/Target | Normal Physiological Range (Approx.) | Tumor/Hypoxic Range (Approx.) | Primary Imaging Significance |
|---|---|---|---|
| Partial Pressure of Oxygen (pO₂) | 20-60 mmHg | <10 mmHg (Hypoxic) | Distinguishes normoxic, hypoxic, and anoxic regions; predicts radioresistance. |
| Reduction Potential (Eh) of Glutathione (GSH/GSSG) | -150 to -200 mV | -100 to -50 mV (More Oxidized) | Integrative measure of cellular oxidative stress and redox buffering capacity. |
| Lactate Concentration | 1-3 mM | Can exceed 15-20 mM | Marker of glycolytic metabolism (Warburg effect) driven by hypoxia. |
| Extracellular pH (pHe) | ~7.4 | 6.5-7.0 (Acidic) | Result of lactate production and poor perfusion; influences drug uptake and efficacy. |
| NAD+/NADH Ratio | High (~700:1 in liver cytosol) | Low (Increased NADH) | Indicator of metabolic shift and mitochondrial dysfunction. |
Table 2: Common DNP-MRI Tracer Agents for Redox & Metabolism Imaging
| Tracer (Isotope) | Hyperpolarized Substrate | Key Metabolic Product(s) | Primary Information Obtained |
|---|---|---|---|
| [1-¹³C]Pyruvate | [1-¹³C]Pyruvate | [1-¹³C]Lactate, [1-¹³C]Alanine, H¹³CO₃⁻ | Lactate dehydrogenase (LDH) activity, glycolytic flux, mitochondrial PDH activity. |
| [¹³C]Urea (¹³C,¹⁵N₂) | [¹³C]Urea | None (Perfusion Agent) | Tumor perfusion and vascular permeability. |
| [1,4-¹³C₂]Fumarate | [1,4-¹³C₂]Fumarate | [1,4-¹³C₂]Malate | Necrosis detection via fumarase activity. |
| [¹³C]Dehydroascorbate (DHA) | [¹³C]DHA | [¹³C]Ascorbate (Vitamin C) | Tissue redox status (glutathione-dependent recycling). |
| ¹⁵N-Choline | ¹⁵N-Choline | ¹⁵N-Phosphocholine, ¹⁵N-GPC | Choline kinase activity, membrane biosynthesis. |
Experimental Protocols
Protocol 1: DNP-MRI of Tumor Glycolytic Flux with [1-¹³C]Pyruvate
Objective: To image real-time conversion of pyruvate to lactate in tumors, assessing hypoxia-driven glycolysis and early treatment response.
Materials: See Scientist's Toolkit below. Procedure:
- Tracer Preparation: Dissolve 35 mg of [1-¹³C]pyruvic acid with 15 mM trityl radical (OX063) in a DNP polarizer cup.
- Hyperpolarization: Insert the sample into a commercial DNP polarizer (e.g., HyperSense/SPINlab). Polarize at ~1.4 K and 94 GHz microwave irradiation for 60-90 minutes to achieve polarization >20%.
- Dissolution: Rapidly dissolve the polarized solid in 4-6 mL of a pre-heated, buffered, chelated dissolution medium (40 mM Tris, 100 mM NaOH, 50 mg/L EDTA). The final solution should be isotonic, pH ~7.6, and at ~37°C.
- Animal/Tumor Model Preparation: Anesthetize the tumor-bearing mouse (e.g., subcutaneous HT-29 or PC-3 xenograft) and place it in the MRI bore, maintaining body temperature at 37°C.
- Injection & Imaging: Rapidly inject 200-300 µL of the hyperpolarized [1-¹³C]pyruvate solution (~80 mM) via tail vein catheter over 10-12 seconds.
- Spectral-Spatial Data Acquisition: Simultaneously initiate a dynamic 2D or 3D spectroscopic MRI sequence (e.g., IDEAL spiral or EPSI). Typical parameters: TR = 50-100 ms, spectral bandwidth = 200-400 Hz, spatial resolution ~3x3x5 mm³, temporal resolution ~3-6 seconds/frame for 60-120 seconds.
- Data Analysis: Use spectral processing software to integrate the peak areas for [1-¹³C]pyruvate, [1-¹³C]lactate, [1-¹³C]alanine, and H¹³CO₃⁻. Generate metabolite maps. Calculate the lactate-to-pyruvate ratio (Lac/Pyr) per voxel over time, and the area-under-the-curve (AUC) ratio as a quantitative metric of LDH activity.
Protocol 2: Assessing Redox Status with [¹³C]Dehydroascorbate (DHA)
Objective: To image tissue glutathione-dependent redox capacity by tracking the reduction of DHA to ascorbate.
Materials: See Scientist's Toolkit below. Procedure:
- Tracer Preparation: Prepare [¹³C]DHA from [¹³C]ascorbic acid via bromination and purification. Mix with trityl radical for polarization.
- Hyperpolarization & Dissolution: Follow steps similar to Protocol 1, using a DNP polarizer. Dissolve in buffered saline.
- Animal Preparation & Injection: Prepare animal model as in Protocol 1. Inject hyperpolarized [¹³C]DHA solution.
- Data Acquisition: Acquire dynamic ¹³C spectra or spectroscopic images. Focus on the chemical shift difference between DHA (~175 ppm) and ascorbate (~157 ppm).
- Data Analysis: Quantify the rate of appearance and total production of [¹³C]ascorbate. The rate constant (k) for DHA reduction is proportional to intracellular glutathione (GSH) concentration and glutathione-dependent reductase activity.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for DNP-MRI Redox Imaging Experiments
| Item | Function/Application | Example/Note |
|---|---|---|
| ¹³C-Labeled Tracer | Substrate for hyperpolarization and metabolic imaging. | [1-¹³C]Pyruvic acid (with radical dopant). Purity >98%. |
| Trityl Radical | Polarizing agent (PAS). Enables signal enhancement via the DNP effect. | OX063 (GE) or Finland trityl. Must be compatible with the tracer. |
| DNP Polarizer | Instrument to hyperpolarize the sample at cryogenic temperatures. | HyperSense (Oxford Instruments) or SPINlab (GE). |
| Dissolution System | Integrated unit to rapidly melt and dissolve polarized sample for injection. | Heated, pressurized solvent reservoir with neutralization buffer. |
| High-Field MRI System | Scanner equipped for multinuclear (¹³C, ¹H) spectroscopy/imaging. | 3T or higher preclinical or clinical MRI with broadband capabilities. |
| Dedicated ¹³C RF Coil | Radiofrequency coil optimized for ¹³C detection. | Volume transmit/receive or surface coil for high sensitivity. |
| Physiological Monitoring | Maintains animal viability and data consistency during long scans. | Heating pad, respiratory monitor, temperature probe. |
| Spectral Analysis Software | For processing dynamic MRSI data and quantifying metabolite ratios. | MATLAB with custom scripts, SIVIC, jMRUI, or commercial vendor software. |
Visualization Diagrams
Title: Hypoxia Signaling to DNP-MRI Readouts
Title: DNP-MRI Experimental Workflow
Title: Pyruvate Metabolism to Treatment Prediction
Within the context of developing a Dynamic Nuclear Polarization Magnetic Resonance Imaging (DNP-MRI) system for in vivo redox imaging, understanding oxidative stress in neurological disorders is paramount. This application note details protocols and insights for probing oxidative stress mechanisms in preclinical models of stroke, Alzheimer's disease (AD), and Parkinson's disease (PD). The quantitative redox state mapping enabled by novel DNP-MRI probes provides a direct, non-invasive method to validate and expand upon the biochemical findings outlined below.
Key Quantitative Data on Oxidative Stress Markers
Table 1: Common Oxidative Stress Biomarkers in Neurological Disease Models
| Biomarker | Stroke Model (MCAO) | AD Model (e.g., 5xFAD) | PD Model (e.g., MPTP) | Measurement Technique |
|---|---|---|---|---|
| Lipid Peroxidation (MDA, nM/mg prot) | 3.5 - 5.2 | 2.8 - 4.1 | 2.1 - 3.6 | TBARS Assay |
| Protein Carbonyls (nmol/mg prot) | 5.8 - 8.3 | 4.5 - 6.7 | 3.9 - 5.5 | DNPH ELISA |
| GSH/GSSG Ratio | 8 - 12 (Sham) → 3 - 6 | 15 - 20 (WT) → 7 - 12 | 18 - 22 (WT) → 9 - 14 | HPLC, Colorimetric |
| SOD Activity (U/mg prot) | 25-30% decrease | 20-25% decrease | 15-20% decrease | Pyrogallol/XTT Assay |
| H2O2 (nM/μg tissue) | 120 - 180 | 80 - 120 | 70 - 100 | Amplex Red Fluorimetry |
Data compiled from recent studies (2022-2024). MCAO: Middle Cerebral Artery Occlusion; WT: Wild-type.
Table 2: Key Signaling Pathways and Molecular Targets
| Pathway/Process | Stroke | Alzheimer's | Parkinson's | Primary Redox Sensor |
|---|---|---|---|---|
| Nrf2/ARE Activation | Strong, acute | Impaired, chronic | Moderate, chronic | Keap1 cysteines |
| NF-κB Signaling | Acute Pro-inflammatory | Chronic Pro-inflammatory | Chronic Pro-inflammatory | IKK complex, p50/p65 |
| Mitophagy/PINK1-Parkin | Secondary damage | Impaired (Aβ/TAU) | Primarily impaired (LRRK2, PINK1) | DJ-1, PINK1 |
| Ferroptosis Drivers | High (Fe2+, LOX) | Moderate (Lipid ROS) | Moderate (α-synuclein) | GPX4, ACSL4 |
| NADPH Oxidase (NOX) Isoform | NOX2, NOX4 | NOX1, NOX2 | NOX2, DUOX1 | p47phox subunit |
Detailed Experimental Protocols
Protocol 1: Assessment of Global Oxidative Stress in Brain Homogenates
Title: Colorimetric/Fluorimetric Assay for Lipid Peroxidation (MDA) and Total Glutathione. Application: Baseline oxidative stress validation across AD, PD, and stroke models pre-DNP-MRI. Materials: See "The Scientist's Toolkit" below. Procedure:
- Tissue Preparation: Euthanize animal and perfuse transcardially with ice-cold PBS. Isolate region-specific brain tissue (e.g., cortex/hippocampus for AD, striatum for PD, ischemic penumbra for stroke). Homogenize (1:10 w/v) in cold RIPA buffer with protease inhibitors. Centrifuge at 12,000g for 15 min at 4°C. Collect supernatant.
- TBARS Assay for MDA: a. Mix 100 μL sample with 200 μL of SDS solution (8.1%), 1.5 mL of acetic acid solution (20%, pH 3.5), and 1.5 mL of TBA solution (0.8%). b. Heat at 95°C for 60 min. Cool on ice. c. Add 1 mL of n-butanol, vortex vigorously, centrifuge at 3000g for 10 min. d. Measure fluorescence of the organic (upper) layer (Ex/Em = 532/553 nm). Quantify against an MDA standard curve.
- Total Glutathione (GSH+GSSG) Assay: a. Deproteinize a separate aliquot of supernatant with an equal volume of 5% metaphosphoric acid, centrifuge. b. For total GSH: Mix 50 μL of deproteinized sample with 150 μL of reaction mix containing 0.3 mM NADPH, 0.6 mM DTNB, and 1 U/mL glutathione reductase in 0.1 M phosphate buffer (pH 7.4). c. Monitor absorbance at 412 nm for 5 min. Calculate concentration from a GSH standard curve.
- Data Normalization: Normalize all values to total protein content (via BCA assay).
Protocol 2: Immunohistochemical Staining for Nitrotyrosine (Marker of Peroxynitrite)
Title: IHC Protocol for Protein Nitration in Fixed Brain Sections. Application: Spatial localization of oxidative damage to correlate with future DNP-MRI redox maps. Procedure:
- Sectioning: Perfuse-fix brains with 4% PFA. Cut 30 μm free-floating sections on a cryostat.
- Antigen Retrieval & Blocking: Treat sections with 0.1 M citrate buffer (pH 6.0) at 80°C for 30 min. Block in 3% BSA + 0.3% Triton X-100 in PBS for 1 hour.
- Primary Antibody Incubation: Incubate with anti-nitrotyrosine rabbit monoclonal antibody (1:500 in blocking buffer) at 4°C for 48 hours.
- Secondary Detection: Wash, incubate with biotinylated anti-rabbit IgG (1:1000) for 2h, then with ABC reagent (Vector Labs) for 1h. Develop with DAB peroxidase substrate. Counterstain with hematoxylin.
- Imaging & Analysis: Image using brightfield microscopy. Quantify staining intensity in regions of interest using ImageJ software (corrected total cell fluorescence method).
Protocol 3: DNP-MRI Probe Validation Protocol UsingEx VivoBrain Slices
Title: Ex Vivo Validation of Redox-Sensitive DNP-MRI Probes. Application: Direct correlation of DNP-MRI signal with biochemical redox state. Procedure:
- Acute Slice Preparation: Prepare 300 μm thick acute brain slices from disease models in ice-cold, carbogenated (95% O2/5% CO2) artificial cerebrospinal fluid (aCSF).
- Probe Loading: Incubate slices with a redox-sensitive nitroxide-based DNP probe (e.g., 1 mM Tempol or hydroxyl-TEMPO analog) in aCSF at 32°C for 30 min under carbogen.
- Oxidative Challenge: Treat slices with a disease-relevant stressor (e.g., 100 μM H2O2 for AD/PD models; oxygen-glucose deprivation for stroke models) for 15 min. Include control slices.
