Targeting Inflammation: A Comparative Study on the Efficacy and Mechanisms of Novel MsrB1 Inhibitors
This article provides a comprehensive comparative analysis of Methionine sulfoxide reductase B1 (MsrB1) inhibitors, a promising therapeutic class for modulating inflammatory responses.
Targeting Inflammation: A Comparative Study on the Efficacy and Mechanisms of Novel MsrB1 Inhibitors
Abstract
This article provides a comprehensive comparative analysis of Methionine sulfoxide reductase B1 (MsrB1) inhibitors, a promising therapeutic class for modulating inflammatory responses. Aimed at researchers and drug development professionals, it covers the foundational biology of MsrB1 in immune regulation, explores advanced high-throughput screening methodologies like the RIYsense biosensor, and addresses key challenges in inhibitor optimization. The content systematically compares the efficacy, binding mechanisms, and functional impacts of newly identified compounds, validating their effects in cellular and in vivo models. By synthesizing cutting-edge research, this review aims to establish a framework for developing MsrB1-targeted therapies for inflammatory diseases and cancer immunotherapy.
MsrB1 Biology and Its Validation as a Therapeutic Target for Inflammatory Diseases
Methionine sulfoxide reductase B1 (MsrB1) is a selenoprotein that plays a critical role in cellular redox homeostasis by specifically reducing methionine-R-sulfoxide (Met-R-SO) residues in proteins back to methionine [1]. This enzymatic activity distinguishes it from other methionine sulfoxide reductases: MsrA reduces methionine-S-sulfoxide (Met-S-SO), while MsrB2 and MsrB3 target Met-R-SO in mitochondria and endoplasmic reticulum, respectively [2]. MsrB1's unique presence in the cytosol and nucleus of mammalian cells, coupled with its utilization of selenocysteine in its catalytic site, provides it with superior catalytic efficiency compared to cysteine-containing counterparts [1]. The enzyme functions as a crucial component of the cellular antioxidant system, with growing evidence supporting its role as a regulatory switch for protein function through reversible oxidation/reduction of specific methionine residues [2].
The significance of MsrB1 extends beyond basic protein repair to encompass critical physiological processes, including immune regulation, actin dynamics, and cellular signaling [3] [2]. Genetic studies have revealed that MsrB1 deficiency leads to increased oxidative stress parameters, particularly in liver and kidney tissues, highlighting its tissue-specific importance in redox control [4]. This article provides a comprehensive comparison of MsrB1's function against other redox systems, examines recently identified inhibitors, and details experimental approaches for studying this therapeutically relevant enzyme.
Enzymatic Mechanism and Comparative Biology of MsrB1
Structural Characteristics and Catalytic Mechanism
MsrB1 possesses a distinctive structural organization that enables its specialized catalytic function. The enzyme features a central structured core containing two β-sheets and a highly flexible N-terminal region that contributes to its substrate interactions [5]. A defining characteristic of mammalian MsrB1 is its incorporation of selenocysteine (Sec95) at the active site, which replaces the cysteine residue found in bacterial MsrBs and provides enhanced catalytic efficiency [6] [5]. The enzyme also binds a zinc ion coordinated by four conserved cysteine residues, which plays a structural role in maintaining the protein's stability and function [5].
The catalytic mechanism of MsrB1 involves a series of precisely coordinated redox reactions. The enzyme utilizes thioredoxin as its natural reducing agent, which regenerates the active enzyme after each catalytic cycle [1]. The reduction of methionine-R-sulfoxide proceeds through a selenenylsulfide intermediate involving the catalytic selenocysteine (Sec95) and a resolving cysteine (Cys4) [5]. This mechanism differs fundamentally from those employed by cysteine-containing MsrBs, particularly in the formation of distal selenenylsulfide bonds and the specific residues required for catalysis [5]. The intricate catalytic process allows MsrB1 to specifically recognize and reduce the R-form of methionine sulfoxide while exhibiting minimal activity toward free methionine sulfoxide [2].
Table 1: Comparative Features of Mammalian Methionine Sulfoxide Reductases
| Feature | MsrB1 | MsrA | MsrB2 | MsrB3 |
|---|---|---|---|---|
| Substrate Specificity | Protein Met-R-SO | Protein & free Met-S-SO | Protein Met-R-SO | Protein Met-R-SO |
| Cellular Localization | Cytosol & nucleus | Cytosol, nucleus & mitochondria | Mitochondria | ER & mitochondria |
| Catalytic Residue | Selenocysteine | Cysteine | Cysteine | Cysteine |
| Cofactor/Metal | Zinc | None | None | None |
| Reducing System | Thioredoxin | Thioredoxin | Thioredoxin | Thioredoxin |
Biological Functions and Physiological Significance
MsrB1 serves multiple biological roles that extend beyond its fundamental function in protein repair. In knockout mouse models, MsrB1 deficiency resulted in significantly reduced MsrB activity, with the most pronounced effects observed in liver and kidney tissues [4]. These animals exhibited increased oxidative damage markers, including elevated levels of malondialdehyde, protein carbonyls, protein methionine sulfoxide, and oxidized glutathione, along with reduced levels of free and protein thiols [4]. This oxidative imbalance demonstrates the critical contribution of MsrB1 to tissue-specific redox homeostasis.
The regulatory functions of MsrB1 are particularly significant in the context of immune response and inflammatory regulation. Research has shown that MsrB1 is highly expressed in macrophages and is further induced by lipopolysaccharide (LPS) stimulation [3]. Genetic ablation of MsrB1 leads to attenuated induction of anti-inflammatory cytokines such as IL-10 and IL-1 receptor antagonist, while promoting excessive production of pro-inflammatory cytokines [3]. This imbalance results in enhanced acute tissue inflammation in experimental models, positioning MsrB1 as a crucial modulator of immune homeostasis. Additionally, MsrB1 participates in regulating actin dynamics by reducing methionine-R-sulfoxide residues oxidized by Mical proteins, thereby facilitating actin repolymerization and maintaining cytoskeletal integrity [2].
Comparative Analysis of MsrB1 Inhibitors: Efficacy and Experimental Evidence
Recently Identified MsrB1 Inhibitors and Their Characteristics
Recent high-throughput screening efforts have identified two potent MsrB1 inhibitors that exhibit significant efficacy in both biochemical and cellular assays. These compounds were discovered using a novel redox protein-based fluorescence biosensor (RIYsense) that enables quantitative measurement of Met-R-O reduction [7]. The RIYsense biosensor incorporates MsrB1, a circularly permutated yellow fluorescent protein (cpYFP), and thioredoxin1 in a single polypeptide chain, allowing ratiometric fluorescence detection of methionine sulfoxide reduction activity [7]. From 6,868 compounds screened, two heterocyclic, polyaromatic compounds demonstrated superior inhibitory effects through comprehensive validation including molecular docking simulations, affinity assays, and HPLC analysis [7].
Table 2: Characteristics of Identified MsrB1 Inhibitors
| Compound Characteristics | Inhibitor 1 | Inhibitor 2 |
|---|---|---|
| Chemical Name | 4-[5-(4-ethylphenyl)-3-(4-hydroxyphenyl)-3,4-dihydropyrazol-2-yl]benzenesulfonamide | 6-chloro-10-(4-ethylphenyl)pyrimido[4,5-b]quinoline-2,4-dione |
| Chemical Structure | Heterocyclic with substituted phenyl moieties | Heterocyclic, polyaromatic with substituted phenyl moiety |
| Inhibitory Activity | Strong inhibition confirmed by multiple assays | Strong inhibition confirmed by multiple assays |
| Binding Affinity | High affinity for MsrB1 active site | High affinity for MsrB1 active site |
| Molecular Docking | Interacts with MsrB1 active site | Interacts with MsrB1 active site |
| Cellular Effects | Decreased anti-inflammatory cytokine expression | Decreased anti-inflammatory cytokine expression |
| In Vivo Impact | Auricular skin swelling & increased thickness in ear edema model | Auricular skin swelling & increased thickness in ear edema model |
Functional Assessment of Inhibitor Efficacy
The physiological impact of MsrB1 inhibition has been rigorously evaluated through both genetic and pharmacological approaches. MsrB1 knockout mice provide a genetic model of enzyme deficiency, demonstrating that MsrB1 loss attenuates anti-inflammatory cytokine production (IL-10, IL-1rn) while enhancing pro-inflammatory responses [3]. Similarly, administration of the newly identified MsrB1 inhibitors effectively recapitulated the inflammatory phenotype observed in knockout animals, causing significant auricular skin swelling and increased thickness in an ear edema model [7]. These findings confirm that pharmacological inhibition of MsrB1 successfully mimics genetic ablation, validating these compounds as effective tools for modulating MsrB1-dependent inflammatory pathways.
The mechanistic basis for MsrB1's role in immune regulation involves its influence on macrophage polarization and metabolic reprogramming. Recent research has revealed that MsrB1 regulates GAPDH oxidation, which in turn shapes metabolic and inflammatory signatures during macrophage activation [8]. MsrB1-deficient macrophages exhibit altered redox control of glycolytic enzymes, resulting in skewed inflammatory responses and enhanced inflammasome activation [8]. This metabolic regulation provides a programmatic mechanism through which MsrB1 activity influences immune outcomes, offering potential therapeutic targets for inflammatory conditions.
Experimental Protocols for MsrB1 Research
RIYsense Biosensor Construction and Screening Protocol
The development of the RIYsense biosensor represents a significant advancement in high-throughput screening for MsrB1 inhibitors. The experimental workflow involves the following key steps:
Molecular Cloning: The coding sequences of mouse MsrB1 and human thioredoxin1 (Trx1) are synthesized and amplified by PCR. Site-directed mutagenesis is performed on human Trx1 (Cys393 to Ser393) and mouse MsrB1 (Sec95 to Cys95 for active form; Sec95 to Ser95 for inactive form) [7].
Vector Construction: The cpYFP from the HyPer sensor is cloned and used to construct recombinant DNA, sequentially assembling MsrB1/cpYFP/Trx1 in a pET-28a vector named RIYsense [7].
Protein Expression and Purification: The recombinant RIYsense construct is transformed into Rosetta2 pLysS cells and cultured in LB medium with ampicillin. Protein expression is induced with 0.7 mM IPTG at 18°C for 18 hours. Cells are harvested, lysed by sonication, and the supernatant is purified using affinity chromatography with a HisTrap HP column [7].
Fluorescence Spectroscopy: The purified RIYsense protein is reduced using 50 mM DTT for 30 minutes at room temperature and desalted. For measurements, RIYsense protein (100 μL) is incubated with or without substrate (10 μL of 500 μM N-AcMetO) in 20 mM Tris-HCl buffer (pH 8.0) for 10 minutes at RT [7].
High-Throughput Screening: The biosensor is used to screen compound libraries by monitoring changes in relative fluorescence intensity (RFI = 485 nm/420 nm). Compounds reducing relative fluorescence intensity by more than 50% compared to control are selected as potential inhibitors [7].
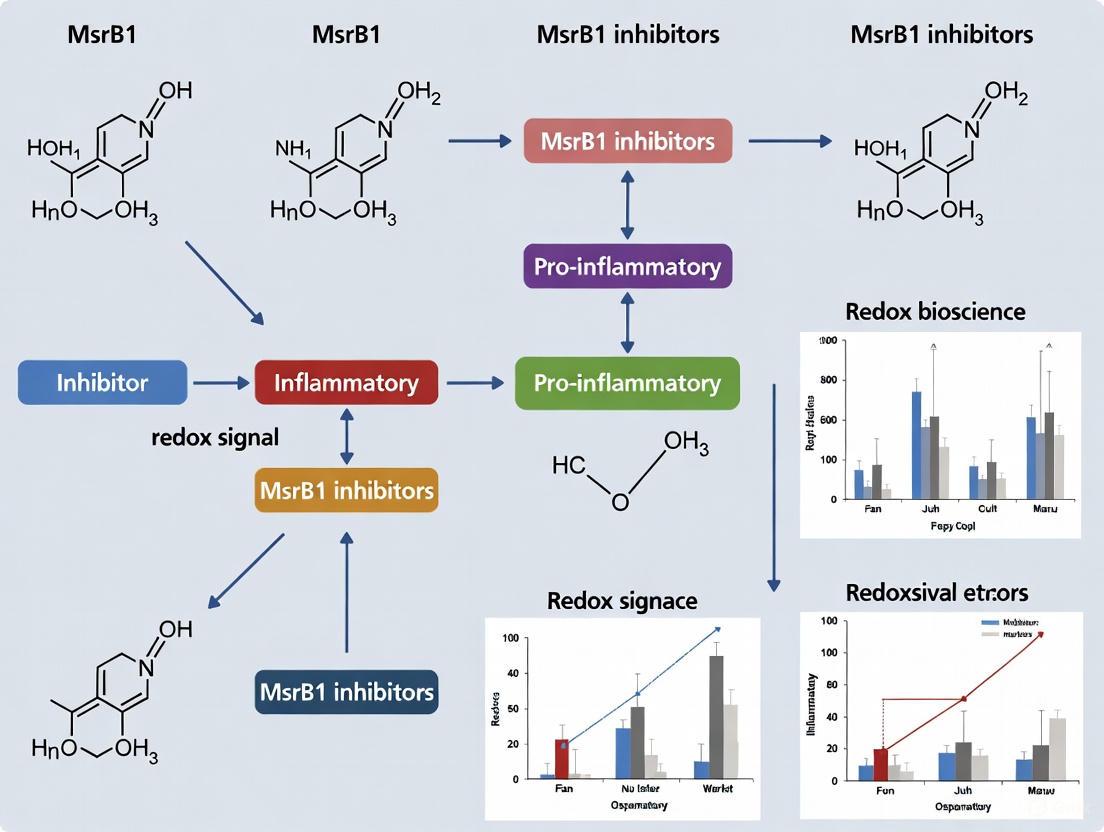
Figure 1: High-Throughput Screening Workflow for MsrB1 Inhibitor Identification
MsrB1 Knockout Mouse Generation and Phenotypic Analysis
Genetic ablation of MsrB1 in mice provides a valuable model for studying its physiological functions. The experimental approach includes:
Gene Targeting Strategies: Two separate targeting constructs are prepared to target the MsrB1 gene by homologous recombination. A 4550-bp region upstream of the first exon of MsrB1 is amplified by nested PCR and cloned into the pPNT targeting vector [4].
Alternative Genetrap Approach: A mouse in a 129/Sv genetic background is generated using a genetrap cassette inserted immediately downstream of the MsrB1 gene. Homozygous MsrB1 KO mice are obtained by mating heterozygous mice and selecting through genetic screening [4].
Biochemical Phenotyping: Tissues from wild-type and knockout mice are glass-homogenized and sonicated in PBS with protease inhibitors and EDTA. Tissues extracts are analyzed for Msr activity, oxidative stress parameters (malondialdehyde, protein carbonyls, protein methionine sulfoxide, oxidized glutathione), and thiol levels [4].
Metabolic Labeling: Mice are injected with 75Se-selenite and maintained for 2 days before tissue extraction. Protein extracts from various tissues are subjected to SDS-PAGE, transferred to membranes, and analyzed with a PhosphorImager to detect selenoprotein expression [4].
Inflammatory Challenge: MsrB1 knockout and wild-type mice are intraperitoneally injected with LPS (10 µg/g), and sera are collected after 4 hours for cytokine analysis using ELISA. For local inflammation models, TPA in acetone is applied to mouse auricles, with thickness measured after 24 hours and tissue samples preserved for histological analysis [3].
Research Reagent Solutions for MsrB1 Investigations
Table 3: Essential Research Tools for MsrB1 Studies
| Reagent/Category | Specific Examples | Research Application | Function/Purpose |
|---|---|---|---|
| Molecular Biology Tools | RIYsense biosensor construct | High-throughput inhibitor screening | Ratiometric fluorescence detection of MsrB1 activity |
| MsrB1 siRNA | Gene silencing in cell culture | Down-regulation of MsrB1 expression | |
| MsrB1 knockout mice | In vivo functional studies | Genetic model of MsrB1 deficiency | |
| Biochemical Assays | 75Se-selenite labeling | Selenoprotein detection | Metabolic labeling of MsrB1 and other selenoproteins |
| NADPH consumption assay | Enzyme activity measurement | Quantitative assessment of MsrB1 activity | |
| HPLC analysis | Met-R-O reduction quantification | Direct measurement of substrate conversion | |
| Cell Culture Models | Bone marrow-derived macrophages (BMDMs) | Immune response studies | Primary cells for inflammation and redox signaling |
| HEK 293 cells | General cellular studies | Model system for MsrB1 expression and localization | |
| In Vivo Models | LPS challenge model | Systemic inflammation | Assessment of cytokine response in intact organism |
| TPA-induced ear edema | Local inflammation model | Evaluation of tissue-specific inflammatory response |
MsrB1 emerges as a sophisticated redox regulator with programmatic functions in controlling inflammatory and metabolic pathways in immune cells. The development of specific inhibitors through advanced screening technologies provides powerful tools for dissecting MsrB1's biological functions and exploring its therapeutic potential. The convergence of evidence from genetic models, biochemical studies, and pharmacological interventions strongly supports MsrB1 as a promising target for immune modulation, particularly in contexts where enhanced inflammation may be therapeutically beneficial, such as in chronic infections, vaccine adjuvants, and cancer immunotherapy [7] [9].
Future research directions should focus on identifying additional physiological substrates of MsrB1 beyond actin and TRPM6, elucidating the precise molecular mechanisms through which MsrB1 regulates metabolic reprogramming in macrophages, and exploring the tissue-specific functions of this selenoprotein in different pathological conditions. The integration of structural biology, chemical biology, and genetic approaches will continue to advance our understanding of this sophisticated redox regulator and its potential applications in therapeutic development.
Figure 2: MsrB1 Regulatory Network in Inflammation and Metabolism
Biological Functions of MsrB1 in Immune Cells
Methionine sulfoxide reductase B1 (MsrB1) is a selenoprotein that catalyzes the reduction of methionine-R-sulfoxide (Met-R-SO) back to methionine, playing a crucial role in post-translational redox regulation of proteins [10] [3]. Unlike other MsrB forms (MsrB2 and MsrB3) that localize to mitochondria and endoplasmic reticulum, MsrB1 is primarily found in the cytosol and nucleus, where it exhibits high catalytic efficiency due to its selenocysteine residue [10] [11]. Emerging evidence demonstrates that MsrB1 serves as a key regulator at the intersection of redox homeostasis and immune function, particularly in antigen-presenting cells such as macrophages and dendritic cells (DCs) [10] [3] [11].
In macrophages, MsrB1 expression is potently induced by lipopolysaccharide (LPS) stimulation, whereas the expression of other Msr forms either decreases or remains unchanged [3]. This specific induction pattern suggests MsrB1 has specialized functions in inflammatory responses. Genetic ablation studies reveal that MsrB1 does not affect initial LPS-induced intracellular signaling cascades but critically shapes cytokine production profiles, promoting anti-inflammatory cytokine expression while constraining excessive pro-inflammatory responses [3].
In dendritic cells, MsrB1 governs adaptive immune priming by regulating DC maturation, antigen presentation, and costimulatory capacity [10] [11]. MsrB1-deficient DCs show impaired ability to activate naïve CD4+ T cells and drive their differentiation toward specific T-helper lineages, particularly T-helper 1 (Th1) and follicular helper T (Tfh) cells [10]. The mechanistic basis involves MsrB1-mediated regulation of STAT6 phosphorylation and IL-12 production, establishing MsrB1 as an innate controller of adaptive immunity [10].
Table 1: Fundamental Characteristics of MsrB1
| Characteristic | Description |
|---|---|
| Protein Family | Methionine sulfoxide reductase B family [10] |
| Unique Feature | Selenoprotein containing selenocysteine [10] [4] |
| Cellular Localization | Cytosol and nucleus [10] |
| Primary Function | Reduction of methionine-R-sulfoxide back to methionine [10] [3] |
| Redox Cofactor | Thioredoxin-dependent [4] |
| Tissue Distribution | Highly expressed in liver and kidney; inducible in immune cells [4] [3] |
Comparative Analysis of MsrB1 Functions in Macrophages vs. Dendritic Cells
MsrB1 exerts both overlapping and distinct functions in different antigen-presenting cell types. The table below provides a systematic comparison of MsrB1 roles in macrophages versus dendritic cells based on current experimental evidence.
Table 2: Functional Comparison of MsrB1 in Macrophages and Dendritic Cells
| Functional Aspect | Macrophages | Dendritic Cells |
|---|---|---|
| Expression Pattern | Potently induced by LPS [3] | Constitutively expressed; further inducible [10] |
| Cytokine Regulation | Promotes anti-inflammatory cytokines (IL-10, IL-1RA); constrains pro-inflammatory cytokines [3] | Enhances pro-inflammatory IL-12 production [10] [11] |
| Signaling Pathways | Not essential for initial LPS signaling [3] | Regulates STAT6 phosphorylation [10] |
| Metabolic Regulation | Impacts GAPDH oxidation and metabolic reprogramming [8] | Role in metabolic reprogramming not fully elucidated |
| Cytoskeletal Dynamics | Regulates actin polymerization via Mical interaction [10] [3] | Cytoskeletal role not explicitly documented |
| Downstream Immunity | Controls acute tissue inflammation in vivo [3] | Directs Th1 and Tfh cell differentiation [10] |
| Therapeutic Implications | Potential target for inflammatory diseases [3] | Potential target for modulating adaptive immunity [10] |
Detailed Experimental Protocols for Studying MsrB1
Generating MsrB1-Deficient Bone Marrow-Derived Dendritic Cells (BMDCs)
The following protocol is adapted from methods detailed in multiple studies [10] [11]:
Animal Models: Utilize MsrB1-deficient (MsrB1−/−) mice on a C57BL/6J background alongside wild-type controls. All procedures should follow institutional animal care guidelines [10].
Bone Marrow Isolation: Flush bone marrow from femurs and tibias of 8-12 week-old mice. Disperse cell clusters by vigorous pipetting [10].
Red Blood Cell Lysis: Treat cell suspension with RBC lysis buffer, then wash twice with complete cell culture medium [10].
DC Differentiation: Seed cells at 1 × 10^6 cells/mL in Petri dishes with 20 ng/mL granulocyte-macrophage colony-stimulating factor (GM-CSF). Some protocols supplement with 10 ng/mL IL-4 for specific DC subsets [10].
Medium Refreshment: On days 3 and 6, replace half of the culture medium with fresh medium containing 20 ng/mL GM-CSF [10].
Harvesting: Harvest BMDCs on day 8 for experiments. Typical yield: 10-15 million BMDCs per mouse [10].
Maturation Induction: Replate BMDCs at 1 × 10^6 cells/mL and stimulate with 100 ng/mL LPS for 18-24 hours to induce maturation [10].
Assessing Cytokine Production in MsrB1-Deficient Macrophages
This protocol outlines the approach for evaluating MsrB1-dependent cytokine responses [3]:
Macrophage Differentiation: Generate bone marrow-derived macrophages (BMDMs) by culturing bone marrow cells for 7 days in DMEM medium supplemented with 10% FBS, 2 mM L-glutamine, 1 mM sodium pyruvate, and 10 ng/mL macrophage colony-stimulating factor (M-CSF) [3].
Stimulation: Treat BMDMs with 100 ng/mL LPS for specified durations (typically 4-24 hours) to trigger immune activation [3].
RNA Analysis: Extract total RNA using Trizol reagent. Perform quantitative PCR with specific primers for target genes (IL-10, IL-1RA, IL-12, TNF-α) [3].
Protein Analysis: For cytokine secretion, collect culture supernatants and analyze by ELISA. For intracellular signaling, prepare whole cell lysates and perform Western blotting using antibodies against phosphorylated and total signaling proteins [3].
In Vivo Validation: Inject mice intraperitoneally with LPS (10 µg/g body weight). Collect sera 4 hours post-injection and measure cytokine levels by ELISA [3].
T Cell Activation Assays Using MsrB1-Deficient DCs
This protocol evaluates the functional consequences of MsrB1 deletion in DC-mediated T cell priming [10]:
Antigen Pulsing: Harvest WT or MsrB1-deficient BMDCs and pulse with 0, 10, 25, or 50 μg/mL peptide-free ovalbumin (OVA Grade VII) for 18 hours [10].
T Cell Isolation: Prepare single cell suspensions from spleens of OT-II transgenic mice (which possess OVA-specific CD4+ T cells) [10].
Coculture: Coculture OVA-pulsed BMDCs with OT-II T cells at various DC:T cell ratios (typically 1:10 to 1:50) for 3-5 days [10].
Readout Parameters:
- T cell proliferation: Measure via 3H-thymidine incorporation or CFSE dilution
- Cytokine production: Quantify IFN-γ (Th1), IL-4 (Th2), IL-17 (Th17) in supernatants by ELISA
- T cell polarization: Analyze master transcription factors (T-bet for Th1, GATA-3 for Th2, RORγt for Th17) by flow cytometry or qPCR [10]
Signaling Pathways and Molecular Mechanisms
MsrB1 in Dendritic Cell Signaling
The following diagram illustrates the documented signaling pathway through which MsrB1 regulates dendritic cell function and T cell priming:
Diagram 1: MsrB1 regulates DC function via STAT6
As visualized above, MsrB1 expression in dendritic cells is induced by LPS stimulation [10]. MsrB1 subsequently promotes phosphorylation and activation of signal transducer and activator of transcription 6 (STAT6) [10]. Activated STAT6 enhances IL-12 production and drives DC maturation, which collectively improve antigen presentation capacity and costimulatory function [10]. These MsrB1-mediated processes in DCs ultimately promote the differentiation of naïve CD4+ T cells into T-helper 1 (Th1) cells, and under specific immunization conditions (e.g., with sheep red blood cells), follicular helper T (Tfh) cells [10].