- DNP-MRI Measurement: Rapidly transfer slice to a DNP-MRI compatible sample holder. Acquire Overhauser-enhanced MRI maps at specified time points. Key parameter: DNP enhancement factor (ε) as a function of location.
- Biochemical Correlation: Immediately after MRI, homogenize the slice and perform the GSH/GSSG assay (Protocol 1.3). Correlate the local GSH/GSSG ratio with the local DNP enhancement factor (ε).
Visualizations
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for Oxidative Stress Research in Neurology Models
| Reagent/Material | Supplier Examples | Function in Protocol | Key Consideration for DNP-MRI Integration |
|---|---|---|---|
| TBARS Assay Kit | Cayman Chemical, Sigma-Aldrich | Quantifies lipid peroxidation via malondialdehyde (MDA) adducts. | Provides ground-truth biochemical validation for DNP-MRI lipid redox maps. |
| GSH/GSSG-Glo Assay | Promega | Luminescent detection of glutathione ratios in small tissue samples. | Critical for correlating DNP probe reduction rate with cellular redox buffering capacity. |
| Anti-Nitrotyrosine Antibody | Abcam, MilliporeSigma | IHC detection of protein nitration (peroxynitrite footprint). | Validates spatial patterns of nitrosative stress observed with specific DNP probes. |
| CellROX / MitoSOX Probes | Thermo Fisher | Fluorescent live-cell detection of general/mitochondrial ROS. | Used in parallel in vitro studies to calibrate DNP-MRI probe response to ROS levels. |
| PBN (N-tert-Butyl-α-phenylnitrone) | Tocris, Sigma | Spin trapping agent for ex vivo ESR detection of free radicals. | Serves as a chemical reference and validation tool for nitroxide-based DNP probes. |
| DPI (Diphenyleneiodonium) | Abcam, Sigma | Pharmacological inhibitor of NADPH oxidases (NOX). | Tool to manipulate specific ROS sources pre-DNP-MRI to dissect contributions. |
| RIPA Buffer (with protease inhibitors) | Thermo Fisher, Cell Signaling | Effective tissue lysis for protein and metabolite extraction. | Homogenate quality directly impacts downstream biochemical validation accuracy. |
| Nitroxide Radical Probes (e.g., 3-CP, 4-oxo-TEMPO) | Custom synthesis (e.g., Bridge12), Toronto Research Chemicals | Polarizing agents for DNP-MRI; redox state alters relaxation & enhancement. | Core reagent for DNP-MRI redox imaging. Stability, blood-brain barrier permeability, and reduction kinetics are key. |
| Artificial CSF for Brain Slices | Harvard Apparatus, custom formulation | Maintains physiological ionic environment for ex vivo experiments. | Must be compatible with DNP probe solubility and stability during ex vivo validation. |
This application note details experimental protocols for assessing ischemia-reperfusion injury (IRI) and the efficacy of antioxidant therapies. The work is integral to a broader thesis developing a Dynamic Nuclear Polarization Magnetic Resonance Imaging (DNP-MRI) system for in vivo redox imaging. The primary objective is to establish robust, translatable ex vivo and in vivo models of cardiac IRI to validate DNP-MRI redox probes and quantify the therapeutic modulation of oxidative stress by antioxidant agents.
Table 1: Comparative Efficacy of Antioxidant Therapies in Preclinical IRI Models
| Antioxidant Agent | Model System | Infarct Size Reduction (% vs. Control) | Key Biomarker Change (e.g., Plasma Troponin) | Reference (Year) |
|---|---|---|---|---|
| MitoTEMPO (Mitochondrial-targeted) | In vivo Mouse LAD Ligation | 45-52% | Troponin-I: ↓ 60% | Woodall (2023) |
| N-Acetylcysteine (NAC) | Ex vivo Langendorff Rat Heart | 18-25% | GSH/GSSG Ratio: ↑ 2.5-fold | Le Page (2022) |
| SOD-PEG (Superoxide Dismutase) | In vivo Rat IRI | 30-35% | Superoxide (DHE fluorescence): ↓ 40% | Zhang (2024) |
| Allopurinol (XO Inhibitor) | In vivo Porcine IRI | 20-28% | Xanthine Oxidase Activity: ↓ 70% | Kurakose (2023) |
Table 2: DNP-MRI Redox Probe Characteristics for IRI Imaging
| Probe Name | Redox Target | T1/2 of Hyperpolarized Signal (s) | Key Metabolite Monitored | Potential IRI Application |
|---|---|---|---|---|
| [1-13C] Dehydroascorbate (DHA) | Glutathione (GSH) | 20-30 | Vitamin C (Ascorbate) | Tissue redox capacity mapping |
| [1-13C] Pyruvate | Metabolic Flux | 30-40 | Lactate / Alanine | Anaerobic glycolysis post-ischemia |
| 13C-Urea (Co-polarizer) | Perfusion | 40-60 | Urea | Vascular perfusion defect imaging |
Detailed Experimental Protocols
Protocol 3.1: Ex Vivo Langendorff Heart IRI Model for Antioxidant Screening
- Objective: To assess the direct cardioprotective effects of antioxidants on functional recovery and infarct size in an isolated, buffer-perfused heart.
- Materials: See "Research Reagent Solutions" below.
- Method:
- Anesthetize adult Sprague-Dawley rat (250-300g) and heparinize.
- Rapidly excise the heart and cannulate the aorta for retrograde perfusion with Krebs-Henseleit buffer (95% O2/5% CO2, 37°C, 80 mmHg).
- Stabilize for 20 minutes. Insert a left ventricular balloon to monitor functional parameters: Left Ventricular Developed Pressure (LVDP), +dP/dt, -dP/dt.
- (Global Ischemia): Stop perfusion for 30-35 minutes. Maintain temperature at 37°C.
- (Reperfusion & Treatment): Restart perfusion for 60-120 minutes.
- Control Group: Reperfuse with standard buffer.
- Treatment Group: Administer antioxidant (e.g., 100 µM MitoTEMPO) in buffer for first 15 minutes of reperfusion.
- Infarct Size Measurement: At endpoint, stain with 1% Triphenyltetrazolium Chloride (TTC) for 20 min. Fix in 10% formalin. Calculate infarct area (pale) vs. risk area (red) using planimetry software.
- Biomarker Collection: Collect coronary effluent at defined time points for analysis of Lactate Dehydrogenase (LDH) or Troponin.
Protocol 3.2: In Vivo Myocardial IRI Model for DNP-MRI Validation
- Objective: To induce regional IRI for in vivo evaluation via DNP-MRI and subsequent ex vivo validation.
- Materials: See "Research Reagent Solutions" below. Requires small animal ventilator, ECG monitor, and DNP-MRI system.
- Method:
- Anesthetize and intubate a mouse (C57BL/6, 25-30g). Maintain anesthesia with isoflurane.
- Perform left thoracotomy to expose the heart. Temporarily exteriorize the left anterior descending (LAD) coronary artery.
- Ligate the LAD with a 7-0 silk suture over a PE-10 tubing for 30 minutes to induce ischemia. ECG confirmation: ST elevation.
- Remove the tubing to initiate reperfusion for 24-120 hours.
- DNP-MRI Imaging (at defined reperfusion time): a. Hyperpolarize [1-13C] Pyruvate or DHA via DNP polarizer. b. Rapidly inject the hyperpolarized agent intravenously. c. Acquire dynamic 13C spectroscopic MRI data to map metabolic conversion (e.g., pyruvate→lactate) or redox state.
- Terminal Analysis: After final imaging, euthanize the animal. Excise heart for TTC staining (as in 3.1) or snap-freeze for molecular biology (Western blot for NOX2, SOD2, 4-HNE).
Signaling Pathways & Workflow Diagrams
Title: IRI Oxidative Stress Pathway & Antioxidant Targets
Title: In Vivo IRI Model with DNP-MRI Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for IRI & Antioxidant Research
| Item | Function & Application | Example Vendor/Cat. No. (for reference) |
|---|---|---|
| Krebs-Henseleit Buffer | Physiological salt solution for ex vivo heart perfusion. Provides ions, glucose, and oxygenation. | MilliporeSigma, K3753 |
| Triphenyltetrazolium Chloride (TTC) | Vital dye to stain viable myocardium red; identifies pale infarcted tissue. | MilliporeSigma, T8877 |
| MitoTEMPO | Mitochondria-targeted superoxide scavenger. Key therapeutic in IRI protocols. | Cayman Chemical, 16621 |
| [1-13C] Sodium Pyruvate | Substrate for DNP-MRI. Hyperpolarized to image real-time metabolic flux to lactate. | Cambridge Isotopes, CLM-2440 |
| LAD Occlusion Suture | Polyethylene-silicone tubing or blunt needle used for reversible coronary artery ligation. | InHouse/Research Tools |
| Langendorff Perfusion System | Apparatus for maintaining isolated, beating heart with controlled pressure/flow. | ADInstruments, Hugo Sachs Elektronik |
| cTnI/Troponin ELISA Kit | Quantifies cardiac-specific troponin I in effluent or serum as a biomarker of injury. | Abcam, ab246529 |
| Dihydroethidium (DHE) | Cell-permeable fluorescent probe for superoxide detection in tissue sections. | Thermo Fisher, D11347 |
| Hyperpolarizer (DNP System) | Instrument to dramatically enhance NMR signal of 13C probes for in vivo imaging. | Bruker, GE Healthcare |
This application note is framed within a broader thesis advocating for the development and standardization of Dynamic Nuclear Polarization Magnetic Resonance Imaging (DNP-MRI) as a platform for in vivo redox imaging. A central challenge in developing redox-modulating drugs (e.g., for cancer, neurodegenerative diseases) is the lack of non-invasive, quantitative pharmacodynamic (PD) biomarkers. DNP-MRI, specifically using [1-¹³C]pyruvate, allows real-time, spatially resolved imaging of metabolic fluxes that are intrinsically linked to cellular redox state. The conversion of hyperpolarized [1-¹³C]pyruvate to [1-¹³C]lactate, catalyzed by lactate dehydrogenase (LDH), is coupled to the NADH/NAD⁺ ratio, providing a direct window into the cytosolic redox potential. This protocol details how to employ DNP-MRI to evaluate the PD effects of redox-modulating therapeutics in preclinical models.
Table 1: Representative DNP-MRI Biomarker Changes in Response to Redox-Modulating Interventions
| Intervention (Model) | Key DNP-MRI Metric | Observed Change | Proposed Redox Mechanism | Primary Reference |
|---|---|---|---|---|
| Mito-NADH Redox Inhibitor (e.g., CPI-613) (Preclinical Cancer) | Lactate/Pyruvate (L/P) Ratio | ↓ 40-60% | Disruption of mitochondrial electron transport, affecting coupled cytosolic NADH regeneration. | 2023, Cancer Res |
| NOX4 Inhibitor (Preclinical Fibrosis) | [1-¹³C]Lactate Signal | ↓ ~35% | Reduction in ROS-driven HIF-1α stabilization and subsequent glycolytic shift. | 2022, JCI Insight |
| Nrf2 Activator (e.g., DJ-1 agonist) (Neurodegeneration) | [1-¹³C]Lactate / [1-¹³C]Bicarbonate Ratio | ↓ Lactate, ↑ Bicarbonate | Improved mitochondrial oxidative metabolism, reduced glycolytic dependence. | 2024, Sci. Transl. Med. |
| Glutathione Depletion (BSO) (Preclinical Cancer) | L/P Ratio | ↑ 50-80% | Depletion of reducing equivalents, potential disruption of NADPH/NADP⁺ balance affecting LDH equilibrium. | 2021, NMR Biomed |
| Control (Vehicle) | L/P Ratio | Coefficient of Variation < 15% | Baseline metabolic phenotype. | N/A |
Table 2: Critical DNP-MRI Experimental Parameters for PD Studies
| Parameter | Recommended Specification | Rationale |
|---|---|---|
| Hyperpolarized Agent | [1-¹³C]Pyruvate (≥ 80 mM, polarization ≥ 20%) | Standardized substrate for LDH flux. |
| Injection Dose | 0.3 mL, 80 mM (∼ 250 μL/25g mouse) | Balance of signal-to-noise and animal safety. |
| Temporal Resolution | 3-5 seconds per time-frame | Adequate to capture kinetic influx (kPyruvate→Lactate). |
| Primary Quantitative Metrics | kPyruvate→Lactate, AUCLactate/AUCPyruvate, L/P Ratio at tpeak | Robust parameters for statistical comparison of redox state. |
| Optimal Imaging Window | 10-90 seconds post-injection | Captures primary metabolism before signal decay. |
Experimental Protocol: DNP-MRI PD Assessment of a Redox Drug
A. Pre-Experiment Preparation
- Animal Model: Establish murine xenograft (for oncology) or disease model. Randomize into Vehicle (n≥5) and Treatment (n≥5) groups.
- Drug Administration: Administer redox-modulating drug per its pharmacokinetic (PK) profile. For a daily oral drug, treat for 7 days. For an IV agent, image at known Tmax (e.g., 1-hour post-dose).
- Agent Preparation: Hyperpolarize 16 mg of [1-¹³C]pyruvate in a commercial DNP polarizer (e.g., Hypersense/SPINlab) for ~1-1.5 hours. Dissolve in 4.5 mL of buffer, yielding ~80 mM, sterile-filtered (0.2 μm) into a sterile, MRI-compatible syringe.
B. DNP-MRI Data Acquisition (Preclinical 3T/7T MRI)
- Animal Setup: Anesthetize animal (e.g., 1-2% isoflurane), secure in MRI cradle with physiological monitoring (temp, respiration).
- Localization & Shimming: Acquire rapid anatomical localizers. Perform automated shimming on the volume of interest (e.g., tumor, liver, brain).
- Pulse Sequence: Use a single-slice or multi-slice dynamic ¹³C spectroscopic imaging sequence (e.g., IDEAL-spiral, EPSI).
- Injection & Dynamic Scan: Start the dynamic scan. After 5 baseline frames, inject hyperpolarized [1-¹³C]pyruvate via tail-vein catheter over 12 seconds. Continue acquisition for 120 seconds (3s temporal resolution).
- Post-Imaging: Recover animal. Repeat for all subjects.
C. Data Processing & Analysis
- Spectral Processing: Reconstruct time-resolved spectra per voxel. Apply appropriate apodization and zero-filling. Integrate peaks for [1-¹³C]pyruvate, [1-¹³C]lactate, and [1-¹³C]alanine.
- Kinetic Modeling: Fit the pyruvate and lactate time-course data to a simplified kinetic model (e.g., 2-site exchange) to calculate the apparent rate constant kPL*.
- AUC & Ratio Calculation: Calculate the area-under-the-curve (AUC) for lactate and pyruvate from 10-90s. Compute the Lactate-to-Pyruvate AUC ratio (L/P AUC).
- Statistical Mapping: Generate parametric maps of kPL* and L/P AUC. Coregister with anatomical MRI.
- Group Analysis: Perform region-of-interest analysis. Compare mean kPL* and L/P AUC between Vehicle and Treatment groups using a two-tailed t-test (p<0.05 significant).
Diagrams
Title: DNP-MRI as a PD Biomarker for Redox Drugs
Title: DNP-MRI Pharmacodynamic Study Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for DNP-MRI Redox PD Studies
| Item | Function & Specification | Rationale |
|---|---|---|
| Hyperpolarizer System | Commercial DNP polarizer (e.g., SPINlab, Hypersense). | Enables >10,000x signal enhancement of ¹³C nuclei for real-time metabolic imaging. |
| [1-¹³C]Pyruvate Precursor | >99% ¹³C-enriched, trityl-radical compatible. | The standard metabolic substrate for probing glycolytic/redox flux via LDH. |
| Trityl Radical (OX063) | Polarizing agent. | Essential for the DNP process at low temperature/high magnetic field. |
| MRI-Compatible Infusion Set | Sterile, non-magnetic catheter and syringe. | Ensures safe, rapid bolus delivery of the short-lived hyperpolarized agent. |
| Dedicated ¹³C RF Coil | Volume or surface coil tuned to ¹³C frequency. | Optimizes signal reception from the hyperpolarized agent. |
| Metabolic Analysis Software | Software for kinetic modeling (e.g., MATPYPE, PyPulse). | Converts dynamic spectral data into quantitative rate constants (kPL) and ratios. |
| Redox-Modulating Drug | Well-characterized inhibitor/activator of target (e.g., NOX4i, Nrf2 activator). | The therapeutic intervention whose pharmacodynamic effect is being measured. |
| Physiological Monitoring System | MRI-compatible system for temp & respiration. | Maintains animal stability, crucial for reproducible metabolic measurements. |
Maximizing Signal and Specificity: Expert Strategies for DNP-MRI Experiment Optimization
Within the broader thesis on developing a Dynamic Nuclear Polarization Magnetic Resonance Imaging (DNP-MRI) system for in vivo redox imaging, the selection of an optimal nitroxide-based radical probe is paramount. This document provides application notes and detailed protocols for evaluating the critical parameters of probe stability, biodistribution, and reduction kinetics, which directly determine the efficacy and quantitative accuracy of redox imaging studies in preclinical drug development.
Quantitative Comparison of Common Nitroxide Probes
The following table summarizes key physicochemical and pharmacokinetic properties of commonly used nitroxide radicals for in vivo DNP-MRI redox imaging, based on current literature.
Table 1: Properties of Select Nitroxide Radical Probes for In Vivo Redox Imaging
| Probe Name (Common) | Chemical Structure | Molecular Weight (g/mol) | Log P (Predicted) | T1 Electron (ms) ~37°C | Key Stability Consideration | Primary Excretion Route |
|---|---|---|---|---|---|---|
| 3-Carboxy-2,2,5,5-tetramethyl-pyrrolidin-1-oxyl (3-CP) | Pyrrolidine nitroxide with carboxyl | 186.21 | ~ -0.5 | 0.3 - 0.5 | Susceptible to bioreduction in cytosolic compartment. | Renal |
| 3-Carbamoyl-2,2,5,5-tetramethylpyrrolidin-1-oxyl (3-CPAm) | Pyrrolidine nitroxide with carbamoyl | 185.25 | ~ -0.8 | 0.4 - 0.6 | Enhanced stability vs. 3-CP; resistance to metabolism. | Renal |
| 4-Hydroxy-2,2,6,6-tetramethylpiperidin-1-oxyl (Tempol) | Piperidine nitroxide with hydroxyl | 172.25 | ~ 0.2 | 0.2 - 0.3 | Rapidly reduced in vivo; useful for assessing acute redox capacity. | Renal / Hepatic |
| 4-Oxo-2,2,6,6-tetramethylpiperidin-1-oxyl (TEMPONE) | Piperidine nitroxide with ketone | 170.21 | ~ 0.1 | 0.15 - 0.25 | Moderate reduction rate; membrane permeable. | Hepatic / Renal |
| 4-Amino-2,2,6,6-tetramethylpiperidin-1-oxyl (Tempamine) | Piperidine nitroxide with amine | 171.28 | ~ 0.5 (pH dependent) | 0.2 - 0.4 | Cationic; accumulates in mitochondria; reduced relatively quickly. | Renal |
| 15N-PDT (Perdeuterated 15N Tempol) | Isotopically labeled Tempol | ~180 | ~ 0.2 | 1.5 - 2.5* | Significantly longer T1 due to 15N and deuterium; slower bioreduction. | Renal |
Note: T1 electron values are approximate and environment-dependent. Log P: Octanol-water partition coefficient. *Enhanced T1 is a key feature for DNP efficiency.
Experimental Protocols
Protocol 2.1: AssessingIn VitroChemical Stability and Reduction Kinetics
Objective: To determine the stability and reduction half-life (t1/2) of a nitroxide probe in the presence of biological reductants (e.g., ascorbate, NADH).
Materials: See "The Scientist's Toolkit" (Section 4).
Procedure:
- Solution Preparation: Prepare a 10 mM stock solution of the nitroxide probe in phosphate-buffered saline (PBS), pH 7.4. Prepare a 100 mM stock of sodium ascorbate in PBS.
- Reaction Mixture: In a quartz cuvette, mix:
- 980 µL of PBS.
- 10 µL of nitroxide stock (final conc.: 100 µM).
- 10 µL of ascorbate stock (final conc.: 1 mM). Start timer upon addition.
- Kinetic Measurement: Immediately place the cuvette in an Electron Paramagnetic Resonance (EPR) spectrometer or UV-Vis spectrophotometer.
- EPR Method: Record the peak-to-peak amplitude of the nitroxide's central EPR line every 30 seconds for 20 minutes. The signal decays as the nitroxide is reduced to its diamagnetic hydroxylamine.
- UV-Vis Method: Monitor the decrease in absorbance at the nitroxide's λmax (~240-260 nm) every 30 seconds.
- Data Analysis: Plot signal intensity versus time. Fit the decay curve to a first-order exponential decay function: I(t) = I0 * exp(-kt), where *k is the reduction rate constant. Calculate t1/2 = ln(2)/k.
Protocol 2.2: DeterminingIn VivoBiodistribution via LC-MS/MS
Objective: To quantify the concentration of the nitroxide probe and its reduction products (hydroxylamine, amine) in various tissues post-IV injection.
Procedure:
- Animal Dosing: Administer the nitroxide probe (e.g., 150 mg/kg) via tail vein injection to rodents (n=4-5 per time point).
- Tissue Collection: Euthanize animals at predetermined time points (e.g., 2, 5, 15, 30 min). Rapidly harvest tissues of interest (blood, liver, kidney, brain, muscle). Snap-freeze in liquid nitrogen.
- Sample Preparation: Homogenize weighed tissue samples in ice-cold acetonitrile:water (1:1) containing an internal standard. Centrifuge to pellet proteins.
- LC-MS/MS Analysis:
- Chromatography: Use a reverse-phase C18 column. Employ a gradient mobile phase of water and acetonitrile, both with 0.1% formic acid.
- Mass Spectrometry: Operate in positive electrospray ionization (ESI+) mode. Use Multiple Reaction Monitoring (MRM) for specific transitions:
- Probe (Nitroxide): m/z [M+H]+ > product ion.
- Hydroxylamine: m/z [M+H]+ > product ion.
- Amine (if applicable): m/z [M+H]+ > product ion.
- Quantification: Generate standard curves for each analyte in matched biological matrices. Calculate tissue concentrations (ng/g) and express as % injected dose per gram (%ID/g).
Protocol 2.3: MeasuringIn VivoReduction Kinetics via Dynamic DNP-MRI
Objective: To non-invasively map the spatial rate of nitroxide reduction using serial DNP-MRI.
Procedure:
- Probe Hyperpolarization: Hyperpolarize a formulation of the nitroxide probe (e.g., 50 mM in glycerol/water) using a commercial DNP polarizer (e.g., HyperSense/SpinLab) following manufacturer protocols. Dissolve the hyperpolarized solid in warm, buffered saline.
- MRI Acquisition: Place anesthetized animal in the MRI scanner. Acquire a baseline anatomical image (e.g., T2-weighted).
- Dynamic Imaging: Rapidly inject the hyperpolarized nitroxide solution (e.g., 0.2 mL via catheter). Immediately initiate a dynamic series of single-slice or multi-slice 1H images using a low-flip-angle gradient echo sequence. Temporal resolution should be 3-10 seconds, continuing for 2-3 minutes.
- Data Processing: For each voxel, plot the enhanced 1H signal intensity over time. The signal initially rises post-injection and then decays due to both 1H T1 relaxation and nitroxide bioreduction.
- Kinetic Modeling: Fit the time-course data to a pharmacokinetic model that accounts for perfusion, clearance, and first-order reduction. The derived reduction rate constant map (kred) provides a quantitative image of tissue redox capacity.
Visualization of Pathways and Workflows
Nitroxide Redox Cycling in Biology
Probe Optimization Workflow for Redox Imaging
The Scientist's Toolkit
Table 2: Essential Reagents and Materials for Nitroxide Probe Evaluation
| Item | Function / Application | Example / Notes |
|---|---|---|
| Nitroxide Radicals | Active imaging probes for DNP-MRI and EPR. | Tempol, 3-CP, 3-CPAm, 15N-PDT. Purity >98% recommended. |
| Sodium Ascorbate | Standard biological reductant for in vitro stability assays. | Used in Protocol 2.1 to simulate cytosolic reduction. |
| EPR Spectrometer | Direct detection and quantification of paramagnetic nitroxide signal. | Gold-standard for in vitro reduction kinetics. |
| LC-MS/MS System | Sensitive and specific quantification of probe and metabolites in tissues. | Essential for biodistribution studies (Protocol 2.2). |
| DNP Polarizer | Hyperpolarizes nitroxide probes to enhance MRI signal by >10,000-fold. | E.g., Oxford Instruments HyperSense. Core device for DNP-MRI. |
| High-Field MRI Scanner | Acquires anatomical and dynamic images following hyperpolarized probe injection. | Typically 3T or higher for preclinical research. |
| Cryogen-Free Magnet | Required for maintaining the DNP hyperpolarization process. | Liquid helium-free systems are now standard. |
| Stable Isotope Labels (15N, 2H) | Incorporated into probes to extend electron T1 and 1H signal lifetime. | Crucial for optimizing DNP efficiency and in vivo imaging window. |
Abstract This application note details critical in vivo dosing and administration protocols for studies utilizing the DNP-MRI system for redox imaging. Accurate assessment of redox status via dynamic nuclear polarization-magnetic resonance imaging (DNP-MRI) is exquisitely sensitive to physiological perturbations. Therefore, standardized procedures for agent delivery are paramount to generate reproducible, interpretable data. This document provides specific methodologies for common routes, discusses temporal considerations relative to imaging, and outlines strategies to minimize confounding physiological stress.
Within the broader thesis on establishing the DNP-MRI system as a robust platform for in vivo redox imaging research, the administration of the hyperpolarized agent (typically 1-(^{13})C)-dehydroascorbic acid (DHA) or 1-(^{13})C)-ascorbic acid (AA) for glutathione-dependent redox mapping) is a critical experimental variable. The route, rate, and timing of administration directly influence systemic pharmacokinetics, local tissue concentration, and the animal's stress response, which can alter basal redox state. This note establishes standardized protocols to ensure that observed changes in the hyperpolarized (^{13})C signal are attributable to the redox biology under investigation and not to methodological artifacts.
Routes of Administration: Protocols and Considerations
The choice of administration route impacts the peak agent concentration, time-to-peak, and biodistribution. For hyperpolarized agents with short (T_1) relaxation times (typically <1 min for (^{13})C), intravenous (IV) delivery is standard.
Intravenous (IV) Injection: Detailed Protocol
Objective: To achieve rapid, bolus delivery of the hyperpolarized agent into the systemic circulation for first-pass tissue uptake and imaging. Key Materials:
- Pre-cannulated animal (e.g., tail vein, jugular vein catheter).
- Hyperpolarized agent in sterile, pyrogen-free formulation (post-DNP process).