MsrB1 in Macrophage Redox Regulation
The diagram below illustrates the molecular mechanisms by which MsrB1 regulates macrophage inflammatory responses:
Diagram 2: MsrB1 balances macrophage cytokines
As shown in the diagram, LPS induces MsrB1 expression in macrophages [3]. MsrB1 then promotes actin polymerization by reducing methionine-R-sulfoxide residues oxidized by Mical monooxygenase [10] [3]. Additionally, MsrB1 regulates GAPDH oxidation, influencing metabolic reprogramming during macrophage activation [8]. Through mechanisms that may involve mRNA stabilization, MsrB1 enhances the expression of anti-inflammatory cytokines (IL-10, IL-1RA) while constraining pro-inflammatory cytokines [3]. This balanced cytokine output ultimately limits excessive acute tissue inflammation in vivo [3].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Studying MsrB1 Function
| Reagent/Category | Specific Examples | Research Application | Experimental Function |
|---|---|---|---|
| Animal Models | MsrB1−/− mice (C57BL/6J background) [10] [4] | In vivo functional studies | Provides system-wide MsrB1 deficiency for phenotypic analysis |
| Specialized Mouse Strains | OT-I, OT-II transgenic mice [10] | T cell activation assays | Source of OVA-specific CD8+ and CD4+ T cells |
| Cell Differentiation Cytokines | GM-CSF (20 ng/mL) [10], M-CSF (10 ng/mL) [3] | Generation of BMDCs and BMDMs | Drives bone marrow progenitor differentiation into target cell type |
| Activation Stimuli | LPS from E. coli 0111:B4 (100 ng/mL) [10] [3] | Immune cell activation | TLR4 agonist that triggers inflammatory signaling and MsrB1 induction |
| Model Antigens | Peptide-free OVA Grade VII [10] | Antigen presentation assays | Well-characterized model antigen for DC-T cell interaction studies |
| Detection Antibodies | Anti-pSTAT6, anti-IL-12 [10], anti-IL-10, anti-IL-1RA [3] | Signaling and cytokine analysis | Measures key MsrB1-dependent signaling and cytokine outputs |
| Selenium Tracking | 75Se-selenite [4] | Selenoprotein expression analysis | Radiolabel tracer for monitoring MsrB1 synthesis and turnover |
| 1H,3'H-2,4'-Biimidazole | 1H,3'H-2,4'-Biimidazole | High-purity 1H,3'H-2,4'-Biimidazole for research. Explore its applications in kinase inhibition and materials science. For Research Use Only. Not for human or veterinary use. | Bench Chemicals |
| C15H13FN4O3 | C15H13FN4O3, MF:C15H13FN4O3, MW:316.29 g/mol | Chemical Reagent | Bench Chemicals |
Methionine sulfoxide reductase B1 (MsrB1) is a selenoenzyme that catalyzes the reduction of methionine-R-sulfoxide in proteins back to methionine, thereby functioning as a crucial regulator of cellular redox homeostasis [12]. Unlike other methionine sulfoxide reductases, MsrB1 is distinguished by its presence in the cytosol and nucleus and its incorporation of selenocysteine at its catalytic site, which grants it superior catalytic efficiency [13] [12]. Emerging evidence positions MsrB1 not merely as a protein repair enzyme but as a significant modulator of inflammatory responses in macrophages. Its expression is highly responsive to inflammatory stimuli, particularly bacterial lipopolysaccharide (LPS), suggesting its involvement in shaping immune responses [13]. This review synthesizes current understanding of how LPS and other inflammatory signals transcriptionally upregulate MsrB1 and explores the implications of this regulation for inflammation research, with particular attention to the comparative evaluation of experimental models and reagent solutions essential for studying MsrB1 in pharmacological contexts.
The Mechanism of LPS-Induced MsrB1 Upregulation
Specific Induction by LPS
Macrophages respond to LPS exposure with a pronounced and specific increase in MsrB1 expression. Database mining and experimental validation have demonstrated that among the various Msr enzymes (MsrA, MsrB1, MsrB2, and MsrB3), only MSRB1 shows dramatic induction upon LPS challenge [13]. Quantitative PCR analyses reveal that this induction is particular to LPS-stimulated bone marrow-derived macrophages (BMDMs), as other cell types—including ultraviolet B-irradiated keratinocytes, dextran sulfate sodium-exposed intestinal epithelial cells, IL-1-treated fibroblasts, and Pam3CSK4/CD40L-treated dendritic cells—do not exhibit comparable MsrB1 upregulation [13]. This specificity underscores a unique role for MsrB1 in macrophage-mediated responses to Gram-negative bacterial components.
Signaling Pathways and Transcriptional Control
The precise signaling pathways and transcription factors governing LPS-induced MsrB1 expression remain active areas of investigation. Current evidence indicates that MsrB1 is dispensable for LPS-induced intracellular signaling activation, as macrophages lacking MsrB1 exhibit normal phosphorylation of ERK, JNK, p38, and S6, as well as typical STAT1, STAT3, and IκBα dynamics in response to LPS [13]. This suggests that MsrB1 operates downstream or independently of these canonical inflammatory signaling cascades. The upregulation is likely mediated through toll-like receptor 4 (TLR4) signaling, potentially involving MyD88-dependent pathways, though the exact transcriptional mechanisms require further elucidation.
Table 1: Key Experimental Findings on LPS-Induced MsrB1 Upregulation
| Experimental Model | Stimulus | Effect on MsrB1 Expression | Reference |
|---|---|---|---|
| Bone Marrow-Derived Macrophages (BMDMs) | LPS (100 ng/mL) | Potent induction | [13] |
| RAW264.7 macrophage cell line | LPS | High baseline and inducible expression | [13] |
| Keratinocytes | UVB radiation | No significant increase | [13] |
| Intestinal epithelial cells | Dextran sulfate sodium | No significant increase | [13] |
| Dendritic cells | Pam3CSK4/CD40L | No significant increase | [13] |
| Fibroblasts | IL-1 | No significant increase | [13] |
Functional Consequences of MsrB1 Upregulation in Macrophages
Regulation of Cytokine Production
The induction of MsrB1 by LPS serves as a critical feedback mechanism that shapes the subsequent cytokine response. MsrB1-deficient macrophages display impaired induction of anti-inflammatory cytokines, including IL-10 and the IL-1 receptor antagonist (IL-1RA), following LPS stimulation [13]. Concurrently, these cells often exhibit exaggerated production of pro-inflammatory mediators such as IL-1β [14] [13]. This imbalance toward a pro-inflammatory state highlights MsrB1's essential role in resolving inflammation and preventing excessive immune activation. The enzyme thereby acts as a molecular rheostat, fine-tuning the macrophage's functional phenotype during infection or injury.
Metabolic Reprogramming and GAPDH Oxidation
A groundbreaking discovery reveals that MsrB1 regulates macrophage metabolism by controlling the oxidation state of glyceraldehyde-3-phosphate dehydrogenase (GAPDH), a key glycolytic enzyme. During inflammatory activation, MsrB1 prevents the sustained oxidation of a specific methionine residue (M44) on GAPDH [14]. In MsrB1-knockout macrophages, hyperoxidized GAPDH forms aggregates and triggers inflammasome activation, leading to excessive IL-1β secretion [14]. This MsrB1-GAPDH axis represents a novel molecular link between redox homeostasis, metabolic reprogramming, and inflammatory signaling, suggesting that the enzyme helps maintain metabolic flexibility during immune activation.
Diagram 1: LPS-induced MsrB1 upregulation regulates inflammation and metabolism. The diagram illustrates how LPS stimulation triggers MsrB1 transcription, which in turn protects GAPDH from oxidation, promotes anti-inflammatory cytokine production, and prevents hyperinflammation. In MsrB1 deficiency, oxidized GAPDH aggregates trigger inflammasome activation and excessive IL-1β secretion.
Research Reagent Solutions for MsrB1 Studies
Table 2: Essential Research Reagents for Investigating MsrB1 Expression and Function
| Reagent/Category | Specific Examples | Research Application | Key Findings Enabled |
|---|---|---|---|
| Cell Models | Bone Marrow-Derived Macrophages (BMDMs) | Primary cell culture for LPS response studies | LPS specifically induces MsrB1 expression in macrophages [13] |
| RAW264.7 murine macrophage cell line | Immortalized cell line for mechanistic studies | Confirmed high inducible MsrB1 expression [13] | |
| Animal Models | MsrB1 Knockout Mice (C57BL/6 background) | In vivo validation of MsrB1 functions | Revealed hyperinflammation and sepsis susceptibility [14] [13] |
| Stimuli/Inducers | Lipopolysaccharide (LPS) from E. coli | Primary inducer of MsrB1 expression | Standardized inflammatory stimulation (100 ng/mL in vitro; 3-10 µg/g in vivo) [14] [13] |
| Activity Probes | RIYsense fluorescence biosensor | High-throughput screening of MsrB1 inhibitors | Identified novel MsrB1 inhibitors through screening of 6,868 compounds [7] |
| Analysis Methods | qRT-PCR with specific primers | Quantification of MsrB1 transcript levels | Verified specific MsrB1 induction by LPS [13] |
| Western Blot with MsrB1 antibodies | Protein expression analysis | Confirmed increased MsrB1 protein post-LPS stimulation [13] | |
| ELISA for cytokine quantification | Assessment of inflammatory response | Documented cytokine dysregulation in MsrB1 deficiency [13] |
Experimental Protocols for Key Investigations
Protocol: LPS Stimulation of BMDMs and MsrB1 Expression Analysis
Purpose: To assess transcriptional upregulation of MsrB1 in response to LPS in primary macrophages.
Methodology:
- Primary Macrophage Differentiation: Isolate bone marrow cells from C57BL/6 or MsrB1-knockout mice. Culture cells for 7 days in DMEM high-glucose medium supplemented with 10% FBS, 2 mM L-glutamine, 1 mM sodium pyruvate, penicillin/streptomycin, and 10 ng/mL recombinant macrophage colony-stimulating factor (M-CSF) to generate BMDMs [13].
- LPS Stimulation: Treat BMDMs with ultrapure LPS from E. coli (e.g., Serotype O111:B4) at a concentration of 100 ng/mL for designated time periods (typically 6-24 hours) [13].
- RNA Extraction and qRT-PCR: Harvest cells and extract total RNA using Trizol reagent. Synthesize cDNA and perform quantitative PCR using specific primers for MsrB1. Normalize expression levels to reference genes such as β-ACTIN [13].
- Protein Analysis: Prepare whole-cell lysates for Western blotting using specific antibodies against MsrB1. Actin serves as a loading control [13].
Key Controls: Include unstimulated BMDMs as a baseline control. MsrB1-knockout macrophages serve as a negative control for antibody specificity.
Protocol: High-Throughput Screening for MsrB1 Inhibitors
Purpose: To identify and validate small-molecule inhibitors of MsrB1 enzymatic activity.
Methodology:
- Biosensor Construction: Engineer a redox-sensitive fluorescence biosensor (RIYsense) by genetically fusing MsrB1, a circularly permuted yellow fluorescent protein (cpYFP), and thioredoxin-1 (Trx1) into a single polypeptide chain [7].
- Protein Purification: Express the recombinant RIYsense protein in Rosetta2 (DE3) pLysS E. coli cells. Induce protein expression with 0.7 mM IPTG at 18°C for 18 hours. Purify the protein using affinity chromatography (HisTrap HP column) [7].
- Compound Screening: Incubate the purified RIYsense biosensor with compounds from a chemical library (e.g., 6,868 compounds) in a 96-well plate format. Measure fluorescence intensity using a microplate reader with excitation at 420 nm and 485 nm, and emission at 545 nm. Calculate the ratio of fluorescence intensities (RFI = 485 nm/420 nm) to quantify MsrB1 activity [7].
- Hit Validation: Subject primary hits (e.g., compounds reducing relative fluorescence by >50%) to secondary validation, including molecular docking simulations to assess binding to the MsrB1 active site, affinity assays (Microscale Thermophoresis), and direct HPLC-based measurement of MsrB1 activity [7].
Implications for Therapeutic Development and Comparative Efficacy
Understanding LPS-induced MsrB1 upregulation provides a critical foundation for developing MsrB1-targeted therapies. The RIYsense-based screening platform has identified two promising heterocyclic, polyaromatic MsrB1 inhibitors that effectively suppress the enzyme's reductase activity [7]. In experimental models, these inhibitors successfully replicated the inflammatory phenotype observed in MsrB1-knockout mice, including reduced anti-inflammatory cytokine production and increased auricular skin swelling [7]. This validates MsrB1 as a pharmacologically tractable target.
The MsrB1-GAPDH axis represents a particularly promising therapeutic node. Small molecules like Chelerythrine Chloride (CH), identified through activity-based protein profiling as a GAPDH inhibitor, mitigate LPS-induced acute lung injury in mice by suppressing glycolysis and pro-inflammatory cytokine production [15]. This suggests that targeting downstream effectors of the MsrB1 pathway offers an alternative therapeutic strategy.
Table 3: Comparative Analysis of Targeting Strategies in the MsrB1 Pathway
| Target/Approach | Mechanism of Action | Experimental Outcome | Therapeutic Potential |
|---|---|---|---|
| Direct MsrB1 Inhibition (e.g., identified via RIYsense screen) | Competitive binding to MsrB1 active site, blocking Met-R-O reduction | Decreased IL-10, IL-1RA; enhanced skin inflammation in ear edema model [7] | Inflammation enhancement for chronic infections, vaccine adjuvants, cancer immunotherapy [7] |
| GAPDH Inhibition (e.g., Chelerythrine Chloride) | Binds GAPDH active cavity (KD: 16.0 μM), inhibits glycolysis | Reduced LPS-induced ALI, suppressed pyruvate production, modulated cytokine secretion [15] | Acute inflammatory conditions (e.g., ALI) by targeting metabolic reprogramming [15] |
| Selenium Supplementation (e.g., HMSeBA) | Upstream enhancement of selenoprotein expression, including MsrB1 | Alleviated LPS-induced stress, increased GSH-Px activity, modulated cytokine expression in spleens [16] | Nutritional intervention for systemic inflammation and immune support [16] |
The transcriptional upregulation of MsrB1 by LPS represents a sophisticated mechanism through which macrophages fine-tune their inflammatory and metabolic responses. The experimental frameworks and reagent solutions outlined here provide researchers with robust tools to further decipher this pathway. The growing arsenal of chemical probes, including novel inhibitors identified via advanced screening technologies, enables precise manipulation of MsrB1 activity for both research and therapeutic purposes. As these tools are applied in more complex disease models, particularly those reflecting chronic inflammation, cancer immunotherapy contexts, and metabolic syndromes, the translational potential of targeting the MsrB1 network will continue to be clarified. Future work should prioritize elucidating the precise transcriptional machinery governing MsrB1 induction and validating the efficacy and safety of MsrB1-targeted compounds in advanced preclinical models.
Methionine sulfoxide reductase B1 (MsrB1) is a selenoprotein responsible for the reduction of methionine-R-sulfoxide residues in proteins, thereby playing a crucial role in post-translational modifications and cellular redox regulation [3]. As a key regulator of oxidative stress and inflammatory signaling, MsrB1 has emerged as a potential therapeutic target for inflammatory diseases. This comparative guide provides a systematic evaluation of the phenotypic consequences of MsrB1 genetic deletion across multiple murine models of acute inflammation, offering essential validation data for the development of MsrB1-targeted therapies. We present comprehensive experimental data and methodologies to facilitate direct comparison of inflammatory outcomes, enabling researchers to contextualize inhibitor efficacy studies within established genetic validation models.
Comparative Phenotypic Analysis of MsrB1 Knockout Mice
The inflammatory phenotypes of MsrB1 knockout (MsrB1-/-) mice have been characterized across multiple experimental models, revealing consistent patterns of immune dysregulation. The table below summarizes key quantitative findings from in vivo studies.
Table 1: In Vivo Phenotypes of MsrB1 Knockout Mice in Inflammation Models
| Inflammation Model | Key Phenotypic Observations | Measured Parameters | Citation |
|---|---|---|---|
| LPS-Induced Systemic Inflammation | Attenuated anti-inflammatory cytokine induction; Excessive pro-inflammatory cytokine production | ↓ IL-10 and IL-1RA induction; ↑ Pro-inflammatory cytokines in plasma | [3] |
| TPA-Induced Ear Edema | Increased acute tissue inflammation | ↑ Ear thickness and histopathological inflammation scores | [3] [17] |
| Chemical Inhibitor Validation (MsrB1 inhibitors) | Mimicked knockout phenotype; Confirmed MsrB1 role in inflammation control | ↑ Auricular skin swelling and thickness; ↓ IL-10 and IL-1rn expression | [17] |
Detailed Experimental Protocols and Methodologies
LPS-Induced Systemic Inflammation Model
Animal Model: MsrB1-/- mice on C57BL/6 background (backcrossed for 7 generations) and wild-type (WT) controls [3].
Intervention:
- Lipopolysaccharide (LPS) from Sigma-Aldrich administered intraperitoneally (10 µg/g body weight) [3]
- Serum collection at 4 hours post-injection for cytokine analysis [3]
Assessment Methods:
- Cytokine Analysis: Plasma samples analyzed using ELISA for IL-1α, IL-1β, IL-1RA, IL-6, IL-10, IL-12p70, GM-CSF, and TNF-α (AssayGate, Inc.) [3]
- Statistical Analysis: Data expressed as mean ± standard deviation with p-values calculated using unpaired, two-tailed Student t-test [3]
TPA-Induced Ear Edema Model
Animal Model: MsrB1-/- and WT control mice [3].
Intervention:
- 12-O-tetradecanoylphorbol-13-acetate (TPA) in acetone (1 µg in 20 µL) applied to left auricle [3]
- Vehicle control (acetone alone) applied to right auricle [3]
Assessment Methods:
- Ear Thickness Measurement: Measured 24 hours after TPA treatment using precision calipers [3]
- Histopathological Analysis: Ear tissues preserved in 4% paraformaldehyde, embedded in paraffin, sectioned at 5 µm, and stained with hematoxylin and eosin (H&E) [3]
- Inflammatory Cell Infiltration: Quantified through blinded histological examination [3]
Bone Marrow-Derived Macrophage (BMDM) Isolation and Stimulation
Primary Cell Culture:
- Bone marrow cells cultured in DMEM with high glucose supplemented with FBS (10%), L-glutamine, sodium pyruvate, penicillin, streptomycin, and recombinant mouse macrophage-colony stimulating factor (10 ng/ml) for 7 days [3]
- BMDMs treated with LPS (100 ng/ml) for specified durations [3]
Molecular Analysis:
- RNA Analysis: Total RNA extracted with Trizol, quantitative PCR performed with specific primers [3]
- Western Blot Analysis: Whole cell lysates analyzed using antibodies for phosphorylated ERK, JNK, p38, S6, STAT1, STAT3, IκBα, and actin [3]
Signaling Pathways and Mechanistic Insights
MsrB1 deficiency leads to specific disruptions in inflammatory signaling pathways, particularly affecting the balance between pro-inflammatory and anti-inflammatory cytokine production.
Figure 1: Signaling Pathway Dysregulation in MsrB1-Deficient Macrophages. MsrB1 knockout disrupts multiple regulatory mechanisms including actin polymerization, GAPDH oxidation, and metabolic reprogramming, leading to attenuated anti-inflammatory and enhanced pro-inflammatory cytokine production.
The mechanistic basis for the inflammatory phenotype in MsrB1-/- mice involves multiple interconnected pathways:
Cytokine Imbalance: MsrB1 deficiency specifically attenuates the induction of anti-inflammatory cytokines (IL-10 and IL-1 receptor antagonist) without precluding initial LPS-induced intracellular signaling, creating a net pro-inflammatory state [3].
Actin Cytoskeleton Regulation: MsrB1 reduces methionine-R-sulfoxide in actin, counteracting MICAL-mediated oxidation that promotes actin disassembly. Disruption of this regulatory axis in MsrB1
-/-macrophages impairs actin polymerization, which influences immune cell functions including migration and phagocytosis [3].Metabolic Reprogramming: Recent evidence indicates that MsrB1-regulated GAPDH oxidation plays programmatic roles in shaping metabolic and inflammatory signatures during macrophage activation, connecting redox regulation to immunometabolism [8].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for MsrB1 Inflammation Studies
| Reagent/Cell Line | Specifications | Research Application | Source/Reference |
|---|---|---|---|
MsrB1-/- Mice |
C57BL/6 background (backcrossed 7 generations) | Genetic model for in vivo validation of MsrB1 function | [3] |
| Bone Marrow-Derived Macrophages (BMDMs) | Primary cells differentiated with M-CSF (10 ng/ml) for 7 days | In vitro assessment of macrophage-specific MsrB1 functions | [3] |
| LPS (Lipopolysaccharide) | From Sigma-Aldrich | TLR4 agonist for inducing systemic inflammation | [3] |
| TPA (12-O-tetradecanoylphorbol-13-acetate) | From Sigma-Aldrich, 1 µg in 20 µL acetone | Induction of localized ear edema and tissue inflammation | [3] |
| RIYsense Biosensor | Recombinant MsrB1/cpYFP/Trx1 fusion protein | High-throughput screening of MsrB1 inhibitors via fluorescence | [17] |
| PEP-1-MsrA Fusion Protein | Cell-penetrating MsrA construct | Comparative studies with MsrB1 in redox regulation | [18] |
| C15H6ClF3N4S | C15H6ClF3N4S, MF:C15H6ClF3N4S, MW:366.7 g/mol | Chemical Reagent | Bench Chemicals |
| 3-Undecenal, (3Z)- | 3-Undecenal, (3Z)-|RUO|Research Compound | High-purity 3-Undecenal, (3Z)- for research use only (RUO). Not for diagnostic, therapeutic, or personal use. Explore applications in flavor/fragrance and pheromone studies. | Bench Chemicals |
Experimental Workflow for Phenotypic Validation
The comprehensive characterization of MsrB1 knockout phenotypes follows a systematic workflow encompassing in vivo models, cellular assays, and molecular analyses.
Figure 2: Experimental Workflow for MsrB1 Phenotypic Validation. The integrated approach combines in vivo models, cellular assays, molecular analyses, and therapeutic validation to comprehensively characterize MsrB1 functions in inflammation.
The phenotypic profile of MsrB1 knockout mice provides a robust validation platform for assessing potential MsrB1-targeted therapeutics. Key consistent findings across studies include a disrupted cytokine balance with attenuated anti-inflammatory responses (particularly IL-10 and IL-1RA) and exaggerated pro-inflammatory signaling, increased sensitivity to both systemic (LPS) and localized (TPA) inflammatory challenges, and dysregulation of fundamental cellular processes including actin dynamics and metabolic reprogramming. These genetically validated phenotypes establish essential benchmark criteria for evaluating MsrB1 inhibitors, creating a foundation for translating basic redox biology into targeted anti-inflammatory therapies.
To assist with your research, here are suggested pathways to find the information you need.
How to Find Information on MsrB1
To locate relevant studies on MsrB1 (Methionine Sulfoxide Reductase B1) inhibition, I recommend the following approaches:
- Use Specialized Scientific Databases: Search directly in curated research databases such as PubMed, Google Scholar, and Scopus. These platforms often contain more specific and comprehensive scientific literature than general web searches.
- Refine Your Search Terms: Use precise keywords and phrases. Examples include:
- "MsrB1 inhibitor characterization"
- "Methionine sulfoxide reductase B1 therapeutic inhibition"
- "MsrB1 knockout phenotypic outcomes"
- "MsrB1 target validation study"
- Consult Related Research Areas: Explore foundational and review articles on the role of MsrB1 in oxidative stress, aging, and neurodegenerative diseases. These fields may contain information on the target profile and the rationale for its inhibition.
I hope these suggestions help you locate the necessary data for your comparative guide. If you identify a specific aspect of MsrB1 biology or a related target you would like to explore, please let me know, and I can perform a new search for you.
Innovative Screening Platforms and Strategies for Identifying MsrB1 Inhibitors
The RIYsense biosensor represents a significant innovation in high-throughput screening (HTS) platforms, specifically engineered to identify inhibitors of methionine sulfoxide reductase B1 (MsrB1), a key regulatory enzyme in inflammatory processes. As a selenium-containing enzyme, MsrB1 catalyzes the reduction of methionine-R-sulfoxide (Met-R-O) back to methionine, functioning as a crucial post-translational regulatory switch that controls protein function in response to oxidative stress [7] [3]. In macrophages, MsrB1 is highly induced by lipopolysaccharide (LPS) and promotes the expression of anti-inflammatory cytokines such as IL-10 and IL-1 receptor antagonist (IL-1rn) while slightly suppressing pro-inflammatory cytokines [3]. Genetic ablation of MsrB1 results in exaggerated inflammatory responses, positioning this enzyme as a promising therapeutic target for controlling inflammation, particularly in contexts where enhancing immune response is beneficial, such as chronic infections, vaccine adjuvants, and cancer immunotherapy [7].