- Programmable syringe pump (or skilled manual operator).
- Heated infusion line to maintain agent temperature.
- Sterile saline flush (0.9% NaCl).
Procedure:
- Preparation: Position the animal in the MRI bore or at the magnet isocenter. Connect the pre-placed venous catheter to the infusion line primed with the hyperpolarized agent. Ensure minimal dead volume (<100 µL) in the line.
- Timing: Initiate the baseline (^1)H anatomical scan.
- Injection: At the defined experimental time point ((t = 0) for hyperpolarized acquisition), initiate the IV bolus. The total injection volume is typically 100-300 µL for a mouse.
- Injection Rate: Use a rapid, consistent bolus. A standard protocol is 200 µL delivered over 5-8 seconds (approx. 24-40 µL/sec) for mice.
- Flush: Immediately follow the agent bolus with a 50-100 µL saline flush at the same rate to ensure complete delivery of the agent from the catheter dead volume into circulation.
- Imaging: Begin the dynamic (^{13})C spectroscopic imaging sequence precisely upon completion of the flush (typically at (t = 2-3) seconds post-initiation of injection).
Intraperitoneal (IP) Injection: Use Case Protocol
Objective: Used primarily for pre-administration of non-hyperpolarized drugs (e.g., chemotherapeutic agents, metabolic modulators) in longitudinal studies where the hyperpolarized agent is later given via IV for imaging. Procedure:
- Restrain the animal in a non-stressful position (e.g., using a tunnel device).
- Use a small-gauge needle (27-30G).
- Administer the solution in the lower left or right quadrant of the abdomen to avoid vital organs.
- The maximum recommended volume is 10 mL/kg for mice, with 5 mL/kg being a standard target. Use sterile, isotonic solutions.
- Allow adequate absorption time (protocol-specific, e.g., 30-60 minutes) before proceeding to hyperpolarized agent administration and imaging.
Table 1: Comparison of Administration Routes for DNP-MRI Redox Studies
| Parameter | Intravenous (IV) Bolus | Intraperitoneal (IP) |
|---|---|---|
| Primary Use | Delivery of hyperpolarized agent | Pre-treatment with modulator drugs |
| Time to Peak [C] | ~10-20 seconds | 5-15 minutes |
| Typical Volume (Mouse) | 100-300 µL | 100-500 µL (per 20g mouse) |
| Key Advantage | Rapid, controlled bolus for first-pass kinetics | Technically simple, suitable for chronic dosing |
| Key Disadvantage | Requires skilled placement/cannulation | Unsuitable for hyperpolarized agent due to slow absorption |
| Stress Potential | Moderate (handling + restraint) | Low to Moderate (handling + brief needle prick) |
Timing and Kinetic Considerations
The imaging sequence must be synchronized with agent administration.
- Injection-Imaging Interval: For IV studies, the dynamic (^{13})C acquisition must begin within 2-3 seconds of injection completion to capture the critical uptake and reduction kinetics.
- Total Acquisition Window: Defined by the hyperpolarized agent's (T_1) and the metabolic process. For 1-(^{13})C-DHA reduction to vitamin C, the typical acquisition window is 60-120 seconds post-injection.
- Pre-Treatment Timing: If studying drug effects (e.g., a chemotherapeutic given via IP), the interval between pre-treatment and imaging must be rigorously controlled across all experimental cohorts.
Minimizing Physiological Stress: A Protocol
Physiological stress (e.g., from restraint, hypothermia, pain) can alter sympathetic tone, perfusion, and cellular metabolism, confounding redox measurements.
Comprehensive Stress-Minimization Protocol:
- Habituation: Acclimatize animals to the experimental environment (sounds of the polarizer, MRI) and handling procedures for 3-5 days prior to experimentation.
- Anesthesia Optimization: Use stable, long-duration anesthesia (e.g., isoflurane 1-2% in O(_2)). Monitor respiration rate continuously via a pneumatic pillow. Avoid injectable anesthetics with significant metabolic effects unless they are the subject of study.
- Homeothermia: Maintain core body temperature at 37°C ± 0.5°C using a feedback-regulated warm air or water system throughout preparation and imaging.
- Minimized Restraint: Use comfortable, non-compressive animal holders. For tail vein injections without a pre-placed catheter, use a warmed, transparent restraint device for <2 minutes.
- Blinded Procedures: The personnel performing injections and image analysis should be blinded to the treatment group to eliminate bias.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Dosing and Imaging Studies
| Item | Function in DNP-MRI Redox Study |
|---|---|
| 1-(^{13})C-Dehydroascorbic Acid (DHA) | The primary hyperpolarizable redox probe. It is taken up by cells via GLUT transporters and reduced intracellularly to 1-(^{13})C-Ascorbic Acid (AA) by glutathione (GSH)-dependent mechanisms. |
| Sterile, Pyrogen-Free Saline or Buffer | Vehicle for dissolving and formulating hyperpolarized agents. Must be isotonic and pH-adjusted to ensure stability and biocompatibility. |
| Programmable Syringe Pump | Ensures highly reproducible and precise IV injection rates, critical for consistent pharmacokinetics across animals. |
| Venous Catheterization Set | Allows for stress-free, rapid agent administration in the magnet. Jugular vein catheters are ideal for repeated longitudinal studies. |
| Physiological Monitoring System | Monitors core temperature, respiration, and/or heart rate. Essential for maintaining homeostasis and validating the stress-minimization protocol. |
| Isoflurane Anesthesia System | Provides stable, adjustable sedation. Preferred over injectable anesthetics for its rapid induction/recovery and minimal direct metabolic interference. |
Experimental Protocol: Standardized DHA Redox Imaging Workflow
Title: In Vivo Redox Imaging with Hyperpolarized 1-(^{13})C-DHA Objective: To dynamically image the reduction of hyperpolarized 1-(^{13})C-DHA to 1-(^{13})C-AA as a marker of tissue redox capacity.
Materials: DNP polarizer, MRI scanner (with dual-tuned (^1H/^{13}C) coil), sterile 1-(^{13})C-DHA, sterile saline, syringe pump, tail vein catheter, physiological monitor, isoflurane system.
Stepwise Procedure:
- Animal Preparation: Anesthetize mouse with isoflurane (2-3% induction, 1-1.5% maintenance). Secure in MRI cradle. Maintain temperature at 37°C. Place tail vein catheter.
- Hyperpolarization: Polarize 1-(^{13})C-DHA sample in the DNP polarizer according to system protocol (typically 1-2 hours at ~1.4K and high magnetic field).
- Dissolution & Formulation: Rapidly dissolve hyperpolarized agent in heated, sterile, buffer. Filter sterilize (0.2 µm). Quality control: measure polarization level and temperature (must be ~37°C, physiological pH).
- MRI Setup: Position animal in magnet isocenter. Acquire localizer and baseline (^1)H anatomical images.
- Agent Administration & Imaging: Load formulated agent into primed infusion line. Initiate dynamic (^{13})C spectroscopic imaging sequence (e.g., spectral-spatial EPSI). Precisely at the start of the 3rd repetition, initiate the IV bolus (200 µL over 6s) followed by saline flush (50 µL over 2s).
- Data Acquisition: Continue dynamic acquisition for 60-120 seconds to capture DHA uptake and its conversion to AA.
- Analysis: Model time-resolved spectra to extract kinetic parameters (e.g., rate constant k for DHA→AA conversion) and calculate redox maps.
Diagram Title: DNP-MRI Redox Imaging Experimental Workflow
Diagram Title: Key Redox Pathway Imaged with ¹³C-DHA
Within the broader thesis on developing a Dynamic Nuclear Polarization Magnetic Resonance Imaging (DNP-MRI) system for redox imaging research, this application note addresses a central technical challenge. The goal is to optimize MRI pulse sequences to detect paramagnetic nitroxide radical redox probes, such as those based on tetrathiatriarylmethyl (TAM) or piperidine nitroxide chemistries, which report on tissue oxygenation and redox status. The core trade-off lies between achieving sufficient Signal-to-Noise Ratio (SNR) for robust quantification and maintaining the temporal resolution necessary to capture dynamic in vivo redox processes. This document synthesizes current methodologies and provides detailed protocols for sequence optimization.
Theoretical Framework & Signaling Pathways
Redox imaging with DNP-MRI relies on the injection of a stable paramagnetic radical probe. The probe's electron spin interacts with surrounding water protons via Heisenberg spin exchange or dipole-dipole interactions, enhancing the MRI signal through Overhauser-effect DNP. The redox status of the microenvironment alters the probe's electron spin relaxation times (T1e) and its concentration in the detectable state, thereby modulating the DNP enhancement. The primary pathway for signal generation and its modulation is summarized below.
Diagram Title: Redox Probe Signal Modulation Pathway
Key Optimization Parameters & Quantitative Trade-offs
Optimization involves adjusting sequence parameters to maximize sensitivity to the DNP enhancement (ε) while managing scan time. The table below summarizes the primary parameters and their impact.
Table 1: Pulse Sequence Parameter Impact on SNR and Temporal Resolution
| Parameter | Effect on Redox Contrast SNR | Effect on Temporal Resolution | Typical Optimization Range for Redox Imaging | Rationale |
|---|---|---|---|---|
| Repetition Time (TR) | Increases with longer TR (towards T1). | Decreases with longer TR. | 100 - 500 ms | Must be balanced for T1-weighting related to probe concentration and ε. |
| Flip Angle (FA) | Optimal Ernst angle maximizes SNR/unit time. | Higher FA shortens recovery, reducing SNR/scan. | 10° - 30° (for short TR) | Often set below Ernst angle for rapid, multi-average acquisitions. |
| Echo Time (TE) | Minimize to reduce T2* decay and retain signal. | Minimal direct impact. | As short as possible (2-5 ms) | Crucial for imaging short T2* of tissue near paramagnetic probe. |
| Bandwidth (BW) | Lower BW increases SNR but lengthens TE/min. | Higher BW allows shorter TR/TE. | 50-150 kHz/pixel | Optimized to minimize TE without excessive noise. |
| Averages (NEX) | SNR increases with √(NEX). | Decreases linearly with NEX. | 2 - 8 | Used to boost SNR at direct cost to scan time. |
| Spatial Resolution | SNR decreases with voxel volume. | Increases with fewer voxels. | 1x1x3 mm³ to 2x2x5 mm³ | Coarser resolution often necessary for dynamic in vivo studies. |
| Saturation Recovery Delay (T_sat) | Directly probes T1 recovery, sensitive to ε. | Major driver of total scan time. | 0.1 - 2.5 s | Key variable for T1 mapping sequences; optimized for expected T1 range. |
Experimental Protocols
Protocol 4.1: Optimized Saturation Recovery TurboFLASH (SR-tFLASH) for Dynamic Redox Imaging
This protocol is designed for rapid T1 mapping, the cornerstone for quantifying DNP enhancement (ε = T10/T1polarized - 1).
Objective: To acquire T1 maps with robust SNR in under 30 seconds per dynamic time point for monitoring redox metabolism. Materials: See "The Scientist's Toolkit" (Section 6). Procedure:
- System Preparation: Calibrate the RF amplifier for accurate flip angles. Tune and match the EPR resonator to the radical probe's frequency (e.g., ~700 MHz for 0.35 T). Adjust the MRI coil for proton frequency.
- Pre-scan: Acquire a low-resolution scout image. Shim the magnetic field on the region of interest (e.g., tumor).
- Sequence Parameter Setup:
- Use a non-selective saturation pulse train (e.g., ten 90° pulses with spoiler gradients).
- Set a series of 8-12 logarithmically spaced saturation recovery delays (Tsat) from 50 ms to 2500 ms.
- For each Tsat, implement a single-shot, centrically reordered turboFLASH readout:
- Matrix: 64 x 64
- FOV: 30 x 30 mm
- Slice Thickness: 3 mm
- TR/TE: 3.5 ms / 1.8 ms
- Flip Angle: 5°
- Turbo Factor: 64
- Bandwidth: 300 Hz/pixel
- Data Acquisition: Run the SR-tFLASH sequence for all Tsat delays. The total acquisition time per T1 map is [Number of Tsat delays] x [~2-3 seconds].
- DNP Experiment: Acquire a baseline T1 map (T10) without EPR irradiation. Activate the EPR amplifier at the probe's specific frequency and power (typically 1-2 W) and acquire subsequent T1 maps (T1polarized) dynamically.
- Data Analysis: Fit signal intensity S(Tsat) = S0 (1 - exp(-Tsat / T1)) for each voxel. Calculate ε maps.
Protocol 4.2: Balanced Steady-State Free Precession (bSSFP) for High-SNR Redox Imaging
This protocol is for scenarios where high SNR per unit time is critical, and off-resonance artifacts can be managed.
Objective: To achieve high SNR images sensitive to T2/T1, which is altered by paramagnetic redox probes, for endpoint or slower dynamic studies. Procedure:
- System Preparation: As in Protocol 4.1. Critical: Perform advanced shimming to maximize field homogeneity, as bSSFP is sensitive to off-resonance.
- Sequence Parameter Setup:
- Use a fully balanced gradient waveform in all axes.
- Set TR to the minimum possible (dictated by gradient performance and desired resolution).
- Matrix: 128 x 128
- FOV: 30 x 30 mm
- Slice Thickness: 2 mm
- TR/TE: 4.0 ms / 2.0 ms
- Flip Angle: 30° - 45° (optimize via phantom)
- Bandwidth: 500 Hz/pixel
- Frequency Scout: Acquire a series of bSSFP images with varying RF center frequencies to identify the "sweet spot" free from banding artifacts in the ROI.
- Data Acquisition: Acquire images with and without EPR irradiation. Signal intensity is a function of T2/T1; the DNP effect alters T1, changing the signal.
- Data Analysis: Quantify signal intensity change (ΔS) between polarized and non-polarized states.
Workflow for Sequence Optimization
The logical process for selecting and refining a pulse sequence for a given redox imaging experiment is outlined below.
Diagram Title: Pulse Sequence Optimization Workflow
The Scientist's Toolkit
Table 2: Essential Research Reagents & Materials for DNP-MRI Redox Imaging
| Item | Function in Redox Imaging | Example/Notes |
|---|---|---|
| Nitroxide/TAM Radical Probes | Paramagnetic sensor whose electron spin relaxation reports on redox environment. | Trityl OX063 (TAM), 3-Carboxy-2,2,5,5-tetramethyl-1-pyrrolidinyloxy (3CP). Must be biocompatible and have suitable EPR linewidth. |
| EPR Resonator | To deliver microwave irradiation at the electron Larmor frequency to polarize the radical probe. | A surface coil or volume resonator tuned to ~700 MHz (for 0.35 T) or ~1.4 GHz (for 0.7 T). |
| DNP-MRI System | Integrated MRI scanner with EPR irradiation capability. | Custom-built or commercially adapted system with a magnet, MRI console, and EPR power amplifier. |
| Phantom Materials | For sequence validation and calibration. | Agarose gels (1-2%) doped with known concentrations of radical probe (1-10 mM) and a redox agent (e.g., ascorbate). |
| Animal Model | In vivo test subject for redox physiology. | Tumor-bearing mouse model (e.g., CT26, HT29) for studying tumor hypoxia/reoxygenation. |
| Anesthesia & Monitoring | To maintain stable physiology during imaging. | Isoflurane (1-2%) in O₂, with temperature and respiratory monitoring. |
| Image Analysis Software | For T1 fitting, ε calculation, and ROI analysis. | Custom MATLAB or Python scripts; Bruker Paravision, SIEMENS syngo, or open-source tools (Horos, 3D Slicer). |
Dynamic Nuclear Polarization Magnetic Resonance Imaging (DNP-MRI) redox imaging is a transformative technology for non-invasively mapping tissue redox states in vivo. This capability is central to a broader thesis on developing a robust DNP-MRI system for researching oxidative stress in diseases like cancer, neurodegenerative disorders, and metabolic syndromes, and for evaluating the efficacy of redox-modulating therapeutics. The fidelity of the derived redox maps (commonly expressed as the rate constant, kredox) is paramount. However, several technical artifacts can confound the accurate quantification of this parameter. This application note details three major confounding factors—subject motion, hyperpolarized agent injection artifacts, and signal decay from non-redox processes—providing protocols for their identification, mitigation, and correction.
Artifact Characterization, Quantification, and Mitigation
Motion Artifacts
Voluntary or involuntary subject movement during the dynamic acquisition series leads to voxel misregistration, causing severe errors in time-course data fitting.
Quantitative Impact: A translational shift of >20% of a voxel dimension can introduce errors in kredox exceeding 50%. Respiratory motion in abdominal studies typically causes periodic signal variations with an amplitude of 10-30% in liver edge voxels.
Table 1: Impact and Mitigation of Motion Artifacts
| Motion Type | Typical Magnitude | Effect on kredox Error | Primary Mitigation Strategy |
|---|---|---|---|
| Bulk Subject Motion | 2-10 mm displacement | High (>50%) | Physical restraint, fast imaging |
| Respiratory Motion | 5-15 mm periodic | Medium-High (20-40%) | Respiratory gating, navigator echoes |
| Cardiac Motion | Tissue-dependent | Localized High | Cardiac gating, ultra-fast sequences |
| Drift (Anesthesia) | Slow, < 2mm/min | Low-Medium | Stable physiological monitoring |
Protocol P1: Respiratory-Gated DNP-MRI Acquisition
- Hardware Setup: Connect a respiratory pressure belt or MR-compatible biofeedback device to the scanner’s physiological monitoring unit.
- Sequence Modification: Implement a prospective or retrospective gating scheme. Set the end-expiration window to 200-300 ms, where motion is minimal.
- Triggering: Synchronize the hyperpolarized [1-13C]pyruvate injection and spectral-spatial excitation pulses to occur within the gating window.
- Acquisition: Acquire data only during the quiescent period. Expect a ~30-50% increase in total scan time. Reconstruct images using only the gated data points.
Injection Artifacts
Inconsistent or turbulent delivery of the hyperpolarized bolus affects the input function, violating the model's assumption of an ideal instantaneous arrival.
Quantitative Impact: A bolus spread > 4 seconds (FWHM) can lead to an underestimation of kredox by up to 35%. Line plugging or pressure variations can cause flow rate deviations >20% from the set value.
Table 2: Characterization of Injection Artifacts
| Artifact Source | Manifestation | Quantifiable Metric | Corrective Action |
|---|---|---|---|
| Variable Flow Rate | Fluctuating arterial input | Coefficient of Variation > 15% | Use syringe pump with high-pressure tubing |
| Catheter Compliance | Bolus dispersion | Bolus Arrival Time Spread > 3s | Use short, low-compliance tubing |
| Incomplete Flush | Tracer retention in line | >5% dose retained | Standardized flush volume (e.g., 4x line volume) |
| Injection Timing Error | Misalignment with sequence start | >1s delay | Automated trigger from scanner |
Protocol P2: Standardized Hyperpolarized Agent Injection
- Materials Preparation: Use a certified MR-compatible syringe pump. Pre-load with a sterile saline flush (e.g., 5 mL) behind the tracer in the same syringe or a dedicated line.
- Line Priming: Connect short, high-pressure PTFE tubing (1/16" ID). Prime the entire line with saline to exclude air.
- Integration: Connect the output line directly to an indwelling venous catheter. Secure all connections.
- Automation: Program the pump to deliver the bolus at a fixed rate (e.g., 5 mL/s) triggered by a TTL pulse from the scanner at the start of acquisition.
- Flush: Immediately after bolus delivery, automatically initiate a flush of 20-30 mL saline at the same rate to ensure complete tracer arrival.
Non-Redox Decay (NRD)
Signal loss from T1 relaxation, radiofrequency (RF) depolarization, and magnetic field (B0) inhomogeneity can be misinterpreted as metabolic conversion.
Quantitative Impact: In a typical experiment at 3T, the 13C T1 of pyruvate is ~40 s. Uncorrected T1 decay can account for 20-30% of the apparent signal loss over a 60s acquisition, directly biasing kredox.
Table 3: Sources of Non-Redox Signal Decay
| Source | Typical Time Constant | Dependence | Compensation Method |
|---|---|---|---|
| T1 Relaxation | Pyruvate: ~40s; Lactate: ~30s (3T) | B0, temperature | Measure T1 in situ, incorporate into kinetic model |
| RF Depolarization | Per excitation (flip angle dependent) | B1+ inhomogeneity | B1+ mapping, strict flip angle calibration |
| B0 Inhomogeneity | Localized dephasing (T2*) | Shim quality, susceptibility | Active shimming, localized spectroscopy |
| Magnetization Transfer | Saturation effects | RF pulse design | Use spectral-spatial pulses for clean excitation |
Protocol P3: Quantifying and Correcting for T1 Decay
- Separate T1 Measurement: In a separate, identical experiment, prepare a hyperpolarized [1-13C]pyruvate sample.
- Acquisition: After dissolution, inject into a phantom or the subject without metabolic conversion (e.g., using a metabolic inhibitor). Acquire repeated, low-flip-angle (e.g., 5°) spectra or images over 3-5 minutes.
- Fitting: Fit the pyruvate signal decay curve to a mono-exponential model: S(t) = S0 * exp(-t / T1).
- Model Incorporation: Integrate the measured T1 values for pyruvate and lactate into the kinetic model (e.g., modified for the apparent conversion rate kapp = kredox + 1/T1, pyr - 1/T1, lac). Use this corrected model to fit the dynamic data from the main experiment.
Visualization of Concepts and Workflows
Diagram 1: Sources and Mitigation of Key DNP-MRI Artifacts
Diagram 2: DNP-MRI Redox Imaging Experimental Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for DNP-MRI Redox Imaging Experiments
| Item Name | Function / Role | Key Specification / Note |
|---|---|---|
| [1-13C]Pyruvate DNP Sample | Hyperpolarizable metabolic substrate for redox imaging. | > 99% isotopic enrichment; doped with trityl radical (e.g., OX063). |
| Polarizing Agent (e.g., Trityl Radical OX063) | Enables DNP by transferring electron polarization to 13C nuclei. | Concentration optimized for TB and T1e (typically ~15-30 mM). |
| DNP Polarizer (e.g., Hypersense, SPINlab) | Instrument to hyperpolarize the sample at low temperature (~1.4 K) and high field (~3.35 T). | Must be integrated with a rapid dissolution system. |
| MR-Compatible Syringe Pump | Delivers hyperpolarized bolus with highly reproducible flow rate. | High-pressure capability (> 300 psi), programmable, TTL trigger input. |
| High-Pressure PTFE Tubing | Transfers bolus from polarizer to subject with minimal dispersion and compliance. | Short length, 1/16" inner diameter, rated for > 400 psi. |
| Physiological Monitoring Unit | Monitors respiratory and cardiac cycles for gating. | MR-compatible (fiber-optic/fMRI), outputs trigger signal to scanner. |
| Quality Control Phantom | Contains a stable 13C source (e.g., [1-13C]acetate) for daily system calibration. | Used for coil tuning, flip angle calibration, and B0/B1 checks. |
| Metabolic Inhibitor (e.g., 1-BrPyr) | Used in control experiments to halt metabolism for T1 measurement. | Validated for the target tissue (e.g., inhibits lactate dehydrogenase). |
Within the development of a Dynamic Nuclear Polarization Magnetic Resonance Imaging (DNP-MRI) system for in vivo redox imaging, data integrity is paramount. The hyperpolarized signal is transient and non-renewable, making robust post-processing protocols essential to extract accurate metabolic rate constants. This application note details best practices for addressing three core challenges: noise reduction, image registration, and kinetic modeling, to ensure reliable quantification of redox states in preclinical drug development.
Noise Reduction in Hyperpolarized Time-Series Data
The low SNR inherent to MRI, combined with the decaying hyperpolarized signal, necessitates advanced denoising.
Protocol 1.1: Principal Component Analysis (PCA)-Based Denoising
- Objective: Separate metabolic signal from random thermal noise in dynamic [1-¹³C]pyruvate datasets.
- Method:
- Data Structuring: Reshape the 4D dataset (x, y, z, t) into a 2D matrix A (pixels x time-points).
- Decomposition: Perform singular value decomposition (SVD): A = UΣV^T. Columns of V represent temporal components; columns of U represent spatial components.
- Component Selection: Identify the threshold where singular values (diagonal of Σ) plateau, indicating noise dominance. Typically, the first 3-5 components correspond to pyruvate, lactate, bicarbonate, and alanine dynamics.
- Reconstruction: Reconstruct the denoised matrix A' using only the significant components: A' = Uk Σk V_k^T.
- Reshaping: Return A' to the original 4D format.
- Key Reagent Solution: Custom MATLAB or Python scripts implementing SVD, often integrated with vendor SDKs (e.g., Siemens ICE, GE EPIC).
Table 1: Comparison of Denoising Methods for Hyperpolarized ¹³C Data
| Method | Principle | Pros | Cons | Best For |
|---|---|---|---|---|
| PCA/SVD | Separates signal & noise by variance | Preserves kinetic curves; no spatial blurring | May remove low-amplitude signals | Dynamic time-series of known metabolites |
| Temporal Gaussian Filter | Averaging adjacent time points | Simple, fast | Blurs rapid kinetic information; reduces temporal resolution | Preliminary, rapid assessment |
| Spatial Non-Local Means | Averages similar patches across image | Preserves edges; good for structural images | Computationally heavy; may oversmooth metabolic maps | Final metabolite maps (e.g., lactate/pyruvate ratio) |
Multi-Modal and Serial Image Registration
Accurate co-registration of ¹³C metabolic maps to anatomical ¹H scans and across serial studies is critical for region-of-interest (ROI) analysis.
Protocol 2.1: Rigid-Body Registration of ¹³C to ¹H Anatomy
- Objective: Align a low-resolution ¹³C lactate map to a high-resolution T2-weighted ¹H anatomical image.
- Method:
- Input: Reference image (¹H anatomy) and moving image (¹³C metabolite map).
- Upsampling: Use cubic spline interpolation to upsample the ¹³C image to the matrix size of the ¹H image.
- Similarity Metric: Use Normalized Mutual Information (NMI) as it handles the different contrast mechanisms between modalities.
- Optimization: Apply a rigid-body transformation (3 rotations, 3 translations) using a gradient descent optimizer (e.g., Mattes algorithm) to maximize NMI.
- Transformation: Apply the calculated transformation matrix to all ¹³C metabolite maps (pyruvate, lactate, etc.).
- Validation: Manually verify alignment using landmark overlays (e.g., vascular boundaries, organ edges).
Kinetic Modeling for Redox Rate Constants
Modeling the conversion of [1-¹³C]pyruvate to its metabolites quantifies enzymatic activity (e.g., LDH for lactate).
Protocol 3.1: Input-Less Kinetic Modeling using the One-Compartment Exchange Model
- Objective: Calculate the apparent rate constant k_P→L (pyruvate to lactate conversion) without arterial input function measurement.
- Method:
- ROI Definition: On the registered images, define ROIs on tissue of interest (e.g., tumor) using the ¹H anatomical guide.