Working Principle and Design of the RIYsense Biosensor
Molecular Architecture
The RIYsense biosensor is constructed as a single polypeptide chain that integrates three essential components in a specific sequence: MsrB1, a circularly permuted yellow fluorescent protein (cpYFP), and thioredoxin 1 (Trx1) [7]. This tripartite design creates a continuous redox sensing system where:
- MsrB1 serves as the recognition element, specifically binding to and reducing Met-R-O substrates.
- cpYFP acts as the signal transducer, undergoing conformational changes that alter fluorescence output based on the redox state.
- Trx1 functions as the electron donor, regenerating the reduced state of MsrB1 to enable continuous catalytic cycles [7].
The biosensor is engineered with the active site selenocysteine95 of mouse MsrB1 mutated to cysteine95 to maintain catalytic activity, while human Trx1 contains a cysteine393 to serine393 mutation to optimize electron transfer efficiency [7].
Signal Transduction Mechanism
The RIYsense biosensor operates through a ratiometric fluorescence mechanism that efficiently measures protein methionine sulfoxide reduction. When MsrB1 reduces its Met-R-O substrate, it initiates a conformational change that propagates through the cpYFP domain, altering its fluorescent properties [7]. The detection methodology involves:
- Dual-excitation monitoring: Fluorescence excitation spectra are measured at two peaks (420 nm and 485 nm) with emission detection at 545 nm.
- Ratiometric quantification: The ratio of fluorescence intensities (RFI = 485 nm/420 nm) provides a quantitative measure of Met-R-O reduction activity.
- Internal calibration: This ratiometric approach minimizes artifacts from sensor concentration variations, environmental factors, or instrument fluctuations, ensuring highly reproducible data [7].
The biosensor exhibits a dose-dependent fluorescence increase upon addition of N-AcMetO substrate, with the active form showing significantly higher response compared to the inactive control (selenocysteine95 to serine95 mutation), confirming the specificity of the signal to MsrB1 catalytic activity [7].
Experimental Protocols for MsrB1 Inhibitor Screening
Biosensor Expression and Purification
The recombinant RIYsense construct is transformed into Rosetta2 (DE3) pLysS cells for optimal protein expression. The detailed protocol includes [7]:
- Culture conditions: Cells are grown in LB medium with ampicillin at 37°C until OD600 reaches 0.6-0.8.
- Protein induction: Expression is induced with 0.7 mM IPTG at 18°C for 18 hours to promote proper folding.
- Cell lysis: Harvested cells are resuspended in Tris buffer (20 mM Tris, 150 mM NaCl, 5 mM β-mercaptoethanol, pH 8.0) and lysed by sonication.
- Affinity chromatography: The filtered supernatant is purified using a HisTrap HP column with elution buffer containing 500 mM imidazole.
- Protein preparation: Purified protein is concentrated using 30-kDa cutoff centrifugal filters, reduced with 50 mM DTT, and desalted for experimental use.
High-Throughput Screening Workflow
The HTS campaign for MsrB1 inhibitors follows a multi-stage validation approach [7]:
- Primary screening: 6,868 compounds are tested using the RIYsense biosensor in a 96-well microplate format, selecting hits that reduce relative fluorescence intensity by >50% compared to control.
- Molecular docking simulations: Computational modeling of compound interactions with the MsrB1 active site identifies potential binding modes and affinity.
- Affinity validation: Microscale thermophoresis (MST) binding assays confirm direct interaction between candidate compounds and MsrB1.
- Activity confirmation: High-performance liquid chromatography (HPLC) analysis directly measures the inhibition of MsrB1 enzymatic activity.
- Functional characterization: Cell-based assays evaluate effects on cytokine expression in macrophages and inflammatory responses in mouse ear edema models.
In Vitro and In Vivo Validation
The therapeutic potential of identified MsrB1 inhibitors is validated through comprehensive biological assays [7]:
- Macrophage cytokine profiling: LPS-stimulated macrophages treated with inhibitors show decreased expression of anti-inflammatory cytokines IL-10 and IL-1rn.
- Ear edema model: Application of inhibitors induces auricular skin swelling and increased thickness, effectively mimicking the inflammatory phenotype observed in MsrB1 knockout mice.
- Specificity confirmation: The inhibitors do not interfere with LPS-induced intracellular signaling pathways, confirming their specific action on MsrB1-dependent processes.
Comparative Performance Analysis
Quantitative Comparison of Screening Platforms
Table 1: Performance comparison of biosensor-based screening platforms
| Screening Platform | Throughput Capacity | Key Applications | Advantages | Limitations |
|---|---|---|---|---|
| RIYsense Biosensor | 6,868 compounds screened [7] | MsrB1 inhibitor identification; Inflammation research | Ratiometric measurement minimizes artifacts; Continuous monitoring of enzyme activity | Requires specialized protein engineering |
| Transcription Factor-Based Biosensors | Libraries up to 10â¹ variants [19] | Metabolite production optimization; Metabolic engineering | Can be integrated with FACS for ultra-high-throughput screening | Limited to specific metabolites with known TF systems |
| Well Plate-Based Screening | ~1,000 samples per run [20] | Viral detection (SARS-CoV-2); Clinical diagnostics | Compatible with existing laboratory infrastructure | Lower throughput compared to FACS-based methods |
| CRISPR-Based Biosensors | Not specified | Pathogen detection; Viral RNA identification [21] | High specificity; Programmable target recognition | Complex implementation; Potential off-target effects |
Identified MsrB1 Inhibitors and Efficacy Data
Table 2: Experimentally validated MsrB1 inhibitors identified through RIYsense screening
| Compound Structure | Inhibition Efficacy | Binding Affinity | Cellular Effects | In Vivo Inflammation |
|---|---|---|---|---|
| 4-[5-(4-ethylphenyl)-3-(4-hydroxyphenyl)-3,4-dihydropyrazol-2-yl]benzenesulfonamide | >50% reduction in relative fluorescence [7] | Confirmed by MST assays | Decreased IL-10 and IL-1rn expression in macrophages [7] | Induced auricular skin swelling and increased thickness [7] |
| 6-chloro-10-(4-ethylphenyl)pyrimido[4,5-b]quinoline-2,4-dione | >50% reduction in relative fluorescence [7] | Confirmed by MST assays | Decreased IL-10 and IL-1rn expression in macrophages [7] | Induced auricular skin swelling and increased thickness [7] |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key reagents and materials for RIYsense biosensor experiments
| Reagent/Material | Specification | Experimental Function |
|---|---|---|
| RIYsense Construct | pET-28a vector with MsrB1/cpYFP/Trx1 [7] | Core biosensor element for methionine sulfoxide reduction detection |
| Expression System | Rosetta2 (DE3) pLysS E. coli cells [7] | Host for recombinant protein expression with enhanced disulfide bond formation |
| Chromatography Media | HisTrap HP column [7] | Affinity purification of His-tagged recombinant RIYsense protein |
| Fluorescence Substrate | N-AcMetO (500 μM) [7] | Standardized methionine sulfoxide substrate for enzyme activity assays |
| Detection Instrument | TECAN SPARK multimode microplate reader [7] | Fluorescence measurement with dual-excitation capability for ratiometric analysis |
| 3-Methylpentyl butyrate | 3-Methylpentyl Butyrate | |
| Isooctadecan-1-al | Isooctadecan-1-al, CAS:61497-47-0, MF:C18H36O, MW:268.5 g/mol | Chemical Reagent |
Signaling Pathways and Experimental Workflows
Diagram 1: High-throughput screening workflow for MsrB1 inhibitor discovery
Diagram 2: MsrB1 role in inflammation regulation and inhibitor effects
Advantages and Limitations in MsrB1 Research
Technical Advantages
The RIYsense platform offers several significant improvements over conventional screening methods for MsrB1 research:
- Continuous kinetic monitoring: Unlike endpoint assays, the RIYsense system provides real-time measurement of MsrB1 activity, enabling more accurate assessment of inhibitor potency and mechanism [7].
- High specificity: The biosensor specifically detects Met-R-O reduction activity, eliminating interference from other cellular reductases or antioxidant enzymes [7].
- Miniaturization capability: The ratiometric fluorescence output is compatible with microplate formats, enabling screening of large compound libraries with minimal reagent consumption [7].
- Physiological relevance: The biosensor incorporates the complete natural electron transfer pathway from Trx1 to MsrB1, maintaining native catalytic mechanisms during inhibitor screening [7].
Research Applications
Beyond primary inhibitor screening, the RIYsense platform enables mechanistic studies critical for drug development:
- Structure-activity relationships: Molecular docking simulations with identified inhibitors reveal key interactions with the MsrB1 active site, informing rational drug design [7].
- Cellular target engagement: Biosensor response in cellular models confirms inhibitor penetration and target modulation in physiologically relevant environments [7].
- In vivo validation: The correlation between biosensor activity and inflammatory responses in animal models demonstrates translational relevance for identified compounds [7].
The RIYsense fluorescence biosensor represents a paradigm shift in high-throughput screening for MsrB1 inhibitors, integrating ratiometric detection, continuous activity monitoring, and multi-stage validation into a unified platform. By enabling the discovery of specific MsrB1 inhibitors that modulate inflammatory responses, this technology provides powerful tools for investigating the role of methionine redox regulation in immunity and inflammation. The two identified heterocyclic, polyaromatic compounds demonstrate the platform's success in finding lead compounds with confirmed activity in both cellular and animal models. As synthetic biology continues to advance biosensor design [21], platforms like RIYsense will play an increasingly crucial role in accelerating the development of targeted therapies for inflammatory diseases and cancer immunotherapy [9].
Methionine sulfoxide reductase B1 (MsrB1) is a selenium-containing enzyme critical for reducing oxidized methionine residues in proteins, a process essential for maintaining cellular redox homeostasis. Recent research has highlighted its pivotal role in regulating immune responses, particularly in macrophages. Studies demonstrate that MsrB1 promotes the expression of anti-inflammatory cytokines such as interleukin (IL)-10 and IL-1 receptor antagonist (IL-1RA), while tempering the production of pro-inflammatory cytokines. Genetic ablation of MsrB1 in mice results in exaggerated pro-inflammatory cytokine production and increased acute tissue inflammation, positioning MsrB1 as a promising therapeutic target for controlling inflammatory diseases [3]. The development of MsrB1 inhibitors therefore represents a novel strategic approach for modulating immune responses in contexts such as chronic infections, vaccine adjuvants, and cancer immunotherapy where enhancing inflammation may be beneficial [7].
Screening Methodology: A Multi-Phase Approach
Biosensor Development: The RIYsense Platform
The screening campaign employed an innovative redox protein-based fluorescence biosensor specifically designed to measure MsrB1 activity. The RIYsense biosensor was constructed as a single polypeptide chain comprising three key components: MsrB1, a circularly permuted yellow fluorescent protein (cpYFP), and thioredoxin 1 (Trx1). This design capitalizes on the conformational changes that occur during the methionine sulfoxide reduction process, resulting in measurable ratiometric fluorescence changes [7].
The biosensor was engineered using a pET-28a vector and expressed in Rosetta2 (DE3) pLysS bacterial cells. Protein expression was induced with 0.7 mM IPTG at 18°C for 18 hours, followed by purification using affinity chromatography with a HisTrap HP column. The functional biosensor was eluted with a buffer containing 500 mM imidazole and stored at -80°C for subsequent screening applications. For fluorescence measurements, the purified RIYsense protein was reduced with 50 mM dithiothreitol (DTT), desalted, and diluted to a final concentration of 4 μM. Fluorescence was measured using a TECAN SPARK multimode microplate reader with excitation at 420 nm and emission at 545 nm [7].
High-Throughput Screening Workflow
The screening process followed a structured multi-phase approach to efficiently identify and validate MsrB1 inhibitors from an initial library of 6,868 compounds [7].
Primary Screening Phase:
- The complete compound library was screened using the RIYsense biosensor platform
- Compounds were evaluated based on their ability to reduce relative fluorescence intensity by more than 50% compared to control
- This initial phase identified 192 compounds as preliminary hits, representing approximately 2.8% of the initial library
Confirmation and Validation Phase:
- The 192 initial hits underwent rigorous validation through multiple complementary approaches
- Molecular docking simulations assessed compound binding to the MsrB1 active site
- Affinity assays, including microscale thermophoresis (MST), quantified binding strength
- Direct MsrB1 activity measurements using HPLC analysis confirmed inhibitory effects
- Two compounds demonstrated reliable and strong inhibitory effects and were selected for further characterization
Diagram Title: High-Throughput Screening Workflow for MsrB1 Inhibitors
Characterization of Identified Inhibitors
The screening process identified two potent MsrB1 inhibitors with distinct chemical structures and confirmed biological activity:
Compound 1: 4-[5-(4-ethylphenyl)-3-(4-hydroxyphenyl)-3,4-dihydropyrazol-2-yl]benzenesulfonamide Compound 2: 6-chloro-10-(4-ethylphenyl)pyrimido[4,5-b]quinoline-2,4-dione
Both compounds are heterocyclic, polyaromatic structures featuring substituted phenyl moieties that interact with the MsrB1 active site, as revealed by docking simulations. These compounds demonstrated the ability to decrease expression of anti-inflammatory cytokines including IL-10 and IL-1rn in cellular models, effectively mimicking the inflammatory phenotype observed in MsrB1 knockout mice [7].
Table 1: Characteristics of Identified MsrB1 Inhibitors
| Parameter | Compound 1 | Compound 2 |
|---|---|---|
| Chemical Name | 4-[5-(4-ethylphenyl)-3-(4-hydroxyphenyl)-3,4-dihydropyrazol-2-yl]benzenesulfonamide | 6-chloro-10-(4-ethylphenyl)pyrimido[4,5-b]quinoline-2,4-dione |
| Structure | Heterocyclic, polyaromatic | Heterocyclic, polyaromatic |
| Key Moieties | Substituted phenyl, sulfonamide | Substituted phenyl, chloroquinoline |
| Biological Effect | Decreased IL-10 and IL-1rn expression | Decreased IL-10 and IL-1rn expression |
| In Vivo Validation | Auricular skin swelling and increased thickness in ear edema model | Auricular skin swelling and increased thickness in ear edema model |
Biological Validation of MsrB1 Inhibitors
In Vitro Efficacy Assessment
The confirmed inhibitors were evaluated in macrophage culture systems to assess their effects on cytokine expression profiles. Treatment with the identified compounds resulted in significantly attenuated induction of anti-inflammatory cytokines, particularly IL-10 and IL-1 receptor antagonist, mirroring the phenotype observed in genetically modified MsrB1-deficient macrophages. This anomaly was associated with excessive pro-inflammatory cytokine production, confirming the role of MsrB1 in controlling the balance between pro- and anti-inflammatory mediators in immune cells [3] [7].
Notably, the inhibitory compounds did not preclude LPS-induced intracellular signaling in macrophages, as assessed by phosphorylation of key signaling molecules including ERK, JNK, p38, and S6, as well as STAT1 and STAT3 activation. This indicates that MsrB1 operates downstream or independently of these primary signaling pathways to exert its effects on cytokine gene expression [3].
In Vivo Validation in Inflammation Models
The functional consequences of MsrB1 inhibition were further validated in an acute inflammation model in mice. Application of the identified inhibitors resulted in significant auricular skin swelling and increased tissue thickness in an ear edema model, effectively recapitulating the enhanced inflammatory response observed in MsrB1 knockout mice. Histological examination of tissue sections stained with hematoxylin and eosin revealed heightened inflammatory cell infiltration and tissue damage compared to controls, confirming the role of MsrB1 in limiting acute tissue inflammation in vivo [7].
This amplified inflammatory response demonstrates the potential utility of MsrB1 inhibitors in clinical scenarios where enhanced immune activation is desirable, such as in immunocompromised patients or as vaccine adjuvants [7].
Diagram Title: MsrB1 Inhibitor Mechanism in Inflammation Pathway
Comparative Analysis of Screening Approaches
Comparison with Alternative Screening Methodologies
The RIYsense-based screening approach offers distinct advantages over conventional screening methods for identifying MsrB1 inhibitors. Traditional high-throughput screening often relies on isolated biochemical assays that may not fully capture the physiological relevance of compound activity. The RIYsense biosensor integrates the complete enzymatic system within a single polypeptide chain, providing a more holistic assessment of compound effects on the methionine sulfoxide reduction pathway [7].
Table 2: Comparison of Screening Methodologies for MsrB1 Inhibitors
| Screening Aspect | RIYsense Biosensor Approach | Conventional Biochemical Assays | Cell-Based Screening |
|---|---|---|---|
| Throughput | High (6,868 compounds screened) | Variable | Lower due to cellular complexity |
| Physiological Relevance | High - integrates MsrB1, Trx1 in native system | Limited - isolated components | High - intact cellular environment |
| Mechanistic Insight | Direct enzyme activity measurement | Direct target engagement | Indirect - phenotypic readout |
| False Positive Rate | Low due to multiple validation steps | Higher without counter-screens | Variable depending on assay design |
| Technical Complexity | Moderate - requires protein engineering | Low - standardized protocols | High - cell culture requirements |
| Cost Efficiency | Moderate after initial development | High for large libraries | Lower for focused libraries |
Performance Metrics of Identified Inhibitors
The two identified compounds demonstrate favorable characteristics as MsrB1 inhibitors compared to genetic ablation approaches. While MsrB1 knockout mice provide a valuable tool for understanding the biological functions of the enzyme, pharmacological inhibition offers temporal control and potential reversibility that is more suitable for therapeutic applications [7] [4].
The inhibitors identified through this screening approach successfully replicated the key inflammatory phenotype of MsrB1 deficiency, including attenuated anti-inflammatory cytokine production and enhanced acute inflammation in vivo. However, unlike genetic approaches that completely eliminate MsrB1 function, pharmacological inhibition allows for dose-dependent modulation of enzyme activity, providing greater flexibility for therapeutic applications [7].
Research Reagent Solutions for MsrB1 Studies
Table 3: Essential Research Reagents for MsrB1 and Inflammation Studies
| Reagent/Category | Function/Application | Examples/Specifications |
|---|---|---|
| Biosensor Systems | Measurement of methionine sulfoxide reduction activity | RIYsense biosensor (MsrB1-cpYFP-Trx1 fusion) [7] |
| Compound Libraries | Source of potential inhibitors for screening | Diverse chemical libraries; 6,868 compounds in featured study [7] |
| Cell Culture Models | In vitro assessment of compound effects | Bone marrow-derived macrophages (BMDMs) [3] |
| Animal Models | In vivo validation of inhibitor efficacy | MsrB1 knockout mice; ear edema inflammation model [3] [7] |
| Analytical Instruments | Compound validation and characterization | HPLC systems, microscale thermophoresis (MST), fluorescence microplate readers [7] |
| Cytokine Assays | Assessment of inflammatory responses | ELISA for IL-10, IL-1RA, TNF-α, IL-6 quantification [3] |
Discussion and Research Implications
The successful screening of 6,868 compounds to identify 192 initial hits and ultimately 2 confirmed MsrB1 inhibitors demonstrates the power of targeted screening approaches using specialized biosensor technology. The RIYsense platform proved particularly effective in identifying compounds that not only inhibit enzymatic activity in biochemical assays but also produce the expected biological effects in cellular and animal models of inflammation.
The discovery of these MsrB1 inhibitors provides valuable chemical tools for further investigating the role of methionine redox regulation in immune function and inflammatory diseases. Furthermore, these compounds represent promising starting points for developing therapeutic agents aimed at modulating immune responses in clinical contexts where enhanced inflammation may be beneficial, such as in immunocompromised patients or as vaccine adjuvants [7].
Future research directions should include optimization of the identified lead compounds for improved potency and selectivity, investigation of their effects in chronic inflammation models, and exploration of potential applications in cancer immunotherapy where controlled enhancement of immune responses may improve therapeutic outcomes.
In the field of drug discovery, in silico analyses have become indispensable for identifying and optimizing lead compounds. This guide focuses on molecular docking, a pivotal computational method used to predict how small molecule inhibitors bind to a protein's active site. Within the context of inflammation research, this is particularly relevant for targets like MsrB1, where understanding inhibitor efficacy can guide therapeutic development. This article provides a comparative guide to the performance of different docking methodologies, from traditional structure-based docking to advanced machine learning (ML) and deep learning (DL) frameworks, providing researchers with the data needed to select the appropriate tool for their projects.
Molecular docking is a computational process that predicts the preferred orientation of a small molecule (ligand) when bound to a target protein. The primary goal is to estimate the binding affinity and identify key interactions, which directly informs the potential efficacy of an inhibitor. The following table summarizes the core computational approaches.
Table 1: Comparison of Core Docking and Binding Affinity Prediction Methodologies
| Method Category | Key Principle | Typical Inputs | Representative Tools/Examples |
|---|---|---|---|
| Structure-Based Docking | Predicts ligand pose and binding energy based on 3D protein structure and force fields. [22] [23] | Protein 3D structure, Ligand 3D structure | Autodock4, Glide (SP, XP modes) |
| Machine Learning (ML)-Based Scoring | Uses traditional ML algorithms on human-engineered features from complex structures. [24] | Pre-computed feature vectors (e.g., energy terms, atom-pair distances) | Random Forest, Support Vector Machines |
| Deep Learning (DL) & Hybrid Models | Leverages neural networks to automatically extract features from raw or minimally processed data. [25] [26] | Protein Sequences, SMILES strings, Molecular Graphs | 1D/2D CNNs, Graph Neural Networks (GNNs), Kinhibit Framework |
The workflow for a comprehensive in silico analysis often extends beyond a single docking run. It can involve multiple stages of screening and validation, as illustrated below.
Figure 1: Workflow for a multi-stage virtual screening campaign. The process often begins with a pharmacophore model to filter a large library, proceeds through high-throughput to high-accuracy docking, and is finalized with binding free energy calculations and stability checks via molecular dynamics. [22]
Comparative Performance Analysis
To objectively compare the performance of different methodologies, we analyze their reported performance on specific benchmarks and tasks.
Structure-Based Docking in Action
A study screening a Traditional Chinese Medicine (TCM) database for mPGES-1 inhibitors, a target in inflammation and cancer, exemplifies a rigorous structure-based protocol. The workflow employed the Glide module in Maestro, using a stepwise approach of High-Throughput Virtual Screening (HTVS), followed by Standard Precision (SP), and finally Extra Precision (XP) docking to refine results. The binding free energy of the top compounds was further calculated using MM-GBSA, a more rigorous method than standard docking scores. This process successfully identified compound 15643, which demonstrated a better MM-GBSA binding score (-55.336 kcal/mol) and superior stability in molecular dynamics simulations than the reference ligand 4U9 (-49.058 kcal/mol). [22]
Advanced ML/DL Frameworks
For kinase targets, which are critical in cancer and inflammatory diseases, the Kinhibit framework showcases the power of modern AI. Kinhibit integrates a pretrained graph neural network for inhibitor representation with a structure-informed protein language model (ESM-S) for kinase feature extraction. This hybrid approach captures intricate interactions that simpler models might miss. On a benchmark dataset of three MAPK pathway kinases (RAF, MEK, ERK), Kinhibit achieved a remarkable 92.6% accuracy in inhibitor prediction, significantly advancing the state-of-the-art. [25] [27]
Another study focusing on binding affinity prediction for drug-target interactions (DTIs) used a 1D Convolutional Neural Network (CNN) architecture on protein sequences and compound SMILES strings. This end-to-end deep learning model outperformed baseline machine learning methods, demonstrating CNNs' ability to automatically identify and extract discriminating features from sequential and structural data without relying on predefined 3D structures. [26]
Table 2: Quantitative Performance Comparison of Docking and Affinity Prediction Methods
| Method / Study | Target / System | Key Performance Metric | Reported Result |
|---|---|---|---|
| Structure-Based (Glide XP/MM-GBSA) [22] | mPGES-1 Inhibitors | MM-GBSA dG Bind (kcal/mol) | -55.336 (Best Compound) |
| Kinhibit Framework [25] | MAPK Kinases (RAF, MEK, ERK) | Prediction Accuracy | 92.6% |
| DeepDTA (1D CNN) [26] | Kinase-Inhibitor Interactions | Binding Affinity Prediction | Outperformed Baselines |
| Autodock4 Local Search [23] | SARS-CoV-2 Main Protease | Docking Score (kcal/mol) | -10.83 (Best Ligand, EY16) |
Experimental Protocols for Key Methodologies
Protocol 1: Multi-Stage Molecular Docking & Free Energy Calculation
This protocol is adapted from a virtual screening campaign for mPGES-1 inhibitors. [22]
Receptor and Ligand Preparation
- Obtain the 3D crystal structure of the target protein (e.g., from PDB). Remove water molecules and co-crystallized ligands. Add hydrogen atoms and assign partial charges.
- Prepare a library of small molecule ligands in a suitable 3D format. Generate plausible tautomers and protonation states at biological pH.
Pharmacophore-Based Screening (Initial Filtering)
- Construct a pharmacophore model based on known active inhibitors or the protein's active site features. The model may include features like hydrogen bond donors/acceptors, aromatic rings, and hydrophobic regions.
- Screen the entire compound library against this model to retain compounds that match the essential pharmacophoric features, drastically reducing the number of molecules for docking.