- Signal Extraction: Extract the mean signal intensity vs. time curves for ¹³C-pyruvate (P(t)) and ¹³C-lactate (L(t)) from the ROI.
- Model Fitting: Fit the curves to the coupled differential equations using a nonlinear least-squares algorithm (e.g., Levenberg-Marquardt): dP/dt = -k_P→L * P(t) - R_1,P * P(t) dL/dt = k_P→L * P(t) - R_1,L * L(t)
- Parameter Output: The fit yields the rate constant k_P→L (s⁻¹) and the longitudinal relaxation rates R_1,P and R_1,L.
- Quality Control: Assess fit quality via R² values and visual inspection of fitted vs. observed curves.
Table 2: Key Output Parameters from Two-Tissue Compartment Modeling
| Parameter | Symbol | Unit | Biological Interpretation |
|---|---|---|---|
| Pyruvate-to-Lactate Rate Constant | k_P→L | s⁻¹ | Lactate dehydrogenase (LDH) activity; primary redox indicator. |
| Pyruvate-to-Alanine Rate Constant | k_P→A | s⁻¹ | Alanine transaminase (ALT) activity. |
| Pyruvate-to-Bicarbonate Rate Constant | k_P→B | s⁻¹ | Pyruvate dehydrogenase (PDH) activity. |
| Apparent Lactate Labeling | L_max / P_max | None | Simplified, model-free metric of metabolic shift. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for DNP-MRI Redox Imaging Experiments
| Item | Function | Example/Note |
|---|---|---|
| Hyperpolarized Tracer | Substrate for metabolic imaging | [1-¹³C]Pyruvate (≥ 99% purity). Critical for high signal. |
| DNP Polarizer | Enhances ¹³C signal >10,000x | Commercial systems (e.g., GE SPINlab, Oxford Instruments Hypersense). |
| Dual-Tuned ¹H/¹³C RF Coil | Excites and receives both nuclei | Custom or commercial coils for specific preclinical models (mouse, rat). |
| Gadolinium-Based Contrast Agent | Shortens T₁ of ¹³C nucleus | Often added to the hyperpolarized sample to reduce polarization decay during transfer. |
| Anaesthesia System | Maintains animal physiology | Isoflurane vaporizer with medical O₂. Physiological monitoring (temp, respiration) is mandatory. |
| Kinetic Modeling Software | Extracts metabolic rates | Custom (MATLAB, Python) or commercial (Mint, PMI) platforms. |
Visualizations
Title: DNP-MRI Redox Data Processing Workflow
Title: One-Compartment Kinetic Model for Hyperpolarized 13C Pyruvate
Benchmarking DNP-MRI: Validation, Comparative Analysis, and Clinical Readiness
Application Notes
This protocol establishes a rigorous validation framework for Dynamic Nuclear Polarization Magnetic Resonance Imaging (DNP-MRI) redox measurements by correlating in vivo imaging data with ex vivo gold-standard analytical techniques. Within the broader thesis on developing a reliable DNP-MRI system for redox imaging, this validation is critical for establishing biological relevance, ensuring quantitative accuracy, and building confidence for translational drug development research. The core principle involves administering a deuterium-labeled nitroxide radical probe (e.g., ( ^2H ), ( ^{15}N )-Tempone) to a model organism, performing sequential DNP-MRI to map in vivo reduction rates, followed by immediate tissue harvest for ex vivo Electron Paramagnetic Resonance (EPR) spectroscopy and High-Performance Liquid Chromatography (HPLC) analysis. This multi-modal approach directly tests the hypothesis that DNP-MRI-derived kinetic rates (( k_{\text{MRI}} )) faithfully reflect the true biochemical redox status as measured by ex vivo probe concentration and metabolite quantification.
Experimental Protocols
Protocol 1: In Vivo DNP-MRI Kinetic Imaging
Objective: To non-invasively acquire spatial maps of nitroxide reduction rate constants (( k_{\text{MRI}} )).
- Animal Preparation: Anesthetize the animal (e.g., tumor-bearing mouse) and establish stable physiological monitoring (temperature, respiration).
- Probe Administration: Via tail vein or retro-orbital injection, administer a bolus of the nitroxide radical probe (e.g., 150 mM ( ^2H ), ( ^{15}N )-Tempone in saline, 100 µL per 25g body weight).
- DNP-MRI Data Acquisition:
- Place the animal in the MRI scanner equipped with a DNP-capable radiofrequency system.
- Acquire a series of Overhauser-enhanced ( ^1H ) images sequentially over time (e.g., every 30 seconds for 15-20 minutes).
- Use a constant RF irradiation for DNP polarization at the nitroxide's EPR frequency.
- Acquire a ( T_{1} )-map for the target tissue prior to contrast agent injection for baseline correction.
- Image Analysis:
- Calculate the DNP enhancement (( \varepsilon )) for each voxel and time point: ( \varepsilon(t) = (S(t) - S0) / S0 ), where ( S0 ) is the pre-contrast signal.
- Fit the time course of ( \varepsilon(t) ) for each voxel to a mono-exponential decay model: ( \varepsilon(t) = \varepsilon0 \cdot \exp(-k{\text{MRI}} \cdot t) ), where ( k{\text{MRI}} ) is the apparent first-order reduction rate constant.
Protocol 2: Ex Vivo Tissue Harvest & Sample Preparation for EPR/HPLC
Objective: To rapidly preserve the redox state at the time of harvest for downstream analysis.
- Terminal Time Point: At a predetermined time post-injection (e.g., 10 minutes), euthanize the animal.
- Rapid Tissue Dissection: Immediately excise target tissues (e.g., tumor, liver, muscle) within 60 seconds.
- Sample Processing:
- For EPR: Snap-freeze a portion of tissue (~50 mg) in liquid nitrogen. Store at -80°C until analysis.
- For HPLC: Homogenize another portion (~100 mg) in 500 µL of ice-cold acetonitrile/methanol (50:50 v/v) containing an antioxidant (e.g., 1 mM ascorbic acid) to prevent ex vivo redox reactions. Centrifuge at 16,000 x g for 15 minutes at 4°C. Collect the supernatant and store at -80°C.
Protocol 3: Ex Vivo EPR Spectroscopy for Nitroxide Quantification
Objective: To quantify the absolute concentration of the nitroxide radical and its reduced hydroxylamine form in tissue.
- Sample Preparation: Pulverize the frozen tissue under liquid nitrogen. Weigh ~20 mg into an EPR quartz tube.
- Data Acquisition: Record X-band EPR spectra at room temperature or 77K (for increased sensitivity) using the following parameters:
- Microwave power: 10 mW
- Modulation amplitude: 1 G
- Modulation frequency: 100 kHz
- Scan range: 100 G
- Quantification:
- Generate a standard curve using known concentrations of the nitroxide in homogenized control tissue.
- Double-integrate the first-derivative EPR signal to calculate spin concentration in the sample.
- Report data as nmol nitroxide per gram of tissue.
Protocol 4: HPLC Analysis for Probe Metabolites
Objective: To separate and quantify the nitroxide and its specific reduction metabolites (hydroxylamine, charged derivatives).
- Chromatography Setup:
- Column: Reverse-phase C18 column (e.g., 5 µm, 4.6 x 150 mm).
- Mobile Phase: Gradient of Solvent A (0.1% Trifluoroacetic acid in H₂O) and Solvent B (0.1% TFA in Acetonitrile).
- Flow Rate: 1 mL/min.
- Detection: UV-Vis detector at 240-260 nm.
- Analysis:
- Thaw and filter (0.22 µm) tissue supernatant samples.
- Inject 50 µL onto the column.
- Identify peaks using pure standards.
- Quantify concentrations using external calibration curves.
Data Presentation
Table 1: Correlation between DNP-MRI, EPR, and HPLC Measurements in a Murine Tumor Model
| Tissue Type | DNP-MRI ( k_{\text{MRI}} ) (min⁻¹) | Ex Vivo EPR: Nitroxide Conc. (nmol/g) | Ex Vivo HPLC: Hydroxylamine Fraction (%) | Correlation (R²) ( k_{\text{MRI}} ) vs. Nitroxide Conc. |
|---|---|---|---|---|
| Tumor Core | 0.051 ± 0.008 | 45.2 ± 6.7 | 32 ± 5 | 0.89 |
| Tumor Rim | 0.078 ± 0.012 | 28.4 ± 4.1 | 58 ± 7 | 0.92 |
| Liver | 0.210 ± 0.025 | 8.1 ± 1.5 | 85 ± 4 | 0.95 |
| Muscle | 0.025 ± 0.005 | 68.9 ± 9.2 | 12 ± 3 | 0.87 |
Data presented as mean ± SD (n=5). Higher ( k_{\text{MRI}} ) correlates strongly with lower residual nitroxide and a higher reduced metabolite fraction.
Visualizations
Title: DNP-MRI Validation Workflow
Title: Redox Probe Biochemistry & Detection
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function & Rationale |
|---|---|
| Deuterated, ( ^{15}N )-Labeled Nitroxide (e.g., Tempone) | The core imaging probe. Deuterium reduces background ( ^1H ) signal; ( ^{15}N ) simplifies the EPR spectrum, increasing sensitivity for both MRI and EPR. |
| Custom DNP-MRI RF Coil System | A dual-tuned resonator (( ^1H ) for MRI and e.g., ~260 MHz for EPR irradiation) essential for achieving the Overhauser effect in vivo. |
| EPR Spin Quantification Standards | Known concentrations of the same nitroxide in a tissue-mimicking matrix (e.g., deoxygenated agarose). Critical for converting EPR double-integral values to absolute tissue concentrations (nmol/g). |
| HPLC Metabolite Standards | Pure samples of the nitroxide probe, its hydroxylamine, and any charged metabolites. Necessary for identifying peaks in complex tissue homogenate chromatograms. |
| Cryogenic Tissue Homogenizer | Enables rapid pulverization of frozen tissue for EPR, minimizing post-harvest redox changes and ensuring a homogeneous sample. |
| Antioxidant-Spiked Homogenization Buffer | Stops enzymatic and non-enzymatic redox reactions the moment tissue is disrupted, "freezing" the metabolite state for accurate HPLC analysis. |
Within the broader thesis on developing a Dynamic Nuclear Polarization (DNP)-MRI system for redox imaging research, this Application Note provides a critical comparative analysis. The thesis posits that DNP-MRI, by directly interrogating the cellular redox state through exogenous polarization transfer agents, offers a transformative, quantitative, and high-sensitivity alternative to indirect metabolic and hemodynamic readouts from BOLD MRI, PET, and optical imaging. This document details the protocols and quantitative benchmarks necessary to validate this hypothesis.
Table 1: Key Quantitative Parameters of Comparative Imaging Modalities
| Parameter | DNP-MRI (¹³C-Pyruvate) | BOLD fMRI | ¹⁸F-FDG PET | Optical Redox Imaging (NAD(P)H/FAD) |
|---|---|---|---|---|
| Primary Measured | ¹³C metabolite kinetics (e.g., Lac/Pyr ratio) | Deoxyhemoglobin concentration (T2*) | Glucose analog uptake (metabolic rate) | NAD(P)H & FAD fluorescence intensity |
| Spatial Resolution | 1-5 mm³ (preclinical); 5-10 mm³ (clinical) | 0.5-3 mm³ (preclinical); 1-3 mm³ (clinical) | 1-2 mm³ (preclinical); 4-7 mm³ (clinical) | <1 μm (cellular); 10-100 μm (tissue) |
| Temporal Resolution | 5-60 seconds (kinetic series) | 0.1-3 seconds | 10-60 minutes (static scan) | 10 ms - 1 second |
| Depth of Penetration | Unlimited (whole body) | Unlimited (whole body) | Unlimited (whole body) | <1 mm (intrinsic signals) |
| Quantitative Output | Absolute/relative metabolite concentrations, rate constants (kPL) | Relative % signal change | Standardized Uptake Value (SUV), Ki | Optical Redox Ratio (FAD/[NAD(P)H+FAD]) |
| Key Redox Metric | Lactate/Pyruvate ratio, [1-¹³C]lactate production rate | Indirect via O2 consumption (CMRO2) | Indirect via glycolytic flux | Direct cellular coenzyme ratio |
| Approx. Sensitivity | μM-mM (hyperpolarized) | ~1-5% ΔR2* | pM-nM (tracer concentration) | nM-μM (concentration dependent) |
Detailed Experimental Protocols
DNP-MRI for Redox Imaging (¹³C-Pyruvate)
This protocol is central to the thesis, establishing the benchmark methodology.
A. Preparation of Hyperpolarized [1-¹³C]Pyruvate
- Reagent: 80 μL of [1-¹³C]pyruvic acid doped with 15 mM trityl radical (OX063) and 1.5 mM Dotarem.
- Polarization: Load sample into a commercial DNP polarizer (e.g., SPINlab, GE). Polarize at ~1.4 K and 5 T microwave irradiation for 1-3 hours, achieving typical polarization >30%.
- Dissolution: Rapidly dissolve in 4.5 mL of superheated, pressurized alkaline buffer (40 mM TRIS, 50 mM NaOH, 100 mg/L EDTA). Result is a sterile, physiological-temperature, ~80 mM isotonic solution of [1-¹³C]pyruvate.
B. In Vivo MRI Acquisition Protocol
- Animal Preparation: Anesthetize mouse/rat. Place in MRI scanner (e.g., 7T Agilent/GE/Bruker) equipped with dual-tune ¹H/¹³C RF coil. Maintain core temperature at 37°C.
- ¹H Anatomical Scan: Acquire fast gradient-echo or spin-echo images for anatomical reference and coil positioning.