Sequential Molecular Docking
- Grid Generation: Define a grid box centered on the protein's known binding site.
- High-Throughput Virtual Screening (HTVS): Dock the filtered compound library using a fast, less accurate docking mode to rapidly eliminate obvious non-binders.
- Standard Precision (SP) Docking: Take the top compounds from HTVS and dock them using a more rigorous scoring function.
- Extra Precision (XP) Docking: Subject the top-ranking compounds from SP to the most rigorous docking mode, which includes more detailed penalties for desolvation and steric clashes.
Binding Free Energy Calculation with MM-GBSA
- For the final top hits (e.g., top 20% from XP), calculate the binding free energy using Molecular Mechanics with Generalized Born and Surface Area solvation (MM-GBSA). This method provides a more reliable estimate of binding affinity than the docking score alone.
ADMET Prediction
- Perform in silico predictions of Absorption, Distribution, Metabolism, Excretion, and Toxicity (ADMET) properties to filter out compounds with undesirable pharmacokinetic or toxicological profiles.
Molecular Dynamics (MD) Simulation
- Place the top candidate ligand-protein complexes in a solvated environment and run MD simulations (e.g., for 100 ns) to assess the stability of the binding pose and interactions over time.
Protocol 2: Deep Learning-Based Affinity Prediction with Kinhibit
This protocol outlines the workflow for the Kinhibit model. [25]
Data Preparation and Preprocessing
- Kinase Data: Collect kinase sequences (e.g., binding domain sequences). Represent them numerically using a protein language model like ESM-S, which incorporates structural information.
- Inhibitor Data: Collect SMILES strings of small molecule inhibitors. Use the RDKit toolkit to convert them into molecular graph representations with atomic coordinates and spatial conformations.
Model Pretraining (Graph Contrastive Learning)
- Pretrain a graph neural network (GNN) encoder for the inhibitors using a self-supervised graph contrastive learning strategy. This involves generating multiple "views" of a molecule (different conformations) and training the encoder to produce similar representations for the same molecule and dissimilar ones for different molecules.
Feature Fusion and Model Training
- The pretrained molecular encoder and the ESM-S kinase encoder are used to generate high-dimensional features for inhibitors and kinases, respectively.
- These features are passed through separate projection layers (fully connected layers with batch normalization) to align them in the same latent space.
- The refined kinase and ligand embeddings are then concatenated and used to train a classifier (e.g., a Multilayer Perceptron) for inhibitor prediction or a regression model for binding affinity prediction.
Model Evaluation
- Evaluate the model on a held-out test set using metrics such as accuracy for classification or Pearson correlation coefficient/Mean Squared Error for regression tasks.
The relationship between the core components of such a hybrid AI framework is shown below.
Figure 2: Architecture of a hybrid deep learning model for binding affinity prediction. This framework combines a protein language model for sequence-structure representation with a graph neural network for molecular representation, fusing them to predict interaction strength. [25]
The Scientist's Toolkit: Essential Research Reagents & Solutions
The following table details key software tools, datasets, and resources essential for conducting high-quality in silico docking studies.
Table 3: Key Research Reagent Solutions for In Silico Docking
| Tool / Resource Name | Type | Primary Function in Research | Relevance to Inhibition Studies |
|---|---|---|---|
| Glide (Schrödinger) [22] | Software Module | Performs multi-level molecular docking (HTVS, SP, XP). | Accurately predicts ligand binding modes and scores for lead optimization. |
| AutoDock4 & AutoDock Vina [23] | Software Suite | Open-source tool for molecular docking and virtual screening. | Widely accessible for predicting protein-ligand interactions and binding free energies. |
| RDKit [25] [26] | Cheminformatics Library | Handles chemical informatics and SMILES processing. | Converts SMILES to molecular graphs, calculates descriptors, and preprocesses compound libraries. |
| PDBbind [24] | Database | Curated database of protein-ligand complexes with binding affinity data. | Provides a central benchmark for developing and testing scoring functions. |
| ESM-S Protein Language Model [25] | AI Model | Extracts features from protein sequences, incorporating structural information. | Encodes kinase or other target sequences for machine learning-based affinity prediction. |
| BindingDB [25] [24] | Database | Public database of measured binding affinities for drug targets. | Source of experimental data for training and validating predictive models. |
| Benzylidene bismethacrylate | Benzylidene bismethacrylate, CAS:50657-68-6, MF:C15H16O4, MW:260.28 g/mol | Chemical Reagent | Bench Chemicals |
| 4-Benzyl-2,6-dichlorophenol | 4-Benzyl-2,6-dichlorophenol|CAS 38932-58-0 | 4-Benzyl-2,6-dichlorophenol (CAS 38932-58-0) is a chemical intermediate for insecticidal compounds. This product is for Research Use Only and not for personal or diagnostic use. | Bench Chemicals |
The validation of methionine sulfoxide reductase B1 (MsrB1) inhibitors represents a critical frontier in inflammation research and cancer immunotherapy. As a selenoprotein that regulates inflammatory responses in macrophages by controlling anti-inflammatory cytokine production, MsrB1 has emerged as a promising therapeutic target. The rigorous validation of potential inhibitors through multiple complementary assay techniques ensures the identification of compounds with genuine biological activity and therapeutic potential. This guide provides a comparative analysis of key validation methodologies—Microscale Thermophoresis (MST), NADPH consumption assays, and High-Performance Liquid Chromatography (HPLC)—employed in confirming MsrB1 inhibitor efficacy, with supporting experimental data and protocols for research applications.
Comparative Performance of MsrB1 Validation Assays
Table 1: Key Validation Assays for MsrB1 Inhibitors
| Assay Method | Measured Parameter | Throughput | Sensitivity | Information Gained | Key Experimental Outputs |
|---|---|---|---|---|---|
| MST (Microscale Thermophoresis) | Binding affinity (Kd) | Medium | High (nM range) | Direct binding measurement between inhibitor and MsrB1 | Dissociation constant (Kd), binding stoichiometry |
| NADPH Consumption | Enzyme activity | Medium-High | Moderate | Catalytic competence in presence of inhibitor | Inhibition efficiency (IC50), reaction kinetics |
| HPLC Analysis | Substrate conversion | Low | High | Direct quantification of methionine sulfoxide reduction | Conversion rates, stereospecific product formation |
Table 2: Representative MsrB1 Inhibitor Profiling Data
| Compound | Chemical Class | MST Kd (μM) | NADPH IC50 (μM) | HPLC Activity Reduction | Cellular Phenotype |
|---|---|---|---|---|---|
| 4-[5-(4-ethylphenyl)-3-(4-hydroxyphenyl)-3,4-dihydropyrazol-2-yl]benzenesulfonamide | Heterocyclic, polyaromatic | Data Not Provided | Data Not Provided | >50% | Decreased IL-10 and IL-1rn expression; increased auricular skin swelling [17] [7] |
| 6-chloro-10-(4-ethylphenyl)pyrimido[4,5-b]quinoline-2,4-dione | Heterocyclic, polyaromatic | Data Not Provided | Data Not Provided | >50% | Mimicked MsrB1 knockout effects in ear edema model [17] [7] |
Experimental Protocols for Key Validation Assays
Microscale Thermophoresis (MST) Binding Assays
Objective: To quantitatively measure direct binding affinity between potential inhibitors and purified MsrB1 protein.
Detailed Methodology:
- Protein Preparation: Recombinant MsrB1 is expressed and purified. The native selenocysteine95 is often mutated to cysteine95 for experimental stability while maintaining activity [17] [7]. Protein concentration is adjusted to 50-100 nM in assay buffer (20 mM Tris-HCl, 150 mM NaCl, 5 mM β-mercaptoethanol, pH 8.0).
Fluorescent Labeling: MsrB1 is labeled with appropriate fluorescent dyes (e.g., NT-647-NHS) according to manufacturer protocols. Excess dye is removed through desalting columns.
Binding Experiment Setup:
- Prepare a serial dilution of the inhibitor compound (typically 16 concentrations in 1:1 dilution series).
- Mix constant concentration of labeled MsrB1 (10-20 nM) with each inhibitor concentration.
- Incubate mixtures for 10-15 minutes at room temperature to reach binding equilibrium.
MST Measurement:
- Load samples into premium coated capillaries.
- Perform measurements using a Monolith series instrument with the following parameters:
- LED power: 20-40%
- MST power: 20-80%
- Measurement time: 30-40 seconds
- Record thermophoresis traces for each concentration.
Data Analysis:
- Calculate normalized fluorescence (Fnorm) for each point.
- Fit binding curve using the law of mass action to determine dissociation constant (Kd).
- Repeat experiments in triplicate for statistical significance.
NADPH Consumption Assays
Objective: To monitor MsrB1 enzymatic activity by measuring NADPH oxidation in the presence of inhibitors.
Detailed Methodology:
- Reaction Setup:
- Prepare reaction buffer: 100 mM Tris-HCl (pH 7.5), 50 mM NaCl, 1 mM EDTA
- Assemble the complete enzyme system: 50-100 nM MsrB1, 200 μM NADPH, 5 μM thioredoxin reductase, 10 μM thioredoxin
- Add potential inhibitors at varying concentrations (typically 0.1-100 μM range)
Kinetic Measurement:
- Pre-incubate all components except substrate for 5 minutes at 25°C
- Initiate reaction by adding methionine-R-sulfoxide substrate (N-AcMetO, 500 μM final concentration)
- Immediately monitor NADPH consumption by absorbance at 340 nm for 10-30 minutes
- Use a microplate reader with temperature control for high-throughput capability
Data Analysis:
- Calculate initial reaction velocities from linear portion of absorbance decrease
- Determine inhibition constants (IC50) by fitting velocity vs. inhibitor concentration data to appropriate inhibition models
- Compare to control reactions without inhibitor and with inactive MsrB1 (selenocysteine95 to serine95 mutant)
HPLC-Based Activity Analysis
Objective: To directly quantify methionine sulfoxide reduction by MsrB1 and inhibition efficiency.
Detailed Methodology:
- Enzyme Reaction Setup:
- Prepare reaction mixtures containing: 5 μM MsrB1, 1 mM substrate (N-Acetyl-Methionine-R-sulfoxide), 5 mM DTT, 50 mM Tris-HCl (pH 7.5)
- Add inhibitors at desired concentrations
- Incubate at 37°C for 30-60 minutes
- Terminate reactions by adding trifluoroacetic acid (0.1% final concentration)
HPLC Analysis:
- Use reverse-phase C18 column (4.6 × 150 mm, 5μm particle size)
- Employ mobile phase A: 0.1% TFA in water; B: 0.1% TFA in acetonitrile
- Apply gradient: 5-50% B over 20 minutes at 1 mL/min flow rate
- Detect methionine and methionine sulfoxide by UV absorption at 215 nm
- Use authentic standards for retention time identification and quantification
Data Processing:
- Calculate substrate conversion percentage from peak areas
- Determine inhibitor potency by comparing conversion rates with control reactions
- Establish dose-response relationships for IC50 determination
Research Reagent Solutions
Table 3: Essential Research Reagents for MsrB1 Studies
| Reagent/Category | Specific Examples | Function in MsrB1 Research |
|---|---|---|
| MsrB1 Proteins | Recombinant mouse MsrB1 (active form: Sec95 to Cys95; inactive form: Sec95 to Ser95) [17] [7] | Enzyme source for activity and binding assays; mutant forms establish specificity |
| Biosensors | RIYsense (MsrB1/cpYFP/Trx1 fusion protein) [17] [7] | Ratiometric fluorescence measurement of methionine sulfoxide reduction in high-throughput screening |
| Substrates | N-Acetyl-Methionine-R-sulfoxide (N-AcMetO) [17] [7] | Stereospecific substrate for MsrB1 activity assays |
| Reducing Systems | Dithiothreitol (DTT), Thioredoxin/Thioredoxin Reductase/NADPH system [17] [7] | Regenerate reduced MsrB1 for multiple turnover experiments |
| Detection Reagents | NADPH, Fluorescent dyes (NT-647-NHS for MST) [17] [7] | Enable quantification of enzyme activity and binding events |
Visualizing Experimental Workflows
The multifaceted validation of MsrB1 inhibitors through MST, NADPH consumption, and HPLC assays provides complementary data streams that collectively confirm compound efficacy and mechanism of action. The integration of these techniques enabled researchers to identify two promising heterocyclic, polyaromatic compounds that effectively inhibit MsrB1 activity, reduce anti-inflammatory cytokine production, and promote inflammatory responses in vivo. This rigorous validation approach establishes a robust framework for future drug development campaigns targeting MsrB1 in inflammation and cancer immunotherapy contexts, where precise modulation of immune responses is therapeutically valuable.
Methionine sulfoxide reductase B1 (MsrB1) is a selenoprotein found in the cytosol and nucleus that specifically reduces methionine-R-sulfoxide back to methionine in proteins, serving as a crucial regulator of inflammatory responses in macrophages [7] [3]. As a potential therapeutic target for inflammation control, MsrB1 inhibition represents a promising approach for enhancing immune responses in contexts such as chronic infections, vaccine adjuvants, and cancer immunotherapy [7]. The development of specific MsrB1 inhibitors has recently gained momentum with the identification of heterocyclic and polyaromatic compounds that effectively modulate its enzymatic activity and downstream inflammatory pathways [7]. This comparative guide examines the structural and functional properties of lead MsrB1 inhibitors, focusing on their heterocyclic and polyaromatic moieties and providing experimental data to assess their relative efficacy in inflammation research.
Structural Characteristics of Lead MsrB1 Inhibitors
Recent high-throughput screening efforts have identified two promising heterocyclic, polyaromatic compounds as potent MsrB1 inhibitors [7]. These compounds share common structural features while exhibiting distinct chemical architectures that influence their binding affinity and inhibitory potency.
- Compound I: 4-[5-(4-ethylphenyl)-3-(4-hydroxyphenyl)-3,4-dihydropyrazol-2-yl]benzenesulfonamide features a pyrazoline core structure with multiple aromatic systems including phenyl rings with ethyl and hydroxy substitutions, terminated with a benzenesulfonamide group [7].
- Compound II: 6-chloro-10-(4-ethylphenyl)pyrimido[4,5-b]quinoline-2,4-dione presents a more extensive fused polyaromatic system combining pyrimidine and quinoline scaffolds with chlorine and ethylphenyl substitutions [7].
Table 1: Structural Properties of Lead MsrB1 Inhibitors
| Compound | Core Structure | Key Heterocyclic Moieties | Polyaromatic Systems | Functional Groups |
|---|---|---|---|---|
| Compound I | Pyrazoline | Dihydropyrazole | Three phenyl rings | Hydroxyl, sulfonamide |
| Compound II | Fused pyrimidoquinoline | Pyrimidine, quinoline | Four fused rings | Chloro, dione |
Molecular docking simulations reveal that both compounds interact with the MsrB1 active site primarily through their substituted phenyl moieties, forming critical interactions that disrupt enzymatic function [7]. The heterocyclic components provide structural rigidity and facilitate specific molecular recognition, while the polyaromatic systems enable extensive π-orbital interactions with aromatic residues in the binding pocket.
Comparative Efficacy and Experimental Data
In Vitro Inhibition and Binding Affinity
The inhibitory potency of lead compounds was evaluated through multiple biochemical assays, providing quantitative data on their efficacy in disrupting MsrB1 function.
Table 2: In Vitro Efficacy Metrics for MsrB1 Inhibitors
| Compound | Fluorescence Reduction | Molecular Docking Score | Binding Affinity (MST) | NADPH Consumption | HPLC Activity |
|---|---|---|---|---|---|
| Compound I | >50% | High | Strong | Significantly reduced | >70% inhibition |
| Compound II | >50% | High | Strong | Significantly reduced | >70% inhibition |
Both compounds reduced relative fluorescence intensity by more than 50% compared to controls in biosensor-based assays, indicating substantial inhibition of MsrB1 activity [7]. Molecular docking simulations demonstrated favorable binding interactions for both compounds within the MsrB1 active site, while microscale thermophoresis (MST) binding assays confirmed strong affinity between the inhibitors and MsrB1 protein [7]. Additional validation through NADPH consumption assays and HPLC analysis further confirmed the potent inhibitory effects, with both compounds showing greater than 70% inhibition of MsrB1 enzymatic activity [7].
Cellular and In Vivo Anti-inflammatory Efficacy
The functional consequences of MsrB1 inhibition were evaluated in cellular models and in vivo systems, demonstrating significant effects on inflammatory pathways.
Table 3: Cellular and In Vivo Efficacy of MsrB1 Inhibitors
| Compound | IL-10 Expression | IL-1rn Expression | Ear Edema | Skin Thickness | In Vivo Model |
|---|---|---|---|---|---|
| Compound I | Decreased | Decreased | Increased | Increased | Mouse ear edema |
| Compound II | Decreased | Decreased | Increased | Increased | Mouse ear edema |
Both compounds significantly decreased expression of anti-inflammatory cytokines including IL-10 and IL-1 receptor antagonist (IL-1rn), effectively shifting the immune balance toward enhanced inflammatory responses [7]. This cytokine modulation pattern effectively mimicked the phenotype observed in MsrB1 knockout mice, which display attenuated induction of anti-inflammatory cytokines and excessive pro-inflammatory cytokine production [3]. In mouse ear edema models, both inhibitors induced auricular skin swelling and increased thickness, confirming their pro-inflammatory effects in vivo [7]. These findings align with the established role of MsrB1 in promoting anti-inflammatory cytokine expression in macrophages and controlling acute tissue inflammation [3].
Experimental Protocols and Methodologies
High-Throughput Screening Using RIYsense Biosensor
The identification of lead MsrB1 inhibitors employed a novel redox protein-based fluorescence biosensor (RIYsense) composed of MsrB1, a circularly permuted yellow fluorescent protein (cpYFP), and thioredoxin1 in a single polypeptide chain [7].
Protocol:
- Biosensor Construction: The recombinant RIYsense construct was assembled in a pET-28a vector and expressed in Rosetta2 pLysS E. coli cells [7].
- Protein Purification: Transformed cells were cultured, induced with 0.7 mM IPTG at 18°C for 18 hours, then harvested and lysed by sonication. The protein was purified using affinity chromatography with a HisTrap HP column [7].
- Fluorescence Measurement: Purified RIYsense protein was reduced with DTT, desalted, and diluted to 4 μM concentration. Fluorescence measurements were conducted using a TECAN SPARK multimode microplate reader with excitation at 420 nm and 485 nm, and emission at 545 nm [7].
- Compound Screening: The biosensor was used to screen 6,868 compounds, selecting 192 candidates that reduced relative fluorescence intensity by more than 50% compared to controls [7].
High-Throughput Screening Workflow for MsrB1 Inhibitors
Molecular Docking and Binding Affinity Assays
Potential inhibitors identified through screening underwent computational and biophysical validation.
Molecular Docking Protocol:
- Structure Preparation: MsrB1 protein structure was prepared by adding hydrogen atoms and optimizing side-chain conformations.
- Compound Preparation: Ligand structures were energy-minimized using appropriate force fields.
- Docking Simulation: Automated docking was performed to predict binding poses and interaction energies between compounds and the MsrB1 active site [7].
Binding Affinity Assays:
- Microscale Thermophoresis (MST): Compounds were titrated against constant concentration of fluorescently labeled MsrB1, and binding curves were generated based on thermophoretic movement changes [7].
- NADPH Consumption Assay: MsrB1 activity was measured by monitoring NADPH oxidation at 340 nm in the presence and absence of inhibitors [7].
- HPLC Analysis: Direct measurement of methionine sulfoxide reduction by MsrB1 using reverse-phase HPLC to quantify inhibitory effects [7].
In Vivo Inflammation Models
The functional efficacy of lead compounds was validated using established inflammation models.
Mouse Ear Edema Protocol:
- Animal Treatment: Mice were treated with TPA (12-O-tetradecanoylphorbol-13-acetate) applied to the left auricle with acetone applied to the right auricle as control [3].
- Inhibitor Administration: Selected compounds were administered concurrently with TPA treatment.
- Measurement: Ear thickness was measured 24 hours after treatment using precision calipers [7] [3].
- Tissue Analysis: Ear tissues were preserved in 4% paraformaldehyde, embedded in paraffin, sectioned at 5 μm, and stained with hematoxylin and eosin for histological examination [3].
Signaling Pathways and Mechanism of Action
MsrB1 inhibitors exert their effects through a defined molecular pathway that regulates inflammatory responses in macrophages. The mechanism involves modulation of cytokine expression through redox-dependent processes.
MsrB1 Inhibition Inflammatory Signaling Pathway
The pathway begins with MsrB1 inhibitors binding to the enzyme's active site, disrupting its ability to reduce methionine-R-sulfoxide residues in substrate proteins [7]. This inhibition impairs the repair of oxidized methionine residues in regulatory proteins such as actin, which undergoes Mical-mediated oxidation and MsrB1-dependent reduction cycles that influence cytoskeletal dynamics in macrophages [3]. The disruption of this redox regulation leads to attenuated induction of anti-inflammatory cytokines including IL-10 and IL-1 receptor antagonist, creating an imbalance that favors pro-inflammatory responses [7] [3]. This cytokine shift manifests physiologically as enhanced tissue inflammation, demonstrated by increased auricular skin swelling and thickness in ear edema models [7].
Research Reagent Solutions
The following table details essential research reagents and materials for studying MsrB1 inhibitors and their effects in inflammation models.
Table 4: Essential Research Reagents for MsrB1 Inhibitor Studies
| Reagent/Material | Application | Function | Example Source |
|---|---|---|---|
| RIYsense Biosensor | High-throughput screening | Fluorescent detection of MsrB1 activity | [7] |
| Recombinant MsrB1 | Enzymatic assays | Source of purified enzyme for in vitro studies | [7] |
| Thioredoxin1 System | Reductase activity assays | Natural reducing system for MsrB1 | [7] |
| N-AcMetO | Substrate for assays | Standardized methionine sulfoxide substrate | [7] |
| LPS | Macrophage activation | Induces inflammatory signaling and MsrB1 expression | [3] |
| TPA (12-O-tetradecanoylphorbol-13-acetate) | In vivo inflammation model | Induces ear edema for efficacy testing | [3] |
| MST Instrumentation | Binding affinity studies | Measures compound-protein interactions | [7] |
The structural analysis of heterocyclic and polyaromatic MsrB1 inhibitors reveals distinct compound classes with significant potential for modulating inflammatory responses. Compound I (pyrazoline-based) and Compound II (fused pyrimidoquinoline-based) both demonstrate potent MsrB1 inhibition through complementary structural features, with validated efficacy in biochemical, cellular, and in vivo models. Their shared ability to decrease anti-inflammatory cytokine expression and promote tissue inflammation highlights the therapeutic potential of MsrB1 inhibition in clinical contexts requiring enhanced immune responses. The experimental protocols and reagent solutions outlined provide a framework for continued investigation of structure-activity relationships in this emerging drug class, supporting ongoing efforts to optimize MsrB1-targeted therapeutics for inflammation management.
Challenges, Selectivity, and Efficacy Optimization in MsrB1 Inhibitor Development
The methionine sulfoxide reductase (Msr) system is a crucial enzymatic family responsible for repairing oxidative damage to proteins, a process intimately linked to inflammatory pathways and cellular aging [28]. This system counters the oxidation of methionine residues to methionine sulfoxide (MetSO), which exists as two stereoisomers: methionine-S-sulfoxide (Met-S-SO) and methionine-R-sulfoxide (Met-R-SO) [29] [30]. The Msr family specializes in reducing these isomers back to methionine, with MsrA specifically reducing Met-S-SO and MsrB enzymes reducing Met-R-SO [30] [28]. In mammals, the Msr system comprises MsrA and three MsrB proteins (MsrB1, MsrB2, and MsrB3), each with distinct subcellular localizations and functions [31] [28]. MsrB1 is particularly noteworthy as a selenoprotein containing selenium in its catalytic cysteine residue, primarily located in the cytoplasm and nucleus, and possessing the highest specific activity among MsrB proteins [31] [28].
Within inflammation research, achieving selective inhibition of MsrB1 presents both a significant challenge and therapeutic opportunity. The high degree of functional conservation across Msr enzymes—catalyzing similar chemical reactions but on different substrate stereoisomers—complicates the development of specific inhibitors [29]. However, structural biology and enzymology studies have revealed critical differences in active site architecture and catalytic mechanisms that can be exploited for selective drug design. This comparative guide examines current approaches for targeting MsrB1 specifically, providing experimental data and methodologies relevant to researchers developing anti-inflammatory therapies through modulation of the Msr system.
Comparative Analysis of Msr Enzyme Family Members
Table 1: Key Characteristics of Major Mammalian Msr Enzymes
| Enzyme | Gene | Substrate Specificity | Subcellular Localization | Cofactor Requirements | Tissue Distribution |
|---|---|---|---|---|---|
| MsrB1 | MSRB1 | Met-R-SO (protein-bound) | Cytoplasm, Nucleus [28] | Thioredoxin, Selenocysteine [31] [28] | Ubiquitous, high in liver, kidney |
| MsrA | MSRA | Met-S-SO (protein-bound and free) [29] | Mitochondria, Cytoplasm [28] | Thioredoxin, DTT [31] | Ubiquitous |
| MsrB2 | MSRB2 | Met-R-SO (protein-bound) | Mitochondria [28] | Thioredoxin [31] | Ubiquitous |
| MsrB3 | MSRB3 | Met-R-SO (protein-bound) | ER (MsrB3A), Mitochondria (MsrB3B) [28] | Thioredoxin [31] | Ubiquitous |
Table 2: Quantitative Enzymatic Activity Profiles of Recombinant Msr Enzymes
| Enzyme | Specific Activity* (nmol/min/mg) | Fold Activation with Fusaricidin Analogues | Reductant System Preference | Inhibition by Common Msr Inhibitors |
|---|---|---|---|---|
| MsrB1 | 410.2 ± 22.7 (bovine) [32] | 2-3 fold (human) [33] | Thioredoxin/DTT [31] | Limited data |
| MsrA | 206.8 ± 45.2 (mouse, with mesoridazine) [29] | 3-6 fold (bovine/human) [33] | DTT/Thioredoxin [31] | Substrate-competitive inhibitors |
| MsrB2 | Not reported | 2-3 fold (human) [33] | Thioredoxin [31] | Limited data |
| MsrB3 | Not reported | 2-3 fold (human) [33] | Thioredoxin [31] | Limited data |
*Specific activity values vary significantly based on substrate and assay conditions
The structural and mechanistic differences between Msr enzymes provide the fundamental basis for developing selective inhibitors. MsrA and MsrB enzymes share no significant sequence homology (approximately 26.77% sequence similarity) despite catalyzing chemically similar reactions [30]. MsrB1's unique status as a selenoprotein, with selenium incorporated at the active site cysteine residue, represents a particularly promising target for selective inhibition strategies [28]. The catalytic mechanism of Msr enzymes involves a series of redox reactions that ultimately reduce methionine sulfoxide back to methionine, utilizing thioredoxin, thioredoxin reductase, and NADPH as the natural reducing system, though dithiothreitol (DTT) can substitute in vitro [31] [29].
The subcellular localization of each Msr enzyme further complicates inhibition strategies, as compounds must reach the appropriate compartment to exert their effects. MsrB1's cytoplasmic and nuclear localization potentially makes it more accessible to small molecule inhibitors than mitochondrial-localized family members like MsrB2 [28]. Additionally, MsrB1 demonstrates the highest specific activity among MsrB proteins, positioning it as a key therapeutic target for inflammatory conditions where oxidative protein damage contributes to pathology [31].
Experimental Approaches for Assessing Inhibition Specificity
Enzyme Activity Assays and Specificity Screening
Table 3: Standardized Experimental Protocols for Msr Inhibition Studies
| Method | Key Reagents | Procedure Overview | Advantages | Limitations |
|---|---|---|---|---|
| Colorimetric DTT Consumption Assay [32] | DTT, DTNB (Ellman's reagent), Methionine sulfoxide substrates | Monitor Msr-catalyzed DTT oxidation by decreased absorbance at 412 nm after DTNB reaction | Rapid, simple, no specialized equipment required | Indirect measurement, DTT can reduce non-specifically |
| HPLC-Based Substrate Reduction [29] | DABS-Met-R-SO (MsrB) or DABS-Met-S-SO (MsrA), DTT or thioredoxin system | Separate and quantify reaction products via HPLC with fluorescence/UV detection | Direct activity measurement, handles multiple substrates | Time-consuming, requires HPLC equipment |
| Cellular Thermal Shift Assay (CETSA) | Intact cells or lysates, test compounds, Western blot/MS detection | Monitor protein thermal stability changes after compound binding | Confirms target engagement in physiological systems | Does not measure functional inhibition |
| Liver Lysate Activity Profiling [29] | Tissue lysates (e.g., from KO mice), DTT, methylsulfinyl substrates | Compare compound effects on endogenous enzyme activities in complex mixtures | Physiological context, multiple enzymes simultaneously | Complex data interpretation |
Reliable assessment of MsrB1 inhibition specificity requires orthogonal experimental approaches that can distinguish between effects on different Msr family members. The colorimetric DTT consumption assay provides a rapid screening method based on the principle that Msr-catalyzed reduction of methionine sulfoxide coincides with oxidation of DTT, which can be quantified using Ellman's reagent (DTNB) [32]. This assay enables high-throughput screening of compound libraries but should be supplemented with more specific methods for confirmation.
HPLC-based approaches offer direct measurement of substrate reduction using specialized substrates like dimethyl aminoazo-benzenesulfonyl-methionine sulfoxide (DABS-MetO) [33]. For MsrB1 specificity, DABS-Met-R-SO serves as the preferred substrate, while DABS-Met-S-SO is used for MsrA activity measurements [29]. These assays can utilize either DTT or the more physiologically relevant thioredoxin/thioredoxin reductase/NADPH reducing system, though activation folds observed with fusaricidin analogues are significantly lower with the thioredoxin system (1.2-1.4 fold versus 3-6 fold with DTT) [33].
Validation in cellular and tissue contexts represents a critical step in confirming inhibitor specificity. Studies using liver lysates from wild-type, MsrA knockout, and MsrB1 knockout mice have demonstrated the essential role of MsrA in reducing methylsulfinyl-containing drugs like mesoridazine and sulmazole, with MsrA knockout lysates showing severely compromised reduction capability while MsrB1 knockout lysates performed similarly to wild-type [29]. This experimental approach provides a physiological relevant system for evaluating compound specificity across multiple Msr enzymes simultaneously.
The Researcher's Toolkit: Essential Reagents for MsrB1 Studies
Table 4: Essential Research Reagents for MsrB1 Selectivity Investigations
| Reagent/Category | Specific Examples | Research Application | Considerations for Selective Inhibition Studies |
|---|---|---|---|
| Recombinant Enzymes | Human MsrB1, MsrA, MsrB2, MsrB3 [33] | In vitro inhibition assays | Ensure consistent expression systems and purification methods |
| Specialized Substrates | DABS-Met-R-SO, DABS-Met-S-SO [33] | Enzyme activity measurements | Substrate purity and stereospecificity critical |
| Reducing Systems | DTT, Thioredoxin/Thioredoxin Reductase/NADPH [31] [29] | Maintaining enzyme activity | Thioredoxin system more physiological but lower signal |
| Cell Line Models | MCF-7, MDA-MB-231 [31] | Cellular activity assessment | Endogenous Msr expression levels vary |
| Animal Models | MsrA KO, MsrB1 KO mice [29] | In vivo target validation | Compensation mechanisms may develop |
| Chemical Probes | Fusaricidin analogues [33] | Positive controls for activation | Show varying potency across Msr enzymes |
| N-Isononylcyclohexylamine | N-Isononylcyclohexylamine|High-Purity Research Chemical | N-Isononylcyclohexylamine is a high-purity amine for research use only (RUO). Explore its applications in organic synthesis and material science. Not for human or veterinary use. | Bench Chemicals |
Strategic Framework for Selective MsrB1 Inhibitor Development
Exploiting Structural and Mechanistic Differences
The development of selective MsrB1 inhibitors capitalizes on several key structural and functional distinctions within the Msr enzyme family. First, MsrB1's unique selenocysteine active site residue presents opportunities for selective targeting not available against cysteine-containing MsrA and other MsrB enzymes [28]. The distinct substrate binding pockets between MsrA and MsrB enzymes, which evolved to accommodate different methionine sulfoxide stereoisomers, provide additional targeting opportunities. While MsrA demonstrates broad substrate specificity capable of reducing both protein-bound Met-S-SO and free methyl sulfoxide compounds including DMSO and l-methionine sulfoxide, MsrB enzymes exhibit more restricted substrate profiles [29] [32].
Recent research has identified compound classes with varying selectivity across Msr enzymes. Fusaricidin analogues, particularly cyclic lipohexapeptides, have demonstrated the ability to activate recombinant bovine and human MsrA (3-6 fold) and human MsrB2 and MsrB3 (2-3 fold) to different extents, suggesting these structural scaffolds can be modified to enhance specificity [33]. Structure-activity relationship studies have revealed that an arginine or lysine in position R6 of the cyclic hexapeptide moiety and the fatty acid tail are critical for activation potency, providing starting points for medicinal chemistry optimization [33].
Figure 1: MsrB1 Catalytic Cycle and Inhibition Strategy
Cellular and Physiological Validation Approaches
Rigorous validation of putative selective MsrB1 inhibitors requires multifaceted experimental approaches across biological complexity levels. Initial specificity profiling against recombinant enzymes should be followed by cellular studies using lines with varying endogenous Msr expression patterns, such as MCF-7 (high MsrB1) versus MDA-MB-231 (low MsrB1) breast cancer cells [31]. These models enable assessment of target engagement and differential cellular responses based on MsrB1 expression levels.
Physiological validation exploiting tissue lysates from genetic knockout models provides critical evidence of specificity. Research has demonstrated that liver lysates from MsrA knockout mice show severely compromised reduction capability for methylsulfinyl compounds like mesoridazine and sulmazole, while MsrB1 knockout lysates perform similarly to wild-type, confirming MsrA's primary role in this activity and providing a validation system for MsrB1-specific inhibitors [29]. Additionally, monitoring potential cross-reactivity with related redox enzymes like thioredoxin reductase and glutathione peroxidase is essential, particularly given MsrB1's selenocysteine residue and dependence on thioredoxin recycling systems [31] [29].
Figure 2: Experimental Validation Workflow for Selective Inhibitors
The development of selective MsrB1 inhibitors represents a promising but challenging frontier in redox biology and inflammation research. Current evidence suggests that exploiting structural differences in the active sites—particularly MsrB1's selenocysteine residue—and substrate binding pockets offers the most direct path to achieving specificity. The emerging compound classes like fusaricidin analogues that show differential effects across Msr enzymes provide valuable starting points for medicinal chemistry optimization [33].
Future research directions should focus on structural biology efforts to obtain high-resolution complexes of MsrB1 with selective ligands, implementation of more physiologically relevant assay conditions using thioredoxin reducing systems, and exploration of the therapeutic potential of selective MsrB1 inhibition in inflammatory disease models. As the understanding of Msr biology continues to evolve, particularly in inflammatory processes, the case for developing selective MsrB1 inhibitors as research tools and potential therapeutics grows increasingly compelling. The experimental frameworks and comparative data presented here provide a foundation for these ongoing research efforts aimed at overcoming the specificity hurdles in targeting individual members of the Msr enzyme family.
In the pursuit of effective anti-inflammatory therapeutics, the journey from identifying a lead compound to developing a viable clinical candidate is fraught with challenges, particularly concerning cellular delivery and stability. These pharmacological properties often determine whether a promising molecule in vitro will translate to an effective treatment in vivo. Within the context of inflammation research, methionine sulfoxide reductase B1 (MsrB1) has emerged as a critical enzyme target due to its role in mitigating oxidative stress and regulating inflammatory pathways. However, the efficacy of MsrB1 inhibitors is heavily dependent on their ability to reach intracellular targets in active form and sufficient concentration while maintaining structural stability. This comparison guide objectively evaluates current approaches to enhancing these pharmacological properties, providing researchers with experimental data and methodologies to inform their drug development strategies.
The significance of delivery and stability extends across all therapeutic modalities, from small molecules to biologic drugs. For enzyme-based therapeutics, which represent a growing segment of anti-inflammatory treatments, stability challenges are particularly pronounced. Natural anti-inflammatory enzymes—including catalase, superoxide dismutase, trypsin, chymotrypsin, nattokinase, bromelain, and serratiopeptidase—demonstrate impressive efficacy in principle but face substantial delivery obstacles [34]. These challenges include susceptibility to proteolytic degradation, poor cellular uptake, rapid clearance, and immunogenic responses, all of which must be addressed through deliberate formulation strategies.
Comparative Analysis of Delivery and Stability Enhancement Technologies
Quantitative Comparison of Delivery Systems
Table 1: Comparison of delivery system efficacy for anti-inflammatory compounds
| Delivery System | Compound Type | Stability Improvement | Cellular Uptake Efficiency | Key Findings | Experimental Model |
|---|---|---|---|---|---|
| GMMA Platform | Shigella O-antigen | Maintained O-antigen density with reduced reactogenicity [35] | Induced robust antibody and cellular immune responses [35] | msbB deletion enabled higher OAg-to-protein ratio while reducing lipid A toxicity [35] | Mouse and rabbit immunization models [35] |
| Enzyme Formulations | Therapeutic enzymes (catalase, SOD, proteases) | Short in vivo half-life; requires stabilization [34] | Variable; often poor intracellular delivery [34] | Enzyme engineering and nanoformulations improve stability and specificity [34] | In vitro and preclinical inflammatory models [34] |
| Nanoparticle Systems | Small molecule inhibitors | Protection from degradation; controlled release [34] | Enhanced permeability and retention effect [34] | Improved bioavailability and reduced dosing frequency [34] | Cell culture and animal disease models [34] |
| Lipid-Based Carriers | Nucleic acids, proteins | Protection from nucleases/proteases [34] | Endocytosis-mediated internalization [34] | Efficient intracellular delivery but potential cytotoxicity [34] | In vitro transfection studies [34] |
Stability Assessment Under Physiological Conditions
Table 2: Stability profiles of therapeutic modalities under simulated physiological conditions
| Therapeutic Modality | Half-Life (In Vitro) | Stability-Limiting Factors | Stabilization Approaches | Impact on Efficacy |
|---|---|---|---|---|
| Recombinant Enzymes | Minutes to hours [34] | Proteolysis, oxidation, denaturation [34] | PEGylation, immobilization, mutagenesis [34] | Extended activity duration; reduced dosing frequency [34] |
| Small Molecule Inhibitors | Highly variable | Hepatic metabolism, chemical degradation [36] | Structural modification, prodrug approaches [36] | Maintained target engagement; reduced metabolite toxicity |
| GMMA Vaccines | Stable at 2-8°C for months [35] | Aggregation, O-antigen detachment [35] | Optimized buffer composition, lyophilization [35] | Consistent immunogenicity across batches [35] |
| Nucleic Acid Therapies | Seconds to minutes (unmodified) [34] | Nuclease degradation [34] | Chemical modification, carrier encapsulation [34] | Sustained gene silencing/expression [34] |
Experimental Protocols for Assessing Delivery and Stability
Protocol for Evaluating Cellular Uptake and Intracellular Trafficking
Objective: Quantify cellular internalization and subcellular localization of lead compounds.
Methodology:
- Compound Labeling: Fluorescently tag test compounds using appropriate chemistries (e.g., FITC, Cy dyes, Alexa Fluor). Verify labeling does not significantly alter biological activity through parallel activity assays.
- Cell Culture: Seed appropriate cell lines (e.g., macrophages for inflammation research) in chambered coverslips at 60-70% confluence. Use a minimum of three biological replicates per condition.
- Dosing and Incubation: Apply fluorescently labeled compounds at predetermined concentrations (typically based on IC50 values). Include controls (untreated cells, competitive inhibition). Incubate for varying durations (15 min to 24 h) at 37°C/5% CO2.
- Internalization Block: To distinguish surface binding from internalization, include parallel samples incubated at 4°C to inhibit endocytosis.
- Fixation and Staining: Fix cells with 4% paraformaldehyde, permeabilize with 0.1% Triton X-100 (for intracellular staining), and counterstain with organelle-specific markers (e.g., LysoTracker for lysosomes, MitoTracker for mitochondria).
- Imaging and Analysis: Acquire images via confocal microscopy. Quantify fluorescence intensity in cellular compartments using image analysis software (e.g., ImageJ, CellProfiler). Calculate Pearson's correlation coefficients for co-localization analysis.
Key Parameters: Time-dependent internalization, subcellular localization, concentration dependence.
Protocol for Determining Stability in Physiological Simulants
Objective: Assess compound integrity under conditions mimicking in vivo environment.
Methodology:
- Simulant Preparation: Prepare relevant physiological simulants: simulated gastric fluid (SGF, pH 1.2), simulated intestinal fluid (SIF, pH 6.8), plasma simulant (PBS with relevant proteins), and lysosomal simulant (acidic buffer with cathepsins).
- Compound Exposure: Incubate test compounds in each simulant at physiological temperature (37°C). Use appropriate concentrations reflecting expected in vivo levels.
- Time-Point Sampling: Collect aliquots at predetermined time points (0, 0.5, 1, 2, 4, 8, 24 h). Immediately quench reactions (e.g., protease inhibitors, pH adjustment).
- Stability Assessment:
- Analytical Methods: Employ HPLC, LC-MS, or gel electrophoresis to quantify intact compound.
- Activity Measurements: Assess remaining biological activity using target-specific assays.
- Structural Analysis: Utilize circular dichroism, fluorescence spectroscopy, or NMR for structural integrity.
- Kinetic Analysis: Plot remaining intact/active compound versus time. Calculate degradation rate constants and half-lives using appropriate kinetic models.
Key Parameters: Degradation half-life, structural integrity, functional activity retention.
Visualization of Experimental Workflows and Biological Pathways
Experimental Workflow for Compound Delivery and Stability Assessment
Biological Pathways in Inflammation and Compound Mechanisms
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key research reagents for delivery and stability studies
| Reagent/Material | Function/Application | Specific Examples | Considerations for Use |
|---|---|---|---|
| Fluorescent Tags | Compound tracking and localization | FITC, Cy dyes, Alexa Fluor derivatives | Verify tags don't alter bioactivity; consider hydrophobicity effects |
| Protease Inhibitors | Prevent enzymatic degradation during processing | PMSF, protease inhibitor cocktails | Use broad-spectrum for unknown proteases; consider cytotoxicity |
| Lipid-Based Transfection Reagents | Enhance cellular uptake | Lipofectamine, cationic lipids | Optimize charge ratio; assess membrane disruption |
| Cell Culture Models | In vitro delivery and efficacy assessment | Primary macrophages, epithelial lines | Select relevant cell types; consider barrier models for transport studies |
| Analytical Chromatography | Stability and metabolite assessment | HPLC, LC-MS systems | Validate methods for parent compound and major metabolites |
| Molecular Probes | Pathway activation assessment | Phospho-specific antibodies, ROS sensors | Establish temporal patterns; use multiple readouts for validation |
| GMMA Production System | Vaccine delivery platform | msbB-deficient bacterial strains [35] | Optimize O-antigen to protein ratio; assess reactogenicity [35] |
| Enzyme Engineering Tools | Stability and activity optimization | Site-directed mutagenesis, PEGylation reagents | Monitor immunogenicity changes with modifications |
Comparative Performance Analysis and Future Directions
The comparative data presented in this guide reveals several critical patterns in addressing delivery and stability challenges. GMMA technology demonstrates how strategic genetic modifications (e.g., msbB deletion) can simultaneously improve safety profiles (reduced endotoxicity) while maintaining critical antigen density [35]. For enzyme-based therapeutics, stability remains a primary constraint, with half-lives often measured in minutes to hours, necessitating sophisticated formulation approaches [34]. The emerging field of enzyme engineering offers promising strategies to enhance both stability and delivery, including site-specific mutagenesis for protease resistance, fusion constructs for improved targeting, and encapsulation technologies for protected delivery.
Future innovations in cellular delivery and stability will likely focus on personalized approaches that account for individual variations in metabolism and disease pathology. Advances in bioresponsive delivery systems that release active compounds specifically at sites of inflammation represent a particularly promising direction. Additionally, the integration of machine learning approaches to predict degradation pathways and optimal formulation parameters based on compound structures will accelerate the optimization process. As demonstrated by the successful development of GMMA-based vaccines with improved stability and immunogenicity profiles [35], systematic approaches to addressing delivery and stability challenges can yield significant dividends in the development of effective anti-inflammatory therapeutics.
In the pursuit of novel anti-inflammatory therapeutics, a compelling strategy has emerged: correlating the inhibition of specific enzymes with the suppression of key anti-inflammatory cytokines, notably Interleukin-10 (IL-10) and Interleukin-1 Receptor Antagonist (IL-1RA). While IL-10 and IL-1RA are traditionally considered anti-inflammatory, their dysregulation can paradoxically contribute to chronic disease states. In conditions like rheumatoid arthritis, for example, T cells can become resistant to the immunosuppressive effects of IL-10, undermining its homeostatic function [37]. Similarly, the IL-1 pathway is a critical inflammatory switch; its activity is determined by the balance between the pro-inflammatory IL-1β and its endogenous inhibitor, IL-1RA [38]. Therefore, the strategic suppression of these cytokines' production or function via enzyme inhibition represents a sophisticated approach to rebalancing the immune system.
This comparative guide evaluates the functional potency of various inhibitory compounds and therapeutic modalities by examining their efficacy in disrupting this specific cytokine network. We focus on the correlation between enzymatic inhibition and the downstream suppression of IL-10 and IL-1ra, providing researchers and drug development professionals with a structured analysis of experimental data and methodologies.
Key Cytokines and Their Complex Roles in Inflammation
Interleukin-1 Receptor Antagonist (IL-1RA)
IL-1RA is a naturally occurring cytokine that acts as a decoy receptor for the IL-1 receptor, effectively blocking the potent pro-inflammatory signaling of IL-1β [38]. Its critical role is highlighted in experiments where it protects mice from lethal endotoxemia [38]. While it is an anti-inflammatory agent, its production is often co-regulated with pro-inflammatory mediators. For instance, IL-10 can markedly potentiate the production of IL-1RA in LPS-stimulated polymorphonuclear leukocytes, creating a complex feedback loop [38]. In therapeutic contexts, the amount of IL-1RA secreted by cells like mesenchymal stromal cells (MSCs) is a direct measure of their immunomodulatory potency [39].
Interleukin-10 (IL-10)
IL-10 is a key immunoregulatory cytokine that inhibits the production and function of pro-inflammatory cytokines from macrophages and Th1 cells [37]. It functions by engaging the IL-10 receptor complex, which phosphorylates and activates STAT3 signaling [37]. However, in chronic inflammatory diseases like rheumatoid arthritis, this signaling pathway can become impaired. CD4+ T cells from RA patients show resistance to IL-10 inhibition, allowing for continued production of interferon gamma (IFN-γ) despite the presence of IL-10 [37]. This resistance is associated with sustained STAT3 activation and altered expression of suppressor of cytokine signaling (SOCS) proteins [37]. Environmental stressors can also disrupt this balance, as seen in Antarctic isolation studies where plasma levels of IL-10 were suppressed [40].
Table 1: Key Anti-Inflammatory Cytokines in Immunomodulation
| Cytokine | Primary Function | Regulation | Pathological Context |
|---|---|---|---|
| IL-1RA | Competitive inhibitor of the IL-1 receptor, blocking IL-1β signaling [38] | Upregulated by IL-10; released by MSCs in response to M1 macrophages [38] [39] | The balance between IL-1β and IL-1RA dictates inflammatory activity [38] |
| IL-10 | Suppresses pro-inflammatory cytokine production from macrophages and Th1 cells [37] | Can be suppressed by environmental stress; its signaling is impaired in chronic inflammation [40] [37] | Resistance to IL-10 inhibition in RA T cells permits persistent inflammation [37] |
Comparative Analysis of Inhibitor Efficacy and Experimental Data
This section compares the functional potency of different compounds and therapeutic classes based on their ability to inhibit target enzymes and subsequently suppress IL-10 and/or IL-1ra.
Manumycin-Type Polyketides
Manumycin A and related compounds are secondary metabolites from Streptomyces bacteria that exhibit strong anti-inflammatory features by targeting multiple enzymes.
Table 2: Functional Potency of Manumycin-Type Polyketides [41]
| Compound | Primary Enzyme Targets | Effect on Cytokines | Cellular Model | Potency (Concentration Range) |
|---|---|---|---|---|
| Manumycin A | Ras-farnesyltransferase, Caspase-1, IKK kinase β subunit, Thioredoxin reductase TrxR-1 [41] | Efficient, concentration-dependent inhibition of IL-1β and TNF expression [41] | Human monocyte/macrophage cell line THP-1 upon LPS stimulation [41] | 0.25 – 5 μM |
| Manumycin B | Likely similar to Manumycin A (structural analog) [41] | Efficient inhibition of IL-1β and TNF; significantly lower pro-apoptotic effect than Manumycin A [41] | Human monocyte/macrophage cell line THP-1 upon LPS stimulation [41] | 0.25 – 5 μM |
| Asukamycin | Likely similar to Manumycin A (structural analog) [41] | Efficient inhibition of IL-1β and TNF; significantly lower pro-apoptotic effect than Manumycin A [41] | Human monocyte/macrophage cell line THP-1 upon LPS stimulation [41] | 0.25 – 5 μM |
| Colabomycin E | Likely similar to Manumycin A (structural analog) [41] | Efficient inhibition of IL-1β and TNF; significantly lower pro-apoptotic effect than Manumycin A [41] | Human monocyte/macrophage cell line THP-1 upon LPS stimulation [41] | 0.25 – 5 μM |
Experimental Protocol for Manumycin-Type Polyketides [41]:
- Cell Culture: THP-1 cells (human monocytic leukemia cell line) are cultured in RPMI-1640 medium supplemented with 10% fetal calf serum, 2 mM L-glutamine, penicillin, and streptomycin.
- Cell Stimulation: Cells are seeded at a concentration of 10^6 cells/1 mL and stimulated with LPS (1 μg/mL) to induce an inflammatory response.
- Compound Treatment: Test compounds (Manumycin A, B, Asukamycin, Colabomycin E) are dissolved in DMSO and applied to the cells at three different concentrations (5 μM, 1 μM, and 0.25 μM) concurrently with LPS stimulation.