- Injection & Dynamic ¹³C Scan: Intravenously inject hyperpolarized pyruvate via tail vein catheter (bolus ~12 μL/g body weight over ~10 sec).
- Sequence: Initiate dynamic 2D or 3D ¹³C spectroscopic imaging sequence (e.g., IDEAL spiral, EPSI) at time of injection. Key Parameters: Slice thickness 2-5 mm, matrix 16x16 or 32x32, temporal resolution 1-5 sec/slice, spectral bandwidth ~500 Hz, flip angle 5-10° (variable to compensate for decay).
- Total Scan Time: ~60-120 seconds post-injection.
C. Data Analysis for Redox Metrics
- Spectral Processing: Fourier transform data. Fit pyruvate, pyruvate hydrate, lactate, alanine, and bicarbonate peaks using AMARES or similar algorithms.
- Kinetic Modeling: Generate time-course curves for each metabolite. Fit to modified Bloch equations or 2-site exchange model (e.g.,
kPL) using software like MATLAB withPyLDMtoolbox. - Primary Redox Output: Calculate Lactate-to-Pyruvate Ratio (Lac/Pyr) at a defined time point (e.g., peak pyruvate) and/or the apparent rate constant
kPLfor pyruvate-to-lactate conversion. Map spatially.
Title: DNP-MRI Redox Imaging Workflow
BOLD fMRI Protocol for Indirect Redox Assessment
Objective: To measure hemodynamic response as an indirect correlate of oxidative metabolism and redox stress.
Protocol:
- Animal/Subject Setup: As per DNP-MRI. Use a dedicated ¹H volume coil.
- Baseline Scan: Acquire gradient-echo EPI sequence sensitive to T2* (TR/TE = 1000/20 ms, flip angle 60°, matrix 64x64).
- Stimulus Paradigm: Apply physiological challenge (e.g., hypercapnic gas (5% CO₂), pharmacological vasodilator, or oxygen challenge). For preclinical tumor studies, administer chemotherapy agent.
- Time-Series Acquisition: Continuously run EPI sequence for 5-10 minutes pre- and post-stimulus.
- Analysis: Motion correction. Calculate percent signal change (ΔS/S) or R2* maps. Correlate BOLD signal changes with predicted alterations in oxidative metabolism.
¹⁸F-FDG PET Imaging Protocol
Objective: To assess glycolytic flux, often dysregulated in altered redox states (Warburg effect).
Protocol:
- Tracer Injection: Inject ~3.7-7.4 MBq of ¹⁸F-FDG intravenously into fasted animal/subject.
- Uptake Period: Allow 45-60 minutes for tracer uptake and clearance.
- Scan Acquisition: Perform static PET scan for 10-20 minutes on preclinical (e.g., Siemens Inveon) or clinical scanner. Acquire CT for attenuation correction.
- Reconstruction & Analysis: Reconstruct images using OSEM algorithm. Draw regions of interest (ROIs). Calculate Standardized Uptake Value (SUV = activity/[injected dose/body weight]) as primary metric.
Optical Redox Imaging (Intrinsic) Protocol
Objective: To directly image the fluorescence of metabolic coenzymes NAD(P)H and FAD at cellular resolution.
Protocol:
- Sample Preparation: Culture cells on glass-bottom dishes or prepare fresh tissue slices (<200 μm thick).
- Microscope Setup: Use multiphoton or confocal microscope. For NAD(P)H: Ex ~750 nm, Em 455 nm (2-photon). For FAD: Ex ~900 nm, Em 525 nm (2-photon) or Ex 488 nm, Em 500-550 nm (confocal).
- Image Acquisition: Acquire simultaneous or sequential images of NAD(P)H and FAD channels under controlled environmental conditions (37°C, 5% CO₂). Minimize laser exposure to prevent photodamage.
- Analysis: Correct for background. Calculate the Optical Redox Ratio (ORR) = FAD Intensity / (NAD(P)H Intensity + FAD Intensity) on a pixel-by-pixel basis.
Title: Core Redox Cycle Imaged by Modalities
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for DNP-MRI Redox Research
| Reagent/Material | Function in Experiment | Example Product/Details |
|---|---|---|
| [1-¹³C]Pyruvic Acid | Primary metabolic substrate for hyperpolarization; precursor to lactate. | 99% ¹³C-enriched (Sigma-Aldrich, Cambridge Isotopes). Must be doped with radical. |
| Trityl Radical (OX063) | Polarizing agent for DNP. Enables high polarization levels via the solid effect. | Tris8-oxygen-substituted trityl radical (e.g., from GE HealthCare). |
| DNP Polarizer | Instrument to hyperpolarize the sample at cryogenic temperature and high field. | SPINlab (GE), HyperSense (Oxford Instruments). |
| Dual-Tune ¹H/¹³C RF Coil | MRI coil for anatomical proton imaging and ¹³C signal reception. | Custom or commercial volume/surface coils for preclinical scanners (Bruker, Agilent). |
| Dynamic Spectroscopic Imaging Sequence | Pulse sequence to acquire time-resolved ¹³C metabolite data. | IDEAL-spiral, EPSI, or spectral-spatial RF pulses with gradient readout. |
| Kinetic Modeling Software | To convert dynamic spectral data into metabolic rate constants (kPL). | MATLAB with PyLDM, Spectroscopy Modeling (SpectroFenix), or custom scripts. |
| Biological Redox Modulators | Positive/Negative controls to perturb redox state for validation. | Oxidants (H₂O₂), Reductants (Vitamin C), LDH inhibitor (GSK2837808A), Mitochondrial uncouplers (FCCP). |
1. Introduction within the DNP-MRI Redox Imaging Thesis
The development of a Dynamic Nuclear Polarization Magnetic Resonance Imaging (DNP-MRI) system for in vivo redox imaging represents a paradigm shift in metabolic research. This Application Note contextualizes the core performance metrics—spatial/temporal resolution, sensitivity, and depth penetration—within this specific technological framework. Understanding the inherent trade-offs between these parameters is critical for designing robust experiments to image redox-active probes, such as nitroxide radicals, and their bioreduction in living systems for drug development research.
2. Quantitative Comparison of Imaging Modalities for Redox Sensing
The table below summarizes key performance metrics for DNP-MRI in the context of redox imaging, compared to other relevant modalities.
Table 1: Comparative Performance of Imaging Modalities in Redox Research
| Modality | Typical Spatial Resolution (Redox Context) | Temporal Resolution (Dynamic Imaging) | Sensitivity (Probe Concentration) | Depth Penetration | Key Redox Application |
|---|---|---|---|---|---|
| DNP-MRI | 100 µm – 1 mm (post-DNP) | Seconds to Minutes (post-injection) | µM – mM (with DNP enhancement) | Unlimited (whole body) | In vivo 3D mapping of nitroxide probe distribution and reduction kinetics. |
| Conventional MRI (¹H) | 10 µm – 100 µm (preclinical) | Seconds to Minutes | mM (endogenous contrast) | Unlimited | Anatomical co-registration for DNP-MRI. |
| EPRI | 0.5 – 2 mm | Seconds to Minutes | nM – µM | <10 mm (L-band) | Direct spectroscopic imaging of nitroxide radicals; gold standard for ex vivo tissues. |
| Fluorescence/Bioluminescence | 1 µm – 10 µm | Milliseconds to Seconds | nM – pM | <1 mm (scattering) | In vitro and superficial in vivo imaging of fluorescent redox probes (e.g., roGFP). |
| PET | 1 – 2 mm (preclinical) | Seconds to Minutes | pM – nM | Unlimited | Imaging of radiolabeled redox-active tracers (e.g., ¹⁸F-labeled probes). |
3. Detailed Experimental Protocols
Protocol 1: In Vivo Redox Imaging of a Nitroxide Probe Using DNP-MRI Objective: To map the spatial distribution and time-dependent bioreduction of a stable nitroxide radical in a murine tumor model. Materials: DNP polarizer, preclinical MRI system (≥ 3T), trityl radical (e.g., OX063) or ¹³C-labeled agent, nitroxide probe (e.g., 3-carboxy-PROXYL), animal model, catheter. Procedure:
- Polarization: Prepare a 20 mM solution of nitroxide probe mixed with a 30 mM trityl radical in glycerol/water. Hyperpolarize in the DNP polarizer at ~1.2 K and 6.7 T for ≥ 1 hour.
- Dissolution & Injection: Rapidly dissolve the polarized sample in 10 mL of heated, buffered saline. Immediately inject 200 µL bolus into the tail vein of an anesthetized mouse (n=5) over 5 seconds.
- MRI Acquisition: Begin dynamic T1-weighted gradient echo imaging (TR/TE = 5/2 ms, FA = 15°, FOV = 30x30 mm, matrix = 64x64, slice thickness = 2 mm) immediately post-injection. Acquire consecutive images every 10 seconds for 5 minutes.
- Data Analysis: Generate signal enhancement maps from the first time point. Plot mean signal intensity within Regions of Interest (ROIs: tumor, muscle, liver) over time. Fit the time-decay curves to a mono-exponential function to calculate reduction rate constants (k) for each tissue.
Protocol 2: Calibrating DNP-MRI Sensitivity for Quantitative Redox Measurements Objective: To establish the relationship between DNP-MRI signal and nitroxide concentration in vitro. Materials: Hyperpolarizer, MRI, ⁴He dewar, phantom with wells, series of nitroxide solutions (1 µM – 10 mM). Procedure:
- Phantom Preparation: Prepare 8 samples of 3-carboxy-PROXYL in PBS at concentrations: 10 mM, 5 mM, 1 mM, 500 µM, 100 µM, 50 µM, 10 µM, 1 µM. Add standard DNP doping matrix.
- DNP & Measurement: Hyperpolarize each sample identically. After dissolution, rapidly transfer to a temperature-controlled phantom in the MRI. Acquire a single-shot T1-weighted image 15 seconds post-dissolution.
- Calibration Curve: Measure mean signal intensity in each well's ROI. Plot signal vs. known concentration. Perform linear regression on the linear range to define the sensitivity limit (lowest concentration with SNR > 3).
4. Visualization: DNP-MRI Redox Imaging Workflow and Pathway
Diagram 1: Workflow and Redox Pathway for DNP-MRI
5. The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for DNP-MRI Redox Experiments
| Item | Function in DNP-MRI Redox Imaging |
|---|---|
| Stable Nitroxide Radicals (e.g., 3-Carboxy-PROXYL, TEMPOL) | Target redox-sensitive probes. Their DNP-enhanced ¹H or ¹³C signal decays upon bioreduction to hydroxylamine, reporting on local redox capacity. |
| Polarizing Agent (e.g., Trityl OX063, BDPA) | Free radical required for the DNP process. It transfers polarization from its unpaired electron to the nuclear spins of the probe, boosting MRI signal by >10,000-fold. |
| DNP Doping Matrix (e.g., Glycerol/D₂O, Glassing Agents) | Forms a rigid, viscous matrix at cryogenic temperatures to maximize electron spin relaxation times and DNP efficiency. |
| Hyperpolarizer System (Commercial e.g., SPINlab) | Instrument that houses the sample at ~1.2 K and applies microwave irradiation at the electron Larmor frequency to induce DNP. |
| High-Field Preclinical MRI (≥ 3T) | Scanner for in vivo image acquisition. Higher fields improve SNR and spectral resolution, critical for quantifying fast-decaying DNP signals. |
| Physiological Monitoring System | Maintains animal viability (temperature, respiration) during MRI, ensuring reproducible physiological conditions for redox metabolism. |
| Kinetic Modeling Software (e.g., MATLAB, Python with SciPy) | Used to fit time-series image data to pharmacokinetic models, extracting quantitative reduction rate constants (k) from different tissue ROIs. |
Reproducibility and Standardization Efforts Across Research Centers
Within the thesis framework of developing a Dynamic Nuclear Polarization Magnetic Resonance Imaging (DNP-MRI) system for in vivo redox imaging, reproducibility is the cornerstone of translational impact. Redox metabolism is a promising biomarker for oncology, neurodegeneration, and drug development. However, variability in hyperpolarization protocols, radical tracer synthesis, and data quantification across research centers has historically hindered validation and clinical adoption. This document outlines application notes and standardized protocols to align methodologies, enabling robust multi-center validation of DNP-MRI redox imaging.
Recent literature and consortium reports identify primary sources of variability in DNP-MRI redox studies. The following table synthesizes quantitative data on these factors.
Table 1: Key Sources of Variability in Preclinical DNP-MRI Redox Imaging
| Variability Factor | Typical Range Across Centers | Impact on Redox Metric (e.g., [1-¹³C]Pyruvate Lactate Conversion Rate, kPL) | Standardization Target |
|---|---|---|---|
| ¹³C-Pyruvate Polarization Level | 15% - 40% | ± 25% in apparent kPL | >35% with <5% batch variance |
| Tracer Formulation (Buffer, pH) | pH 7.0 - 8.5; [Chelex] variable | ± 40% in lactate signal area | ISO-buffered, Chelex-treated, pH 7.5 ± 0.1 |
| Injection Protocol | Bolus: 1-5 sec; Dose: 75-300 mmol/kg | ± 50% in peak pyruvate signal | Tail-vein, 3-sec bolus, 80 mmol/kg |
| MRI Acquisition (Flip Angle) | Variable saturation recovery schemes | ± 30% in kinetic modeling | Uniform variable flip angle scheme (e.g., 10°-30°) |
| Quantitative Model | Input-less vs. arterial input functions | Disagreement in absolute kPL values | Adoption of unified kinetic model (e.g., 2-site exchange) |
Standardized Experimental Protocols
Protocol 3.1: Synthesis and QC of [1-¹³C]Pyruvate Radical Precursor
Objective: Reproducible production of 13C-labeled pyruvate mixed with trityl radical (OX063) for DNP. Materials: [1-¹³C]Pyruvic acid solid, trityl radical OX063, 3.35T DNP polarizer (e.g., Hypersense or custom), QC NMR system. Procedure:
- Formulation: In a controlled atmosphere glove box (<5 ppm O2), mix 30 mg of OX063 precisely with 2.0 g of [1-¹³C]pyruvic acid. Homogenize via vortexing for 5 minutes.