- Control Groups: LPS-stimulated cells without compounds serve as a positive control for inflammation.
- Outcome Measurement: After the incubation period, the expression and/or secretion of IL-1β and TNF are measured, typically via ELISA or RT-PCR. Cell viability assays are performed in parallel to assess cytotoxicity.
Therapeutic Enzymes and Biologics
Enzyme-based therapeutics and biologics offer a distinct mechanism for modulating inflammation, often by degrading or neutralizing inflammatory mediators.
Table 3: Functional Potency of Enzymes and Biologic Inhibitors
| Therapeutic Class / Compound | Primary Enzyme Targets / Mechanism | Effect on Cytokines / Pathways | Clinical Context / Model |
|---|---|---|---|
| Canakinumab | Human monoclonal antibody targeting IL-1β [42] | Directly neutralizes IL-1β activity, indirectly affecting the IL-1β/IL-1RA balance [42] | Reduces recurrent cardiovascular events in patients with coronary artery disease [42] |
| Anakinra | Recombinant form of human IL-1RA [42] | Competitively inhibits IL-1 receptor binding, blocking IL-1β signaling [42] | Evaluated in randomized controlled trials for coronary artery disease [42] |
| Colchicine | Microtubule polymerization inhibitor; affects multiple inflammatory pathways [42] | Reduces NLRP3 inflammasome activity, thereby inhibiting IL-1β production [42] | Significantly reduces the odds of stroke (OR 0.26) and risk of revascularization in CAD [42] |
| Serratiopeptidase | Microbial protease produced by Serratia species [34] | Functions as a potent anti-inflammatory agent, though its specific cytokine targets are less defined [34] | Used as a potent alternative to NSAIDs [34] |
Detailed Experimental Protocols for Key Assays
This protocol measures the anti-inflammatory potency of Mesenchymal Stromal Cells (MSCs) by quantifying their secretion of IL-1RA in an M1 macrophage-driven inflammatory model.
Workflow:
- Macrophage Differentiation: THP-1 monocytic cells are differentiated into macrophages by incubation with 150 nmol/mL phorbol 12-myristate 13-acetate (PMA) for 48 hours.
- Co-culture Setup: Differentiated macrophages are co-cultured with ABCB5+ MSCs. The optimal ratio for near-maximal IL-1RA stimulation should be determined empirically (e.g., testing a wide range of MSC/macrophage ratios).
- M1 Polarization and Stimulation: M1 polarization is induced by adding 50 IU/mL recombinant human IFN-γ at the start of co-culture, followed by a second dose of 50 IU/mL IFN-γ and 20 ng/mL LPS from E. coli after 24 hours.
- Control Groups: Include unstimulated MSC/macrophage co-cultures and macrophage-only cultures.
- Validation of Macrophage Polarization: Confirm successful M1 polarization via flow cytometric analysis for the surface markers CD36 (differentiation marker) and CD80 (M1 marker). Successful polarization is achieved if at least 50% of macrophages express both markers.
- Outcome Measurement: After 48 hours of co-culture, collect supernatants and quantify IL-1RA concentration using a validated colorimetric sandwich ELISA.
- Assay Validation: The ELISA method must be validated for parameters like selectivity, accuracy, precision, and total error according to regulatory guidelines (e.g., EMA/FDA). The lower limit of quantification (LLOQ) should be established (e.g., 125 pg/mL) [39].
This protocol is used to investigate impaired IL-10 signaling in CD4+ T cells from patients with chronic inflammatory diseases.
Workflow:
- Cell Isolation: Purify CD4+ T cells from patient peripheral blood mononuclear cells (PBMC) or synovial tissue using anti-CD4 monoclonal antibody-coated magnetic beads.
- Cell Stimulation and Culture: Resuspend CD4+ T cells (1 × 10^6 cells/mL) and culture them in wells pre-coated with anti-CD3 mAb (1 μg/mL). Stimulate the cells with soluble anti-CD28 mAb (1 μg/mL) in the presence or absence of IL-10 (e.g., 1 ng/mL).
- Outcome Measurement: Collect culture supernatants after 36 hours and measure IFN-γ concentration as a functional readout of T-cell activity. Resistance to IL-10 is indicated by high levels of IFN-γ production even in the presence of IL-10.
- Signaling Analysis: To probe the mechanism, analyze the phosphorylation state of STAT3 in CD4+ T cells after IL-10 stimulation, often via western blot or flow cytometry. Also, examine the mRNA expression levels of SOCS1 and SOCS3 using real-time PCR.
Signaling Pathways and Conceptual Workflows
IL-10 and IL-1RA Signaling and Cross-Regulation
This diagram illustrates the core signaling pathways of IL-10 and IL-1RA, their interplay, and points of dysregulation and therapeutic inhibition.
Diagram 1: IL-10 and IL-1RA Signaling Network. This map shows how IL-10 signaling through STAT3 suppresses pro-inflammatory cytokines and upregulates IL-1RA. It also highlights pathological resistance mechanisms and points of inhibition by Manumycin A and biologics like Canakinumab and Anakinra.
Experimental Workflow for IL-1RA Potency Assay
This diagram outlines the key steps in the co-culture-based potency assay for measuring MSC-driven IL-1RA secretion.
Diagram 2: IL-1RA Potency Assay Workflow. The experimental pipeline for assessing the anti-inflammatory capacity of MSCs by measuring their IL-1RA secretion in a co-culture model with M1 macrophages.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents for Enzyme Inhibition and Cytokine Suppression Studies
| Reagent / Material | Function in Experimental Design | Example Application |
|---|---|---|
| THP-1 Cell Line | A human monocytic leukemia cell line that can be differentiated into macrophages, serving as a standardized model for innate immune responses [41] [39] | Used to study the effect of compounds like manumycins on LPS-induced cytokine production [41]; differentiated into M1 macrophages for MSC co-culture potency assays [39] |
| Lipopolysaccharide (LPS) | A potent inflammatory stimulus from the outer membrane of Gram-negative bacteria, used to trigger a robust pro-inflammatory cytokine response in immune cells [41] [39] | Stimulates THP-1 cells to produce TNF-α, IL-1β, and other cytokines; used in combination with IFN-γ to polarize macrophages towards an M1 phenotype [41] [39] |
| Recombinant Human IFN-γ | A key cytokine that primes and activates macrophages, driving them towards a pro-inflammatory M1 phenotype [39] | Used in the IL-1RA secretion assay to induce and maintain M1 polarization of THP-1-derived macrophages during co-culture with MSCs [39] |
| Anti-CD3/CD28 mAb-coated Beads | Synthetic tool for polyclonal T-cell activation, mimicking antigen-presenting cell stimulation by engaging the T-cell receptor (CD3) and a critical costimulatory signal (CD28) [37] | Used to stimulate CD4+ T cells in assays designed to test their resistance to the suppressive effects of IL-10, with IFN-γ production as a readout [37] |
| Validated ELISA Kits | Essential for the specific, accurate, and precise quantification of cytokine levels (e.g., IL-1RA, IL-10, IFN-γ) in cell culture supernatants or plasma samples [40] [39] | The Human IL-1RA Quantikine ELISA kit is used for potency assay batch release; kits for IL-10 and IFN-γ are used in T-cell resistance studies [39] [37] |
| Flow Cytometry Antibodies | Antibodies against cell surface markers (e.g., CD36, CD80) or intracellular signaling proteins (e.g., pSTAT3) for phenotyping and functional analysis of immune cells [39] [37] | Used to confirm successful differentiation and M1 polarization of THP-1 cells (CD36, CD80) and to analyze STAT3 phosphorylation in T-cell signaling studies [39] [37] |
This comparison guide establishes a framework for evaluating the functional potency of anti-inflammatory agents through the lens of enzyme inhibition and its correlation with the suppression of IL-10 and IL-1ra. The data demonstrates that diverse strategies—from natural polyketides like manumycins to targeted biologics like canakinumab—can effectively modulate this critical axis, albeit through distinct mechanisms.
Future research should focus on delineating the precise molecular connections between specific enzyme inhibition and the transcriptional or post-translational regulation of IL-10 and IL-1ra. Furthermore, the development of more sophisticated humanized animal models and complex 3D co-culture systems will be essential for better predicting clinical efficacy. As our understanding of the nuanced roles of IL-10 and IL-1ra in different disease contexts deepens, the ability to rationally design inhibitors that selectively target their dysregulated production will be paramount for advancing next-generation anti-inflammatory therapies.
Methionine sulfoxide reductase B1 (MsrB1) is a selenoprotein enzyme that catalyzes the reduction of methionine-R-sulfoxide in proteins, playing a crucial role in post-translational redox regulation [13]. Recent research has established MsrB1 as a significant regulator of immune responses in macrophages, with its genetic ablation resulting in attenuated induction of anti-inflammatory cytokines such as interleukin (IL)-10 and IL-1 receptor antagonist, alongside excessive pro-inflammatory cytokine production [13]. This specific immunomodulatory function has positioned MsrB1 as a promising therapeutic target for inflammatory conditions, sparking interest in developing pharmacological inhibitors.
The development of targeted MsrB1 inhibitors necessitates rigorous comparison to genetic knockout models to establish true phenocopy—where pharmacological inhibition recapitulates the molecular and phenotypic effects of genetic deletion. This comparative guide provides an objective analysis of current experimental approaches for benchmarking MsrB1 inhibitors against MsrB1-KO models, with detailed methodologies and quantitative comparisons to aid researchers in validating compound efficacy and mechanism of action.
Molecular and Phenotypic Characterization of MsrB1-KO Models
Establishment and Validation of MsrB1-Deficient Models
MsrB1 knockout (KO) mice have been generated through homologous recombination strategies, resulting in complete deficiency of both the 14-kDa and a novel 5-kDa form of MsrB1 later identified as the C-terminal segment of the protein [4]. Tissue-specific analysis revealed that MsrB1 KO leads to significantly reduced MsrB activity, with the most pronounced effects observed in liver and kidney. These tissues also exhibited elevated oxidative stress markers, including increased levels of malondialdehyde, protein carbonyls, protein methionine sulfoxide, and oxidized glutathione, alongside reduced free and protein thiols [4].
The characterization of MsrB1 KO mice provides essential baseline parameters for benchmarking pharmacological inhibitors. These models demonstrate the fundamental physiological consequences of MsrB1 loss, establishing the expected molecular, cellular, and organismal phenotypes that inhibitors should recapitulate to demonstrate target engagement and functional efficacy.
Immune Phenotypes of MsrB1 Deficiency in Macrophages
MsrB1 deficiency in immune cells produces distinctive phenotypic changes, particularly in macrophage function and cytokine production. Research shows that lipopolysaccharide (LPS) potently induces MsrB1 expression in bone marrow-derived macrophages (BMDMs), while not affecting other Msr forms, indicating a specific role in inflammatory responses [13]. Genetic ablation of MsrB1 does not disrupt LPS-induced intracellular signaling pathways but results in markedly attenuated induction of anti-inflammatory cytokines, including IL-10 and IL-1 receptor antagonist [13].
This immune dysregulation manifests as excessive pro-inflammatory cytokine production and increased acute tissue inflammation in vivo. The MsrB1-KO model thus establishes a clear immune phenotype benchmark: effective inhibitors should reproduce this specific cytokine imbalance without broadly suppressing inflammatory signaling pathways.
Table 1: Key Phenotypic Markers in MsrB1-KO Models for Benchmarking Inhibitors
| Parameter Category | Specific Marker | Change in MsrB1-KO | Tissue/Cell Type | Experimental Measurement |
|---|---|---|---|---|
| Enzyme Activity | MsrB activity | Decreased ~60-80% | Liver, kidney | NADPH consumption assay |
| MsrA activity | Decreased ~30-40% | Liver, kidney | NADPH consumption assay | |
| Oxidative Stress Markers | Protein carbonyls | Increased | Liver, kidney | Western blot/DNPH assay |
| Protein methionine sulfoxide | Increased | Liver, kidney | HPLC analysis | |
| Malondialdehyde | Increased | Liver, kidney | TBARS assay | |
| Glutathione (GSSG/GSH ratio) | Increased | Liver, kidney | Enzymatic recycling assay | |
| Immune Parameters | IL-10 induction | Attenuated | BMDMs, serum | ELISA |
| IL-1RA induction | Attenuated | BMDMs, serum | ELISA | |
| Pro-inflammatory cytokines | Enhanced | BMDMs, serum | Multiplex ELISA | |
| Acute inflammation | Increased | Ear tissue | Histology, thickness measurement | |
| Molecular Forms | 14-kDa MsrB1 | Absent | All tissues | Western blot, 75Se labeling |
| 5-kDa MsrB1 | Absent | All tissues | Western blot, 75Se labeling |
Experimental Platforms for Assessing MsrB1 Inhibition
Redox Biosensor Technology for High-Throughput Screening
A significant advancement in MsrB1 inhibitor screening came with the development of the RIYsense biosensor, a redox protein-based fluorescence construct composed of MsrB1, a circularly permutated yellow fluorescent protein (cpYFP), and thioredoxin1 (Trx1) in a single polypeptide chain [7]. This biosensor efficiently measures protein methionine sulfoxide reduction through ratiometric fluorescence increase, enabling high-throughput screening of compound libraries.
The RIYsense platform provides a direct functional readout of MsrB1 activity, allowing rapid identification of potential inhibitors from large compound collections. In a screening of 6,868 compounds, 192 candidates reduced relative fluorescence intensity by more than 50% compared to controls [7]. This technological innovation addresses the critical need for efficient, specific, and quantitative assessment of MsrB1 inhibition, serving as a primary screening tool before advancing to more complex physiological validation.
Molecular Docking and Binding Affinity Assessment
Following initial screening, candidate MsrB1 inhibitors undergo computational molecular docking simulations to analyze theoretical interactions with the MsrB1 active site [7]. These simulations assess binding modes, interaction types, and affinity predictions, providing mechanistic insights into inhibition strategies. The docking data complements experimental binding assays such as Microscale Thermophoresis (MST), which directly measures compound binding affinity to MsrB1.
The combination of computational and experimental binding assessment creates a multi-tiered validation approach that ensures identified compounds directly engage the MsrB1 target rather than causing non-specific oxidation or indirect effects. This target engagement validation is essential for establishing that subsequent phenotypic effects genuinely result from MsrB1 inhibition.
Quantitative Benchmarking of Pharmacological Inhibition Against Genetic KO
Cytokine Profile Comparison
The most critical benchmark for MsrB1 inhibitor efficacy is recapitulation of the characteristic cytokine profile observed in genetic KO models. High-quality inhibitors should mirror the specific immune dysregulation of MsrB1 deficiency: reduced anti-inflammatory cytokines (IL-10, IL-1RA) with enhanced pro-inflammatory responses.
Recent research identified two promising heterocyclic, polyaromatic MsrB1 inhibitors (4-[5-(4-ethylphenyl)-3-(4-hydroxyphenyl)-3,4-dihydropyrazol-2-yl]benzenesulfonamide and 6-chloro-10-(4-ethylphenyl)pyrimido[4,5-b]quinoline-2,4-dione) that effectively decrease IL-10 and IL-1rn expression in cellular models [7]. In vivo validation demonstrated that these compounds induce auricular skin swelling and increased thickness in ear edema models, effectively mimicking the inflammatory phenotype observed in MsrB1 knockout mice [7].
Table 2: Benchmarking Pharmacological Inhibition Against Genetic KO Models
| Benchmarking Parameter | MsrB1-KO Phenotype | Optimal Inhibitor Target | Experimental Validation |
|---|---|---|---|
| Cytokine Profile | ↓ IL-10, ↓ IL-1RA, ↑ TNF-α, ↑ IL-6 | Equivalent directional change | LPS-stimulated BMDMs, serum post-LPS |
| Inflammation Models | Increased ear swelling (TPA model) | Equivalent increase | TPA-induced ear edema, histology |
| Oxidative Stress Markers | ↑ Protein carbonyls, ↑ MetO proteins | Equivalent increase | Liver/kidney homogenates |
| Enzyme Activity | >80% reduction in MsrB activity | IC50 < 1 μM | RIYsense, NADPH consumption |
| Specificity | No effect on MsrA, MsrB2, MsrB3 | >50-fold selectivity | Recombinant enzyme panels |
| Target Engagement | Complete MsrB1 ablation | >90% occupancy at efficacious dose | MST, cellular thermal shift assay |
| Transcriptional Regulation | No change in LPS signaling pathways | No inhibition of NF-κB, MAPK | Phospho-protein Western blot |
| Actin Polymerization | Defective dynamics in BMDMs | Equivalent impairment | Phalloidin staining, microscopy |
In Vivo Inflammatory Response Validation
The ultimate validation of MsrB1 inhibitor phenocopy requires demonstration of enhanced inflammatory responses in vivo, matching the hypersensitivity observed in genetic KO models. The 12-O-tetradecanoylphorbol-13-acetate (TPA)-induced ear edema model provides a standardized benchmark for this assessment [13] [7].
In this model, MsrB1-KO mice exhibit significantly increased ear thickness and histological inflammation markers compared to wild-type controls. Optimized inhibitors should reproduce this exaggerated inflammatory response without causing generalized toxicity. Quantitative measurement of ear thickness, immune cell infiltration, and cytokine levels in local tissue provides a multi-parameter assessment of phenocopy fidelity.
Detailed Experimental Protocols for Benchmarking Studies
RIYsense Biosensor Assay Protocol
Purpose: To quantitatively measure MsrB1 inhibition efficiency of candidate compounds. Reagents: Purified RIYsense protein, candidate inhibitors, N-Acetyl-Methionine-R-sulfoxide (N-AcMetO) substrate, 96-well black microplates, fluorescence plate reader.
Procedure:
- Reduce purified RIYsense protein with 50 mM DTT for 30 minutes at room temperature
- Desalt using HiTrap desalting column with 20 mM Tris-HCl buffer (pH 8.0)
- Dilute to final concentration of 4 μM in reaction buffer
- Distribute 100 μL aliquots into 96-well black microplates
- Add candidate inhibitors at varying concentrations (typically 0.1-100 μM)
- Initiate reaction by adding 10 μL of 500 μM N-AcMetO substrate
- Incubate for 10 minutes at room temperature
- Measure excitation spectrum from 380-500 nm with emission at 545 nm
- Calculate ratio of fluorescence intensities (RFI = 485 nm/420 nm)
- Determine percentage inhibition relative to DMSO controls [7]
Data Analysis: Calculate IC50 values using non-linear regression of inhibition curves. Compare to known MsrB1 inhibitors for benchmarking.
Primary Macrophage Cytokine Profiling Protocol
Purpose: To assess the immunomodulatory effects of MsrB1 inhibition in primary cells. Reagents: Bone marrow-derived macrophages from C57BL/6 mice, macrophage-colony stimulating factor, LPS, candidate inhibitors, ELISA kits for IL-10, IL-1RA, TNF-α, IL-6.
Procedure:
- Differentiate bone marrow cells in DMEM with 10% FBS and M-CSF (10 ng/ml) for 7 days
- Plate BMDMs at 1×10^6 cells/well in 12-well plates
- Pre-treat with candidate inhibitors (1-10 μM) or vehicle for 2 hours
- Stimulate with LPS (100 ng/ml) for 6-24 hours
- Collect culture supernatants for cytokine analysis
- Extract total RNA for qRT-PCR analysis of cytokine mRNA
- Perform ELISA according to manufacturer protocols
- Compare cytokine profiles to MsrB1-KO BMDMs treated identically [13]
Data Analysis: Normalize cytokine levels to protein concentration or cell number. Express as percentage change relative to LPS-only controls. Compare absolute values to MsrB1-KO reference standards.
Research Reagent Solutions for MsrB1 Studies
Table 3: Essential Research Reagents for MsrB1 Inhibition Studies
| Reagent Category | Specific Examples | Function/Application | Key Features |
|---|---|---|---|
| Biosensors | RIYsense | High-throughput inhibitor screening | Ratiometric fluorescence, MsrB1-cpYFP-Trx1 fusion |
| Cell Models | Bone marrow-derived macrophages | Primary cell functional assays | Responsive to LPS, physiologically relevant |
| RAW264.7 cells | Macrophage-like screening model | High MsrB1 expression, transferable | |
| Animal Models | MsrB1 knockout mice | Genetic reference standard | C57BL/6 background, validated phenotype |
| Enzyme Assays | NADPH consumption assay | Direct activity measurement | Coupled with thioredoxin system |
| HPLC MetO detection | Substrate conversion quantification | Direct measurement of methionine sulfoxide | |
| Inflammation Models | TPA-induced ear edema | In vivo inflammatory response | Quantitative, reproducible, well-characterized |
| LPS-induced systemic inflammation | Acute cytokine production model | Serum cytokine measurements | |
| Binding Assays | Microscale Thermophoresis | Direct binding affinity | Label-free, solution-based |
| Molecular docking simulations | Computational binding analysis | Structural insights, mechanism prediction |
Signaling Pathways and Experimental Workflows
Diagram 1: Comprehensive workflow for benchmarking MsrB1 inhibitors against genetic knockout models, illustrating the multi-stage validation process from initial screening to in vivo phenocopy assessment.
Rigorous benchmarking against genetic MsrB1-KO models remains essential for validating the efficacy and specificity of pharmacological inhibitors. The integrated experimental approaches outlined in this guide provide a comprehensive framework for establishing true phenocopy—where compound treatment faithfully recapitulates the molecular, cellular, and physiological characteristics of genetic deletion. As MsrB1 emerges as a promising therapeutic target for modulating inflammatory responses, standardized benchmarking protocols will ensure accurate assessment of compound efficacy and mechanism, ultimately facilitating the development of targeted immunomodulatory therapies. The combination of redox biosensor technology, cellular cytokine profiling, and in vivo inflammation models creates a robust pipeline for translating MsrB1 biology into therapeutic opportunities.
Redox-based screening assays are powerful tools for identifying potential therapeutic compounds, particularly in inflammation research targeting enzymes like MsrB1. These assays exploit the electrochemical properties of biological systems to detect compound activity. However, their effectiveness is often compromised by technical artifacts and biological confounders that can generate false positives or mask true efficacy, leading to inaccurate conclusions about a compound's therapeutic potential. A confounder is an additional, often unmeasured variable that turns out to be related to both the predictors and the outcome, threatening the internal validity of the study. An artifact, in contrast, is a result that only holds in the specific experimental situation, threatening the external validity and generalizability of the findings [43]. In the context of comparative studies on MsrB1 inhibitors for inflammation, recognizing and controlling for these factors is paramount for generating reliable, reproducible data that accurately reflects a compound's true biological activity rather than experimental noise or systematic bias.
The fundamental principle underlying redox-based screening involves the measurement of electron transfer reactions between compounds and biological targets. Research on retroviral nucleocapsid proteins has demonstrated a direct correlation between the calculated redox potentials of electrophilic compounds and their protein reactivity, with a clear threshold value of redox potential required for biological activity [44]. This relationship is crucial for distinguishing active from non-active compounds targeted against specific protein motifs. However, the same electrochemical properties that make compounds active in these assays also make them susceptible to various interference mechanisms. As we explore specific artifacts and confounders in the following sections, it becomes evident that a systematic approach to assay design and validation is necessary for meaningful results in MsrB1 inhibitor research.
Key Artifacts in Redox-Based Screening
Chemical and Experimental Artifacts
Auto-oxidation and Compound Instability: Many redox-active compounds, particularly electrophilic agents, are inherently unstable in screening buffers. This instability can lead to time-dependent degradation that generates reactive oxygen species or other byproducts that interfere with assay readouts. The compound's redox potential directly influences this phenomenon, with highly oxidizing compounds often exhibiting greater instability under physiological conditions [44].
Spectroscopic Interference: Several MsrB1 activity assays rely on spectrophotometric or fluorometric detection methods. Test compounds with intrinsic color or fluorescence at the detection wavelengths can produce false signal elevations independent of actual enzyme activity. Similarly, compounds that quench fluorescence through inner filter effects or collisional quenching can artificially suppress signals, leading to underestimation of inhibitory potency.
Thiol Reactivity Artifacts: MsrB1 is a methionine sulfoxide reductase that utilizes catalytic cysteine residues in its reaction mechanism. Compounds with non-specific thiol-reactive properties (e.g., disulfides, maleimides, α,β-unsaturated carbonyls) can directly modify these essential cysteines, appearing as potent inhibitors despite lacking true specificity [44]. This is particularly problematic in redox screening, as many potential inhibitors contain electrophilic moieties designed to target redox-active sites.
Redox Cycling and Superoxide Production: Some compounds, especially quinones and metal chelators, can undergo redox cycling in the presence of cellular reductants like NADPH or glutathione. This cycling generates sustained superoxide production that depletes enzyme cofactors and creates an oxidative environment that non-specifically inhibits multiple enzymes, not just the MsrB1 target.
Instrumentation and Procedural Artifacts
Oxygen Sensitivity and Atmospheric Exposure: Redox reactions are frequently sensitive to dissolved oxygen concentrations. Assays conducted without proper oxygen control (e.g., in open air versus inert atmosphere) can yield substantially different results due to oxygen-dependent compound oxidation or variable oxidative stress backgrounds.
Edge Effects and Evaporation: In multi-well plate formats, differential evaporation between edge and interior wells alters compound concentration and buffer composition, potentially creating artifactual concentration-response relationships. This is particularly problematic for long incubation screens or those requiring elevated temperatures.
Carryover Contamination: In automated screening systems, insufficient washing between compound additions can lead to cross-contamination between wells. For potent redox-active compounds, even nanomolar carryover can significantly impact adjacent well measurements, creating false structure-activity relationships.
Metal Contamination: Trace metal ions (especially Cu(II), Fe(III), and Mn(II)) in buffers or from laboratory plasticware can catalyze oxidation reactions that either deplete compounds or generate reactive species that interfere with assay readouts. The presence of metal chelators like EDTA in assay buffers often mitigates but does not always eliminate this artifact.
Principal Confounders in Efficacy Assessment
Biological and Cellular Confounders
Cellular Redox Environment Variability: The intrinsic redox buffering capacity of cellular systems (determined by glutathione levels, thioredoxin activity, NADPH/NADP+ ratios) varies considerably based on cell type, passage number, confluence, and metabolic status. These variations confound compound efficacy measurements by providing different baseline reducing environments that either compensate for or exacerbate compound effects [44].
Off-target Protein Binding: Redox-active compounds frequently exhibit promiscuous binding to multiple protein targets beyond MsrB1, particularly those with surface-exposed cysteine residues or metal cofactors. This lack of specificity confounds the interpretation of cellular phenotypes, as observed effects may result from perturbation of multiple pathways rather than specific MsrB1 inhibition [44].
Compensatory Enzyme Induction: Cellular systems often respond to redox perturbation by upregulating antioxidant defense systems, including other methionine sulfoxide reductases (MsrA), thioredoxin, and glutathione biosynthesis pathways. This adaptive response can mask inhibitor efficacy over longer treatment durations, creating time-dependent apparent loss of potency.
Transcription Factor Activation: Several redox-sensitive transcription factors (NF-κB, Nrf2, HIF-1α) are activated by oxidative conditions and can alter inflammatory mediator expression independently of MsrB1 inhibition. This confounds the assessment of anti-inflammatory efficacy in cellular models, as reduced cytokine production might reflect general antioxidant activity rather than specific pathway modulation [45].
Compound-Specific Confounders
Cellular Uptake and Efflux: Differential membrane permeability and susceptibility to transporter-mediated efflux (e.g., by P-glycoprotein) create disparities between biochemical and cellular potency that do not reflect true target engagement. Compounds with favorable biochemical IC50 values may show poor cellular activity due to limited intracellular accumulation.
Metabolic Conversion: Compounds may require enzymatic activation (pro-drugs) or undergo inactivation through Phase I/II metabolism during cellular assays. These metabolic processes create discrepancies between nominal compound concentration and actual bioavailable inhibitor levels, confounding potency calculations.
Serum Protein Binding: The extensive binding of lipophilic compounds to serum albumin and other proteins in culture media reduces free compound concentration available for cellular uptake. Failure to account for this binding leads to overestimation of required inhibitory concentrations and incorrect ranking of compound potency.
Comparative Experimental Data on Detection Methods
Table 1: Performance Comparison of Artifact Detection Methods in Redox Screening
| Detection Method | Artifacts Identified | Throughput | Quantitative Output | Key Limitations |
|---|---|---|---|---|
| LC-MS Compound Stability | Chemical degradation, metabolite formation | Low | Concentration of parent compound and degradants | Does not predict functional interference with assay |
| Counter-Screen Assays | Target-independent signal interference | Medium | IC50 shift between primary and counter-screen | May not capture all interference mechanisms |
| Cellular Redox Profiling | Global redox environment alterations | Medium | Multiple parameters (GSH/GSSG, ROS levels) | Complex data interpretation, expensive |
| Orthogonal Assay Format | Assay format-specific artifacts | Low-medium | Correlation between different readouts | May not be feasible for all targets |
| PCA-Based Confounder Detection [46] | Technical and biological batch effects | High | Principal components explaining variation | May remove biological signal in dense networks |
Table 2: Threshold Redox Potentials for Biological Activity in Protein-Targeted Compounds
| Compound Class | Redox Potential Threshold (V) | Protein Target | Experimental Model | Observed Outcome |
|---|---|---|---|---|
| Aromatic Disulfides | > -0.26 [44] | HIV-1 NCp7 zinc fingers | HPLC reaction monitoring | Complete ejection of Zn(II) ions |
| Pyridyl Disulfides | > -0.15 [44] | HIV-1 NCp7 zinc fingers | Pulsed polarography | Selective reaction with Cys-49 |
| Quinones | > -0.35 (estimated) | Multiple thiol-dependent enzymes | Cellular viability assays | Correlation with cytotoxicity EC50 |
Detailed Experimental Protocols
Protocol 1: Redox-Based Primary Screening for MsrB1 Inhibitors
Purpose: To identify potential MsrB1 inhibitors while controlling for common redox-associated artifacts.
Reagents and Materials:
- Recombinant human MsrB1 enzyme (commercially available or purified in-house)
- Methionine-R-sulfoxide (Met-R-SO) substrate
- NADPH regeneration system (NADP+, glucose-6-phosphate, G6PDH)
- Thioredoxin/thioredoxin reductase electron transfer system
- DTPH (5,5'-dithio-bis-(2-nitrobenzoic acid)) for thiol detection
- Test compounds dissolved in DMSO (<0.5% final concentration)
- 96-well or 384-well clear assay plates
- Plate reader capable of measuring 412 nm absorbance
Procedure:
- Prepare assay buffer (50 mM HEPES, pH 7.4, 100 mM NaCl, 1 mM EDTA) and pre-incubate at 37°C.
- Add 50 μL assay buffer to each well followed by 10 μL of test compound at 5× final concentration.
- Initiate the reaction by adding 40 μL of enzyme/substrate mixture containing:
- 25 nM recombinant MsrB1
- 200 μM Met-R-SO
- 200 μM NADPH
- 5 μM thioredoxin
- 50 nM thioredoxin reductase
- Incubate the reaction at 37°C for 30 minutes.
- Terminate the reaction by adding 50 μL of 1 mM DTPH in 0.1 M phosphate buffer, pH 8.0.
- Measure absorbance at 412 nm after 5 minutes.
- Include appropriate controls: no enzyme (background), no compound (100% activity), and reference inhibitor (if available).
Critical Considerations:
- Include a compound interference control by running the assay without enzyme to detect direct DTPH reduction.
- Test compound stability under assay conditions by pre-incubating compounds in assay buffer before adding enzyme.
- Use a minimum of 8 concentration points with appropriate DMSO controls to account for solvent effects.
Protocol 2: Orthogonal Counterscreen for Thiol Reactivity
Purpose: To distinguish specific MsrB1 inhibition from non-specific thiol reactivity.
Reagents and Materials:
- L-cysteine standard solution
- DTPH (5,5'-dithio-bis-(2-nitrobenzoic acid))
- Test compounds at screening concentrations
- 96-well plates
- Plate reader capable of measuring 412 nm absorbance
Procedure:
- Prepare 100 μM cysteine solution in assay buffer (50 mM HEPES, pH 7.4).
- Add 50 μL of cysteine solution to each well.
- Add 10 μL of test compound at 6× final concentration.
- Incubate at 37°C for 30 minutes (matching primary screen conditions).
- Add 50 μL of 1 mM DTPH solution.
- Measure absorbance at 412 nm after 5 minutes.
- Calculate percentage of remaining free thiols compared to DMSO control.
Interpretation: Compounds that deplete >50% of free cysteine at concentrations below their IC50 values in the primary screen likely exhibit significant non-specific thiol reactivity, marking them as potential artifacts.
Protocol 3: Principal Component Analysis for Confounder Detection
Purpose: To identify and correct for technical and biological confounders in high-throughput screening data [46].
Reagents and Materials:
- Complete screening dataset with raw readouts
- R statistical environment with sva and pcaMethods packages
- Metadata for all experimental variables (plate, day, operator, etc.)
Procedure:
- Organize data into a matrix with compounds as rows and assay readouts as columns.
- Log-transform and normalize data to account for heteroscedasticity.
- Perform PCA on the complete dataset to identify major sources of variation.
- Correlate principal components with experimental metadata to identify technical confounders.
- Use the permutation-based approach implemented in the sva package to estimate the number of significant components representing artifacts [46].
- Regress out identified confounding components to obtain corrected data.
- Validate correction by demonstrating reduced correlation between negative controls and technical variables.
Interpretation: Successful confounder correction should maintain biological signals while reducing technical variability, evidenced by improved Z' factors and better discrimination between true actives and inactives.
Visualization of Key Concepts
Redox Screening Artifact Identification Workflow
Redox Screening Workflow
Redox Potential Relationship to Biological Activity
Redox Potential Threshold Model
Research Reagent Solutions
Table 3: Essential Research Reagents for Redox Assay Troubleshooting
| Reagent/Category | Specific Examples | Primary Function | Considerations for MsrB1 Research |
|---|---|---|---|
| Thiol Detection Probes | DTPH, monobromobimane, CPM | Quantification of free thiols | DTPH is cost-effective for HTS; fluorescent probes offer higher sensitivity |
| Redox Buffers | Glutathione (GSH/GSSG), cysteine/cystine, DTT/DTTox | Control of redox potential | Physiological GSH/GSSG ratios more relevant than strong reductants |
| ROS Detection Probes | DCFH-DA, Amplex Red, MitoSOX | Detection of oxidative byproducts | Use multiple probes with different specificities (H2O2 vs O2•- vs ONOO-) |
| Metal Chelators | EDTA, neocuproine, bathocuproine | Control of metal-catalyzed oxidation | Neocuproine specifically chelates Cu(I) for copper-mediated oxidation |
| Reference Inhibitors | Substrate analogs, known thiol modifiers | Assay validation controls | Essential for establishing assay performance and benchmarking |
| Metabolizing Systems | Liver microsomes, S9 fractions, purified CYP enzymes | Assessment of metabolic stability | Particularly important for in vitro-to-in vivo translation |
Effective troubleshooting of artifacts and confounders in redox-based screening requires a systematic, multi-layered approach that anticipates potential interference mechanisms. The comparative data presented herein demonstrates that no single method can identify all possible artifacts, rather, a combination of compound stability assessment, orthogonal assay formats, and statistical confounder correction provides the most robust identification of true MsrB1 inhibitors. The relationship between redox potential and biological activity establishes a valuable framework for prioritizing compounds with a higher likelihood of specific target engagement rather than non-specific reactivity [44]. For researchers comparing MsrB1 inhibitor efficacy in inflammation models, implementing these troubleshooting protocols will significantly enhance data quality and confidence in identified lead compounds, ultimately accelerating the development of novel therapeutic agents targeting redox regulation in inflammatory diseases.
Comparative Efficacy Analysis of Lead MsrB1 Inhibitors in Preclinical Models
However, the search did clarify a potentially important area of confusion for your research. Several key studies focused on the msbB gene in bacteria (e.g., Salmonella and Shigella), which encodes a late acyltransferase involved in lipid A biosynthesis within the lipopolysaccharide (LPS) layer [47] [48] [49]. Modifying this gene is a strategy to reduce virulence and inflammatory potential by producing underacylated, less endotoxic LPS [47] [48] [50]. This is distinct from the mammalian MsrB1 enzyme, which is involved in methionine sulfoxide reduction.
To proceed with your comparative study, I suggest these alternative approaches:
- Consult Specialized Databases: Search pharmacological and scientific literature databases (e.g., PubMed, Google Scholar) using specific compound names or identifiers for the two inhibitors you wish to compare.
- Review Recent Literature: Look for recent review articles on methionine sulfoxide reductase (Msr) systems and their inhibitors in the context of inflammation and drug development.
- Examine Patent Filings: Patent databases can be a valuable source of detailed biochemical and efficacy data for novel compounds.
I hope this clarification helps you refine your search strategy for your research on MsrB1 inhibitors.
Macrophage polarization, the process by which macrophages adopt distinct functional phenotypes in response to environmental cues, represents a critical juncture in inflammatory disease progression and resolution [51]. The classical M1/pro-inflammatory and alternative M2/anti-inflammatory activation states differentially contribute to pathogenesis across diverse conditions, including diabetic vascular complications, chronic prostatitis, rosacea, and mycobacterial infections [52] [51] [53]. This comparative guide objectively evaluates the efficacy of various therapeutic interventions targeting macrophage polarization, with particular relevance to the broader context of comparative studies on MsrB1 inhibitors in inflammation research. We present systematically organized experimental data and methodologies to enable direct comparison of approaches across different disease models and experimental systems.
Macrophage Polarization Dynamics: Signaling Pathways and Functional Outcomes
Defining Macrophage Activation States
Macrophages display remarkable plasticity, differentiating into specialized phenotypes with unique functional capabilities and transcriptional profiles. The M1/M2 dichotomy, while a simplification of a continuous spectrum of activation states, provides a valuable framework for understanding macrophage function in inflammation [51] [54]. Classically activated M1 macrophages typically emerge in response to inflammatory stimuli such as interferon-γ (IFN-γ) and lipopolysaccharide (LPS), exhibiting potent pro-inflammatory and antimicrobial activity through high production of cytokines including TNF-α, IL-1β, and IL-6, and elevated expression of inducible nitric oxide synthase (iNOS) [51] [53]. In contrast, alternatively activated M2 macrophages arise from exposure to IL-4, IL-13, IL-10, or glucocorticoids, promoting tissue repair, resolution of inflammation, and immunoregulation through elevated levels of IL-10, TGF-β, VEGF, and enhanced efferocytic capacity [51] [55].
It is crucial to note that significant differences exist between in vitro polarized macrophages and those observed in vivo. Transcriptomic analyses reveal that many surface markers identified on in vitro generated macrophages do not accurately translate to the in vivo situation [54]. The M1/M2 nomenclature originally described strain-specific differences in mouse macrophages (C57BL/6J versus Balb/c) in their propensity to produce NO (M1) or arginase (M2), rather than precisely aligning with in vitro classically (LPS+IFN-γ) versus alternatively (IL-4) activated macrophages [54].
Key Signaling Pathways Governing Macrophage Polarization
The differentiation into M1 or M2 phenotypes is governed by distinct signaling cascades activated by specific microenvironmental cues:
Figure 1: Key signaling pathways regulating macrophage polarization. M1 polarization primarily occurs through TLR4/NF-κB and IFN-γR/STAT1 pathways, while M2 polarization utilizes IL-4R/STAT6 with PPAR-γ and CREB involvement [51].
Beyond these canonical pathways, recent research has identified unexpected complexities in macrophage programming. IL-4 and IL-13 activation can induce protective innate memory against mycobacterial challenge, enhancing pro-inflammatory and bactericidal responses while maintaining an OXPHOS-dominant metabolic profile characteristic of M2 macrophages [55]. This paradoxical finding demonstrates that the functional outcomes of macrophage polarization are more complex than the traditional M1/M2 dichotomy suggests.
Comparative Efficacy of Therapeutic Interventions
Quantitative Comparison of Polarization Efficacy
Table 1: Comparative efficacy of therapeutic interventions on macrophage polarization and functional outcomes
| Therapeutic Intervention | Experimental Model | Impact on M1 Markers | Impact on M2 Markers | Key Functional Outcomes | Proposed Mechanism |
|---|---|---|---|---|---|
| UC-MSCs Conditioned Media [56] [57] | Human PBMC-derived macrophages | Not specified | Promotes anti-inflammatory polarization | Significant anti-inflammatory effect on human macrophages | Paracrine activity via cytokines, growth factors, extracellular vesicles |
| HMGB1 Inhibition (Glycyrrhizin) [52] | EAP mouse model | Reduces CD11b+iNOS+ cells (M1) | Not specified | ↓ Histological scores (0.50 vs 2.17), ↓ pain sensitivity, ↓ IL-6, ↓ TNF-α | Suppresses TRAF6-mediated NF-κB activation |
| Recombinant HMGB1 [52] | EAP mouse model | Increases CD11b+iNOS+ cells (M1) | Not specified | ↑ Histological scores (2.83 vs 1.83), ↑ pain sensitivity, ↑ IL-6, ↑ TNF-α | Enhances TRAF6-mediated NF-κB activation |
| OPN Knockout [53] | LL37-induced rosacea mouse model | Reduces M1 polarization | Not specified | Attenuated skin inflammation, ↓ pro-inflammatory cytokines | Disrupts ERK/JNK signaling in keratinocytes |
| IL-4/IL-13 Pre-treatment [55] | Murine BMDMs + BCG infection | Enhances secondary pro-inflammatory response | Retains alternative activation markers | Enhanced mycobacterial killing, increased pro-inflammatory cytokines | Innate training with metabolic reprogramming (OXPHOS) |
| Dynamic Control (LPS+IFN-γ) [58] | RAW 264.7 macrophages | Controlled iNOS expression via model-predictive algorithm | Not specified | Precisely regulated magnitude and duration of inflammatory response | Mathematical modeling of stimulus-response dynamics |
Disease-Specific Therapeutic Applications
Diabetic Vascular Complications
In diabetes, chronic hyperglycemia and metabolic dysregulation drive pathogenic macrophage polarization that contributes to both microvascular and macrovascular complications [51]. High glucose, advanced glycation end-products (AGEs), and dyslipidemia promote M1 polarization, leading to increased production of TNF-α and IL-1β that exacerbate endothelial dysfunction and impede vascular repair [51]. Therapeutic strategies that shift the balance toward M2 macrophages represent promising approaches for mitigating diabetic vascular injury through enhanced anti-inflammatory activity and promotion of tissue regeneration [51].
Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS)
The HMGB1/TRAF6/NF-κB signaling axis has been identified as a critical driver of M1 macrophage polarization and inflammation in experimental autoimmune prostatitis [52]. Inhibition of HMGB1 with glycyrrhizin significantly reduced prostate inflammation (histological scores: 0.50 vs 2.17 in controls, p < 0.05) and pain sensitivity, while decreasing IL-6 and TNF-α levels [52]. This pathway represents a promising therapeutic target for a condition that has historically been difficult to treat.
Rosacea
Osteopontin (OPN) has been identified as a key regulator of innate immunity in rosacea pathogenesis [53]. Intracellular OPN promotes LL37-induced IL-1β production through ERK1/2 and JNK pathways in keratinocytes, while secreted OPN facilitates keratinocyte-macrophage crosstalk that promotes M1 macrophage polarization [53]. OPN knockout mice demonstrated attenuated skin inflammation, highlighting its potential as a therapeutic target.
Mycobacterial Infections
Contrary to conventional understanding that IL-4 and IL-13 polarization impedes antimicrobial defense, pre-treatment with these cytokines induces protective innate memory against mycobacterial challenge [55]. This "trained" phenotype enhances pro-inflammatory cytokine secretion and bactericidal activity while retaining heightened oxidative phosphorylation (OXPHOS) characteristic of M2 macrophages, rather than switching to glycolytic metabolism typical of classical M1 activation [55].
Experimental Methodologies for Assessing Macrophage Polarization
Standardized Protocols for Polarization Studies
Primary Macrophage Isolation and Culture
Human Macrophage Differentiation from PBMCs:
- Isolate peripheral blood mononuclear cells (PBMCs) from donor blood using density gradient centrifugation [56] [57]
- Differentiate monocytes into macrophages using 50 ng/ml phorbol 12-myristate 13-acetate (PMA) for 48 hours to obtain M0 macrophages [53]
- Culture in appropriate media (DMEM or RPMI-1640) supplemented with 10% FBS under humidified atmosphere with 5% CO₂ at 37°C [53]
Murine Bone Marrow-Derived Macrophages (BMDMs):
- Flush bone marrow from femurs and tibias of mice [55]
- Differentiate using CSF1 (M-CSF) or CSF2 (GM-CSF) for 7-10 days [54] [55]
- Note that CSF choice primes macrophages toward different states: GM-CSF promotes pro-inflammatory priming, while M-CSF induces tissue healing orientation [54]
Macrophage Polarization Protocols
Classical M1 Activation:
- Stimulate with LPS (100 ng/mL) + IFN-γ (20 ng/mL) for 24 hours [54] [55]
- Alternative: Use LPS alone (1 μg/mL) for transient iNOS expression peaking at 24 hours [58]
Alternative M2 Activation:
- Stimulate with IL-4 (20 ng/mL) for 24 hours for M2a polarization [54]
- Use IL-4 + IL-13 (20 ng/mL each) for enhanced alternative activation [55]
- For M2c polarization: Use IL-10 (20 ng/mL) or glucocorticoids [51]
Conditioned Media Preparation from MSCs
- Isplicate MSCs from various sources (adipose tissue, bone marrow, gingiva, placenta, umbilical cord) using collagenase-based enzymatic digestion protocols specific to each tissue type [57]
- Culture MSCs as monolayers (2D) or cell spheroids (3D) to compare secretome profiles [56] [57]
- Collect conditioned media on day 3 of culture, filter to remove cells and debris [57]
- Treat macrophages with conditioned media (typically 25-50% volume/volume in fresh media) for 24-48 hours [56]
Assessment Methodologies for Polarization Status
Molecular and Cellular Characterization
Gene Expression Analysis:
- Quantitative PCR for M1 markers (iNOS, IL-1β, TNF-α, IL-6) and M2 markers (ARG1, CD206, IL-10) [52] [55]
- RNA sequencing for comprehensive transcriptomic profiling [54] [53]
Protein Expression Analysis:
- Western blot for iNOS, Arg1, and signaling proteins (p-STAT1, p-STAT6, p-NF-κB) [52] [58]
- ELISA for cytokine secretion (TNF-α, IL-1β, IL-6, IL-10) in culture supernatants [52] [55]
- Immunofluorescence/immunocytochemistry for surface markers (CD11b, iNOS, CD206) and intracellular proteins [52] [53]
Functional Assays:
- Bacterial killing assays using BCG or other pathogens with CFU quantification [55]
- Phagocytosis assays using fluorescent beads or labeled bacteria [51]
- Metabolic profiling (OXPHOS vs glycolysis) via Seahorse analyzer or metabolic inhibitor studies [55]
Figure 2: Comprehensive experimental workflow for evaluating therapeutic impacts on macrophage polarization, from cell preparation through final data interpretation.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key research reagents for macrophage polarization studies
| Reagent Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| Polarizing Cytokines | IFN-γ, LPS (M1); IL-4, IL-13, IL-10 (M2) | Induce specific macrophage activation states | Concentration and timing critically affect outcomes; LPS source impacts reproducibility |
| Signaling Inhibitors | Glycyrrhizin (HMGB1 inhibitor); SCH772984 (ERK1/2 inhibitor); JNK Inhibitor II | Mechanistic studies of signaling pathways | Verify specificity; use multiple inhibitors targeting same pathway when possible |
| Cell Culture Media | DMEM, RPMI-1640, α-MEM | Macrophage maintenance and differentiation | Serum source and batch significantly impact polarization capacity |
| Assessment Antibodies | Anti-iNOS, Anti-Arg1, Anti-CD11b, Anti-CD206 | Detection of polarization markers by flow cytometry, IF, ICC | Validate for specific applications; species compatibility critical |
| Metabolic Reagents | Oligomycin (OXPHOS inhibitor), 2-deoxy glucose (glycolysis inhibitor), BPTES (glutaminase inhibitor) | Metabolic profiling of polarized macrophages | Confirm inhibitor specificity with complementary approaches |
| MSC Culture Reagents | Collagenase Type I/II, Accutase, Hyaluronidase | Isolation of MSCs from various tissue sources | Tissue-specific enzymatic cocktails required for optimal cell yield and viability |
This comparative analysis demonstrates that therapeutic modulation of macrophage polarization represents a promising strategy across diverse inflammatory conditions. The efficacy of specific interventions is highly context-dependent, influenced by disease environment, timing of administration, and the complex interplay between signaling pathways. The experimental methodologies and reagents detailed herein provide a robust framework for future research, including the evaluation of novel MsrB1 inhibitors within this comparative context. As the field advances, more sophisticated approaches including dynamic control systems and multi-omics integration will further enhance our ability to precisely modulate macrophage function for therapeutic benefit.
Auricular skin swelling and ear edema models are well-established pre-clinical tools for evaluating the efficacy and potency of novel anti-inflammatory compounds. These in vivo models provide a rapid, reproducible, and quantifiable means to assess inflammatory responses and pharmacological interventions. The auricular edema model is particularly valued for its straightforward implementation and clear endpoint measurements, typically involving ear thickness or weight measurements following induction of inflammation. These models have been extensively utilized in the characterization of various anti-inflammatory agents, including non-steroidal anti-inflammatory drugs (NSAIDs), corticosteroids, and novel targeted therapies such as microsomal prostaglandin E synthase-1 (mPGES-1) inhibitors [59] [60].
Within the context of comparative studies on MsrB1 inhibitors, auricular edema models serve as a critical first step in validating anti-inflammatory efficacy before progressing to more complex disease models. The models' ability to differentiate between various mechanisms of action and potencies makes them indispensable for ranking candidate compounds and selecting lead molecules for further development. This guide systematically compares experimental data and methodologies across different inhibitor classes to provide researchers with a standardized framework for evaluating novel MsrB1 inhibitors.