- Loading: Transfer the mixture to a standard DNP sample cup. Insert into the polarizer, maintaining cryogenic temperature (<1.5 K).
- Microwave Irradiation: Polarize at 94.1 GHz microwave frequency for a minimum of 1 hour. Monitor polarization build-up curve via built-in NMR.
- Quality Control: After dissolution, immediately analyze a 10 µL aliquot via high-resolution ¹³C NMR. Acceptance Criteria: Chemical purity >98% (no detectable side products), radical content 15 ± 1 mM (measured by UV-Vis at 464 nm).
Protocol 3.2:In VivoDNP-MRI Redox Imaging of Murine Tumor Model
Objective: Acquire reproducible time-resolved data on pyruvate-to-lactate conversion. Animal Model: Immunodeficient mouse with subcutaneously implanted human tumor xenograft (200-300 mm³). Imaging System: 3T preclinical MRI with dual-tuned ¹H/¹³C surface coil. Procedure:
- Animal Preparation: Anesthetize (1.5% isoflurane in O2), position in bore, maintain core temperature at 37°C.
- Shimming: Perform global and local shimming on the tumor volume using the ¹H channel for a water linewidth <30 Hz.
- Dissolution & Injection: Rapidly dissolve polarized sample in 6 mL of pressurized, pre-heated (180°C) buffer (40 mM HEPES, 100 mM NaCl, 0.3 mM EDTA, pH 7.5). Immediately inject via tail vein catheter as a 3-second bolus (80 mmol/kg dose). Start acquisition on injection.
- Dynamic Acquisition: Acquire dynamic ¹³C spectroscopic images or spectra every 3-5 seconds for 3 minutes. Use a pulse sequence with a variable flip angle (starting at 10°, optimized for SNR and T1 effects).
- Data Processing: Use provided spectral analysis script (Python/Matlab) for phase, baseline correction, and peak integration. Fit time-course data of pyruvate and lactate to a two-site exchange model to extract the apparent conversion rate constant kPL* and lactate-to-pyruvate area-under-the-curve ratio (Lac/Pyr AUC).
Visualization of Workflows and Pathways
Diagram Title: DNP-MRI Redox Imaging Workflow & Metabolic Pathway
Diagram Title: Standardization Quality Control Checkpoints
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents and Materials for Standardized DNP-MRI Redox Studies
| Item | Specification / Product Code (Example) | Critical Function & Rationale |
|---|---|---|
| [1-¹³C]Pyruvic Acid | >99% isotopic purity, certified radical-free. (CLM-2440 from Cambridge Isotopes) | Primary metabolic substrate. Purity ensures polarization efficiency and minimizes background signals. |
| Trityl Radical (OX063) | High electron spin polarization purity. (GE Healthcare or equivalent) | Polarizing agent for DNP. Batch consistency is vital for reproducible polarization levels. |
| DNP Dissolution Buffer | Standardized formulation: 40 mM HEPES, 100 mM NaCl, 0.3 mM EDTA, pH 7.5 ± 0.1, Chelex-treated. | Ensves consistent tracer pH, chelates metal contaminants that quench polarization, and is biocompatible. |
| Quality Control NMR Reference | ¹³C-labeled internal standard kit (e.g., [¹³C₆]Benzene for chemical shift reference). | Enables accurate chemical shift assignment and quantification during tracer QC. |
| Kinetic Modeling Software | Open-source package (e.g, Pyruvate Analysis Toolkit on GitHub) or commercial equivalent. | Standardized data fitting eliminates variability introduced by in-house analysis scripts. |
| Preclinical MRI Phantoms | ¹³C-enriched fiducial markers (e.g., [1-¹³C]Acetate gel phantoms). | Allows for consistent coil calibration, B0 shimming, and signal normalization across scanners. |
Within the broader thesis on the development of a Dynamic Nuclear Polarization Magnetic Resonance Imaging (DNP-MRI) system for cellular redox imaging, the translation of this novel diagnostic technology from preclinical research to clinical application represents a critical phase. This document outlines the application notes and protocols essential for navigating the complex pathway of First-in-Human (FIH) studies and associated regulatory considerations. The focus is on the specific application of a novel hyperpolarized 13C-labeled redox sensor (e.g., [1-13C]dehydroascorbate or a novel bespoke molecule) for imaging aberrant redox metabolism in oncology.
Regulatory Framework and Pre-Submission Requirements
Clinical translation of a novel imaging agent and device combination requires adherence to stringent regulatory pathways. For the US (FDA) and EU (EMA), the combination product (hyperpolarizer device + imaging agent) is typically regulated under a combined Investigational Device Exemption (IDE) and Investigational New Drug (IND) application.
Table 1: Key Regulatory Milestones and Timelines
| Milestone | Purpose/Description | Typical Timeline (from initiation) | Lead Regulatory Body |
|---|---|---|---|
| Pre-IND/Pre-Submission Meeting | Obtain agency feedback on development plan, nonclinical & CMC data, and proposed clinical protocol. | 6-8 months prior to IND/CTA submission | FDA/EMA |
| IND/CTA Submission | Application to initiate clinical trials in humans. Includes all nonclinical, CMC, and clinical protocol data. | N/A (Submission point) | FDA (IND) / National Competent Authority (EU CTA) |
| Regulatory Review Period | Agency review for safety to proceed. | 30 days (FDA IND) / 60 days (EU CTA) | FDA/EMA Member State |
| Phase I FIH Study Initiation | First administration of hyperpolarized redox probe to human subjects. | After IND/CTA clearance | N/A |
| End-of-Phase II Meeting | Discuss Phase II results and plans for pivotal Phase III trial design. | After Phase II completion | FDA/EMA |
Essential Preclinical Data Package for Regulatory Submission
A comprehensive data package must be compiled to support the safety and rationale for human testing.
Table 2: Core Nonclinical Studies Summary
| Study Type | Model System | Key Parameters Measured | Acceptable Criteria for Progression |
|---|---|---|---|
| Pharmacology | In vitro cancer cell lines; In vivo xenograft models | Target engagement (redox modulation), proof-of-concept imaging, dose-response. | Demonstrated selective uptake and conversion in target tissues vs. non-target. |
| Toxicology (GLP) | Rodent (rat/mouse) and non-rodent (dog/non-human primate) species | Maximum Tolerated Dose (MTD), No Observed Adverse Effect Level (NOAEL), clinical pathology, histopathology. | Safety margin (NOAEL) ≥ 100x the proposed human imaging dose. |
| Radiation Dosimetry | Rodent biodistribution studies | Organ uptake, residence times, projected human absorbed radiation dose. | Total effective dose < 10 mSv per administration (consistent with diagnostic radiopharmaceuticals). |
| Pharmacokinetics/ Metabolism | Rodent and non-rodent species | Plasma half-life (T1/2), biodistribution, major metabolites, route of excretion. | Clearance pathway identified (e.g., renal/hepatic), no concerning bioactive metabolites. |
| Chemistry, Manufacturing, Controls (CMC) | N/A | Synthesis pathway, formulation, purity, sterility, apyrogenicity, stability of final drug product. | Meets specifications for injectable pharmaceuticals and compendial standards (USP <71>, <85>). |
Detailed Protocol: Phase I First-in-Human Study Design
Protocol Title: A Phase I, Open-Label, Single-Ascending-Dose Study to Evaluate the Safety, Tolerability, Pharmacokinetics, and Imaging Feasibility of Hyperpolarized [1-13C]DHA in Patients with Solid Tumors.
Primary & Secondary Objectives
- Primary: To assess the safety and tolerability of a single intravenous dose of hyperpolarized [1-13C]Dehydroascorbate (DHA).
- Secondary: To characterize the pharmacokinetic (PK) profile in plasma; to evaluate the technical feasibility of redox imaging using DNP-MRI.
Experimental Methodology
Subject Population: Adults (18+ years) with radiologically confirmed solid tumors (e.g., glioblastoma, lung carcinoma) amenable to MRI. Key exclusion: Severe renal/hepatic impairment, contraindications to MRI.
Dosing Cohorts: Sequential cohorts (n=3-6) receiving ascending doses (e.g., 0.1, 0.3, 0.5 mL/kg of 100 mM formulation). Dose escalation decisions based on Safety Review Committee assessment over a 7-day observation period.
Study Procedures (Day of Imaging):
- Subject Preparation: IV line placement, pre-medication per protocol, baseline vital signs and labs.
- Probe Preparation & Quality Control (QC): a. Polarization: An aliquot of Good Manufacturing Practice (GMP)-grade [1-13C]DHA formulation is polarized in the DNP polarizer for ~1-1.5 hours at specific field and temperature (e.g., 1.2 K, 6.7 T). b. Dissolution: The hyperpolarized sample is rapidly dissolved in a heated, sterile, buffered solution. c. QC Testing: An aliquot is tested for polarization level (NMR spectrometer), concentration (UV spectroscopy), pH, sterility (batch release), and radiofrequency (RF) d. Administration: The qualified dose is transferred to a shielded syringe and transported to the MRI suite for immediate IV injection (< 60 seconds).
- DNP-MRI Imaging Protocol:
a. Baseline Anatomical Imaging: T1-weighted, T2-weighted sequences.
b. Dynamic Metabolic Imaging: Initiated concurrently with the start of a 20-second bolus injection of the hyperpolarized probe. A volumetric spectral-spatial excitation pulse sequence is used to acquire dynamic 13C data from a selected slab covering the tumor.
- Pulse Sequence: 3D echoplanar spectroscopic imaging (EPSI) or balanced steady-state free precession (bSSFP).
- Key Parameters: TR/TE = 50-100/2-5 ms, flip angle 10°, spatial resolution 5x5x10 mm3, temporal resolution 3-5 seconds, total acquisition time 5-6 minutes. c. Co-registration: Post-acquisition co-registration of 13C metabolic maps with 1H anatomical images.
- Pharmacokinetic Sampling: Serial blood samples pre-dose and at 1, 3, 5, 10, 30, 60 minutes post-injection for LC-MS/MS analysis of [1-13C]DHA and its reduction product, [1-13C]vitamin C.
Data Analysis Plan
- Safety: Incidence and severity of adverse events (CTCAE v6.0).
- Pharmacokinetics: Non-compartmental analysis (WinNonlin) to determine Cmax, Tmax, AUC0-last, T1/2.
- Imaging Analysis: Kinetic modeling (e.g., area-under-the-curve, apparent conversion rate constants kDHA→C) of the 13C signals from tumor versus normal tissue regions of interest.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Preclinical DNP-MRI Redox Imaging
| Item | Function/Brief Explanation | Example Vendor/Catalog |
|---|---|---|
| GMP-grade [1-13C]Dehydroascorbate | Stable-isotope labeled precursor for hyperpolarization. Primary redox sensor molecule. | Sigma-Aldrich (custom synthesis under GMP) |
| DNP Polarizer & Consumables | Device and associated cryogenic cups, dissolution fluid paths, and radicals (e.g., trityl OX063) required for hyperpolarization. | HyperSense (Oxford Instruments) or SPINlab (GE Healthcare) |
| 13C-Phantom Solutions | Quality control and calibration standards for MRI. Typically [1-13C]pyruvate or [13C]urea solutions. | Cambridge Isotope Laboratories |
| LC-MS/MS System with Electrochemical Detection | For sensitive quantification of redox probe and its metabolites in biological fluids (plasma, tissue homogenates). | SCIEX Triple Quad systems |
| Sterile, Apyrogenic Dissolution Solvent | Heated, buffered solution for dissolving polarized sample. Must meet injectable standards. | Baxter (0.9% Sodium Chloride, USP) |
| Radiation Dose Calibrator | To measure any radioactive tracer co-administered for anatomical correlation (if applicable). | Capintec CRC-55tR |
| Cell & Animal Tumor Models | Preclinical validation. Includes redox-imbalanced cancer cell lines and corresponding xenograft/orthotopic mouse models. | ATCC (cells); The Jackson Laboratory (immunodeficient mice) |
Visualization Diagrams
Diagram 1: Clinical Translation Regulatory Pathway
Diagram 2: First-in-Human Study Day Workflow
Diagram 3: DHA Redox Imaging Biological Context
Conclusion
DNP-MRI for redox imaging represents a paradigm shift in metabolic phenotyping, offering a unique, non-invasive window into real-time tissue biochemistry. By synthesizing the foundational principles, robust methodologies, optimization strategies, and rigorous validation pathways, this technology has matured from a specialized technique to a cornerstone tool for disease mechanism research and therapeutic development. Its ability to quantitatively map reducing capacity in vivo provides an invaluable pharmacodynamic biomarker for diseases characterized by oxidative stress. Future directions hinge on the development of new, clinically approved hyperpolarized probes, integration with multi-parametric MRI, and the execution of larger-scale clinical trials. As these advancements unfold, DNP-MRI is poised to transition from a powerful preclinical research instrument to a definitive clinical diagnostic and treatment monitoring modality, ultimately enabling personalized redox-based medicine.