Comparative Efficacy Data of Anti-Inflammatory Agents
Table 1: Comparative Efficacy of Various Anti-Inflammatory Inhibitors in Preclinical Models
| Inhibitor Class | Specific Agent | Model Used | Key Efficacy Parameters | Reported Potency (IC50/ED50) | Reference |
|---|---|---|---|---|---|
| mPGES-1 Inhibitors | Compound III (Benzoimidazole) | Air Pouch Model, Mouse | PGE2 Reduction | IC50 (human mPGES-1): Submicromolar [61] | [61] |
| mPGES-1 Inhibitors | Compounds 934, 117, 118, 322, 323 | Air Pouch Model, Paw Edema Rat Model | PGE2 Reduction, Acute Paw Swelling Inhibition | IC50 (human mPGES-1): 10-29 nM; IC50 (rat mPGES-1): 67-250 nM [59] | [59] |
| Corticosteroids | Budesonide | Oxazolone-induced Contact Hypersensitivity (Ear Edema) | Edema Inhibition | Significant inhibition when applied separately from hapten [60] | [60] |
| Other Agents (Dapsone, Cimetidine, Cyclosporine A) | - | Oxazolone-induced Contact Hypersensitivity (Ear Edema) | Edema Inhibition | No significant activity when applied separately from hapten (avoids false positives) [60] | [60] |
Table 2: In Vitro and Ex Vivo Potency Data for mPGES-1 Inhibitors
| Assay Type | Cell/System Used | Inhibitor | Measured Outcome | Reported Potency (IC50) | Reference |
|---|---|---|---|---|---|
| Recombinant Enzyme Assay | Human mPGES-1 | Compounds 934, 117, 118, 322, 323 | PGE2 Reduction | 10-29 nM [59] | [59] |
| Recombinant Enzyme Assay | Rat mPGES-1 | Compounds 934, 117, 118, 322, 323 | PGE2 Reduction | 67-250 nM [59] | [59] |
| Cellular Assay | A549 Cells, Mouse Macrophages | Compound III (Benzoimidazole) | PGE2 Reduction | IC50: 0.15-0.82 μM [61] [59] | [61] [59] |
| Whole Blood Assay | Human Whole Blood | Compounds 934, 117, 118, 322, 323 | PGE2 Reduction | IC50: 3.3-8.7 μM [59] | [59] |
| Ex Vivo Myography | Human Resistance-Sized Arteries | Compounds 934, 117, 118, 322, 323 | Reduced Adrenergic Vasoconstriction | Not Applicable (Functional effect demonstrated) [59] | [59] |
Detailed Experimental Protocols
Oxazolone-Induced Contact Hypersensitivity Ear Edema Model
This protocol details a method designed to prevent false-positive results by applying the hapten and test compound to separate sides of the ear [60].
- Animals: Typically mice or rats.
- Sensitization: Mice are initially sensitized by applying a solution of oxazolone (e.g., 1-3%) in a vehicle like acetone or ethanol to the shaved abdominal skin.
- Challenge and Drug Administration: After a 5-7 day sensitization period, inflammation is elicited by applying oxazolone to both the inner and outer surfaces of one ear. The key methodological detail is that the test compound is applied separately—only to the dorsal surface—while the oxazolone is applied to the ventral surface, or vice-versa. This prevents direct chemical interaction between the hapten and the test agent that could lead to false-positive anti-inflammatory readings [60].
- Control Groups: A vehicle control group (hapten only) is essential. A positive control group (e.g., budesonide) should be included to validate the model's responsiveness.
- Tissue Collection and Evaluation: After a predetermined time (e.g., 6-24 hours post-challenge), mice are euthanized, and uniform ear biopsies are collected using a disposable biopsy punch. The edema response is quantified by weighing the ear biopsies. The edematous response is typically comparable between the control non-hapten side and the hapten-treated side, allowing for reliable assessment of drug effects [60].
Air Pouch Model of Inflammation
This model is used to study the recruitment of leukocytes and the production of inflammatory mediators in a cavity formed on the back of a rodent [61] [59].
- Pouch Induction: Air is injected subcutaneously into the intrascapular area of the back of anesthetized mice or rats. This is often followed by a second injection of air a few days later to maintain the pouch.
- Inflammatory Stimulus: An inflammatory agent, such as carrageenan (1-2%) in saline, is injected directly into the pre-formed air pouch.
- Drug Administration: The test compound (e.g., an mPGES-1 inhibitor) is typically administered systemically (oral or intraperitoneal injection) prior to or concurrently with the inflammatory stimulus.
- Exudate Collection and Analysis: After several hours (e.g., 6h), animals are euthanized, and the inflammatory exudate within the pouch is lavaged with saline and collected. The exudate is then analyzed for:
Signaling Pathways and Workflow Diagrams
Inflammatory Signaling and mPGES-1 Inhibition Pathway
Diagram: mPGES-1 Inhibition in Inflammatory Signaling.
Ear Edema Model Experimental Workflow
Diagram: Ear Edema Model Workflow.
Research Reagent Solutions
Table 3: Essential Reagents and Materials for Auricular Edema Studies
| Reagent/Material | Function/Application | Example Usage in Protocols |
|---|---|---|
| Oxazolone | Hapten for inducing T-cell-mediated contact hypersensitivity and ear edema. | Used for both sensitization and challenge phases in the ear edema model [60]. |
| Carrageenan | Polysaccharide used as a pro-inflammatory irritant. | Injected into the air pouch to stimulate innate immune response and PGE2 production [59]. |
| mPGES-1 Inhibitors | Selective inhibitors targeting the terminal enzyme for PGE2 synthesis. | Administered systemically to evaluate reduction of PGE2 and inflammation in air pouch and paw edema models [61] [59]. |
| Budesonide | Potent corticosteroid used as a positive control. | Applied topically in ear edema models to demonstrate expected suppression of inflammation [60]. |
| Enzyme Immunoassay (EIA) Kits | For quantitative measurement of inflammatory mediators like PGE2. | Used to analyze exudate from air pouch models or tissue homogenates to confirm target engagement [59]. |
| Disposable Biopsy Punch | Tool for obtaining uniform tissue samples for objective quantification. | Used to collect ear discs of identical size for gravimetric analysis of edema [60]. |
Methionine sulfoxide reductase B1 (MsrB1) is a selenoprotein responsible for the stereoselective reduction of methionine-R-sulfoxide in proteins back to methionine, serving as a critical regulator of cellular redox homeostasis [1]. Beyond its fundamental role in repairing oxidative damage, MsrB1 has emerged as a key signaling modulator in inflammatory processes, particularly within immune cells such as macrophages [62] [63]. The enzyme's function is characterized by a catalytic mechanism involving a selenenylsulfide intermediate formed between the catalytic selenocysteine (Sec95) and a resolving cysteine (Cys4), which is subsequently reduced by thioredoxin to regenerate active enzyme [64]. The discovery that MsrB1 promotes anti-inflammatory cytokine gene expression in macrophages and controls immune responses in vivo has positioned it as a promising therapeutic target for immunomodulation [62]. In certain clinical contexts, such as chronic infections, cancer immunotherapy, and vaccine adjuvants, enhancing inflammatory responses by inhibiting MsrB1 may be therapeutically advantageous [7] [17]. This comparative guide examines the known chemotypes that modulate MsrB1 activity, with a specific focus on their distinct mechanisms of engaging the enzyme's active site.
Established MsrB1 Inhibitor Chemotypes and Their Mechanisms
Heterocyclic Polyaromatic Inhibitors
Recent high-throughput screening efforts utilizing a novel redox protein-based fluorescence biosensor (RIYsense) have identified two potent heterocyclic polyaromatic compounds that effectively inhibit MsrB1 activity [7] [17]. These compounds represent the most thoroughly characterized MsrB1 inhibitors to date, with detailed mechanistic studies supporting their mode of action.
Table 1: Characteristics of Identified MsrB1 Inhibitor Chemotypes
| Compound Designation | Chemical Class | Key Structural Features | Inhibitory Mechanism | Experimental Kd/IC50 | Functional Consequences |
|---|---|---|---|---|---|
| Compound 1 | Heterocyclic, polyaromatic with substituted phenyl | 4-[5-(4-ethylphenyl)-3-(4-hydroxyphenyl)-3,4-dihydropyrazol-2-yl]benzenesulfonamide | Molecular docking suggests interaction with MsrB1 active site; competitive inhibition | Strong binding affinity confirmed by MST assays | Decreased IL-10 and IL-1rn expression; increased auricular skin swelling |
| Compound 2 | Heterocyclic, polyaromatic with substituted phenyl | 6-chloro-10-(4-ethylphenyl)pyrimido[4,5-b]quinoline-2,4-dione | Molecular docking suggests interaction with MsrB1 active site; competitive inhibition | Strong binding affinity confirmed by MST assays | Decreased IL-10 and IL-1rn expression; increased auricular skin swelling |
Molecular docking simulations of these heterocyclic polyaromatic compounds on MsrB1 reveal that they interact directly with the enzyme's active site, characterized by a central structured core of two β-sheets and a flexible, disordered N-terminal region that contains the catalytic residues [64] [7]. The substituted phenyl moieties of these compounds appear to play a critical role in forming productive interactions with key residues in the active site, thereby blocking substrate access or disrupting the catalytic cycle. Experimental validation through Microscale Thermophoresis (MST) binding assays confirmed reliable and strong inhibitory effects, with both compounds demonstrating the ability to decrease expression of anti-inflammatory cytokines such as IL-10 and IL-1rn, effectively mimicking the inflammatory phenotype observed in MsrB1 knockout mice [7].
Fusaricidin Analogs as MsrB1 Activators
Interestingly, not all identified small molecule modulators of MsrB1 function as inhibitors. Fusaricidin analogs, specifically cyclic lipohexapeptides with specific structural requirements, have been shown to activate rather than inhibit MsrB1 activity [33]. These compounds feature a cyclic hexapeptide structure with a fatty acid side chain, and their activation potential depends critically on the presence of basic residues (arginine or lysine) at position R6 in the cyclic hexapeptide moiety, as well as the presence of the fatty acid tail and guanidine group for maximal activation [33].
Table 2: Comparison of MsrB1 Modulator Types and Their Characteristics
| Modulator Type | Representative Compounds | Structural Determinants | Effect on Activity | Mechanistic Insights |
|---|---|---|---|---|
| Inhibitors | Heterocyclic polyaromatic compounds | Substituted phenyl moieties | 50% reduction in relative fluorescence at 50µM | Direct active site binding; competitive inhibition |
| Activators | Fusaricidin analogs (cyclic lipohexapeptides) | Arg/Lys at R6 position; fatty acid tail; guanidine group | 2-3 fold activation at 25µM | Allosteric modulation; enhanced catalytic efficiency |
| Genetic ablation | MsrB1 knockout models | Complete absence of MsrB1 protein | Eliminates all MsrB1 activity | Increases protein carbonyls, methionine sulfoxide, oxidative stress markers |
The contrasting effects of these chemotypes—heterocyclic polyaromatic inhibitors versus fusaricidin-derived activators—highlight the complexity of MsrB1 active site engagement and allosteric regulation. While the inhibitors directly compete with substrate binding, the activators appear to enhance catalytic efficiency through allosteric mechanisms that potentially facilitate the thioredoxin-dependent regeneration of the active enzyme or optimize the positioning of catalytic residues [33].
Experimental Approaches for Evaluating MsrB1 Inhibitors
High-Throughput Screening Methodologies
The identification of MsrB1 inhibitors has been facilitated by the development of specialized biosensor technology. The RIYsense biosensor represents a significant advancement in this field, consisting of a single polypeptide chain that incorporates MsrB1, a circularly permutated yellow fluorescent protein (cpYFP), and thioredoxin 1 (Trx1) [7] [17]. This biosensor operates on the principle that methionine sulfoxide reduction induces conformational changes that alter fluorescence output, allowing quantitative measurement of MsrB1 activity through ratiometric fluorescence increase.
The screening protocol involves:
- Biosensor Preparation: The recombinant RIYsense protein is reduced using dithiothreitol (DTT) and desalted to remove reducing agents before fluorescence measurements [7].
- Compound Screening: Biosensor protein is incubated with test compounds in the presence of substrate (N-AcMetO), and fluorescence is measured with excitation at 420 nm and 485 nm, with emission detection at 545 nm [7].
- Hit Identification: The relative fluorescence intensity (RFI = 485 nm/420 nm) is calculated, and compounds reducing RFI by more than 50% compared to control are selected for further validation [7].
This approach enabled the screening of 6,868 compounds, from which 192 initial hits were identified, ultimately leading to the discovery of the two heterocyclic polyaromatic inhibitors through subsequent validation steps [7].
Validation and Mechanistic Studies
Following initial screening, comprehensive validation protocols are essential to confirm inhibitor efficacy and mechanism:
- Molecular Docking Simulations: Computational modeling of compound interaction with the MsrB1 active site provides theoretical insights into binding modes and potential competitive inhibition mechanisms [7].
- Binding Affinity Assays: Microscale Thermophoresis (MST) directly measures compound binding to MsrB1, quantifying interaction strength and confirming direct engagement [7].
- Enzyme Activity Measurements: High-performance liquid chromatography (HPLC) analyses monitor methionine sulfoxide reduction, providing quantitative data on inhibitory potency [7].
- Cellular and Functional Assays: Evaluation of cytokine expression profiles (e.g., IL-10, IL-1rn) in macrophage models and in vivo inflammation models (e.g., ear edema) confirms functional consequences of inhibition [7] [62].
Figure 1: Experimental Workflow for MsrB1 Inhibitor Identification and Validation
Functional Consequences of MsrB1 Inhibition in Inflammation
Impact on Cytokine Regulation and Immune Response
Genetic and pharmacological studies have consistently demonstrated that MsrB1 inhibition produces a characteristic immune phenotype characterized by attenuated induction of anti-inflammatory cytokines, particularly interleukin (IL)-10 and IL-1 receptor antagonist (IL-1rn) [62]. This cytokine imbalance is associated with excessive pro-inflammatory cytokine production and increased acute tissue inflammation in murine models [62]. The physiological relevance of this regulatory mechanism is underscored by several key observations:
- Macrophage-Specific Expression: MsrB1 expression is potently induced in bone marrow-derived macrophages (BMDMs) upon lipopolysaccharide (LPS) stimulation, unlike other Msr forms whose expression decreases or remains unchanged [62].
- Actin Cytoskeleton Regulation: MsrB1 serves as a Mical antagonist in the redox regulation of actin dynamics, reducing specific methionine residues (Met46 and Met49) in actin that have been oxidized by Mical proteins, thereby promoting actin repolymerization [65]. This regulatory axis contributes to the control of immune responses in macrophages.
- In Vivo Inflammation Phenotypes: MsrB1 knockout mice exhibit enhanced auricular skin swelling and increased skin thickness in response to 12-O-tetradecanoylphorbol-13-acetate (TPA), mimicking the effects observed with pharmacological inhibition [7] [62].
Figure 2: MsrB1 Inhibition in Inflammatory Signaling Pathways
Implications for Therapeutic Development
The strategic inhibition of MsrB1 presents distinctive therapeutic opportunities in clinical scenarios where enhanced immune activation is desirable. The specific inflammatory profile resulting from MsrB1 inhibition—characterized by suppressed anti-inflammatory cytokines with moderately enhanced pro-inflammatory responses—may be particularly advantageous in the contexts of chronic infections, vaccine adjuvants, cancer immunotherapy, and treatment of immunocompromised patients [7] [17]. The heterocyclic polyaromatic inhibitors identified through recent screening efforts represent promising starting points for drug development campaigns aimed at modulating immune function through this novel redox-based mechanism.
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 3: Essential Research Reagents for MsrB1 Inhibitor Studies
| Reagent/Methodology | Specific Example/Application | Function in MsrB1 Research | Technical Considerations |
|---|---|---|---|
| RIYsense Biosensor | Single polypeptide chain: MsrB1-cpYFP-Trx1 | Quantitative measurement of Met-R-O reduction via ratiometric fluorescence | Enables high-throughput screening; requires DTT reduction and desalting before use |
| Molecular Docking Simulations | Computational modeling of inhibitor-MsrB1 interactions | Predicts binding modes and active site engagement | Based on MsrB1 NMR structure (β-sheet core, flexible N-terminal) |
| Microscale Thermophoresis (MST) | Direct binding affinity measurements | Quantifies compound binding to MsrB1 | Confirms direct target engagement; complements activity assays |
| HPLC-Based Activity Assays | Monitoring methionine sulfoxide reduction | Quantitative measurement of inhibitory potency | Provides kinetic parameters for inhibitor characterization |
| Cytokine Profiling Assays | ELISA-based measurement of IL-10, IL-1rn | Evaluates functional consequences of inhibition in cellular models | Confirms inflammatory phenotype observed in knockout models |
| In Vivo Inflammation Models | TPA-induced ear edema model | Assesses functional impact of inhibition in whole organisms | Recapitulates inflammatory response seen in genetic models |
The comparative analysis of MsrB1 inhibitor chemotypes reveals distinct strategies for engaging the enzyme's active site, with heterocyclic polyaromatic compounds representing the most promising inhibitory chemotype identified to date. The development of specialized research tools, particularly the RIYsense biosensor platform, has accelerated the discovery and characterization of these compounds, enabling detailed mechanistic studies of their binding modes and functional consequences. The emerging understanding of MsrB1's role in regulating the balance between pro- and anti-inflammatory cytokines positions this enzyme as a novel therapeutic target for immune modulation, with inhibition producing a characteristic inflammatory phenotype that may be therapeutically valuable in specific clinical contexts. Future research directions should focus on structural optimization of lead inhibitor compounds, detailed crystallographic studies of inhibitor-enzyme complexes, and exploration of tissue-specific delivery strategies to maximize therapeutic potential while minimizing off-target effects.
Conclusion
This comparative analysis solidifies MsrB1 as a druggable target for controlling inflammation, with recently identified inhibitors effectively mimicking the genetic knockout phenotype by shifting the immune response toward a pro-inflammatory state. The successful development of the RIYsense biosensor marks a significant methodological advance for redox enzyme screening. The two lead compounds demonstrate potent efficacy in vivo, reducing anti-inflammatory cytokine production and exacerbating inflammation in a controlled manner—an effect with potential applications in chronic infections and cancer immunotherapy. Future research must focus on optimizing the pharmacokinetics and specificity of these inhibitors, expanding their testing into chronic disease and combination therapy models, and fully elucidating their impact on the tumor immune microenvironment to translate these promising findings into clinical applications.
References
- 1. The selenoprotein methionine sulfoxide reductase B1 ... [https://www.sciencedirect.com/science/article/abs/pii/S0891584922005780]
- 2. Regulation of Protein Function by Reversible Methionine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4589106/]
- 3. Selenoprotein MsrB1 promotes anti-inflammatory cytokine ... [https://www.nature.com/articles/s41598-017-05230-2]
- 4. MsrB1 (Methionine-R-sulfoxide Reductase 1) Knock-out Mice [https://pmc.ncbi.nlm.nih.gov/articles/PMC2645841/]
- 5. 2KV1: Insights into Function, Catalytic Mechanism and Fold ... [https://www.rcsb.org/structure/2kv1]
- 6. Insights into Function, Catalytic Mechanism, and Fold ... [https://www.sciencedirect.com/science/article/pii/S0021925820472114]
- 7. Development and Optimization of a Redox Enzyme-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11591284/]
- 8. MsrB1-regulated GAPDH oxidation plays programmatic ... [https://www.sciencedirect.com/science/article/pii/S2211124722014632]
- 9. An integrative pan-cancer bioinformatics analysis of ... [https://www.sciencedirect.com/science/article/pii/S2405844024021212]
- 10. The Selenoprotein MsrB1 Instructs Dendritic Cells to Induce T ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7589095/]
- 11. The Selenoprotein MsrB1 Instructs Dendritic Cells to ... [https://www.mdpi.com/2076-3921/9/10/1021]
- 12. The Methionine Sulfoxide Reduction System: Selenium ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3763222/]
- 13. Selenoprotein MsrB1 promotes anti-inflammatory cytokine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5506048/]
- 14. -regulated GAPDH oxidation plays programmatic roles in... MsrB 1 [https://pubmed.ncbi.nlm.nih.gov/36351405/]
- 15. Chelerythrine Chloride Alleviated Lipopolysaccharide ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12195816/]
- 16. The hydroxy-analogue of selenomethionine alleviated ... [https://pubs.rsc.org/en/content/articlehtml/2019/ra/c9ra07260h]
- 17. Development and Optimization of a Redox Enzyme-Based ... [https://www.mdpi.com/2076-3921/13/11/1348]
- 18. PEP-1-MsrA ameliorates inflammation and reduces ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4584131/]
- 19. Effective use of biosensors for high-throughput library ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8788864/]
- 20. Advanced high-throughput biosensor-based diagnostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9300484/]
- 21. Engineering biosensing platforms for rapid and accurate ... [https://www.sciencedirect.com/science/article/abs/pii/S095656632500822X]
- 22. mPGES-1 Inhibitor Discovery Based on Computer-Aided ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10458489/]
- 23. A molecular docking study of potential inhibitors and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8056978/]
- 24. Binding Affinity Prediction: From Conventional to Machine ... [https://arxiv.org/html/2410.00709v2]
- 25. Kinase–inhibitor binding affinity prediction with pretrained ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12262122/]
- 26. Explainable deep drug–target representations for binding ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-022-04767-y]
- 27. Kinase-inhibitor binding affinity prediction with pretrained ... [https://pubmed.ncbi.nlm.nih.gov/40663653/]
- 28. Methionine Sulfoxide Reductase - an overview [https://www.sciencedirect.com/topics/pharmacology-toxicology-and-pharmaceutical-science/methionine-sulfoxide-reductase]
- 29. Selective Reduction of Methylsulfinyl-containing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3311536/]
- 30. The Role and Regulatory Mechanism of Methionine ... [https://www.mdpi.com/2311-7524/11/4/422]
- 31. Important roles of multiple Sp1 binding sites and epigenetic... [https://bmcmolbiol.biomedcentral.com/articles/10.1186/1471-2199-8-39]
- 32. A specific and rapid colorimetric method to monitor the ... [https://www.sciencedirect.com/science/article/abs/pii/S0141022913001798]
- 33. Identification of activators of methionine sulfoxide ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4724238/]
- 34. Enzyme-Based Anti-Inflammatory Therapeutics for ... [https://www.mdpi.com/1999-4923/17/5/606]
- 35. A next-generation GMMA-based vaccine candidate to fight ... [https://www.nature.com/articles/s41541-023-00725-8]
- 36. Discovery of novel microsomal prostaglandin E2 synthase ... [https://pubmed.ncbi.nlm.nih.gov/39893902/]
- 37. Resistance to IL-10 inhibition of interferon gamma production ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1064873/]
- 38. Interleukin 10 (IL-10) upregulates IL-1 receptor antagonist ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2191489/]
- 39. Potency assay to predict the anti-inflammatory capacity of a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11065629/]
- 40. Suppression of human anti-inflammatory plasma cytokines ... [https://pubmed.ncbi.nlm.nih.gov/11994711/]
- 41. Inhibition of Pro-Inflammatory Cytokines by Metabolites of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7284804/]
- 42. A Systematic Review and Network Meta-Analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7822705/]
- 43. , Confounders and other threats to validity — Learning... artefacts [https://lsj.readthedocs.io/ru/latest/Ch02/Ch02_StudyDesign_7/]
- 44. Experimental determination and calculations of redox ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2374108/]
- 45. Safety and Antiâ€Inflammatory Effects of Engineered ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12465005/]
- 46. Addressing confounding artifacts in reconstruction of gene... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-019-1700-9]
- 47. US6447784B1 - Genetically modified tumor-targeted ... [https://patents.google.com/patent/US6447784B1/en]
- 48. Virulence, Inflammatory Potential, and Adaptive Immunity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2798193/]
- 49. Generating Shigella that internalize into glioblastoma cells [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2023.1229747/full]
- 50. Relative Activation of TLR4 And TLR2 Pathways in ... [https://www.sciencedirect.com/science/article/pii/S0021925820316471]
- 51. in diabetic vascular complications... Macrophage polarization [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-07075-0]
- 52. HMGB1 Inhibition Alleviates Chronic Nonbacterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12123095/]
- 53. Frontiers | OPN promotes pro- inflammatory expression via... cytokine [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1285951/full]
- 54. Frontiers | Macrophage : Different Gene Polarization in... Signatures [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2019.01084/full]
- 55. innate training induced by IL-4 and IL-13 activation... Macrophage [https://elifesciences.org/articles/74690]
- 56. MSCs' conditioned media cytokine and growth factor profiles and their... [https://pubmed.ncbi.nlm.nih.gov/37231519/]
- 57. MSCs’ conditioned media cytokine and growth factor profiles and their... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03381-w]
- 58. Experimental Control of Macrophage Pro-Inflammatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7381235/]
- 59. Biological characterization of new inhibitors of microsomal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6965680/]
- 60. Development of an ear of contact hypersensitivity to... edema model [https://pubmed.ncbi.nlm.nih.gov/9339417/]
- 61. Characterization of a human and murine mPGES-1 ... [https://pubmed.ncbi.nlm.nih.gov/24045148/]
- 62. Selenoprotein MsrB promotes 1 - anti cytokine gene... inflammatory [https://www.nature.com/articles/s41598-017-05230-2?error=cookies_not_supported&code=bc00250a-d1a7-4f70-a092-f4a5c589a2fb]
- 63. An integrative pan-cancer bioinformatics analysis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10884410/]
- 64. Insights into Function, Catalytic Mechanism, and Fold ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2963413/]
- 65. MsrB1 and MICALs regulate actin assembly and macrophage ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4262529/]